Maternal and Infant Factors Associated with Human Milk Oligosaccharides Concentrations According to Secretor and Lewis Phenotypes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Considerations
2.3. HMOs Analysis
2.3.1. HMOs Extraction
2.3.2. HMOs Identification and Quantification by LC-MS
2.4. Secretor and Lewis Phenotype Determination
2.5. Statistics
3. Results
3.1. Study Population
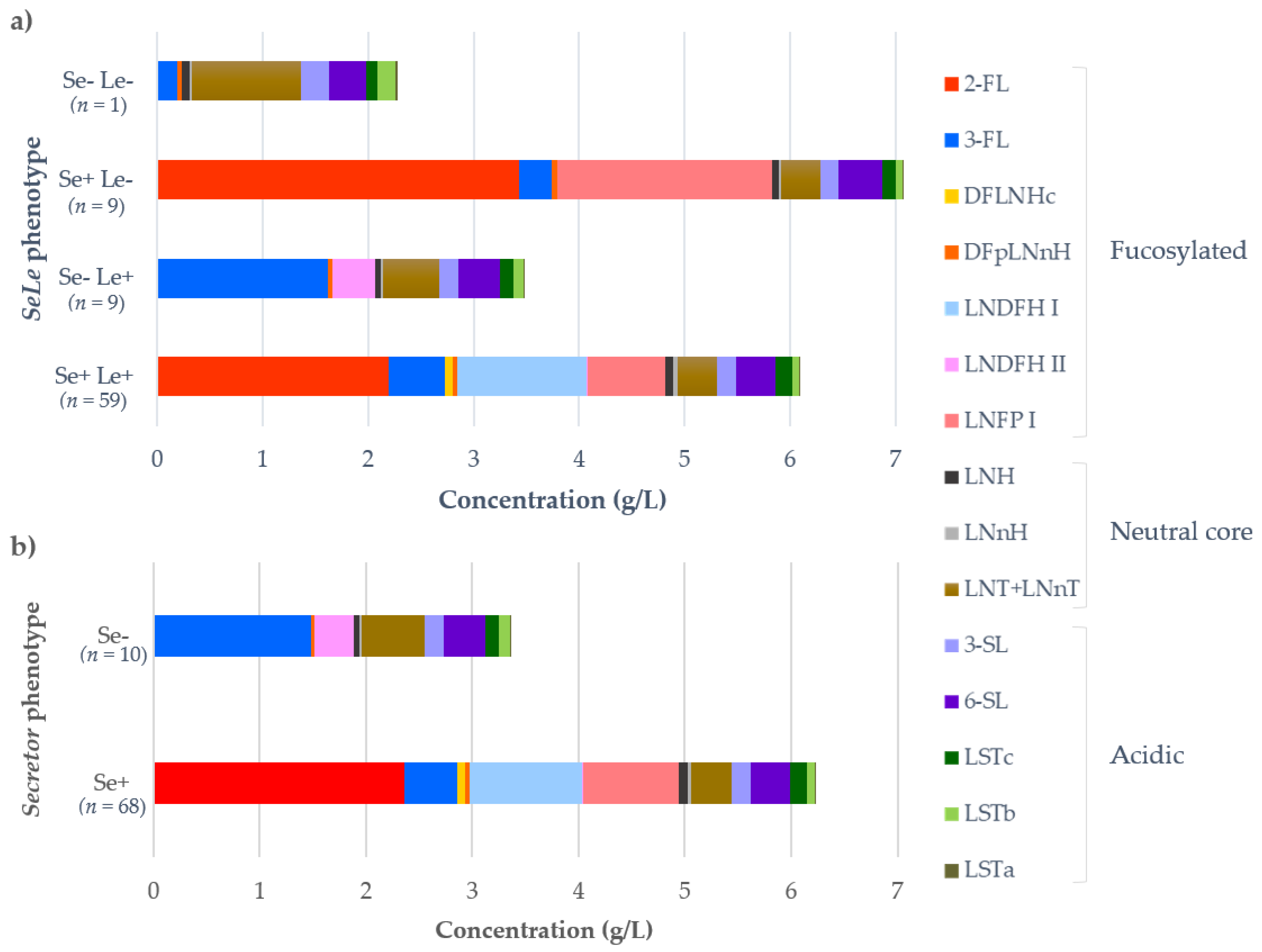
3.2. HMOs Composition and Concentrations
3.3. Associations of Maternal and Infant Factors with HMOs Concentrations in SeLe Groups
Associations Regarding Se Status Alone
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| HMOs Concentrations | Maternal Variables | Infant Variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parity | Age | Postpartum Days | BMI | Weight | PG Weight | PPG BMI | Gestational Age | Weight at Birth | Weight | Length | Weight Gain | |
| Fucosylated | ||||||||||||
| 3’-FL | 0.28 | −0.06 | 0.35 | −0.58 | −0.52 | −0.41 | −0.14 | −0.26 | −0.14 | 0.46 | 0.49 | 0.77 |
| LNDFH II | 0.39 | 0.42 | −0.08 | −0.30 | 0.00 | −0.32 | 0.11 | −0.04 | −0.29 | −0.04 | 0.05 | 0.14 |
| DFpLNnH | −0.06 | −0.28 | 0.25 | −0.02 | −0.19 | −0.28 | −0.08 | −0.18 | −0.10 | 0.36 | 0.40 | 0.09 |
| Neutral core | ||||||||||||
| LNH | −0.17 | 0.01 | −0.50 | 0.08 | −0.21 | −0.08 | −0.42 | −0.54 | −0.26 | −0.56 | −0.75 | −0.06 |
| LNnH | −0.17 | −0.44 | 0.11 | −0.32 | −0.60 | −0.32 | −0.61 | −0.49 | −0.21 | 0.11 | −0.02 | 0.26 |
| LNT+LNnT | 0.17 | 0.73 | −0.35 | 0.00 | 0.19 | −0.18 | −0.16 | 0.22 | −0.19 | −0.43 | −0.45 | −0.49 |
| Acidic | ||||||||||||
| 3’-SL | 0.62 | 0.38 | −0.34 | −0.08 | 0.05 | −0.22 | 0.19 | −0.22 | −0.36 | −0.46 | −0.52 | 0.60 |
| 6’-SL | −0.06 | 0.89 | −0.70 | 0.00 | 0.36 | −0.05 | 0.12 | −0.18 | −0.50 | −0.71 | −0.72 | −0.37 |
| LSTa | −0.39 | 0.49 | −0.69 | 0.40 | 0.45 | 0.41 | 0.12 | −0.07 | −0.19 | −0.57 | −0.58 | −0.66 |
| LSTb | 0.28 | 0.37 | −0.16 | −0.37 | −0.12 | −0.72 | −0.46 | −0.11 | −0.36 | −0.46 | −0.47 | −0.31 |
| LSTc | −0.39 | 0.45 | −0.90 | 0.03 | 0.17 | −0.29 | −0.19 | −0.72 | −0.83 | −0.75 | −0.74 | −0.49 |
| Total | ||||||||||||
| Fucosylated | 0.51 | 0.23 | 0.19 | −0.57 | −0.40 | −0.47 | −0.08 | −0.10 | −0.26 | 0.29 | 0.29 | 0.66 |
| Neutral core | 0.00 | 0.64 | −0.46 | 0.02 | 0.05 | −0.18 | −0.40 | 0.02 | −0.31 | −0.38 | −0.52 | −0.41 |
| Acidic | 0.00 | 0.84 | −0.66 | 0.03 | 0.32 | −0.07 | 0.14 | −0.19 | −0.50 | −0.61 | −0.63 | −0.20 |
| Total HMOs | 0.17 | 0.66 | −0.38 | −0.25 | 0.12 | −0.25 | 0.11 | −0.11 | −0.55 | −0.36 | −0.31 | 0.09 |
| HMOs Concentrations | Maternal Variables | Infant variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parity | Age | Postpartum Days | BMI | Weight | PG Weight | PG BMI | Gestational Age | Weight at Birth | Weight | Length | Weight Gain | |
| Fucosylated | ||||||||||||
| 2’-FL | −0.32 | 0.46 | 0.03 | 0.38 | 0.40 | 0.17 | 0.13 | 0.59 | 0.07 | −0.04 | 0.04 | 0.07 |
| 3’-FL | −0.79 | −0.23 | −0.08 | −0.28 | −0.28 | −0.50 | −0.55 | −0.05 | −0.38 | −0.57 | −0.50 | 0.18 |
| LNFP I | 0.79 | 0.01 | −0.12 | 0.28 | 0.38 | 0.48 | 0.68 | −0.17 | 0.33 | 0.29 | 0.32 | −0.61 |
| DFpLNnH | 0.00 | −0.62 | −0.03 | 0.23 | 0.13 | 0.13 | −0.08 | −0.37 | 0.00 | 0.04 | 0.09 | −0.11 |
| Neutral core | ||||||||||||
| LNH | 0.79 | −0.15 | 0.00 | −0.20 | −0.18 | 0.10 | 0.23 | −0.48 | 0.21 | 0.21 | −0.02 | −0.36 |
| LNnH | 0.63 | 0.34 | 0.21 | 0.05 | 0.02 | 0.33 | 0.35 | 0.05 | 0.36 | 0.61 | 0.36 | 0.00 |
| LNT+LNnT | 0.79 | −0.26 | −0.11 | −0.22 | −0.13 | 0.03 | 0.18 | −0.49 | 0.19 | 0.00 | −0.05 | −0.50 |
| Acidic | ||||||||||||
| 3’-SL | −0.32 | −0.63 | −0.38 | −0.37 | −0.28 | −0.59 | −0.50 | −0.50 | −0.43 | −0.82 | −0.59 | 0.07 |
| 6’-SL | −0.16 | −0.16 | −0.83 | −0.02 | 0.28 | 0.06 | 0.48 | −0.38 | −0.45 | −0.61 | −0.81 | −0.29 |
| LSTa | 0.79 | −0.34 | −0.09 | −0.57 | −0.53 | −0.44 | −0.15 | −0.67 | 0.10 | −0.04 | −0.02 | −0.46 |
| LSTb | 0.79 | −0.55 | 0.09 | 0.32 | 0.25 | 0.30 | 0.23 | −0.44 | 0.50 | 0.14 | 0.23 | −0.82 |
| LSTc | 0.16 | −0.79 | −0.44 | 0.22 | 0.27 | 0.19 | 0.23 | −0.69 | −0.12 | −0.21 | −0.40 | −0.75 |
| Total | ||||||||||||
| Fucosylated | 0.32 | 0.56 | −0.15 | 0.37 | 0.53 | 0.40 | 0.55 | 0.39 | 0.40 | 0.04 | −0.09 | −0.32 |
