The Effects of Iodine Supplementation in Pregnancy on Iodine Status, Thyroglobulin Levels and Thyroid Function Parameters: Results from a Randomized Controlled Clinical Trial in a Mild-to-Moderate Iodine Deficiency Area
Abstract
1. Introduction
2. Materials and Methods
2.1. Laboratory Assays
2.2. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO: UNICEF, International Council for Control of Iodine Deficienc Disorders. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination. A guide for Programme Managers; World Health Organization: Geneva, Switzerland, 2007; Available online: http://www.who.int/nutrition/publications/micronutrients/iodine_deficiency/9789241595827/en/ (accessed on 21 August 2017).
- Alexander, E.K.; Pearce, E.N.; Brent, G.A.; Brown, R.S.; Chen, H.; Dosiou, C.; Grobman, W.A.; Laurberg, P.; Lazarus, J.H.; Mandel, S.J.; et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017, 27, 315–389. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. The Adverse Effects of Mild-to-Moderate Iodine Deficiency during Pregnancy and Childhood: A Review. Thyroid 2007, 17, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.N.; Okosieme, O.E.; Dayan, C.M.; Lazarus, J.H. Therapy of Endocrine Disease: Impact of iodine supplementation in mild-to-moderate iodine deficiency: Systematic review and meta-analysis. Eur. J. Endocrinol. 2014, 170, R1–R15. [Google Scholar] [CrossRef] [PubMed]
- Berghout, A.; Wiersinga, W. Thyroid size and thyroid function during pregnancy: An analysis. Eur. J. Endocrinol. 1998, 138, 536–542. [Google Scholar] [CrossRef]
- Moreno-Reyes, R.; Glinoer, D.; Van Oyen, H.; Vandevijvere, S. High Prevalence of Thyroid Disorders in Pregnant Women in a Mildly Iodine-deficient Country: A Population-Based Study. J. Clin. Endocrinol. Metab. 2013, 98, 3694–3701. [Google Scholar] [CrossRef]
- Bath, S.C.; Steer, C.D.; Golding, J.; Emmett, P.; Rayman, M.P. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 2013, 382, 331–337. [Google Scholar] [CrossRef]
- Levie, D.; Korevaar, T.I.M.; Bath, S.C.; Murcia, M.; Dineva, M.; Llop, S.; Espada, M.; van Herwaarden, A.E.; de Rijke, Y.B.; Ibarluzea, J.M.; et al. Association of maternal iodine status with child IQ: A meta-analysis of individual-participant data. J. Clin. Endocrinol. Metab. 2019, 104, 5957–5967. [Google Scholar] [CrossRef]
- Rohner, F.; Zimmermann, M.; Jooste, P.; Pandav, C.; Caldwell, K.; Raghavan, R.; Raiten, D.J. Biomarkers of nutrition for development—Iodine review. J. Nutr. 2014, 144, 1322S–1342S. [Google Scholar] [CrossRef]
