Improvement of Attention, Executive Functions, and Processing Speed in Elderly Women as a Result of Involvement in the Nordic Walking Training Program and Vitamin D Supplementation
Abstract
:1. Introduction
1.1. Cognitive Functioning in the Elderly
1.2. Nordic Walking—A Proposition for Physical Activity for the Elderly
1.3. Physical Activity Protecting against Aging Processes
1.4. Vitamin D Supplementation
1.5. Present Study
2. Methods
2.1. Participants
2.2. Procedure
2.2.1. Training Sessions
2.2.2. Vitamin D Supplementation
2.2.3. Cognitive and Psychological Assessment
2.2.4. Ethics Statement
2.3. Measurement Tools
2.3.1. NW Training Units
2.3.2. D2 Test of Attention (D2)
2.3.3. Trail Making Test A&B (TMT A&B)
2.3.4. Short Form Health Survey (SF-36 v. II)
2.3.5. The Beck Depression Inventory (BDI-2)
2.3.6. Statistical Analysis
3. Results
3.1. Nordic Walking with Vitamin D Supplementation and Cognitive Functioning Improvement
3.2. Nordic Walking with Vitamin D Supplementation and Quality of Life Improvement
3.3. Severity of Depressive Symptoms after Nordic Walking Program and Vitamin D Supplementation
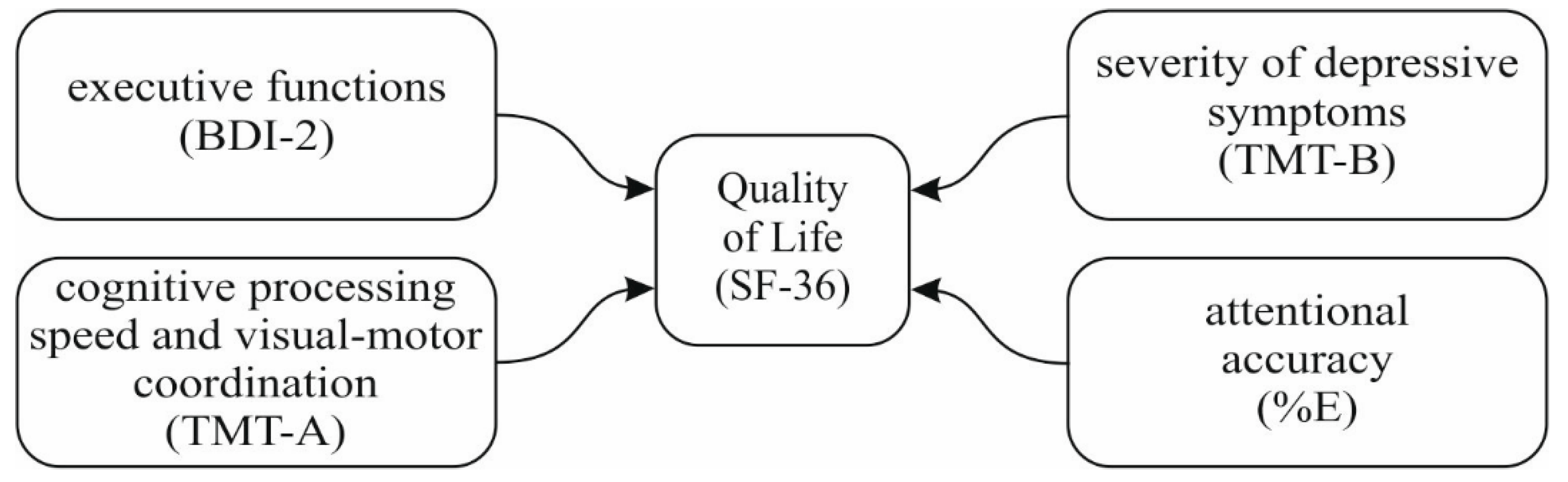
3.4. Quality of Life, Cognitive Functioning, and Severity of Depressive Symptoms
3.4.1. Before Participating in the Program
3.4.2. After the Program
3.4.3. Changes in Vitamin D Concentration
4. Discussion
4.1. Attention and Executive Functions
4.2. Quality of Life
4.3. Depressive Symptoms
4.4. Quality of Life Predictors
5. Limitations
6. Conclusions
- The involvement in Nordic Walking training supported by vitamin D supplementation can strengthen the cognitive functioning of older people—specifically, attention and executive functions.
