Energy Intake Requirements in Pregnancy
Abstract
1. Introduction
2. Overview of Energy Intake Requirements of Healthy Pregnancy
2.1. Definition of Energy Requirements
2.2. Energy Requirements in Pregnancy
3. Energy Requirements for Expenditure
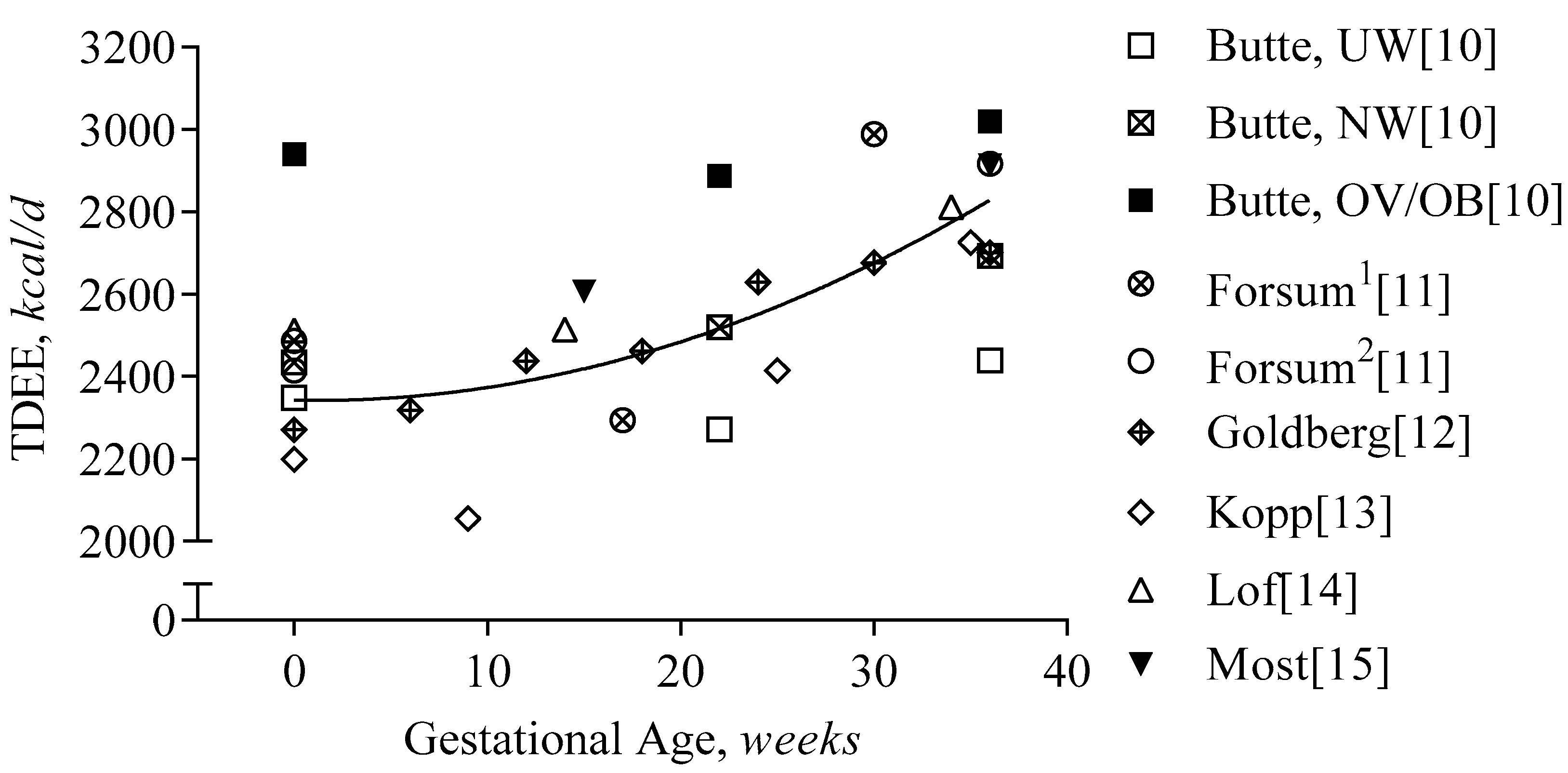
3.1. Total Energy Expenditure
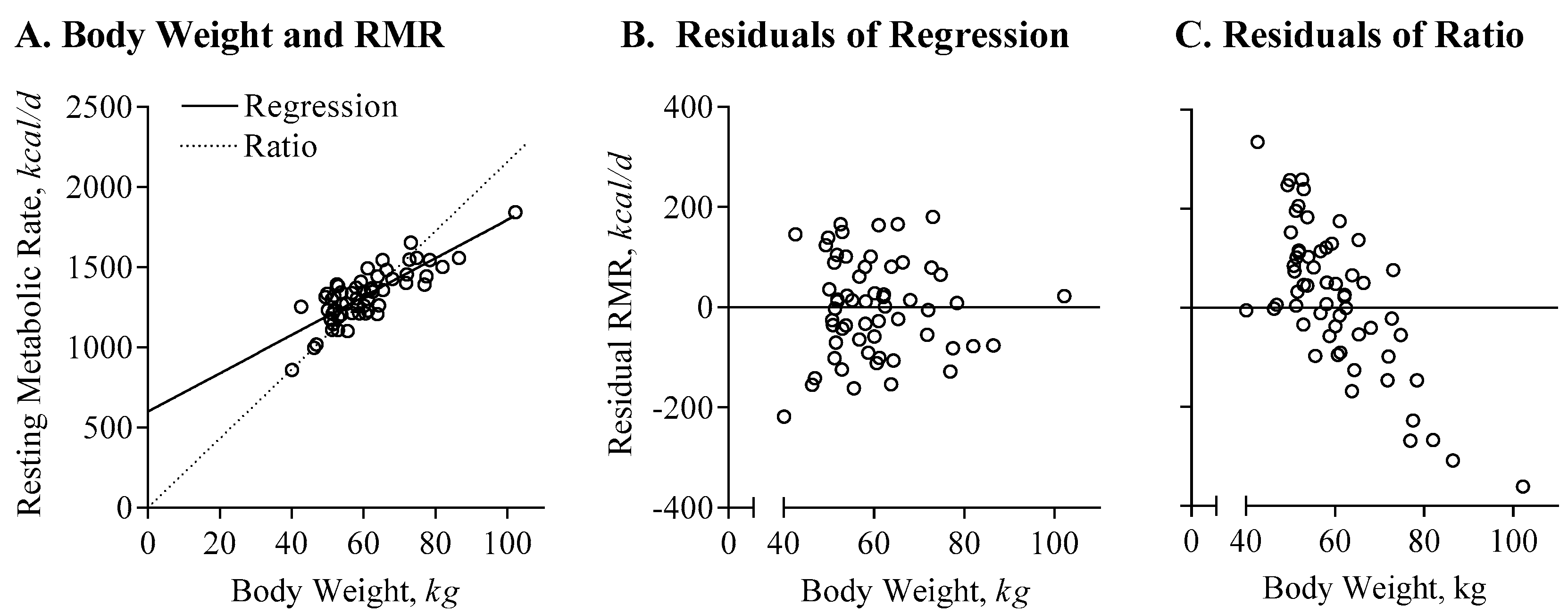
3.1.1. Appropriate Adjustment of Energy Expenditure Data
3.1.2. Measurement by Doubly Labeled Water
3.1.3. First Trimester
3.1.4. Second and Third Trimester
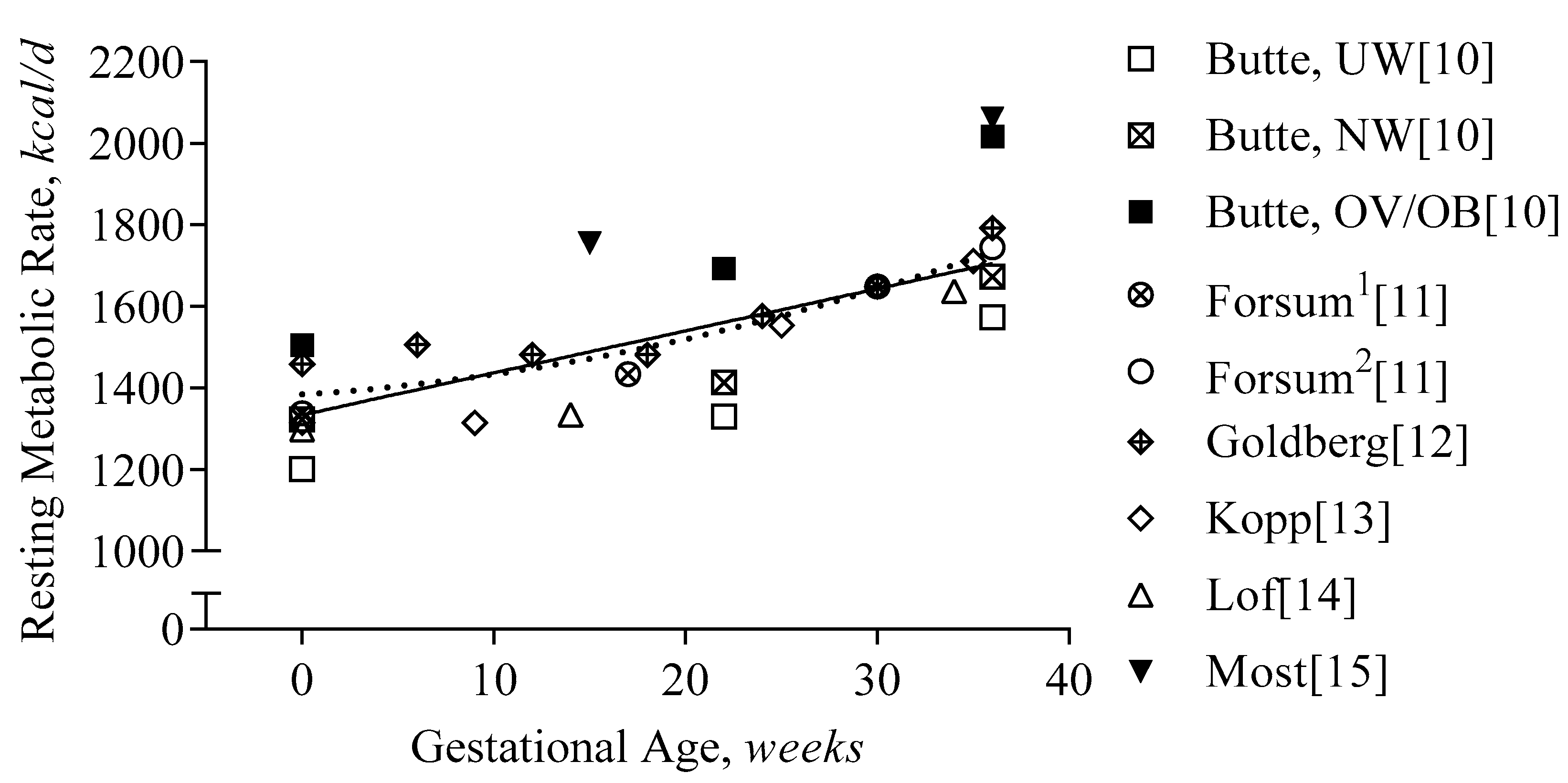
3.2. Basal Metabolism
3.2.1. Measurement by Indirect Calorimetry
3.2.2. First Trimester
3.2.3. Second and Third Trimester
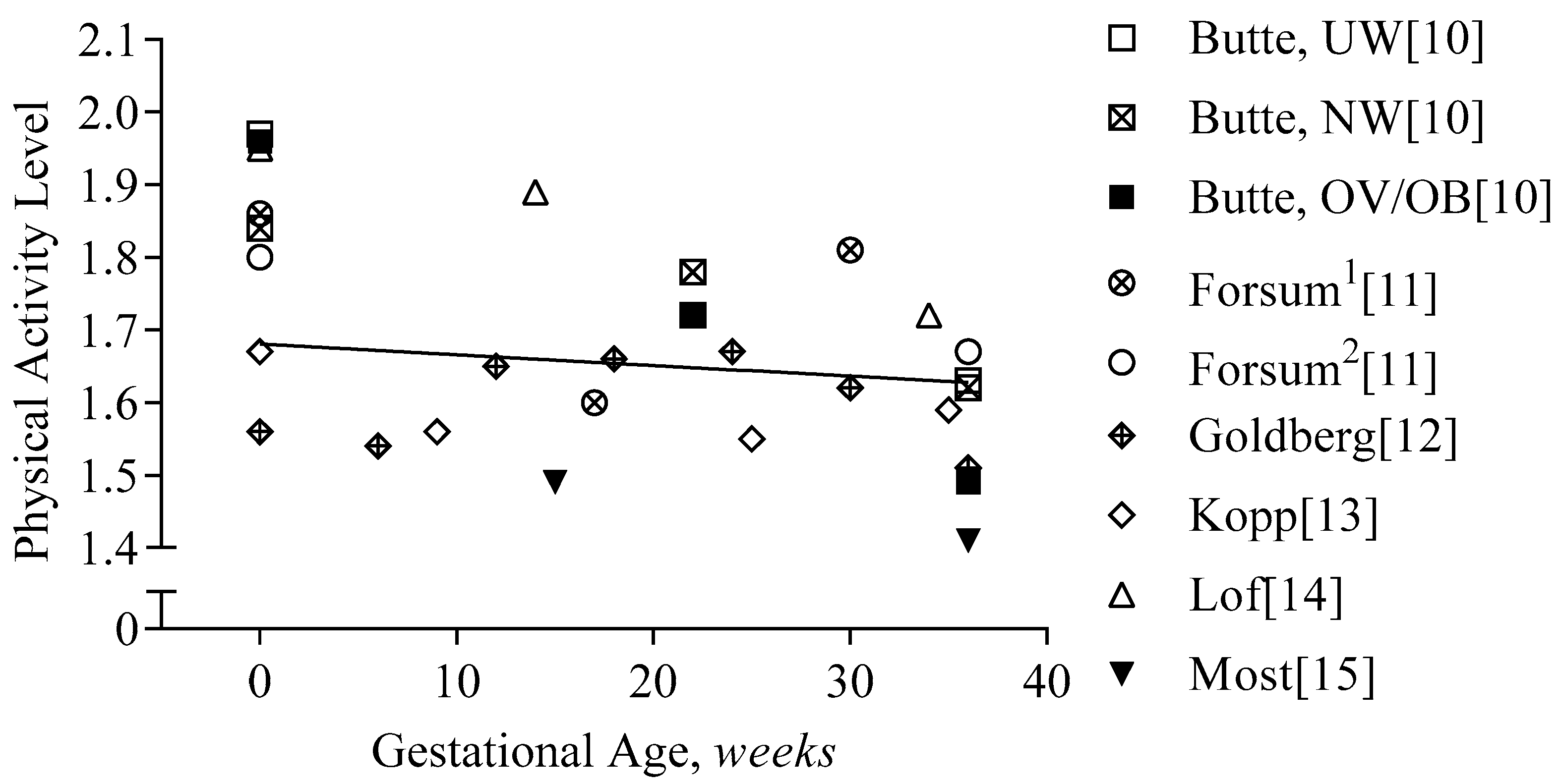
3.3. Physical Activity/Exercise
3.3.1. Measurement of Physical Activity
3.3.2. First Trimester
3.3.3. Second and Third Trimester
4. Energy Cost for Weight Gain
4.1. Determination of Appropriate Weight Gain and Composition
4.2. Measurement of Body Composition in Pregnancy
4.3. First Trimester
4.4. Second and Third Trimester
5. Models that Estimate Energy Intake Requirements
5.1. First Trimester
5.2. Second and Third Trimester
6. Limitations and Practical Considerations
6.1. First Trimester
6.2. Variability in Energy Expenditure
6.3. Communication of Recommendations
7. Summary
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Determining optimal weight gain. In Weight Gain during Pregnancy: Reexamining the Guidelines; Rasmussen, K.M., Yaktine, A.L., Eds.; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Kominiarek, M.A.; Peaceman, A.M. Gestational weight gain. Am. J. Obstet. Gynecol. 2017, 217, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, J.; Jaaskelainen, A.; Hartikainen, A.L.; Sovio, U.; Vaarasmaki, M.; Pouta, A.; Kaakinen, M.; Jarvelin, M.R. Maternal weight gain during the first half of pregnancy and offspring obesity at 16 years: A prospective cohort study. BJOG 2012, 119, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Catalano, P.M.; Farrell, K.; Thomas, A.; Huston-Presley, L.; Mencin, P.; de Mouzon, S.H.; Amini, S.B. Perinatal risk factors for childhood obesity and metabolic dysregulation. Am. J. Clin. Nutr. 2009, 90, 1303–1313. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, S.B.; Darbinian, J.; Ehrlich, S.F.; Markman, M.A.; Gunderson, E.P.; Ferrara, A.; Hedderson, M.M. Maternal gestational weight gain and offspring risk for childhood overweight or obesity. Am. J. Obstet. Gynecol. 2014, 211, 259.e1–259.e8. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, R.M.; Allan, K.M.; Raja, E.A.; Bhattacharya, S.; McNeill, G.; Hannaford, P.C.; Sarwar, N.; Lee, A.J.; Bhattacharya, S.; Norman, J.E. Maternal obesity during pregnancy and premature mortality from cardiovascular event in adult offspring: Follow-up of 1 323 275 person years. BMJ 2013, 347, f4539. [Google Scholar] [CrossRef] [PubMed]
- Mamun, A.A.; Kinarivala, M.; O’Callaghan, M.J.; Williams, G.M.; Najman, J.M.; Callaway, L.K. Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: Evidence from 21 y postpartum follow-up. Am. J. Clin. Nutr. 2010, 91, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Lederman, S.A.; Paxton, A.; Heymsfield, S.B.; Wang, J.; Thornton, J.; Pierson, R.N., Jr. Body fat and water changes during pregnancy in women with different body weight and weight gain. Obstet. Gynecol. 1997, 90, 483–488. [Google Scholar] [CrossRef]
