Dietary Intake Patterns among Lactating and Non-Lactating Women of Reproductive Age in Rural Zambia
Abstract
1. Introduction
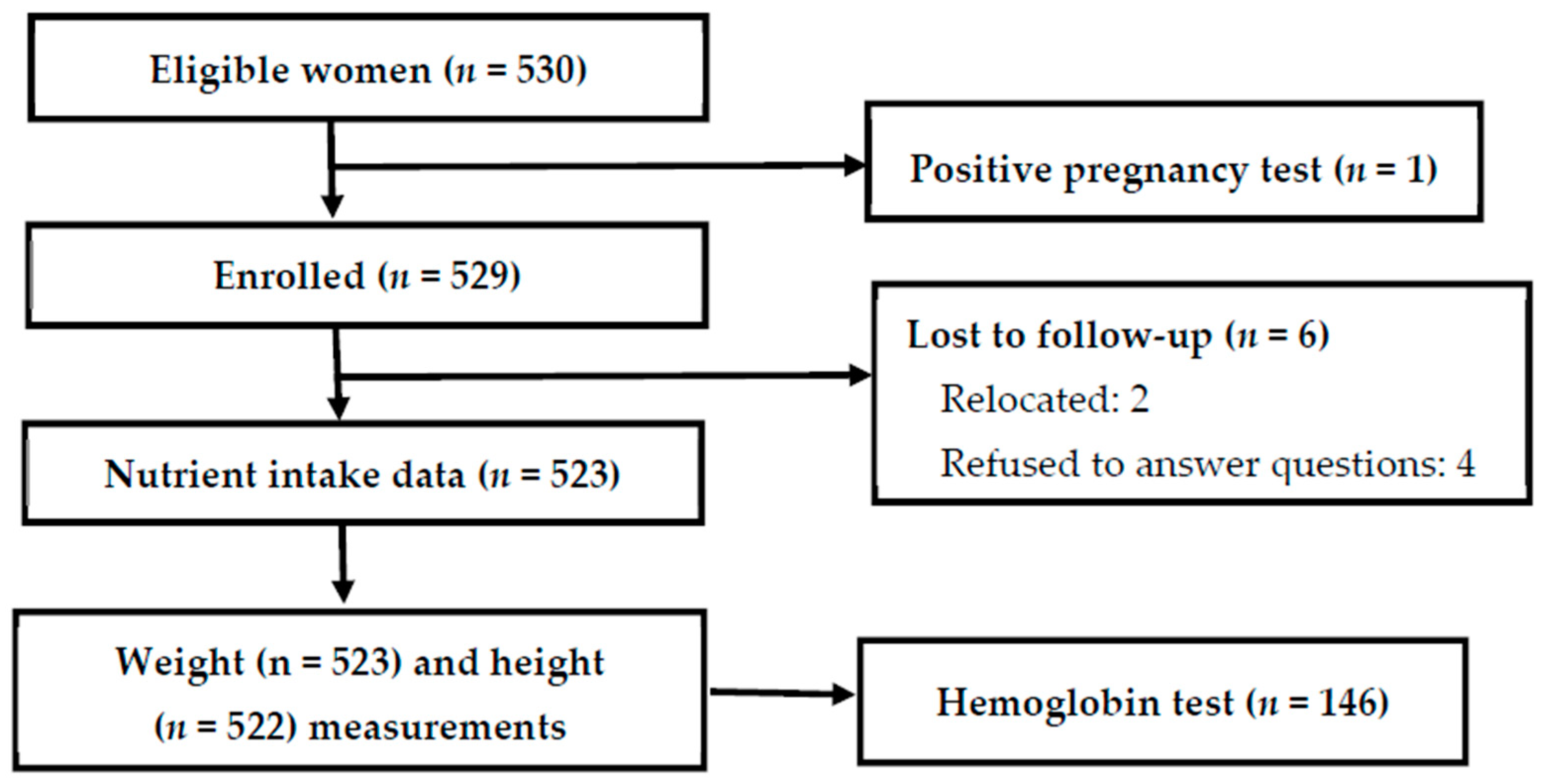
2. Materials and Methods
2.1. Ethics
2.2. Study Design and Target Population
2.3. Data Collection and Management
2.4. Dietary Intake Analysis
3. Results
3.1. Subject Characteristics
