Abstract
Stroke is the second leading cause of death worldwide but also of disability. Stroke induces certain alterations of muscle metabolism associated with gross muscle atrophy and a decrease in muscle function, leading to sarcopenia. The vast majority of stroke cases occur in adults over 65 years of age, and the prevalence is expected to massively increase in the coming years in this population. Sarcopenia is associated with higher mortality and functional decline. Therefore, the identification of interventions that prevent muscle alterations after stroke is of great interest. The purpose of this review is to carry out a systematic literature review to identify evidence for nutritional and pharmacological interventions, which may prevent loss of muscle mass in the elderly after stroke. The search was performed on Medline in December 2018. Randomized controlled studies, observational studies and case reports conducted in the last 20 years on post-stroke patients aged 65 or older were included. In total, 684 studies were screened, and eight randomized control trials and two cohort studies were finally included and examined. This review reveals that interventions such as amino acid supplementation or anabolic steroid administration are efficient to prevent muscle mass. Little evidence is reported on nutritional aspects specifically in sarcopenia prevention after stroke. It pinpoints the need for future studies in this particular population.
1. Introduction
Stroke is the second leading cause of disability in the world. The number of stroke survivors with residual disabilities is constantly growing [1]. Two-thirds of hospitalized stroke cases are 65 years or more [2]. In the older patient population, the stroke outcomes are poorer with a higher mortality rate and higher functional decline [3]. Moreover, age is considered as a negative predictive factor of the rehabilitation outcome [4,5]. The factors influencing poor stroke outcome in older patients may include the higher number of comorbidities and poor nutritional status [6,7].
Sarcopenia classically refers to an age-related condition and typically incorporates the concept of loss of muscle mass and function [8]. It is also recognized as a type of malnutrition by the European Society of Clinical Nutrition and Metabolism (ESPEN) [9]. Sarcopenia is recognized as a geriatric syndrome, which is associated with higher mortality, higher functional decline, an increased rate of falls and a higher incidence of hospitalizations [10]. The most widely recognized etiologic factors include genetic, hormonal changes (insulin resistance), nutritional status, reduced physical activity, immobilization and inflammation [11,12].
The concept of stroke-related sarcopenia has emerged less than 10 years ago. This entity is supported by the existence of adaptive muscle changes after stroke and the high prevalence of malnutrition in stroke patients [13]. In stroke patients, malnutrition or dysphagia occur in up to 49% or 52.6%, respectively [14]. Stroke can directly induce neurogenic dysphagia through sensory or motor impairment in the swallowing process. An association between malnutrition and dysphagia has