- Flegal, K.M.; Kruszon-Moran, D.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Trends in obesity among adults in the united states, 2005 to 2014. JAMA 2016, 315, 2284–2291. [Google Scholar] [CrossRef]
- Butte, N.F.; Wong, W.W.; Treuth, M.S.; Ellis, K.J.; O’Brian Smith, E. Energy requirements during pregnancy based on total energy expenditure and energy deposition. Am. J. Clin. Nutr. 2004, 79, 1078–1087. [Google Scholar] [CrossRef]
- Forsum, E.; Kabir, N.; Sadurskis, A.; Westerterp, K. Total energy expenditure of healthy swedish women during pregnancy and lactation. Am. J. Clin. Nutr. 1992, 56, 334–342. [Google Scholar] [CrossRef]
- Goldberg, G.R.; Prentice, A.M.; Coward, W.A.; Davies, H.L.; Murgatroyd, P.R.; Wensing, C.; Black, A.E.; Harding, M.; Sawyer, M. Longitudinal assessment of energy expenditure in pregnancy by the doubly labeled water method. Am. J. Clin. Nutr. 1993, 57, 494–505. [Google Scholar] [CrossRef] [PubMed]
- Kopp-Hoolihan, L.E.; van Loan, M.D.; Wong, W.W.; King, J.C. Longitudinal assessment of energy balance in well-nourished, pregnant women. Am. J. Clin. Nutr. 1999, 69, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Lof, M.; Forsum, E. Activity pattern and energy expenditure due to physical activity before and during pregnancy in healthy swedish women. Br. J. Nutr. 2006, 95, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; St Amant, M.; Hsia, D.; Altazan, A.; Thomas, D.; Gilmore, A.; Vallo, P.; Beyl, R.; Ravussin, E.; Redman, L. Evidence-based recommendations for energy intake in pregnant women with obesity. J. Clin. Invest. 2019, 130. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Energy. In Dietary Reference Intake for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; The National Academies Press: Washington, DC, USA, 2005; pp. 107–264. [Google Scholar]
- Bracero, L.A.; Byrne, D.W. Optimal maternal weight gain during singleton pregnancy. Gynecol. Obstet. Investig. 1998, 46, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Cedergren, M.I. Optimal gestational weight gain for body mass index categories. Obstet. Gynecol. 2007, 110, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Nohr, E.A.; Vaeth, M.; Baker, J.L.; Sorensen, T.; Olsen, J.; Rasmussen, K.M. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am. J. Clin. Nutr. 2008, 87, 1750–1759. [Google Scholar] [CrossRef]
- Blomberg, M. Maternal and neonatal outcomes among obese women with weight gain below the new institute of medicine recommendations. Obstet. Gynecol. 2011, 117, 1065–1070. [Google Scholar] [CrossRef]
- Bodnar, L.M.; Pugh, S.J.; Lash, T.L.; Hutcheon, J.A.; Himes, K.P.; Parisi, S.M.; Abrams, B. Low gestational weight gain and risk of adverse perinatal outcomes in obese and severely obese women. Epidemiology 2016, 27, 894–902. [Google Scholar] [CrossRef]
