Feasibility and Preliminary Efficacy of the Eating Advice to Students (EATS) Brief Web-Based Nutrition Intervention for Young Adult University Students: A Pilot Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Intervention: Eating Advice to Students
2.4. Attention Control Group
2.5. Measures
2.5.1. Process Evaluation Measures
2.5.2. Impact Evaluation Measures
2.5.3. Measures of Potential Contamination
2.6. Sample Size
2.7. Randomization
2.8. Data Analysis Plan
3. Results
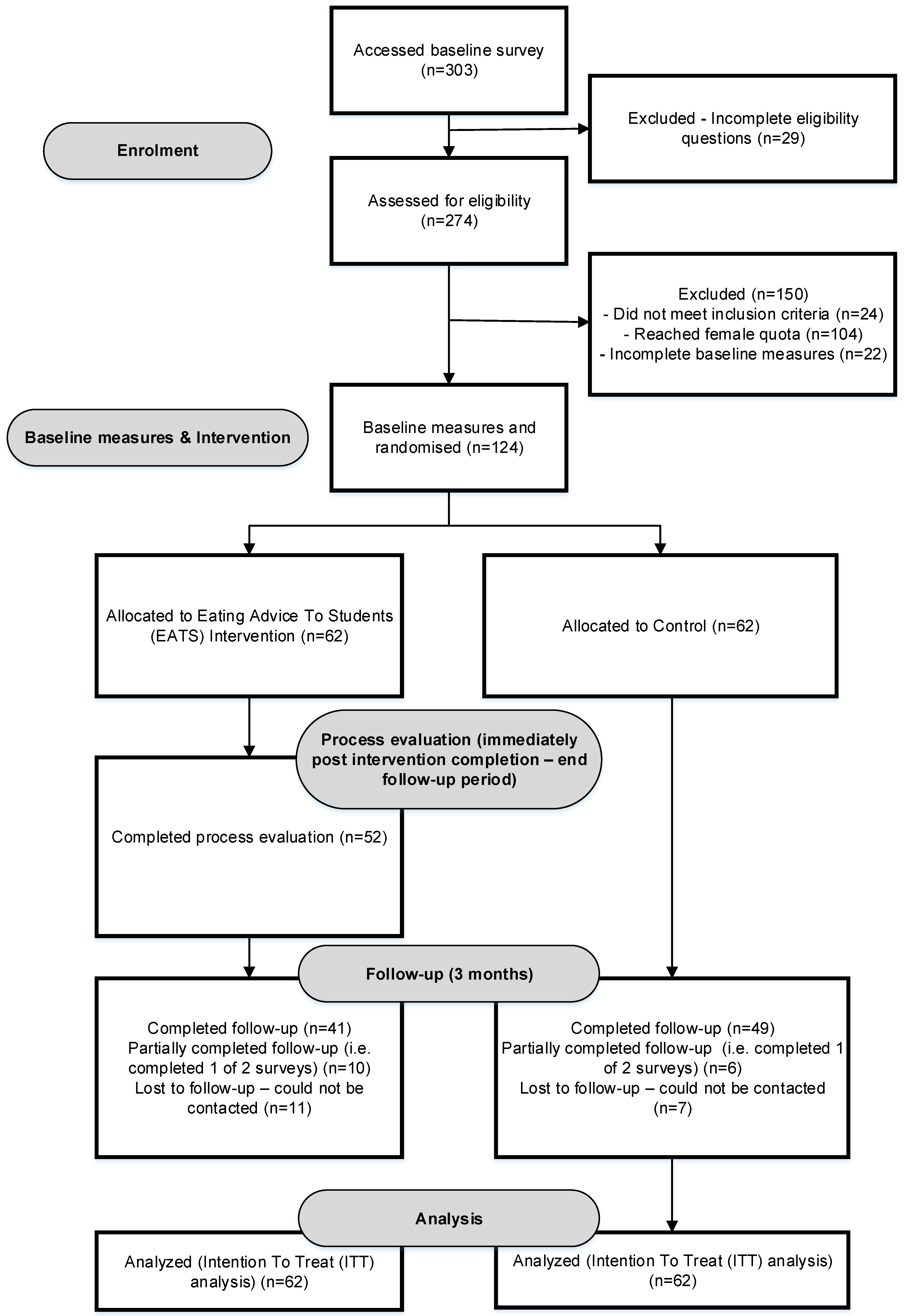
3.1. Recruitment
3.2. Participants at Baseline
3.3. Retention
3.4. Intervention Usage
3.5. Program Acceptability
3.6. Measures of Potential Contamination
3.7. Estimation of Treatment Effect
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Winpenny, E.M.; van Sluijs, E.M.F.; White, M.; Klepp, K.-I.; Wold, B.; Lien, N. Changes in diet through adolescence and early adulthood: Longitudinal trajectories and association with key life transitions. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 86. [Google Scholar] [CrossRef]
- Munt, A.E.; Partridge, S.R.; Allman-Farinelli, M. The barriers and enablers of healthy eating among young adults: A missing piece of the obesity puzzle: A scoping review. Obes. Rev. 2017, 18, 1–17. [Google Scholar] [CrossRef]
- Deliens, T.; Van Crombruggen, R.; Verbruggen, S.; De Bourdeaudhuij, I.; Deforche, B.; Clarys, P. Dietary interventions among university students: A systematic review. Appetite 2016, 105, 14–26. [Google Scholar] [CrossRef]
- Liu, K.; Daviglus, M.L.; Loria, C.M.; Colangelo, L.A.; Spring, B.; Moller, A.C.; Lloyd-Jones, D.M. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The coronary artery risk development in (young) adults (CARDIA) study. Circulation 2012, 125, 996–1004. [Google Scholar] [CrossRef]
- Wattick, R.A.; Hagedorn, R.L.; Olfert, M.D. Relationship between diet and mental health in a young adult appalachian college population. Nutrients 2018, 10, 25. [Google Scholar] [CrossRef] [PubMed]
- Tran, A.; Tran, L.; Geghre, N.; Darmon, D.; Rampal, M.; Brandone, D.; Gozzo, J.M.; Haas, H.; Rebouillat-Savy, K.; Caci, H.; et al. Health assessment of french university students and risk factors associated with mental health disorders. PLoS ONE Electron. Resour. 2017, 12, e0188187. [Google Scholar] [CrossRef]
- Burrows, T.L.; Whatnall, M.C.; Patterson, A.J.; Hutchesson, M.J. Associations between dietary intake and academic achievement in college students: A systematic review. Healthcare 2017, 5, 60. [Google Scholar] [CrossRef] [PubMed]
