Effectiveness of a Locally Produced, Fish-Based Food Product on Weight Gain among Cambodian Children in the Treatment of Acute Malnutrition: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Setting
2.2. Trial Population
2.3. Ethical Considerations
2.4. Trial Design
2.5. Data Collection and Follow-Up
2.6. Treatment Protocol
2.7. RUTFs Used in the Trial
2.8. Sample Size and Outcome of Interest
2.9. Statistical Analysis
3. Results
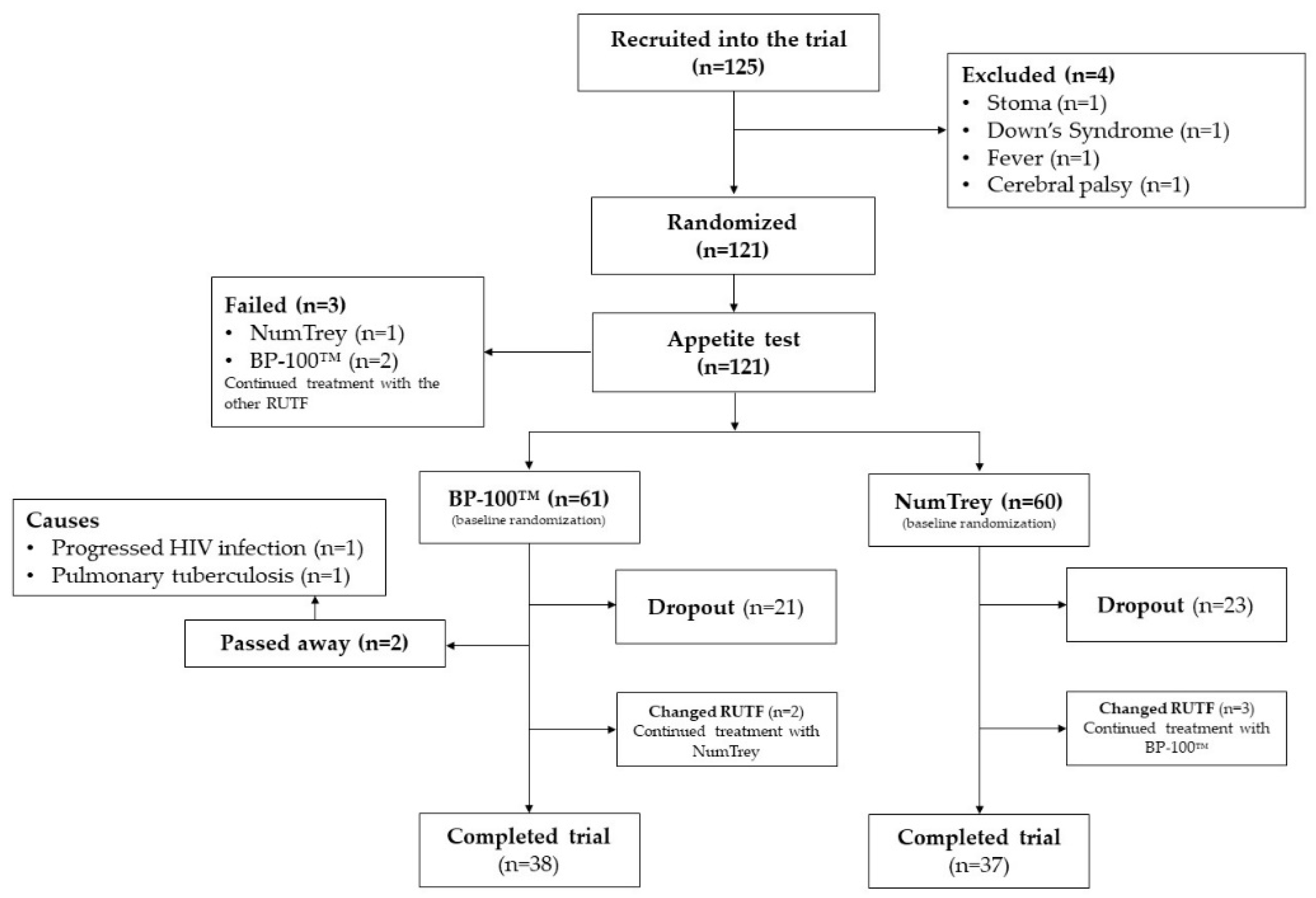
3.1. Participants
3.2. The Effectiveness of the Intervention on Anthropometric Changes
3.2.1. Primary Outcome Weight Gain g/kg/day
3.2.2. Analysis of Secondary Outcomes
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CI | Confidence interval |
| CMAM | Community-based management of acute malnutrition |
| HAZ | Height-for-age z-score |
| HIV | Human immunodeficiency virus |
| MAM | Moderate acute malnutrition |
| MUAC | Mid-upper-arm circumference |
| RUTF | Ready-to-use-therapeutic food |
| SAM | Severe acute malnutrition |
| SD | Standard deviation |
| SE | Standard Error |
| UNICEF | United Nations Children’s Fund |
| WAZ | Weight-for-age z-score |
| WHZ | Weight-for-height z-score |
| WHO | World Health Organization |
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-Mcgregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- World Health Organization and United Nations Children’s Fund. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children; A Joint Statement by the World Health Organization and the United Nations Children’s Fund; World Health Organization: Geneva, Switzerland; United Nations Children’s Fund: New York, NY, USA, 2009. [Google Scholar]
- Food and Agriculture Organization. Cambodia Country Fact Sheet on Food and Agriculture Policy Trends; Food and Agriculture Policy Decision Analysis: Phnom Penh, Cambodia, 2014. [Google Scholar]
- National Institute of Statistics, Directorate General for Health and ICF International. Cambodia Demographic and Health Survey 2014; National Institute of Statistics, Directorate General for Health: Phnom Penh, Cambodia; ICF International: Rockville, MD, USA, 2015. [Google Scholar]
- Harris, S.; Jack, S. Home-based treatment of acute malnutrition in Cambodian urban poor communities. Food Nutr. Bull. 2011, 32, 333–339. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Management of Severe Malnutrition: A Manual for Physicians and Other Senior Health Workers; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar] [CrossRef]
