Dietary Patterns and Their Sociodemographic and Lifestyle Determinants in Switzerland: Results from the National Nutrition Survey menuCH
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Ethics
2.3. Dietary Assessment
2.4. Food Grouping
2.5. Identification of Dietary Patterns
2.6. Sociodemographic, Lifestyle and Anthropometric Variables
2.7. Determinants of Dietary Patterns
2.8. Weighting
2.9. Software and Packages
2.10. Reporting
3. Results
3.1. Population Characteristics
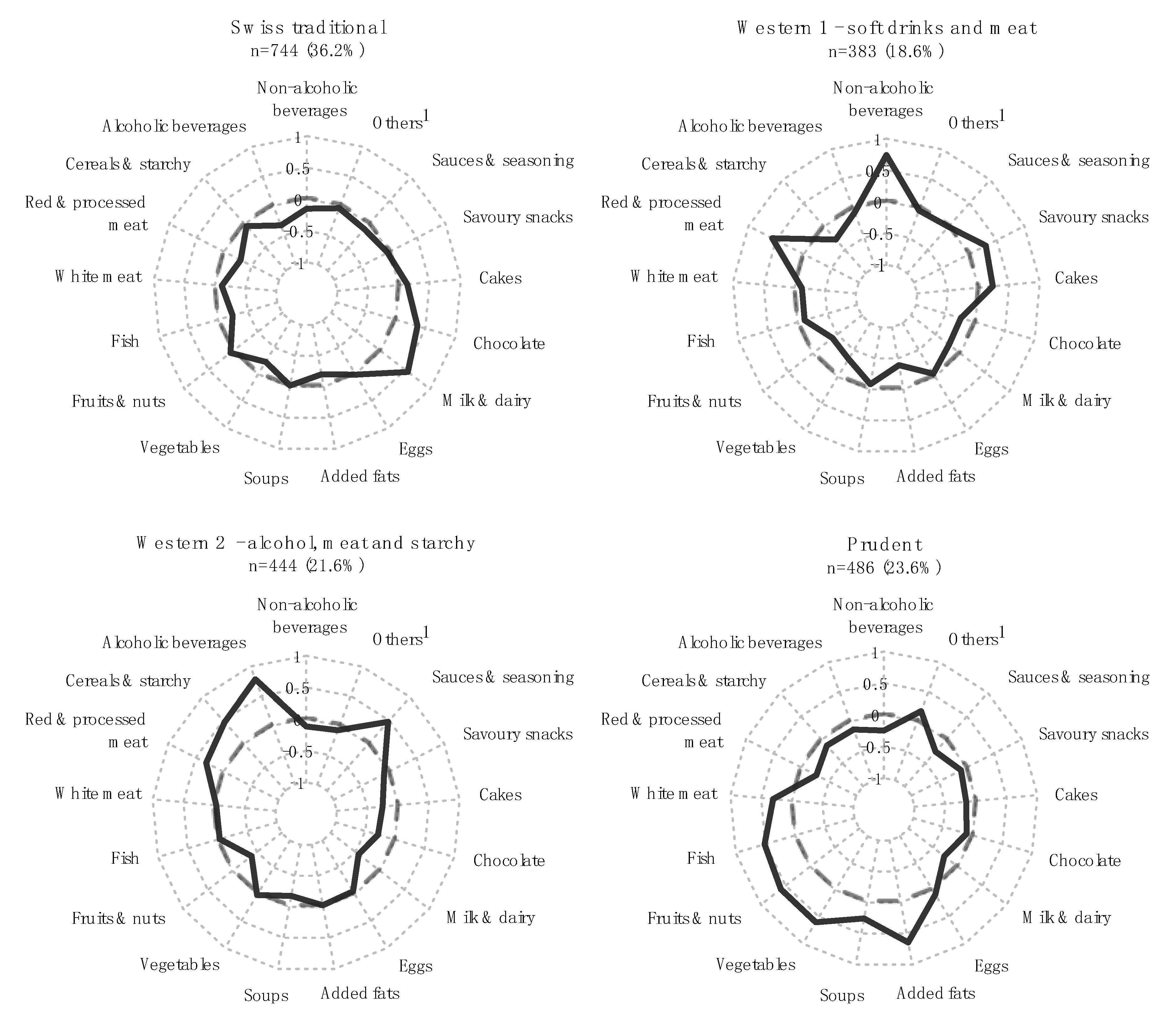
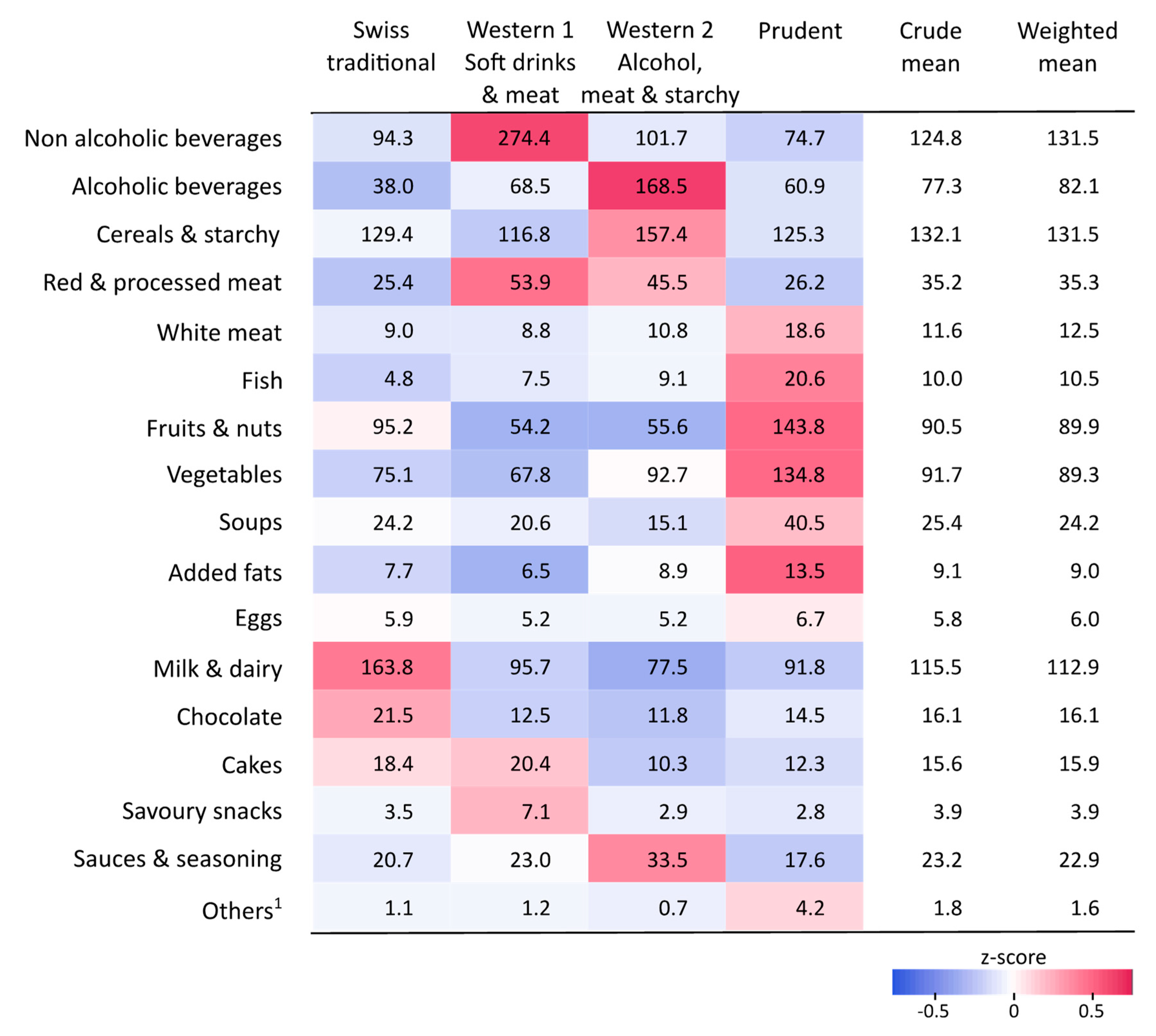
3.2. Dietary Patterns: Food Consumption
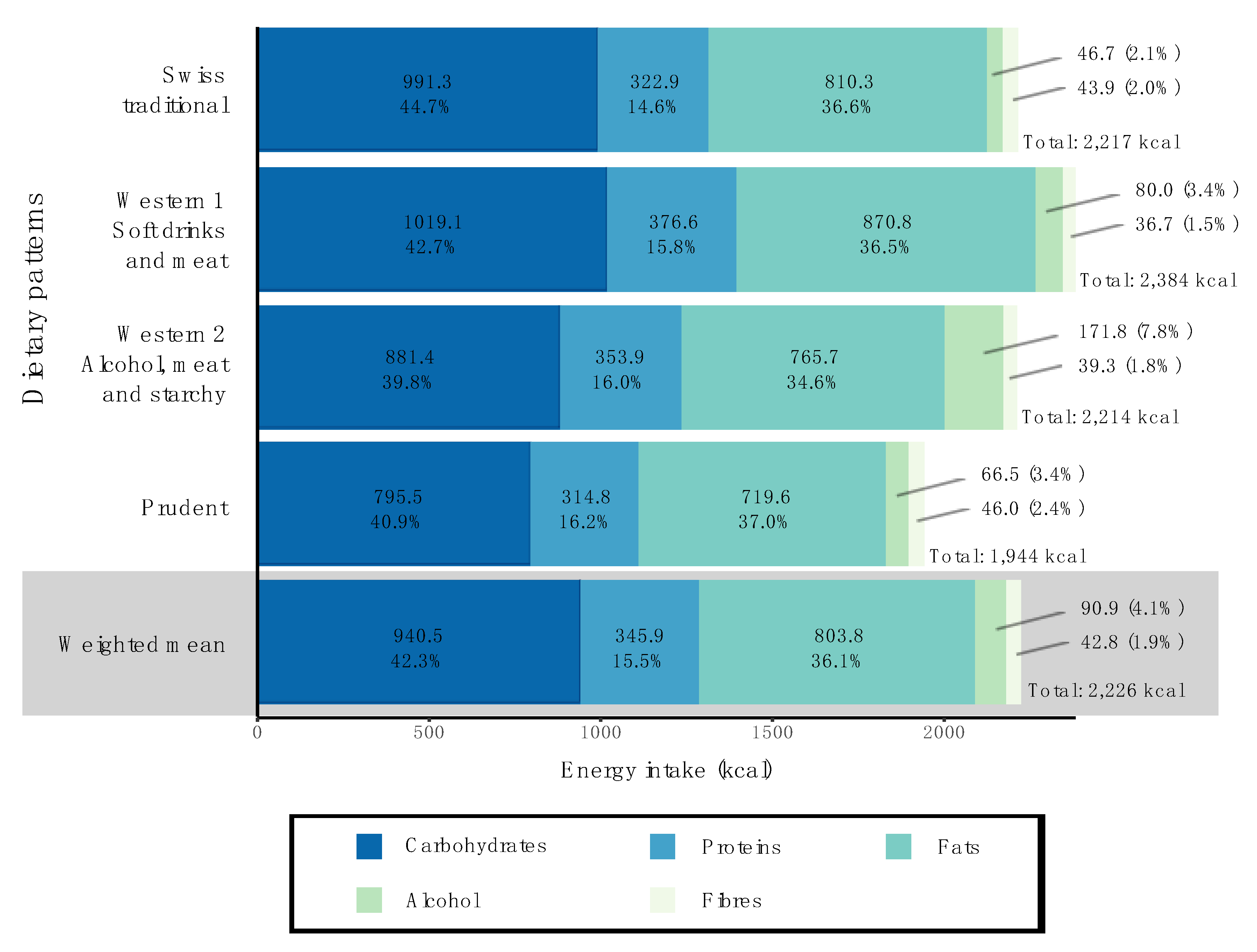
3.3. Dietary Patterns: Macronutrient Intake
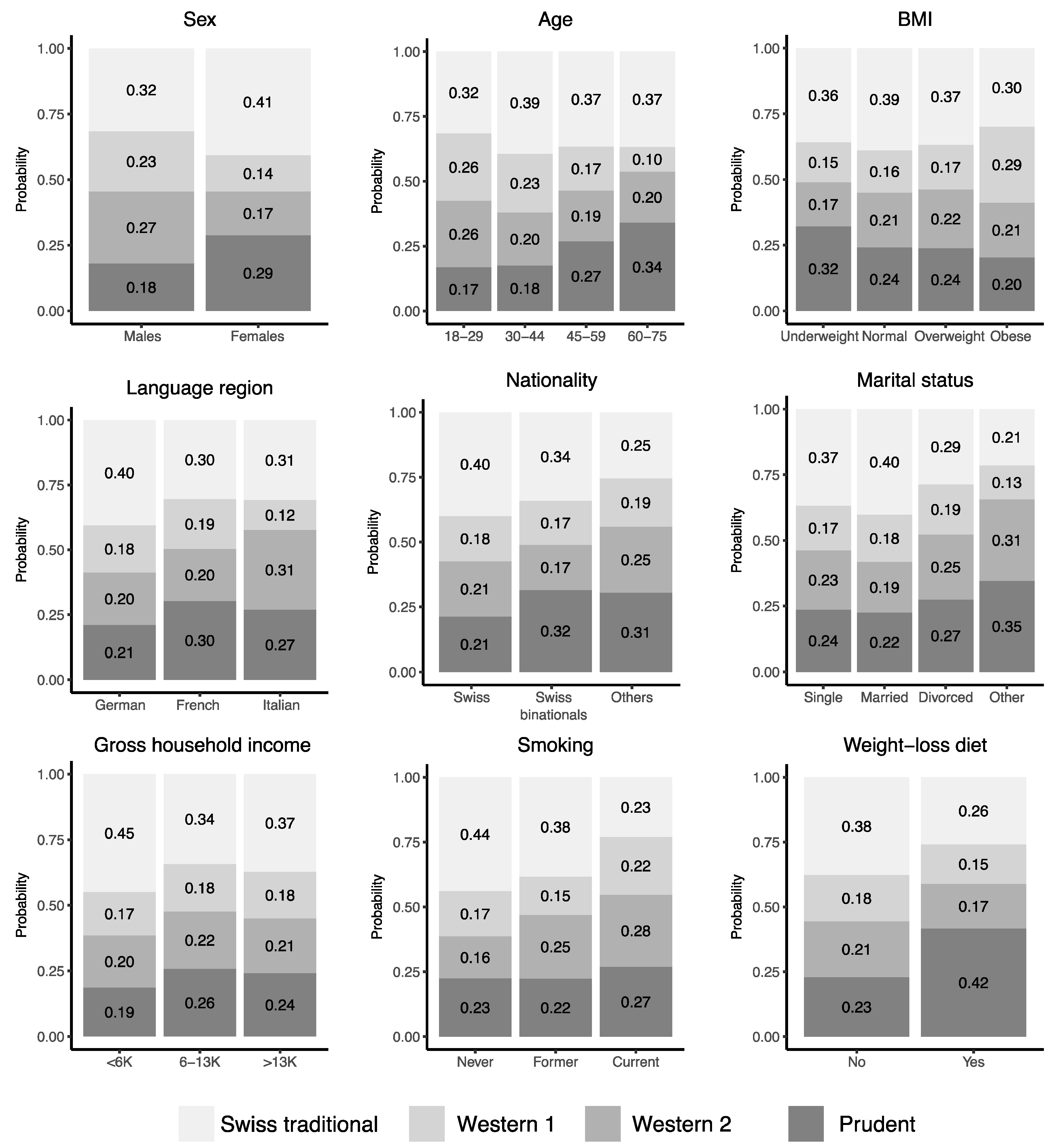
3.4. Sociodemographic and Lifestyle Determinants of Dietary Patterns
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Annex B: Tables of Health Statistics by Country, WHO Region and Globally. In World Health Statistics 2016: Monitoring Health for the SDGs; WHO Press: Geneva, Switzerland, 2016. [Google Scholar]
- Organisation for Economic Co-Operation and Development. Obesity and the Economics of Prevention: Fit Not Fat Key Facts—Switzerland, Update 2014; OECD Publishing: Paris, France, 2014. [Google Scholar]
- Swiss Health Observatory. Indicators. 2018. Available online: https://www.obsan.admin.ch/de/indikatoren (accessed on 12 February 2018).