- Nordic Walking training with vitamin D supplementation may have a partial influence on the perceived quality of life of older women.
- Nordic Walking training can contribute to the improvement in the mental health of older women, reflected in a decrease of depressive symptoms.
- Improvement of cognitive functions and mental state, as a result of involvement in the Nordic Walking training, may partially transfer to subjectively perceived quality of life.
- Physical activity and proper nutrition can be key factors in maintaining self-reliance in old age.
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Mazzonna, F.; Peracchi, F. Unhealthy Retirement? J. Hum. Resour. 2017, 52, 128–151. [Google Scholar] [CrossRef]
- Brown, C.J.; Flood, K.L. Mobility limitation in the older patient: A clinical review. JAMA 2013, 310, 1168–1177. [Google Scholar] [CrossRef]
- Duan, D.; Dong, Y.; Zhang, H.; Zhao, Y.; Diao, Y.; Cui, Y.; Wang, J.; Chai, Q.; Liu, Z. Empty-nest-related psychological distress is associated with progression of brain white matter lesions and cognitive impairment in the elderly. Sci. Rep. 2017, 7, 43816. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.; McMunn, A.; Demakakos, P.; Hamer, M.; Steptoe, A. Social isolation and loneliness: Prospective associations with functional status in older adults. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2017, 36, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Perissinotto, C.M.; Stijacic, C.I.; Covinsky, K.E. Loneliness in older persons: A predictor of functional decline and death. Arch. Internal Med. 2012, 172, 1078–1083. [Google Scholar] [CrossRef] [PubMed]
- Eloranta, S.; Arve, S.; Isoaho, H.; Lehtonen, A.; Viitanen, M. Loneliness of older people aged 70: A comparison of two Finnish cohorts born 20 years apart. Arch. Gerontol. Geriatr. 2015, 61, 254–260. [Google Scholar] [CrossRef]
- Li, D.; Zhang, D.J.; Shao, J.J.; Qi, X.D.; Tian, L. A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Arch. Gerontol. Geriatr. 2014, 58, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gangolli, V. Recent advances in the understanding of cognitive decline among the elderly. J. Geriatr. Mental Health 2016, 3, 36–43. [Google Scholar] [CrossRef]
- Garcia, S.; Gunstad, J. Sleep and physical activity as modifiable risk factors in age-associated cognitive decline. Sleep Biol. Rhythm. 2016, 14, 3–11. [Google Scholar] [CrossRef]
- Maruya, K.; Fujita, H.; Arai, T.; Hosoi, T.; Ogiwara, K.; Moriyama, S.; Ishibashi, H. Identifying elderly people at risk for cognitive decline by using the 2-step test. J. Phys. Ther. Sci. 2018, 30, 145–149. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Chen, K.; Pan, Y.; Jing, F.; Liu, H. Associations and Impact Factors between Living Arrangements and Functional Disability among Older Chinese Adults. PLoS ONE 2013, 8, e53879. [Google Scholar] [CrossRef] [PubMed]
- Raz, N.; Lindenberger, U.; Rodrigue, K.M.; Kennedy, K.M.; Head, D.; Williamson, A.; Dahle, C.; Gerstorf, D.; Acker, J.D. Regional brain changes in aging healthy adults: General trends, individual differences and modifiers. Cereb. Cortex 2005, 15, 1676–1689. [Google Scholar] [CrossRef] [PubMed]
- Resnick, S.M.; Pham, D.L.; Kraut, M.A.; Zonderman, A.B.; Davatzikos, C. Longitudinal magnetic resonance imaging studies of older adults: A shrinking brain. J. Neurosci. Off. J. Soc. Neurosci. 2003, 23, 3295–3301. [Google Scholar] [CrossRef]