| Neutral core | 0.80 | −0.21 | 0.01 | −0.19 | −0.15 | 0.11 | 0.22 | −0.44 | 0.26 | 0.25 | 0.10 | −0.47 |
| Acidic | −0.16 | −0.48 | −0.74 | −0.18 | 0.09 | −0.13 | 0.20 | −0.55 | −0.47 | −0.67 | −0.72 | −0.41 |
| Total HMOs | 0.32 | 0.43 | −0.22 | 0.43 | 0.63 | 0.57 | 0.75 | 0.28 | 0.33 | −0.04 | −0.13 | −0.36 |
| HMOs Concentrations | Maternal Variables | Infant Variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parity | Age | Postpartum Days | BMI | Weight | PG Weight | PG BMI | Gestational Age | Weight at Birth | Weight | Length | Weight Gain | |
| Fucosylated | ||||||||||||
| 2’-FL | −0.04 | 0.00 | −0.10 | 0.30 | 0.29 | 0.23 | 0.25 | −0.04 | 0.11 | −0.04 | 0.08 | −0.15 |
| 3’-FL | 0.09 | 0.10 | 0.31 | −0.23 | −0.14 | −0.13 | −0.20 | −0.08 | −0.09 | 0.16 | 0.07 | 0.17 |
| LNFP I | −0.04 | −0.18 | −0.43 | 0.24 | 0.21 | 0.16 | 0.18 | 0.06 | 0.09 | −0.30 | −0.09 | −0.28 |
| LNDFH I | 0.04 | −0.04 | −0.07 | −0.08 | −0.02 | 0.06 | 0.02 | 0.18 | 0.09 | −0.19 | 0.11 | −0.28 |
| LNDFH II | 0.10 | 0.09 | 0.29 | −0.16 | −0.09 | −0.05 | −0.10 | −0.10 | −0.10 | 0.09 | 0.05 | 0.00 |
| DFLNHc | 0.01 | 0.15 | −0.08 | 0.03 | −0.02 | 0.02 | 0.05 | 0.13 | 0.07 | −0.03 | 0.13 | 0.04 |
| DFpLNnH | 0.07 | −0.14 | −0.01 | −0.04 | −0.02 | 0.07 | 0.05 | −0.11 | −0.16 | −0.15 | −0.17 | −0.14 |
| Neutral core | ||||||||||||
| LNH | 0.05 | 0.04 | −0.34 | 0.09 | −0.03 | −0.03 | 0.04 | 0.08 | 0.11 | −0.15 | −0.16 | 0.03 |
| LNnH | −0.01 | 0.13 | 0.12 | 0.19 | 0.08 | 0.13 | 0.24 | −0.02 | 0.13 | 0.13 | 0.09 | 0.06 |
| LNT+LNnT | 0.12 | −0.14 | −0.45 | −0.10 | −0.15 | −0.12 | −0.11 | 0.07 | 0.10 | −0.35 | −0.26 | −0.14 |
| Acidic | ||||||||||||
| 3’-SL | −0.06 | −0.03 | −0.28 | −0.14 | −0.16 | −0.22 | −0.22 | −0.12 | −0.18 | −0.37 | −0.33 | −0.24 |
| 6’-SL | 0.07 | 0.04 | −0.73 | −0.02 | −0.01 | 0.01 | −0.03 | 0.14 | 0.00 | −0.51 | −0.31 | −0.30 |
| LSTa | 0.01 | 0.03 | −0.53 | −0.18 | −0.19 | −0.18 | −0.20 | 0.14 | 0.02 | −0.39 | −0.24 | −0.21 |
| LSTb | 0.14 | −0.22 | −0.23 | −0.04 | −0.04 | −0.07 | −0.08 | −0.06 | 0.11 | −0.28 | −0.16 | −0.25 |
| LSTc | 0.06 | −0.06 | −0.72 | −0.07 | −0.06 | 0.00 | −0.05 | 0.15 | 0.02 | −0.53 | −0.27 | −0.39 |
| Total | ||||||||||||
| Fucosylated | −0.06 | −0.12 | −0.28 | 0.24 | 0.25 | 0.22 | 0.21 | 0.08 | 0.12 | −0.25 | −0.01 | −0.33 |
| Neutral core | 0.09 | −0.07 | −0.42 | −0.01 | −0.10 | −0.10 | −0.05 | 0.11 | 0.15 | −0.29 | −0.24 | −0.07 |
| Acidic | 0.03 | −0.03 | −0.80 | −0.08 | −0.08 | −0.07 | −0.11 | 0.16 | −0.03 | −0.63 | −0.39 | −0.43 |
| Total HMOs | −0.02 | −0.11 | −0.44 | 0.24 | 0.25 | 0.23 | 0.20 | 0.10 | 0.14 | −0.37 | −0.10 | −0.39 |
| HMOs Concentrations | Maternal Variables | Infant Variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parity | Age | Postpartum Days | BMI | Weight | PG Weight | PG BMI | Gestational Age | Weight at Birth | Weight | Length | Weight Gain | |
| Fucosylated | ||||||||||||
| 3’-FL | 0.43 | −0.24 | 0.18 | −0.18 | −0.36 | −0.33 | 0.20 | −0.37 | 0.07 | 0.31 | 0.32 | 0.29 |
| LNDFH II | 0.52 | 0.14 | −0.22 | 0.22 | −0.10 | −0.29 | 0.38 | −0.14 | −0.02 | −0.14 | −0.08 | −0.25 |
| DFpLNnH | −0.09 | −0.19 | 0.26 | −0.42 | −0.19 | −0.37 | −0.28 | −0.10 | −0.13 | 0.29 | 0.31 | 0.14 |
| Neutral core | ||||||||||||
| LNH | −0.26 | 0.07 | −0.35 | −0.25 | 0.05 | −0.03 | −0.49 | −0.43 | −0.33 | −0.43 | −0.59 | 0.11 |
| LNnH | −0.26 | −0.28 | 0.18 | −0.57 | −0.35 | −0.25 | −0.62 | −0.39 | −0.30 | 0.12 | 0.01 | 0.36 |
| LNT+LNnT | −0.09 | 0.78 | −0.24 | −0.10 | −0.12 | −0.18 | −0.41 | 0.33 | −0.28 | −0.33 | −0.35 | −0.14 |
| Acidic | ||||||||||||
| 3’-SL | 0.35 | 0.44 | −0.28 | −0.12 | −0.22 | −0.23 | −0.12 | −0.10 | −0.35 | −0.43 | −0.46 | 0.57 |
| 6’-SL | 0.09 | 0.70 | −0.78 | 0.37 | 0.08 | −0.11 | 0.14 | −0.23 | −0.43 | −0.81 | −0.81 | −0.46 |
| LSTa | −0.43 | 0.53 | −0.51 | 0.15 | 0.24 | 0.37 | −0.15 | 0.04 | −0.28 | −0.48 | −0.48 | −0.32 |
| LSTb | 0.09 | 0.54 | −0.11 | −0.23 | −0.42 | −0.65 | −0.52 | 0.14 | −0.35 | −0.38 | −0.38 | −0.04 |
| LSTc | −0.26 | 0.32 | −0.91 | 0.15 | 0.07 | −0.28 | −0.18 | −0.69 | −0.75 | −0.83 | −0.83 | −0.54 |
| Total | ||||||||||||