3.2. Minimum Dietary Diversity for Women of Reproductive Age (MDD-W)
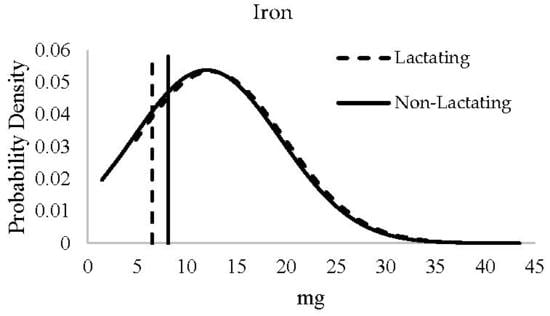
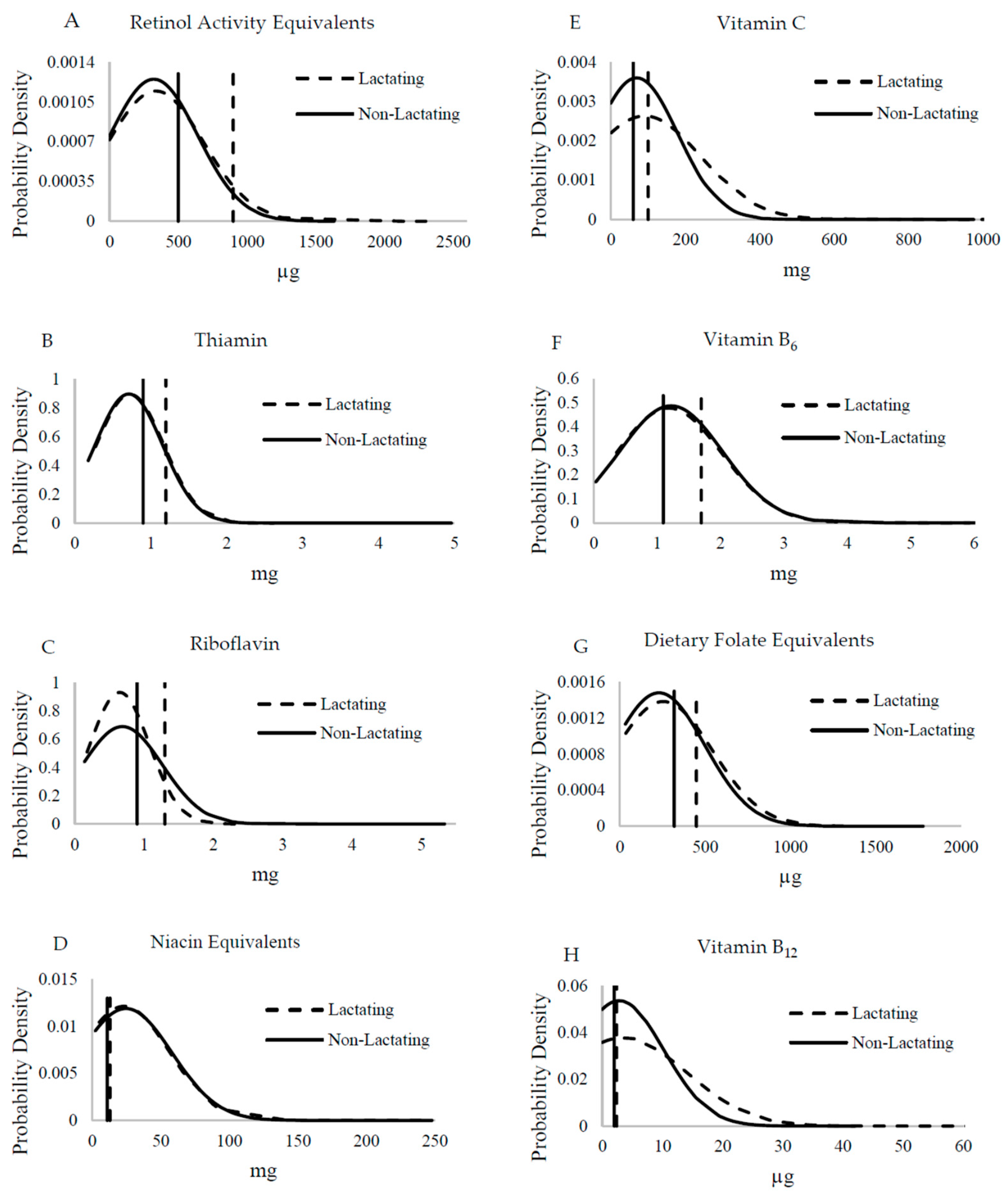
3.3. Dietary Intake
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Majid Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and Child Nutrition 1: Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 27 November 2018).