- Bodnar, L.M.; Siminerio, L.L.; Himes, K.P.; Hutcheon, J.A.; Lash, T.L.; Parisi, S.M.; Abrams, B. Maternal obesity and gestational weight gain are risk factors for infant death. Obesity 2016, 24, 490–498. [Google Scholar] [CrossRef]
- Faucher, M.A.; Barger, M.K. Gestational weight gain in obese women by class of obesity and select maternal/newborn outcomes: A systematic review. Women Birth 2015, 28, e70–e79. [Google Scholar] [CrossRef] [PubMed]
- Robillard, P.Y.; Dekker, G.; Boukerrou, M.; Le Moullec, N.; Hulsey, T.C. Relationship between pre-pregnancy maternal bmi and optimal weight gain in singleton pregnancies. Heliyon 2018, 4, e00615. [Google Scholar] [CrossRef] [PubMed]
- Durie, D.E.; Thornburg, L.L.; Glantz, J.C. Effect of second-trimester and third-trimester rate of gestational weight gain on maternal and neonatal outcomes. Obstet. Gynecol. 2011, 118, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.; Eekhout, I.; Voerman, E.; Gaillard, R.; Barros, H.; Charles, M.A.; Chatzi, L.; Chevrier, C.; Chrousos, G.P.; Corpeleijn, E.; et al. Gestational weight gain charts for different body mass index groups for women in europe, north america, and oceania. BMC Med. 2018, 16, 201. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Redman, L.M. Does energy expenditure influence body fat accumulation in pregnancy? Am. J. Obstet. Gynecol. 2019, 220, 119–120. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Vallo, P.M.; Gilmore, L.A.; St Amant, M.; Hsia, D.S.; Altazan, A.D.; Beyl, R.A.; Ravussin, E.; Redman, L.M. Energy expenditure in pregnant women with obesity does not support energy intake recommendations. Obesity 2018, 26, 992–999. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. Assessment of Body Composition and Total Energy Expenditure in Humans Using Stable Isotope Techniques; IAEA: Vienna, Austria, 2009. [Google Scholar]
- Black, A.E.; Prentice, A.M.; Coward, W.A. Use of food quotients to predict respiratory quotients for the doubly-labelled water method of measuring energy expenditure. Hum. Nutr. Clin. Nutr. 1986, 40, 381–391. [Google Scholar] [PubMed]
- Gilmore, L.A.; Butte, N.F.; Ravussin, E.; Han, H.; Burton, J.H.; Redman, L.M. Energy intake and energy expenditure for determining excess weight gain in pregnant women. Obstet. Gynecol. 2016, 127, 884–892. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, L.A.; Ravussin, E.; Bray, G.A.; Han, H.; Redman, L.M. An objective estimate of energy intake during weight gain using the intake-balance method. Am. J. Clin. Nutr. 2014, 100, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Gilmore, L.A.; Altazan, A.D.; St Amant, M.; Beyl, R.A.; Ravussin, E.; Redman, L.M. Propensity for adverse pregnancy outcomes in african-american women may be explained by low energy expenditure in early pregnancy. Am. J. Clin. Nutr. 2018, 107, 957–964. [Google Scholar] [CrossRef]
- Thomas, D.M.; Navarro-Barrientos, J.E.; Rivera, D.E.; Heymsfield, S.B.; Bredlau, C.; Redman, L.M.; Martin, C.K.; Lederman, S.A.; Linda, M.C.; Butte, N.F. Dynamic energy-balance model predicting gestational weight gain. Am. J. Clin. Nutr. 2012, 95, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Broskey, N.T.; Altazan, A.D.; Beyl, R.A.; St Amant, M.; Hsia, D.S.; Ravussin, E.; Redman, L.M. Is energy balance in pregnancy involved in the etiology of gestational diabetes in women with obesity? Cell Metab. 2019, 29, 231–233. [Google Scholar] [CrossRef] [PubMed]
