Glycemic Index, Glycemic Load and Cancer Risk: An Updated Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Statistical Analysis
3. Results
3.1. Results of the Individual Studies
3.1.1. Multiple Cancer Sites
3.1.2. Hormone-Related Cancers
3.1.3. Cancers of the Digestive Tract
3.1.4. Other Neoplasms
3.2. Update of the Summary Estimates
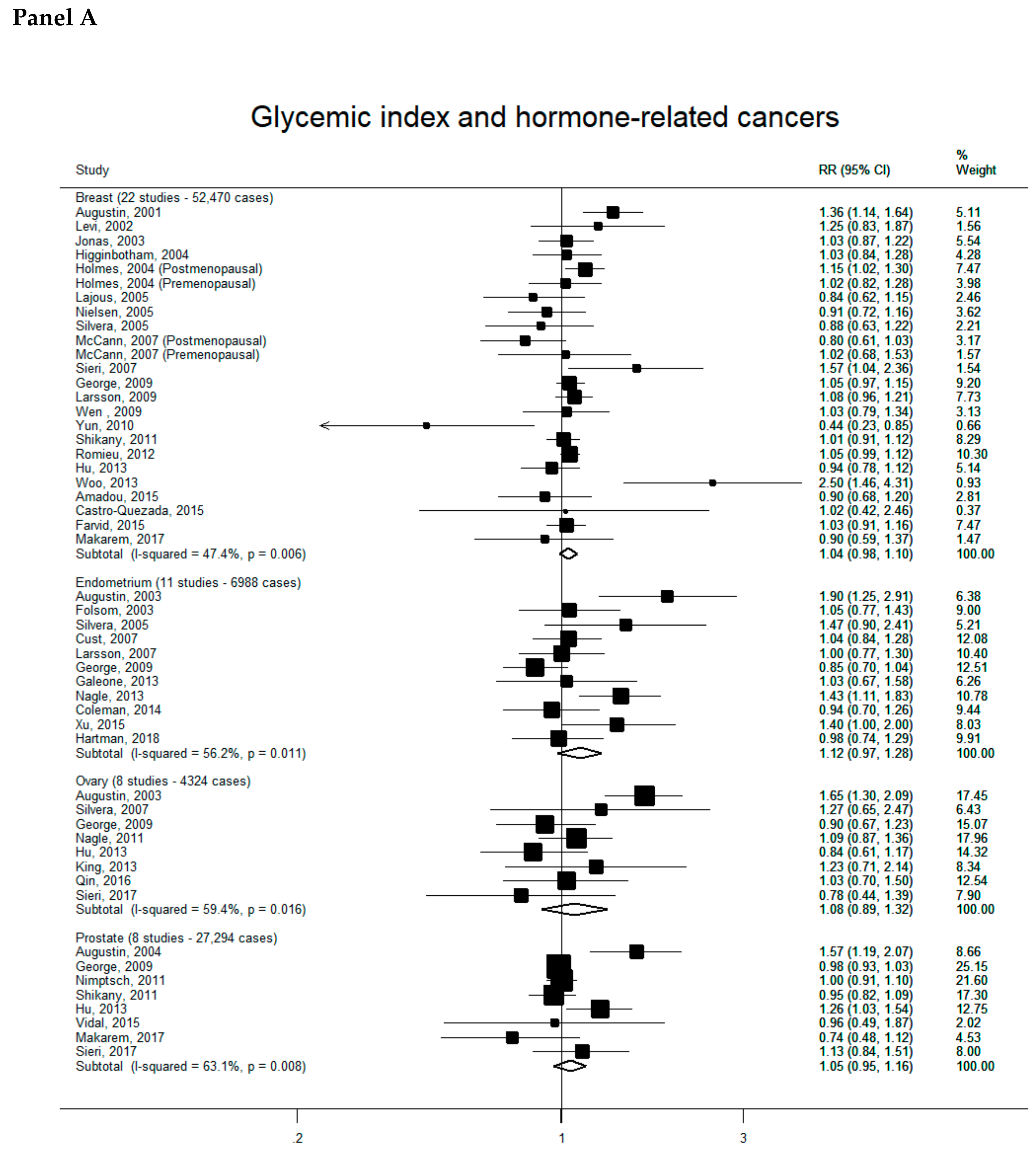
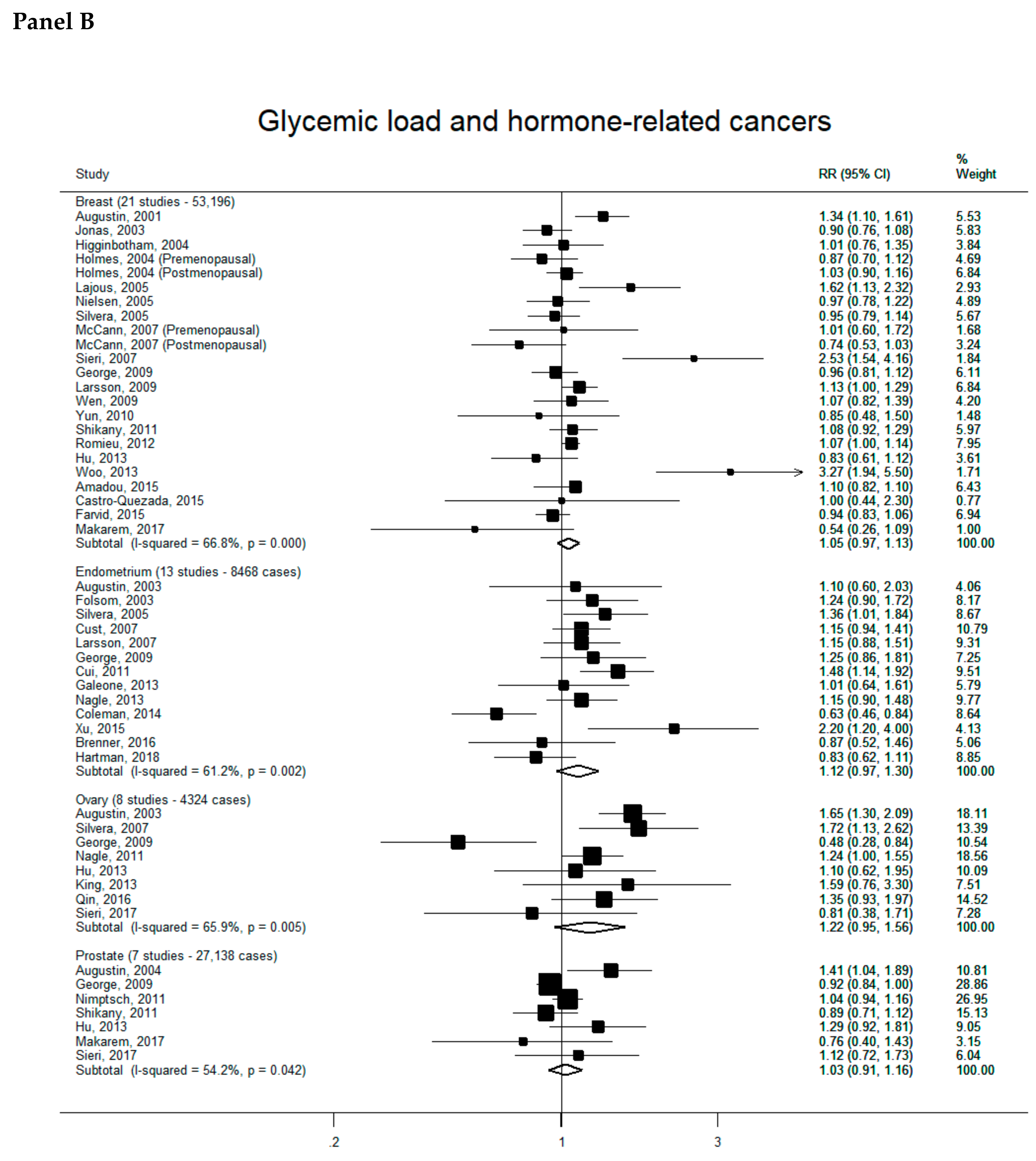
3.2.1. Hormone-Related Cancers
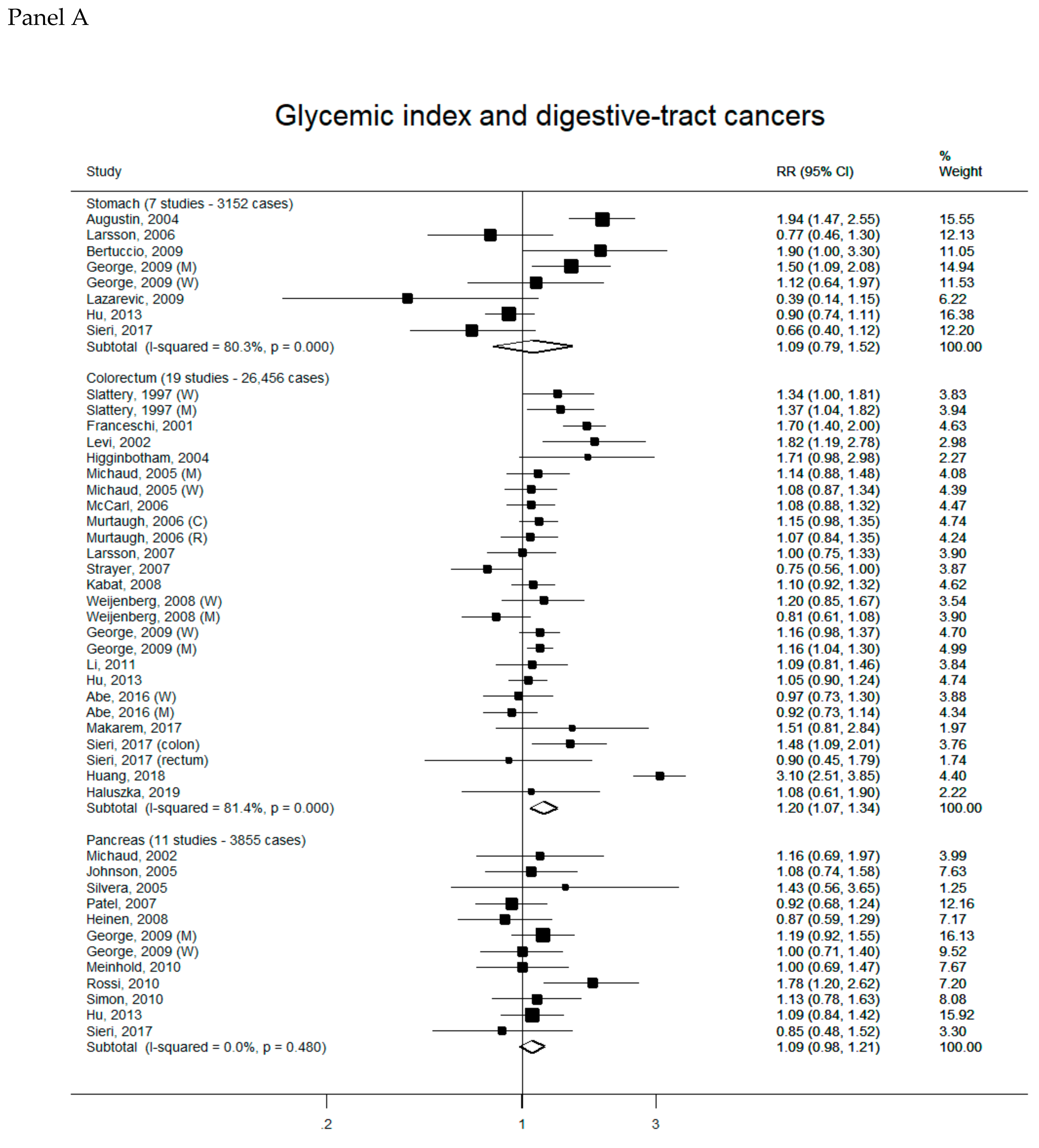
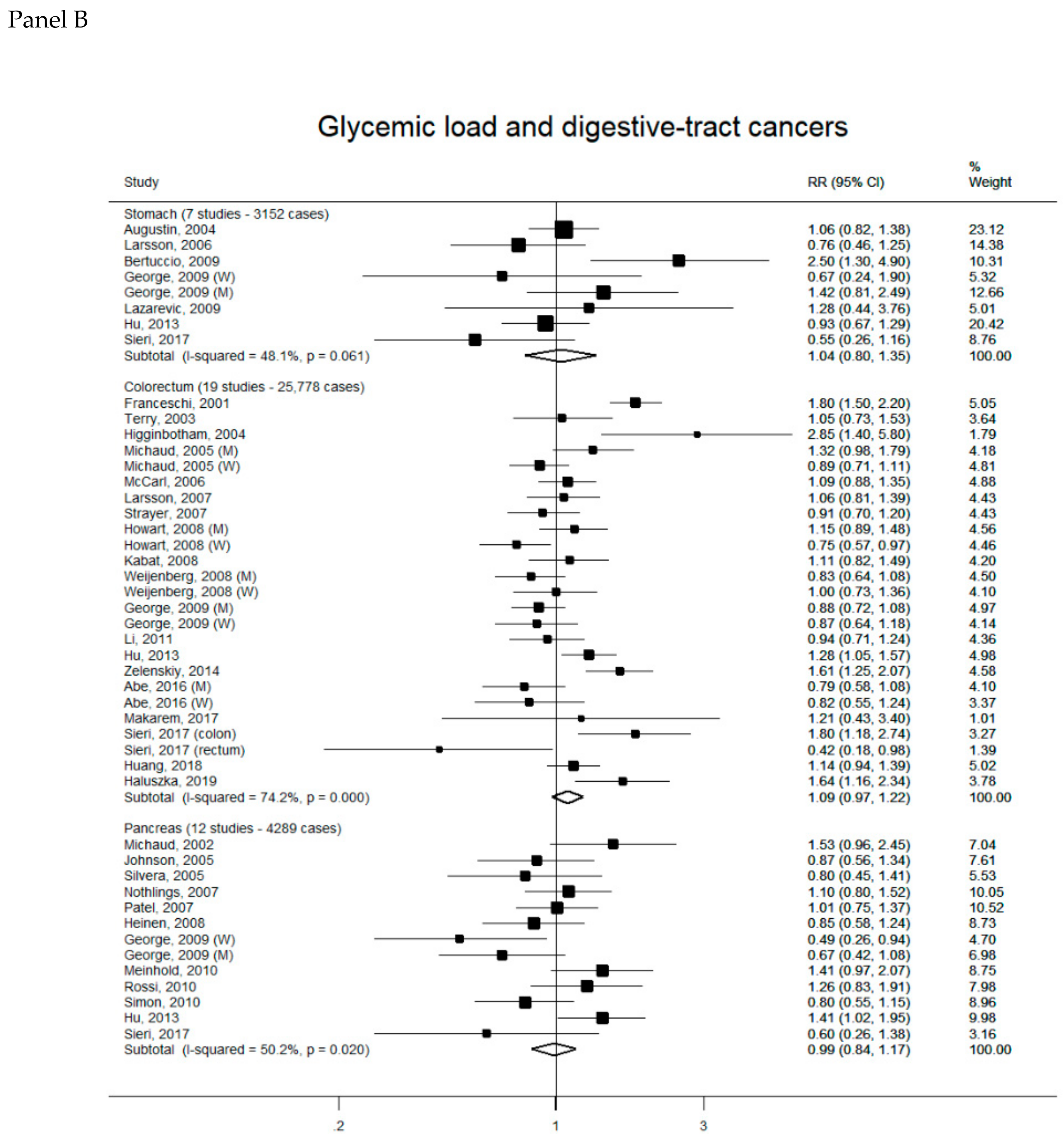
3.2.2. Digestive-Tract Cancers
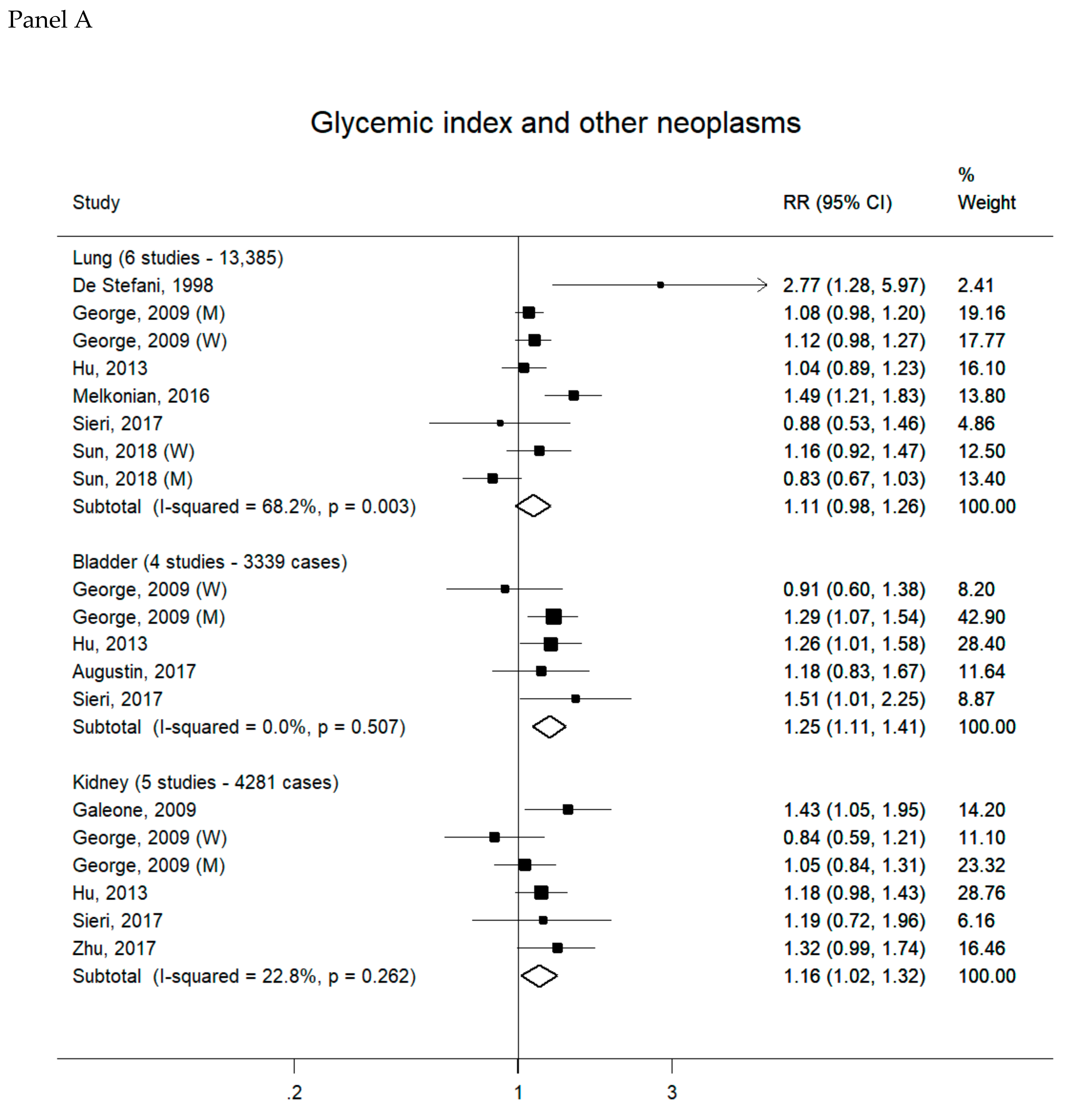
3.2.3. Other Neoplasms
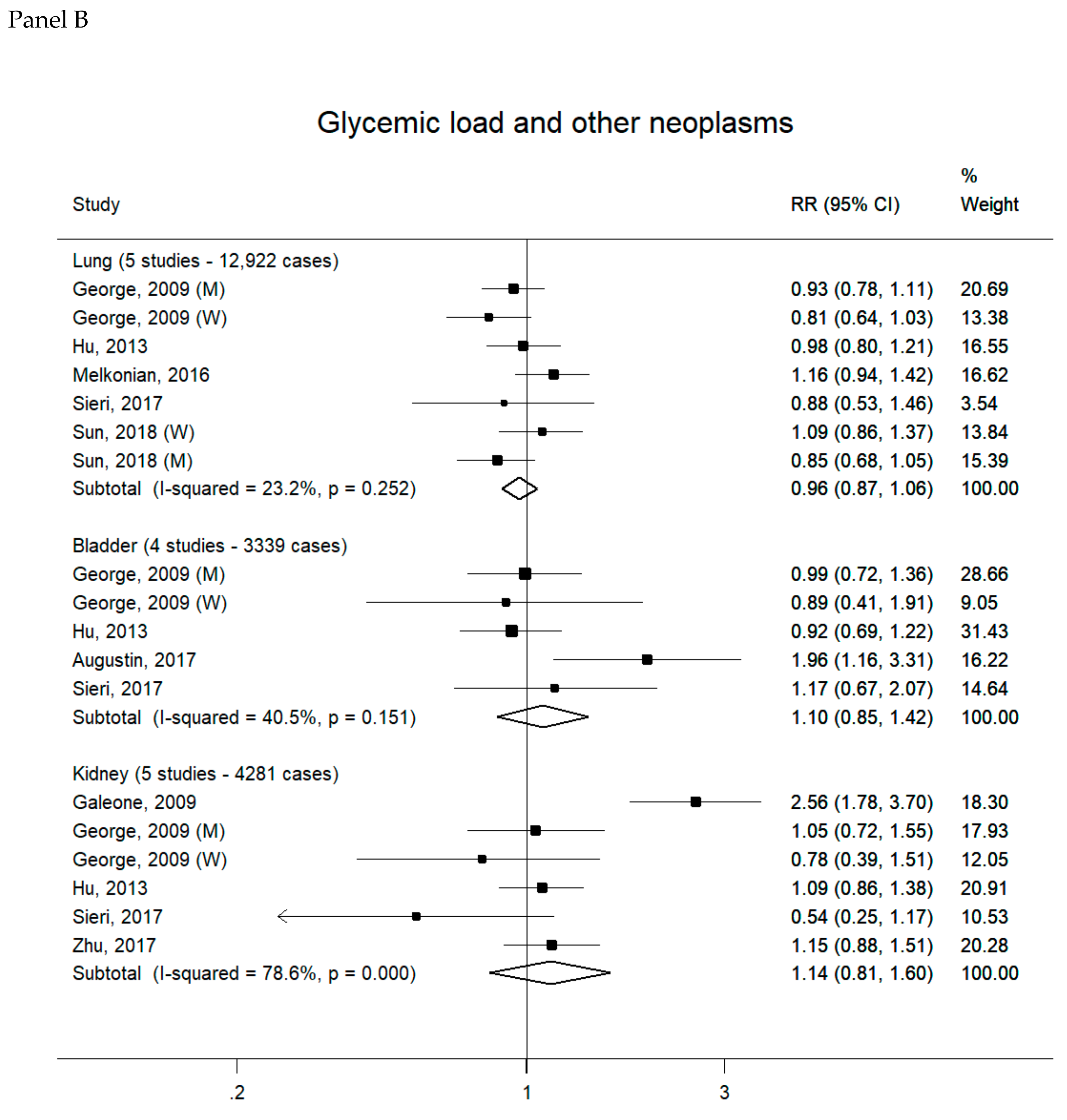
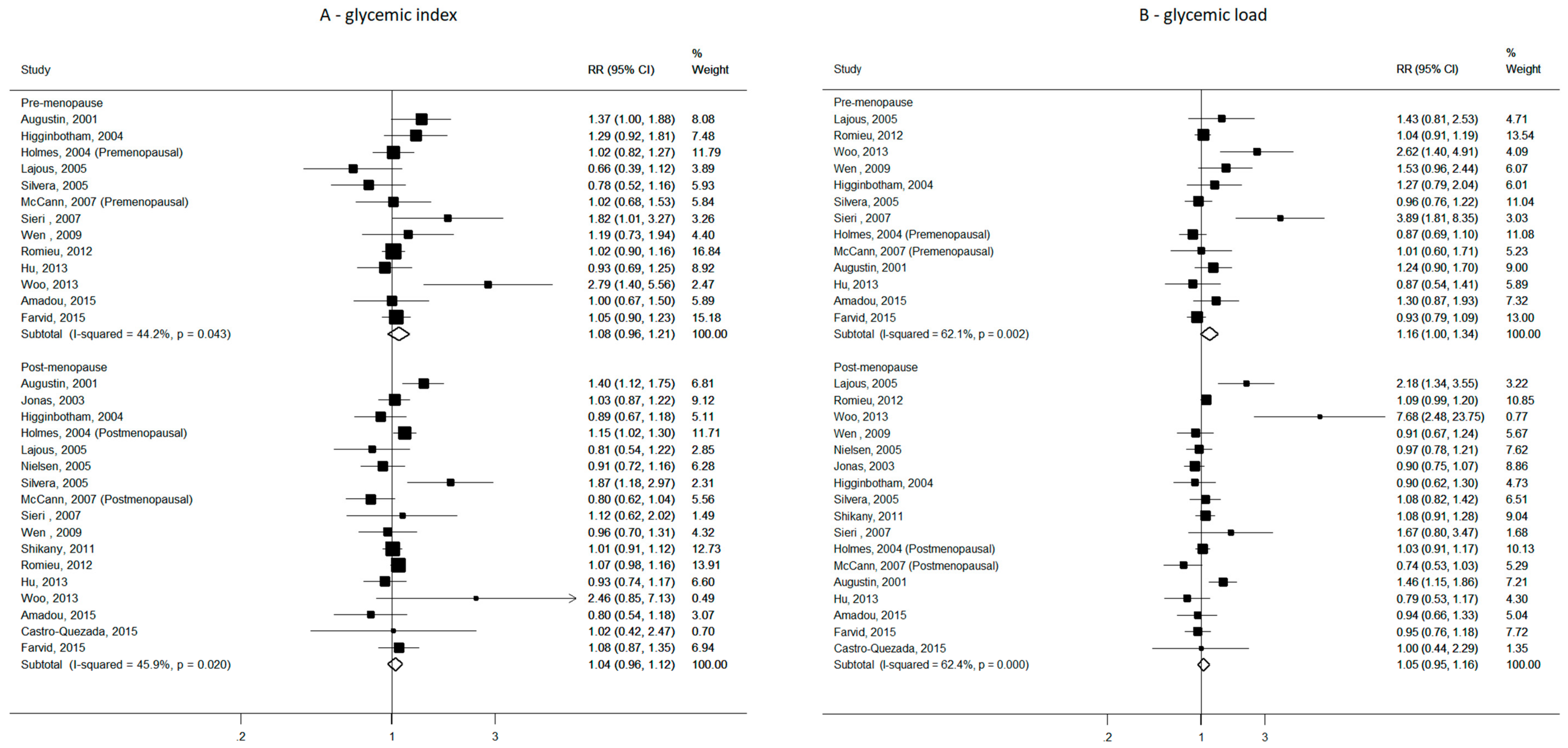
3.2.4. Subgroup Analyses for Breast Cancer
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jenkins, D.J.; Wolever, T.M.; Taylor, R.H.; Barker, H.; Fielden, H.; Baldwin, J.M.; Bowling, A.C.; Newman, H.C.; Jenkins, A.L.; Goff, D.V. Glycemic index of foods: A physiological basis for carbohydrate exchange. Am. J. Clin. Nutr. 1981, 34, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, F.S.; Foster-Powell, K.; Brand-Miller, J.C. International tables of glycemic index and glycemic load values: 2008. Diabetes Care 2008, 31, 2281–2283. [Google Scholar] [CrossRef] [PubMed]
- Augustin, L.S.; Kendall, C.W.; Jenkins, D.J.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Bjorck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An international scientific consensus summit from the international carbohydrate quality consortium (icqc). Nutr. Metab. Cardiovasc. Dis. 2015, 25, 795–815. [Google Scholar] [CrossRef] [PubMed]
- Brand-Miller, J.C. Glycemic load and chronic disease. Nutr. Rev. 2003, 61, S49–S55. [Google Scholar] [CrossRef] [PubMed]
- Augustin, L.S.; Franceschi, S.; Jenkins, D.J.; Kendall, C.W.; La Vecchia, C. Glycemic index in chronic disease: A review. Eur. J. Clin. Nutr. 2002, 56, 1049–1071. [Google Scholar] [CrossRef] [PubMed]
- Sieri, S.; Krogh, V. Dietary glycemic index, glycemic load and cancer: An overview of the literature. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 18–31. [Google Scholar] [CrossRef]
- Reynolds, A.; Mann, J.; Cummings, J.; Winter, N.; Mete, E.; Te Morenga, L. Carbohydrate quality and human health: A series of systematic reviews and meta-analyses. Lancet 2019, 393, 434–445. [Google Scholar] [CrossRef]
- Kaaks, R.; Lukanova, A. Energy balance and cancer: The role of insulin and insulin-like growth factor-i. Proc. Nutr. Soc. 2001, 60, 91–106. [Google Scholar] [CrossRef]
- Renehan, A.G.; Zwahlen, M.; Minder, C.; O’Dwyer, S.T.; Shalet, S.M.; Egger, M. Insulin-like growth factor (igf)-i, igf binding protein-3, and cancer risk: Systematic review and meta-regression analysis. Lancet 2004, 363, 1346–1353. [Google Scholar] [CrossRef]
- Jee, S.H.; Ohrr, H.; Sull, J.W.; Yun, J.E.; Ji, M.; Samet, J.M. Fasting serum glucose level and cancer risk in korean men and women. JAMA 2005, 293, 194–202. [Google Scholar] [CrossRef]
- Lauby-Secretan, B.; Scoccianti, C.; Loomis, D.; Grosse, Y.; Bianchini, F.; Straif, K. Body fatness and cancer—Viewpoint of the iarc working group. N. Engl. J. Med. 2016, 375, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Rosato, V.; Polesel, J.; Levi, F.; Talamini, R.; Montella, M.; Negri, E.; Tavani, A.; Zucchetto, A.; Franceschi, S.; et al. Diabetes mellitus and cancer risk in a network of case-control studies. Nutr. Cancer 2012, 64, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Turati, F.; Galeone, C.; Gandini, S.; Augustin, L.S.; Jenkins, D.J.; Pelucchi, C.; La Vecchia, C. High glycemic index and glycemic load are associated with moderately increased cancer risk. Mol. Nutr. Food Res. 2015, 59, 1384–1394. [Google Scholar] [CrossRef] [PubMed]