- Lotrean, L.M.; Stan, O.; Codruta, L.; Laza, V. Dietary patterns, physical activity, body mass index, weight-related behaviours and their interrelationship among romanian university students-trends from 2003 to 2016. Nutr. Hosp. 2018, 35, 375–383. [Google Scholar] [PubMed]
- Chourdakis, M.; Tzellos, T.; Pourzitaki, C.; Toulis, K.A.; Papazisis, G.; Kouvelas, D. Evaluation of dietary habits and assessment of cardiovascular disease risk factors among greek university students. Appetite 2011, 57, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Allman-Farinelli, M.A. Nutrition promotion to prevent obesity in young adults. Healthcare 2015, 3, 809–821. [Google Scholar] [CrossRef]
- Plotnikoff, R.C.; Costigan, S.A.; Williams, R.L.; Hutchesson, M.J.; Kennedy, S.G.; Robards, S.L.; Allen, J.; Collins, C.E.; Callister, R.; Germov, J. Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 45–55. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, L.M.; Palfai, T.P. Efficacy of a brief web-based intervention with and without sms to enhance healthy eating behaviors among university students. Eat. Behav. 2016, 23, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Brookie, K.L.; Mainvil, L.A.; Carr, A.C.; Vissers, M.C.; Conner, T.S. The development and effectiveness of an ecological momentary intervention to increase daily fruit and vegetable consumption in low-consuming young adults. Appetite 2017, 108, 32–41. [Google Scholar] [CrossRef]
- Rompotis, C.J.; Grove, J.R.; Byrne, S.M. Benefits of habit-based informational interventions: A randomised controlled trial of fruit and vegetable consumption. Aust. N. Z. J. Public Health 2014, 38, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Oosterveen, E.; Tzelepis, F.; Ashton, L.; Hutchesson, M.J. A systematic review of ehealth behavioral interventions targeting smoking, nutrition, alcohol, physical activity and/or obesity for young adults. Prev. Med. 2017. [Google Scholar] [CrossRef]
- Werch, C.C.; Grenard, J.L.; Burnett, J.; Watkins, J.A.; Ames, S.; Jobli, E. Translation as a function of modality: The potential of brief interventions. Eval. Health Prof. 2006, 29, 89–125. [Google Scholar] [CrossRef]
- Whatnall, M.C.; Patterson, A.J.; Ashton, L.M.; Hutchesson, M.J. Effectiveness of brief nutrition interventions on dietary behaviours in adults: A systematic review. Appetite 2018, 120, 335–347. [Google Scholar] [CrossRef] [PubMed]
- Dotson, K.B.; Dunn, M.E.; Bowers, C.A. Stand-alone personalized normative feedback for college student drinkers: A meta-analytic review, 2004 to 2014. PLoS ONE 2015, 10, e0139518. [Google Scholar] [CrossRef] [PubMed]
