Abstract
Prospective cohort studies have described an association between coffee or tea consumption and the risk of developing diabetes. However, whether coffee or tea improves glucose metabolism remains uncertain. We investigated the effect of coffee and tea on glucose metabolism by conducting a systematic review and meta-analysis of randomized controlled trials. Electronic databases were searched for articles published up 19 February 2017. The primary endpoint was the mean difference in post-intervention fasting blood glucose (FBG) levels between the groups. Of 892 citations screened, 27 studies (1898 participants) were included in our meta-analysis. A network meta-analysis suggested that green tea, but not caffeinated/decaffeinated coffee or black tea, may reduce FBG levels, compared with placebo/water (−2.10 mg/dL; 95% confidence interval (CI), −3.96 to −0.24 mg/dL; p = 0.03; moderate quality of evidence). In a subgroup analysis, the effect of green tea on FBG levels was statistically significant only in studies with a mean age of < 55-years-old or Asian-based studies. The oolong tea group also showed a significant decrease in FBG, but the quality of evidence was very low. In conclusion, green tea consumption might decrease FBG levels, especially in < 55-year-olds or Asian-based populations.
1. Introduction
The number of people with diabetes is increasing rapidly, worldwide. The International Diabetes Federation reported that in 2015, 415 million adults had diabetes and that by 2040, this number is expected to rise to 642 million [1]. In 2015, the global economic burden associated with diabetes reached US$1.31 trillion, becoming a substantial global economic burden [2]. Therefore, low-cost and easily accessible strategies for preventing diabetes are required. Globally, coffee and tea are widely consumed beverages and their consumption is integrated into people’s daily lives. A large body of epidemiological evidence, from prospective cohort studies, suggests a strong association between coffee/tea consumption and a decreased risk of diabetes [3,4,5,6]. If the associations are causal, there would be substantial public health implications. However, whether or not these beverages reduce glucose metabolism remains uncertain. Previous meta-analyses of clinical trial data have investigated the effects of coffee or tea consumption on glucose metabolism [7,8,9]. Unfortunately, these meta-analyses have not evaluated tea and coffee comprehensively; have included duplicate studies [7]; have evaluated only acute effects [10]; and did not evaluate the quality of evidence across studies [7,8,9], using approaches such as the Grading of Recommendations Assessment Development and Evaluation (GRADE) system [11]. Together, these weaknesses limit the interpretation of the results and provide insufficient information to make relevant judgments.
Network meta-analysis (NMA) is a method that enables the comparison of multiple interventions using direct and indirect comparison evidence even when direct comparisons of data are insufficient [12]. Hence, we performed a systematic review that involved an NMA, using the GRADE system to comprehensively evaluate the effects of coffee and tea consumption on glucose metabolism.
2. Materials and Methods
2.1. Literature Search
This study was conducted according to a predetermined protocol (PROSPERO # CRD42015029597) developed using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Protocols [13,14]. We systematically searched PubMed, Embase, and the Cochrane library for eligible randomized, controlled clinical trials published before February 19, 2017 without any language restrictions. The literature search involved querying the terms “coffee,” “tea,” “glucose,” “HbA1c,” “insulin,” “insulin resistance,” and “randomized controlled trial (RCT).” In addition, we manually searched the references included in each original article retrieved. The details of the literature search strategy are described in the Supplementary Table S1.
2.2. Study Selection
We included studies examining the effects of caffeinated coffee, decaffeinated coffee, black tea, oolong tea, and green tea (caffeinated or decaffeinated), given as a drink or crude extract, with follow-up durations of at least 2 weeks. We excluded studies examining multi-nutrient supplements, in addition to coffee or tea as interventions. Studies were selected for this analysis only if they also described an RCT in human adults involving either a parallel or crossover design and had at minimum, fasting blood glucose (FBG) or hemoglobin A1c (HbA1c) results available for each group. In cases involving multiple publications of the same study, the most informative article was included.
2.3. Data Extraction
Two investigators extracted data independently and resolved any discrepancies through discussion. The extracted information included study characteristics (authors, design, publication year, sample size, duration of intervention, and follow-up), participant characteristics (age, sex, ethnicity, body mass index, HbA1c, FBG concentration), 2-h post-load glucose concentration from an oral glucose tolerance test (75-g OGTT 2h-PG), fasting blood insulin (fasting IRI) concentration, homeostasis model assessment for insulin resistance (HOMA-IR) and HOMA-ß, and intervention (type of tea or coffee).
2.4. Risk of Bias Assessment
The risk of bias was assessed using Cochrane’s risk of bias tool [15]. In addition, quality of evidence was assessed using the GRADE system [11].
2.5. Strategy for Data Synthesis
We examined the effects of the studied interventions after combining green tea and green tea extract into a single group referred to as green tea. Decaffeinated green tea and decaffeinated green tea extract interventions were also combined into a single decaffeinated green tea group. A standard, pairwise meta-analysis was conducted for each pairwise direct comparison of interventions (caffeinated coffee, decaffeinated coffee, black tea, oolong tea, caffeinated green tea, and decaffeinated green tea). The outcome data (post-intervention values) were extracted for subsequent analyses. When studies reported data for different durations of intervention, the duration for the pre-defined primary endpoint in each study, was used in the analyses. If the standard deviations of the endpoints were missing, pooled standard deviations were calculated from the other included studies [16]. We used a random-effects model to incorporate the assumption that different studies estimated different yet related intervention effects. Publication biases or small study effects were examined using conventional funnel plots.
In addition, we conducted network meta-analyses within the frequentist framework using multivariate random-effects meta-analysis models, which consider the heterogeneity of effects across studies. The results for the comparative effects are presented as mean difference estimates and 95% confidence intervals (CIs). We plotted a comparison-adjusted funnel plot to detect the presence of publication bias in the network meta-analysis. We also evaluated the ranking of the intervention effect, i.e., the most efficacious beverage, second best, third best, etc. Inconsistency between the direct and indirect evidence on the network was evaluated using global and local inconsistency tests [17].
