Efficacy and Mechanism of Polymerized Anthocyanin from Grape-Skin Extract on High-Fat-Diet-Induced Nonalcoholic Fatty Liver Disease
Abstract
:1. Introduction
2. Materials and Methods
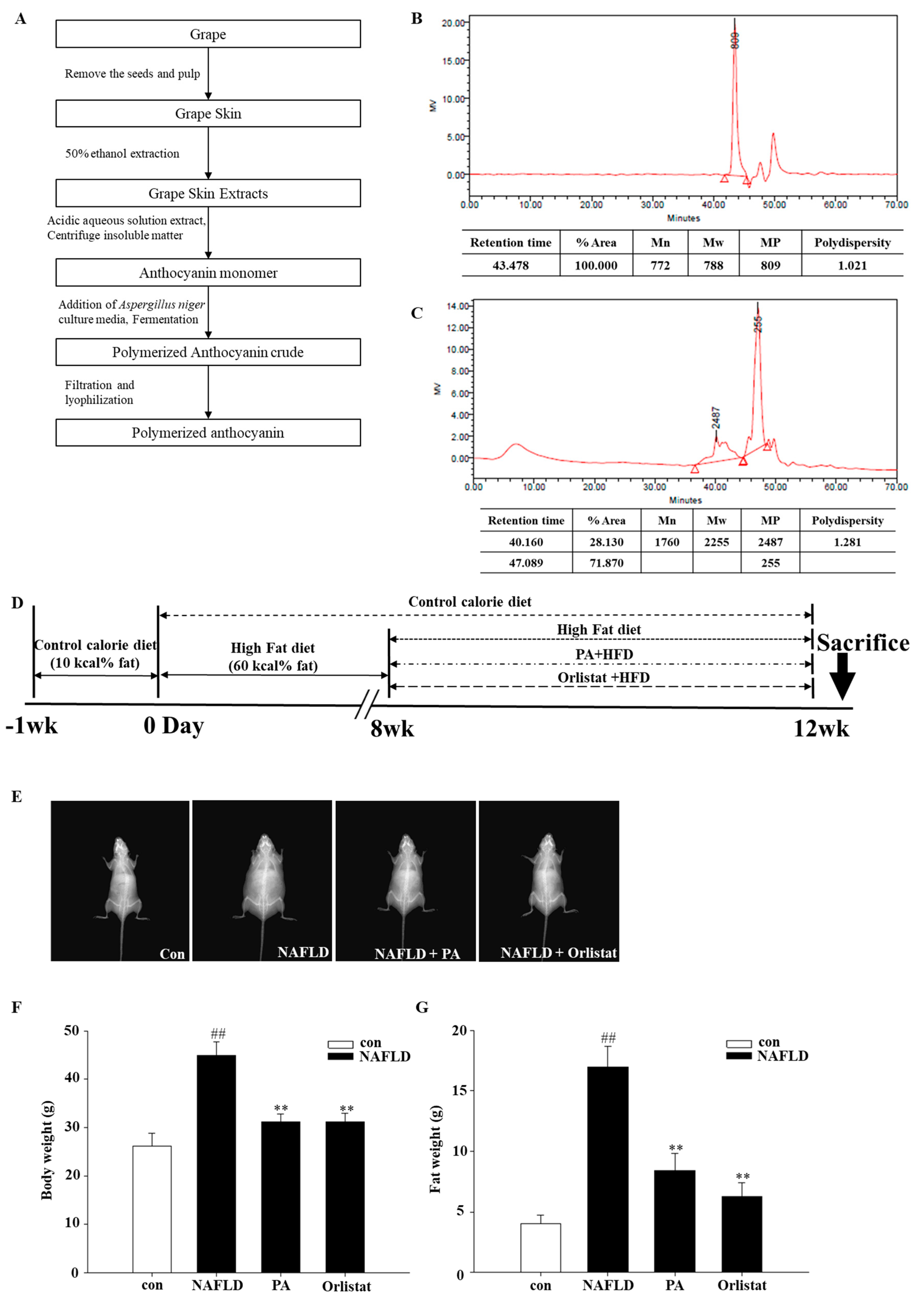
2.1. Polymerized-Anthocyanin Synthesis
2.2. Experiment Animals, Diet, and Treatments
2.3. Body-Fat-Composition Analysis
2.4. Histological Analysis
2.5. Blood Biochemical Analysis
2.6. mRNA Expression
2.7. Protein Expression
2.8. Statistical Analysis
3. Results
3.1. Effects of PA on Body Composition in High-Fat-Diet-Induced NAFLD Mice
3.2. Effects of PA on Lipid Accumulation and Hepatocellular Damage
3.3. Effects of PA on Blood Biochemical Parameters
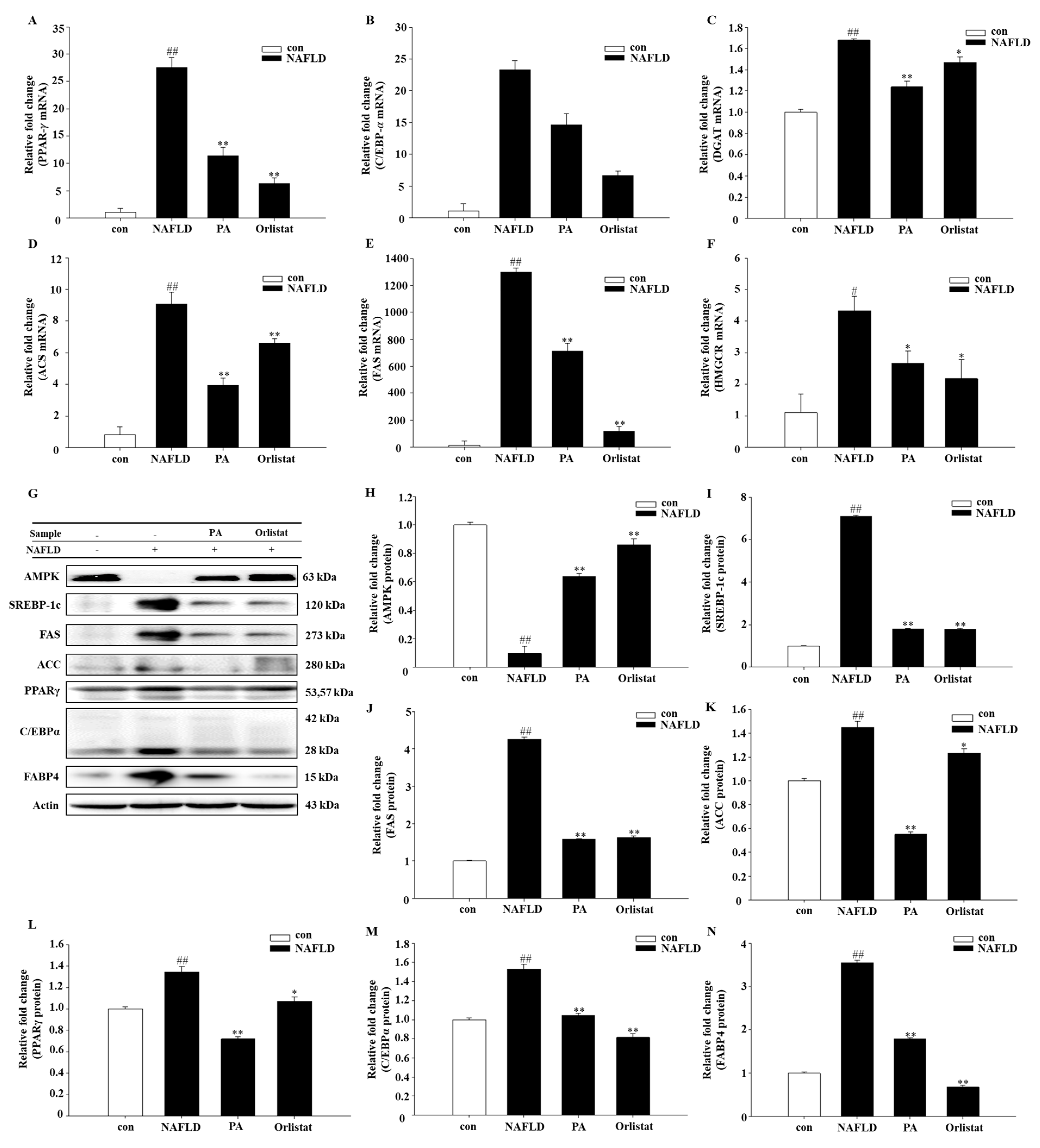
3.4. Effects of PA on Lipogenic Molecule Signal Pathway
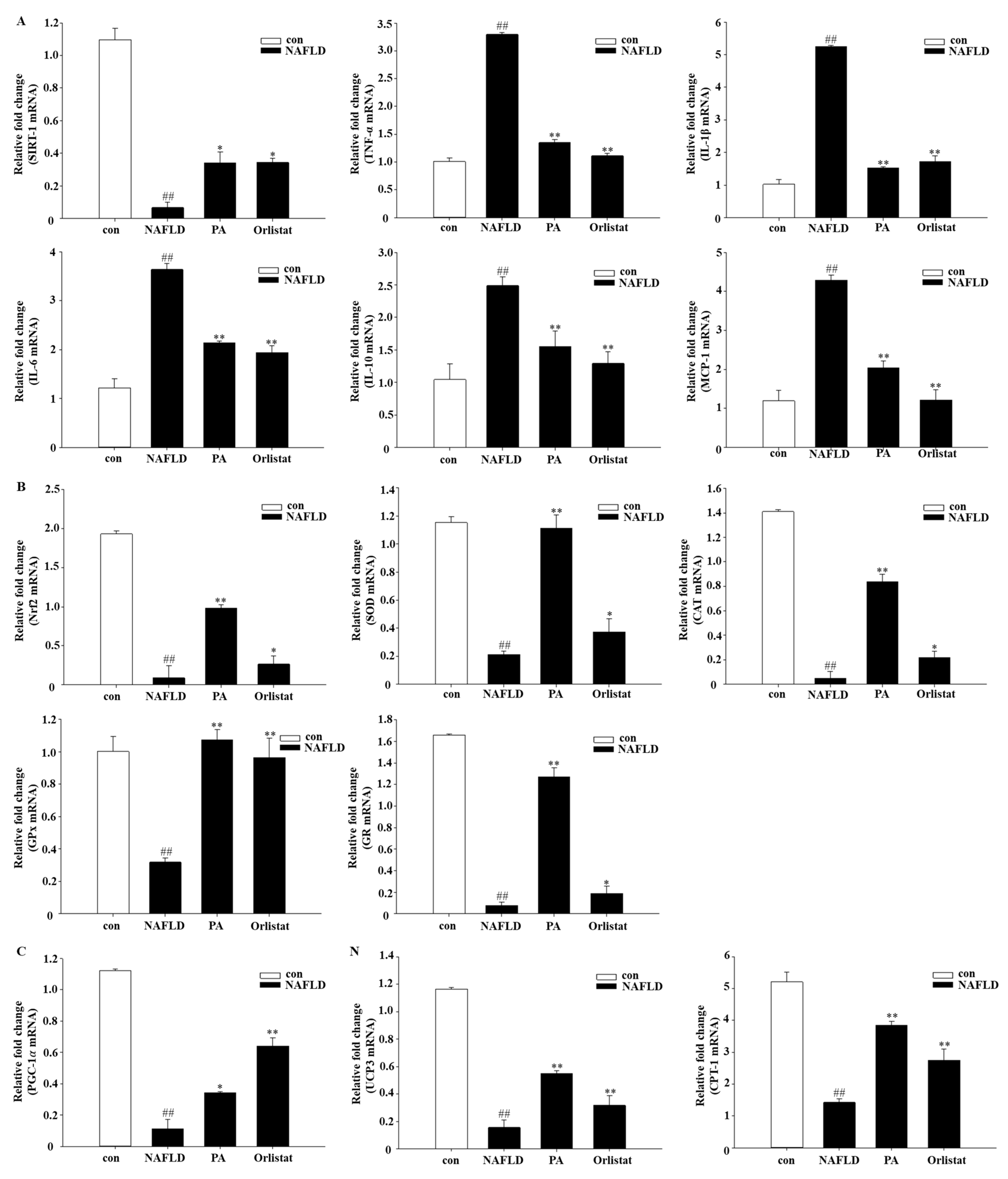
3.5. Effects of PA on Inflammatory Molecules
3.6. Effects of PA on Oxidative Stress and Mitochondrial Dysfunction
4. Discussion
4.1. Effects of PA on Body Composition and Pathomorphology
4.2. Effects of PA on Blood Biochemical Parameters
4.3. Effects of PA on Adiponectin and Leptin
4.4. Effects of PA on Lipid Accumulation
4.5. Effects of PA on Inflammatory Molecules
4.6. Effects of PA on Oxidative Stress and Mitochondrial Dysfunction
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Rector, R.S.; Thyfault, J.P.; Wei, Y.; Ibdah, J.A. Non-alcoholic fatty liver disease and the metabolic syndrome: An update. WJG 2008, 14, 185. [Google Scholar] [CrossRef] [PubMed]
- Browning, J.D.; Horton, J.D. Molecular mediators of hepatic steatosis and liver injury. J. Clin. Invest. 2004, 114, 147–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Kader, S.M.A.; El-Den Ashmawy, E.M.S. Non-alcoholic fatty liver disease: The diagnosis and management. WJH. 2015, 7, 846. [Google Scholar] [CrossRef] [PubMed]
- Kaniak, B.C.B.; da Cunha, G.M.; Choi, J.-Y.; Sirlin, C.B. Steatosis, Steatohepatitis, Nonalcoholic Fatty Liver Disease, and Nonalcoholic Steatohepatitis. In Gastrointestinal Imaging, 1st ed.; Levy, A.D., Mortele, K.J., Yeh, B.M., Eds.; Oxford University Press: New York, NY, USA, 2015; pp. 309–315. [Google Scholar]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef]
- Kotronen, A.; Peltonen, M.; Hakkarainen, A.; Sevastianova, K.; Bergholm, R.; Johansson, L.M.; Lundbom, N.; Rissanen, A.; Ridderstråle, M.; Groop, L. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology 2009, 137, 865–872. [Google Scholar] [CrossRef]
- Byrne, C.D.; Targher, G. NAFLD: A multisystem disease. J. Hepatol. 2015, 62, S47–S64. [Google Scholar] [CrossRef] [Green Version]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef]
- Ruiz-Ojeda, F.J.; Olza, J.; Gil, Á.; Aguilera, C.M. Oxidative Stress and Inflammation in Obesity and Metabolic Syndrome. In Obesity; Elsevier: Amsterdam, The Netherlands, 2018; pp. 1–15. [Google Scholar]
