Curcumin as a Therapeutic Strategy in Liver Diseases
Abstract
1. Editorial
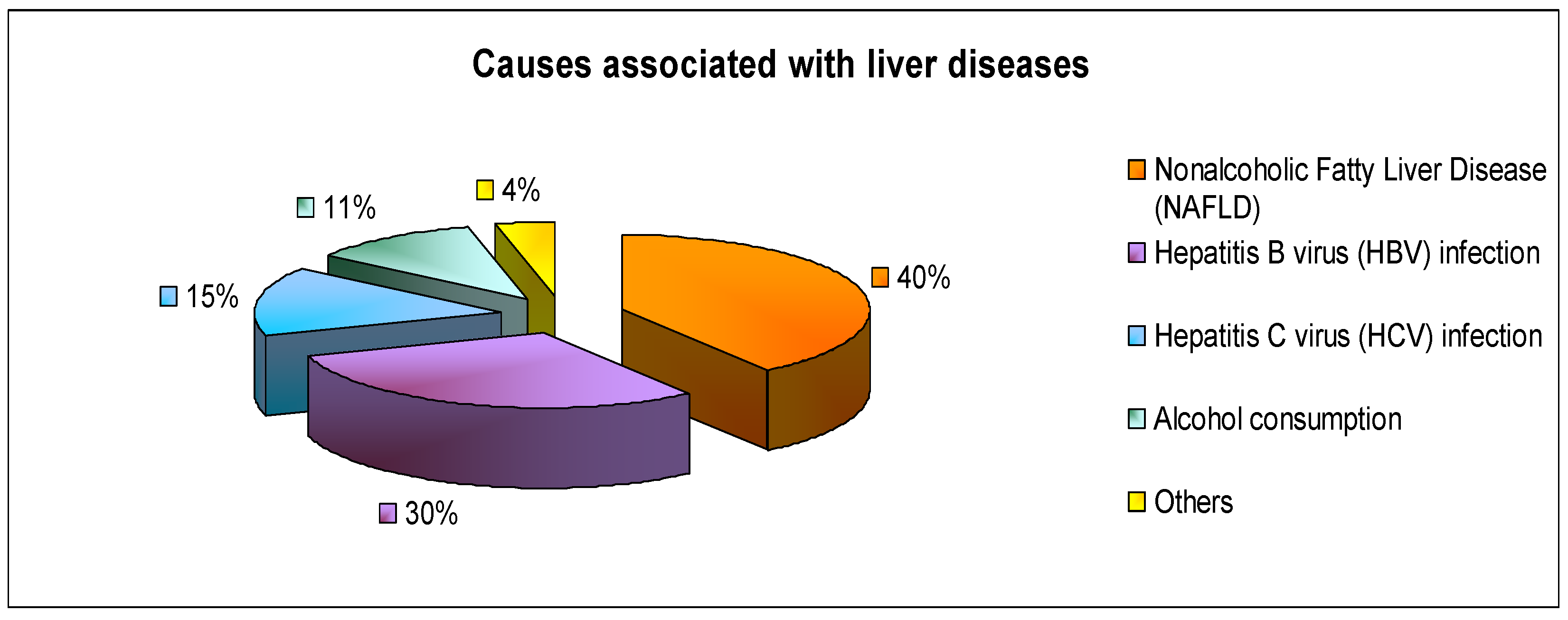
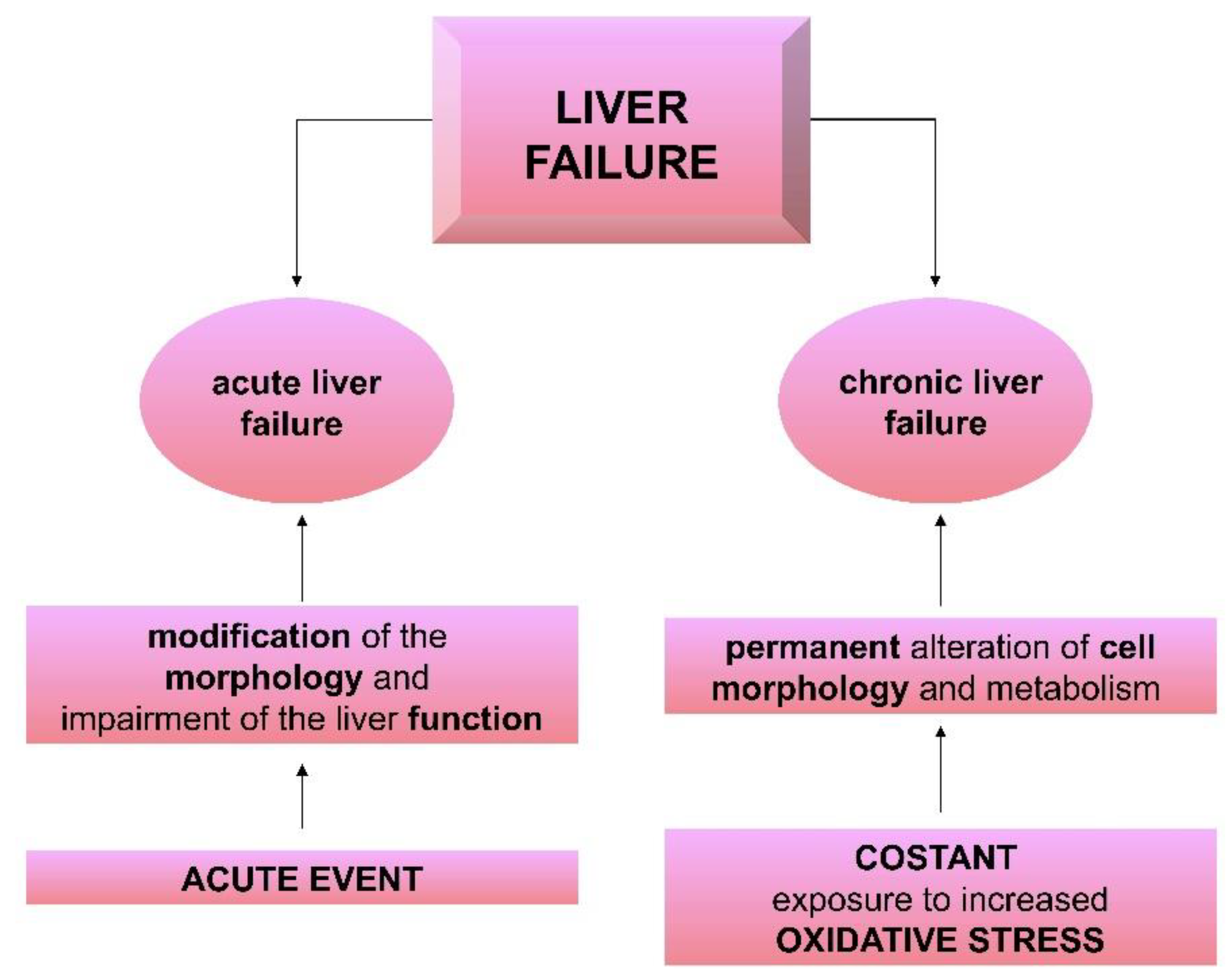
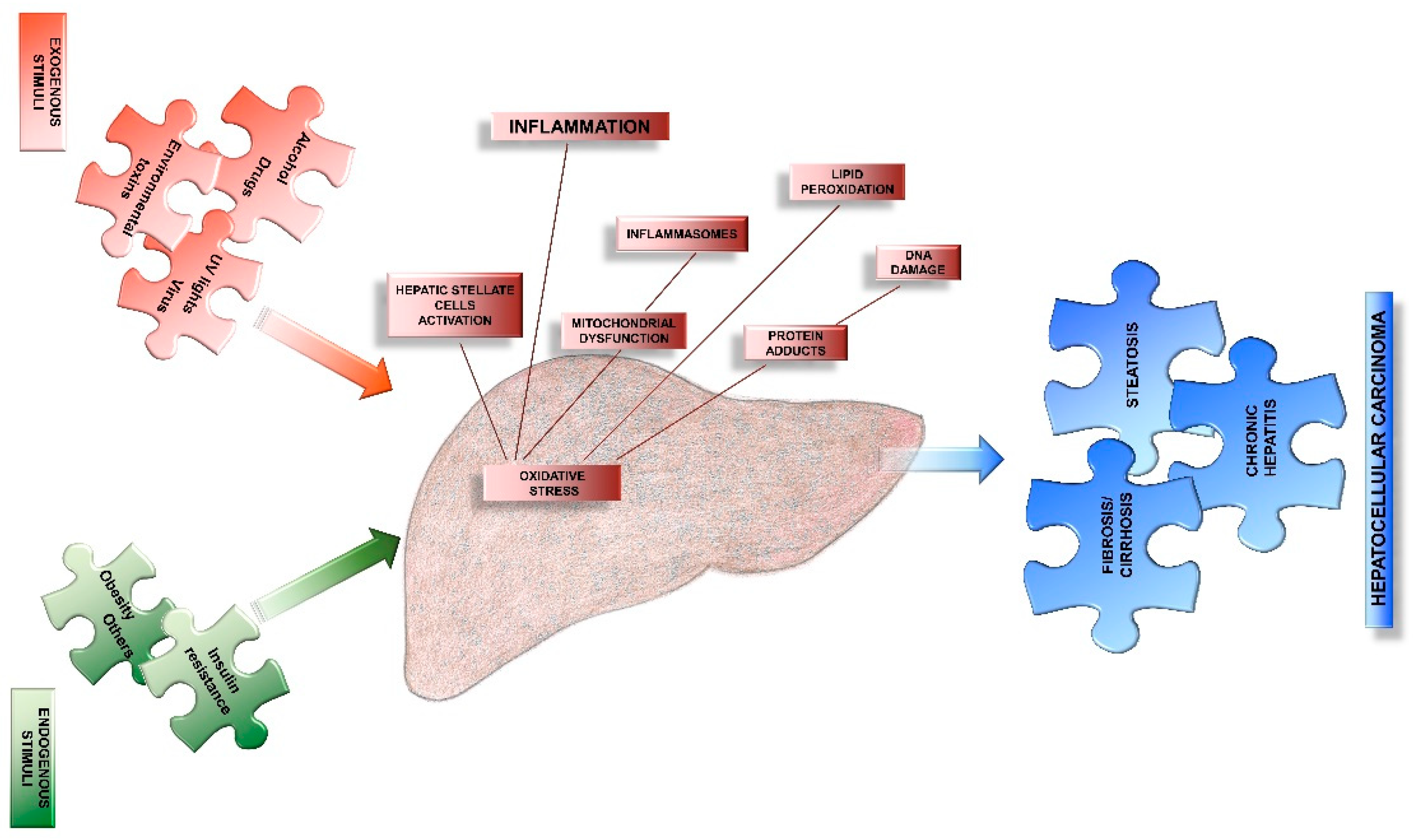
2. Liver in Acute and Chronic Diseases
3. Oxidative Stress as Major Causes of Liver Diseases
4. Curcumin and Oxidative Stress Associated to the Liver Injuries
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Muriel, P. The Liver: General Aspects and Epidemiology. In Liver Pathophysiology; Muriel, P., Ed.; Elsevier: Waltham, MA, USA, 2017; pp. 3–22. [Google Scholar]
- Mokdad, A.A.; Lopez, A.D.; Shahraz, S.; Lozano, R.; Mokdad, A.H.; Stanaway, J.; Murray, C.J.; Naghavi, M. Liver cirrhosis mortality in 187 countries between 1980 and 2010: A systematic analysis. BMC Med. 2014, 1, 145–169. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health Estimates 2015: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2015; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Asrani, S.K.; Devarbhavi, H.; Eaton, J.; Kamath, P.S. Burden of liver diseases in the world. J. Hepatol. 2019, 70, 151–171. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health Estimates 2015: Disease Burden by Cause, Age, Sex, by Country and by Region, 2000–2015; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Farzaei, M.H.; Zobeiri, M.; Parvizi, F.; El-Senduny, F.F.; Marmouzi, I.; Coy-Barrera, E.; Naseri, R.; Nabavi, S.M.; Rahimi, R.; Abdollahi, M. Curcumin in Liver Diseases: A Systematic Review of the Cellular Mechanisms of Oxidative Stress and Clinical Perspective. Nutrients 2018, 10, 855. [Google Scholar] [CrossRef] [PubMed]