Stata 14 software (Stata, College Station, TX, USA) was used for the analyses. The “metan” package [18] was used to conduct the pairwise random-effects meta-analyses and the “metareg” package [19] was used for the meta-regression analyses; the “network” package [20] was used for the NMAs. The p-values < 0.05 were considered statistically significant.
2.6. Subgroup or Subset Analysis
In the pairwise direct comparison meta-analyses, the heterogeneity of the intervention effects across studies were investigated using the heterogeneity test and the I2 statistic.
The sources of possible clinical heterogeneity were listed a priori, such as age, sex, ethnicity, body mass index, baseline fasting blood glucose level, and the baseline HbA1c level. Among these, data on age, sex, ethnicity, body mass index, baseline fasting blood glucose level were available. These were examined as effect modifiers in the meta-regression or subgroup analyses. Sensitivity analyses were also conducted for assessing possible biases.
3. Results
3.1. Study Selection and Characteristics
Of the 892 citations identified, 27 studies involving 1898 subjects were included in our meta-analysis (Figure 1) [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. The characteristics of the included studies are shown in Table 1. Of these studies, effects were reported on FBG concentrations (26 studies), 75-g OGTT 2h-PG concentrations (4 studies), HbA1c (10 studies), fasting IRI concentrations (13 studies), and HOMA-IR (8 studies); no studies reported results on HOMA-ß. Figure 2 shows the network plots of eligible comparisons for FBG, 75-g OGTT 2h-PG, HbA1c, fasting IRI, and HOMA-IR. Six classes of interventions (coffee, decaffeinated coffee, green tea, decaffeinated green tea, black tea, oolong tea) had adequate numbers of studies for NMA. The effects of coffee and decaffeinated coffee were indirectly and directly compared. The differences between direct and indirect evidence in closed loops in the network showed no indication of inconsistency.
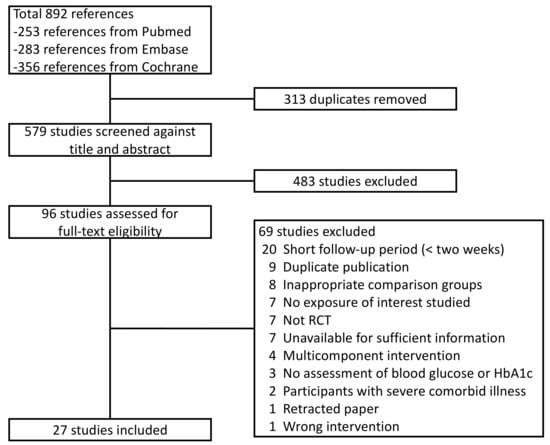
Figure 1.
Study selection flow.

Table 1.
Characteristics of the included studies.
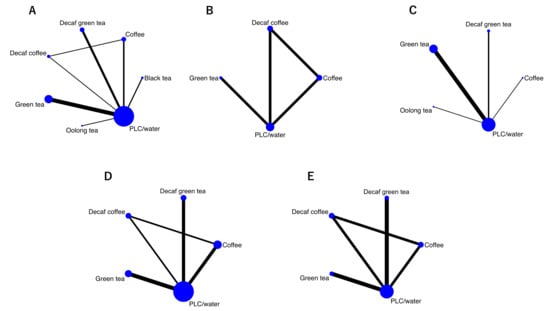
Figure 2.
Network maps. (A) Fasting blood glucose; (B) 2-h post-load glucose concentration from an oral glucose tolerance test; (C) HbA1c; (D) fasting blood insulin; (E) HOMA-IR; Nodes represent the interventions and their sizes represent the number of participants. Edges represent the available direct comparisons between pairs of interventions; the width represents the number of studies comparing the pair of interventions. Abbreviations: Decaf, decaffeinated; PLC, placebo.
3.2. Risk of Bias for Included Studies
The included studies generally had unclear or high risks of bias for random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessments, and selective outcome reporting. The Cochrane risk of bias analysis indicated among the studies with a high risk of bias, blinding of the participants and personnel was highest (51.9%); selective reporting contributed the most to the unclear-domain bias (63.0%). Furthermore, 59.3% of the studies were judged to have an unclear or high risk of bias for either domain or selection bias, which may have seriously distorted the validity of each study. Details regarding the risk of biases are shown in Figure 3.
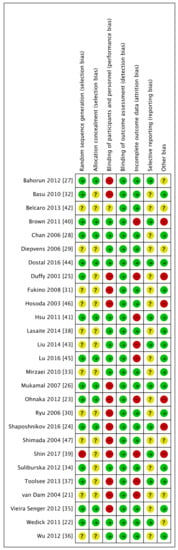
Figure 3.
Risk of bias summary.
3.3. Primary Endpoint: FBG
Twenty-six studies reported effects on FBG concentrations. Of these, 2 [22,23] reported the effects of both coffee and decaffeinated coffee on FBG concentrations. Thus, the effects on FBG concentrations were reported for coffee (4 studies [21,22,23,24]), decaffeinated coffee (2 studies [22,23]), black tea (3 studies [25,26,27]), green tea (11 studies [28,29,30,31,32,33,34,35,36,37,39]), decaffeinated green tea (6 studies [40,41,42,43,44,45]), oolong tea (2 studies [46,47]).
A direct pairwise meta-analysis (−2.10 mg/dL; 95% CI, −3.93 to −0.27 mg/dL; p = 0.02) and NMA for studies with a moderate quality of evidence (−2.10 mg/dL; 95% CI, −3.96 to −0.24 mg/dL; p = 0.03) suggested that green tea consumption slightly but significantly reduced FBG concentrations compared with placebo/water (Table 2, Figure 4).

Table 2.
Intervention effect on fasting blood glucose vs. placebo/water.