been reported in the post-acute stroke phase. However, the causality link between the two remains unclear [14]. After motor stroke, predominantly in the paretic limb but not only, the size of muscle fibers typically decreases [15]. The muscle fiber type switches from II to I (fast to slow) progressively [16,17]. Moreover, as the muscle mass decreases after stroke, the proportion of intramuscular fat increases in the paretic limb [18,19]. Stroke-related sarcopenia and its combination with poor nutritional status appear highly interlinked, especially, in the older stroke population in which it may affect the stroke outcome. Therefore, methods that prevent muscle loss and improve muscle function after stroke are of great interest. This systematic review aims at identifying nutritional and pharmacological interventions which may prevent loss of muscle mass in the elderly after stroke.
2. Materials and Methods
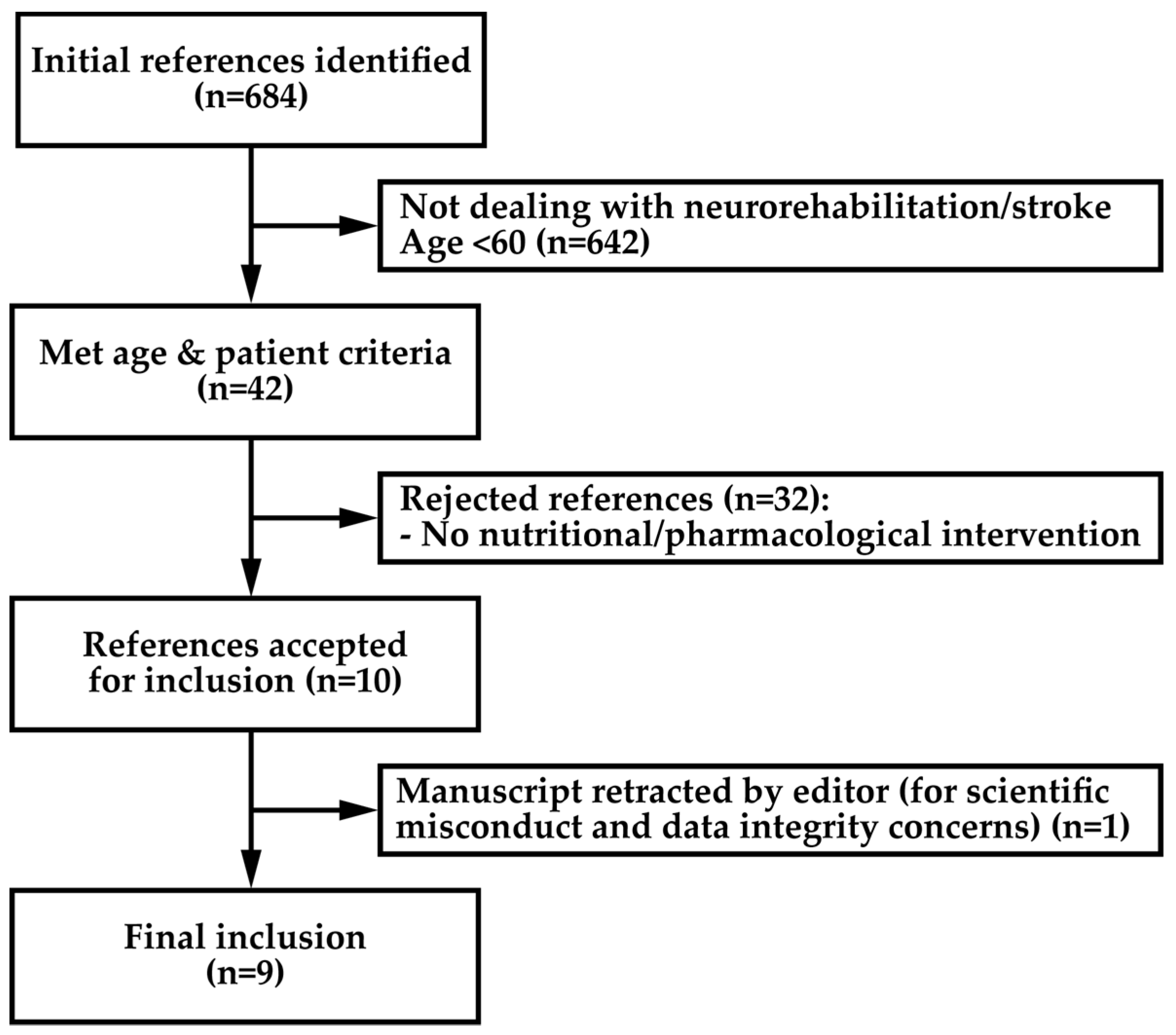
A systemic literature search was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines [20]. The information source was the MEDLINE electronic database (PubMed search platform, 1998 onwards). The initial search was performed in December 2018, with the last search performed on April 2 2019. The eligibility criteria were defined before performing the search and were as follows. Study design: Randomized controlled trials, controlled trials, prospective cohort studies, retrospective comparative cohort studies, case control studies and case-matched studies. Subject characteristics: Geriatric subject (mean age of groups > 60 years old), who were stroke survivors, who went through a neurorehabilitation program. Timing: Minimum 1 month follow up. Language: English. Based on the association of six blocks using Boolean operators, the search strategy was the following: [“Evidence” OR “Randomized controlled trial” OR “Cohort study” OR “Case-control study” OR “Qualitative research”] AND [“Neurological rehabilitation” OR "Stroke”] AND [“Elderly” OR “Aged” OR “Geriatric” OR “Frail”] AND [“Sarcopenia” OR “Muscle” OR “Muscle atrophy” OR “Muscle strength”] AND [“Occupational therapy” OR “Physical therapy” OR “Cognitive therapy” OR “Recreation therapy” OR “Nutrition” OR “Nutrition therapy” OR ”Intervention” OR “Hormonal replacement” OR “Drug”] OR [nutrition AND aged AND "stroke rehabilitation"]. One reviewer assessed the abstracts retrieved from the literature search. For abstracts fulfilling the major eligibility criteria (neurorehabilitation, stroke survivors), the full text was further screened to address the age of the subjects. Then, from all the papers that met the age criteria, those evaluating interventions based on nutritional or pharmacological strategies that affect muscle mass or muscle function were selected. The study selection process is depicted in the flow chart of Figure 1. A standardized scale for quality assessment was used to rate the selected studies. The checklist proposed by Downs and Black [21] was modified. Item number 27 was rated as 1 if a sample size calculation was reported by authors or 0 if not. Therefore, the maximum score was 28.
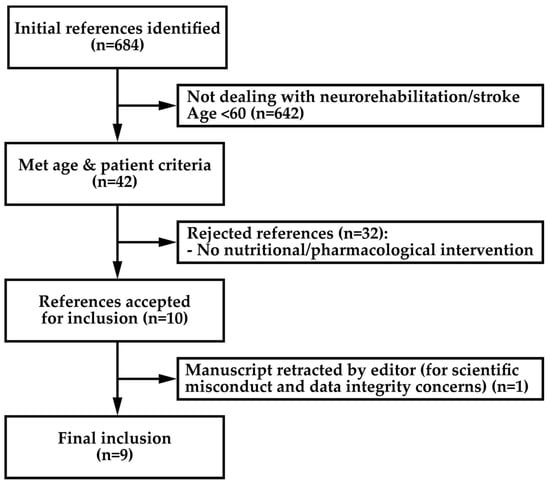
Figure 1.