- Green, L.W.; Kreuter, M.W.; Deeds, S.G.; Partridge, K.B.; Bartlett, E. Health Education Planning: A Diagnostic Approach; Mayfield Publishing Company: Palo Alto, CA, USA, 1980. [Google Scholar]
- Whatnall, M.; Patterson, A.; Hutchesson, M. A brief web-based nutrition intervention for young adult university students: Development and evaluation protocol using the precede-proceed model. JMIR Res. Protoc. 2019, 8, e11992. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. Consort 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013. [Google Scholar]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall, Inc.: Englewood Cliffs, NJ, USA, 1986; pp. 617–630. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Kypri, K.; Hallett, J.; Howat, P.; McManus, A.; Maycock, B.; Bowe, S.; Horton, N.J. Randomized controlled trial of proactive web-based alcohol screening and brief intervention for university students. Arch. Intern. Med. 2009, 169, 1508–1514. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Boggess, M.M.; Watson, J.F.; Guest, M.; Duncanson, K.; Pezdirc, K.; Rollo, M.; Hutchesson, M.J.; Burrows, T.L. Reproducibility and comparative validity of a food frequency questionnaire for australian adults. Clin. Nutr. 2014, 33, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Burrows, T.L.; Rollo, M.E.; Boggess, M.M.; Watson, J.F.; Guest, M.; Duncanson, K.; Pezdirc, K.; Hutchesson, M.J. The comparative validity and reproducibility of a diet quality index for adults: The australian recommended food score. Nutrients 2015, 7, 785–798. [Google Scholar] [CrossRef]
- Centre for Epidemiology and Evidence. NSW Population Health Survey 2014—Questionnaire; NSW Ministry of Health: North Sydney, Sydney, 2014. [Google Scholar]
- Neumark-Sztainer, D.R.; Wall, M.M.; Haines, J.I.; Story, M.T.; Sherwood, N.E.; van den Berg, P.A. Shared risk and protective factors for overweight and disordered eating in adolescents. Am. J. Prev. Med. 2007, 33, 359–369.e3. [Google Scholar] [CrossRef]
- Mick, E.; Faraone, S.V.; Spencer, T.; Zhang, H.F.; Biederman, J. Assessing the validity of the quality of life enjoyment and satisfaction questionnaire short form in adults with adhd. J. Atten. Disord. 2008, 11, 504–509. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Collaborating Center for Mental Health. Who (Five) Well-Being Index. Available online: https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_English.pdf (accessed on 21 August 2017).