- Castro-Quezada, I.; Sanchez-Villegas, A.; Martinez-Gonzalez, M.A.; Salas-Salvado, J.; Corella, D.; Estruch, R.; Schroder, H.; Alvarez-Perez, J.; Ruiz-Lopez, M.D.; Artacho, R.; et al. Glycemic index, glycemic load and invasive breast cancer incidence in postmenopausal women: The predimed study. Eur. J. Cancer Prev. 2016, 25, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Amadou, A.; Degoul, J.; Hainaut, P.; Chajes, V.; Biessy, C.; Torres Mejia, G.; Huybrechts, I.; Moreno Macia, H.; Ortega, C.; Angeles-Llerenas, A.; et al. Dietary carbohydrate, glycemic index, glycemic load, and breast cancer risk among mexican women. Epidemiology 2015, 26, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Farvid, M.S.; Eliassen, A.H.; Cho, E.; Chen, W.Y.; Willett, W.C. Adolescent and early adulthood dietary carbohydrate quantity and quality in relation to breast cancer risk. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1111–1120. [Google Scholar] [CrossRef] [PubMed]
- Abe, S.K.; Inoue, M.; Sawada, N.; Ishihara, J.; Iwasaki, M.; Yamaji, T.; Shimazu, T.; Sasazuki, S.; Tsugane, S. Glycemic index and glycemic load and risk of colorectal cancer: A population-based cohort study (jphc study). Cancer Causes Control 2016, 27, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Ros, R.; Rinaldi, S.; Tsilidis, K.K.; Weiderpass, E.; Boutron-Ruault, M.C.; Rostgaard-Hansen, A.L.; Tjonneland, A.; Clavel-Chapelon, F.; Mesrine, S.; Katzke, V.A.; et al. Energy and macronutrient intake and risk of differentiated thyroid carcinoma in the european prospective investigation into cancer and nutrition study. Int. J. Cancer 2016, 138, 65–73. [Google Scholar] [CrossRef][Green Version]
- Larsson, S.C.; Giovannucci, E.L.; Wolk, A. Prospective study of glycemic load, glycemic index, and carbohydrate intake in relation to risk of biliary tract cancer. Am. J. Gastroenterol. 2016, 111, 891–896. [Google Scholar] [CrossRef]
- Brenner, D.R.; Speidel, T.; Csizmadi, I.; Biel, R.K.; Cook, L.S.; Courneya, K.S.; Friedenreich, C.M. Glycemic load and endometrial cancer risk in a case-control study of canadian women. Cancer Epidemiol. 2015, 39, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Qin, B.; Moorman, P.G.; Alberg, A.J.; Barnholtz-Sloan, J.S.; Bondy, M.; Cote, M.L.; Funkhouser, E.; Peters, E.S.; Schwartz, A.G.; Terry, P.; et al. Dietary carbohydrate intake, glycaemic load, glycaemic index and ovarian cancer risk in african-american women. Br. J. Nutr. 2016, 115, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Melkonian, S.C.; Daniel, C.R.; Ye, Y.; Pierzynski, J.A.; Roth, J.A.; Wu, X. Glycemic index, glycemic load, and lung cancer risk in non-hispanic whites. Cancer Epidemiol. Biomark. Prev. 2016, 25, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Malavolti, M.; Malagoli, C.; Crespi, C.M.; Brighenti, F.; Agnoli, C.; Sieri, S.; Krogh, V.; Fiorentini, C.; Farnetani, F.; Longo, C.; et al. Glycaemic index, glycaemic load and risk of cutaneous melanoma in a population-based, case-control study. Br. J. Nutr. 2017, 117, 432–438. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, N.; Petrick, J.L.; Steck, S.E.; Bradshaw, P.T.; McClain, K.M.; Niehoff, N.M.; Engel, L.S.; Shaheen, N.J.; Risch, H.A.; Vaughan, T.L.; et al. A pooled analysis of dietary sugar/carbohydrate intake and esophageal and gastric cardia adenocarcinoma incidence and survival in the USA. Int. J. Epidemiol. 2017, 46, 1836–1846. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.W.; Zheng, W.; Li, H.L.; Gao, J.; Yang, G.; Gao, Y.T.; Rothman, N.; Lan, Q.; Shu, X.O.; Xiang, Y.B. Dietary glycemic load, glycemic index, and carbohydrate intake on the risk of lung cancer among men and women in shanghai. Nutr. Cancer 2018, 70, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Sieri, S.; Agnoli, C.; Pala, V.; Grioni, S.; Brighenti, F.; Pellegrini, N.; Masala, G.; Palli, D.; Mattiello, A.; Panico, S.; et al. Dietary glycemic index, glycemic load, and cancer risk: Results from the epic-italy study. Sci. Rep. 2017, 7, 9757. [Google Scholar] [CrossRef]
- Zhu, J.; Tu, H.; Matin, S.F.; Tannir, N.M.; Wood, C.G.; Wu, X. Glycemic index, glycemic load and carbohydrate intake in association with risk of renal cell carcinoma. Carcinogenesis 2017, 38, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Augustin, L.S.A.; Taborelli, M.; Montella, M.; Libra, M.; La Vecchia, C.; Tavani, A.; Crispo, A.; Grimaldi, M.; Facchini, G.; Jenkins, D.J.A.; et al. Associations of dietary carbohydrates, glycaemic index and glycaemic load with risk of bladder cancer: A case-control study. Br. J. Nutr. 2017, 118, 722–729. [Google Scholar] [CrossRef]