- Wan, X.; Xu, C.; Yu, C.; Li, Y. Role of NLRP3 inflammasome in the progression of NAFLD to NASH. Can. J. Gastroenterol. Hepatol. 2016, 2016. [Google Scholar] [CrossRef]
- Fang, Y.-L.; Chen, H.; Wang, C.-L.; Liang, L. Pathogenesis of non-alcoholic fatty liver disease in children and adolescence: From “two hit theory” to “multiple hit model”. World J. Gastroenterol. 2018, 24, 2974. [Google Scholar] [CrossRef]
- Derosa, G.; Maffioli, P. Histological Biomarkers of Nonalcoholic Fatty Liver Disease. Biomark. Liver Disease 2017, 693–705. [Google Scholar] [CrossRef]
- Parkash, O.; Saeed, S. Molecular Basis for Pathogenesis of Steatohepatitis: Contemporary Understanding and New Insights. In Non-Alcoholic Fatty Liver Disease-Molecular Bases, Prevention and Treatment; IntechOpen: London, UK, 2018. [Google Scholar] [Green Version]
- Sanyal, A.J.; Friedman, S.L.; McCullough, A.J.; Dimick-Santos, L. Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: Findings and recommendations from an American Association for the Study of Liver Diseases–US Food and Drug Administration Joint Workshop. Hepatology 2015, 61, 1392–1405. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.L.; Neuschwander-Tetri, B.A.; Rinella, M.; Sanyal, A.J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 2018, 24, 908. [Google Scholar] [CrossRef] [PubMed]
- Guerciolini, R. Mode of action of orlistat. Int. J. Obes. Relat. Metab. D 1997, 21, S12–S23. [Google Scholar]
- Zelber–Sagi, S.; Kessler, A.; Brazowsky, E.; Webb, M.; Lurie, Y.; Santo, M.; Leshno, M.; Bl ndis, L.; Halpern, Z.; Oren, R. A double-blind randomized placebo-controlled trial of orlistat for the treatment of nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2006, 4, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Ni, X.; Wang, H. Silymarin attenuated hepatic steatosis through regulation of lipid metabolism and oxidative stress in a mouse model of nonalcoholic fatty liver disease (NAFLD). Am. J. Transl. Res. 2016, 8, 1073. [Google Scholar] [PubMed]
- Guo, Y.; Ding, P.-H.; Liu, L.-J.; Shi, L.; Mao, T.-Y.; Li, J.-X.; Wang, Y.-L. Gegen Qinlian Decoction Attenuates High-Fat Diet-Induced Steatohepatitis in Rats via Gut Microbiota. Evid. Based Compl. Alt. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Boban, M.; Stockley, C.; Teissedre, P.-L.; Restani, P.; Fradera, U.; Stein-Hammer, C.; Ruf, J.-C. Drinking pattern of wine and effects on human health: Why should we drink moderately and with meals? Food Funct. 2016, 7, 2937–2942. [Google Scholar] [CrossRef]
- Snopek, L.; Mlcek, J.; Sochorova, L.; Baron, M.; Hlavacova, I.; Jurikova, T.; Kizek, R.; Sedlackova, E.; Sochor, J. Contribution of red wine consumption to human health protection. Molecules 2018, 23, 1684. [Google Scholar] [CrossRef]