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The who-5 well-being index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Shanyinde, M.; Pickering, R.M.; Weatherall, M. Questions asked and answered in pilot and feasibility randomized controlled trials. BMC Med. Res. Methodol. 2011, 11, 117. [Google Scholar] [CrossRef]
- Lam, E.; Partridge, S.R.; Allman-Farinelli, M. Strategies for successful recruitment of young adults to healthy lifestyle programmes for the prevention of weight gain: A systematic review. Obes. Rev. 2016, 17, 178–200. [Google Scholar] [CrossRef]
- Black, A.E. Critical evaluation of energy intake using the goldberg cut-off for energy intake: Basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1119–1130. [Google Scholar] [CrossRef]
- The University of Newcastle. Annual Report 2015; The University of Newcastle: Callaghan, Australia, 2016. [Google Scholar]
- Australian Government Department of Education and Training. 2016 First Half Year Higher Education Statistics; Australian Government Department of Education and Training: Canberra, Australia, 2017. [Google Scholar]
- Topolovec-Vranic, J.; Natarajan, K. The use of social media in recruitment for medical research studies: A scoping review. J. Med. Internet Res. 2016, 18, e286. [Google Scholar] [CrossRef] [PubMed]
- Moe, S.G.; Lytle, L.A.; Nanney, M.S.; Linde, J.A.; Laska, M.N. Recruiting and retaining young adults in a weight gain prevention trial: Lessons learned from the choices study. Clin. Trials 2016, 13, 205–213. [Google Scholar] [CrossRef]
- Short, C.E.; DeSmet, A.; Woods, C.; Williams, S.L.; Maher, C.; Middelweerd, A.; Müller, A.M.; Wark, P.A.; Vandelanotte, C.; Poppe, L.; et al. Measuring engagement in ehealth and mhealth behavior change interventions: Viewpoint of methodologies. J. Med. Internet Res. 2018, 20, e292. [Google Scholar] [CrossRef]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and promoting effective engagement with digital behavior change interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef]
- Williams, D.R.; Lewis, N.M. Effectiveness of nutrition counseling in young adult males. Nutr. Res. 2002, 22, 911–917. [Google Scholar] [CrossRef][Green Version]
- Kerr, D.A.; Harray, A.J.; Pollard, C.M.; Dhaliwal, S.S.; Delp, E.J.; Howat, P.A.; Pickering, M.R.; Ahmad, Z.; Meng, X.; Pratt, I.S.; et al. The connecting health and technology study: A 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 52. [Google Scholar] [CrossRef] [PubMed]

| Recruitment strategy | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
|---|---|---|---|---|---|---|
| University of Newcastle Social Media | ✓ | ✓ | ✓ | |||
| Posters on campus | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Digital signage on campus | ✓ | ✓ | ||||
| University of Newcastle Health Promotion Working Group | ✓ | ✓ | ||||
| EATS Steering committee | ✓ | ✓ | ||||
| University of Newcastle Teaching staff | ✓ |
| Characteristic | Total (n = 124) | Intervention (n = 62) | Control (n = 62) |
|---|---|---|---|
| Mean ± SD or %(n) | |||