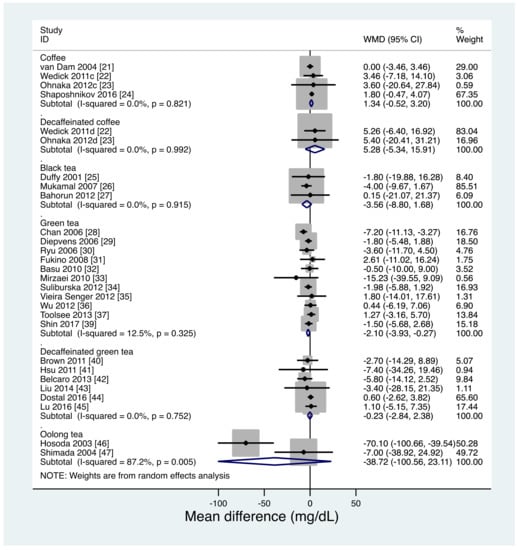
Figure 4.
Direct pairwise meta-analysis of effects on fasting blood glucose levels. c, coffee study arm; d, decaffeinated coffee study arm.
The meta-regression analysis showed a tendency for the FBG reductive effect of green tea to be stronger in studies with a mean age < 55-years-old than in studies with an older mean age (β = 0.17; standard error (SE), 0.10; 95% CI, −0.04 to 0.41; p = 0.10; Supplemental Figure S1a). In the NMA, stratified by mean participant age, the effect of green tea on FBG concentrations was significant only in younger individuals (age < 55: −2.51 mg/dL; 95% CI, −4.67 to −0.35; p = 0.02; age ≥ 55: −0.72 mg/dL; 95% CI, −4.61 to 3.17 mg/dL; p = 0.72). In the direct pairwise meta-analysis, stratified by Asian-based studies and non-Asian-based studies, the effect of green tea on FBG concentrations was significant only in Asian-based studies (Asian: −3.81 mg/dL; 95% CI, −7.58 to −0.04; p = 0.04; non-Asian: −0.92 mg/dL; 95% CI, −3.01 to 1.16 mg/dL; p = 0.39; Figure 5).
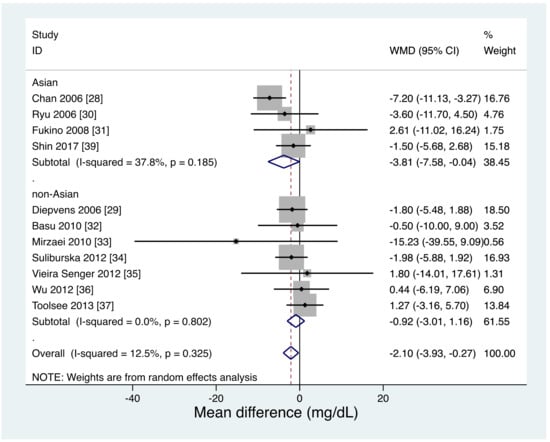
Figure 5.
Direct pairwise meta-analysis: effects of green tea on fasting blood glucose levels stratified by Asian-based studies and non-Asian based studies.
Meta-regression analysis indicated that the intervention duration did not modify the effects of green tea on FBG concentrations (β = 0.01; SE, 0.08; 95% CI, −0.16 to 0.19; p = 0.87; Supplemental Figure S1b). Meta-regression analysis also indicated that the percentage of male sex, BMI, and baseline FBG did not modify the effects of green tea on FBG concentrations (percentage of male sex: β = 0.04; SE, 0.03; 95% CI, −0.04 to 0.12; p = 0.25, BMI: β = −0.20; SE, 0.32; 95%, CI −0.92 to 0.52; p = 0.55, baseline FBG: β = −0.01; SE, 0.11; 95% CI, −0.25 to 0.24; p = 0.96). In a post-hoc stratified analysis according to non-diabetic [28,29,34,36,39], prediabetic (including subjects with metabolic syndrome) [31,32,35,37], and diabetic subjects [30,33], the significant effect of green tea on FBG concentrations was only evident in a subgroup with non-diabetic subjects (non-diabetic: −2.74 mg/dL; 95% CI, −5.19 to −0.29 mg/dL; p = 0.03, prediabetic: 1.13 mg/dL; 95% CI, −2.62 to 4.87 mg/dL; p = 0.56, diabetic: −4.76 mg/dL; 95% CI, −12.45 to 2.92 mg/dL; p = 0.23; Supplemental Figure S1c). Further, a post-hoc meta-regression analysis suggested that prediabetes or diabetes did not modify the effects of green tea on FBG concentrations (meta-regression heterogeneity; prediabetes: p = 0.24, diabetes: p = 0.64).
The oolong tea group also had lower FBG concentrations than did the water group in the NMA (−39.91 mg/dL; 95% CI, −62.04 to −17.78 mg/dL; p < 0.001; Table 2) but not in the direct pairwise meta-analysis. However, the quality of evidence was very low because of a serious risk of bias due to unclear allocation concealment in all oolong tea studies and a potential financial bias, serious heterogeneity (I2 of 87.2%), and very serious imprecision due to having a small sample size and wide confidence interval. Coffee, decaffeinated coffee, black tea, and decaffeinated green tea did not show significant effects on FBG concentrations in either the direct pairwise meta-analysis or the NMA.
Ranking the effects of the interventions on FBG concentrations, after NMA, showed that oolong tea had a mean rank of 1.0 (surface under the cumulative ranking curve (SUCRA), 1.0), black tea had a mean rank of 2.8 (SUCRA, 0.7), and green tea had a mean rank of 3.8 (SUCRA, 0.7). The oolong tea intervention had a one-order larger effect on FBG concentrations as compared with the other interventions, although the quality of evidence was very low. The resulting large heterogeneity in effect sizes across the interventions may have led to unstable NMA estimates. However, excluding the oolong tea studies did not materially change the NMA results (Supplemental Table S2). As shown in the comparison-adjusted funnel plot (Supplemental Figure S2), there was no apparent evidence of asymmetry.