| Fucosylated | 0.61 | −0.01 | 0.01 | −0.08 | −0.33 | −0.39 | 0.24 | −0.22 | 0.00 | 0.12 | 0.12 | 0.14 |
| Neutral core | −0.26 | 0.68 | −0.32 | −0.20 | −0.12 | −0.16 | −0.58 | 0.15 | −0.45 | −0.31 | −0.40 | −0.07 |
| Acidic | −0.09 | 0.83 | −0.63 | 0.23 | 0.07 | −0.02 | 0.00 | −0.01 | −0.50 | −0.55 | −0.57 | −0.11 |
| Total HMOs | 0.26 | 0.49 | −0.50 | 0.17 | −0.18 | −0.33 | 0.16 | −0.21 | −0.43 | −0.48 | −0.44 | −0.18 |
References
- Dieterich, C.M.; Felice, J.P.; O’Sullivan, E.; Rasmussen, K.M. Breastfeeding and health outcomes for the mother-infant dyad. Pediatr. Clin. North Am. 2013, 60, 31–48. [Google Scholar] [CrossRef]
- Ballard, O.; Morrow, A.L. Human milk composition: nutrients and bioactive factors. Pediatr. Clin. North Am. 2013, 60, 49–74. [Google Scholar] [CrossRef] [PubMed]
- Newburg, D.S.; Neubauer, S.H. Carbohydrates in milk: analysis, quantities and significance. In Handbook of Milk Composition; Jensen, R.G., Ed.; Academic Press: San Diego, CA, USA, 1995. [Google Scholar]
- Bode, L. Human milk oligosaccharides: Every baby needs a sugar mama. Glycobiology 2012, 22, 1147–1162. [Google Scholar] [CrossRef] [PubMed]
- De Leoz, M.L.A.; Kalanetra, K.M.; Bokulich, N.A.; Strum, J.S.; Underwood, M.A.; German, J.B.; Mills, D.A.; Lebrilla, C.B. Human Milk Glycomics and Gut Microbial Genomics in Infant Feces Show a Correlation between Human Milk Oligosaccharides and Gut Microbiota: A Proof-of-Concept Study. J. Proteome Res. 2015, 14, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Marcobal, A.; Barboza, M.; Froehlich, J.W.; Block, D.E.; German, J.B.; Lebrilla, C.B.; Mills, D. a Consumption of human milk oligosaccharides by gut-related microbes. J. Agric. Food Chem. 2010, 58, 5334–5340. [Google Scholar] [CrossRef] [PubMed]
- Asakuma, S.; Hatakeyama, E.; Urashima, T.; Yoshida, E.; Katayama, T.; Yamamoto, K.; Kumagai, H.; Ashida, H.; Hirose, J.; Kitaoka, M. Physiology of consumption of human milk oligosaccharides by infant gut-associated bifidobacteria. J. Biol. Chem. 2011, 286, 34583–34592. [Google Scholar] [CrossRef]
- Lin, A.E.; Autran, C.A.; Szyszka, A.; Escajadillo, T.; Huang, M.; Godula, K.; Prudden, A.R.; Boons, G.-J.; Lewis, A.L.; Doran, K.S.; et al. Human milk oligosaccharides inhibit growth of group B Streptococcus. J. Biol. Chem. 2017, 292, 11243–11249. [Google Scholar] [CrossRef]
- Newburg, D.S.; Ruiz-Palacios, G.M.; Morrow, A.L. Human milk glycans protect infants against enteric pathogens. Annu. Rev. Nutr. 2005, 25, 37–58. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Palacios, G.M.; Cervantes, L.E.; Ramos, P.; Chavez-Munguia, B.; Newburg, D.S. Campylobacter jejuni Binds Intestinal H(O) Antigen (Fuc 1, 2Gal 1, 4GlcNAc), and Fucosyloligosaccharides of Human Milk Inhibit Its Binding and Infection. J. Biol. Chem. 2003, 278, 14112–14120. [Google Scholar] [CrossRef] [PubMed]
- Morrow, A.L.; Ruiz-Palacios, G.M.; Altaye, M.; Jiang, X.; Lourdes Guerrero, M.; Meinzen-Derr, J.K.; Farkas, T.; Chaturvedi, P.; Pickering, L.K.; Newburg, D.S. Human milk oligosaccharides are associated with protection against diarrhea in breast-fed infants. J. Pediatr. 2004, 145, 297–303. [Google Scholar] [CrossRef]
- Donovan, S.M.; Comstock, S.S. Human Milk Oligosaccharides Influence Neonatal Mucosal and Systemic Immunity. Ann. Nutr. Metab. 2016, 69, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Wang, B. Molecular Mechanism Underlying Sialic Acid as an Essential Nutrient for Brain Development and Cognition. Adv. Nutr. An Int. Rev. J. 2012, 3, 465S–472S. [Google Scholar] [CrossRef] [PubMed]
- Lis-Kuberka, J.; Orczyk-Pawiłowicz, M. Sialylated Oligosaccharides and Glycoconjugates of Human Milk. The Impact on Infant and Newborn Protection, Development and Well-Being. Nutrients 2019, 11, 306. [Google Scholar] [CrossRef] [PubMed]
- Chen, X. Human Milk Oligosaccharides (HMOS): Structure, Function, and Enzyme-Catalyzed Synthesis. In Advances in Carbohydrate Chemistry and Biochemistry; Elsevier Inc.: Waltham, MA, USA, 2015; Volume 72, pp. 113–190. ISBN 9780128021415. [Google Scholar]
- Ninonuevo, M.R.; Park, Y.; Yin, H.; Zhang, J.; Ward, R.E.; Clowers, B.H.; German, J.B.; Freeman, S.L.; Killeen, K.; Grimm, R.; et al. A strategy for annotating the human milk glycome. J. Agric. Food Chem. 2006, 54, 7471–7480. [Google Scholar] [CrossRef] [PubMed]