- Tuccilli, C.; Baldini, E.; Truppa, E.; D’Auria, B.; De Quattro, D.; Cacciola, G.; Aceti, T.; Cirillo, G.; Faiola, A.; Indigeno, P.; et al. Iodine deficiency in pregnancy: Still a health issue for the women of Cassino city, Italy. Nutrition 2018, 50, 60–65. [Google Scholar] [CrossRef]
- Vesterinen, H.M.; Johnson, P.I.; Atchley, D.S.; Sutton, P.; Lam, J.; Zlatnik, M.G.; Sen, S.; Woodruff, T.J. Fetal growth and maternal glomerular filtration rate: A systematic review. J. Matern. Neonatal Med. 2015, 28, 2176–2181. [Google Scholar] [CrossRef]
- Li, C.; Peng, S.; Zhang, X.; Xie, X.; Wang, D.; Mao, J.; Teng, X.; Shan, Z.; Teng, W. The Urine Iodine to Creatinine as an Optimal Index of Iodine During Pregnancy in an Iodine Adequate Area in China. J. Clin. Endocrinol. Metab. 2016, 101, 1290–1298. [Google Scholar] [CrossRef] [PubMed]
- Bílek, R.; Čeřovská, J.; Zamrazil, V. The relationship between iodine intake and serum thyroglobulin in the general population. Physiol. Res. 2015, 64, 345–353. [Google Scholar] [PubMed]
- Bath, S.C.; Pop, V.J.M.; Furmidge-Owen, V.L.; Broeren, M.A.C.; Rayman, M.P. Thyroglobulin as a Functional Biomarker of Iodine Status in a Cohort Study of Pregnant Women in the United Kingdom. Thyroid 2017, 27, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Koukkou, E.; Ilias, I.; Mamalis, I.; Adonakis, G.G.; Markou, K.B. Serum Thyroglobulin Concentration Is a Weak Marker of Iodine Status in a Pregnant Population with Iodine Deficiency. Eur. Thyroid J. 2016, 5, 120–124. [Google Scholar] [CrossRef]
- Katko, M.; Gazso, A.A.; Hircsu, I.; Bhattoa, H.P.; Molnar, Z.; Kovacs, B.; Andrasi, D.; Aranyosi, J.; Makai, R.; Veress, L.; et al. Thyroglobulin level at week 16 of pregnancy is superior to urinary iodine concentration in revealing preconceptual and first trimester iodine supply. Matern. Child. Nutr. 2018, 14, e12470. [Google Scholar] [CrossRef]
- Andersson, M.; de Benoist, B.; Delange, F.; Zupan, J.; Zupan, J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: Conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007, 10, 1606–1611. [Google Scholar]
- Olivieri, A.; De Angelis, S.; Rotondi, D.; Pastorelli, A.; Stacchini, P.; Da Cas, R.; Regionali, C. Attività di monitoraggio del programma nazionale per la prevenzione dei disordini da carenza iodica: La situazione italiana a 14 anni dall’approvazione della Legge 55/2005. L’Endocrinologo 2019, 20, 245–248. [Google Scholar] [CrossRef]
- Watutantrige-Fernando, S.; Barollo, S.; Bertazza, L.; Cavedon, E.; Censi, S.; Manso, J.; Vianello, F.; Mian, C.; Andrighettoni, S.; Chiamenti, A.M.; et al. Efficacy of educational intervention to improve awareness of the importance of iodine, use of iodized salt, and dietary iodine intake in northeastern Italian schoolchildren. Nutrition 2018, 53, 134–139. [Google Scholar] [CrossRef]