- Xing, T.J. Clinical Classification of Liver Failure: Consensus, Contradictions and New Recommendations. J. Clin. Gastroenterol. Hepatol. 2017, 1, 2. [Google Scholar] [CrossRef]
- Weiss, E.; Velly, L. Management of liver failure in General Intensive Care Unit. Anaesth. Crit. Care Pain Med. 2019. [Google Scholar] [CrossRef]
- Cichoż-Lach, H.; Michalak, A. Oxidative stress as a crucial factor in liver diseases. World J. Gastroenterol. 2014, 20, 8082–8091. [Google Scholar] [CrossRef]
- Ezhilarasan, D. Oxidative stress is bane in chronic liver diseases: Clinical and experimental perspective. Arab J. Gastroenterol. 2018, 19, 56–64. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, L.; Ouyang, X.; Jiang, Z.; Xie, Z.; Fan, L.; Zhu, D.; Li, L. Advanced oxidation protein products play critical roles in liver diseases. Eur. J. Clin. Investig. 2019. [Google Scholar] [CrossRef]
- Negi, A.S.; Kumar, J.K.; Luqman, S.; Shanker, K.; Gupta, M.M.; Khanuja, S.P.S. Recent Advances in Plant Hepatoprotectives: A Chemical and Biological Profile of Some Important Leads. Med. Res. Rev. 2008, 28, 746–772. [Google Scholar] [CrossRef]