- Makarem, N.; Bandera, E.V.; Lin, Y.; Jacques, P.F.; Hayes, R.B.; Parekh, N. Carbohydrate nutrition and risk of adiposity-related cancers: Results from the framingham offspring cohort (1991–2013). Br. J. Nutr. 2017, 117, 1603–1614. [Google Scholar] [CrossRef]
- Haluszka, E.; Davila, V.L.; Aballay, L.R.; Del Pilar Diaz, M.; Osella, A.R.; Niclis, C. Association of the glycaemic index and the glycaemic load with colorectal cancer in the population of cordoba (argentina): Results of a case-control study using a multilevel modelling approach. Br. J. Nutr. 2019. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Fang, Y.J.; Xu, M.; Luo, H.; Zhang, N.Q.; Huang, W.Q.; Pan, Z.Z.; Chen, Y.M.; Zhang, C.X. Carbohydrate, dietary glycaemic index and glycaemic load, and colorectal cancer risk: A case-control study in china. Br. J. Nutr. 2018, 119, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Guerrero, C.H.; Gamboa-Loira, B.; Merida-Ortega, A.; Lopez-Carrillo, L. Dietary glycemic index and glycemic load and risk of breast cancer by molecular subtype in mexican women. Nutr. Cancer 2019. [Google Scholar] [CrossRef] [PubMed]
- Hartman, T.J.; McCullough, M.L.; Hodge, J.M.; Gaudet, M.M.; Wang, Y.; Gapstur, S.M. Dietary energy density, glycemic load, glycemic index, and risk for endometrial cancer in the cps-ii nutrition cohort. Cancer Epidemiol. Biomark. Prev. 2018, 27, 113–115. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, S.; Chan, D.S.M.; Vingeliene, S.; Vieira, A.R.; Abar, L.; Polemiti, E.; Stevens, C.A.T.; Greenwood, D.C.; Aune, D.; Norat, T. Carbohydrates, glycemic index, glycemic load, and breast cancer risk: A systematic review and dose-response meta-analysis of prospective studies. Nutr. Rev. 2017, 75, 420–441. [Google Scholar] [CrossRef] [PubMed]
- Mullie, P.; Koechlin, A.; Boniol, M.; Autier, P.; Boyle, P. Relation between breast cancer and high glycemic index or glycemic load: A meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 2016, 56, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zhu, Y.; Li, J.; Wang, S. Dietary fiber, glycemic index, glycemic load, and renal cell carcinoma risk. Carcinogenesis 2019, 40, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Wu, Y.; Xu, J.; Ding, K.; Shan, X.; Xia, D. Association between dietary carbohydrate intake, glycemic index and glycemic load, and risk of gastric cancer. Eur. J. Nutr. 2017, 56, 1169–1177. [Google Scholar] [CrossRef]
- Wang, R.J.; Tang, J.E.; Chen, Y.; Gao, J.G. Dietary fiber, whole grains, carbohydrate, glycemic index, and glycemic load in relation to risk of prostate cancer. Onco Targets Ther. 2015, 8, 2415–2426. [Google Scholar]
- Sadeghi, A.; Sadeghi, O.; Khodadost, M.; Pirouzi, A.; Hosseini, B.; Saedisomeolia, A. Dietary glycemic index and glycemic load and the risk of prostate cancer: An updated systematic review and dose-response meta-analysis. Nutr. Cancer 2019. [Google Scholar] [CrossRef]
- Willett, W.C.; Liu, S. Carbohydrate quality and health: Distilling simple truths from complexity. Am. J. Clin. Nutr. 2019, 110, 803–804. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Nagata, C.; Wada, K.; Tsuji, M.; Kawachi, T.; Nakamura, K. Dietary glycaemic index and glycaemic load in relation to all-cause and cause-specific mortality in a japanese community: The takayama study. Br. J. Nutr. 2014, 112, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Giles, G.G.; Simpson, J.A.; English, D.R.; Hodge, A.M.; Gertig, D.M.; Macinnis, R.J.; Hopper, J.L. Dietary carbohydrate, fibre, glycaemic index, glycaemic load and the risk of postmenopausal breast cancer. Int. J. Cancer 2006, 118, 1843–1847. [Google Scholar] [CrossRef] [PubMed]