- Diop, E.H.I.; Dossou, N.I.; Ndour, M.M.; Briend, A.; Wade, S. Comparison of the efficacy of a solid ready-to-use food and a liquid, milk-based diet for the rehabilitation of severely malnourished children: A randomized trial. Am. J. Clin. Nutr. 2003, 78, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.; Sadler, K.; Dent, N.; Khara, T.; Guerrero, S.; Myatt, M.; Saboya, M.; Walsh, A. Key issues in the success of community-based management of severe malnutrition. Food Nutr. Bull. 2006, 27, 49–82. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.; Dent, N.; Binns, P.; Bahwere, P.; Sadler, K.; Hallam, A. Management of severe acute malnutrition in children. Lancet 2006, 368, 1992–2000. [Google Scholar] [CrossRef]
- World Health Organization, World Food Programme, System Standing Committee on Nutrition and United Nations Children’s Fund. Community-Based Management of Severe Acute Malnutrition; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Briend, A.; Lacsala, R.; Prudhon, C.; Mounier, B.; Grellety, Y.; Golden, M.H.N. Ready-to-use therapeutic food for treatment of marasmus. Lancet 1999, 353, 1767–1768. [Google Scholar] [CrossRef]
- Bourdier, F. Socio-Anthropological Investigation Related to the Acceptability of Plumpy’nut in Cambodia; Institut de Recherce Pour le Développement: Phnom Penh, Cambodia, 2009. [Google Scholar]
- National Nutrition Program. Results from the Initial Demonstration of RUTF for the Treatment of Acute Malnutrition in Cambodian Children; National Nutrition Program: Phnom Penh, Cambodia, 2009. [Google Scholar]
- Ketsana, C. Draft Report of Rutf Acceptability Trial in Prey Veng; RACHA and IRD: Phnom Penh, Cambodia, 2013; unpublished. [Google Scholar]
- Roos, N.; Wahab, M.A.; Chamnan, C.; Thilsted, S.H. The role of fish in food-based strategies to combat vitamin A and mineral deficiencies in developing countries. J. Nutr. 2007, 137, 1106–1109. [Google Scholar] [CrossRef] [PubMed]
- Skau, J.K.H.; Touch, B.; Chhoun, C.; Chea, M.; Unni, U.S.; Makurat, J.; Filteau, S.; Wieringa, F.T.; Dijkhuizen, M.A.; Ritz, C.; et al. Effects of animal source food and micronutrient fortification in complementary food products on body composition, iron status, and linear growth: A randomized trial in Cambodia. Am. J. Clin. Nutr. 2015, 101, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Sigh, S.; Roos, N.; Sok, D.; Borg, B.; Chamnan, C.; Laillou, A.; Dijkhuizen, A.M.; Wieringa, T.F. Development and acceptability of locally-made fish-based, ready-to-use products for the prevention and treatment of malnutrition in Cambodia. Food Nutr. Bull. 2018, in press. [Google Scholar]
- World Health Organization. Guideline. Updates on the Management of Severe Acute Malnutrition in Infants and Children; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Food and Nutrition Techincal Assistance. Community-Based Management of Acute Malnutrition: Trainer’s Guide. Outpatient Care for the Management of SAM without Medical Complications. 2008. Available online: https://www.fantaproject.org/sites/default/files/resources/CMAM_Training_Mod4_ENGLISH_Nov2008.pdf (accessed on 21 June 2018).