- Mian, C.; Vitaliano, P.; Pozza, D.; Barollo, S.; Pitton, M.; Callegari, G.; Di Gianantonio, E.; Casaro, A.; acamulli, D.N.; Busnardo, B.; et al. Iodine status in pregnancy: Role of dietary habits and geographical origin. Clin. Endocrinol. 2009, 70, 776–780. [Google Scholar] [CrossRef]
- Marangoni, F.; Cetin, I.; Verduci, E.; Canzone, G.; Giovannini, M.; Scollo, P.; Corsello, G.; Poli, A. Maternal Diet and Nutrient Requirements in Pregnancy and Breastfeeding. An Italian Consensus Document. Nutrients 2016, 8, 629. [Google Scholar] [CrossRef]
- Stagnaro-Green, A.; Sullivan, S.; Pearce, E.N. Iodine supplementation during pregnancy and lactation. JAMA 2012, 308, 2463–2464. [Google Scholar] [CrossRef]
- Du, Y.; Gao, Y.H.; Feng, Z.Y.; Meng, F.G.; Fan, L.J.; Sun, D.J. Serum Thyroglobulin—A Sensitive Biomarker of Iodine Nutrition Status and Affected by Thyroid Abnormalities and Disease in Adult Populations. Biomed. Environ. Sci. 2017, 30, 508–516. [Google Scholar]
- Watutantrige Fernando, S.; Barollo, S.; Nacamulli, D.; Pozza, D.; Giachetti, M.; Frigato, F.; Redaelli, M.; Zagotto, G.; Girelli, M.E.; Mantero, F.; et al. Iodine status in schoolchildren living in northeast italy: The importance of iodized-salt use and milk consumption. Eur. J. Clin. Nutr. 2013, 67, 366–370. [Google Scholar] [CrossRef]
- Glinoer, D.; De Nayer, P.; Delange, F.; Lemone, M.; Toppet, V.; Spehl, M.; Grün, J.P.; Kinthaert, J.; Lejeune, B. A randomized trial for the treatment of mild iodine deficiency during pregnancy: Maternal and neonatal effects. J. Clin. Endocrinol. Metab. 1995, 80, 258–269. [Google Scholar]
- Watutantrige Fernando, S.; Cavedon, E.; Nacamulli, D.; Pozza, D.; Ermolao, A.; Zaccaria, M.; Girelli, M.E.; Bertazza, L.; Barollo, S.; Mian, C. Iodine status from childhood to adulthood in females living in North-East Italy: Iodine deficiency is still an issue. Eur. J. Nutr. 2016, 55, 335–340. [Google Scholar] [CrossRef]
- Gowachirapant, S.; Jaiswal, N.; Melse-Boonstra, A.; Galetti, V.; Stinca, S.; Mackenzie, I.; Thomas, S.; Thomas, T.; Winichagoon, P.; Srinivasan, K.; et al. Effect of iodine supplementation in pregnant women on child neurodevelopment: A randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017, 5, 853–863. [Google Scholar] [CrossRef]
