Comparison of Accuracy of NUTRIC and Modified NUTRIC Scores in Predicting 28-Day Mortality in Patients with Sepsis: A Single Center Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Participants
3.2. Discrepancy between Scores
3.3. 28-Day Mortality According to Score
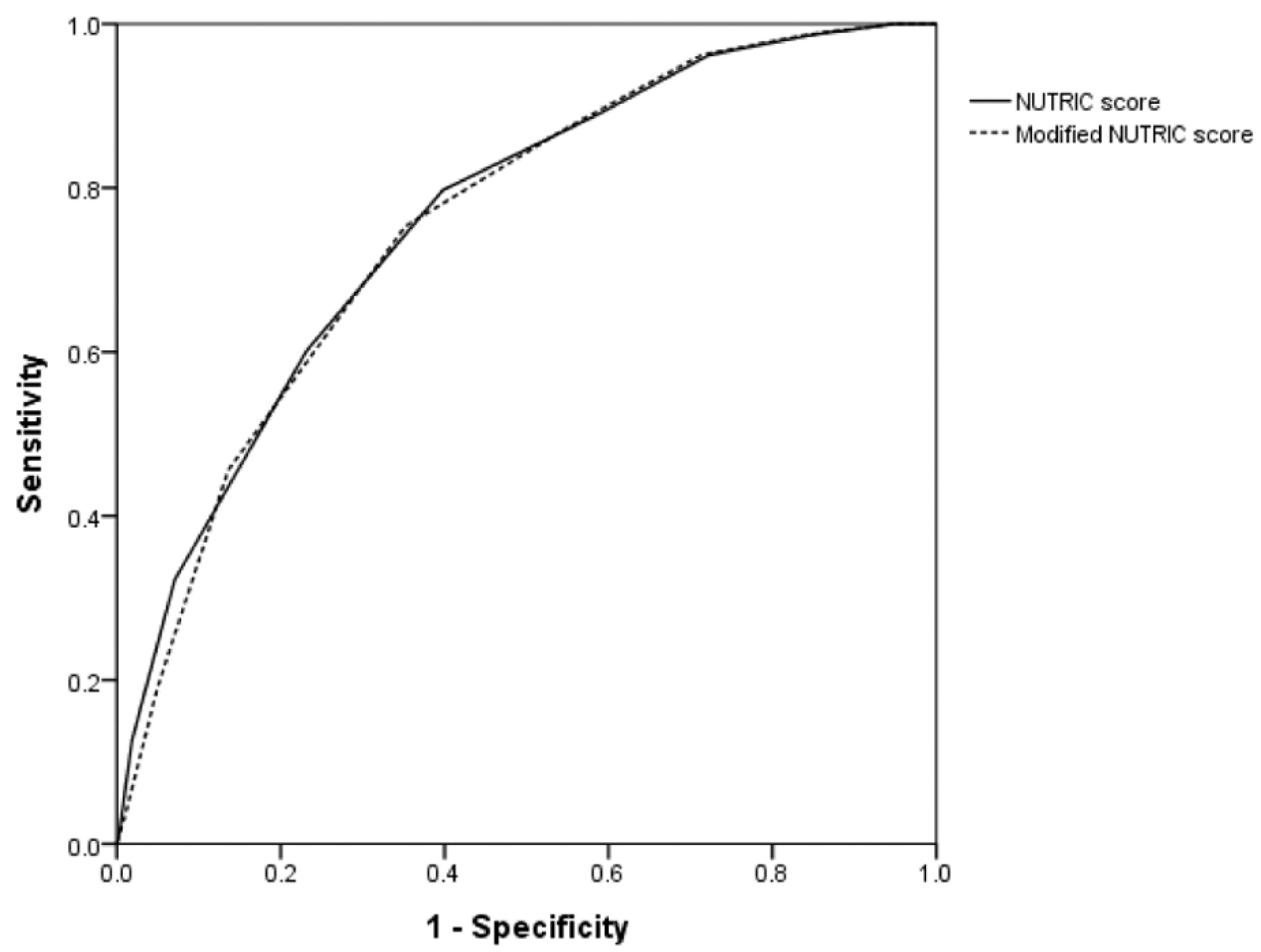
3.4. Area under the Curve of Scores for Predicting 28-Day Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Villet, S.; Chiolero, R.L.; Bollmann, M.D.; Revelly, J.P.; Cayeux, R.N.M.; Delarue, J.; Berger, M.M. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin. Nutr. 2005, 24, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Doig, G.S.; Simpson, F.; Finfer, S.; Delaney, A.; Davies, A.R.; Mitchell, I.; Dobb, G. Effect of evidence-based feeding guidelines on mortality of critically ill adults: A cluster randomized controlled trial. JAMA 2008, 300, 2731–2741. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.M.; Veyres, P.; Pivot, X.; Soummer, A.M.; Jambou, P.; Filippi, J.; van Obberghen, E.; Hebuterne, X. Malnutrition is an independent factor associated with nosocomial infections. Br. J. Nutr. 2004, 92, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Pirlich, M.; Schuetz, T.; Lochs, H.; Pichard, C. Is nutritional depletion by nutritional risk index associated with increased length of hospital stay? A population-based study. J. Parent. Enter. Nutr. 2004, 28, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Giner, M.; Laviano, A.; Meguid, M.M.; Gleason, J.R. In 1995 a correlation between malnutrition and poor outcome in critically ill patients still exists. Nutrition 1996, 12, 23–29. [Google Scholar] [CrossRef]
- McClave, S.A.; Taylor, B.E.; Martindale, R.G.; Warren, M.M.; Johnson, D.R.; Braunschweig, C.; McCarthy, M.S.; Davanos, E.; Rice, T.W.; Cresci, G.A.; et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of critical care medicine (sccm) and American society for parenteral and enteral nutrition (a.S.P.E.N.). J. Parent. Enter. Nutr. 2016, 40, 159–211. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, C.; Scherag, A.; Adhikari, N.K.