- Martin, M.A.; Goya, L.; Ramos, S. Protective effects of tea, red wine and cocoa in diabetes. Evidences from human studies. Food Chem. Toxicol. 2017, 109, 302–314. [Google Scholar] [CrossRef] [Green Version]
- Park, H.J.; Jung, U.J.; Lee, M.K.; Cho, S.J.; Jung, H.K.; Hong, J.H.; Choi, M.S. Modulation of lipid metabolism by polyphenol-rich grape skin extract improves liver steatosis and adiposity in high fat fed mice. Mol. Nutr. Food Res. 2013, 57, 360–364. [Google Scholar] [CrossRef]
- Da Costa, G.F.; Santos, I.B.; de Bem, G.F.; Cordeiro, V.S.C.; da Costa, C.A.; de Carvalho, L.C.R.M.; Ognibene, D.T.; Resende, A.C.; de Moura, R.S. The beneficial effect of anthocyanidin-rich Vitis vinifera L. grape skin extract on metabolic changes induced by high-fat diet in mice involves antiinflammatory and antioxidant actions. Phytother. Res. 2017, 31, 1621–1632. [Google Scholar] [CrossRef] [PubMed]
- Chu, Q.; Zhang, S.; Chen, M.; Han, W.; Jia, R.; Chen, W.; Zheng, X. Cherry Anthocyanins Regulate NAFLD by Promoting Autophagy Pathway. Oxid. Med. Cell. Longev. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.K.; Jo, D.-G. Mulberry Fruit Extract Ameliorates Nonalcoholic Fatty Liver Disease (NAFLD) through Inhibition of Mitochondrial Oxidative Stress in Rats. Evid Based Compl. Alt. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Prior, R.L.; Lazarus, S.A.; Cao, G.; Muccitelli, H.; Hammerstone, J.F. Identification of procyanidins and anthocyanins in blueberries and cranberries (Vaccinium spp.) using high-performance liquid chromatography/mass spectrometry. J. Agr. Food Chem. 2001, 49, 1270–1276. [Google Scholar] [CrossRef]
- Caillet, S.; Côté, J.; Doyon, G.; Sylvain, J.-F.; Lacroix, M. Effect of juice processing on the cancer chemopreventive effect of cranberry. Food Res. Int. 2011, 44, 902–910. [Google Scholar] [CrossRef]
- Kim, E.K.; Choi, E.-J. SMN1 functions as a novel inhibitor for TRAF6-mediated NF-κB signaling. BBA Mol. Cell Res. 2017, 1864, 760–770. [Google Scholar] [CrossRef]
- Hotamisligil, G.S. Inflammation and metabolic disorders. Nature 2006, 444, 860. [Google Scholar] [CrossRef]
- Fernandez-Sanchez, A.; Madrigal-Santillan, E.; Bautista, M.; Esquivel-Soto, J.; Morales-Gonzalez, A.; Esquivel-Chirino, C.; Durante-Montiel, I.; Sanchez-Rivera, G.; Valadez-Vega, C.; Morales-Gonzalez, J.A. Inflammation, oxidative stress, and obesity. Int. J. Mol. Sci. 2011, 12, 3117–3132. [Google Scholar] [CrossRef]
- Feng, R.-N.; Du, S.-S.; Wang, C.; Li, Y.-C.; Liu, L.-Y.; Guo, F.-C.; Sun, C.-H. Lean-non-alcoholic fatty liver disease increases risk for metabolic disorders in a normal weight Chinese population. WJG. 2014, 20, 17932. [Google Scholar] [CrossRef]