- Heini, A.; Schutz, Y.; Diaz, E.; Prentice, A.M.; Whitehead, R.G.; Jequier, E. Free-living energy expenditure measured by two independent techniques in pregnant and nonpregnant gambian women. Am. J. Physiol. 1991, 261, E9–E17. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Prentice, A.M.; Diaz, E.; Coward, W.A.; Ashford, J.; Sawyer, M.; Whitehead, R.G. Energy expenditure of gambian women during peak agricultural activity measured by the doubly-labelled water method. Br. J. Nutr. 1989, 62, 315–329. [Google Scholar] [CrossRef] [PubMed]
- Lof, M. Physical activity pattern and activity energy expenditure in healthy pregnant and non-pregnant swedish women. Eur. J. Clin. Nutr. 2011, 65, 1295–1301. [Google Scholar] [CrossRef] [PubMed]
- Gradmark, A.; Pomeroy, J.; Renstrom, F.; Steiginga, S.; Persson, M.; Wright, A.; Bluck, L.; Domellof, M.; Kahn, S.E.; Mogren, I.; et al. Physical activity, sedentary behaviors, and estimated insulin sensitivity and secretion in pregnant and non-pregnant women. BMC Pregnancy Childbirth 2011, 11, 44. [Google Scholar] [CrossRef] [PubMed]
- Diem, K. Metabolisme basal. In Tables Scientifiques; Geigy, J.R.S.A., Ed.; Departement Pharmaceutique: Basel, Switzerland, 1963; Volume 6, pp. 637–643. [Google Scholar]
- Sparks, J.W.; Girard, J.R.; Battaglia, F.C. An estimate of the caloric requirements of the human fetus. Neonatology 1980, 38, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Lam, Y.Y.; Ravussin, E. Analysis of energy metabolism in humans: A review of methodologies. Mol. Metab. 2016, 5, 1057–1071. [Google Scholar] [CrossRef] [PubMed]
- Meah, V.L.; Cockcroft, J.R.; Backx, K.; Shave, R.; Stohr, E.J. Cardiac output and related haemodynamics during pregnancy: A series of meta-analyses. Heart 2016, 102, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Napso, T.; Yong, H.E.J.; Lopez-Tello, J.; Sferruzzi-Perri, A.N. The role of placental hormones in mediating maternal adaptations to support pregnancy and lactation. Front. Physiol. 2018, 9, 1091. [Google Scholar] [CrossRef]
- Mottola, M.F. Physical activity and maternal obesity: Cardiovascular adaptations, exercise recommendations, and pregnancy outcomes. Nutr. Rev. 2013, 71 (Suppl. 1), S31–S36. [Google Scholar] [CrossRef]
- Ferraro, Z.M.; Contador, F.; Tawfiq, A.; Adamo, K.B.; Gaudet, L. Gestational weight gain and medical outcomes of pregnancy. Obstet. Med. 2015, 8, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Davenport, M.H.; Sobierajski, F.; Mottola, M.F.; Skow, R.J.; Meah, V.L.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Riske, L.; et al. Glucose responses to acute and chronic exercise during pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1357–1366. [Google Scholar] [CrossRef] [PubMed]