3.4. Secondary Endpoints:
3.4.1. 75-g OGTT 2h-PG
Four studies [22,23,28,33] reported the effects of the interventions on 75-g OGTT 2h-PG concentrations, including two studies [28,33] involving green tea and two [22,23] involving both coffee and decaffeinated coffee. Neither the direct pairwise meta-analysis nor the NMA showed any significant effects associated with coffee, decaffeinated coffee, or green tea on 75-g OGTT 2h-PG concentrations relative to a placebo/water (Table 3, Supplemental Figure S3). The comparison-adjusted funnel plot (Supplemental Figure S4) does not show any evidence of asymmetry.

Table 3.
Intervention effect on 2-h oral glucose tolerance test results for blood glucose vs. placebo/water.
3.4.2. HbA1c
Ten studies reported the interventions’ effects on HbA1c, including 1 [24] showing the effects of coffee, six [31,32,33,36,37,38] showing the effects of green tea, 2 [41,43] showing the effects of decaffeinated green tea, and 1 [47] showing the effects of oolong tea. Thus, we conducted meta-analyses examining green tea (6 studies [31,32,33,36,37,38]) and decaffeinated green tea (2 studies [41,43]) vs. placebo/water. Neither direct pairwise meta-analysis nor NMA showed any significant effect for these interventions on HbA1c (Table 4, Supplemental Figure S5). The comparison-adjusted funnel plot (Supplemental Figure S6) does not show any asymmetry related to green tea.

Table 4.
Intervention effect on HbA1c vs. placebo/water.
3.4.3. Fasting IRI
Fifteen studies [21,22,23,24,28,30,31,33,36,40,41,42,43] reported the effects of the interventions on fasting IRI concentrations relative to a placebo/water, including two [21,24] involving coffee, two [22,23] involving both coffee and decaffeinated coffee, five [28,30,31,33,36] involving green tea, and four [40,41,43] involving decaffeinated green tea. Only coffee showed significant impacts on fasting IRI concentrations, in both the direct pairwise meta-analyses (+1.1 μIU/mL; 95% CI, 0.22.0 μIU/mL; Supplemental Figure S7) and in the NMA (+1.1 μIU/mL; 95% CI, 0.2–2.0 μIU/mL; Table 5). However, the comparison-adjusted funnel plot (Supplemental Figure S8) did not show any evidence of asymmetry.

Table 5.
Intervention effect on fasting blood insulin vs. placebo/water.
3.4.4. HOMA-IR
Eight studies [22,23,30,31,32,41,42,43] reported the effects of the interventions on HOMA-IR, including two involving both coffee and decaffeinated coffee [22,23], 3 [30,31,32] involving green tea, and three [41,42,43] involving decaffeinated green tea. There were no significant effects of these interventions on HOMA-IR levels relative to placebo/water in the direct pairwise meta-analysis or in the NMA (Table 6, Supplemental Figure S9). Additionally, the comparison-adjusted funnel plot (Supplemental Figure S10) did not show any evidence of asymmetry.

Table 6.
Intervention effect on HOMA-IR vs. placebo/water.
4. Discussion
In this systematic review and NMA, we evaluated the effects of various coffee and tea consumptions on glucose metabolism across available RCT data. We found 27 studies, involving 1898 subjects with study durations of 4–72 weeks. With regard to the primary endpoint, the studies with a moderate quality of evidence suggested that green tea consumption, but not consumption of caffeinated/decaffeinated coffee or black tea, may reduce FBG concentrations, as compared with a placebo/water. The effect estimates were also statistically significant for oolong tea, but the quality of evidence was very low due to the risk of bias and imprecision in the studies. As for the secondary endpoint, studies with a moderate quality of evidence indicated that caffeinated coffee consumption may increase insulin concentrations. The potential effects of green tea on glucose metabolism have substantial public health implications given the global diabetes epidemic, such that even a small potential downward shift in the distribution of FBG concentrations would result in substantial numbers of individuals avoiding diabetes. Although further efforts are required to confirm the evidence, our findings support the notion that green tea may be a preventative strategy for reducing the number of people developing diabetes.
Some mechanisms have been suggested to explain the ability of green tea to reduce FBG concentrations. Previous rodent-based studies reported that the potential beneficial effect of green tea on glucose metabolism may be mediated by epigallocatechin gallate (EGCG), the most abundant catechin present in green tea [48]. Waltner-Law et al. reported that EGCG reduces hepatic glucose production by increasing tyrosine phosphorylation of the insulin receptor and insulin receptor substrate-1 in H4IIE rat hepatoma cell models [49]. Recent studies have also suggested that green tea increases insulin sensitivity and glucose metabolism, helping to prevent type 2 diabetes from developing. Ortsäter et al. also reported that EGCG preserves islet structure and enhances glucose tolerance in genetically diabetic mice (young db/db mice) [50]. Further, Ueda et al. reported that EGCG may reduce hyperglycemic events by promoting glucose transporter-4 translocation in skeletal muscle via a mechanism that is partially different from the action of insulin because EGCG promoted the translocation in insulin-resistant L6 myotubes and had neither a synergistic nor an additive effect on insulin [51]. Surprisingly, Fu et al. reported that EGCG increases the concentrations of the circulating anti-inflammatory cytokine, interleukin-10, and delayed type 1 diabetes onset in non-obese diabetic mice [52]. In our meta-analysis, green tea and its extract reduced FBG concentrations. In the NMA, the effect of green tea on FBG concentrations was confined to younger (< 55-years-old) subjects. Beta-cell function is known to decrease continuously from euglycemia until the onset of type 2 diabetes [53,54]. Therefore, early green tea intervention, which may help maintain beta-cell function, might be a prerequisite for its potential effects on FBG concentrations, at least via the proposed beta-cell protection mechanism. The reason for the discrepancy between results derived from Asian-based studies and non-Asian-based studies is unclear. In both Asian and non-Asian studies, 75% of studies used green tea extract for the intervention. If the EGCG content was not provided, we assumed that one cup of green tea contains 110 mg of EGCG [32] and 100 mg of green tea extract contains 21.4 mg of EGCG [29] from similar studies. The mean daily EGCG doses were not different between the Asian and non-Asian studies (367.3 ± 175.5 mg/day vs. 374.6 ± 186.8 mg/day, p = 0.95). The meta-regression analysis showed there was no significant interaction between daily the EGCG dose contained in green tea and the FBG (β = 0.00; SE, 0.01; 95% CI, −0.02 to 0.01; p = 0.54; Supplemental Figure S11).