- Fedirko, V.; Lukanova, A.; Bamia, C.; Trichopolou, A.; Trepo, E.; Nothlings, U.; Schlesinger, S.; Aleksandrova, K.; Boffetta, P.; Tjonneland, A.; et al. Glycemic index, glycemic load, dietary carbohydrate, and dietary fiber intake and risk of liver and biliary tract cancers in western europeans. Ann. Oncol. 2013, 24, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. Quantitative methods in the review of epidemiologic literature. Epidemiol. Rev. 1987, 9, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.; Spiegelman, D.; Hunter, D.J.; Chen, W.Y.; Colditz, G.A.; Willett, W.C. Premenopausal dietary carbohydrate, glycemic index, glycemic load, and fiber in relation to risk of breast cancer. Cancer Epidemiol. Biomark. Prev. 2003, 12, 1153–1158. [Google Scholar]
- Sieri, S.; Krogh, V.; Agnoli, C.; Ricceri, F.; Palli, D.; Masala, G.; Panico, S.; Mattiello, A.; Tumino, R.; Giurdanella, M.C.; et al. Dietary glycemic index and glycemic load and risk of colorectal cancer: Results from the epic-italy study. Int. J. Cancer 2015, 136, 2923–2931. [Google Scholar] [CrossRef] [PubMed]
- Romieu, I.; Ferrari, P.; Rinaldi, S.; Slimani, N.; Jenab, M.; Olsen, A.; Tjonneland, A.; Overvad, K.; Boutron-Ruault, M.C.; Lajous, M.; et al. Dietary glycemic index and glycemic load and breast cancer risk in the european prospective investigation into cancer and nutrition (epic). Am. J. Clin. Nutr. 2012, 96, 345–355. [Google Scholar] [CrossRef]
- Cust, A.E.; Slimani, N.; Kaaks, R.; van Bakel, M.; Biessy, C.; Ferrari, P.; Laville, M.; Tjonneland, A.; Olsen, A.; Overvad, K.; et al. Dietary carbohydrates, glycemic index, glycemic load, and endometrial cancer risk within the european prospective investigation into cancer and nutrition cohort. Am. J. Epidemiol. 2007, 166, 912–923. [Google Scholar] [CrossRef] [PubMed]
- King, M.G.; Olson, S.H.; Paddock, L.; Chandran, U.; Demissie, K.; Lu, S.E.; Parekh, N.; Rodriguez-Rodriguez, L.; Bandera, E.V. Sugary food and beverage consumption and epithelial ovarian cancer risk: A population-based case-control study. BMC Cancer 2013, 13, 94. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Mayne, S.T.; Leitzmann, M.F.; Park, Y.; Schatzkin, A.; Flood, A.; Hollenbeck, A.; Subar, A.F. Dietary glycemic index, glycemic load, and risk of cancer: A prospective cohort study. Am. J. Epidemiol. 2009, 169, 462–472. [Google Scholar] [CrossRef] [PubMed]
- La Vecchia, C.; Chatenoud, L.; Negri, E.; Franceschi, S. Session: Whole cereal grains, fibre and human cancer wholegrain cereals and cancer in italy. Proc. Nutr. Soc. 2003, 62, 45–49. [Google Scholar] [CrossRef]
- Kawakita, D.; Lee, Y.A.; Gren, L.H.; Buys, S.S.; La Vecchia, C.; Hashibe, M. Fiber intake and the risk of head and neck cancer in the prostate, lung, colorectal and ovarian (plco) cohort. Int. J. Cancer 2019, 145, 2342–2348. [Google Scholar] [CrossRef]
- Aune, D.; Chan, D.S.; Vieira, A.R.; Navarro Rosenblatt, D.A.; Vieira, R.; Greenwood, D.C.; Cade, J.E.; Burley, V.J.; Norat, T. Dietary fructose, carbohydrates, glycemic indices and pancreatic cancer risk: A systematic review and meta-analysis of cohort studies. Ann. Oncol. 2012, 23, 2536–2546. [Google Scholar] [CrossRef]
- Choi, Y.; Giovannucci, E.; Lee, J.E. Glycaemic index and glycaemic load in relation to risk of diabetes-related cancers: A meta-analysis. Br. J. Nutr. 2012, 108, 1934–1947. [Google Scholar] [CrossRef]
- Gnagnarella, P.; Gandini, S.; La Vecchia, C.; Maisonneuve, P. Glycemic index, glycemic load, and cancer risk: A meta-analysis. Am. J. Clin Nutr. 2008, 87, 1793–1801. [Google Scholar] [CrossRef]
- World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective; Continuous Update Project Expert Report; World Cancer Research Fund/American Institute for Cancer Research: Washington, DC, USA, 2018. [Google Scholar]
- Galeone, C.; Augustin, L.S.; Filomeno, M.; Malerba, S.; Zucchetto, A.; Pelucchi, C.; Montella, M.; Talamini, R.; Franceschi, S.; La Vecchia, C. Dietary glycemic index, glycemic load, and the risk of endometrial cancer: A case-control study and meta-analysis. Eur. J. Cancer Prev. 2013, 22, 38–45. [Google Scholar] [CrossRef]
- Nagle, C.M.; Olsen, C.M.; Ibiebele, T.I.; Spurdle, A.B.; Webb, P.M. Glycemic index, glycemic load and endometrial cancer risk: Results from the australian national endometrial cancer study and an updated systematic review and meta-analysis. Eur. J. Nutr. 2013, 52, 705–715. [Google Scholar] [CrossRef]