- Basaranoglu, M.; Basaranoglu, G.; Sentürk, H. From fatty liver to fibrosis: A tale of “second hit”. WJG. 2013, 19, 1158. [Google Scholar] [CrossRef]
- Takahashi, Y.; Soejima, Y.; Fukusato, T. Animal models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. WJG. 2012, 18, 2300. [Google Scholar] [CrossRef] [PubMed]
- Hebbard, L.; George, J. Animal models of nonalcoholic fatty liver disease. Nat. Rev. Gastro. Hepat. 2011, 8, 35. [Google Scholar] [CrossRef] [PubMed]
- Mirza, M. Obesity, visceral fat, and NAFLD: Querying the role of adipokines in the progression of nonalcoholic fatty liver disease. ISRN Gastroenterol. 2011, 2011. [Google Scholar] [CrossRef] [PubMed]
- Hutley, L.; Prins, J.B. Fat as an endocrine organ: Relationship to the metabolic syndrome. Am. J. Med. Sci. 2005, 330, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Bedossa, P.; Poitou, C.; Veyrie, N.; Bouillot, J.L.; Basdevant, A.; Paradis, V.; Tordjman, J.; Clement, K. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology 2012, 56, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Bellentani, S.; Scaglioni, F.; Marino, M.; Bedogni, G. Epidemiology of non-alcoholic fatty liver disease. Digest. Dis. 2010, 28, 155–161. [Google Scholar] [CrossRef]
- Semple, S.C.; Chonn, A.; Cullis, P.R. Interactions of liposomes and lipid-based carrier systems with blood proteins: Relation to clearance behaviour in vivo. Adv. Drug Deliver. Rev. 1998, 32, 3–17. [Google Scholar] [CrossRef]
- Athyros, V.G.; Mikhailidis, D.P.; Didangelos, T.P.; Giouleme, O.I.; Liberopoulos, E.N.; Karagiannis, A.; Kakafika, A.I.; Tziomalos, K.; Burroughs, A.K.; Elisaf, M.S. Effect of multifactorial treatment on non-alcoholic fatty liver disease in metabolic syndrome: A randomised study. Curr. Med. Res. Opin. 2006, 22, 873–883. [Google Scholar] [CrossRef]
- Vanni, E.; Bugianesi, E.; Kotronen, A.; De Minicis, S.; Yki-Järvinen, H.; Svegliati-Baroni, G. From the metabolic syndrome to NAFLD or vice versa? Digest. Liver Dis. 2010, 42, 320–330. [Google Scholar] [CrossRef] [Green Version]
- Verma, S.; Jensen, D.; Hart, J.; Mohanty, S.R. Predictive value of ALT levels for non-alcoholic steatohepatitis (NASH) and advanced fibrosis in non-alcoholic fatty liver disease (NAFLD). Liver Int. 2013, 33, 1398–1405. [Google Scholar] [CrossRef]
- Kadowaki, T.; Yamauchi, T. Adiponectin and adiponectin receptors. Endocr. Rev. 2005, 26, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Arita, Y.; Kihara, S.; Ouchi, N.; Takahashi, M.; Maeda, K.; Miyagawa, J.-I.; Hotta, K.; Shimomura, I.; Nakamura, T.; Miyaoka, K. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem. Bioph. Res. Commun. 1999, 257, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, E.; Mitry, R.R.; Quaglia, A.; Hussain, M.J.; Dhawan, A. Serum levels of CK18 M30 and leptin are useful predictors of steatohepatitis and fibrosis in paediatric NAFLD. J. Pediatr. Gastr. Nutr. 2010, 51, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Siersbæk, R.; Nielsen, R.; Mandrup, S. PPARγ in adipocyte differentiation and metabolism–Novel insights from genome-wide studies. FEBS Lett. 2010, 584, 3242–3249. [Google Scholar] [CrossRef]