| Age (years) (mean ± SD) | 22.4 ± 4.0 | 21.8 ± 3.2 | 23.0 ± 4.6 |
| Gender %(n) | |||
| Female | 72.6 (90) | 71.0 (44) | 74.2 (46) |
| Male | 27.4 (34) | 29.0 (18) | 25.8 (16) |
| Australian born %(n) | 83.1 (103) | 77.4 (48) | 88.7 (55) |
| Aboriginal or Torres Strait Islander %(n) | 3.2 (4) | 1.6 (1) | 4.8 (3) |
| IRSAD (mean ± SD) a | 6.0 ± 2.5 | 6.0 ± 2.4 | 6.0 ± 2.6 |
| Marital status %(n) | |||
| Never married | 85.5 (106) | 88.7 (55) | 82.3 (51) |
| Married | 8.9 (11) | 4.8 (3) | 12.9 (8) |
| Defacto | 4.8 (6) | 6.5 (4) | 3.2 (2) |
| Separated/divorced/widowed | 0.8 (1) | 0 (0) | 1.6 (1) |
| Living situation %(n) | |||
| Own home | 5.7 (7) | 4.8 (3) | 6.5 (4) |
| Parents home | 32.3 (40) | 33.9 (21) | 30.7 (19) |
| On-campus | 16.1 (20) | 19.4 (12) | 12.9 (8) |
| Renting | 41.9 (52) | 38.7 (24) | 45.2 (28) |
| Boarding/homestay | 2.4 (3) | 1.6 (1) | 3.2 (2) |
| Irregular | 1.6 (2) | 1.6 (1) | 1.6 (1) |
| Paid work (hours/week) (mean ± SD) | 8.4 ± 10.1 | 7.6 ± 10.0 | 9.3 ± 10.2 |
| Receiving financial support %(n) | 76.6 (95) | 72.6 (45) | 80.7 (50) |
| Student type %(n) | |||
| Undergraduate | 87.1 (108) | 90.3 (56) | 83.9 (52) |
| Postgraduate (course) | 0.8 (1) | 0 (0) | 1.6 (1) |
| Postgraduate (HDR) | 7.3 (9) | 4.8 (3) | 9.7 (6) |
| Enabling | 4.0 (5) | 3.2 (2) | 4.8 (3) |
| Non-award | 0.8 (1) | 1.6 (1) | 0 (0) |
| Domestic/International %(n) | |||
| Domestic | 90.3 (112) | 87.1 (54) | 93.6 (58) |
| International | 9.7 (12) | 12.9 (7) | 6.4 (4) |
| Number of years studying %(n) | |||
| 1st year | 32.3 (40) | 29.0 (18) | 35.5 (22) |
| 2nd year | 21.8 (27) | 25.8 (16) | 17.7 (11) |
| 3rd year | 18.6 (23) | 21.0 (13) | 16.1 (10) |
| 4th year | 16.9 (21) | 12.9 (8) | 21.0 (13) |
| 5th year or later | 10.5 (13) | 11.3 (7) | 9.7 (6) |
| Faculty of study %(n) | |||
| Business & law | 7.3 (9) | 8.1 (5) | 6.5 (4) |
| Education & arts | 21.0 (26) | 9.7 (6) | 32.3 (20) |
| Engineering/built environment | 7.3 (9) | 4.8 (3) | 9.7 (6) |
| Health & medicine | 46.8 (58) | 50.0 (31) | 43.6 (27) |
| Science | 15.3 (19) | 24.2 (15) | 6.5 (4) |
| English language/foundation studies | 2.4 (3) | 3.2 (2) | 1.6 (1) |
| Dietary intake | |||
| ARFS (/73) (mean ± SD) | 30.5 ± 9.8 | 32.2 ± 10.1 | 28.9 ± 9.3 |
| Fruit ARFS sub-scale (/12) (mean ± SD) | 4.9 ± 2.8 | 5.3 ± 2.9 | 4.4 ± 2.7 |
| Fruit (grams/day) | 232.2 ± 186.3 | 243.5 ± 219.6 | 220.9 ± 146.5 |
| Fruit (% energy/day) | 7.6 ± 6.0 | 7.6 ± 5.6 | 7.7 ± 6.4 |
| Vegetables ARFS sub-scale (/21) (mean ± SD) | 10.9 ± 4.7 | 11.4 ± 4.9 | 10.5 ± 4.4 |
| Vegetables (grams/day) | 265.9 ± 160.7 | 283.4 ± 163.2 | 248.5 ± 157.6 |
| Vegetables (% energy/day) | 8.0 ± 5.1 | 8.3 ± 5.0 | 7.6 ± 5.2 |
| Discretionary foods (% energy/day) | 36.6 ± 14.0 | 36.8 ± 13.4 | 36.3 ± 14.8 |
| Breakfast %(n) | |||
| Never | 4.0 (5) | 3.2 (2) | 4.8 (3) |
| 1–2 days/week | 10.5 (13) | 9.7 (6) | 11.3 (7) |
| 3–4 days/week | 18.6 (23) | 16.1 (10) | 21.0 (13) |
| 5 or more days/week | 66.9 (83) | 71.0 (44) | 62.9 (39) |
| Diet self-efficacy scores (mean ± SD) | |||
| Fruit | 3.2 ± 0.9 | 3.1 ± 1.0 | 3.3 ± 0.8 |