- Bachmeier, B.E.; Melchart, D. Therapeutic Effects of Curcumin-From Traditional Past to Present and Future Clinical Applications. Int. J. Mol. Sci. 2019, 20, 3757. [Google Scholar] [CrossRef]
- Mirzaei, H.; Shakeri, A.; Rashidi, B.; Jalili, A.; Banikazemi, Z.; Sahebkar, A. Phytosomal curcumin: A review of pharmacokinetic, experimental and clinical studies. Biomed. Pharmacother. 2017, 85, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Amalraj, A.; Pius, A.; Gopi, S.; Gopi, S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives—A review. J. Tradit. Complement. Med. 2016, 7, 205–233. [Google Scholar] [CrossRef] [PubMed]
- Ak, T.; Gülçin, I. Antioxidant and radical scavenging properties of curcumin. Chem. Biol. Interact. 2008, 174, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Tokaç, M.; Taner, G.; Aydın, S.; Ozkardeş, A.B.; Dündar, H.Z.; Taşlıpınar, M.Y.; Arıkök, A.T.; Kılıç, M.; Başaran, A.A.; Basaran, N. Protective effects of curcumin against oxidative stress parameters and DNA damage in the livers and kidneys of rats with biliary obstruction. Food Chem. Toxicol. 2013, 61, 28–35. [Google Scholar] [CrossRef]
- Ghoreshi, Z.A.; Kabirifar, R.; Safari, F.; Karimollah, A.; Moradi, A.; Eskandari-Nasab, E. Hepatoprotective effects of curcumin in rats after bile duct ligation via downregulation of Rac1 and NOX1. Nutrition 2017, 36, 72–78. [Google Scholar] [CrossRef]