- Chammartin, F.; Probst-Hensch, N.; Utzinger, J.; Vounatsou, P. Mortality atlas of the main causes of death in Switzerland, 2008–2012. Swiss. Med. Wkly. 2016, 146, w14280. [Google Scholar] [CrossRef] [PubMed]
- Faeh, D.; Minder, C.; Gutzwiller, F.; Bopp, M.; Swiss National Cohort Study Group. Culture, risk factors and mortality: Can Switzerland add missing pieces to the European puzzle? J. Epidemiol. Community Health 2009, 63, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Gazan, R.; Bechaux, C.; Crepet, A.; Sirot, V.; Drouillet-Pinard, P.; Dubuisson, C.; Havard, S. Dietary patterns in the French adult population: A study from the second French national cross-sectional dietary survey (INCA2) (2006-2007). Br. J. Nutr. 2016, 116, 300–315. [Google Scholar] [CrossRef] [PubMed]
- Naska, A.; Fouskakis, D.; Oikonomou, E.; Almeida, M.D.V.; Berg, M.A.; Gedrich, K.; Moreiras, O.; Nelson, M.; Trygg, K.; Turrini, A.; et al. Dietary patterns and their socio-demographic determinants in 10 European countries: Data from the DAFNE databank. Eur. J. Clin. Nutr. 2006, 60, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Villegas, A.; Delgado-Rodríguez, M.; Martínez-González, M.A.; De Irala-Estevez, J. for the SUN Group (Seguimiento Universidad de Navarra). Gender, age, socio-demographic and lifestyle factors associated with major dietary patterns in the Spanish Project SUN (Seguimiento Universidad de Navarra). Eur. J. Clin. Nutr. 2003, 57, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Swiss Confederation—Federal Office of Public Health and the Food Safety and Veterinary Office (2018) Swiss Nutrition Strategy. Available online: https://www.blv.admin.ch/blv/en/home/das-blv/strategien/schweizer-ernaehrungsstrategie.html (accessed on 12 February 2018).
- Storni, M.; Kaeser, M.; Lieberherr, R. Swiss Health Survey 2012—Overview; Federal Statistical Office: Neuchâtel, Switerland, 2013. [Google Scholar]
- De Mestral, C.; Khalatbari-Soltani, S.; Stringhini, S.; Marques-Vidal, P. Fifteen-year trends in the prevalence of barriers to healthy eating in a high-income country. Am. J. Clin. Nutr. 2017, 105, 660–668. [Google Scholar] [CrossRef] [PubMed]
- De Abreu, D.; Guessous, I.; Vaucher, J.; Preisig, M.; Waeber, G.; Vollenweider, P.; Marques-Vidal, P. Low compliance with dietary recommendations for food intake among adults. Clin. Nutr. 2013, 32, 783–788. [Google Scholar] [CrossRef] [PubMed]
- De Abreu, D.; Guessous, I.; Gaspoz, J.-M.; Marques-Vidal, P. Compliance with the Swiss Society for Nutrition’s Dietary Recommendations in the Population of Geneva, Switzerland: A 10-Year Trend Study (1999–2009). J. Acad. Nutr. Diet. 2014, 114, 774–780. [Google Scholar] [CrossRef]
- Chatelan, A.; Marques-Vidal, P.; Bucher, S.; Siegenthaler, S.; Metzger, N.; Zuberbuehler, C.; Camenzind-Frey, E.; Renggli, A.; Bochud, M.; Beer-Borst, S. Lessons learnt about conducting a multilingual nutrition survey in Switzerland: Results from menuCH pilot survey. Int. J. Vitam. Nutr. Res. 2018. [Google Scholar] [CrossRef]
- Chatelan, A.; Beer-Borst, S.; Randriamiharisoa, A.; Pasquier, J.; Blanco, J.M.; Siegenthaler, S.; Paccaud, F.; Slimani, N.; Nicolas, G.; Camenzind-Frey, E.; et al. Major Differences in Diet across Three Linguistic Regions of Switzerland: Results from the First National Nutrition Survey menuCH. Nutrients 2017, 9, 1163. [Google Scholar] [CrossRef]
- Bochud, M.; Chatelan, A.; Blanco, J.-M.; Beer-Borst, S. Anthropometric Characteristics and Indicators of Eating and Physical Activity Behaviors in the Swiss Adult Population; Swiss Confederation. Federal Office of Public Health and the Food Safety and Veterinary Office: Bern, Switzerland, 2017. [Google Scholar]
- Swiss Health Observatory. Gesundheitsverhalten in der Schweiz—Sozio-ökonomische und Kulturelle Unterschiede unter der Lupe; Swiss Health Observatory OBSAN: Neuchâtel, Switzerland, 2016. [Google Scholar]
- Slimani, N.; Casagrande, C.; Nicolas, G.; Freisling, H.; Huybrechts, I.; Ocké, M.C.; Niekerk, E.M.; Van Rossum, C.; Bellemans, M.; De Maeyer, M.; et al. The standardized computerized 24-h dietary recall method EPIC-Soft adapted for pan-European dietary monitoring. Eur. J. Clin. Nutr. 2011, 65 (Suppl. 1), S5–S15. [Google Scholar] [CrossRef] [PubMed]