Flow chart of studies selection process.
3. Results
Using the defined criteria, eight randomized and two cohort studies were selected for further review. However, one of the studies was excluded because it had been retracted by the editors because of concerns about data integrity and scientific misconduct [22,23]. From the nine remaining studies, see Table 1, four were multicenter studies [24,25,26,27]. Two interventions were commenced in the acute stroke phase [25,28] while others were including chronic stroke patients either during rehabilitation as inpatients [29,30] or outpatients [24]. Randomized control trials were categorized as unimodal when the methods included a single specific intervention in addition to a classical neurorehabilitation program or multimodal when the protocol combined different approaches. As in most studies in neurorehabilitation, they are not standardized; therefore, the functional outcomes measured in these studies could vary according to the intervention.

Table 1.
Selected studies.
3.1. Unimodal Interventions
Ha et al. showed that careful nutritional risk assessment (by estimating energy need and dietary intake) and an individual nutritional support (to cover estimated energy need) performed during the first seven days after admission for acute stroke could reduce the number of patients with a body weight loss ≥5% at three months (risk reduction of 15.7%, p = 0.055) [28]. While the intervention was associated with a stable protein intake across groups (0.8 vs. 0.7 g/kg, p = 0.065) the overall energy intake was 14.6% higher than that in the control group (1197 vs. 1045 kcal/day, p = 0.032). As a consequence, in the intervention group, there was a higher number of patients with improved handgrip strength (risk increase of 28.6%, p = 0.001). The mean handgrip strength was increased by 10.6% as compared to the control group (p = 0.002). Moreover, the patients reported a significant improvement in the quality of life in the mobility items of the EQ-5D questionnaire. All the outcomes of the study were measured three months after study entry. The only information provided on patient trajectory is the length of hospital stay, which was not significantly different between the groups. The authors did not provide data on the proportion of patients that went through a formal rehabilitation program after the acute stroke phase and their distribution in the study groups. Such data would have allowed for excluding potential bias in this study.
Rabadi et al. compared the effects of two commercially available nutritional supplements (standard: 127 kcal, 5 g proteins vs. intensive: 240 kcal, 11g proteins) on functional outcomes in a neurological rehabilitation setting in patients who presented with a minimal 2.5% weight loss within 14 days following stroke onset [31]. As compared to standard nutritional supplementation, upon discharge, patients in the intensive supplement arm of the study had a significantly greater motor functionality (motor items of the Functional Independence Measure (FIM scale) score of 24.25 vs. 16.7, p < 0.001). This beneficial effect on motor skills was also confirmed in the 2-minute and 6-minute walk tests in which patients from the intensive arm had a significantly greater improvement (2-minute: 101.6 vs. 43.98 feet, p < 0.001; 6-minute: 299.28 vs. 170.59 feet, p < 0.001). This effect allowed significantly more patients to return home (63 vs. 43%, p < 0.05). While the daily dietary intake was not monitored in this study, the intensive nutritional supplementation led to a non-significant higher weight gain (2.31 vs. 0.67 lbs, p = 0.37).
Some epidemiological data support the effect of omega-3 fatty acids intake in the prevention of ischemic stroke [33]. Moreover, the plasmatic antioxidative activity, as well as antioxidant vitamin levels, seem to be associated with stroke lesion size and neurological outcomes. Therefore, the Nutristroke trial evaluated the supplementation with omega-3 fatty acids (0.5 mg/day) and/or antioxidant (vitamin C 240 mg/day, vitamin E 290 mg/day, beta-carotene 19 mg/day and polyphenols 150 mg/day) during rehabilitation of post-stroke patients [32]. This study failed to demonstrate a significant functional improvement in treated patients. There was, nevertheless, a trend toward a lower mortality rate at the one-year-follow-up point in subgroups of patients treated with antioxidants with or without omega-3 fatty acids (p = 0.06). However, this finding needs to be interpreted with caution because of the low number of patients per group.
Edaravone is a powerful intravenous free radical scavenging compound that has demonstrated some neuroprotective effects in many preclinical models [34,35]. It was approved in Japan in the acute stroke phase. Despite the fact that no placebo group was included in their study, Naritomi et al. reported that 10–14 days treatment with edaravone, as opposed to three days treatment, could significantly reduce muscle atrophy of a paretic leg three months after a stroke (difference of 4.7% atrophy in paretic leg, p < 0.01) [25]. Interestingly, an effect on walking speed was also reported and may indicate a functional effect related to this observation on muscle trophicity (97.9 ± 67.3 cm/second vs. 53.6 ± 54.8 cm/second, p < 0.05).