- Liu, W.; Xu, Z.; Li, H.; Guo, M.; Yang, T.; Feng, S.; Xu, B.; Deng, Y. Protective effects of curcumin against mercury-induced hepatic injuries in rats, involvement of oxidative stress antagonism, and Nrf2-ARE pathway activation. Hum. Exp. Toxicol. 2017, 36, 949–966. [Google Scholar] [CrossRef]
- Shapiro, H.; Ashkenazi, M.; Weizman, N.; Shahmurov, M.; Aeed, H.; Bruck, R. Curcumin ameliorates acute thioacetamide-induced hepatotoxicity. J. Gastroenterol. Hepatol. 2006, 21, 358–366. [Google Scholar] [CrossRef]
- Reyes-Gordillo, K.; Segovia, J.; Shibayama, M.; Vergara, P.; Moreno, M.G.; Muriel, P. Curcumin protects against acute liver damage in the rat by inhibiting NF-κB, proinflammatory cytokines production and oxidative stress. Biochim. Biophys. Acta 2007, 1770, 989–996. [Google Scholar] [CrossRef]
- Vera-Ramirez, L.; Pérez-Lopez, P.; Varela-Lopez, A.; Ramirez-Tortosa, M.; Battino, M.; Quiles, J.L. Curcumin and liver disease. Biofactors 2013, 39, 88–100. [Google Scholar] [CrossRef]
- Akila, G.; Rajakrishnan, V.; Viswanathan, P.; Rajashekaran, K.N.; Menon, V.P. Effects of curcumin on lipid profile and lipid peroxidation status in experimental hepatic fibrosis. Hepatol. Res. 1998, 11, 147–157. [Google Scholar] [CrossRef]
- DeMello, V.D.; Matte, A.; Perfilyev, A.; Männistö, V.; Rönn, T.; Nilsson, E.; Käkelä, P.; Ling, C.; Pihlajamäki, J. Human liver epigenetic alterations in non-alcoholic steatohepatitis are related to insulin action. Epigenetics 2017, 12, 287–295. [Google Scholar] [CrossRef] [PubMed]