- Bhutta, Z.A.; Salam, R.A. Global nutrition epidemiology and trends. Ann. Nutr. Metab. 2012, 61 (Suppl. 1), 19–27. [Google Scholar] [CrossRef] [PubMed]
- Wessels, K.R.; Singh, G.M.; Brown, K.H. Estimating the global prevalence of inadequate zinc intake from national food balance sheets: Effects of methodological assumptions. PLoS ONE. 2012, 7, e50565. [Google Scholar] [CrossRef]
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; Bhutta, Z.A.; Ezzati, M.; Nutrition Impact Model Study Group. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef]
- United Nations General Assembly. Transforming Our World: The 2030 Agenda for Sustainable Development. A/RES/70/1. 2015. Available online: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E (accessed on 9 October 2018).
- Tanumihardjo, S.A.; Russell, R.M.; Stephensen, C.B.; Gannon, B.M.; Craft, N.E.; Haskell, M.J.; Lietz, G.; Schulze, K.; Raiten, D.J. Biomarkers of Nutrition for Development (BOND)-Vitamin A review. J. Nutr. 2016, 146, 1816S–1848S. [Google Scholar] [CrossRef] [PubMed]
- National Food and Nutrition Commission (NFNC); University of Zambia/MOST: The USAID Micronutrient Program/US Centers for Disease Control and Prevention. Report of the National Survey to Evaluate the Impact of Vitamin A Interventions in Zambia in July and November; NFNC: Lusaka, Zambia, 2003. [Google Scholar]
- Ministry of Health. National Malaria Indicator Survey; Ministry of Health: Lusaka, Zambia, 2015.
- Central Statistical Office; Ministry of Health; ICF International. Zambia Demographic and Health Survey 2013–2014; Central Statistical Office, Ministry of Health, ICF International: Rockville, ML, USA, 2014.
- Tanumihardjo, S.A.; Kaliwile, C.; Boy, E.; Dhansay, M.A.; van Stuijvenberg, M.E. Overlapping vitamin A interventions in the United States, Guatemala, Zambia, and South Africa: Case studies. Ann. N. Y. Acad. Sci. 2018. [Google Scholar] [CrossRef] [PubMed]
- Alaofė, H.; Kohler, L.; Taren, D.; Mofu, M.; Chileshe, J.; Kalungwana, N. Zambia Food Consumption and Micronutrient Status Survey Report; National Food and Nutrition Commission: Lusaka, Zambia, 2014. [Google Scholar]
- Grech, A.M.; Alders, R.; Darton-Hill, I.; Bagnol, B.; Hikeezi, D.; O’Leary, F.M. Nutrition knowledge, attitudes and dietary intake of women of reproductive age in women in Bundabunda Ward, Zambia. Clin. J. Nutr. Diet. 2018, 1, 1–12. [Google Scholar]
- de Bruyn, J.; Bagnol, B.; Darnton-Hill, I.; Maulaga, W.; Thomson, P.; Alders, R. Characterising infant and young child feeding practices and the consumption of poultry products in rural Tanzania: A mixed methods approach. Matern. Child Nutr. 2017, 14, e12550. [Google Scholar] [CrossRef]
- de Bruyn, J.; Wong, J.; Bagnol, B.; Pengelly, B.; Alders, R. Family poultry and food and nutrition security. CAB Rev. 2015, 10, 1–9. [Google Scholar] [CrossRef]
- Wong, J.T.; de Bruyn, J.; Bagnol, B.; Grieve, H.; Li, M.; Pym, R.; Alders, R.G. Small-scale poultry in resource-poor settings: A review. Glob. Food Secur. 2017, 15, 43–52. [Google Scholar] [CrossRef]
- Tanumihardjo, S.A.; Anderson, C.; Kaufer-Horwitz, M.; Bode, L.; Emenaker, N.J.; Haqq, A.M.; Satia, J.A.; Silver, H.J.; Stadler, D.D. Poverty, obesity and malnutrition: An international perspective recognizing the paradox. J. Am. Diet. Assoc. 2007, 107, 1966–1972. [Google Scholar] [CrossRef]
- Liu, R.H. Health-promoting components of fruits and vegetables in the diet. Adv. Nutr. 2013, 4, 384S–392S. [Google Scholar] [CrossRef]
- Turati, F.; Rossi, M.; Pelucchi, C.; Levi, F.; La Vecchia, C. Fruit and vegetables and cancer risk: A review of southern European studies. Br. J. Nutr. 2015, 113 (Suppl. 2), S102–S110. [Google Scholar] [CrossRef]