Okamoto et al. tested the effect on thigh muscle of the intramuscular injections of the anabolic steroid, metenolone enanthate (ME) over a six-week timeframe in hemiplegic stroke patients [30]. Authors reported a significant increase in the cross-sectional area (CSA) of the thigh in both affected and unaffected legs. Despite a low number of treated patients, after six weeks, a significant increase in CSA was observed in the intervention group as compared to controls (13.4% vs. 3.3% increase in the paretic side and 14.5% vs. 5.2% in non-paretic side, p < 0.05). The authors did not provide any information on the sustainability of this effect after six weeks. Unexpectedly, this increase seemed to be greater in patients with a lower score for the motor items of the FIM scale. The authors suggest that this observation might be related to the fact that patients with lower motor FIM admitted to their rehabilitation ward are, typically, more inactive in the acute care hospital and, therefore, have more room for improvement.
3.2. Multimodal Interventions
Yoshimura et al. combined a 3 g of leucin 40% enriched amino acids supplement with low-intensity resistance training on top of a classical rehabilitation program [29]. Both groups received the resistance training, which consisted of a sit-to-stand exercise, from 10 up to 120 repetitions as the strength and durability improved during the protocol. The rehabilitation program was tailored to the patient’s need and included physical, occupational and speech therapy. After eight weeks, a greater improvement was observed in motor functionality (+9.2 points in FIM-motor score, 95%CI 1.5–15.8, p = 0.045) and handgrip strength (+3.8 kg, 95%CI 1.09–7.22, p = 0.002) in the intervention group.
In an attempt to prevent falls after discharge from hospital in stroke patients at risk, Batchelor et al. evaluated a multimodal intervention [24]. The intervention group received an individualized exercise program, an educative program, the implementation of multiple fall and injury prevention strategies and adequate vitamin D and calcium supplementation. However, this study could not demonstrate a clinical benefit as the fall rate and other outcomes did not significantly differ between groups.
3.3. Cohort Studies
In a retrospective multicenter cohort study including 192 geriatric stroke patients with prescribed rehabilitation, Kokura et al. evaluated the impact of energy intake during the first week after admission on the functional stroke outcomes [26]. The patient population was segregated into two subgroups according to their daily energy intake. The mean energy intake in the “energy sufficiency” group was 1206 ± 257 kcal/day, whereas it was 807 ± 394 kcal/day in the “energy shortage” group (p < 0.001). In a multivariate statistical analysis, energy sufficiency was significantly independently associated with total FIM gain (27 vs. 9; β = −0.166, 95%CI −7.295 to −0.175, p = 0.039) and motor-FIM gain (26 vs. 6; β = −0.205, 95%CI −7.191 to −1.027, p = 0.009). The absence of energy sufficiency was independently associated with the presence of complications (pneumonia, urinary tract infection or pressure ulcer) during hospitalization (OR 3.794, 95% CI 0.148–1.266, p = 0.017).
James et al. compared stroke patients who received tube feeding for nutritional support with those who did not in a post-stroke inpatient rehabilitation database [27]. This study highlights major variability in the use of tube feeding across centers. Nevertheless, in a regression analysis, tube feeding for 1–24% or ≥25% of the rehabilitation stay was significantly associated with increased total FIM (45.1 ± 12.6 and 33.9 ± 20.3, respectively, p = 0.002 and 0.005) and motor-FIM scores (36.6 ± 13.0 and 26.9 ± 16.8, respectively, p = 0.006 and p = 0.004) in severe strokes at discharge. Tube feeding for ≥25% of the rehabilitation stay also had a greater improvement in the severity of illness at discharge measured by the Comprehensive Severity Index (CSI) (16.8 ± 12.4; p = 0.001). Interestingly, the group exclusively fed by tube was associated with poor functional recovery, reflecting more post-stroke significant impairment. Despite the fact that energy intake was not reported in this study, it confirms the importance of early nutritional support in stroke rehabilitation.
4. Discussion
The literature reveals that interventions were heterogeneous and very limited in number in elderly post-stroke patients regarding muscle mass and muscle functions.