- Crispim, S.P.; de Vries, J.H.M.; Geelen, A.; Souverein, O.W.; Hulshof, P.J.; Lafay, L.; Rousseau, A.S.; Lillegaard, I.T.; Andersen, L.F.; Huybrechts, I.; et al. Two non-consecutive 24 h recalls using EPIC-Soft software are sufficiently valid for comparing protein and potassium intake between five European centres—Results from the European Food Consumption Validation (EFCOVAL) study. Br. J. Nutr. 2011, 105, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Camenzind-Frey, E.; Zuberbuehler, C.A. menuCH—Schweizerisches Fotobuch/livre Photo Suisse/Manuale Fotografico Svizzero; Federal Office of Public Health and Federal Food Safety and Veterinary Office: Bern, Switzerland, 2014. [Google Scholar]
- Crispim, S.P.; Nicolas, G.; Casagrande, C.; Knaze, V.; Illner, A.K.; Huybrechts, I.; Slimani, N. Quality assurance of the international computerised 24 h dietary recall method (EPIC-Soft). Br. J. Nutr. 2014, 111, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Federal Food Safety and Veterinary Office. Swiss Food Composition Database. 2018. Available online: http://www.naehrwertdaten.ch/ (accessed on 19 February 2018).
- Husson, F.; Lê, S.; Pagès, J. Exploratory Multivariate Analysis by Example Using R, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Abdi, H.; Williams, L.J.; Valentin, D. Multiple factor analysis: Principal component analysis for multitable and multiblock data sets. Wiley Interdiscip. Res. Comput. Stat. 2013, 5, 149–179. [Google Scholar] [CrossRef]
- Kostov, B.; Bécue-Bertaut, M.; Husson, F. Multiple Factor Analysis for Contingency Tables in the FactoMineR Package. R J. 2013, 5, 29–38. [Google Scholar]
- Pagès, J. Multiple Factor Analysis by Example Using R, 1st ed.; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Ward, J.H., Jr. Hierarchical Grouping to Optimize an Objective Function. J. Am. Stat. Assoc. 1963, 58, 236–244. [Google Scholar] [CrossRef]
- Fransen, H.P.; May, A.M.; Stricker, M.D.; Boer, J.M.; Hennig, C.; Rosseel, Y.; Ocké, M.C.; Peeters, P.H.; Beulens, J.W. A posteriori dietary patterns: How many patterns to retain? J. Nutr. 2014, 144, 1274–1282. [Google Scholar] [CrossRef]
- Pasquier, J.; Chatelan, A.; Bochud, M. Weighting Strategy; Institute of Social and Preventive Medicine: Lausanne, Switzerland, 2017. [Google Scholar]
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- IPAQ Research Committee. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ); Karolinska Institute: Stockholm, Sweden, 2005. [Google Scholar]
- MONICA. Manual, Part III, Section 1: Population Survey Data Component. 4.6 Height, Weight, Waist and Hip Measurement; WHO Press: Geneva, Switzerland, 1997. [Google Scholar]
- Buuren, S.V.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2001, 45, 1–67. [Google Scholar] [CrossRef]
- Lê, S.; Josse, J.; Husson, F. FactoMineR: An R Package for Multivariate Analysis. J. Stat. Softw. 2008, 25, 1–18. [Google Scholar] [CrossRef]
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S, 4th ed.; Springer: Berlin, Germany, 2002. [Google Scholar]
- Fox, J.; Andersen, R. Effect displays for multinomial and proportional-odds logit models. Sociol. Methodol. 2006, 36, 225–255. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Lachat, C.; Hawwash, D.; Ocké, M.C.; Berg, C.; Forsum, E.; Hörnell, A.; Larsson, C.; Sonestedt, E.; Wirfält, E.; Åkesson, A.; et al. Strengthening the Reporting of Observational Studies in Epidemiology-Nutritional Epidemiology (STROBE-nut): An Extension of the STROBE Statement. PLoS Med. 2016, 13, e1002036. [Google Scholar] [CrossRef]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Kant, A.K. Dietary patterns and health outcomes. J. Am. Diet. Assoc. 2004, 104, 615–635. [Google Scholar] [CrossRef]
- Wu, K.; Hu, F.B.; Willett, W.C.; Giovannucci, E. Dietary patterns and risk of prostate cancer in U.S. men. Cancer Epidemiol. Biomark. Prev. 2006, 15, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Bertrais, S.; Péneau, S.; Estaquio, C.; Dauchet, L.; Vergnaud, A.C.; Czernichow, S.; Galan, P.; Hercberg, S.; Bellisle, F. Dietary patterns and their sociodemographic and behavioural correlates in French middle-aged adults from the SU.VI.MAX cohort. Eur. J. Clin. Nutr. 2009, 63, 521–528. [Google Scholar] [CrossRef]