- Zivkovic, A.M.; German, J.B.; Lebrilla, C.B.; Mills, D.A. Human milk glycobiome and its impact on the infant gastrointestinal microbiota. Proc. Natl. Acad. Sci. 2011, 108, 4653–4658. [Google Scholar] [CrossRef]
- Bode, L.; Jantscher-Krenn, E. Structure-Function Relationships of Human Milk Oligosaccharides. Adv. Nutr. An Int. Rev. J. 2012, 3, 383S–391S. [Google Scholar] [CrossRef] [PubMed]
- Kumazaki, T.; Yoshida, A. Biochemical evidence that secretor gene, Se, is a structural gene encoding a specific fucosyltransferase. Proc. Natl. Acad. Sci. 1984, 81, 4193–4197. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.H.; Watkins, W.M. Purification of the Lewis blood-group gene associated a-3/4-fucosyltransferase from human milk: an enzyme transferring fucose primarily to Type 1 and lactose-based oligosaccharide chains. Glycoconj. J. 1992, 9, 241–249. [Google Scholar] [CrossRef]
- Kobata, A. Structures and application of oligosaccharides in human milk. Proc. Japan Acad. Ser. B 2010, 86, 731–747. [Google Scholar] [CrossRef]
- Thurl, S.; Henker, J.; Siegel, M.; Tovar, K.; Sawatzki, G. Detection of four human milk groups with respect to Lewis blood group dependent oligosaccharides. Glycoconj. J. 1997, 14, 795–799. [Google Scholar] [CrossRef]
- Thurl, S.; Munzert, M.; Henker, J.; Boehm, G.; Müller-Werner, B.; Jelinek, J.; Stahl, B. Variation of human milk oligosaccharides in relation to milk groups and lactational periods. Br. J. Nutr. 2010, 104, 1261–1271. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, M.; Simpore, J.; D’Agata, A.; Sotgiu, S.; Musumeci, S. Oligosaccharides in colostrum of Italian and Burkinabe women. J. Pediatr. Gastroenterol. Nutr. 2006, 43, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Gabrielli, O.; Zampini, L.; Galeazzi, T.; Padella, L.; Santoro, L.; Peila, C.; Giuliani, F.; Bertino, E.; Fabris, C.; Coppa, G.V. Preterm milk oligosaccharides during the first month of lactation. Pediatrics 2011, 128, e1520. [Google Scholar] [CrossRef] [PubMed]
- Kunz, C.; Meyer, C.; Collado, M.C.; Geiger, L.; García-Mantrana, I.; Bertua-Ríos, B.; Martínez-Costa, C.; Borsch, C.; Rudloff, S. Influence of Gestational Age, Secretor, and Lewis Blood Group Status on the Oligosaccharide Content of Human Milk. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Elwakiel, M.; Hageman, J.A.; Wang, W.; Szeto, I.M.; van Goudoever, J.B.; Hettinga, K.A.; Schols, H.A. Human Milk Oligosaccharides in Colostrum and Mature Milk of Chinese Mothers: Lewis Positive Secretor Subgroups. J. Agric. Food Chem. 2018, 66, 7036–7043. [Google Scholar] [CrossRef] [PubMed]
- McGuire, M.K.; Meehan, C.L.; McGuire, M.A.; Williams, J.E.; Foster, J.; Sellen, D.W.; Kamau-Mbuthia, E.W.; Kamundia, E.W.; Mbugua, S.; Moore, S.E.; et al. What’s normal? Oligosaccharide concentrations and profiles in milk produced by healthy women vary geographically. Am. J. Clin. Nutr. 2017, 105, 1086–1100. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Robertson, B.; Atakora, F.; Becker, A.B.; Subbarao, P.; Moraes, T.J.; Mandhane, P.J.; Turvey, S.E.; Lefebvre, D.L.; Sears, M.R.; et al. Human Milk Oligosaccharide Concentrations Are Associated with Multiple Fixed and Modifiable Maternal Characteristics, Environmental Factors, and Feeding Practices. J. Nutr. 2018, 148, 1733–1742. [Google Scholar] [CrossRef]
- Sprenger, N.; Odenwald, H.; Kukkonen, A.K.; Kuitunen, M.; Savilahti, E.; Kunz, C. FUT2-dependent breast milk oligosaccharides and allergy at 2 and 5 years of age in infants with high hereditary allergy risk. Eur. J. Nutr. 2017, 56, 1293–1301. [Google Scholar] [CrossRef]
- Bode, L.; Kuhn, L.; Kim, H.-Y.; Hsiao, L.; Nissan, C.; Sinkala, M.; Kankasa, C.; Mwiya, M.; Thea, D.M.; Aldrovandi, G.M. Human milk oligosaccharide concentration and risk of postnatal transmission of HIV through breastfeeding. Am. J. Clin. Nutr. 2012, 96, 831–839. [Google Scholar] [CrossRef]
- Kuhn, L.; Kim, H.-Y.; Hsiao, L.; Nissan, C.; Kankasa, C.; Mwiya, M.; Thea, D.M.; Aldrovandi, G.M.; Bode, L. Oligosaccharide Composition of Breast Milk Influences Survival of Uninfected Children Born to HIV-Infected Mothers in Lusaka, Zambia. J. Nutr. 2015, 145, 66–72. [Google Scholar] [CrossRef]