The two studies evaluating nutritional interventions demonstrated a significant improvement in muscle mass or handgrip strength [28,29]. Handgrip isometric strength is a validated quantitative marker of muscle function that is related to lower limb muscle function and calf cross-sectional muscle area [36]. It has been proposed as a valuable tool for the diagnosis of age-related sarcopenia [8]. The interventions tested by Yoshimura et al. resulted in an increased protein intake (>1.2 g/day), which is consistent with nutritional recommendations for the prevention of age-related sarcopenia [37]. Because stroke- and age-related sarcopenia share similar features [38], the generalization of these recommendations to older stroke patients seems to be confirmed by the identified studies. Interestingly, leucin-enriched amino acid supplementation may be less effective when not combined with exercise [39]. It means that such nutritional intervention is more effective for muscle mass when combined with resistance exercise as previously demonstrated in other settings [40]. The retrospective study by Kokura et al. confirmed that post-stroke elderly patients with insufficient energy intake have inferior motor and functional outcomes [26]. Nevertheless, the routine administration of nutritional supplements in a broad range of post-stroke patients did not provide beneficial effects on stroke outcomes [41]. However, the study by Rabadi et al., performed in selected undernourished patients (with evidence of weight loss after acute stroke), demonstrated that an increased dietary intake provided by nutritional supplements improved motor recovery and functionality [31]. Interestingly, in this study, more than 55% of the included patients had dysphagia, a condition that is strongly associated with malnutrition and higher morbidity and mortality rates [14,42]. James et al. demonstrated that nutritional support with tube feeding in rehabilitation is associated with greater motor improvement [27]. Taken together, these data support a systematic nutritional assessment and treatment of malnutrition in elderly stroke patients.
The consumption of higher relative levels of omega-3 fatty acids and antioxidants in the Mediterranean diet or through the consumption of fish is associated with a lower incidence of stroke and other cardiovascular events [43,44]. However, the Nutristroke trial failed to demonstrate significant effects of omega-3 fatty acids and antioxidant supplementation during stroke rehabilitation on patient functional status [32]. The mechanisms involved in the preventive effects of these dietary compounds on stroke occurrence may differ from those involved in stroke recovery and, therefore, this supplementation is not recommended.
Vitamin D supplementation has demonstrated a slight but significant effect on muscle strength particularly, in people aged 65 and over [45]. However, the study by Batchelor et al. failed to demonstrate the efficacy of a multimodal fall prevention intervention after stroke [24]. These findings are consistent with recent meta-analyses showing no effect of vitamin D supplementation on muscle health [46].
Anabolic steroids, especially testosterone, have been proposed to counteract age-related sarcopenia in older men. Testosterone replacement therapy is currently recommended to increase muscle mass and muscle function in older men only when serum testosterone levels are low [47]. Treatment for six weeks with the anabolic steroid metenolone enenthate during stroke rehabilitation increased the thigh muscle cross-sectional area [30]. However, this study could not demonstrate an effect on functional outcomes. Adverse events reported during the study included an increased fasting blood sugar level, hyperproteinemia or liver dysfunction. Anabolic steroids are classically associated with hepatic, metabolic or cardiovascular events [48,49]. Despite the fact that these observations were resolved at the end of the treatment, they confirm that the safety profile of such treatment should be carefully addressed in this specific patient population. As testosterone doesn’t seem to improve function in such a setting, and as their effect is reversible also for the beneficial effect on muscle mass [50], it doesn’t seem to be reasonable to propose this treatment after a stroke.
Edaravone was approved in 2001 in Japan for the treatment of ischemic stroke. The approval was based on the results of a phase-3 randomized, placebo-controlled, double-blinded multicenter study that demonstrated a significant improvement of stroke outcomes in treated patients (higher proportion of patient with lower disability measured by the modified Rankin scale) [51]. A recent retrospective observational study based on the Japanese stroke registry confirmed a potential benefit of this drug in the treatment of strokes [52]. Moreover, edaravone was recently approved in many countries for the treatment of amyotrophic lateral sclerosis (ALS) after a smaller decline of muscle strength in treated subjects was demonstrated [53]. The study by Naritomi et al. compared two treatment regimens with edaravone during the acute stroke phase [25]. Despite the fact that no placebo group was included in the study, longer treatment duration may be associated with a decreased muscle atrophy three months after stroke, suggesting a potential myoprotective effect of this drug. However, this effect needs to be confirmed in a larger patient population in randomized controlled trials. It would also be interesting to include, in future trials, some measures of muscle strength and function to confirm the benefit of this drug. There is currently not enough data to support its use.
The present review has some limitations. The literature search was performed only in one database (MEDLINE). Using different sources may have resulted in additional references and would have possibly allowed the inclusion of unpublished data. The strengths of this work rely on its systematic methodology and its originality as an effort to study a specific patient population in a specific setting.