- Charreire, H.; Kesse-Guyot, E.; Bertrais, S.; Simon, C.; Chaix, B.; Weber, C.; Touvier, M.; Galan, P.; Hercberg, S.; Oppert, J.M. Associations between dietary patterns, physical activity (leisure-time and occupational) and television viewing in middle-aged French adults. Br. J. Nutr. 2011, 105, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Bessaoud, F.; Tretarre, B.; Daurès, J.-P.; Gerber, M. Identification of dietary patterns using two statistical approaches and their association with breast cancer risk: A case-control study in Southern France. Ann. Epidemiol. 2012, 22, 499–510. [Google Scholar] [CrossRef]
- Darmon, N.; Drewnowski, A. Does social class predict diet quality? Am. J. Clin. Nutr. 2008, 87, 1107–1117. [Google Scholar] [CrossRef] [PubMed]
- Vlismas, K.; Stavrinos, V.; Panagiotakos, D.B. Socio-economic status, dietary habits and health-related outcomes in various parts of the world: A review. Cent. Eur. J. Public Health 2009, 17, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Naska, A.; Costacou, T.; DAFNE III Group. Disparities in food habits across Europe. Proc. Nutr. Soc. 2002, 61, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Vormund, K.; Braun, J.; Rohrmann, S.; Bopp, M.; Ballmer, P.; Faeh, D. Mediterranean diet and mortality in Switzerland: An alpine paradox? Eur. J. Nutr. 2015, 54, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Slimani, N.; Fahey, M.; Welch, A.A.; Wirfält, E.; Stripp, C.; Bergström, E.; Linseisen, J.; Schulze, M.B.; Bamia, C.; Chloptsios, Y.; et al. Diversity of dietary patterns observed in the European Prospective Investigation into Cancer and Nutrition (EPIC) project. Public Health Nutr. 2002, 5, 1311–1328. [Google Scholar] [CrossRef] [PubMed]
- Linseisen, J.; Bergström, E.; Gafá, L.; Gonzalez, C.A.; Thiébaut, A.; Trichopoulou, A.; Tumino, R.; Sánchez, C.N.; Garcia, C.M.; Mattisson, I.; et al. Consumption of added fats and oils in the European Prospective Investigation into Cancer and Nutrition (EPIC) centres across 10 European countries as assessed by 24-hour dietary recalls. Public Health Nutr. 2002, 5, 1227–1242. [Google Scholar] [CrossRef]
- Pestoni, G.; Krieger, J.-P.; Sych, J.M.; Faeh, D.; Rohrmann, S. Determinants of diet quality and variations in diet between language regions of Switzerland: Results from the National Nutrition Survey menuCH. Nutrients 2018. in revision. [Google Scholar]
- De Ridder, K.; Lebacq, T.; Ost, C.; Teppers, E.; Brocatus, L. Rapport 4: La consommation alimentaire. Résumé des principaux résultats. In Enquête de Consommation Alimentaire 2014–2015; WIV-ISP: Brussel, Beligum, 2016. [Google Scholar]
- Batal, M.; Makvandi, E.; Imbeault, P.; Gagnon-Arpin, I.; Grenier, J.; Chomienne, M.H.; Bouchard, L. Comparison of dietary intake between Francophones and Anglophones in Canada: Data from CCHS 2.2. Can. J. Public Health 2013, 104, S31–S38. [Google Scholar] [CrossRef] [PubMed]
- Freisling, H.; Fahey, M.T.; Moskal, A.; Ocké, M.C.; Ferrari, P.; Jenab, M.; Norat, T.; Naska, A.; Welch, A.A.; Navarro, C.; et al. Region-specific nutrient intake patterns exhibit a geographical gradient within and between European countries. J. Nutr. 2010, 140, 1280–1286. [Google Scholar] [CrossRef]
- Traill, W.B.; Chambers, S.A.; Butler, L. Attitudinal and demographic determinants of diet quality and implications for policy targeting. J. Hum. Nutr. Diet. 2012, 25, 87–94. [Google Scholar] [CrossRef]
- Arabshahi, S.; Lahmann, P.H.; Williams, G.M.; Marks, G.C.; van der Pols, J.C. Longitudinal change in diet quality in Australian adults varies by demographic, socio-economic, and lifestyle characteristics. J. Nutr. 2011, 141, 1871–1879. [Google Scholar] [CrossRef] [PubMed]