- Aune, D.; Chan, D.S.; Lau, R.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Carbohydrates, glycemic index, glycemic load, and colorectal cancer risk: A systematic review and meta-analysis of cohort studies. Cancer Causes Control 2012, 23, 521–535. [Google Scholar] [CrossRef] [PubMed]
- Galeone, C.; Pelucchi, C.; La Vecchia, C. Added sugar, glycemic index and load in colon cancer risk. Curr. Opin. Clin. Nutr. Metab. Care 2012, 15, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, H.G.; Murray, L.J.; Cardwell, C.R.; Cantwell, M.M. Glycemic index, glycemic load, and risk of digestive tract neoplasms: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2009, 89, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, H.G.; Murray, L.J.; Cardwell, C.R.; Cantwell, M.M. Dietary glycaemic index, glycaemic load and breast cancer risk: A systematic review and meta-analysis. Br. J. Cancer 2008, 99, 1170–1175. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.Y.; Qin, L.Q. Dietary glycemic index, glycemic load, and risk of breast cancer: Meta-analysis of prospective cohort studies. Breast Cancer Res. Treat. 2011, 126, 287–294. [Google Scholar] [CrossRef]
- Esposito, K.; Chiodini, P.; Colao, A.; Lenzi, A.; Giugliano, D. Metabolic syndrome and risk of cancer: A systematic review and meta-analysis. Diabetes Care 2012, 35, 2402–2411. [Google Scholar] [CrossRef]
- Brown, J.S.; Wessells, H.; Chancellor, M.B.; Howards, S.S.; Stamm, W.E.; Stapleton, A.E.; Steers, W.D.; Van Den Eeden, S.K.; McVary, K.T. Urologic complications of diabetes. Diabetes Care 2005, 28, 177–185. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Lin, T.; Fan, X.; Liang, Y.; Heemann, U. High dose human insulin and insulin glargine promote t24 bladder cancer cell proliferation via pi3k-independent activation of akt. Diabetes Res. Clin. Pract. 2011, 91, 177–182. [Google Scholar] [CrossRef]
- Ornskov, D.; Nexo, E.; Sorensen, B.S. Insulin-induced proliferation of bladder cancer cells is mediated through activation of the epidermal growth factor system. FEBS J. 2006, 273, 5479–5489. [Google Scholar] [CrossRef]
- Murakami, K.; McCaffrey, T.A.; Livingstone, M.B. Associations of dietary glycaemic index and glycaemic load with food and nutrient intake and general and central obesity in british adults. Br. J. Nutr. 2013, 110, 2047–2057. [Google Scholar] [CrossRef]
- Du, H.; van der, A.D.; van Bakel, M.M.; van der Kallen, C.J.; Blaak, E.E.; van Greevenbroek, M.M.; Jansen, E.H.; Nijpels, G.; Stehouwer, C.D.; Dekker, J.M.; et al. Glycemic index and glycemic load in relation to food and nutrient intake and metabolic risk factors in a dutch population. Am. J. Clin. Nutr. 2008, 87, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Mendez, M.A.; Covas, M.I.; Marrugat, J.; Vila, J.; Schroder, H. Glycemic load, glycemic index, and body mass index in spanish adults. Am. J. Clin. Nutr. 2009, 89, 316–322. [Google Scholar] [PubMed]
- Schulz, M.; Liese, A.D.; Mayer-Davis, E.J.; D’Agostino, R.B., Jr.; Fang, F.; Sparks, K.C.; Wolever, T.M. Nutritional correlates of dietary glycaemic index: New aspects from a population perspective. Br. J. Nutr. 2005, 94, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Favero, A.; Salvini, S.; Russo, A.; Parpinel, M.; Negri, E.; Decarli, A.; La Vecchia, C.; Giacosa, A.; Franceschi, S. Sources of macro- and micronutrients in italian women: Results from a food frequency questionnaire for cancer studies. Eur. J. Cancer Prev. 1997, 6, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Slimani, N.; Fahey, M.; Welch, A.A.; Wirfalt, E.; Stripp, C.; Bergstrom, E.; Linseisen, J.; Schulze, M.B.; Bamia, C.; Chloptsios, Y.; et al. Diversity of dietary patterns observed in the european prospective investigation into cancer and nutrition (epic) project. Public Health Nutr. 2002, 5, 1311–1328. [Google Scholar] [CrossRef]
- Wirfalt, E.; McTaggart, A.; Pala, V.; Gullberg, B.; Frasca, G.; Panico, S.; Bueno-de-Mesquita, H.B.; Peeters, P.H.; Engeset, D.; Skeie, G.; et al. Food sources of carbohydrates in a european cohort of adults. Public Health Nutr. 2002, 5, 1197–1215. [Google Scholar] [CrossRef]