5. Conclusions
The present systematic review demonstrates that little evidence supports interventions to prevent a decrease in muscle mass and function in elderly post-stroke patients. It tends to suggest that nutritional interventions recommended in the prevention of age-related sarcopenia, in association with a rehabilitation program, may be effective after stroke. However, this review highlights the need for future studies in this particular patient population as the number of older stroke patients with a residual disability is expected to continue growing in the years to come.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Feigin, V.L. Anthology of stroke epidemiology in the 20th and 21st centuries: Assessing the past, the present, and envisioning the future. Int. J. Stroke 2019. [Google Scholar] [CrossRef]
- Hall, M.J.; Levant, S.; DeFrances, C.J. Hospitalization for stroke in U.S. Hospitals, 1989–2009. Diabetes 2012, 18, 23. [Google Scholar]
- Saposnik, G.; Cote, R.; Phillips, S.; Gubitz, G.; Bayer, N.; Minuk, J.; Black, S.; Stroke Outcome Research Canada Working Group. Stroke outcome in those over 80: A multicenter cohort study across canada. Stroke 2008, 39, 2310–2317. [Google Scholar] [CrossRef] [PubMed]
- Sze, K.H.; Wong, E.; Or, K.H.; Lum, C.M.; Woo, J. Factors predicting stroke disability at discharge: A study of 793 chinese. Arch. Phys. Med. Rehabil. 2000, 81, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Macciocchi, S.N.; Diamond, P.T.; Alves, W.M.; Mertz, T. Ischemic stroke: Relation of age, lesion location, and initial neurologic deficit to functional outcome. Arch. Phys. Med. Rehabil. 1998, 79, 1255–1257. [Google Scholar] [CrossRef]
- Fischer, U.; Arnold, M.; Nedeltchev, K.; Schoenenberger, R.A.; Kappeler, L.; Hollinger, P.; Schroth, G.; Ballinari, P.; Mattle, H.P. Impact of comorbidity on ischemic stroke outcome. Acta Neurol. Scand. 2006, 113, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.P.; Wong, A.A.; Schluter, P.J.; Henderson, R.D.; O’Sullivan, J.D.; Read, S.J. Impact of premorbid undernutrition on outcome in stroke patients. Stroke 2004, 35, 1930–1934. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the european working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; Van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.; et al. Diagnostic criteria for malnutrition—An espen consensus statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.Y.; Bruyere, O. Health outcomes of sarcopenia: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef]
- Fielding, R.A.; Vellas, B.; Evans, W.J.; Bhasin, S.; Morley, J.E.; Newman, A.B.; Abellan van Kan, G.; Andrieu, S.; Bauer, J.; Breuille, D.; et al. Sarcopenia: An undiagnosed condition in older adults. Current consensus definition: Prevalence, etiology, and consequences. International working group on sarcopenia. J. Am. Med. Dir. Assoc. 2011, 12, 249–256. [Google Scholar] [CrossRef]
- Kortebein, P.; Ferrando, A.; Lombeida, J.; Wolfe, R.; Evans, W.J. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 2007, 297, 1772–1774. [Google Scholar] [CrossRef]
- Gariballa, S.E.; Parker, S.G.; Taub, N.; Castleden, M. Nutritional status of hospitalized acute stroke patients. Br. J. Nutr. 1998, 79, 481–487. [Google Scholar] [CrossRef]
- Foley, N.C.; Martin, R.E.; Salter, K.L.; Teasell, R.W. A review of the relationship between dysphagia and malnutrition following stroke. J. Rehabil. Med. 2009, 41, 707–713. [Google Scholar] [CrossRef]
- Hachisuka, K.; Umezu, Y.; Ogata, H. Disuse muscle atrophy of lower limbs in hemiplegic patients. Arch. Phys. Med. Rehabil. 1997, 78, 13–18. [Google Scholar] [CrossRef]
- De Deyne, P.G.; Hafer-Macko, C.E.; Ivey, F.M.; Ryan, A.S.; Macko, R.F. Muscle molecular phenotype after stroke is associated with gait speed. Muscle Nerve 2004, 30, 209–215. [Google Scholar] [CrossRef]
- Scelsi, R.; Lotta, S.; Lommi, G.; Poggi, P.; Marchetti, C. Hemiplegic atrophy. Morphological findings in the anterior tibial muscle of patients with cerebral vascular accidents. Acta Neuropathol. 1984, 62, 324–331. [Google Scholar] [CrossRef]
- Ryan, A.S.; Dobrovolny, C.L.; Smith, G.V.; Silver, K.H.; Macko, R.F. Hemiparetic muscle atrophy and increased intramuscular fat in stroke patients. Arch. Phys. Med. Rehabil. 2002, 83, 1703–1707. [Google Scholar] [CrossRef]