One possible explanation could be the differences in dietary habits or genetic predisposition for impaired glucose metabolism that might interact with the glucose-lowering effects of green tea. However, further investigations are certainly needed to understand this possible ethnic difference. Caffeine is known to reduce insulin sensitivity in the short term and have adverse effects such as arrhythmias, pregnancy complications, and drug interactions from clinical trials [55]. Thus, such potential risks associated with caffeine should also be evaluated in order to make recommendations regarding caffeine-related beverages such as caffeinated coffee and tea. In our meta-analysis, green tea reduced FBG levels but did not reduce HbA1c levels. Two-thirds of the included green tea studies with HbA1c data were followed up in less than 12 weeks. This might be too short a period for assessing the effects for change in HbA1c levels accurately.
Oolong tea also showed potential protective effects on FBG concentrations in the NMA. Both green tea and oolong tea are derived from Camellia sinensis, with their only difference being in the level of fermentation; green tea is unfermented whereas oolong tea is partially fermented. Therefore, both may exert protective effects on glucose metabolism through similar mechanisms. However, the two oolong tea studies included in our meta-analysis were supported by oolong tea manufacturers and had a very low quality of evidence due to the presence of very serious risks of bias and serious imprecisions. Thus, our inferences regarding the potential protective effects of oolong tea are limited. Indeed, a five-day, cross-over trial of 19 participants failed to show the protective effects of oolong tea on glucose metabolism, i.e., FBG concentrations and incremental glucose areas under the concentration time curve remained largely unchanged in the trial arms [56,57,58]. To assess the true effects of oolong tea on glucose metabolism, more precisely designed, larger-scale RCTs are required. A series of prospective cohort studies reported that coffee and decaffeinated coffee intakes were linked to reducing the risk of type 2 diabetes [57]. In a meta-analysis and systematic review that summarized the findings from 28 prospective studies, the relative risk of diabetes associated with a 1-cup/day consumption increase was 0.91 (95% CI, 0.89–0.94) for caffeinated coffee consumption and 0.94 (95% CI, 0.91–0.98) for decaffeinated coffee consumption [21]. Further, these findings also suggested a dose-response relationship. However, in our meta-analysis, coffee and decaffeinated coffee consumption were unrelated to FBG concentrations. Furthermore, our meta-analysis showed that coffee resulted in slight increases in fasting IRI concentrations, raising concerns that coffee may impair insulin sensitivity. Because the follow-up periods of the included studies were far shorter than for the cohort studies and the total number of participants of coffee trials was small (below optimal information criterion), the long-term effect of coffee on glucose metabolism remains uncertain and longer (a few years) RCTs with a sufficient number of participants are required.
To date, this meta-analysis is the most comprehensive analysis, using a combined NMA and GRADE approach to evaluate the effects of tea and coffee on glucose metabolism. However, several limitations merit further consideration. First, complete blinding of coffee or tea interventions is difficult due to their taste. Thus, most studies were conducted using an open-label design. Second, the study durations were relatively short (median, 9 weeks; interquartile range, 6.5–16 weeks). Therefore, additional randomized studies, having longer durations and sufficient washout periods, are needed to determine the long-term effects of coffee and tea consumption on glucose metabolism.
5. Conclusions
In conclusion, this systematic review and NMA of 27 studies, involving 1898 subjects and having a moderate quality of evidence, indicates that green tea consumption, compared with a placebo/water, might slightly lower FBG concentrations. Oolong tea consumption also resulted in significant decreases in FBG concentrations in the NMA but the studies suffered from a very low quality of evidence. Further, studies with a moderate quality of evidence indicated that caffeinated coffee consumption may increase insulin concentrations. The effects of consuming coffee or tea on HbA1c, 75-g OGTT 2h-PG, HOMA-IR, and HOMA-ß are limited and uncertain. Although further efforts are required to confirm the benefit of green tea on glucose metabolism, our study provides supportive evidence that green tea might lower FBG concentrations, possibly leading to a reduction in the number of people developing diabetes as a result of regular consumption.
Supplementary Materials
The following are available online at http://www.mdpi.com/2072-6643/11/1/48/s1, Search strategy, supplemental Figure S1a: Meta-regression graph between effects of green tea on fasting blood glucose and study mean age; Figure S1b: Meta-regression graph between effects of green tea on fasting blood glucose and intervention duration (weeks); Figure S1c: Direct pairwise meta-analysis, effects of green tea on fasting blood glucose levels, stratified by non-diabetic, prediabetic, and diabetic subjects; Figure S2: Comparison-adjusted funnel plot of effects on fasting blood glucose level; Figure S3: Direct pairwise meta-analysis forest plot of effects on 2-h oral glucose tolerance test results for blood glucose vs. placebo/water; Figure S4: Comparison-Adjusted Funnel Plot of effects on 2-h oral glucose tolerance test results for blood glucose vs. placebo/water; Figure S5: Direct pairwise meta-analysis forest plot of effects on HbA1c vs. placebo/water; Figure S6: Comparison-Adjusted Funnel Plot of effects on HbA1c vs. placebo/water; Figure S7: Direct pairwise meta-analysis forest plot of effects on fasting blood insulin vs. placebo/water; Figure S8: Comparison-Adjusted Funnel Plot of effects on fasting blood insulin vs. placebo/water; Figure S9: Direct pairwise meta-analysis forest plot of effects on HOMA-IR vs. placebo/water; Figure S10: Comparison-Adjusted Funnel Plot of effects on HOMA-IR vs. placebo/water; Figure S11: Meta-regression graph between effects of green tea on fasting blood glucose and daily EGCG dose (mg); Table S1 Search strategy, Table S2 Effects on fasting blood glucose vs. placebo/water, analyzed without oolong tea.
