1. Introduction
Irritable bowel syndrome (IBS) is an intestinal functional disorder characterized by recurrent abdominal pain or discomfort in association with changes in consistency or frequency of stool (diarrhea or constipation). This definition is in line with the Rome III criteria, because the new criteria (Rome IV) have excluded this parameter. The natural history of the disease includes both periods of relapse and remission [
1,
2].
Although many studies have investigated IBS, the pathophysiology remains unclear and controversial. Several mechanisms have been extensively investigated ranging from inflammation and immunological involvement to dysbiosis, brain–gut interaction, genetic or dietary factors [
3,
4,
5,
6,
7]. Therapeutic management of IBS focuses on treatment to relieve symptoms, which is frequently unsatisfactory. Therefore, in addition to standard pharmacological treatment, alternative/integrative therapeutic approaches are needed.
One hypothesis is that overgrowth of certain bacteria in the gut can cause fermentation resulting in overproduction of gas, alteration of gastrointestinal motility and disruption of the mucosal barrier [
8,
9]. Considering this hypothesis, it would be possible to alleviate IBS symptoms in three ways: (1) Reducing the number of pathogenic bacteria using antibiotics [
10,
11]; (2) restoring intestinal homeostasis with probiotics [
12]; and (3) consuming a low- Fermentable, Oligo-, Di-, Monosaccharide and Polyol (FODMAP) diet which contributes to the relief of gastrointestinal symptoms by reducing fermentable nutrients in the colon, gas production and abdominal distension. However, sometimes this type of diet can be dangerous, because it can cause nutrient deficiency or reduce the amount of fiber that are the substrate for microbiome development [
13,
14].
However, there are some limitations of these treatment methods. Due to the risk of both side effects and development of resistance, antibiotics have not been extensively used for IBS. Moreover, antibiotic use is associated with a reduction in gut microbial species such as archaea and metanobacter, generally responsable for small intestinal bacterial overgrowth (SIBO). Nevertheless, rifaximin is an antibiotic with a grade 2 recommendation and level of evidence grade B in patients with diarrhea-IBS, likely because it acts primarily in the gut and has low bioavailability and poor absorption [
15]. Probiotics have a beneficial effect on the host by suppressing pathogens, producing bacteriocins and neurotransmitters and improving intestinal barrier function [
16].
IBS treatments include medication (antibiotics, antidiarrheal, laxatives, antispastics), nutraceuticals (probiotics, prebiotics, symbiotics), diet, lifestyle change or a combination of these methods. There are limited studies comparing the efficacy of different treatment methods in patients with IBS. Additionally, the efficacy of conventional antibiotic combined with diet or nutritional agents versus probiotic spores has not yet been investigated in these patients.
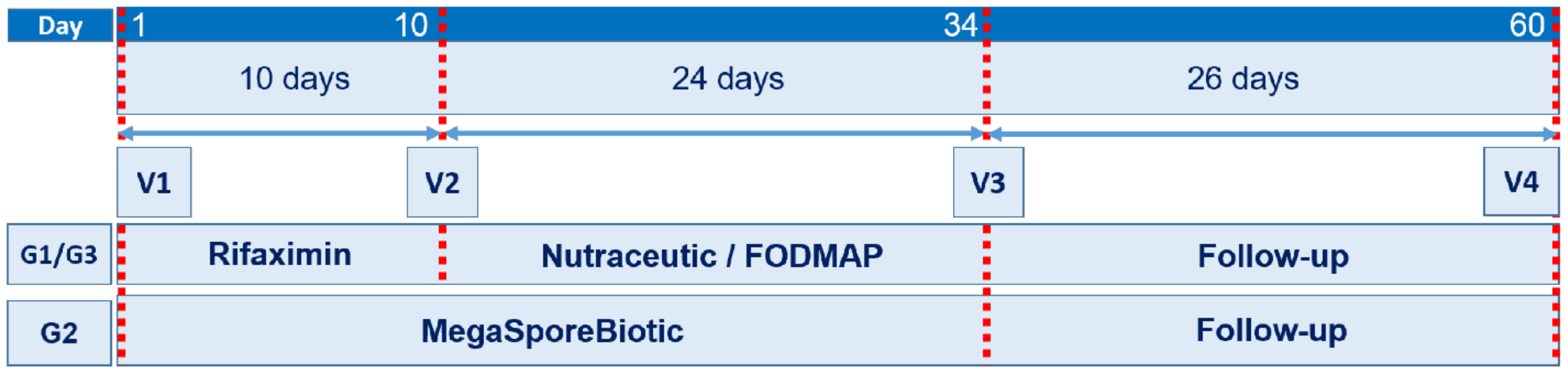
The aim of the current study was to compare the effects of short-term treatment (10 days) with rifaximin, followed by 24 days of low-FODMAP diet or treatment with a nutraceutical agent containing a combination of prebiotics, probiotics and vitamins, with the effects of long-term treatment (34 days) with MegaSporeBiotic (100% spore-based probiotic containing Bacillus licheniformis, Bacillus indicus HU36 ™, Bacillus subtilis HU58 ™, Bacillus clausii, Bacillus coagulans).