- Ruchat, S.M.; Mottola, M.F.; Skow, R.J.; Nagpal, T.S.; Meah, V.L.; James, M.; Riske, L.; Sobierajski, F.; Kathol, A.J.; Marchand, A.A.; et al. Effectiveness of exercise interventions in the prevention of excessive gestational weight gain and postpartum weight retention: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C.; et al. Physical activity and public health. A recommendation from the centers for disease control and prevention and the american college of sports medicine. JAMA 1995, 273, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, B. Acsm’s guidelines for exercise testing and prescription 9th ed. 2014. J. Can. Chiropr. Assoc. 2014, 58, 328. [Google Scholar]
- Lauer, E.E.; Jackson, A.W.; Martin, S.B.; Morrow, J.R., Jr. Meeting usdhhs physical activity guidelines and health outcomes. Int. J. Exerc. Sci. 2017, 10, 121–127. [Google Scholar] [PubMed]
- Davenport, M.H.; Ruchat, S.M.; Mottola, M.F.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Garcia, A.J.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 canadian guideline for physical activity throughout pregnancy: Methodology. J. Obstet. Gynaecol. Can. 2018, 40, 1468–1483. [Google Scholar] [CrossRef] [PubMed]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.-M.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 canadian guideline for physical activity throughout pregnancy. Br. J. Sports Med. 2018, 52, 1339. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro Santos, P.C.; Abreu, S.; Moreira, C.; Lopes, D.; Santos, R.; Alves, O.; Silva, P.; Montenegro, N.; Mota, J. Impact of compliance with different guidelines on physical activity during pregnancy and perceived barriers to leisure physical activity. J. Sports Sci. 2014, 32, 1398–1408. [Google Scholar] [CrossRef]
- Hesketh, K.R.; Evenson, K.R. Prevalence of us pregnant women meeting 2015 acog physical activity guidelines. Am. J. Prev. Med. 2016, 51, e87–e89. [Google Scholar] [CrossRef] [PubMed]
- Di Fabio, D.R.; Blomme, C.K.; Smith, K.M.; Welk, G.J.; Campbell, C.G. Adherence to physical activity guidelines in mid-pregnancy does not reduce sedentary time: An observational study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 27. [Google Scholar] [CrossRef] [PubMed]
- Hayman, M.; Short, C.; Reaburn, P. An investigation into the exercise behaviours of regionally based australian pregnant women. J. Sci. Med. Sport 2016, 19, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.M.; Campbell, C.G. Physical activity during pregnancy: Impact of applying different physical activity guidelines. J. Pregnancy 2013, 2013, 165617. [Google Scholar] [CrossRef] [PubMed]
- Renault, K.M.; Norgaard, K.; Nilas, L.; Carlsen, E.M.; Cortes, D.; Pryds, O.; Secher, N.J. The treatment of obese pregnant women (top) study: A randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am. J. Obstet. Gynecol. 2014, 210, 134.e1–134.e9. [Google Scholar] [CrossRef] [PubMed]
- Medek, H.; Halldorsson, T.; Gunnarsdottir, I.; Geirsson, R.T. Physical activity of relatively high intensity in mid-pregnancy predicts lower glucose tolerance levels. Acta Obstet. Gynecol. Scand. 2016, 95, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Renault, K.M.; Carlsen, E.M.; Haedersdal, S.; Nilas, L.; Secher, N.J.; Eugen-Olsen, J.; Cortes, D.; Olsen, S.F.; Halldorsson, T.I.; Norgaard, K. Impact of lifestyle intervention for obese women during pregnancy on maternal metabolic and inflammatory markers. Int. J. Obes. 2017, 41, 598–605. [Google Scholar] [CrossRef]