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.J.; Bao, S.; Napolitano, J.R.; Burris, D.L.; Yu, L.; Tridandapani, S.; Knoell, D.L. Zinc regulates the acute phase response and serum amyloid a production in response to sepsis through JAK-STA3 signaling. PLoS ONE 2014, 9, e94934. [Google Scholar] [CrossRef]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Tappenden, K.A.; Quatrara, B.; Parkhurst, M.L.; Malone, A.M.; Fanjiang, G.; Ziegler, T.R. Critical role of nutrition in improving quality of care: An interdisciplinary call to action to address adult hospital malnutrition. J. Parent. Enter. Nutr. 2013, 37, 482–497. [Google Scholar] [CrossRef] [PubMed]
- Detsky, A.S.; McLaughlin, J.R.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? 1987. Classical article. Nutr. Hosp. 2008, 23, 400–407. [Google Scholar] [PubMed]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Kruizenga, H.M.; Seidell, J.C.; de Vet, H.C.; Wierdsma, N.J. Development and validation of a hospital screening tool for malnutrition: The short nutritional assessment questionnaire (SANQ). Clin. Nutr. 2005, 24, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Heyland, D.K.; Dhaliwal, R.; Jiang, X.; Day, A.G. Identifying critically ill patients who benefit the most from nutrition therapy: The development and initial validation of a novel risk assessment tool. Crit. Care 2011, 15, R268. [Google Scholar] [CrossRef] [PubMed]
- Ozbilgin, S.; Hanci, V.; Omur, D.; Ozbilgin, M.; Tosun, M.; Yurtlu, S.; Kucukguclu, S.; Arkan, A. Morbidity and mortality predictivity of nutritional assessment tools in the postoperative care unit. Medicine 2016, 95, e5038. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Hasan, R.M.; Agarwala, R.; Martin, C.; Day, A.G.; Heyland, D.K. Identifying critically-ill patients who will benefit most from nutritional therapy: Further validation of the “modified nutric” nutritional risk assessment tool. Clin. Nutr. 2016, 35, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.; Policarpo, S.; Fortuna, P.; Alves, M.; Virella, D.; Heyland, D.K. Nutritional risk assessment and cultural validation of the modified nutric score in critically ill patients-a multicenter prospective cohort study. J. Crit. Care 2017, 37, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, A.; Henry, J.; Ong, V.; Leong, C.S.; Teh, A.L.; van Dam, R.M.; Kowitlawakul, Y. Association of modified nutric score with 28-day mortality in critically ill patients. Clin. Nutr. 2016. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef] [PubMed]