- Jantscher-Krenn, E.; Zherebtsov, M.; Nissan, C.; Goth, K.; Guner, Y.S.; Naidu, N.; Choudhury, B.; Grishin, A.V.; Ford, H.R.; Bode, L. The human milk oligosaccharide disialyllacto-N-tetraose prevents necrotising enterocolitis in neonatal rats. Gut 2012, 61, 1417–1425. [Google Scholar] [CrossRef] [PubMed]
- Autran, C.A.; Kellman, B.P.; Kim, J.H.; Asztalos, E.; Blood, A.B.; Spence, E.C.H.; Patel, A.L.; Hou, J.; Lewis, N.E.; Bode, L. Human milk oligosaccharide composition predicts risk of necrotising enterocolitis in preterm infants. Gut 2018, 67, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Alderete, T.L.; Autran, C.; Brekke, B.E.; Knight, R.; Bode, L.; Goran, M.I.; Fields, D.A. Associations between human milk oligosaccharides and infant body composition in the first 6 mo of life. Am. J. Clin. Nutr. 2015, 102, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Charbonneau, M.R.; O’Donnell, D.; Blanton, L.V.; Totten, S.M.; Davis, J.C.C.; Barratt, M.J.; Cheng, J.; Guruge, J.; Talcott, M.; Bain, J.R.; et al. Sialylated Milk Oligosaccharides Promote Microbiota-Dependent Growth in Models of Infant Undernutrition. Cell 2016, 164, 859–871. [Google Scholar] [CrossRef] [PubMed]
- Associação Brasileira das Empresas de Pesquisa. Critério de Classificação Econômica Brasil. Available online: http://www.abep.org/criterio-brasil (accessed on 7 June 2019).
- Vanna, A.T.; Yamada, E.; Arruda, L.K.; Naspitz, C.K.; Sole, D. International Study of Asthma and Allergies in Childhood: Validation of the rhinitis symptom questionnaire and prevalence of rhinitis in schoolchildren in Sao Paulo, Brazil. Pediatr. Allergy Immunol. 2001, 12, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Solé, D.; Vanna, A.T.; Yamada, E.; Rizzo, M.C.; Naspitz, C.K. International Study of Asthma and Allergies in Childhood (ISAAC) written questionnaire: Validation of the asthma component among Brazilian children. J. Investig. Allergol. Clin. Immunol. 1998, 8, 376–382. [Google Scholar] [PubMed]
- Yamada, E.; Vanna, A.T.; Naspitz, C.K.; Solé, D. International Study of Asthma and Allergies in Childhood (ISAAC): Validation of the written questionnaire (eczema component) and prevalence of atopic eczema among Brazilian children. J. Investig. Allergol. Clin. Immunol. 2002, 12, 34–41. [Google Scholar] [PubMed]
- Tonon, K.M.; Miranda, A.; Abrão, A.C.F.V.; de Morais, M.B.; Morais, T.B. Validation and application of a method for the simultaneous absolute quantification of 16 neutral and acidic human milk oligosaccharides by graphitized carbon liquid chromatography—Electrospray ionization—Mass spectrometry. Food Chem. 2019, 274, 691–697. [Google Scholar] [CrossRef]
- Bai, Y.; Tao, J.; Zhou, J.; Fan, Q.; Liu, M.; Hu, Y.; Xu, Y.; Zhang, L.; Yuan, J.; Li, W.; et al. Fucosylated Human Milk Oligosaccharides and N-Glycans in the Milk of Chinese Mothers Regulate the Gut Microbiome of Their Breast-Fed Infants during Different Lactation Stages. mSystems 2018, 3, e00206-18. [Google Scholar] [CrossRef]
- Totten, S.M.; Zivkovic, A.M.; Wu, S.; Ngyuen, U.; Freeman, S.L.; Ruhaak, L.R.; Darboe, M.K.; German, J.B.; Prentice, A.M.; Lebrilla, C.B. Comprehensive profiles of human milk oligosaccharides yield highly sensitive and specific markers for determining secretor status in lactating mothers. J. Proteome Res. 2012, 11, 6124–6133. [Google Scholar] [CrossRef]
- Blank, D.; Dotz, V.; Geyer, R.; Kunz, C. Human Milk Oligosaccharides and Lewis Blood Group: Individual High-Throughput Sample Profiling to Enhance Conclusions From Functional Studies. Adv. Nutr. An Int. Rev. J. 2012, 3, 440S–449S. [Google Scholar] [CrossRef] [PubMed]
- Cangür, Ş.; Sungur, M.A.; Ankarali, H. The Methods Used in Nonparametric Covariance Analysis. Duzce Tıp Fak Derg 2018, 20, 1–6. [Google Scholar] [CrossRef]
- Cangür, Ş.; Sungur, M.A.; Ankarali, H. A web-based program for the Quade, Puri & Sen, and McSweeny & Porter Ranked ANCOVA Methods (Post Hoc Tukey-Kramer Test) for One-factor Covariance Model with Single-Covariate. Available online: http://www.masungur.com/nancova0.php (accessed on 7 June 2019).