- Salat, D.H.; Lee, S.Y.; van der Kouwe, A.J.; Greve, D.N.; Fischl, B.; Rosas, H.D. Age-associated alterations in cortical gray and white matter signal intensity and gray to white matter contrast. Neuroimage 2009, 48, 21–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedden, T.; Gabrieli, J.D. Insights into the ageing mind: A view from cognitive neuroscience. Nat. Rev. Neurosci. 2004, 5, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Kremen, W.S.; Lachman, M.E.; Pruessner, J.C.; Sliwinski, M.; Wilson, R.S. Mechanisms of age-related cognitive change and targets for intervention: Social interactions and stress. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 760–765. [Google Scholar] [CrossRef] [PubMed]
- DeCarli, C.; Kawas, C.; Morrison, J.H.; Reuter-Lorenz, P.A.; Sperling, R.A.; Wright, C.B. Session II: Mechanisms of age-related cognitive change and targets for intervention: Neural circuits, networks, and plasticity. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 747–753. [Google Scholar] [CrossRef]
- Huffman, K. The developing, aging neocortex: How genetics and epigenetics influence early developmental patterning and age-related change. Front. Genet. 2012, 3, 212. [Google Scholar] [CrossRef] [PubMed]
- Ossowski, Z.; Prusik, K.; Prusik, K.; Kortas, J.; Wiech, M.; Bielawa, Ł. Nordic Walking Training and Physical Fitness in Elderly. Pol. J. Sport Touris. 2015, 21, 253–257. [Google Scholar] [CrossRef]
- Saulicz, M.; Saulicz, E.; Myśliwiec, A.; Wolny, T.; Linek, P.; Knapik, A.; Rottermund, J. Effect of a 4-week Nordic walking training on the physical fitness and self-assessment of the quality of health of women of the perimenopausal age. Menopause Rev. Przegląd Menopauzalny 2015, 14, 105–111. [Google Scholar] [CrossRef]
- Soboleva, A.A.; Iskakova, G.S.; Khasanova, R.R.; Andreev, V.I.; Zagrevsky, O.I.; Nikonova, D.U. The impact of Nordic walking trainings on social well-being of women at the age of 50–60. SHS Web Conf. 2016, 28, 01097. [Google Scholar] [CrossRef]
- Kocur, P.; Wilk, M. Nordic Walking—A new form of exercise in rehabilitation. Med. Rehabil. 2006, 10, 1–8. [Google Scholar]
- Gomenuka, N.A.; Oliveira, H.B.; Silva, E.S.; Costa, R.R.; Kanitz, A.C.; Liedtke, G.V.; Schuch, F.B.; Peyre-Tartaruga, L.A. Effects of Nordic walking training on quality of life, balance and functional mobility in elderly: A randomized clinical trial. PLoS ONE 2019, 14, e0211472. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.; Kwon, H.; Kim, H.; Kim, B.; Jung, J. Comparison of the Effects of Walking with and without Nordic Pole on Upper Extremity and Lower Extremity Muscle Activation. J. Phys. Ther. Sci. 2013, 25, 1553–1556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boccia, G.; Zoppirolli, C.; Bortolan, L.; Schena, F.; Pellegrini, B. Shared and task-specific muscle synergies of Nordic walking and conventional walking. Scand. J. Med. Sci. Sports 2018, 28, 905–918. [Google Scholar] [CrossRef] [PubMed]
- Takeshima, N.; Islam, M.M.; Rogers, M.E.; Rogers, N.L.; Sengoku, N.; Koizumi, D.; Kitabayashi, Y.; Imai, A.; Naruse, A. Effects of nordic walking compared to conventional walking and band-based resistance exercise on fitness in older adults. J. Sports Sci. Med. 2013, 12, 422–430. [Google Scholar] [PubMed]