- Kraal, J.J.; Sartor, F.; Papini, G.; Stut, W.; Peek, N.; Kemps, H.M.; Bonomi, A.G. Energy expenditure estimation in beta-blocker-medicated cardiac patients by combining heart rate and body movement data. Eur. J. Prev. Cardiol. 2016, 23, 1734–1742. [Google Scholar] [CrossRef]
- Kim, D.; Cho, J.; Oh, H.; Chee, Y.; Kim, I. The estimation method of physical activity energy expenditure considering heart rate variability. In Proceedings of the 2009 36th Annual Computers in Cardiology Conference (CinC), Park City, UT, USA, 13–16 September 2009; pp. 413–416. [Google Scholar]
- Chasan-Taber, L.; Schmidt, M.D.; Roberts, D.E.; Hosmer, D.; Markenson, G.; Freedson, P.S. Development and validation of a pregnancy physical activity questionnaire. Med. Sci. Sports Exerc. 2004, 36, 1750–1760. [Google Scholar] [CrossRef]
- Ara, I.; Aparicio-Ugarriza, R.; Morales-Barco, D.; Nascimento de Souza, W.; Mata, E.; Gonzalez-Gross, M. Physical activity assessment in the general population; validated self-report methods. Nutr. Hosp. 2015, 31 (Suppl. 3), 211–218. [Google Scholar]
- Bell, R.; Tennant, P.W.; McParlin, C.; Pearce, M.S.; Adamson, A.J.; Rankin, J.; Robson, S.C. Measuring physical activity in pregnancy: A comparison of accelerometry and self-completion questionnaires in overweight and obese women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.L.; Thompson, R.G.; Teede, H.J.; Lombard, C.B. Measuring physical activity during pregnancy. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Brett, K.E.; Wilson, S.; Ferraro, Z.M.; Adamo, K.B. Self-report pregnancy physical activity questionnaire overestimates physical activity. Can. J. Public Health 2015, 106, e297–e302. [Google Scholar] [CrossRef] [PubMed]
- Lemmens, P.M.C.; Sartor, F.; Cox, L.G.E.; den Boer, S.V.; Westerink, J. Evaluation of an activity monitor for use in pregnancy to help reduce excessive gestational weight gain. BMC Pregnancy Childbirth 2018, 18, 312. [Google Scholar] [CrossRef] [PubMed]
- Conway, M.R.; Marshall, M.R.; Schlaff, R.A.; Pfeiffer, K.A.; Pivarnik, J.M. Physical activity device reliability and validity during pregnancy and postpartum. Med. Sci. Sports Exerc. 2018, 50, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Mudd, L.M.; Evenson, K.R. Review of impacts of physical activity on maternal metabolic health during pregnancy. Curr. Diabetes Rep. 2015, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Acog Committee Opinion. Exercise during pregnancy and the postpartum period. Int. J. Gynaecol. Obstet. 2002, 77, 79–81. [Google Scholar] [CrossRef]
- Horns, P.N.; Ratcliffe, L.P.; Leggett, J.C.; Swanson, M.S. Pregnancy outcomes among active and sedentary primiparous women. J. Obstet. Gynecol. Neonatal Nurs. 1996, 25, 49–54. [Google Scholar] [CrossRef]
- Gaston, A.; Cramp, A. Exercise during pregnancy: A review of patterns and determinants. J. Sci. Med. Sport 2011, 14, 299–305. [Google Scholar] [CrossRef]