- Carin-Levy, G.; Greig, C.; Young, A.; Lewis, S.; Hannan, J.; Mead, G. Longitudinal changes in muscle strength and mass after acute stroke. Cerebrovasc. Dis. 2006, 21, 201–207. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Sato, Y.; Iwamoto, J.; Kanoko, T.; Satoh, K. Low-dose vitamin d prevents muscular atrophy and reduces falls and hip fractures in women after stroke: A randomized controlled trial. Cerebrovasc. Dis. 2005, 20, 187–192. [Google Scholar] [CrossRef]
- Retraction statement. Paper ‘low-dose vitamin d prevents muscular atrophy and reduces falls and hip fractures in women after stroke: A randomized controlled trial’ by sato et al. Cerebrovasc dis 2005;20:187-192. Cerebrovasc. Dis. 2017, 44, 240. [CrossRef] [PubMed]
- Batchelor, F.A.; Hill, K.D.; Mackintosh, S.F.; Said, C.M.; Whitehead, C.H. Effects of a multifactorial falls prevention program for people with stroke returning home after rehabilitation: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2012, 93, 1648–1655. [Google Scholar] [CrossRef] [PubMed]
- Naritomi, H.; Moriwaki, H.; Metoki, N.; Nishimura, H.; Higashi, Y.; Yamamoto, Y.; Yuasa, H.; Oe, H.; Tanaka, K.; Saito, K.; et al. Effects of edaravone on muscle atrophy and locomotor function in patients with ischemic stroke: A randomized controlled pilot study. Drugs R&D 2010, 10, 155–163. [Google Scholar] [CrossRef]
- Kokura, Y.; Wakabayashi, H.; Nishioka, S.; Maeda, K. Nutritional intake is associated with activities of daily living and complications in older inpatients with stroke. Geriatr. Gerontol. Int. 2018, 18, 1334–1339. [Google Scholar] [CrossRef]
- James, R.; Gines, D.; Menlove, A.; Horn, S.D.; Gassaway, J.; Smout, R.J. Nutrition support (tube feeding) as a rehabilitation intervention. Arch. Phys. Med. Rehabil. 2005, 86, S82–S92. [Google Scholar] [CrossRef]
- Ha, L.; Hauge, T.; Spenning, A.B.; Iversen, P.O. Individual, nutritional support prevents undernutrition, increases muscle strength and improves qol among elderly at nutritional risk hospitalized for acute stroke: A randomized, controlled trial. Clin. Nutr. 2010, 29, 567–573. [Google Scholar] [CrossRef]
- Yoshimura, Y.; Bise, T.; Shimazu, S.; Tanoue, M.; Tomioka, Y.; Araki, M.; Nishino, T.; Kuzuhara, A.; Takatsuki, F. Effects of a leucine-enriched amino acid supplement on muscle mass, muscle strength, and physical function in post-stroke patients with sarcopenia: A randomized controlled trial. Nutrition 2019, 58, 1–6. [Google Scholar] [CrossRef]
- Okamoto, S.; Sonoda, S.; Tanino, G.; Tomida, K.; Okazaki, H.; Kondo, I. Change in thigh muscle cross-sectional area through administration of an anabolic steroid during routine stroke rehabilitation in hemiplegic patients. Am. J. Phys. Med. Rehabil. 2011, 90, 106–111. [Google Scholar] [CrossRef]
- Rabadi, M.H.; Coar, P.L.; Lukin, M.; Lesser, M.; Blass, J.P. Intensive nutritional supplements can improve outcomes in stroke rehabilitation. Neurology 2008, 71, 1856–1861. [Google Scholar] [CrossRef]
- Garbagnati, F.; Cairella, G.; De Martino, A.; Multari, M.; Scognamiglio, U.; Venturiero, V.; Paolucci, S. Is antioxidant and n-3 supplementation able to improve functional status in poststroke patients? Results from the nutristroke trial. Cerebrovasc. Dis. 2009, 27, 375–383. [Google Scholar] [CrossRef]
- He, K.; Song, Y.; Daviglus, M.L.; Liu, K.; Van Horn, L.; Dyer, A.R.; Goldbourt, U.; Greenland, P. Fish consumption and incidence of stroke: A meta-analysis of cohort studies. Stroke 2004, 35, 1538–1542. [Google Scholar] [CrossRef]
- Watanabe, K.; Tanaka, M.; Yuki, S.; Hirai, M.; Yamamoto, Y. How is edaravone effective against acute ischemic stroke and amyotrophic lateral sclerosis? J. Clin. Biochem. Nutr. 2018, 62, 20–38. [Google Scholar] [CrossRef]
- Lapchak, P.A. A critical assessment of edaravone acute ischemic stroke efficacy trials: Is edaravone an effective neuroprotective therapy? Expert Opin. Pharmacother. 2010, 11, 1753–1763. [Google Scholar] [CrossRef]
- Lauretani, F.; Russo, C.R.; Bandinelli, S.; Bartali, B.; Cavazzini, C.; Di Iorio, A.; Corsi, A.M.; Rantanen, T.; Guralnik, J.M.; Ferrucci, L. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 2003, 95, 1851–1860. [Google Scholar] [CrossRef] [PubMed]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.; Krznaric, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the espen expert group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef]