- George, S.M.; Ballard-Barbash, R.; Manson, J.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: Evidence to inform national dietary guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef]
- Grace, D.; Dominguez-Salas, P.; Alonso, S.; Lannerstad, M.; Muunda, E.; Ngwili, N.; Omar, A.; Khan, M.; Otobo, E. The Influence of Livestock-Derived Foods on Nutrition During the First 1000 Days of Life; ILRI Research Report 44; ILRI: Nairobi, Kenya, 2018. [Google Scholar]
- FAO and FHI 360. Minimum Dietary Diversity for Women: A Guide for Measurement; FAO: Rome, Italy, 2016. [Google Scholar]
- Andy, F. Discovering Statistics using IBM SPSS Statistics, 4th ed.; Sage Publications: Washington, DC, USA, 2013. [Google Scholar]
- Brandt, A.M. Racism and research: The case of the Tuskegee Syphilis Study. Hastings Cent. Rep. 1978, 8, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Alders, R.; Aongola, A.; Bagnol, B.; de Bruyn, J.; Kimboka, S.; Kock, R.; Li, M.; Maulaga, W.; McConchie, R.; Mor, S.; et al. Using a One Health approach to promote food and nutrition security in Tanzania and Zambia. Planet@Risk (Special Issue on One Health) 2014, 2, 187–190. [Google Scholar]
- Gibson, R.S.; Ferguson, E.L. An Interactive 24-Hour Recall for Assessing the Adequacy of Iron and Zinc Intakes in Developing Countries; HarvestPlus: Washington, DC, USA, 2008. [Google Scholar]
- World Health Organization (WHO). Training Course on Child Growth Assessment; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Eidelman, A.I.; Schanler, R.J. American Academy of Pediatrics Policy Statement: Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc: A Report of the Panel on Micronutrients; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Hotz, C.; Chileshe, J.; Siamusantu, W.; Palaniappan, U.; Kafwembe, E. Vitamin A intake and infection are associated with plasma retinol among pre-school children in rural Zambia. Public Health Nutr. 2012, 15, 1688–1696. [Google Scholar] [CrossRef] [PubMed]
- Hotz, C.; Lubowa, A.; Sison, C.; Moursi, M.; Loechl, C. A Food Composition Table for Central and Eastern Uganda; HarvestPlus and International Food Policy Research Institute and International Center for Tropical Agriculture: Cali, DC, USA, 2012. [Google Scholar]
- U.S. Department of Agriculture, Agricultural Research Service, USDA Nutrient Data Laboratory. USDA National Nutrient Database for Standard Reference, Release 21; USDA: Beltsville, MD, USA, 2008.
- National Food and Nutrition Commission. The 3rd Edition of Zambian Food Composition Tables; National Food and Nutrition Commission: Lusaka, Zambia, 2007. [Google Scholar]
- Kruger, M.; Hertzmark, E.; Mlingi, N.; Assey, V.; Ndossi, G.; Fawzi, W. Tanzania Food Composition Tables, 1st ed.; MUHAS-TFNC, HSPH: Dar es Salaam, Tanzania, 2008. [Google Scholar]
- Puwastien, P.; Burlingame, B.; Raroengwichit, M.; Sungpuag, P. ASEAN Food Composition Tables, 1st ed.; Institute of Nutrition, Mahidol University, and INFOODS Regional Database Centre: Bangkok, Thailand, 2000. [Google Scholar]
- Portugal, T.; Apilado, R.; Ardeña, J.; Avena, E.; Matibag, P.; Reyes, G.; Castillo, E.; Aguinaldo, A.; Abdon, I.; Lontoc, A. The Philippine Food Composition Tables; Food and Nutrition Research Institute, Department of Science and Technology: Manila, Philippines, 1997. [Google Scholar]
- Bunch, S.; Murphy, S.P. User’s Guide to the Operation of the World: Food Dietary Assessment System, Version 2.0; Office of Technology Licensing, University of California: Berkeley, CA, USA, 1997. [Google Scholar]
- West, C.E.; Pepping, F.; Temalilwa, C.R. The Composition of Foods Commonly Eaten in East Africa; Wageningen Agricultural University: Wageningen, The Netherlands, 1998. [Google Scholar]
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 19; USDA: Beltsville, MD, USA, 2006.