- Thurl, S.; Munzert, M.; Boehm, G.; Matthews, C.; Stahl, B. Systematic review of the concentrations of oligosaccharides in human milk. Nutr. Rev. 2017, 75, 920–933. [Google Scholar] [CrossRef] [PubMed]
- Van Niekerk, E.; Autran, C. Milk Oligosaccharides Differ between HIV-Infected and HIV-Uninfected Mothers and Are Related to Necrotizing Enterocolitis Incidence in Their Preterm Very-Low-Birth. J. Nutr. 2014, 144, 1227–1233. [Google Scholar] [CrossRef]
- Seppo, A.E.; Autran, C.A.; Bode, L.; Järvinen, K.M. Human milk oligosaccharides and development of cow’s milk allergy in infants. J. Allergy Clin. Immunol. 2017, 139, 708–711.e5. [Google Scholar] [CrossRef] [PubMed]
- King, J.R.; Varadé, J.; Hammarström, L. Fucosyltransferase Gene Polymorphisms and Lewisb-Negative Status Are Frequent in Swedish Newborns, With Implications for Infectious Disease Susceptibility and Personalized Medicine. J. Pediatric Infect. Dis. Soc. 2018. [Google Scholar] [CrossRef]
- Guo, M.; Luo, G.; Lu, R.; Shi, W.; Cheng, H.; Lu, Y.; Jin, K.; Yang, C.; Wang, Z.; Long, J.; et al. Distribution of Lewis and Secretor polymorphisms and corresponding CA19-9 antigen expression in a Chinese population. FEBS Open Bio 2017, 7, 1660–1671. [Google Scholar] [CrossRef] [PubMed]
- Nordgren, J.; Sharma, S.; Bucardo, F.; Nasir, W.; Günaydin, G.; Ouermi, D.; Nitiema, L.W.; Becker-Dreps, S.; Simpore, J.; Hammarström, L.; et al. Both lewis and secretor status mediate susceptibility to rotavirus infections in a rotavirus genotype-dependent manner. Clin. Infect. Dis. 2014, 59, 1567–1573. [Google Scholar] [CrossRef]
- Corvelo, T.C.O.; Aguiar, D.C.F.; Sagica, F.E.S. The expression of ABH and Lewis antigens in Brazilian semi-isolated Black communities. Genet. Mol. Biol. 2002, 25, 259–263. [Google Scholar] [CrossRef]
- Bernardo, C.R.; Camargo, A.V.S.; Ronchi, L.S.; de Oliveira, A.P.; de Campos Júnior, E.; Borim, A.A.; Brandão de Mattos, C.C.; Bestetti, R.B.; de Mattos, L.C. ABO, Secretor and Lewis histo-blood group systems influence the digestive form of Chagas disease. Infect. Genet. Evol. 2016, 45, 170–175. [Google Scholar] [CrossRef]
- Coppa, G.V.; Gabrielli, O.; Zampini, L.; Galeazzi, T.; Ficcadenti, A.; Padella, L.; Santoro, L.; Soldi, S.; Carlucci, A.; Bertino, E.; et al. Oligosaccharides in 4 different milk groups, Bifidobacteria, and Ruminococcus obeum. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Sprenger, N.; Lee, L.Y.; De Castro, C.A.; Steenhout, P.; Thakkar, S.K. Longitudinal change of selected human milk oligosaccharides and association to infants’ growth, an observatory, single center, longitudinal cohort study. PLoS ONE 2017, 12, e0171814. [Google Scholar] [CrossRef] [PubMed]
- Erney, R.M.; Malone, W.T.; Skelding, M.B.; Marcon, A.A.; Kleman-Leyer, K.M.; O’Ryan, M.L.; Ruiz-Palacios, G.; Hilty, M.D.; Pickering, L.K.; Prieto, P. A Variability of human milk neutral oligosaccharides in a diverse population. J. Pediatr. Gastroenterol. Nutr. 2000, 30, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, P.; Warren, C.D.; Altaye, M.; Morrow, A.L.; Ruiz-Palacios, G.; Pickering, L.K.; Newburg, D.S. Fucosylated human milk oligosaccharides vary between individuals and over the course of lactation. Glycobiology 2001, 11, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Austin, S.; De Castro, C.; Bénet, T.; Hou, Y.; Sun, H.; Thakkar, S.; Vinyes-Pares, G.; Zhang, Y.; Wang, P. Temporal Change of the Content of 10 Oligosaccharides in the Milk of Chinese Urban Mothers. Nutrients 2016, 8, 346. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.; Davis, J.C.; Goonatilleke, E.; Smilowitz, J.T.; German, J.B.; Lebrilla, C.B. Absolute Quantitation of Human Milk Oligosaccharides Reveals Phenotypic Variations during Lactation. J. Nutr. 2017, 147, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Doherty, A.M.; Lodge, C.J.; Dharmage, S.C.; Dai, X.; Bode, L.; Lowe, A.J. Human Milk Oligosaccharides and Associations With Immune-Mediated Disease and Infection in Childhood: A Systematic Review. Front. Pediatr. 2018, 6, 91. [Google Scholar] [CrossRef]
- Sjögren, Y.M.; Duchén, K.; Lindh, F.; Björkstén, B.; Sverremark-Ekström, E. Neutral oligosaccharides in colostrum in relation to maternal allergy and allergy development in children up to 18 months of age. Pediatr. Allergy Immunol. 2007, 18, 20–26. [Google Scholar] [CrossRef]
- Munblit, D.; Peroni, D.; Boix-Amorós, A.; Hsu, P.; Land, B.; Gay, M.; Kolotilina, A.; Skevaki, C.; Boyle, R.; Collado, M.; et al. Human Milk and Allergic Diseases: An Unsolved Puzzle. Nutrients 2017, 9, 894. [Google Scholar] [CrossRef]
- Chen, Y.-L.; Chen, J.-C.; Lin, T.-M.; Huang, T.-J.; Wang, S.-T.; Lee, M.-F.; Wang, J.-Y. ABO/secretor genetic complex is associated with the susceptibility of childhood asthma in Taiwan. Clin. Exp. Allergy 2005, 35, 926–932. [Google Scholar] [CrossRef]