Author Contributions
Y.K. and A.G. designed the protocol of systematic review. Y.K. and A.G. did the literature search and selected studies for inclusion. Y.K. and A.G. extracted data for analysis. Y.K. and A.G. performed the statistical analysis and interpreted the data. H.N. checked statistical methodology. Y.K. wrote the first draft and all authors revised the manuscript for important intellectual content. All authors approved the final draft.
Funding
Health sciences research grants (comprehensive research on lifestyle-related diseases, including cardiovascular diseases and diabetes mellitus, H25-016 and H25-029) from the Ministry of Health, Labour and Welfare of Japan. JSPS KAKENHI (grant number 15K21389, 18K10095) from the Japan Society for the Promotion of Science (JSPS). AMED (grant number JP18ck0106370) from Japan Agency for Medical Research and Development.
Conflicts of Interest
All authors have no potential conflict of interest.
References
- Ogurtsova, K.; da Rocha Fernandes, J.D.; Huang, Y.; Linnenkamp, U.; Guariguata, L.; Cho, N.H.; Cavan, D.; Shaw, J.E.; Makaroff, L.E. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res. Clin. Pract. 2017, 128, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Bommer, C.; Heesemann, E.; Sagalova, V.; Manne-Goehler, J.; Atun, R.; Barnighausen, T.; Vollmer, S. The global economic burden of diabetes in adults aged 20–79 years: A cost-of-illness study. Lancet Diabetes Endocrinol. 2017, 5, 423–430. [Google Scholar] [CrossRef]
- Van Dam, R.M.; Feskens, E.J. Coffee consumption and risk of type 2 diabetes mellitus. Lancet 2002, 360, 1477–1478. [Google Scholar] [CrossRef]
- Salazar-Martinez, E.; Willett, W.C.; Ascherio, A.; Manson, J.E.; Leitzmann, M.F.; Stampfer, M.J.; Hu, F.B. Coffee consumption and risk for type 2 diabetes mellitus. Ann. Intern. Med. 2004, 140, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Odegaard, A.O.; Pereira, M.A.; Koh, W.P.; Arakawa, K.; Lee, H.P.; Yu, M.C. Coffee, tea, and incident type 2 diabetes: The Singapore Chinese Health Study. Am. J. Clin. Nutr. 2008, 88, 979–985. [Google Scholar] [CrossRef] [PubMed]
- Iso, H.; Date, C.; Wakai, K.; Fukui, M.; Tamakoshi, A. The relationship between green tea and total caffeine intake and risk for self-reported type 2 diabetes among Japanese adults. Ann. Intern. Med. 2006, 144, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Zhou, R.; Wang, B.; Chen, K.; Shi, L.Y.; Zhu, J.D.; Mi, M.T. Effect of green tea on glucose control and insulin sensitivity: A meta-analysis of 17 randomized controlled trials. Am. J. Clin. Nutr. 2013, 98, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.J.; Stanley, M.; Parkhouse, N.; Cook, K.; Smith, M. Acute caffeine ingestion enhances strength performance and reduces perceived exertion and muscle pain perception during resistance exercise. Eur. J. Sport Sci. 2013, 13, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, C.; Huai, Q.; Guo, F.; Liu, L.; Feng, R.; Sun, C. Effects of tea or tea extract on metabolic profiles in patients with type 2 diabetes mellitus: A meta-analysis of ten randomized controlled trials. Diabetes Metab. Res. Rev. 2016, 32, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Xue, W.; Liang, S.; Zhao, J.; Zhang, X. Acute caffeine ingestion reduces insulin sensitivity in healthy subjects: A systematic review and meta-analysis. Nutr. J. 2016, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Efthimiou, O.; Debray, T.P.; van Valkenhoef, G.; Trelle, S.; Panayidou, K.; Moons, K.G.; Reitsma, J.B.; Shang, A.; Salanti, G.; GetReal Methods Review Group. GetReal in network meta-analysis: A review of the methodology. Res. Synth. Methods 2016, 7, 236–263. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.A.; Barbui, C.; Cipriani, A.; Brambilla, P.; Watanabe, N. Imputing missing standard deviations in meta-analyses can provide accurate results. J. Clin. Epidemiol. 2006, 59, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Jackson, D.; Barrett, J.K.; Lu, G.; Ades, A.E.; White, I.R. Consistency and inconsistency in network meta-analysis: Concepts and models for multi-arm studies. Res. Synth. Methods 2012, 3, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.; Bradburn, M.; Deeks, J.; Harbord, R.; Altman, D.; Sterne, J. Metan: Fixed- and random-effects meta-analysis. Stata J. 2008, 8, 3–28. [Google Scholar] [CrossRef]
- Harbord, R.M.; Higgins, J.P.T. Meta-regression in Stata. Stata J. 2008, 8, 493–519. [Google Scholar] [CrossRef]
- White, I.R. Network meta-analysis. Stata J. 2015, 15, 951–985. [Google Scholar] [CrossRef]
- van Dam, R.M.; Pasman, W.J.; Verhoef, P. Effects of coffee consumption on fasting blood glucose and insulin concentrations: Randomized controlled trials in healthy volunteers. Diabetes Care 2004, 27, 2990–2992. [Google Scholar] [CrossRef] [PubMed]