- La Vecchia, C.; Giordano, S.H.; Hortobagyi, G.N.; Chabner, B. Overweight, obesity, diabetes, and risk of breast cancer: Interlocking pieces of the puzzle. Oncologist 2011, 16, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E.; Harlan, D.M.; Archer, M.C.; Bergenstal, R.M.; Gapstur, S.M.; Habel, L.A.; Pollak, M.; Regensteiner, J.G.; Yee, D. Diabetes and cancer: A consensus report. CA Cancer J. Clin. 2010, 60, 207–221. [Google Scholar] [CrossRef]
- Larsson, S.C.; Giovannucci, E.; Wolk, A. Dietary carbohydrate, glycemic index, and glycemic load in relation to risk of colorectal cancer in women. Am. J. Epidemiol. 2007, 165, 256–261. [Google Scholar] [CrossRef]
- Folsom, A.R.; Demissie, Z.; Harnack, L. Glycemic index, glycemic load, and incidence of endometrial cancer: The iowa women’s health study. Nutr. Cancer 2003, 46, 119–124. [Google Scholar] [CrossRef]
| Study^, Year (Sex) | Cancer Site | Study Design Study Area and Period of Enrolment or Follow-Up (Years) | Cases | Controls/Cohort size | Dietary Assessment Method; Reference Food for GI/GL | RR (95% CI) Comparison Level (Highest vs. Lowest) | Matching and Adjustment Factors | |
|---|---|---|---|---|---|---|---|---|
| Glycemic Index | Glycemic Load | |||||||
| Li 2017 [24] (M + W) US Multicenter Study (1) L.A. Multi-Ethnic study (2) | EA, GCA | CC, pb USA, in (1): 1993-1995 in (2): 1992-1997 | 500 EA 529 GCA | 2027 | in (1): Validated 104-items FFQ in (2): validated 124-items FFQ; not specified | EA OR: 1.58 (1.13–2.21) V vs. I study-specific quintile GCA OR: 1.21 (0.88–1.67) V vs. I study-specific quintile | EA OR: 0.81 (0.51–1.29) V vs. I study-specific quintile GCA OR: 0.86 (0.55–1.35) V vs. I study-specific quintile | Age, sex, study, fruit and vegetables, smoking, GERD, energy, BMI (only for GL) |
| Haluszka 2019 [30] (M + W) | CRC | CC, pb Argentina 2008-2016 | 161 | 331 | validated 127-items FFQ; white bread | OR: 1.08 (0.61–1.90) > 82.5 vs. <77.2 III vs. I tertile | OR: 1.64 (1.16–2.34) >298.7 vs. <200.4 III vs. I tertile | Age, sex, socio-economic status, urbanization, BMI, smoking, analgesic use, family history, |
| Huang 2018 [31] (M + W) | CRC | CC, hb and pb China, 2010-2017 | 1944 | 2027 (1168 hb, 859 pb) | validated 81-items FFQ; glucose | OR: 3.10 (2.51–3.85) >69.8 vs. <64.3 IV vs. I quartile | OR: 1.14 (0.94–1.39) >187.2 vs. <134.4 IV vs. I quartile | Age, sex, marital status, residence, education, occupation, income, smoking, passive smoking, alcohol, family history of cancer, occupational physical activity, household and leisure-time activities, energy |
| Abe 2016 [17] JPHC Study (M, W) | CRC | Cohort Japan, 1995/1999–2010 average FU: 12.5 years | 1468 | 73,501 pr 919,276 py | validated 128-items FFQ; not specified | RR, M: 0.92 (9.73–1.14) 65.77-78.46 vs. 28.12-59.10 IV vs. I quartile RR, W: 0.97 (0.73–1.30) 64.05-80.19 vs. 14.25-57.57 IV vs. I quartile | RR, M: 0.79 (0.58–1.08) IV vs. I quartile RR, W: 0.82 (0.55–1.24) IV vs. I quartile | Stratified by sex and adjusted for age, area, alcohol, smoking, BMI, MET, history of diabetes, colorectal screening, calcium, magnesium, vitamin B6, vitamin B12, folate, vitamin D, n-3 PUFA, fiber, red meat, and for women only, menopausal status and use of exogenous female hormones. |
| Larsson 2016 [19] SMC and CSM (M+W) | Biliary tract | Cohort Sweden, 1998–2012 mean FU: 13.3 years | 163 # | 76,014 pr 1,010,777 py | validated 96-items FFQ; white bread | Total extrahepatic BTC (n = 140): RR: 2.12 (1.25–3.58) Gallbladder (n = 77): RR: 1.58 (0.81–3.08) Intrahepatic BTC (n = 23) RR: 1.47 (0.54–3.97) IV (median: 88 in M and 80 in W) vs. I (median: 73 in M and 69 in W) quartile | Total extrahepatic BTC (n = 140): RR: 1.63 (1.01–2.63) Gallbladder (n = 77): RR: 2.14 (1.06–4.33) Intrahepatic BTC (n = 23) RR: 3.46 (1.22–9.84) M: >213 vs. <177 W: >202 vs. <166 IV vs. I (sex-specific) quartile | Age, sex, education, smoking, BMI, diabetes, energy |