- Walthouwer, M.J.L.; Oenema, A.; Soetens, K.; Lechner, L.; de Vries, H. Are clusters of dietary patterns and cluster membership stable over time? Results of a longitudinal cluster analysis study. Appetite 2014, 82, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Engeset, D.; Alsaker, E.; Ciampi, A.; Lund, E. Dietary patterns and lifestyle factors in the Norwegian EPIC cohort: The Norwegian Women and Cancer (NOWAC) study. Eur. J. Clin. Nutr. 2005, 59, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Millen, B.E.; Quatromoni, P.A.; Gagnon, D.R.; Cupples, L.A.; Franz, M.M.; D’Agostino, R.B. Dietary patterns of men and women suggest targets for health promotion: The Framingham Nutrition Studies. Am. J. Health Promot. 1996, 11, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Gorst-Rasmussen, A.; Dahm, C.C.; Dethlefsen, C.; Scheike, T.; Overvad, K. Exploring dietary patterns by using the treelet transform. Am. J. Epidemiol. 2011, 173, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Jacques, P.F.; Tucker, K.L. Are dietary patterns useful for understanding the role of diet in chronic disease? Am. J. Clin. Nutr. 2001, 73, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Panaretos, D.; Tzavelas, G.; Vamvakari, M.; Panagiotakos, D. Repeatability of dietary patterns extracted through multivariate statistical methods: A literature review in methodological issues. Int. J. Food Sci. Nutr. 2017, 68, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B.; Rimm, E.; Smith-Warner, S.A.; Feskanich, D.; Stampfer, M.J.; Ascherio, A.; Sampson, L.; Willett, W.C. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am. J. Clin. Nutr. 1999, 69, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Nanri, A.; Shimazu, T.; Ishihara, J.; Takachi, R.; Mizoue, T.; Inoue, M.; Tsugane, S. Reproducibility and validity of dietary patterns assessed by a food frequency questionnaire used in the 5-year follow-up survey of the Japan Public Health Center-Based Prospective Study. J. Epidemiol. 2012, 22, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Khani, B.R.; Ye, W.; Terry, P.; Wolk, A. Reproducibility and validity of major dietary patterns among Swedish women assessed with a food-frequency questionnaire. J. Nutr. 2004, 134, 1541–1545. [Google Scholar] [CrossRef] [PubMed]
- Sauvageot, N.; Schritz, A.; Leite, S.; Alkerwi, A.A.; Stranges, S.; Zannad, F.; Streel, S.; Hoge, A.; Donneau, A.F.; Albert, A. Stability-based validation of dietary patterns obtained by cluster analysis. Nutr. J. 2017, 16, 4. [Google Scholar] [CrossRef] [PubMed]
| Crude | Weighted 1 | |
|---|---|---|
| Participants with 2 complete 24HDRs; n | 2057 | |
| Sum of weights for weighted analysis; n | - | 4,627,878 |
| Sex | ||
| Males | 45.4% | 49.8% |
| Females | 54.6% | 50.2% |
| Age groups 2 | ||
| 18–29 years old | 19.4% | 18.8% |
| 30–44 years old | 25.9% | 29.9% |
| 45–59 years old | 30.4% | 29.8% |
| 60–75 years old | 24.3% | 21.6% |
| BMI categories 3 | ||
| Underweight (BMI < 18.5 kg/m2) | 2.5% | 2.4% |
| Normal weight (18.5 ≤ BMI < 25 kg/m2) | 54.2% | 54.1% |
| Overweight (25 ≤ BMI < 30 kg/m2) | 30.6% | 30.6% |
| Obese (BMI ≥ 30 kg/m2) | 12.7% | 12.9% |
| Language region 4 | ||
| German-speaking | 65.2% | 69.2% |
| French-speaking | 24.4% | 25.2% |
| Italian-speaking | 10.4% | 5.6% |
| Nationality | ||
| Swiss | 72.5% | 61.4% |
| Swiss binationals | 14.4% | 13.8% |
| Other | 13.0% | 24.8% |
| Education, highest degree | ||
| Primary school or no degree | 4.3% | 4.7% |
| Secondary | 47.1% | 42.6% |
| Tertiary | 48.5% | 52.6% |
| Marital status | ||
| Single | 30.8% | 31.1% |
| Married or in registered partnership | 54.7% | 52.2% |
| Divorced or terminated partnership | 10.8% | 12.1% |
| Other | 3.5% | 4.4% |
| Gross household income (CHF/month) | ||
| <6000 | 16.8% | 17.7% |
| 6000 to 13,000 | 40.9% | 39.8% |
| >13,000 | 13.9% | 14.9% |
| Imputed | 28.4% | 27.6% |
| Self-reported physical activity | ||
| Low | 12.2% | 12.9% |
| Moderate | 22.1% | 22.7% |
| High | 40.2% | 40.3% |
| Imputed | 25.5% | 24.2% |
| Smoking | ||
| Never smoker | 44.4% | 42.9% |
| Former smoker | 33.4% | 33.6% |
| Current smoker | 21.9% | 23.3% |
| Self-reported health | ||
| Very bad to medium | 13.2% | 12.7% |
| Good to very good | 86.6% | 87.1% |
| Currently on a weight-loss diet | ||
| No | 94.3% | 94.4% |
| Yes | 5.5% | 5.4% |
| “Western 1”—Soft Drinks and Meat | “Western 2”—Alcohol, Meat and Starchy | “Prudent” | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sex | ||||||