- Wedick, N.M.; Brennan, A.M.; Sun, Q.; Hu, F.B.; Mantzoros, C.S.; van Dam, R.M. Effects of caffeinated and decaffeinated coffee on biological risk factors for type 2 diabetes: A randomized controlled trial. Nutr. J. 2011, 10, 93. [Google Scholar] [CrossRef] [PubMed]
- Ohnaka, K.; Ikeda, M.; Maki, T.; Okada, T.; Shimazoe, T.; Adachi, M.; Nomura, M.; Takayanagi, R.; Kono, S. Effects of 16-week consumption of caffeinated and decaffeinated instant coffee on glucose metabolism in a randomized controlled trial. J. Nutr. Metab. 2012, 2012, 207426. [Google Scholar] [CrossRef] [PubMed]
- Shaposhnikov, S.; Hatzold, T.; Yamani, N.; Stavro, P.; Lorenzo, Y.; Dusinska, M.; Reus, A.; Pasman, W.; Collins, A. Coffee and oxidative stress: A human intervention study. Eur. J. Nutr. 2016. [Google Scholar] [CrossRef] [PubMed]
- Duffy, S.J.; Keaney, J.F., Jr.; Holbrook, M.; Gokce, N.; Swerdloff, P.L.; Frei, B.; Vita, J.A. Short- and long-term black tea consumption reverses endothelial dysfunction in patients with coronary artery disease. Circulation 2001, 104, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; MacDermott, K.; Vinson, J.A.; Oyama, N.; Manning, W.J.; Mittleman, M.A. A 6-month randomized pilot study of black tea and cardiovascular risk factors. Am. Heart J. 2007, 154, 724.e1–724.e6. [Google Scholar] [CrossRef] [PubMed]
- Bahorun, T.; Luximon-Ramma, A.; Neergheen-Bhujun, V.S.; Gunness, T.K.; Googoolye, K.; Auger, C.; Crozier, A.; Aruoma, O.I. The effect of black tea on risk factors of cardiovascular disease in a normal population. Prev. Med. 2012, 54, S98–S102. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.C.; Koo, M.W.; Ng, E.H.; Tang, O.S.; Yeung, W.S.; Ho, P.C. Effects of Chinese green tea on weight, and hormonal and biochemical profiles in obese patients with polycystic ovary syndrome—A randomized placebo-controlled trial. J. Soc. Gynecol. Investig. 2006, 13, 63–68. [Google Scholar] [CrossRef]
- Diepvens, K.; Kovacs, E.M.; Vogels, N.; Westerterp-Plantenga, M.S. Metabolic effects of green tea and of phases of weight loss. Physiol. Behav. 2006, 87, 185–191. [Google Scholar] [CrossRef]
- Ryu, O.H.; Lee, J.; Lee, K.W.; Kim, H.Y.; Seo, J.A.; Kim, S.G.; Kim, N.H.; Baik, S.H.; Choi, D.S.; Choi, K.M. Effects of green tea consumption on inflammation, insulin resistance and pulse wave velocity in type 2 diabetes patients. Diabetes Res. Clin. Pract. 2006, 71, 356–358. [Google Scholar] [CrossRef]
- Fukino, Y.; Ikeda, A.; Maruyama, K.; Aoki, N.; Okubo, T.; Iso, H. Randomized controlled trial for an effect of green tea-extract powder supplementation on glucose abnormalities. Eur. J. Clin. Nutr. 2008, 62, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Sanchez, K.; Leyva, M.J.; Wu, M.; Betts, N.M.; Aston, C.E.; Lyons, T.J. Green tea supplementation affects body weight, lipids, and lipid peroxidation in obese subjects with metabolic syndrome. J. Am. Coll. Nutr. 2010, 29, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei, K.; Hosseinzadeh-Attar, M.J.; Hossein-Nezhad, A.; Karimi, M.; Kamalinejad, M.; Jafari, N.; Najmafshar, A.; Karimi, F.; Eshraghian, M.R.; Mohammadzadeh, N.; et al. Visfatin genotype may influence the effects of green tea extract (Camellia sinensis) in Type 2 diabetes patients. Double blind placebo-controlled clinical trial study. Gazz. Med. Ital. 2010, 169, 137–147. [Google Scholar]
- Suliburska, J.; Bogdanski, P.; Szulinska, M.; Stepien, M.; Pupek-Musialik, D.; Jablecka, A. Effects of green tea supplementation on elements, total antioxidants, lipids, and glucose values in the serum of obese patients. Biol. Trace Elem. Res. 2012, 149, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Vieira Senger, A.E.; Schwanke, C.H.; Gomes, I.; Valle Gottlieb, M.G. Effect of green tea (Camellia sinensis) consumption on the components of metabolic syndrome in elderly. J. Nutr. Health Aging 2012, 16, 738–742. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.H.; Spicer, D.; Stanczyk, F.Z.; Tseng, C.C.; Yang, C.S.; Pike, M.C. Effect of 2-month controlled green tea intervention on lipoprotein cholesterol, glucose, and hormone levels in healthy postmenopausal women. Cancer Prev. Res. 2012, 5, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Toolsee, N.A.; Aruoma, O.I.; Gunness, T.K.; Kowlessur, S.; Dambala, V.; Murad, F.; Googoolye, K.; Daus, D.; Indelicato, J.; Rondeau, P.; et al. Effectiveness of green tea in a randomized human cohort: Relevance to diabetes and its complications. Biomed. Res. Int. 2013, 2013, 412379. [Google Scholar] [CrossRef]
- Lasaite, L.; Spadiene, A.; Savickiene, N.; Skesters, A.; Silova, A. The effect of Ginkgo biloba and Camellia sinensis extracts on psychological state and glycemic control in patients with type 2 diabetes mellitus. Nat. Prod. Commun. 2014, 9, 1345–1350. [Google Scholar]
- Shin, C.M.; Lee, D.H.; Seo, A.Y.; Lee, H.J.; Kim, S.B.; Son, W.-C.C.; Kim, Y.K.; Lee, S.J.; Park, S.-H.H.; Kim, N.; et al. Green tea extracts for the prevention of metachronous colorectal polyps among patients who underwent endoscopic removal of colorectal adenomas: A randomized clinical trial. Clin. Nutr. 2017. [Google Scholar] [CrossRef]