| Sun 2018 [25] (M, W) SWHS and SMHS | Lung | Cohort Shanghai, 1997/2000–2013 in SWHS 2002/2006–2013 in SMHS average FU: 14.8 years in SWHS and 9.3 years in SMHS | 1312 (649 in SWHS and 663 in SMHS) | 130,852 pr 1.612,703 py | SWHS: validated 77-items FFQ SMHS: validated 81-items FFQ; not reported | RR, W (SWHS): 1.16 (0.92–1.47) IV (median 76.74) vs. I (median 63.63) quartile RR, M (SMHS): 0.83 (0.67–1.03) IV (median 77.02) vs. I (median 64.13) quartile | RR, W (SWHS): 1.09 (0.86–1.37) IV (median 144.8 g/1000 kcal/d) vs. I (median 97.72 g/1000 kcal/d) quartile RR, M (SMHS): 0.85 (0.68–1.05) IV (median 143.77 g/1000 kcal/d) vs. I (median 95.79 g/1000 kcal/d) quartile | Age, education, income, BMI, physical activity, energy, smoking, alcohol (men only), history of lung disease, hypertension, diabetes, family history of cancer, menopausal status (women only) |
| Melkonian 2016 [22] (M+W) | Lung | CC, hb USA, not reported | 1905 | 2413 | validated FFQ; glucose | OR: 1.49 (1.21–1.83) V vs. I (sex-specific) quintile | OR: 1.16 (0.94–1.42) V vs. I (sex-specific) quintile | Age, education, gender, smoking, history of emphysema, pneumonia, hay fever, family history of lung cancer, physical activity, BMI, energy |
| Malavolti 2017 [23] (M+W) | Melanoma | CC, pb Italy, 2005–2006 | 380 | 719 | validated 188-items FFQ; glucose | OR: 0.88 (0.55–1.42) V (median: 55.7) vs. I (median: 47.7) quintile | OR: 1.35 (0.80–2.27) V (median:149.7) vs. I (median: 92.0) quintile | Age, sex, residence, education, BMI, phototype, skin sensitivity to sun exposure, sunburns history, SFA, vitamin C, vitamin D, fiber, energy |
| Guerrero 2019 [32] (W) | Breast | CC, pb Mexico, 2007–2011 | 509 | 509 | validated 133-items FFQ; glucose | OR: 1.15 (1.09–1.23) each unit increment | OR: 1.00 (0.99–1.02) each unit increment | Age, education, energy, saturated fats, breastfeeding duration |
| Castro-Quezada 2016 [14] PREDIMED * (W) | Breast | Cohort Spain, 2003/2009–2010 median FU: 4.8 years | 32 | 4010 pr (postmenopausal W) 17,757 py | validated 137-items FFQ; glucose | RR: 1.02 (0.42–2.46) III (mean: 60.8) vs. I (mean: 50.8) tertile | RR: 1.00 (0.44–2.30) III (mean: 129.0) vs. I (mean: 82.2) tertile | Age, center, intervention group, smoking, education, physical activity, BMI, WHtR, family history of cancer, age at menopause, HRT use, statin use, energy, alcohol, dietary fiber, folate |
| Amadou 2015 [15] Cáncer de la Mamá study (W) | Breast | CC, pb Mexico, 2004–2007 | 1000 | 1074 | validated 104-items FFQ; glucose | OR: 0.90 (0.68–1.12) >52.5 vs. <46.8 IV vs. I quartile Premenopausal W: 1.0 (0.67–1.5) Postmenopausal W: 0.80 (0.55–1.2) | OR: 1.1 (0.82–1.1) >173 vs. <145.8 IV vs. I quartile Premenopausal W: 1.3 (0.86–1.9) Postmenopausal W: 0.94 (0.65–1.3) | Age, age at menarche, SES, breastfeeding, age at first pregnancy, family history of breast cancer, alcohol, physical activity, energy, native ancestry, BMI |
| Farvid 2015 [16] NHSII (W) | Breast | Cohort USA, 1991–2011 | 2833 | 90,534 pr 1,725,295 py | validated 128-items FFQ; glucose | RR: 1.03 (0.91–1.16) V (median: 57.9) vs. I (median: 49.7) quintile Premenopausal W RR: 1.05 (0.90–1.23) Postmenopausal W RR: 1.08 (0.87–1.35) | RR: 0.94 (0.83–1.06) V (median: 149) vs. I (median: 96) quintile Premenopausal W RR: 0.93 (0.79–1.09) Postmenopausal W RR: 0.95 (0.76–1.18) | Age, race, family history of breast cancer, history of BBD, smoking, height, BMI at 18 years, weight change since age 18 years, age at menarche, parity and age at first birth, OC use, alcohol, energy, menopausal status and age at menopause, postmenopausal hormone use. |
| Hartman 2018 [33] CPS-II Nutrition Cohort (W) | Endometrium | Cohort USA, 1999–2013 average FU: 13.6 years | 425 | 30,997 pr postmenopausal W 377,265 py | validated 152-items FFQ; not specified | RR: 0.98 (0.74–1.29) ≥54.48 vs. <50.43 IV vs. I quartile | RR: 0.83 (0.62–1.11) ≥126.82 vs. <100.47 IV vs. I quartile | Age, smoking, age at menarche, age at menopause, parity, HRT, OC, physical activity, BMI |
| Brenner 2015 [20] (W) | Endometrium | CC, pb Canada, 2002-2006 | 511 | 980 | adapted NCI DHQ (validated); not specified | Not provided | OR: 0.87 (0.52–1.46) >114.1 vs. ≤68.7 IV vs. I quartile | Age, parity, menopausal status, HRT, rural residence, weight, waist circumference, comorbidity (diabetes, hypertension, thrombosis, pulmonary embolism, myocardial infarction, angina pectoris, stroke, high cholesterol), fiber, energy |