- Butte, N.F.; Ellis, K.J.; Wong, W.W.; Hopkinson, J.M.; Smith, E.O. Composition of gestational weight gain impacts maternal fat retention and infant birth weight. Am. J. Obstet. Gynecol. 2003, 189, 1423–1432. [Google Scholar] [CrossRef]
- Berggren, E.K.; Groh-Wargo, S.; Presley, L.; Hauguel-de Mouzon, S.; Catalano, P.M. Maternal fat, but not lean, mass is increased among overweight/obese women with excess gestational weight gain. Am. J. Obstet. Gynecol. 2016, 214, e741–e745. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Marlatt, K.L.; Altazan, A.D.; Redman, L.M. Advances in assessing body composition during pregnancy. Eur. J. Clin. Nutr. 2018, 72, 645–656. [Google Scholar] [CrossRef] [PubMed]
- van Raaij, J.M.; Peek, M.E.; Vermaat-Miedema, S.H.; Schonk, C.M.; Hautvast, J.G. New equations for estimating body fat mass in pregnancy from body density or total body water. Am. J. Clin. Nutr. 1988, 48, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Tataranni, P.A.; Harper, I.T.; Snitker, S.; Del Parigi, A.; Vozarova, B.; Bunt, J.; Bogardus, C.; Ravussin, E. Body weight gain in free-living pima indians: Effect of energy intake vs. expenditure. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 1578–1583. [Google Scholar] [CrossRef] [PubMed]
- Butte, N.F.; King, J.C. Energy requirements during pregnancy and lactation. Public Health Nutr. 2005, 8, 1010–1027. [Google Scholar] [CrossRef] [PubMed]
- Durnin, J.V. Energy requirements of pregnancy. Diabetes 1991, 40 (Suppl. 2), 152–156. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Nutrition in pregnancy. In Your Pregnancy and Childbirth: Month to Month, 6th ed.; ACOG: Washington, DC, USA, 2016; pp. 313–327. [Google Scholar]
- IOM (Institute of Medicine); NRC (National Research Council). Weight Gain during Pregnancy: Reexamining the Guidelines; The National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Ravussin, E.; Lillioja, S.; Knowler, W.C.; Christin, L.; Freymond, D.; Abbott, W.G.; Boyce, V.; Howard, B.V.; Bogardus, C. Reduced rate of energy expenditure as a risk factor for body-weight gain. N. Engl. J. Med. 1988, 318, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Berggren, E.K.; O’Tierney-Ginn, P.; Lewis, S.; Presley, L.; De-Mouzon, S.H.; Catalano, P.M. Variations in resting energy expenditure: Impact on gestational weight gain. Am. J. Obstet. Gynecol. 2017, 217, 445.e1–445.e6. [Google Scholar] [CrossRef] [PubMed]
- Lof, M.; Olausson, H.; Bostrom, K.; Janerot-Sjoberg, B.; Sohlstrom, A.; Forsum, E. Changes in basal metabolic rate during pregnancy in relation to changes in body weight and composition, cardiac output, insulin-like growth factor I, and thyroid hormones and in relation to fetal growth. Am. J. Clin. Nutr. 2005, 81, 678–685. [Google Scholar] [CrossRef]
- Meng, Y.; Groth, S.W.; Stewart, P.; Smith, J.A. An exploration of the determinants of gestational weight gain in african american women: Genetic factors and energy expenditure. Biol. Res. Nurs. 2018, 20, 118–125. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Most, J.; Redman, L.M.; Rood, J.; Ravussin, E. Energy expenditure and substrate oxidation in white and african american young adults without obesity. Eur. J. Clin. Nutr. 2018, 72, 920–922. [Google Scholar] [CrossRef] [PubMed]