- Jahns, L.; Arab, L.; Carriquiry, A.; Popkin, B.M. The use of external within-person variance estimates to adjust nutrient intake distributions over time and across populations. Public Health Nutr. 2005, 8, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Black, A.E.; Morris, J.A.; Cole, T.J. Between- and within-subject variation in nutrient intake from infancy to old age: Estimating the number of days required to rank dietary intakes with desired precision. Am. J. Clin. Nutr. 1989, 50, 155–167. [Google Scholar] [CrossRef]
- Dodd, K.W.; Guenther, P.M.; Freedman, L.S.; Subar, A.F.; Kipnis, V.; Midthune, D.; Tooze, J.A.; Krebs-Smith, S.M. Statistical methods for estimating usual intake of nutrients and foods: A review of the theory. J. Am. Diet. Assoc. 2006, 106, 1640–1650. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes: Applications in Dietary Assessment; National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- World Health Organization. Pellagra and Its Prevention and Control in Major Emergencies; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Martin-Prevel, Y.; Becquey, E.; Arimond, M. Food group diversity indicators derived from qualitative list-based questionnaire misreported some foods compared to same indicators derived from quantitative 24-hour recall in urban Burkina Faso. J. Nutr. 2010, 140, 2086S–2093S. [Google Scholar] [CrossRef]
- Moursi, M.M.; Arimond, M.; Dewey, K.G.; Trèche, S.; Ruel, M.T.; Delpeuch, F. Dietary diversity is a good predictor of the micronutrient density of the diet of 6- to 23-month-old children in Madagascar. J. Nutr. 2008, 138, 2448–2453. [Google Scholar] [CrossRef] [PubMed]
- Mirmiran, P.; Azadbakht, L.; Esmaillzadeh, A.; Azizi, F. Dietary diversity score in adolescents—A good indicator of the nutritional adequacy of diets: Tehran lipid and glucose study. Asia Pac. J. Clin. Nutr. 2004, 13, 56–60. [Google Scholar]
- Hop le, T., Jr.; Son, T.H.; Ogle, B. Improvement of nutrition knowledge and practices among reproductive-aged women through participatory communication in two communes of Yenthe district in Bacgiang province, Vietnam. Malays. J. Nutr. 2007, 13, 121–129. [Google Scholar]
- U.S. Department of Agriculture Agricultural Research Service. USDA Food Composition Databases. Available online: https://ndb.nal.usda.gov/ndb/search/list (accessed on 10 October 2018).
- Bartter, J.; Diffey, H.; Yeung, Y.H.; O’Leary, F.; Häsler, B.; Maulaga, W.; Alders, R. Use of chicken eggshell to improve dietary calcium intake in rural sub-Saharan Africa. Matern. Child Nutr. 2018, 14, e12649. [Google Scholar] [CrossRef]
- World Health Organization and Food and Agriculture Organization of the United Nations. Vitamin and Mineral Requirements in Human Nutrition, 2nd ed.; WHO: Geneva, Switzerland, 2004; pp. 17–44. [Google Scholar]
- Tanumihardjo, S.A. Food-based approaches for ensuring adequate vitamin A nutrition. Compr. Rev. Food Sci. Food Saf. 2008, 7, 373–381. [Google Scholar]
- Tanumihardjo, S.A.; Gannon, B.M.; Kaliwile, C.; Chileshe, J. Hypercarotenodermia in Zambia: Which children turned orange during mango season? Eur. J. Clin. Nutr. 2015, 69, 1346–1349. [Google Scholar] [CrossRef]
- Nuss, E.T.; Arscott, S.A.; Bresnahan, K.; Pixley, K.V.; Rocheford, T.; Hotz, C.; Siamusantu, W.; Chileshe, J.; Tanumihardjo, S.A. Comparative intake of white- versus orange-colored maize by Zambian children in the context of promotion of biofortified maize. Food Nutr. Bull. 2012, 33, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Schmaelzle, S.; Kaliwile, C.; Arscott, S.A.; Gannon, BM.; Masi, C.; Tanumihardjo, S.A. Nutrient and nontraditional food intakes by Zambian children in a controlled feeding trial. Food Nutr. Bull. 2014, 35, 60–67. [Google Scholar] [CrossRef]
- Titcomb, T.J.; Schmaelzle, S.T.; Nuss, E.T.; Gregory, J.F., III; Tanumihardjo, S.A. Suboptimal vitamin B intakes of Zambian preschool children: Evaluation of 24-hour dietary recalls. Food Nutr. Bull. 2018, 39, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Food Fortification Initiative. Country Profile—Zambia. Available online: http://www.ffinetwork.org/country_profiles/country.php?record=251 (accessed on 27 November 2018).