- Brown, A.L.; Lane, J.; Holyoak, C.; Nicol, B.; Mayes, A.E.; Dadd, T. Health effects of green tea catechins in overweight and obese men: A randomised controlled cross-over trial. Br. J. Nutr. 2011, 106, 1880–1889. [Google Scholar] [CrossRef]
- Hsu, C.H.; Liao, Y.L.; Lin, S.C.; Tsai, T.H.; Huang, C.J.; Chou, P. Does supplementation with green tea extract improve insulin resistance in obese type 2 diabetics? A randomized, double-blind, and placebo-controlled clinical trial. Altern. Med. Rev. 2011, 16, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Belcaro, G.; Ledda, A.; Hu, S.; Cesarone, M.R.; Feragalli, B.; Dugall, M. Greenselect phytosome for borderline metabolic syndrome. Evid. Based Complement. Alternat. Med. 2013, 2013, 869061. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Y.; Huang, C.J.; Huang, L.H.; Chen, I.J.; Chiu, J.P.; Hsu, C.H. Effects of green tea extract on insulin resistance and glucagon-like peptide 1 in patients with type 2 diabetes and lipid abnormalities: A randomized, double-blinded, and placebo-controlled trial. PLoS ONE 2014, 9, e91163. [Google Scholar] [CrossRef] [PubMed]
- Dostal, A.M.; Samavat, H.; Espejo, L.; Arikawa, A.Y.; Stendell-Hollis, N.R.; Kurzer, M.S. Green Tea Extract and Catechol-O-Methyltransferase Genotype Modify Fasting Serum Insulin and Plasma Adiponectin Concentrations in a Randomized Controlled Trial of Overweight and Obese Postmenopausal Women. J. Nutr. 2016, 146, 38–45. [Google Scholar] [CrossRef]
- Lu, P.H.; Hsu, C.H. Does supplementation with green tea extract improve acne in post-adolescent women? A randomized, double-blind, and placebo-controlled clinical trial. Complement. Ther. Med. 2016, 25, 159–163. [Google Scholar] [CrossRef]
- Hosoda, K.; Wang, M.F.; Liao, M.L.; Chuang, C.K.; Iha, M.; Clevidence, B.; Yamamoto, S. Antihyperglycemic effect of oolong tea in type 2 diabetes. Diabetes Care 2003, 26, 1714–1718. [Google Scholar] [CrossRef]
- Shimada, K.; Kawarabayashi, T.; Tanaka, A.; Fukuda, D.; Nakamura, Y.; Yoshiyama, M.; Takeuchi, K.; Sawaki, T.; Hosoda, K.; Yoshikawa, J. Oolong tea increases plasma adiponectin levels and low-density lipoprotein particle size in patients with coronary artery disease. Diabetes Res. Clin. Pract. 2004, 65, 227–234. [Google Scholar] [CrossRef]
- Eng, Q.Y.; Thanikachalam, P.V.; Ramamurthy, S. Molecular understanding of Epigallocatechin gallate (EGCG) in cardiovascular and metabolic diseases. J. Ethnopharmacol. 2018, 210, 296–310. [Google Scholar] [CrossRef]
- Waltner-Law, M.E.; Wang, X.L.; Law, B.K.; Hall, R.K.; Nawano, M.; Granner, D.K. Epigallocatechin gallate, a constituent of green tea, represses hepatic glucose production. J. Biol. Chem. 2002, 277, 34933–34940. [Google Scholar] [CrossRef]
- Ortsater, H.; Grankvist, N.; Wolfram, S.; Kuehn, N.; Sjoholm, A. Diet supplementation with green tea extract epigallocatechin gallate prevents progression to glucose intolerance in db/db mice. Nutr. Metab. 2012, 9, 11. [Google Scholar] [CrossRef]
- Ueda, M.; Nishiumi, S.; Nagayasu, H.; Fukuda, I.; Yoshida, K.; Ashida, H. Epigallocatechin gallate promotes GLUT4 translocation in skeletal muscle. Biochem. Biophys. Res. Commun. 2008, 377, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Fu, Z.; Zhen, W.; Yuskavage, J.; Liu, D. Epigallocatechin gallate delays the onset of type 1 diabetes in spontaneous non-obese diabetic mice. Br. J. Nutr. 2011, 105, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- U.K. Prospective Diabetes Study Group. U.K. Prospective Diabetes Study 16: Overview of 6 Years’ Therapy of Type II Diabetes: A Progressive Disease. Diabetes 1995, 44, 1249–1258. [Google Scholar] [CrossRef]
- Saisho, Y. Beta-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J. Diabetes 2015, 6, 109–124. [Google Scholar] [CrossRef] [PubMed]
- Higdon, J.V.; Frei, B. Coffee and health: A review of recent human research. Crit. Rev. Food Sci. Nutr. 2006, 46, 101–123. [Google Scholar] [CrossRef] [PubMed]
- van Dam, R.M.; Willett, W.C.; Manson, J.E.; Hu, F.B. Coffee, caffeine, and risk of type 2 diabetes: A prospective cohort study in younger and middle-aged U.S. women. Diabetes Care 2006, 29, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Bhupathiraju, S.N.; Chen, M.; van Dam, R.M.; Hu, F.B. Caffeinated and decaffeinated coffee consumption and risk of type 2 diabetes: A systematic review and a dose-response meta-analysis. Diabetes Care 2014, 37, 569–586. [Google Scholar] [CrossRef] [PubMed]
- Lofvenborg, J.E.; Andersson, T.; Carlsson, P.O.; Dorkhan, M.; Groop, L.; Martinell, M.; Rasouli, B.; Storm, P.; Tuomi, T.; Carlsson, S. Coffee consumption and the risk of latent autoimmune diabetes in adults—Results from a Swedish case-control study. Diabetes Med. 2014, 31, 799–805. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).