- Sions, J.M.; Tyrell, C.M.; Knarr, B.A.; Jancosko, A.; Binder-Macleod, S.A. Age- and stroke-related skeletal muscle changes: A review for the geriatric clinician. J. Geriatr. Phys. Ther. 2012, 35, 155–161. [Google Scholar] [CrossRef]
- Verhoeven, S.; Vanschoonbeek, K.; Verdijk, L.B.; Koopman, R.; Wodzig, W.K.; Dendale, P.; van Loon, L.J. Long-term leucine supplementation does not increase muscle mass or strength in healthy elderly men. Am. J. Clin. Nutr. 2009, 89, 1468–1475. [Google Scholar] [CrossRef]
- Cermak, N.M.; Res, P.T.; de Groot, L.C.; Saris, W.H.; van Loon, L.J. Protein supplementation augments the adaptive response of skeletal muscle to resistance-type exercise training: A meta-analysis. Am. J. Clin. Nutr. 2012, 96, 1454–1464. [Google Scholar] [CrossRef] [PubMed]
- Dennis, M.S.; Lewis, S.C.; Warlow, C.; Collaboration, F.T. Routine oral nutritional supplementation for stroke patients in hospital (food): A multicentre randomised controlled trial. Lancet 2005, 365, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Paciaroni, M.; Mazzotta, G.; Corea, F.; Caso, V.; Venti, M.; Milia, P.; Silvestrelli, G.; Palmerini, F.; Parnetti, L.; Gallai, V. Dysphagia following stroke. Eur. Neurol. 2004, 51, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Tang, H.; Yang, X.; Luo, X.; Wang, X.; Shao, C.; He, J. Fish consumption and stroke risk: A meta-analysis of prospective cohort studies. J. Stroke Cerebrovasc. Dis. 2019, 28, 604–611. [Google Scholar] [CrossRef]
- Paterson, K.E.; Myint, P.K.; Jennings, A.; Bain, L.K.M.; Lentjes, M.A.H.; Khaw, K.T.; Welch, A.A. Mediterranean diet reduces risk of incident stroke in a population with varying cardiovascular disease risk profiles. Stroke 2018, 2415–2420. [Google Scholar] [CrossRef]
- Beaudart, C.; Buckinx, F.; Rabenda, V.; Gillain, S.; Cavalier, E.; Slomian, J.; Petermans, J.; Reginster, J.Y.; Bruyere, O. The effects of vitamin d on skeletal muscle strength, muscle mass, and muscle power: A systematic review and meta-analysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 2014, 99, 4336–4345. [Google Scholar] [CrossRef]
- Bolland, M.J.; Grey, A.; Avenell, A. Effects of vitamin d supplementation on musculoskeletal health: A systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 2018, 6, 847–858. [Google Scholar] [CrossRef]
- De Spiegeleer, A.; Beckwee, D.; Bautmans, I.; Petrovic, M.; the Sarcopenia Guidelines Development group of the Belgian Society of Gerontology and Geriatrics. Pharmacological interventions to improve muscle mass, muscle strength and physical performance in older people: An umbrella review of systematic reviews and meta-analyses. Drugs Aging 2018, 35, 719–734. [Google Scholar] [CrossRef] [PubMed]
- Basaria, S.; Coviello, A.D.; Travison, T.G.; Storer, T.W.; Farwell, W.R.; Jette, A.M.; Eder, R.; Tennstedt, S.; Ulloor, J.; Zhang, A.; et al. Adverse events associated with testosterone administration. N. Engl. J. Med. 2010, 363, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Socas, L.; Zumbado, M.; Perez-Luzardo, O.; Ramos, A.; Perez, C.; Hernandez, J.R.; Boada, L.D. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: A report of two cases and a review of the literature. Br. J. Sports Med. 2005, 39, e27. [Google Scholar] [CrossRef]
- O’Connell, M.D.; Roberts, S.A.; Srinivas-Shankar, U.; Tajar, A.; Connolly, M.J.; Adams, J.E.; Oldham, J.A.; Wu, F.C. Do the effects of testosterone on muscle strength, physical function, body composition, and quality of life persist six months after treatment in intermediate-frail and frail elderly men? J. Clin. Endocrinol. Metab. 2011, 96, 454–458. [Google Scholar] [CrossRef]
- Edaravone Acute Infarction Study Group. Effect of a novel free radical scavenger, edaravone (mci-186), on acute brain infarction. Randomized, placebo-controlled, double-blind study at multicenters. Cerebrovasc. Dis. 2003, 15, 222–229. [Google Scholar] [CrossRef]
- Enomoto, M.; Endo, A.; Yatsushige, H.; Fushimi, K.; Otomo, Y. Clinical effects of early edaravone use in acute ischemic stroke patients treated by endovascular reperfusion therapy. Stroke 2019, 50, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Writing, G.; Edaravone, A.L.S.S.G. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: A randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017, 16, 505–512. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).