- Allen, L.H. B vitamins in breast milk: Relative importance of maternal status and intake, and effects on infant status and function. Adv. Nutr. 2012, 3, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Black, M.M. Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr. Bull. 2008, 29 (Suppl. 2), S126–S131. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.; Haddad, L.; Grütz, S.S. Turning Rapid Growth into Meaningful Growth: Sustaining the Commitment to Nutrition in Zambia; Institute of Development Studies: Brighton, UK, 2014. [Google Scholar]
- Mondloch, S.; Gannon, B.M.; Davis, C.R.; Chileshe, J.; Kaliwile, C.; Masi, C.; Rios-Avila, L.; Gregory, J.F., III; Tanumihardjo, S.A. High provitamin A carotenoid serum concentrations, elevated retinyl esters, and saturated retinol-binding protein in Zambian preschool children are consistent with the presence of high liver vitamin A stores. Am. J. Clin. Nutr. 2015, 102, 497–504. [Google Scholar] [CrossRef] [PubMed]

| Frequency | Mean ± SD or % | 95% Confidence Interval | |
|---|---|---|---|
| Household characteristics (n = 523) | |||
| Level of education attained | |||
| Never attended school | 79 | 15.1 | 12.4, 18.4 |
| Primary | 305 | 58.3 | 54.1, 62.1 |
| Secondary | 127 | 24.3 | 20.9, 27.9 |
| Post-secondary | 12 | 2.3 | 1.1, 3.4 |
| Main occupational status | |||
| Crop production | 295 | 56.4 | 51.8, 60.8 |
| Other jobs | 228 | 43.6 | 39.4, 47.8 |
| Own a mosquito net | |||
| No | 166 | 31.7 | 27.7, 35.5 |
| Yes | 357 | 68.3 | 64.5, 72.3 |
| Characteristics of women | |||
| Age, years (n = 523; 27.6 ± 8.7 years) | |||
| 15–19 | 109 | 20.8 | 17.6, 24.5 |
| 20–29 | 217 | 41.5 | 37.1, 45.9 |
| 30–39 | 136 | 26.0 | 22.2, 30.0 |
| 40–49 | 61 | 11.7 | 9.2, 14.4 |
| Marital status (n = 523) | |||
| Married/living with a man | 368 | 70.4 | 66.5, 74.4 |
| Not in union | 155 | 29.6 | 25.6, 33.5 |
| Body mass index, kg/m2 (n = 522) 1 | 23.0 ± 3.2 | 22.8, 23.3 | |
| Underweight (<18.4) | 18 | 3.4 | 1.9, 5.0 |
| Normal (18.5–24.9) | 396 | 75.9 | 71.8, 79.9 |
| Overweight/obese (≥ 25) | 108 | 20.7 | 17.2, 24.5 |
| Iron status (n = 146) | |||
| Hemoglobin, g/L | |||
| ˂115 | 12 | 8.2 | 4.1, 13.0 |
| ≥115 | 134 | 91.8 | 87.0, 95.9 |
| Women dietary diversity score (mean ± SD; n = 523) | 3.75 ± 1.11 | ||
| Women dietary diversity score | |||
| ≥ 5 | 122 | 23.3 | 19.7, 27.0 |
| ˂ 5 | 401 | 76.7 | 73.0, 80.3 |
| Parameter | DDSs |
|---|---|
| Median | 3.75 |
| Mean | 4 |
| Minimum | 1 |
| Maximum | 8 |
| Percentiles | |
| 25 | 3 |
| 75 | 4 |
| Item consumed | % of women |
| Grains, white roots and tubers, and plantains | 99.4 |
| Pulses (beans, peas, and lentils) | 23.5 |
| Nuts and seeds | 11.3 |
| Dairy | 3.1 |
| Meat, poultry and fish | 36.7 |
| Eggs | 10.7 |
| Dark green leafy vegetables | 70.0 |