- Schiffer, T.; Knicker, A.; Hoffman, U.; Harwig, B.; Hollmann, W.; Struder, H.K. Physiological responses to nordic walking, walking and jogging. Eur. J. Appl. Physiol. 2006, 98, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Ossowski, Z.; Prusik, K.; Kortas, J.; Wiech, M.; Prusik, K.; Słomska, H.; Bielawa, Ł. Zmiany poziomu siły konczyn gornych i dolnych pod wplywem treningu Nordic Walking u kobiet w starszym wieku [Changes in the level of strength of upper and lower limbs under Nordic walking training in elderly women]. Rocz. Nauk. 2010, 20, 71–78. [Google Scholar]
- Church, T.S.; Earnest, C.P.; Morss, G.M. Field testing of physiological responses associated with Nordic Walking. Res. Q. Exerc. Sport 2002, 73, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Porcari, J.P.; Hendrickson, T.L.; Walter, P.R.; Terry, L.; Walsko, G. The physiological responses to walking with and without Power Poles on treadmill exercise. Res. Q. Exerc. Sport 1997, 68, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Hagner, W.; Hagner-Derengowska, M.; Wiacek, M.; Zubrzycki, I.Z. Changes in level of VO2max, blood lipids, and waist circumference in the response to moderate endurance training as a function of ovarian aging. Menopause 2009, 16, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.Y.; Becke, A.; Berron, D.; Becker, B.; Sah, N.; Benoni, G.; Janke, E.; Lubejko, S.T.; Greig, N.H.; Mattison, J.A.; et al. Running-induced systemic Cathepsin B secretion is associated with memory function. Cell Metab. 2016, 24, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Tschentscher, M.; Niederseer, D.; Niebauer, J. Health benefits of Nordic walking: A systematic review. Am. J. Prev. Med. 2013, 44, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Cugusi, L.; Manca, A.; Yeo, T.J.; Bassareo, P.P.; Mercuro, G.; Kaski, J.C. Nordic walking for individuals with cardiovascular disease: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Prev. Cardiol. 2017, 24, 1938–1955. [Google Scholar] [CrossRef] [PubMed]
- Warlop, T.; Detrembleur, C.; Buxes Lopez, M.; Stoquart, G.; Lejeune, T.; Jeanjean, A. Does Nordic Walking restore the temporal organization of gait variability in Parkinson’s disease? J. Neuroeng. Rehabil. 2017, 14, 17. [Google Scholar] [CrossRef]
- Upeniece, I.; Vīnberga, I.; Arnis, V.; Erts, R. Women’s motivation to engage with the Nordic Walking. Soc. Integr. Educ. Proc. Int. Sci. Conf. 2016, 3, 581–591. [Google Scholar]
- Knapik, A.; Saulicz, E.; Mysliwiec, A.; Saulicz, M.; Warmuz-Wancisiewicz, A. Motivations and effects of practicing Nordic Walking by elderly people. Balt. J. Health Phys. Act. 2014, 6, 34–40. [Google Scholar] [CrossRef]
- Kumar, A.; Kopra, J.; Varendi, K.; Porokuokka, L.L.; Panhelainen, A.; Kuure, S.; Marshall, P.; Karalija, N.; Härma, M.A.; Vilenius, C.; et al. GDNF Overexpression from the Native Locus Reveals its Role in the Nigrostriatal Dopaminergic System Function. PLoS Genet. 2015, 11, e1005710. [Google Scholar] [CrossRef]
- Gamrowska, A.; Steuden, S. Coping with the events of daily life and quality of life of the socially active elderly. Health Psychol. Rep. 2014, 2, 123–131. [Google Scholar] [CrossRef]
- Park, S.D.; Yu, S.H. The effects of Nordic and general walking on depression disorder patients’ depression, sleep, and body composition. J. Phys. Ther. Sci. 2015, 27, 2481–2485. [Google Scholar] [CrossRef]