- Ip, E.; Farrell, G.; Hall, P.; Robertson, G.; Leclercq, I. Administration of the potent PPARalpha agonist, Wy-14,643, reverses nutritional fibrosis and steatohepatitis in mice. Hepatology 2004, 39, 1286–1296. [Google Scholar] [CrossRef]
- Farmer, S.R. Transcriptional control of adipocyte formation. Cell Metab. 2006, 4, 263–273. [Google Scholar] [CrossRef] [Green Version]
- Siraj, F.M.; SathishKumar, N.; Kim, Y.J.; Kim, S.Y.; Yang, D.C. Ginsenoside F2 possesses anti-obesity activity via binding with PPARγ and inhibiting adipocyte differentiation in the 3T3-L1 cell line. J. Enzym. Inhib. Med. Chem. 2015, 30, 9–14. [Google Scholar] [CrossRef]
- Hua, T.N.; Kim, M.-K.; Vo, V.T.; Choi, J.-W.; Choi, J.H.; Kim, H.-W.; Cha, S.-K.; Park, K.-S.; Jeong, Y. Inhibition of oncogenic Src induces FABP4-mediated lipolysis via PPARγ activation exerting cancer growth suppression. EBioMedicine 2019, 41, 134–145. [Google Scholar] [CrossRef]
- Cabré, A.; Babio, N.; Lázaro, I.; Bulló, M.; Garcia-Arellano, A.; Masana, L.; Salas-Salvadó, J. FABP4 predicts atherogenic dyslipidemia development. The PREDIMED study. Atherosclerosis 2012, 222, 229–234. [Google Scholar] [CrossRef]
- Søndergaard, E.; Johansen, R.F.; Jensen, M.D.; Nielsen, S. Postprandial VLDL-TG metabolism in type 2 diabetes. Metabolism 2017, 75, 25–35. [Google Scholar] [CrossRef]
- Yan, W.; Zhang, H.; Liu, P.; Wang, H.; Liu, J.; Gao, C.; Liu, Y.; Lian, K.; Yang, L.; Sun, L. Impaired mitochondrial biogenesis due to dysfunctional adiponectin-AMPK-PGC-1α signaling contributing to increased vulnerability in diabetic heart. Basic Res. Cardiol. 2013, 108, 329. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, S.; Mihaylova, M.M.; Zheng, B.; Hou, X.; Jiang, B.; Park, O.; Luo, Z.; Lefai, E.; Shyy, J.Y.-J. AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice. Cell Metab. 2011, 13, 376–388. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.-H.; Jang, J.; Chung, S.-I.; Yoon, Y. AMPK and SREBP-1c mediate the anti-adipogenic effect of β-hydroxyisovalerylshikonin. Int. J. Mol. Med. 2016, 37, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Berlanga, A.; Guiu-Jurado, E.; Porras, J.A.; Auguet, T. Molecular pathways in non-alcoholic fatty liver disease. Clin. Exp. Gastroenterol. 2014, 7, 221. [Google Scholar]
- Sharpe, L.J.; Brown, A.J. Controlling cholesterol synthesis beyond 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR). J. Biol. Chem. 2013, 288, 18707–18715. [Google Scholar] [CrossRef]