| Other vitamin A-rich fruits and vegetables | 17.2 |
| Other vegetables | 84.9 |
| Other fruits | 11.9 |
| Lactating | Non-Lactating | p3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 180 | n = 343 | ||||||||||
| Age Range 15–47 Years | Age Range 15–49 Years | ||||||||||
| Nutrient | EAR 1 | Mean | SD | Median | Percent Inadequate 2 | EAR 1 | Mean | SD | Median | Percent Inadequate 2 | |
| Energy (kcal) | - | 1845 | 880 | 1697 | - | - | 1903 | 753 | 1919 | - | - |
| Vitamin A 4 (μg) | 900 | 337 | 348 | 239 | 99.9 | 500 | 322 | 319 | 210 | 91.0 | <0.001 |
| Thiamin (mg) | 1.2 | 0.73 | 0.45 | 0.57 | 97.1 | 0.9 | 0.71 | 0.44 | 0.58 | 77.6 | <0.003 |
| Riboflavin (mg) | 1.3 | 0.65 | 0.43 | 0.54 | 98.7 | 0.9 | 0.69 | 0.58 | 0.55 | 73.8 | <0.003 |
| Niacin 5 (mg) | 13 | 23.2 | 32.9 | 13.5 | 28.0 | 11 | 24.6 | 33.5 | 14.8 | 22.3 | NS 6 |
| Vitamin B6 (mg) | 1.7 | 1.19 | 0.83 | 0.94 | 90.1 | 1.1 | 1.22 | 0.82 | 1.00 | 36.4 | <0.001 |
| Folate 7 (μg) | 450 | 257 | 288 | 116 | 91.0 | 320 | 231 | 269 | 121 | 74.6 | NS |
| Vitamin B12 (μg) | 2.4 | 3.51 | 10.5 | 0.00 | 37.7 | 2.0 | 2.82 | 7.43 | 0.00 | 37.1 | NS |
| Vitamin C (mg) | 100 | 90.9 | 152 | 51.0 | 54.9 | 60 | 69.2 | 111 | 43.8 | 51.3 | <0.001 |
| Calcium (mg) | 800 | 231 | 172 | 178 | 99.9 | 800 | 190 | 145 | 146 | 99.9 | NS |
| Iron (mg) 8 | 6.5 | 12.4 | 7.48 | 9.52 | 36.9 | 8.1 | 12.0 | 7.42 | 7.39 | 37.1 | NS |
| Zinc (mg) | 10.4 | 7.88 | 4.55 | 6.38 | 86.1 | 6.8 | 7.82 | 3.94 | 6.93 | 33.6 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaliwile, C.; Michelo, C.; Titcomb, T.J.; Moursi, M.; Donahue Angel, M.; Reinberg, C.; Bwembya, P.; Alders, R.; Tanumihardjo, S.A. Dietary Intake Patterns among Lactating and Non-Lactating Women of Reproductive Age in Rural Zambia. Nutrients 2019, 11, 288. https://doi.org/10.3390/nu11020288
Kaliwile C, Michelo C, Titcomb TJ, Moursi M, Donahue Angel M, Reinberg C, Bwembya P, Alders R, Tanumihardjo SA. Dietary Intake Patterns among Lactating and Non-Lactating Women of Reproductive Age in Rural Zambia. Nutrients. 2019; 11(2):288. https://doi.org/10.3390/nu11020288
Chicago/Turabian StyleKaliwile, Chisela, Charles Michelo, Tyler J. Titcomb, Mourad Moursi, Moira Donahue Angel, Chelsea Reinberg, Pheobe Bwembya, Robyn Alders, and Sherry A. Tanumihardjo. 2019. "Dietary Intake Patterns among Lactating and Non-Lactating Women of Reproductive Age in Rural Zambia" Nutrients 11, no. 2: 288. https://doi.org/10.3390/nu11020288
APA StyleKaliwile, C., Michelo, C., Titcomb, T. J., Moursi, M., Donahue Angel, M., Reinberg, C., Bwembya, P., Alders, R., & Tanumihardjo, S. A. (2019). Dietary Intake Patterns among Lactating and Non-Lactating Women of Reproductive Age in Rural Zambia. Nutrients, 11(2), 288. https://doi.org/10.3390/nu11020288