- Suija, K.; Pechter, U.; Kalda, R.; Tahepold, H.; Maaroos, J.; Maaroos, H.I. Physical activity of depressed patients and their motivation to exercise: Nordic Walking in family practice. Int. J. Rehabil. Res. Int. Z. Rehabil. Rev. Int. Rech. Readapt. 2009, 32, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Chenet, A.; Gosseaume, A.; Wiertlewski, S.; Perrouin-Verbe, B. Efficacity of exercise training on multiple sclerosis patients with cognitive impairments. Ann. Phys. Rehabil. Med. 2016, 59, e42. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, J.H. Effects of Nordic walking on physical functions and depression in frail people aged 70 years and above. J. Phys. Ther. Sci. 2015, 27, 2453–2456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zając-Lamparska, L.; Trempała, J. Effects of working memory and attentional control training and their transfer onto fluid intelligence in early and late adulthood. Health Psychol. Rep. 2016, 4, 41–53. [Google Scholar] [CrossRef]
- Muscari, A.; Giannoni, C.; Pierpaoli, L.; Berzigotti, A.; Maietta, P.; Foschi, E.; Ravaioli, C.; Poggiopollini, G.; Bianchi, G.; Magalotti, D.; et al. Chronic endurance exercise training prevents aging-related cognitive decline in healthy older adults: A randomized controlled trial. Int. J. Geriatr. Psychiatry 2010, 25, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Shubert, T.E.; McCulloch, K.; Hartman, M.; Giuliani, C.A. The effect of an exercise-based balance intervention on physical and cognitive performance for older adults: A pilot study. J. Geriatr. Phys. Ther. 2010, 33, 157–164. [Google Scholar]
- Langlois, F.; Vu, T.T.; Chasse, K.; Dupuis, G.; Kergoat, M.J.; Bherer, L. Benefits of physical exercise training on cognition and quality of life in frail older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2013, 68, 400–404. [Google Scholar] [CrossRef]
- Wang, H.X.; Jin, Y.; Hendrie, H.C.; Liang, C.; Yang, L.; Cheng, Y.; Unverzagt, F.W.; Ma, F.; Hall, K.S.; Murrell, J.R.; et al. Late life leisure activities and risk of cognitive decline. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 205–213. [Google Scholar] [CrossRef]
- Wienert, J.; Kuhlmann, T.; Lippke, S. Direct effects of a domain-specific subjective age measure on self-reported physical activity—Is it more important how old you are or how old you feel? Health Psychol. Rep. 2015, 3, 131–139. [Google Scholar] [CrossRef]
- Young, J.; Angevaren, M.; Rusted, J.; Tabet, N. Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst. Rev. 2015, 4, CD005381. [Google Scholar] [CrossRef]
- Appelman, A.P.; van der Graaf, Y.; Vincke, K.L.; Mali, W.P.; Geerlings, M.I. Combined effect of cerebral hypoperfusion and white matter lesions on executive functioning—The SMART-MR study. Dement. Geriatr. Cogn. Disord. 2010, 29, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Meissner, A. Hypertension and the Brain: A Risk Factor for More than Heart Disease. Cerebrovasc. Dis. 2016, 42, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Voss, M.W.; Heo, S.; Prakash, R.S.; Erickson, K.I.; Alves, H.; Chaddock, L.; Szabo, A.N.; Mailey, E.L.; Wójcicki, T.R.; White, S.M.; et al. The influence of aerobic fitness on cerebral white matter integrity and cognitive function in older adults: Results of a one-year exercise intervention. Hum. Brain Mapp. 2013, 4, 2972–2985. [Google Scholar] [CrossRef] [PubMed]