- Day, C.P.; Oliver, F.W.J. Steatohepatitis: A tale of two “hits”? Gastroerentology 1998, 114, 842–845. [Google Scholar] [CrossRef]
- Lewis, J.R.; Smruti, R.M. Nonalcoholic fatty liver disease: A review and update. Digest. Dis. Sci. 2010, 55, 560–578. [Google Scholar] [CrossRef]
- Chalkiadaki, A.; Guarente, L. Sirtuins mediate mammalian metabolic responses to nutrient availability. Nat. Rev. Endocrinol. 2012, 8, 287. [Google Scholar] [CrossRef]
- Purushotham, A.; Schug, T.T.; Xu, Q.; Surapureddi, S.; Guo, X.; Li, X. Hepatocyte-specific deletion of SIRT1 alters fatty acid metabolism and results in hepatic steatosis and inflammation. Cell Metab. 2009, 9, 327–338. [Google Scholar] [CrossRef]
- Stojsavljević, S.; Palčić, M.G.; Jukić, L.V.; Duvnjak, L.S.; Duvnjak, M. Adipokines and proinflammatory cytokines, the key mediators in the pathogenesis of nonalcoholic fatty liver disease. WJG. 2014, 20, 18070. [Google Scholar] [CrossRef]
- Procaccini, C.; Galgani, M.; De Rosa, V.; Carbone, F.; La Rocca, C.; Ranucci, G.; Matarese, G. Leptin: The prototypic adipocytokine and its role in NAFLD. Curr. Pharm. Des. 2010, 16, 1902–1912. [Google Scholar] [CrossRef] [PubMed]
- Mridha, A.R.; Wree, A.; Robertson, A.A.; Yeh, M.M.; Johnson, C.D.; Van Rooyen, D.M.; Haczeyni, F.; Teoh, N.C.-H.; Savard, C.; Ioannou, G.N. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J. Hepatol. 2017, 66, 1037–1046. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Zhao, Y.; Wang, K.; Shi, X.; Wang, Y.; Huang, H.; Zhuang, Y.; Cai, T.; Wang, F.; Shao, F. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 2015, 526, 660. [Google Scholar] [CrossRef] [PubMed]
- Braud, L.; Battault, S.; Meyer, G.; Nascimento, A.; Gaillard, S.; de Sousa, G.; Rahmani, R.; Riva, C.; Armand, M.; Maixent, J.-M. Antioxidant properties of tea blunt ROS-dependent lipogenesis: Beneficial effect on hepatic steatosis in a high fat-high sucrose diet NAFLD obese rat model. J. Nutr. Biochem. 2017, 40, 95–104. [Google Scholar] [CrossRef]
- Petta, S.; Muratore, C.; Craxi, A. Non-alcoholic fatty liver disease pathogenesis: The present and the future. Digest. Liver Dis. 2009, 41, 615–625. [Google Scholar] [CrossRef]
- Divya, T.; Dineshbabu, V.; Soumyakrishnan, S.; Sureshkumar, A.; Sudhandiran, G. Celastrol enhances Nrf2 mediated antioxidant enzymes and exhibits anti-fibrotic effect through regulation of collagen production against bleomycin-induced pulmonary fibrosis. Chem. Biol. Interact. 2016, 246, 52–62. [Google Scholar] [CrossRef]
- Ng, C.F.; Schafer, F.Q.; Buettner, G.R.; Rodgers, V.G.J. The rate of cellular hydrogen peroxide removal shows dependency on GSH: Mathematical insight into in vivo H2O2 and GPx concentrations. Free Radical Res. 2007, 41, 1201–1211. [Google Scholar] [CrossRef]