- Reignier, J.; Boisrame-Helms, J.; Brisard, L.; Lascarrou, J.B.; Ait Hssain, A.; Anguel, N.; Argaud, L.; Asehnoune, K.; Asfar, P.; Bellec, F.; et al. Enteral versus parenteral early nutrition in ventilated adults with shock: A randomised, controlled, multicentre, open-label, parallel-group study (nutrirea-2). Lancet 2018, 391, 133–143. [Google Scholar] [CrossRef]
- Alberda, C.; Gramlich, L.; Jones, N.; Jeejeebhoy, K.; Day, A.G.; Dhaliwal, R.; Heyland, D.K. The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. Intensive Care Med. 2009, 35, 1728–1737. [Google Scholar] [CrossRef] [PubMed]
- Artinian, V.; Krayem, H.; DiGiovine, B. Effects of early enteral feeding on the outcome of critically ill mechanically ventilated medical patients. Chest 2006, 129, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Arabi, Y.M.; Aldawood, A.S.; Al-Dorzi, H.M.; Tamim, H.M.; Haddad, S.H.; Jones, G.; McIntyre, L.; Solaiman, O.; Sakkijha, M.H.; Sadat, M.; et al. Permissive underfeeding or standard enteral feeding in high- and low-nutritional-risk critically ill adults. Post hoc analysis of the permit trial. Am. J. Respir. Crit. Care Med. 2017, 195, 652–662. [Google Scholar] [CrossRef] [PubMed]
- Compher, C.; Chittams, J.; Sammarco, T.; Nicolo, M.; Heyland, D.K. Greater protein and energy intake may be associated with improved mortality in higher risk critically ill patients: A multicenter, multinational observational study. Crit. Care Med. 2017, 45, 156–163. [Google Scholar] [CrossRef] [PubMed]


| Variable | NUTRIC Score (n = 482) | Modified NUTRIC Score (n = 482) | ||||
|---|---|---|---|---|---|---|
| Low Score (n = 227) | High Score (n = 255) | p-Value | Low Score (n = 166) | High Score (n = 316) | p-Value | |
| Age, years | 63 (52–72) | 68 (57–75) | <0.001 | 62 (48–71) | 68 (57–75) | <0.001 |
| Height, cm | 163 (158–170) | 163 (155–170) | 0.175 | 163 (158–170) | 163 (155–170) | 0.456 |
| Weight, kg | 59 (52–66) | 58 (51–67) | 0.945 | 59 (52–67) | 59 (52–66) | 0.842 |
| BMI, kg/m2 | 23 (20–25) | 23 (20–25) | 0.456 | 23 (20–25) | 22 (20–25) | 0.827 |
| Female, n (%) | 68 (30) | 86 (33.7) | 0.376 | 52 (31.3) | 102 (32.3) | 0.831 |
| APACHE II score | 16 (13–20) | 27 (22–32) | <0.001 | 15 (12–18) | 25 (21–31) | <0.001 |
| SOFA score | 7 (5–10) | 13 (11–16) | <0.001 | 6 (5–9) | 12 (10–15) | <0.001 |
| Days from hospital to ICU | 0 (0–0) | 0 (0–9) | <0.001 | 0 (0–0) | 0 (0–8) | <0.001 |
| Co-morbidities | 1 (1–2) | 2 (1–3) | <0.001 | 1 (1–2) | 2 (1–3) | <0.001 |
| IL-6, pg/mL | 71 (21–169) | 366 (54–1910) | <0.001 | |||