- Innes, A.L.; McGrath, K.W.; Dougherty, R.H.; McCulloch, C.E.; Woodruff, P.G.; Seibold, M.A.; Okamoto, K.S.; Ingmundson, K.J.; Solon, M.C.; Carrington, S.D.; et al. The H Antigen at Epithelial Surfaces Is Associated with Susceptibility to Asthma Exacerbation. Am. J. Respir. Crit. Care Med. 2011, 183, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Denborough, M.A.; Downing, H.J. Secretor Status in Asthma and Hay Fever*. J. Med. Genet 1968, 5, 302–305. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mandić, Z.; Pirički, A.P.; Kenjerić, D.; Haničar, B.; Tanasić, I. Breast vs. bottle: Differences in the growth of Croatian infants. Matern. Child Nutr. 2011, 7, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Feldman-Winter, L.; Burnham, L.; Grossman, X.; Matlak, S.; Chen, N.; Merewood, A. Weight gain in the first week of life predicts overweight at 2 years: A prospective cohort study. Matern. Child Nutr. 2017, 14, e12472. [Google Scholar] [CrossRef] [PubMed]
- Horta, B.; Victora, C. Long-Term Health Effects of Breastfeeding: A Systematic Review (update); World Health Organization: Geneva, Switzerland, 2013; Volume 129. [Google Scholar]
- Vandenplas, Y.; Berger, B.; Carnielli, V.; Ksiazyk, J.; Lagström, H.; Sanchez Luna, M.; Migacheva, N.; Mosselmans, J.-M.; Picaud, J.-C.; Possner, M.; et al. Human Milk Oligosaccharides: 2′-Fucosyllactose (2′-FL) and Lacto-N-Neotetraose (LNnT) in Infant Formula. Nutrients 2018, 10, 1161. [Google Scholar] [CrossRef] [PubMed]
- Kunz, C.; Rudloff, S. Compositional Analysis and Metabolism of Human Milk Oligosaccharides in Infants. In Intestinal Microbiome: Functional Aspects in Health and Disease; Isolauri, E., Sherman, P., Walker, W., Eds.; Nutr Inst Workshop Ser. Nestec Ltd., Vevey/S. Karger AG: Basel, Switzerland, 2017; Volume 88, pp. 137–147. [Google Scholar]
- Goehring, K.C.; Kennedy, A.D.; Prieto, P.A.; Buck, R.H. Direct evidence for the presence of human milk oligosaccharides in the circulation of breastfed infants. PLoS ONE 2014, 9, e101692. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, P.; Li, C.; Stanya, K.J.; Jacobi, D.; Dai, L.; Liu, S.; Gangl, M.R.; Harn, D.A.; Lee, C.-H. Immunomodulatory glycan LNFPIII alleviates hepatosteatosis and insulin resistance through direct and indirect control of metabolic pathways. Nat. Med. 2012, 18, 1665–1672. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Li, M.; Wu, S.; Lebrilla, C.B.; Chapkin, R.S.; Ivanov, I.; Donovan, S.M. Fecal Microbiota Composition of Breast-Fed Infants Is Correlated With Human Milk Oligosaccharides Consumed. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.C.C.; Lewis, Z.T.; Krishnan, S.; Bernstein, R.M.; Moore, S.E.; Prentice, A.M.; Mills, D.A.; Lebrilla, C.B.; Zivkovic, A.M. Growth and Morbidity of Gambian Infants are Influenced by Maternal Milk Oligosaccharides and Infant Gut Microbiota. Sci. Rep. 2017, 7, 40466. [Google Scholar] [CrossRef]
| HMO | Structure | Fucose Linkages | Group 1: Se+Le+ | Group 2: Se−Le+ | Group 3: Se+Le− | Group 4: Se−Le− |
|---|---|---|---|---|---|---|
| 2’-FL | Fucα1-2Galβ1-4Glc | α1-2 | + | - | + | - |
| LNFP I | Fucα1-2Galβ1-3GlcNAcβ1-3Galβ1-4Glc | α1-2 | + | - | + | - |
| LNDFH I | Fucα1-2Galβ1-3(Fucα1-4)GlcNAcβ1-3Galβ1-4Glc | α1-2 α1-4 | + | - | - | - |
| DFLNH c | 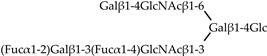 | α1-2 α1-4 | + | - | - | - |
| LNDFH II | Galβ1-3(Fucα1-4)GlcNAcβ1-3Galβ1-4(Fucα1-3)Glc | α1-3 α1-4 | + | + | - | - |
| DFpLNnH | Galβ1-4(Fucα1-3)GlcNAcβ1-3Galβ1-4(Fucα1-3)GlcNAcβ1-3Galβ1-4Glc | α1-3 | + | + | + | + |
| 3’-FL | Galβ1-4(Fucα1-3)Glc | α1-3 | + | + | + | + |
| Variables | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Se+ Le+ | Se− Le+ | Se+ Le− | |
| n = 59 (75.6%) | n = 9 (11.5%) | n = 9 (11.5%) | |
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Age, years | 31 ± 7 | 29 ± 7 | 27 ± 4 |
| BMI, kg/m2 | |||
| At inclusion | 27 ± 5 | 26 ± 4 | 28 ± 5 |
| Pre-gestational | 25 ± 5 | 24 ± 4 | 26 ± 6 |
| Parity, n | 2 ± 1 | 2 ± 1 | 1 ± 0 |
| Postpartum, days | 38 ± 14 | 32 ± 11 | 31 ± 13 |
| n (%) | n (%) | n (%) | |
| Cesarean delivery | 32 (54) | 6 (67) | 2 (22) |
| Allergic disease, yes a | 19 (32) | 0 (0) | 4 (50) |
| Pets, yes b | 18 (38) | 3 (38) | 3 (43) |
| Socioeconomic status | |||
| Class A (n = 6) | 4 (7) | 1 (11) | 1 (11) |
| Class B (n = 45) | 34 (58) | 5 (56) | 6 (67) |
| Class C (n = 26) | 21 (36) | 3 (33) | 2 (22) |
| Education c | |||
| Elementary school (n = 6) | 6 (12) | 0 (0) | 0 (0) |
| High school (n = 31) | 22 (42) | 5 (63) | 4 (50) |
| Graduate (n = 24) | 17 (33) | 3 (38) | 4 (50) |
| Postgraduate (n = 7) | 7 (13) | 0 (0) | 0 (0) |
| Variables | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Se+ Le+ | Se− Le+ | Se+ Le− | |
| n = 59 (75.6%) | n = 9 (11.5%) | n = 9 (11.5%) | |
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Age, days | 38 ± 14 | 32 ± 11 | 31 ± 13 |
| Gestational age, weeks | 39 ± 1 | 39 ± 1 | 39 ± 1 |
| Weight at birth, g | 3237 ± 392 | 3358 ± 579 | 3173 ± 434 |
| Weight at inclusion, g | 4262 ± 764 | 4448 ± 1052 | 4148 ± 730 |
| Length at inclusion, cm | 54 ± 3 | 54 ± 3 | 51 ± 6 |
| Weight gain, g/day a | 26 ± 16 | 24 ± 16 | 25 ± 6 |
| HMOs | Concentration (g/L) | Statistical Analysis a | Multiple Comparison Analysis b | ||
|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | |||
| Se+ Le+ | Se− Le+ | Se+ Le− | |||
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| (CV, %) | (CV, %) | (CV, %) | |||
| Fucosylated | |||||