- Kmieć, P.; Żmijewski, M.; Lizakowska-Kmieć, M.; Sworczak, K. Widespread vitamin D deficiency among adults from northern Poland (54°N) after months of low and high natural UVB radiation. Endokrynologia Polska 2015, 66, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Annweiler, C.; Schott, A.M.; Allali, G.; Bridenbaugh, S.A.; Kressig, R.W.; Allain, P.; Herrmann, F.R.; Beauchet, O. Association of vitamin D deficiency with cognitive impairment in older women: Cross-sectional study. Neurology 2010, 74, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, D.J.; Lang, I.A.; Langa, K.M.; Melzer, D. Vitamin D and cognitive impairment in the elderly U.S. population. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Pettersen, J.A. Does high dose vitamin D supplementation enhance cognition?: A randomized trial in healthy adults. Exp. Gerontol. 2017, 90, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Buell, J.S.; Scott, T.M.; Dawson-Hughes, B.; Dallal, G.E.; Rosenberg, I.H.; Folstein, M.F.; Tucker, K.L. Vitamin D Iis associated with cognitive function in elders receiving home health services. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2009, 64A, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Balion, C.; Griffith, L.E.; Strifler, L.; Henderson, M.; Patterson, C.; Heckman, G.; Llewellyn, D.J.; Raina, P. Vitamin D, cognition, and dementia: A systematic review and meta-analysis. Neurology 2012, 79, 1397–1405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wicherts, I.S.; van Schoor, N.M.; Boeke, A.J.; Visser, M.; Deeg, D.J.; Smit, J.; Knol, D.L.; Lips, P. Vitamin D status predicts physical performance and its decline in older persons. J. Clin. Endocrinol. Metab. 2007, 92, 2058–2065. [Google Scholar] [CrossRef]
- Gmiat, A.; Jaworska, J.; Micielska, K.; Kortas, J.; Prusik, K.; Prusik, K.; Lipowski, M.; Radulska, A.; Szupryczynska, N.; Antosiewicz, J.; et al. Improvement of cognitive functions in response to a regular Nordic walking training in elderly women—A change dependent on the training experience. Exp. Gerontol. 2018, 104, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Brickenkamp, R.; Zillmer, E. The d2 Test of Attention; Hogrefe Huber Publishers: Washington, DC, USA, 1998. [Google Scholar]
- Kądzielawa, D. (Ed.) Podręcznik do Baterii Testów Neuropsychologicznych Halsteada-Reitana [Manual for the Battery of Halstead-Rean’s Neuropsychological Tests]; Faculty of Psychology University of Warsaw: Warsaw, Poland, 1990; Unpublished manuscript. [Google Scholar]
- Reitan, R.M. Validity of the Trail Making Test as an Indicator of Organic Brain Damage. Percept. Motor Skills 1958, 8, 271–276. [Google Scholar] [CrossRef]
- Gandek, B.; Sinclair, S.J.; Kosinski, M.; Ware, J.E., Jr. Psychometric evaluation of the SF-36 health survey in Medicare managed care. Health Care Financ. Rev. 2004, 25, 5–25. [Google Scholar] [PubMed]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J. Pers. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Dajek, E.R.; Brickenkamp, R. Polska Standaryzacja Testu d2, Testu Badania Uwagi R; Brickenkampa, Erda: Warszawa, Poland, 2003. [Google Scholar]
- Talarowska, M.; Zboralski, K.; Mossakowska-Wójcik, J.; Gałecki, P. Wykonanie Testu Łączenia Punktów przez osoby z depresją i organicznymi zaburzeniami depresyjnymi [Results of the Trail Making Test among patients suffering from depressive disorders and organic depressive disorders]. Psychiatr. Polska 2012, 46, 273–282. [Google Scholar]
- Miyake, A.; Friedman, N.P.; Emerson, M.J.; Witzki, A.H.; Howerter, A.; Wager, T.D. The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: A latent variable analysis. Cogn. Psychol. 2000, 41, 49–100. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports. Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef] [PubMed]
- Scicchitano, P.; Cameli, M.; Maiello, M.; Modesti, P.A.; Muiesan, M.L.; Novo, S.; Ciccone, M.M. Nutraceuticals and dyslipidaemia: Beyond the common therapeutics. J. Funct. Foods 2014, 6, 11–32. [Google Scholar] [CrossRef]