| Vegetables | 2.8 ± 0.9 | 2.8 ± 1.0 | 2.7 ± 0.9 |
| Takeaway foods | 3.1 ± 0.9 | 3.1 ± 1.0 | 3.0 ± 0.8 |
| EDNP snack foods | 2.6 ± 1.0 | 2.8 ± 1.0 | 2.5 ± 1.0 |
| Sugar sweetened drinks | 3.4 ± 0.9 | 3.4 ± 1.0 | 3.4 ± 0.8 |
| Alcohol | 3.4 ± 1.0 | 3.4 ± 1.0 | 3.4 ± 1.0 |
| Breakfast | 3.4 ± 1.0 | 3.3 ± 1.1 | 3.4 ± 0.9 |
| Alcohol intake %(n) | |||
| Exceeding single occasion risk | 32.3 (40) | 33.9 (21) | 30.7 (19) |
| Exceeding lifetime risk | 50.8 (63) | 51.6 (32) | 50.0 (31) |
| BMI (mean ± SD) | 24.6 ± 4.8 | 24.9 ± 5.3 | 24.2 ± 4.3 |
| Underweight %(n) | 3.2 (4) | 3.2 (2) | 3.2 (2) |
| Healthy weight %(n) | 57.3 (71) | 53.2 (33) | 61.3 (38) |
| Overweight %(n) | 26.6 (33) | 29.0 (18) | 24.2 (15) |
| Obese %(n) | 12.9 (16) | 14.5 (9) | 11.3 (7) |
| WHO-5 score (mean ± SD) b | 14.7 ± 4.3 | 15.2 ± 4.0 | 14.3 ± 4.6 |
| Q-LES-Q-SF score (mean ± SD) c | 51.3 ± 7.5 | 52.6 ± 7.1 | 50.0 ± 7.7 |
| Acceptability Measures | Website Overall | ||
| Useful information about healthy eating | 4.1 ± 0.7 | ||
| Relevant information about healthy eating | 4.2 ± 0.6 | ||
| New information about healthy eating | 3.5 ± 1.0 | ||
| Motivated me to eat more healthy foods | 3.8 ± 0.8 | ||
| Motivated me to eat less discretionary foods | 3.8 ± 0.7 | ||
| Was easy to use | 4.3 ± 0.7 | ||
| Was visually appealing | 4.3 ± 0.6 | ||
| Acceptability Measures | Quiz Component | Goal Setting Component | Creating Strategies Component |
| Was useful | 4.1 ± 0.6 | 3.9 ± 0.8 | 4.1 ± 0.7 |
| Was relevant | 4.2 ± 0.7 | 4.1 ± 0.7 | 4.1 ± 0.7 |
| Was easy to use | 4.4 ± 0.6 | 4.3 ± 0.8 | 4.3 ± 0.7 |
| Motivated me to eat more healthy foods | 4.1 ± 0.8 | 3.9 ± 0.8 | 3.9 ± 0.9 |
| Motivated me to eat less discretionary foods | 4.0 ± 0.7 | 4.0 ± 0.8 | 3.9 ± 0.8 |
| Made me more aware of what I was eating | 4.2 ± 0.8 | NA | NA |
| Provided me with useful examples for setting goals/creating strategies | NA | 4.2 ± 0.8 | 4.1 ± 0.8 |
| Outcome | Mean Change from Baseline to 3-Months (95%CI) | Mean Difference between Groups (95% CI) | Group by Time p-Value | Effect Size (Cohen’s d) | |||
|---|---|---|---|---|---|---|---|
| Intervention (n = 62) | p-Value | Control (n = 62) | p-Value | ||||
| Diet quality (ARFS) | 0.1 (−1.9, 2.1) | 0.927 | 1.1 (−0.8, 3.0) | 0.243 | −1.0 (−3.8, 1.7) | 0.468 | -0.10 |
| Fruit (ARFS sub-scale score) | 0.2 (−0.5, 0.8) | 0.620 | −0.1 (−0.7, 0.6) | 0.834 | 0.2 (−0.7, 1.1) | 0.613 | 0.08 |
| Fruit (grams/day) | 0.02 (−58.5, 58.5) | 0.999 | 9.5 (−19.8, 38.7) | 0.525 | −9.5 (−74.9, 55.9) | 0.776 | -0.05 |
| Fruit (grams/day) (adjusted model) a | 21.7 (−13.6, 56.9) | 0.228 | 7.6 (−24.6, 39.8) | 0.645 | 14.1 (−33.7, 61.9) | 0.563 | 0.09 |
| % energy from fruit | 0.4 (−1.1, 2.0) | 0.606 | 0.1 (−1.3, 1.6) | 0.870 | 0.3 (−1.8, 2.4) | 0.790 | 0.05 |
| Vegetable (ARFS sub-scale score) | 0.1 (−1.0, 1.2) | 0.870 | 0.7 (−0.3, 1.8) | 0.165 | −0.6 (−2.2, 0.9) | 0.410 | −0.14 |
| Vegetable (grams/day) | 18.8 (−19.1, 56.6) | 0.332 | −8.1 (−43.3, 27.0) | 0.650 | 26.9 (−24.7, 78.5) | 0.307 | 0.17 |