2. Materials and Methods
2.1. Study Design and Patients
This was a prospective, randomized controlled clinical study conducted in a single medical center in Romania. The study protocol was approved by the institutional review board of Iuliu Hațieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania (No. 18/2014), prior to patient recruitment. The study was conducted according to the principles of the Declaration of Helsinki of 1975, revised in 2013, and Good Clinical Practice guidelines.
2.2. Patients
Patients who presented with IBS at the Medical Center between March 2016 and March 2019 that met the inclusion criteria, did not meet the exclusion criteria and signed the informed consent were included in the study. The inclusion criteria were individuals diagnosed with non-constipation IBS based on Rome III criteria, no constipation, aged 18 to 75 years, normal colonoscopy in the last 5 years, blood counts within reference values and normal fecal calprotectin. We applied the Rome III criteria because we started the study before the Rome IV criteria were published (May 2016).
Patients with documented food allergies, gluten intolerance or celiac disease, diabetes, thyroid disease, intestinal inflammatory disease or other organic diseases, eating disorders (anorexia or bulimia), probiotics one month before the study, antibiotic treatment in the previous 6 months or those using specific diets (e.g., vegetarian) were excluded. Patients were not excluded if they had used diarrheal treatment, laxatives and/or antispasmodic medications; however, patients were required to discontinue such medications at study enrollment and signed the informed consent.
2.3. Intervention
Enrolled patients were randomly assigned to one of three study groups (G1, G2 and G3). G1 and G3 were treated for 10 days with rifaximin (1200 mg daily) followed by treatment with a nutraceutical agent (probiotic—
Bifidobacterium longum W11 in combination with prebiotics—soluble fiber and group B vitamins—B1, B2, B6, B12) (G1) or a low-FODMAP diet (G3). G2 received a spore-based probiotic formulation consisting of five
Bacillus spp. (MegaSporeBiotic, Microbiome Labs, St. Augustine, FL, USA) for 34 days (one capsule daily for the first 7 days followed by two capsules daily for 27 days). To increase the rate of eradication and extend the period of remission, treatment with rifaximin and a combination of probiotics or diet are recommended in patients with IBS [
17]. Patients in G1 and G3 were evaluated at baseline/first day of the study (V1), 10 days (V2), 34 days (V3) and 60 days (V4, end of study) after study initiation. Patients in G2 were evaluated at V1, V3 and V4 (
Figure 1).
2.4. Randomization
Patients were randomized equally (1:1:1) into each of the three groups. Each patient included in the study received their assigned treatment according to the schedule for a period of 2 months, treatment was initiated at (V1). This was an open-label study.
2.5. Measurements and Study Endpoints
2.5.1. IBS Severity Score (IBS-SS)
To determine the IBS severity score (IBS-SS), patients completed a questionnaire developed by Francis et al. [
18], which examined severity of abdominal pain, number of days with abdominal pain, distension and the impact of each on quality of life (QL). Each question had a score range from 0 (not at all impaired) to 100 (extremely impaired) and the questionnaire could have a total score of 0 to 500, with 500 being the highest possible IBS-SS score. Higher scores are correlated with greater severity of symptoms. Mild, moderate and severe cases are indicated by scores of 75–175, 175–300 and more than 300, respectively [
18].
2.5.2. Quality of Life for IBS Patients (IBS-QL)
Quality of life (QL) was evaluated using the irritable bowel syndrome questionnaire which has 36 items (SF-36). It measures the patient’s state of health on eight points: Functional status (physical and social functioning, physical and emotional problems), well-being (mental health, vitality and pain) and general health assessment (general perception of health) [
19,
20].
Both questionnaires (IBS-SS and IBS-QL) were completed by patients in the presence of apsychologist.
2.5.3. Rectal Volume Sensation Test
For the rectal volume sensation test we used a single use 8 channel anorectal catheter (4.9 mm 2300E, Mediplus, UK) with a universal thermoplastic balloon that expands from 60 to 400 mL attached to a Sandhill Insight manometry system. The patients received a sodium phosphate solution to clean the lower rectum before testing. Patients were placed in a left lateral position and the lubricated barista bag was slowly inserted into the rectum. Patients had 2–3 min to adapt, then the bag was progressively inflated with air. The thresholds for the first sensation of swollen balloon, tenesmus and discomfort were indicated by the patients. Every perceived sensation was correlated with sphincter relaxation. The balloon was inflated until the patient first reported pain [
21,
22]. The test was performed on all patients by the same medical team.