| LOS in ICU, days | 5 (3–9) | 9 (4–17) | <0.001 | 5 (3–9) | 8 (4–17) | <0.001 |
| MV | 102 (44.9) | 210 (82.4) | <0.001 | 65 (20.8) | 247 (78.2) | <0.001 |
| Vasopressor use | 172(75.8) | 245 (96.1) | <0.001 | 123 (74.1) | 294 (93.0) | <0.001 |
| RRT | 26 (11.5) | 126 (49.4) | <0.001 | 17 (10.2) | 135 (42.7) | <0.001 |
| Diagnosis | 0.693 | 0.465 | ||||
| Respiratory disease | 103 (45.4) | 118 (46.3) | 69 (41.6) | 152 (48.1) | ||
| Liver/GI disease | 60 (26.4) | 63 (24.7) | 48 (28.9) | 75 (23.7) | ||
| Cardiovascular disease | 4 (1.8) | 6 (2.4) | 2 (1.2) | 8 (2.5) | ||
| Renal disease | 22 (9.7) | 18 (7.1) | 17 (10.2) | 23 (7.3) | ||
| Febrile neutropenia | 14 (6.2) | 14 (5.5) | 9 (5.4) | 19 (6) | ||
| SSTI | 10 (4.4) | 10 (3.9) | 9 (5.4) | 11 (3.5) | ||
| Other | 14 (6.2) | 26 (10.2) | 12 (7.2) | 28 (8.9) | ||
| NUTRIC Score | mNUTRIC Score (Cutoff = 5) | p-Value | mNUTRIC Score (Cutoff = 6) | p-Value | |
|---|---|---|---|---|---|
| Sensitivity | 0.797 | 0.873 | <0.001 | 0.753 | 0.016 |
| Specificity | 0.602 | 0.451 | <0.001 | 0.648 | <0.001 |
| Youden index | 0.399 | 0.324 | 0.401 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, D.H.; Hong, S.-B.; Lim, C.-M.; Koh, Y.; Seo, J.; Kim, Y.; Min, J.-Y.; Huh, J.W. Comparison of Accuracy of NUTRIC and Modified NUTRIC Scores in Predicting 28-Day Mortality in Patients with Sepsis: A Single Center Retrospective Study. Nutrients 2018, 10, 911. https://doi.org/10.3390/nu10070911
Jeong DH, Hong S-B, Lim C-M, Koh Y, Seo J, Kim Y, Min J-Y, Huh JW. Comparison of Accuracy of NUTRIC and Modified NUTRIC Scores in Predicting 28-Day Mortality in Patients with Sepsis: A Single Center Retrospective Study. Nutrients. 2018; 10(7):911. https://doi.org/10.3390/nu10070911
Chicago/Turabian StyleJeong, Dae Hyun, Sang-Bum Hong, Chae-Man Lim, Younsuck Koh, Jarim Seo, Younkyoung Kim, Ji-Yeon Min, and Jin Won Huh. 2018. "Comparison of Accuracy of NUTRIC and Modified NUTRIC Scores in Predicting 28-Day Mortality in Patients with Sepsis: A Single Center Retrospective Study" Nutrients 10, no. 7: 911. https://doi.org/10.3390/nu10070911
APA StyleJeong, D. H., Hong, S.-B., Lim, C.-M., Koh, Y., Seo, J., Kim, Y., Min, J.-Y., & Huh, J. W. (2018). Comparison of Accuracy of NUTRIC and Modified NUTRIC Scores in Predicting 28-Day Mortality in Patients with Sepsis: A Single Center Retrospective Study. Nutrients, 10(7), 911. https://doi.org/10.3390/nu10070911