- Murase, T.; Aoki, M.; Tokimitsu, I. Supplementation with α-linolenic acid-rich diacylglycerol suppresses fatty liver formation accompanied by an up-regulation of β-oxidation in Zucker fatty rats. B.B.A. Mol. Cell Biol. Lipids 2005, 1733, 224–231. [Google Scholar] [CrossRef]
- Machado, M.V.; Diehl, A.M. Pathogenesis of nonalcoholic steatohepatitis. Gastroenterology 2016, 150, 1769–1777. [Google Scholar] [CrossRef]
- Mello, T.; Materozzi, M.; Galli, A. PPARs and Mitochondrial Metabolism: From NAFLD to HCC. PPAR Res. 2016, 2016, 7403230. [Google Scholar] [CrossRef]
- Lin, J.; Handschin, C.; Spiegelman, B.M. Metabolic control through the PGC-1 family of transcription coactivators. Cell Metab. 2005, 1, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Gene Name | Sequence | Sequence | ||
|---|---|---|---|---|
| PPAR-𝛾 | Forward | 5-GAA AGA CAA CGG ACA AAT CAC-3 | Reverse | 5-GAA ACT GGC ACC CTT GAA-3 |
| C/EBP-𝛼 | Forward | 5-CGT CTA AGA TGA GGG AGT C-3 | Reverse | 5-GGC ACA AGG TTA CTT CCT-3 |
| SREBP−1c | Forward | 5-CTT CTG GAG ACA TCG CAA AC-3 | Reverse | 5-GGT AGA CAA CAG CCG CAT C-3 |
| ACS | Forward | 5-AAG CCC AGA GTT ACG AGT AT-3 | Reverse | 5-ACA CAG GAA TAG AGG AGT TCT-3 |
| FAS | Forward | 5-CTT GGG TGC TGA CTA CAA CC-3 | Reverse | 5-GCC CTC CCG TAC ACT CAC TC-3 |
| HMGCR | Forward | 5-TTC TGC TCT TGA TTG ACC TTT C-3 | Reverse | 5-TTT CCC TTA CTT CAT CCT GTG A-3 |
| SIRT1 | Forward | 5-GGC GGG GAA CGA CTG CG-3 | Reverse | 5-GGA GTC ATG GGG GCT GTA CTG-3 |
| TNF-α | Forward | 5-AAG CCT GTA GCC CAC GTC GT-3 | Reverse | 5-GGC ACC ACT AGT TGG TTG TC-3 |
| IL-1β | Forward | 5-AAC CAA GCA ACG AVA AAA TA-3 | Reverse | 5-AGG TGC TGA TGT ACC AGT TG-3 |
| IL-6 | Forward | 5-CCG GAG AGG AGA CTT CAC AG-3 | Reverse | 5-GGA AAT TGG GGT AGG AAG GA-3 |
| IL-10 | Forward | 5-TCA GCT GTG TCT GGG CCA CT-3 | Reverse | 5-TTA TGA GTA GGG ACA GGA AG-3 |
| MCP-1 | Forward | 5-TGA TCC CAA TGA GTA GGC TGG AG-3 | Reverse | 5-ATG TCT GGA CCC ATT CCT TCT TG-3 |
| PGC-1α | Forward | 5-ATT CGG GAG CTG GAT GGC TT-3 | Reverse | 5-CCG ATT GGT CGC TAC ACC AC-3 |
| UCP3 | Forward | 5-ACC CGA TAC ATG AAC GCT CC-3 | Reverse | 5-TCA TCA CGT TCC AAG CTC CC-3 |
| CPT-1 | Forward | 5-TGT GTG AGG ATG CTG CTT CC-3 | Reverse | 5-CTC GGA GAG CTA AGC TTG TC-3 |
| Nrf2 | Forward | 5-AGC ACA TCC AGA CAG ACA CCA GT-3 | Reverse | 5-TTC AGC GTG GCT GGG GAT AT-3 |
| SOD | Forward | 5-CAA TGG TGG GGG ACA TAT TA-3 | Reverse | 5-TTG ATA GCC TCC AGC AAC TC-3 |
| CAT | Forward | 5-GAA CGA GGA GGA GAG GAA AC-3 | Reverse | 5-TGA AAT TCT TGA CCG CTT TC-3 |
| GPx | Forward | 5-ACA TTC CCA GTC ATT CTA CC-3 | Reverse | 5-TTC AAG CAG GCA GAT ACG-3 |
| GR | Forward | 5-CGG CGA TCT CCA CAG CAA TG-3 | Reverse | 5-ACC GCT CCA CAC ATC CTG ATT G-3 |