- Abel, M.H.; Korevaar, T.I.M.; Erlund, I.; Villanger, G.D.; Caspersen, I.H.; Arohonka, P.; Alexander, J.; Meltzer, H.M.; Brantsæter, A.L. Iodine Intake is Associated with Thyroid Function in Mild to Moderately Iodine Deficient Pregnant Women. Thyroid 2018, 28, 1359–1371. [Google Scholar] [CrossRef]
- Lopes van Balen, V.A.; van Gansewinkel, T.A.G.; de Haas, S.; Spaan, J.J.; Ghossein-Doha, C.; van Kuijk, S.M.J.; van Drongelen, J.; Cornelis, T.; Spaanderman, M.E.A. Kidney function during pregnancy: A systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2018, 54, 279–307. [Google Scholar] [CrossRef]
- Ma, Z.F.; Skeaff, S.A. Thyroglobulin as a Biomarker of Iodine Deficiency: A Review. Thyroid 2014, 24, 1195–1209. [Google Scholar] [CrossRef]
- Raverot, V.; Bournaud, C.; Sassolas, G.; Orgiazzi, J.; Claustrat, F.; Gaucherand, P.; Mellier, G.; Claustrat, B.; Borson-Chazot, F.; Zimmermann, M. Pregnant French women living in the Lyon area are iodine deficient and have elevated serum thyroglobulin concentrations. Thyroid 2012, 22, 522–528. [Google Scholar] [CrossRef]
- Mitchell, M.L.; Klein, R.Z.; Sargent, J.D.; Meter, R.A.; Haddow, J.E.; Waisbren, S.E.; Faix, J.D. Iodine sufficiency and measurements of thyroid function in maternal hypothyroidism. Clin. Endocrinol. 2003, 58, 612–616. [Google Scholar] [CrossRef]
- Stinca, S.; Andersson, M.; Weibel, S.; Aeberli-Herter, I.; Fingerhut, R.; Gowachirapant, S.; Hess, S.Y.; Jaiswal, N.; Jukić, T.; Kusic, Z.; et al. Dried blood spot thyroglobulin as a biomarker of iodine status in pregnant women. J. Clin. Endocrinol. Metab. 2016, 102, 23–32. [Google Scholar] [CrossRef]
- Eltom, A.; Elnagar, B.; Elbagir, M.; Gebre-Medhin, M. Thyroglobulin in serum as an indicator of iodine status during pregnancy. Scand. J. Clin. Lab. Investig. 2000, 60, 1–7. [Google Scholar]
- Moleti, M.; Trimarchi, F.; Vermiglio, F. Thyroid Physiology in Pregnancy. Endocr. Pract. 2014, 20, 589–596. [Google Scholar] [CrossRef]
- Glinoer, D. What Happens to the Normal Thyroid During Pregnancy? Thyroid 1999, 9, 631–635. [Google Scholar] [CrossRef]
- Moleti, M.; Di Bella, B.; Giorgianni, G.; Mancuso, A.; De Vivo, A.; Alibrandi, A.; Trimarchi, F.; Vermiglio, F. Maternal thyroid function in different conditions of iodine nutrition in pregnant women exposed to mild-moderate iodine deficiency: An observational study. Clin. Endocrinol. 2011, 74, 762–768. [Google Scholar] [CrossRef]
- Hynes, K.L.; Otahal, P.; Hay, I.; Burgess, J.R. Mild Iodine Deficiency During Pregnancy Is Associated with Reduced Educational Outcomes in the Offspring: 9-Year Follow-up of the Gestational Iodine Cohort. J. Clin. Endocrinol. Metab. 2013, 98, 1954–1962. [Google Scholar] [CrossRef]