| Dependent Variables | First Measurement | Second Measurement | t-Test | p-Value | Post Hoc Power | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| TN 1 | 405.39 | 88.39 | 419.91 | 93.85 | −1.64 | n.s. | 0.16 |
| %E 2 | 9.39% | 4.60% | 7.71% | 5.26% | 3.36 | 0.001 | 0.40 |
| TN-E 3 | 364.90 | 82.34 | 383.84 | 82.78 | −2.37 | 0.011 | 0.26 |
| CP 4 | 132.96 | 33.33 | 142.53 | 32.09 | −3.10 | 0.002 | 0.34 |
| Dependent Variables | First Measurement | Second Measurement | t-Test | p-Value | Post Hoc Power | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| TMT-A 1 (s) | 30.14 | 6.74 | 27.93 | 9.39 | 1.71 | 0.047 | 0.28 |
| TMT-B 2 (s) | 87.17 | 27.69 | 79.07 | 31.45 | 1.76 | 0.043 | 0.32 |
| Dependent Variables | First Measurement | Second Measurement | t-Test | p-Value | Post Hoc Power | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Physical functioning | 82.70 | 13.98 | 81.17 | 14.96 | 0.80 | n.s. | 0.08 |
| Role limitations due to physical health | 68.75 | 16.79 | 69.02 | 19.84 | −0.11 | n.s. | 0.06 |
| Bodily pain | 20.42 | 9.32 | 18.30 | 9.77 | 1.34 | n.s. | 0.22 |
| General health | 51.44 | 15.11 | 47.02 | 13.01 | 2.48 | 0.009 | 0.38 |
| Vitality | 68.50 | 15.06 | 69.28 | 15.65 | −0.40 | n.s. | 0.08 |
| Social functioning | 82.25 | 18.70 | 78.46 | 21.39 | 1.33 | n.s. | 0.20 |
| Role limitations due to emotional problems | 82.17 | 17.70 | 79.79 | 19.92 | 1.13 | n.s. | 0.14 |
| Mental health | 75.10 | 15.35 | 77.34 | 13.09 | −1.14 | n.s. | 0.16 |
| Physical health component | 60.41 | 10.93 | 58.35 | 11.74 | 1.55 | n.s. | 0.18 |
| Mental health component | 75.75 | 13.23 | 75.72 | 13.52 | 0.02 | n.s. | 0.06 |
| Quality of life index | 67.45 | 10.99 | 66.32 | 11.57 | 0.88 | n.s. | 0.10 |
| Dependent Variables | First Measurement | Second Measurement | t-Test | p-Value | Post Hoc Power | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| BDI-2 | 8.83 | 5.46 | 7.73 | 5.50 | 2.00 | 0.026 | 0.18 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lipowski, M.; Walczak-Kozłowska, T.; Lipowska, M.; Kortas, J.; Antosiewicz, J.; Falcioni, G.; Ziemann, E. Improvement of Attention, Executive Functions, and Processing Speed in Elderly Women as a Result of Involvement in the Nordic Walking Training Program and Vitamin D Supplementation. Nutrients 2019, 11, 1311. https://doi.org/10.3390/nu11061311
Lipowski M, Walczak-Kozłowska T, Lipowska M, Kortas J, Antosiewicz J, Falcioni G, Ziemann E. Improvement of Attention, Executive Functions, and Processing Speed in Elderly Women as a Result of Involvement in the Nordic Walking Training Program and Vitamin D Supplementation. Nutrients. 2019; 11(6):1311. https://doi.org/10.3390/nu11061311
Chicago/Turabian StyleLipowski, Mariusz, Tamara Walczak-Kozłowska, Małgorzata Lipowska, Jakub Kortas, Jędrzej Antosiewicz, Giancarlo Falcioni, and Ewa Ziemann. 2019. "Improvement of Attention, Executive Functions, and Processing Speed in Elderly Women as a Result of Involvement in the Nordic Walking Training Program and Vitamin D Supplementation" Nutrients 11, no. 6: 1311. https://doi.org/10.3390/nu11061311
APA StyleLipowski, M., Walczak-Kozłowska, T., Lipowska, M., Kortas, J., Antosiewicz, J., Falcioni, G., & Ziemann, E. (2019). Improvement of Attention, Executive Functions, and Processing Speed in Elderly Women as a Result of Involvement in the Nordic Walking Training Program and Vitamin D Supplementation. Nutrients, 11(6), 1311. https://doi.org/10.3390/nu11061311