| GAPDH | Forward | 5-GCA CAG TCA AGG CCG AGA AT-3 | Reverse | 5-GCC TTC TCC ATG GTG GTG AA-3 |
| CON | HFD | HFD + PA | HFD + Orlistat | |
|---|---|---|---|---|
| Initial body weight (g) | 16.85 ± 0.58 a | 17.29 ± 0.44 a | 17.32 ± 0.72 a | 16.68 ± 0.93 a |
| Final body weight (g) | 26.14 ± 2.67 c | 44.86 ± 2.8 a | 31.27 ± 1.53 b | 31.20 ± 1.77 b |
| Body-weight gain (g) | 9.29 ± 2.43 d | 27.57 ± 2.55 a | 13.95 ± 3.6 c | 14.52 ± 3.21 b,c |
| Total energy intake (kcal) | 749.73 ± 26.02 c | 1194.97 ± 35.89 a | 973.68 ± 29.43 b | 975.14 ± 32.32 b |
| Lean mass (g) | 0.25 ± 0.07 d | 2.07 ± 0.64 a | 0.88 ± 0.39 b | 0.57 ± 0.24 c |
| Epididymal-adipose-tissue weight (g) | 0.20 ± 0.02 d | 3.50 ± 0.4 a | 1.02 ± 0.2 b | 0.75 ± 0.09 c |
| Subcutaneous-adipose-tissue weight (g) | 0.07 ± 0.05 d | 1.50 ± 0.08 a | 0.47 ± 0.04 b | 0.23 ± 0.14 c |
| Visceral-adipose-tissue weight (g) | 0.16 ± 0.03 c | 0.33 ± 0.08 a | 0.23 ± 0.02 b | 0.21 ± 0.04 b |
| interscapular adipose tissue weight (g) | 16.85 ± 0.58 a | 17.29 ± 0.44 a | 17.32 ± 0.72 a | 16.68 ± 0.93 a |
| ALT (U/L) | 34.50 ± 3.42 b | 66.00 ± 3.54 a | 39.00 ± 1.73 b | 35.00 ± 2.65 b |
| AST (U/L) | 73.50 ± 5.45 c | 344.50 ± 0.71 a | 125.75 ± 1.49 b | 129.33 ± 4.24 b |
| TP (g/dL) | 4.68 ± 0.59 c | 5.45 ± 0.64 a | 5.05 ± 0.38 b | 5.20 ± 0.50 a,b |
| TC (mg/dL) | 107.20 ± 4.21 d | 184.50 ± 3.27 a | 116.25 ± 5.29 c | 128.00 ± 4.97 b |
| LDL-C (mg/dL) | 21.40 ± 2.70 c | 114.00 ± 4.05 a | 45.50 ± 1.78 b | 46.00 ± 5.66 b |
| HDL-C (mg/dL) | 67.67 ± 4.02 a | 33.40 ± 2.70 c | 56.50 ± 3.54 b | 54.25 ± 2.35 b |
| TG (mg/dL) | 115.20 ± 3.0 c | 261.83 ± 3.32 a | 137.50 ± 2.36 b | 113.25 ± 1.66 c |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, M.; Choi, Y.-J.; Tang, Y.; Bae, S.M.; Yang, H.P.; Kim, E.-K. Efficacy and Mechanism of Polymerized Anthocyanin from Grape-Skin Extract on High-Fat-Diet-Induced Nonalcoholic Fatty Liver Disease. Nutrients 2019, 11, 2586. https://doi.org/10.3390/nu11112586
Fan M, Choi Y-J, Tang Y, Bae SM, Yang HP, Kim E-K. Efficacy and Mechanism of Polymerized Anthocyanin from Grape-Skin Extract on High-Fat-Diet-Induced Nonalcoholic Fatty Liver Disease. Nutrients. 2019; 11(11):2586. https://doi.org/10.3390/nu11112586
Chicago/Turabian StyleFan, Meiqi, Young-Jin Choi, Yujiao Tang, Sung Mun Bae, Hyun Pil Yang, and Eun-Kyung Kim. 2019. "Efficacy and Mechanism of Polymerized Anthocyanin from Grape-Skin Extract on High-Fat-Diet-Induced Nonalcoholic Fatty Liver Disease" Nutrients 11, no. 11: 2586. https://doi.org/10.3390/nu11112586
APA StyleFan, M., Choi, Y.-J., Tang, Y., Bae, S. M., Yang, H. P., & Kim, E.-K. (2019). Efficacy and Mechanism of Polymerized Anthocyanin from Grape-Skin Extract on High-Fat-Diet-Induced Nonalcoholic Fatty Liver Disease. Nutrients, 11(11), 2586. https://doi.org/10.3390/nu11112586