| Parameter | Iodine Group | Placebo Group | p | ||
|---|---|---|---|---|---|
| N = 52 | Median (IC95%) | N = 38 | Median (IC95%) | ||
| Age (years) | 31 (IC95% 29–33) | 33 (IC95% 31–33.5) | 0.23 | ||
| Italian nationality | 36/64 (56%) | 28/64 (44%) | 0.65 | ||
| BMI (kg/m2) | 22.0 | 20.5 (IC95% 19.0–22.0) | 0.24 | ||
| (IC95% 20.59–22.41) | |||||
| Gestational weeks at recruitment | 11 (IC95% 10–12) | 10 (IC95% 9.5–11) | 0.05 | ||
| Education | |||||
| • Bachelor | 30/52 (58%) | 20/36 (56%) | 0.84 | ||
| • Degree | 22/52 (42%) | 16/36 (44%) | “ | ||
| Cow’s milk consumption | |||||
| • no/rarely | 30/52 (58%) | 22/38 (58%) | 0.98 | ||
| • daily | 22/52 (42%) | 16/38 (42%) | “ | ||
| Iodized salt | 50/52 (96%) | 35/38 (92%) | 0.18 | ||
| UI/Creat (µg/g) | 55.37 | 50.98 | |||
| (IC95% 35.39–71.07) | (IC95% 40.39–75.04) | 0.66 | |||
| 10823.80 | 9701.12 | ||||
| Thyroid volume (mm3) | (IC95% 9813.94–12588.26) | (IC95% 9208.78–12181.21) | 0.25 | ||
| TSH (mIU/L) | 1.06 | 1.16 | 0.37 | ||
| (IC95% 0.78–1.56) | (IC95% 0.99–1.55) | ||||
| Tg (ng/mL) | 8.3 | 8.36 | 0.78 | ||
| (IC95% 6.62–10.45) | (IC95% 6.82–11.01) | ||||
| fT4 (pmol/L) | 14.91 | 15.08 | 0.27 | ||
| (IC95%14.21–15.25) | (IC95%14.34–15.89) | ||||
| fT3 (pmol/L) | 4.71 | 4.75 | 0.63 | ||
| (IC95% 4.60–4.98) | (IC95% 4.59–5.09) | ||||
| Baseline | Second Trimester | Third Trimester | Post-Partum | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Median (IC95%) | N | Median (IC95%) | p | N | Median (IC95%) | p | N | Median (IC95%) | p | ||
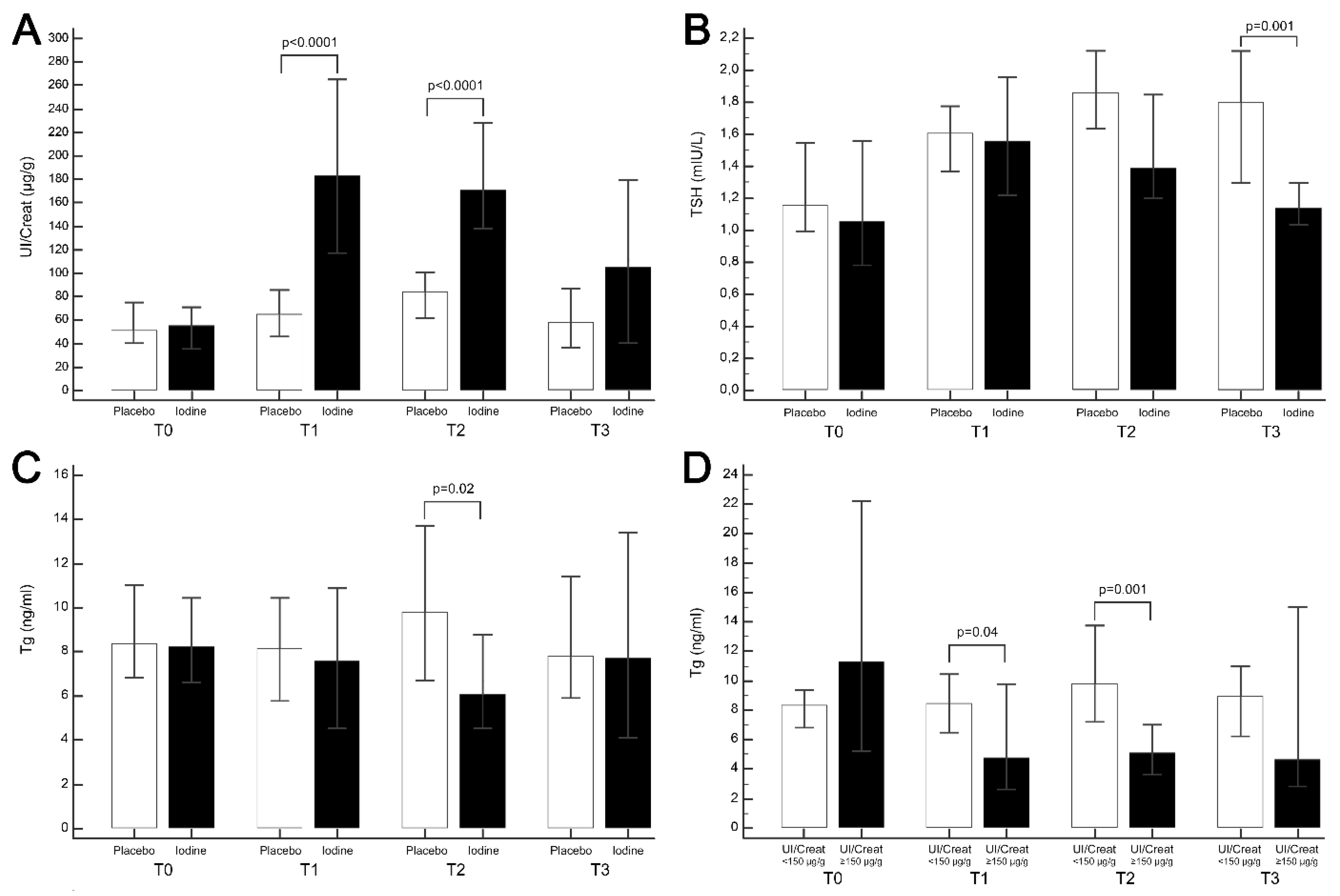
| UI/Creat (ug/g) | Placebo | 38 | 55.37 (35.39–71.07) | 38 | 65.55 (46.62–86.00) | <0.0001 | 33 | 84.19 (61.86 to 100.61) | <0.0001 | 31 | 58.24 (36.63 to 87.09) | 0.10 |
| Iodine | 52 | 50.98 (40.39–75.04) | 50 | 183.23 (117.39–264.92) | 40 | 171.16 (138.05–228.46) | 38 | 104.88 (40.70 to 179.66) | ||||
| Tg (ng/mL) | Placebo | 38 | 8.3 (6.62–10.45) | 38 | 8.16 (5.79–10.44) | 0.56 | 33 | 9.8 (6.69–14.29) | 0.02 | 31 | 7.79 (5.90–11.41) | 0.67 |
| Iodine | 52 | 8.36 (6.82–11.01) | 50 | 7.56 (4.53–10.89) | 40 | 6.07 (4.52–8.78) | 38 | 7.67 (4.11 to 13.42) | ||||
| Thyroid volume (mm3) | Placebo | 38 | 9701.12 (9208.78–12181.21) | 38 | 10592.40 (8563.97–12142.60) | 0.11 | 33 | 10743.20 (10136.81–11943.49) | 0.31 | 31 | 0.20 | |
| Iodine | 52 | 10823.80 (9208.78–12181.21) | 50 | 11222.64 (9801.17–14952.06) | 40 | 11550.24 (10232.54–13237.92) | 38 | 11662.04 (9168.88–13099.32) | ||||
| TSH (mIU/L) | Placebo | 38 | 1.16 (0.99–1.55) | 38 | 1.60 (1.37–1.78) | 1.00 | 33 | 1.86 (1.64–2.12) | 0.09 | 31 | 1.80 (1.29–2.12) | 0.001 |