2.5.4. Statistical Analysis
IBM SPSS version 22 (IBM Corp., Armonk, NY, USA) software was used for statistical analyses. Descriptive statistics were calculated for all variables. Data are shown as mean ± standard deviation (SD). Intra- and intergroup differences before/during/after therapy were analyzed. For longitudinal intragroup comparisons between consecutive measurements in the same sample of patients, multiple paired-samples t-tests for dependent variables were used. ANOVA and Bonferroni post-hoc tests for independent variables were applied when comparisons were made between groups. The threshold for statistical significance was considered as p > 0.05.
4. Discussion
In this study we compared the effects of treatment with a spore-based probiotic mixture of five Bacillus spp. (MegaSporeBiotic) on IBS-SS, IBS-QL and rectal volume sensation in IBS patients to two standard treatment regimens for these patients: Rifaximin followed by a nutraceutical agent (Lactobacillus strain, prebiotics and vitamins) or rifaximin followed by a low-FODMAP diet.
Bacillus spp. are of particular interest to humans due to their tolerance of and ability to survive in environments of gastric acidity or the hostile environment of the intestine. These microorganisms are also important for other animals as growth regulators and for providing protection against diseases in aquaculture [
23]. Although
Bacillus spp. have a high biotherapeutic potential for production of antimicrobial peptides, production of additional vitamins (e.g., cobalamin, riboflavin) and for modulating the host microbiota, studies of this species as probiotics have only been on the rise over the past 10 years [
24]. Currently,
Bacillus spp. are some of the most studied and well-characterized probiotics; their use as probiotics expanding rapidly because of their inherent ability to form endospores [
25].
In our study, the mean IBS-SS ranged from 175 to 300 for all groups at V1. Thus, we can reasonably assume similar severity of disease in all groups (moderate disease) at the beginning of the study. IBS-SS decreased with each visit for all groups, all of the treatments tested had a positive impact on IBS-SS. Between groups (intergroup), significant difference were only observed at V3 (34 days). The results showed that treatment with
Bacillus spores (G2) attenuated the IBS-SS score better than rifaximin plus the nutraceutical agent (G1) and similarly to rifaximin plus a low-FODMAP diet (G3). If the IBS is linked to dysbiosis, our results demonstrate that
Bacillus spp. spore-based probiotics have the capacity to reduce gut dysbiosis to a similar degree as antibiotic treatment. The efficacy of rifaximin has been demonstrated in previous studies, but many of these were compared with placebo rather than a combination of treatments (rifaximin and other pharmacological or non-pharmacological agents) or with other therapies [
10,
26,
27]. The positive effect of a low-FODMAP diet on the severity score in patients with IBS has been demonstrated in meta-analyses [
28,
29]. The efficacy of this treatment to alleviate IBS symptoms could be explained by its impact on SIBO. This condition may be a cause of IBS [
30]. It is known that rifaximin is a clinically effective antibiotic in patients with SIBO, but rifaximin monotherapy may cause rapid relapse [
17]. For this reason, we recommended rifaximin and either a nutraceutical agent (G1) or a low-FODMAP diet (G3). Rifaximin destroys certain bacteria, while the nutraceutical agent and low-FODMAP diet stimulate the growth of “good” bacteria restoring the intestinal microbial balance. This could be considered reset–recovery effect of gut microbiota.
Bacillus spp. are spore forming bacteria and thus more resistant to passage through the upper digestive tract than other probiotics [
31]. Studies have shown that certain species of
Bacillus spores are capable of quorum sensing. Through quorum sensing, they exert an important regulatory effect on intestinal microbiota resulting in positive effects on both the colon and ileum [
32]. It is likely that the positive effect of MegaSporeBiotic is a consequence of both microbiota modulation and influence on the gut–brain axis through the intestinal enterochromaffin cells [
33]. Regarding QL, we monitored general health, physical functioning and physical role functioning; we observed a statistically significant difference for these parameters in V3 and V4. The results showed that after 34 days of treatment, the impact of
Bacillus spores on QL was superior to treatment with rifaximin combined with either a nutraceutical agent or a low-FODMAP diet.
Bacillus spp. have the capacity to produce more extracellular molecules than
Lactobacillus. This could explain the superior effect of MegaSporeBiotic observed in our study [
34].
The parameters evaluated using the rectal volume sensation test showed that rifaximin had a beneficial effect on all the measured parameters (FS, T and P), while the nutraceutical agent only had a beneficial effect on T and the low-FODMAP diet had an effect on FS and P. However, at 34 days (V3), all of the treatments tested had beneficial effects on all parameters of the rectal volume sensation test.
The FS parameter of the rectal volume sensation test and those related to QL have a high degree of subjectivity. The results reported in this study may be due to modulation of the microbiota and the influence of the gut–brain axis.