| % energy from vegetables | 0.3 (−0.8, 1.5) | 0.561 | 0.3 (−0.8, 1.3) | 0.612 | 0.1 (−1.5, 1.6) | 0.935 | 0.01 |
| % energy from discretionary foods | −3.6 (−6.4, −0.8) | 0.010 | 1.2 (−1.3, 3.8) | 0.349 | −4.8 (−8.6, −1.1) | 0.012 | −0.34 |
| QLESQ total score | 0.6 (−1.3, 2.5) | 0.561 | −0.04 (−1.9, 1.8) | 0.962 | 0.6 (−2.3, 3.2) | 0.652 | 0.08 |
| WHO-5 score | 0.3 (−0.8, 1.3) | 0.580 | −0.4 (−1.4, 0.6) | 0.422 | 0.7 (−0.7, 2.2) | 0.339 | 0.17 |
| Below categorical variables presented as odds ratio b | |||||||
| Breakfast (frequency consumed) | 1.7 (0.4, 6.8) | 0.475 | 7.4 (1.7, 32.1) | 0.008 | 0.2 (0.03, 1.7) | 0.153 | −0.35 |
| Alcohol (quantity consumed) | 1.5 (0.6, 3.8) | 0.383 | 2.5 (1.0, 6.3) | 0.044 | 0.6 (0.2, 2.1) | 0.424 | −0.42 |
| Fruit self-efficacy (confidence score) | 0.8 (0.3, 1.7) | 0.516 | 0.3 (0.1, 0.6) | 0.002 | 3.0 (0.9, 10.0) | 0.071 | 0.26 |
| Vegetables self-efficacy (confidence score) | 1.0 (0.4, 2.1) | 0.927 | 0.8 (0.4, 1.6) | 0.455 | 1.3 (0.4, 3.8) | 0.657 | 0.06 |
| Takeaway foods self-efficacy (confidence score) | 0.6 (0.3, 1.4) | 0.240 | 0.6 (0.3, 1.3) | 0.188 | 1.0 (0.3, 1.0) | 0.977 | 0.00 |
| EDNP snack foods self-efficacy (confidence score) | 0.7 (0.3, 1.6) | 0.393 | 1.3 (0.6, 2.8) | 0.462 | 0.5 (0.2, 1.6) | 0.261 | −0.15 |
| Sugar sweetened drinks self-efficacy (confidence score) c | 0.8 (0.3, 2.0) | 0.619 | 0.8 (0.3, 1.9) | 0.614 | 1.0 (0.3, 3.5) | 0.966 | −0.01 |
| Alcohol self-efficacy (confidence score) | 0.2 (0.05, 0.5) | 0.002 | 0.9 (0.3, 2.5) | 0.800 | 0.2 (0.04, 0.8) | 0.031 | −0.42 |
| Breakfast self-efficacy (confidence score) | 0.5 (0.2, 1.5) | 0.245 | 0.9 (0.4, 2.5) | 0.902 | 0.6 (0.1, 2.4) | 0.447 | −0.13 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Whatnall, M.C.; Patterson, A.J.; Chiu, S.; Oldmeadow, C.; Hutchesson, M.J. Feasibility and Preliminary Efficacy of the Eating Advice to Students (EATS) Brief Web-Based Nutrition Intervention for Young Adult University Students: A Pilot Randomized Controlled Trial. Nutrients 2019, 11, 905. https://doi.org/10.3390/nu11040905
Whatnall MC, Patterson AJ, Chiu S, Oldmeadow C, Hutchesson MJ. Feasibility and Preliminary Efficacy of the Eating Advice to Students (EATS) Brief Web-Based Nutrition Intervention for Young Adult University Students: A Pilot Randomized Controlled Trial. Nutrients. 2019; 11(4):905. https://doi.org/10.3390/nu11040905
Chicago/Turabian StyleWhatnall, Megan C, Amanda J Patterson, Simon Chiu, Christopher Oldmeadow, and Melinda J Hutchesson. 2019. "Feasibility and Preliminary Efficacy of the Eating Advice to Students (EATS) Brief Web-Based Nutrition Intervention for Young Adult University Students: A Pilot Randomized Controlled Trial" Nutrients 11, no. 4: 905. https://doi.org/10.3390/nu11040905
APA StyleWhatnall, M. C., Patterson, A. J., Chiu, S., Oldmeadow, C., & Hutchesson, M. J. (2019). Feasibility and Preliminary Efficacy of the Eating Advice to Students (EATS) Brief Web-Based Nutrition Intervention for Young Adult University Students: A Pilot Randomized Controlled Trial. Nutrients, 11(4), 905. https://doi.org/10.3390/nu11040905