| 2’-FL | 2.20 ± 0.98 (45) | – | 3.43 ± 1.75 (51) | p = 0.019 | |
| 3’-FL | 0.53 ± 0.33 (63) | 1.62 ± 0.42 (26) | 0.31 ± 0.58 (189) | p < 0.001 | G3 < G1 < G2 |
| LNFP I | 0.73 ± 0.52 (71) | – | 2.03 ± 1.51 (75) | p = 0.015 | |
| LNDFH I | 1.22 ± 0.81 (66) | – | – | – | |
| LNDFH II | 0.02 ± 0.05 (293) | 0.41 ± 0.22 (55) | – | p < 0.001 | |
| DFLNHc | 0.08 ± 0.05 (71) | – | – | – | |
| DFpLNnH | 0.04 ± 0.07 (154) | 0.04 ± 0.03 (72) | 0.05 ± 0.10 (184) | p = 0.702 | |
| Neutral core | |||||
| LNH | 0.08 ± 0.06 (75) | 0.05 ± 0.06 (116) | 0.07 ± 0.06 (94) | p = 0.013 | G1 = G3; G2 = G3; G2 < G1 |
| LNnH | 0.04 ± 0.03 (85) | 0.02 ± 0.03 (151) | 0.02 ± 0.02 (87) | p = 0.010 | G2 = G3; G1 = G3; G2 < G1 |
| LNT + LNnT | 0.38 ± 0.17 (46) | 0.54 ± 0.25 (47) | 0.37 ± 0.25 (67) | p = 0.146 | |
| Acidic | |||||
| 3’-SL | 0.18 ± 0.04 (24) | 0.18 ± 0.05 (28) | 0.17 ± 0.03 (18) | p = 0.736 | |
| 6’-SL | 0.37 ± 0.15 (40) | 0.39 ± 0.23 (59) | 0.41 ± 0.15 (37) | p = 0.640 | |
| LSTa | 0.01 ± 0.01 (104) | 0.01 ± 0.01 (90) | 0.01 ± 0.00 (62) | p = 0.074 | |
| LSTb | 0.07 ± 0.04 (54) | 0.10 ± 0.06 (58) | 0.06 ± 0.03 (53) | p = 0.152 | |
| LSTc | 0.16 ± 0.09 (59) | 0.13 ± 0.08 (64) | 0.14 ± 0.06 (45) | p = 0.005 | G1 = G3; G2 = G3; G2 < G1 |
| Total | |||||
| Fucosylated c | 4.81 ± 1.62 (34) | 2.07 ± 0.61 (29) | 5.83 ± 1.97 (34) | p < 0.001 | G1 = G3; G2 < G1; G2 < G3 |
| Neutral core d | 0.50 ± 0.20 (41) | 0.61 ± 0.26 (42) | 0.46 ± 0.31 (67) | p = 0.243 | |
| Acidic e | 0.79 ± 0.25 (31) | 0.81 ± 0.35 (43) | 0.79 ± 0.21 (27) | p = 0.245 | |
| Total HMOs f | 6.10 ± 1.76 (29) | 3.50 ± 0.84 (24) | 7.08 ± 2.07 (29) | p < 0.001 | G1 = G3; G2 < G1; G2 < G3 |
| HMOs Concentrations | Maternal Variables | Infant Variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parity | Age | Postpartum Days | BMI | Weight | PG Weight | PG BMI | Gestational Age | Weight at Birth | Weight | Length | Weight Gain | |
| Fucosylated | ||||||||||||
| 2’-FL | −0.02 | 0.02 | −0.07 | 0.18 | 0.20 | 0.14 | 0.18 | −0.12 | 0.14 | −0.05 | 0.11 | −0.14 |
| 3’-FL | 0.09 | 0.06 | 0.35 | 0.06 | −0.09 | 0.04 | −0.09 | −0.07 | −0.10 | 0.23 | 0.11 | 0.17 |
| LNFP I | −0.07 | −0.15 | −0.47 | 0.05 | 0.11 | 0.01 | 0.05 | 0.09 | 0.08 | −0.37 | −0.14 | −0.28 |
| LNDFH I | −0.04 | −0.21 | −0.25 | 0.12 | 0.02 | 0.21 | 0.10 | 0.20 | 0.08 | −0.29 | 0.04 | −0.37 |
| LNDFH II | 0.07 | 0.04 | 0.27 | −0.02 | −0.13 | 0.01 | −0.08 | −0.14 | −0.14 | 0.08 | 0.01 | −0.02 |
| DFLNHc | −0.08 | 0.01 | −0.24 | 0.13 | 0.16 | 0.15 | 0.14 | 0.12 | 0.05 | −0.06 | 0.07 | 0.04 |
| DFpLNnH | 0.05 | −0.09 | 0.01 | 0.01 | −0.03 | 0.12 | 0.08 | −0.08 | −0.20 | −0.16 | −0.22 | −0.14 |
| Neutral core | ||||||||||||
| LNH | −0.05 | 0.01 | −0.42 | 0.02 | 0.17 | −0.03 | 0.04 | 0.17 | 0.04 | −0.20 | −0.23 | 0.06 |
| LNnH | −0.12 | 0.05 | 0.10 | 0.11 | 0.23 | 0.14 | 0.25 | −0.04 | 0.06 | 0.09 | 0.02 | 0.07 |
| LNT+LNnT | 0.02 | −0.15 | −0.54 | −0.13 | −0.08 | −0.13 | −0.13 | 0.21 | 0.04 | −0.39 | −0.32 | −0.13 |
| Acidic | ||||||||||||
| 3’-SL | −0.07 | 0.01 | −0.25 | −0.12 | −0.10 | −0.16 | −0.18 | −0.08 | −0.17 | −0.34 | −0.32 | −0.25 |
| 6’-SL | 0.11 | 0.05 | −0.71 | −0.02 | −0.07 | −0.01 | −0.09 | 0.22 | 0.07 | −0.49 | −0.25 | −0.30 |
| LSTa | −0.06 | 0.01 | −0.62 | −0.15 | −0.12 | −0.14 | −0.17 | 0.25 | 0.01 | −0.41 | −0.29 | −0.20 |
| LSTb | 0.05 | −0.17 | −0.26 | −0.08 | −0.07 | −0.12 | −0.11 | 0.01 | 0.03 | −0.30 | −0.22 | −0.21 |
| LSTc | 0.05 | −0.01 | −0.76 | −0.04 | −0.07 | 0.02 | −0.05 | 0.25 | 0.02 | −0.54 | −0.28 | −0.36 |
| Total | ||||||||||||
| Fucosylated | −0.10 | −0.13 | −0.24 | 0.14 | 0.13 | 0.13 | 0.13 | 0.05 | 0.11 | −0.27 | 0.01 | −0.32 |
| Neutral core | −0.03 | −0.07 | −0.51 | −0.07 | 0.04 | −0.11 | −0.07 | 0.25 | 0.09 | −0.33 | −0.32 | −0.03 |
| Acidic | 0.05 | 0.02 | −0.79 | −0.07 | −0.10 | −0.05 | −0.13 | 0.26 | 0.01 | −0.61 | −0.35 | −0.42 |
| Total HMOs | −0.06 | −0.11 | −0.43 | 0.15 | 0.13 | 0.14 | 0.11 | 0.10 | 0.13 | −0.39 | −0.10 | −0.37 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
M. Tonon, K.; B. de Morais, M.; F. V. Abrão, A.C.; Miranda, A.; B. Morais, T. Maternal and Infant Factors Associated with Human Milk Oligosaccharides Concentrations According to Secretor and Lewis Phenotypes. Nutrients 2019, 11, 1358. https://doi.org/10.3390/nu11061358
M. Tonon K, B. de Morais M, F. V. Abrão AC, Miranda A, B. Morais T. Maternal and Infant Factors Associated with Human Milk Oligosaccharides Concentrations According to Secretor and Lewis Phenotypes. Nutrients. 2019; 11(6):1358. https://doi.org/10.3390/nu11061358
Chicago/Turabian StyleM. Tonon, Karina, Mauro B. de Morais, Ana Cristina F. V. Abrão, Antonio Miranda, and Tania B. Morais. 2019. "Maternal and Infant Factors Associated with Human Milk Oligosaccharides Concentrations According to Secretor and Lewis Phenotypes" Nutrients 11, no. 6: 1358. https://doi.org/10.3390/nu11061358
APA StyleM. Tonon, K., B. de Morais, M., F. V. Abrão, A. C., Miranda, A., & B. Morais, T. (2019). Maternal and Infant Factors Associated with Human Milk Oligosaccharides Concentrations According to Secretor and Lewis Phenotypes. Nutrients, 11(6), 1358. https://doi.org/10.3390/nu11061358