| Qin 2016 [21] AACES (W) | Ovary | CC, pb USA, 2010–2014 | 406 | 609 | Block 2005 FFQ (110 items, validated); glucose | OR: 1.03 (0.70–1.50) ≥54.9 vs. ≤49.9 IV vs. I quartile | OR: 1.35 (0.93–1.97) ≥65.0 vs. ≤50.8 units/1000 kcal IV vs. I quartile | Age, education, region, energy, parity, OC use, menopausal status, tubal ligation, family history of breast/ovarian cancer |
| Augustin 2017 [28] (M+W) | Bladder | CC, hb Italy, 2003–2014 | 578 | 608 | validated 78-items FFQ; white bread | OR: 1.18 (0.83–1.67) >83 vs. <75 IV vs. I quartile | OR: 1.96 (1.16–3.31) ≥275 vs. <169 IV vs. I quartile | Age, sex, study center, education, smoking, alcohol, abdominal obesity, energy |
| Zhu 2017 [27] (M+W) | Kidney | CC, pb USA, 2002–2017 (ongoing) | 854 | 1255 | validated FFQ; glucose | OR: 1.32 (0.99–1.74) IV vs. I (sex-specific) quartile | OR: 1.15 (0.88–1.51) IV vs. I (sex-specific) quartile | Age, sex, education, BMI, physical activity, smoking, hypertension, family history, energy, HEI-2015 |
| Zamora-Ros 2016 [18] EPIC (M+W) | Thyroid | Cohort 10 European countries, 1992/2000–2006/2009 mean FU: 11 years | 556 | 477,274 pr 5,262,772 py | country-specific validated dietary questionnaires;glucose | RR: 0.94 (0.73–1.20) >58.5 vs. <53.6 IV vs. I (cohort-wide) quartile | RR: 0.95 (0.74–1.24) >69.6 vs. <54.4 unit/1000 kcal day IV vs. I (cohort-wide) quartile | Age, sex, center, BMI, smoking, education, physical activity, energy, alcohol, and for women only, menopausal status and type |
| Makarem 2017 [29] (M+W) Framingham Offspring cohort | Adiposity-related cancers | Cohort USA, 1991/1995-2013 | 565 adiposity-related cancers§ 124 breast 157 prostate 68 CRC | 3184 pr | validated 126-items FFQ; not specified | Adiposity-related cancers RR: 0.95 (0.73–1.24) >57.5 vs. <51.9 Breast RR: 0.90 (0.59–.37) >56.2 vs. <53.3 III vs. I tertile Prostate RR: 0.74 (0.48–1.12) >56.4 vs. <53.6 III vs. I tertile CRC RR: 1.51 (0.81–2.84) >56.3 vs. <53.5 III vs. I tertile | Adiposity-related cancers RR: 0.93 (0.58–1.49) >169.9 vs. <85.6 Breast RR: 0.54 (0.26–1.09) >136.0 vs. <96.7 g/d III vs. I tertile Prostate RR: 0.76 (0.40–1.43) >154.4 vs. <106.3 g/d III vs. I tertile CRC RR: 1.21 (0.43–3.40) >143.7 vs. <100.7 g/d III vs. I tertile | Age, sex, smoking, alcohol, energy Breast: additional adjustment for menopausal status, age at menopause, hormone therapy, n. of live births. CRC: additional adjustment for red and processed meat, fiber For breast, prostate and CRC: additional adjustment for education, BMI, waist circumference, physical activity, history of diabetes and CVD, and antioxidant supplements did not change the results. |
| Sieri 2017 [26] (M+W) EPIC-Italy | Various sites | Cohort Italy 1993/1998–2009/2010 median FU: 14.9 years | 5112 cancers | 45,148 pr | 3 validated FFQs; glucose | All cancers combined RR: 1.06 (0.97–1.16) V (mean: 57.4) vs. I (mean: 50.0) quintile The paper reported RRs of 20 different cancer sites | All cancers combined RR: 1.05 (0.93–1.20) V (mean: 235.2) vs. I (mean: 86.0) quintile The paper reported RRs of 20 different cancer sites | Age, sex, education, BMI, physical activity, smoking, FFQ, alcohol, non-alcohol energy, fiber, saturated fat |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turati, F.; Galeone, C.; Augustin, L.S.A.; La Vecchia, C. Glycemic Index, Glycemic Load and Cancer Risk: An Updated Meta-Analysis. Nutrients 2019, 11, 2342. https://doi.org/10.3390/nu11102342
Turati F, Galeone C, Augustin LSA, La Vecchia C. Glycemic Index, Glycemic Load and Cancer Risk: An Updated Meta-Analysis. Nutrients. 2019; 11(10):2342. https://doi.org/10.3390/nu11102342
Chicago/Turabian StyleTurati, Federica, Carlotta Galeone, Livia S. A. Augustin, and Carlo La Vecchia. 2019. "Glycemic Index, Glycemic Load and Cancer Risk: An Updated Meta-Analysis" Nutrients 11, no. 10: 2342. https://doi.org/10.3390/nu11102342
APA StyleTurati, F., Galeone, C., Augustin, L. S. A., & La Vecchia, C. (2019). Glycemic Index, Glycemic Load and Cancer Risk: An Updated Meta-Analysis. Nutrients, 11(10), 2342. https://doi.org/10.3390/nu11102342