| Males (reference) | 1 | 1 | 1 | |||
| Females | 0.47 | [0.35–0.61] | 0.47 | [0.36–0.61] | 1.24 | [0.95–1.61] |
| Age groups 1 | ||||||
| 18–29 years old | 1.43 | [0.93–2.18] | 1.57 | [1.03–2.39] | 1.20 | [0.78–1.84] |
| 30–44 years old (reference) | 1 | 1 | 1 | |||
| 45–59 years old | 0.80 | [0.57–1.13] | 1.03 | [0.73–1.46] | 1.65 | [1.19–2.29] |
| 60–76 years old | 0.45 | [0.29–0.71] | 1.04 | [0.70–1.55] | 2.08 | [1.43–3.03] |
| BMI categories 2 | ||||||
| Underweight (BMI < 18.5 kg/m2) | 1.02 | [0.41–2.53] | 0.88 | [0.36–2.11] | 1.45 | [0.70–2.98] |
| Normal (18.5 ≤ BMI < 25 kg/m2)—(reference) | 1 | 1 | 1 | |||
| Overweight (25 ≤ BMI < 30 kg/m2) | 1.11 | [0.82–1.51] | 1.13 | [0.85–1.52] | 1.04 | [0.78–1.39] |
| Obese (BMI ≥ 30 kg/m2) | 2.32 | [1.54–3.50] | 1.30 | [0.85–2.00] | 1.09 | [0.72–1.67] |
| Language region 3 | ||||||
| German-speaking (reference) | 1 | 1 | 1 | |||
| French-speaking | 1.40 | [1.03–1.91] | 1.33 | [0.98–1.80] | 1.92 | [1.45–2.53] |
| Italian-speaking | 0.83 | [0.43–1.61] | 2.00 | [1.19–3.38] | 1.68 | [0.98–2.90] |
| Nationality | ||||||
| Swiss (reference) | 1 | 1 | 1 | |||
| Swiss binationals | 1.13 | [0.77–1.68] | 0.96 | [0.64–1.43] | 1.73 | [1.22–2.45] |
| Others | 1.67 | [1.20–2.33] | 1.88 | [1.36–2.59] | 2.25 | [1.64–3.08] |
| Education, highest degree | ||||||
| Primary school or no degree | 0.90 | [0.46–1.77] | 0.85 | [0.45–1.60] | 1.15 | [0.62–2.12] |
| Secondary (reference) | 1 | 1 | 1 | |||
| Tertiary | 0.77 | [0.58–1.02] | 0.79 | [0.61–1.04] | 1.25 | [0.96–1.63] |
| Marital status | ||||||
| Single (reference) | 1 | 1 | 1 | |||
| Married or in registered partnership | 0.97 | [0.67–1.39] | 0.78 | [0.55–1.11] | 0.87 | [0.62–1.22] |
| Divorced or terminated partnership | 1.44 | [0.85–2.45] | 1.41 | [0.86–2.33] | 1.49 | [0.92–2.40] |
| Other | 1.30 | [0.57–2.98] | 2.36 | [1.20–4.64] | 2.51 | [1.31–4.80] |
| Gross household income (CHF/month) | ||||||
| <6000 | 0.70 | [0.49–1.00] | 0.69 | [0.49–0.97] | 0.55 | [0.39–0.78] |
| 6000 to 13,000 (reference) | 1 | 1 | 1 | |||
| >13,000 | 0.91 | [0.63–1.31] | 0.88 | [0.61–1.26] | 0.86 | [0.62–1.21] |
| Self-reported physical activity | ||||||
| Low (reference) | 1 | 1 | 1 | |||
| Moderate | 0.72 | [0.48–1.09] | 1.73 | [1.12–2.67] | 1.15 | [0.77–1.71] |
| High | 0.88 | [0.61–1.27] | 1.51 | [1.01–2.27] | 1.00 | [0.69–1.45] |
| Smoking | ||||||
| Never smoker (reference) | 1 | 1 | 1 | |||
| Former smoker | 0.97 | [0.71–1.31] | 1.75 | [1.31–2.34] | 1.14 | [0.87–1.49] |
| Current smoker | 2.42 | [1.72–3.40] | 3.30 | [2.34–4.64] | 2.28 | [1.62–3.20] |
| Self-reported health | ||||||
| Very bad to medium | 1.06 | [0.70–1.61] | 1.38 | [0.94–2.03] | 1.05 | [0.71–1.55] |
| Good to very good (reference) | 1 | 1 | 1 | |||
| Currently on a diet | ||||||
| No (reference) | 1 | 1 | 1 | |||
| Yes | 1.25 | [0.67–2.33] | 1.17 | [0.62–2.20] | 2.65 | [1.56–4.51] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krieger, J.-P.; Pestoni, G.; Cabaset, S.; Brombach, C.; Sych, J.; Schader, C.; Faeh, D.; Rohrmann, S. Dietary Patterns and Their Sociodemographic and Lifestyle Determinants in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients 2019, 11, 62. https://doi.org/10.3390/nu11010062
Krieger J-P, Pestoni G, Cabaset S, Brombach C, Sych J, Schader C, Faeh D, Rohrmann S. Dietary Patterns and Their Sociodemographic and Lifestyle Determinants in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients. 2019; 11(1):62. https://doi.org/10.3390/nu11010062
Chicago/Turabian StyleKrieger, Jean-Philippe, Giulia Pestoni, Sophie Cabaset, Christine Brombach, Janice Sych, Christian Schader, David Faeh, and Sabine Rohrmann. 2019. "Dietary Patterns and Their Sociodemographic and Lifestyle Determinants in Switzerland: Results from the National Nutrition Survey menuCH" Nutrients 11, no. 1: 62. https://doi.org/10.3390/nu11010062
APA StyleKrieger, J.-P., Pestoni, G., Cabaset, S., Brombach, C., Sych, J., Schader, C., Faeh, D., & Rohrmann, S. (2019). Dietary Patterns and Their Sociodemographic and Lifestyle Determinants in Switzerland: Results from the National Nutrition Survey menuCH. Nutrients, 11(1), 62. https://doi.org/10.3390/nu11010062