| Iodine | 52 | 1,05 (0.78–1156) | 50 | 1.55 (1.22–1.96) | 40 | 1.39 (1.19–1.85) | 38 | 1.14 (1.04–1.29) | ||||
| FT4 (pmol/L) | Placebo | 38 | 15.08 (14.34–15.98) | 38 | 12.94 (12.41–13.57) | 0.52 | 33 | 13.04 (12.60–13.34) | 0.83 | 31 | 13.45 (12.91–13.99) | 0.48 |
| Iodine | 52 | 14.91 (14.20–15.25) | 50 | 12.82 (11.99–13.62) | 40 | 12.66 (12.08–13.52) | 38 | 13.08 (12.42–14.06) | ||||
| FT3 (pmol/L) | Placebo | 38 | 4.75 (4.59–5.09) | 38 | 4.06 (3.96–4.27) | 0.18 | 33 | 4.33 (4.04–4.47) | 0.86 | 31 | 4,4450 (4.19–4.69) | 0.12 |
| Iodine | 52 | 4.71 (4.60–4.99) | 50 | 4.33 (4.17–4.47) | 40 | 4.21 (4.07–4.43) | 38 | 4.27 (4.08–4.39) | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Censi, S.; Watutantrige-Fernando, S.; Groccia, G.; Manso, J.; Plebani, M.; Faggian, D.; Mion, M.M.; Venturini, R.; Andrisani, A.; Casaro, A.; et al. The Effects of Iodine Supplementation in Pregnancy on Iodine Status, Thyroglobulin Levels and Thyroid Function Parameters: Results from a Randomized Controlled Clinical Trial in a Mild-to-Moderate Iodine Deficiency Area. Nutrients 2019, 11, 2639. https://doi.org/10.3390/nu11112639
Censi S, Watutantrige-Fernando S, Groccia G, Manso J, Plebani M, Faggian D, Mion MM, Venturini R, Andrisani A, Casaro A, et al. The Effects of Iodine Supplementation in Pregnancy on Iodine Status, Thyroglobulin Levels and Thyroid Function Parameters: Results from a Randomized Controlled Clinical Trial in a Mild-to-Moderate Iodine Deficiency Area. Nutrients. 2019; 11(11):2639. https://doi.org/10.3390/nu11112639
Chicago/Turabian StyleCensi, Simona, Sara Watutantrige-Fernando, Giulia Groccia, Jacopo Manso, Mario Plebani, Diego Faggian, Monica Maria Mion, Roberta Venturini, Alessandra Andrisani, Anna Casaro, and et al. 2019. "The Effects of Iodine Supplementation in Pregnancy on Iodine Status, Thyroglobulin Levels and Thyroid Function Parameters: Results from a Randomized Controlled Clinical Trial in a Mild-to-Moderate Iodine Deficiency Area" Nutrients 11, no. 11: 2639. https://doi.org/10.3390/nu11112639
APA StyleCensi, S., Watutantrige-Fernando, S., Groccia, G., Manso, J., Plebani, M., Faggian, D., Mion, M. M., Venturini, R., Andrisani, A., Casaro, A., Vita, P., Avogadro, A., Camilot, M., Scaroni, C., Bertazza, L., Barollo, S., & Mian, C. (2019). The Effects of Iodine Supplementation in Pregnancy on Iodine Status, Thyroglobulin Levels and Thyroid Function Parameters: Results from a Randomized Controlled Clinical Trial in a Mild-to-Moderate Iodine Deficiency Area. Nutrients, 11(11), 2639. https://doi.org/10.3390/nu11112639