| Deaths (000s) | % of Total Deaths | |
|---|---|---|
| World | 1162 | 2.1 |
| East Asia and Pacific | 328 | 2.0 |
| Europe and Central Asia | 115 | 1.2 |
| Latin America and Caribbean | 98 | 2.7 |
| Middle East and North Africa | 77 | 3.5 |
| North America | 50 | 1.7 |
| South Asia | 314 | 2.5 |
| Sub-Saharan Africa | 179 | 1.9 |
| DALY (000s) | YLL (000s) | |
|---|---|---|
| Global | 41,486 | 40,986 |
| WHO African Region | 7242 | 7195 |
| WHO Region of the Americas | 4890 | 4826 |
| WHO South-East Asia Region | 15,581 | 15,450 |
| WHO European Region | 33,608 | 3502 |
| WHO Eastern Mediterranean Region | 3409 | 3371 |
| WHO Western Pacific Region | 6518 | 6407 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rezzani, R.; Franco, C.; Rodella, L.F. Curcumin as a Therapeutic Strategy in Liver Diseases. Nutrients 2019, 11, 2498. https://doi.org/10.3390/nu11102498
Rezzani R, Franco C, Rodella LF. Curcumin as a Therapeutic Strategy in Liver Diseases. Nutrients. 2019; 11(10):2498. https://doi.org/10.3390/nu11102498
Chicago/Turabian StyleRezzani, Rita, Caterina Franco, and Luigi Fabrizio Rodella. 2019. "Curcumin as a Therapeutic Strategy in Liver Diseases" Nutrients 11, no. 10: 2498. https://doi.org/10.3390/nu11102498
APA StyleRezzani, R., Franco, C., & Rodella, L. F. (2019). Curcumin as a Therapeutic Strategy in Liver Diseases. Nutrients, 11(10), 2498. https://doi.org/10.3390/nu11102498