- Deputy, N.P.; Sharma, A.J.; Kim, S.Y.; Olson, C.K. Achieving appropriate gestational weight gain: The role of healthcare provider advice. J. Womens Health 2018, 27, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M.; et al. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef]
| First Author | Measurement Time Points | Cohort Size | Ethnicity | Age | BMI | Excess GWG |
|---|---|---|---|---|---|---|
| Weeks Gestation | N | White, AA, Other | ||||
| Butte, UW [10] | 0, 22, 36 | 17 | 15, 0, 2 | 31 ± 4 | 18.9 ± 0.8 | 18% |
| Butte, NW [10] | 0, 22, 36 | 34 | 24, 4, 5 | 30 ± 3 | 22.1 ± 1.5 | 35% |
| Butte, OV/OB [10] | 0, 22, 36 | 12 | 9, 2, 1 | 31 ± 5 | 28.8 ± 2.6 | 100% |
| Forsum1 [11] | 0, 17, 30 | 22 | 29 ± 4 | 22.3 ± 3.1 | ||
| Forsum2 [11] | 0, 36 | 19 | 28 ± 4 | 22.1 ± 3.4 | ||
| Goldberg [12] | 0, 6, 12, 18, 24, 30, 36 | 12 | 12, 0, 0 | 29 ± 3 | 23.0 ± 3.3 | |
| Kopp [13] | 0, 9, 25, 35 | 10 | 29 ± 5 | 23.1 ± 2.1 | 10% | |
| Lof [14] | 0, 14, 34 | 23 | 30 ± 4 | 24.2 ± 4.8 | ||
| Most [15] | 15, 36 | 54 | 28, 22, 4 | 28 ± 5 | 35.8 ± 5.0 | 67% |
| Tri- Mester | Body Weight | Fat-Free Mass | Fat Mass | TDEE | TDEE, Pred | TDEE, Res | RMR | RMR, Pred | RMR, Res | |
|---|---|---|---|---|---|---|---|---|---|---|
| Non-Obesity | ||||||||||
| Forsum1 | 1 | 2.1 | 0.2 | 1.9 | −146 | 26 | −172 | 73 | 25 | 48 |
| Goldberg | 1 | 1.7 | 0.2 | 1.5 | 181 | 22 | 159 | 26 | 21 | 5 |
| Butte, UW | 1 | 4.6 | 2.1 | 2.5 | −45 | 91 | −136 | 76 | 67 | 9 |
| Butte, NW | 1 | 3.4 | 1.7 | 1.7 | 51 | 68 | −18 | 53 | 50 | 3 |
| Butte, OV/OB | 1 | 5.0 | 1.9 | 3.1 | −31 | 93 | −124 | 111 | 71 | 41 |
| Lof | 1 | 2.3 | 0.9 | 1.4 | 2 | 41 | −39 | 33 | 32 | 1 |
| Average | 1 | 3.2 | 1.2 | 2.0 | 2 | 57 | −55 | 62 | 44 | 18 |
| Non-Obesity | ||||||||||
| Forsum1 | 2 and 3 | 11.5 | 10.4 | 1.1 | 1226 | 312 | 914 | 381 | 199 | 181 |
| Goldberg | 2 and 3 | 8.0 | 5.9 | 2.0 | 252 | 193 | 59 | 298 | 129 | 168 |
| Butte, UW | 2 and 3 | 8.7 | 7.1 | 1.6 | 274 | 221 | 54 | 399 | 145 | 254 |
| Butte, NW | 2 and 3 | 11.7 | 8.9 | 2.8 | 284 | 290 | −5 | 427 | 192 | 235 |
| Butte, OV/OB | 2 and 3 | 13.1 | 9.7 | 3.5 | 219 | 323 | −104 | 531 | 215 | 316 |
| Lof | 2 and 3 | 10.8 | 7.5 | 3.3 | 341 | 256 | 85 | 349 | 173 | 176 |
| Average | 10.6 | 8.2 | 2.4 | 433 | 266 | 167 | 397 | 176 | 222 | |
| Obesity | ||||||||||
| Most | 2 and 3 | 8.5 | 8.2 | 0.3 | 335 | 237 | 98 | 335 | 150 | 185 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Most, J.; Dervis, S.; Haman, F.; Adamo, K.B.; Redman, L.M. Energy Intake Requirements in Pregnancy. Nutrients 2019, 11, 1812. https://doi.org/10.3390/nu11081812
Most J, Dervis S, Haman F, Adamo KB, Redman LM. Energy Intake Requirements in Pregnancy. Nutrients. 2019; 11(8):1812. https://doi.org/10.3390/nu11081812
Chicago/Turabian StyleMost, Jasper, Sheila Dervis, Francois Haman, Kristi B Adamo, and Leanne M Redman. 2019. "Energy Intake Requirements in Pregnancy" Nutrients 11, no. 8: 1812. https://doi.org/10.3390/nu11081812
APA StyleMost, J., Dervis, S., Haman, F., Adamo, K. B., & Redman, L. M. (2019). Energy Intake Requirements in Pregnancy. Nutrients, 11(8), 1812. https://doi.org/10.3390/nu11081812