- Wilcox, A.B.; Gallagher, K.D.; Boden-albala, B.; Bakken, S.R. Research Data Collection Methods: From Paper to Tablet Computers from Paper to Tablet Computers. Med. Care 2012, 50, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Leisher, C. A Comparison of Tablet-Based and Paper-Based Survey Data Collection in Conservation Projects. Soc. Sci. 2014, 3, 264–271. [Google Scholar] [CrossRef]
- National Nutrition Program. National Interim Guidelines for the Management of Acute Malnutrition; National Nutrition Program: Phnom Penh, Cambodia, 2011. [Google Scholar]
- Ministry of Health Cambodia. Community Engagement Handbook. Guidelines for the Treatment of Acute Malnutrition; Ministry of Health: Phnom Penh, Cambodia, 2018.
- Ministry of Health Cambodia. Guidelines for Inpatient Treatment of Severe Acute Malnutrition; Ministry of Health: Phnom Penh, Cambodia, 2018.
- Ministry of Health Cambodia. Guidelines for the Outpatient Treatment of Severe Acute Malnutrition; Ministry of Health: Phnom Penh, Cambodia, 2018.
- Peters, R. Development and Acceptability of a Fish-Based Local Ready-to-Use- Therapeutic Food (RUTF): An Intervention in Pre-School Children in Cambodia. Master’s Thesis, University of Copenhagen, Copenhagen, Denmark, 15 October 2014. [Google Scholar]
- World Health Organization; United Nations Children’s Fund; System Standing Committee on Nutrition. WHO, UNICEF, and SCN Informal Consultation on Community-Based Management of Severe Malnutrition in Children. Nutr. Bull. 2006, 27, 1–108. [Google Scholar]
- World Health Organization; United Nations Children’s Fund; World Food Programme. Consultation on the Dietary Management of Moderate Malnutrition in children under 5 years of age. Nutr. Bull. 2009, 30, 200. [Google Scholar]
- Nguyen, M.; Nga, T.T.; Wieringa, F. Effectiveness Study of a Locally Made RUTF among Children with Moderate and Severe Acute Malnutrition under 5 Years Old in Kon Tum Province, Vietnam; Final Report for UNICEF Vietnam; Institut de recherche pour le développement: Hanoi, Vietnam, 2013. [Google Scholar]
- The R Foundation. R Sofware Program. Available online: https://www.r-project.org/ (accessed on 20 June 2018).
- Hollis, S.; Campbell, F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999, 319, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.G.; van der Pols, J.C.; Dobson, A.J. Regression to the mean: What it is and how to deal with it. Int. J. Epidemiol. 2005, 34, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Shewade, H.D.; Patro, B.K.; Bharti, B.; Soundappan, K.; Kaur, A.; Taneja, N. Effectiveness of indigenous ready-to-use therapeutic food in community-based management of uncomplicated severe acute malnutrition: A randomized controlled trial from India. J. Trop. Pediatr. 2013, 59, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, N.; Mohan, S.B.; Bose, A.; Iyengar, S.D.; Taneja, S.; Mazumder, S.; Pricilla, R.A.; Iyengar, K.; Sachdev, H.S.; Mohan, V.R.; et al. Efficacy of three feeding regimens for home-based management of children with uncomplicated severe acute malnutrition: A randomised trial in India Efficacy of three feeding regimens for home-based management of children with uncomplicated severe acute mal. BMJ Glob. Health 2016, 11, 1–12. [Google Scholar] [CrossRef]
- Ciliberto, M.A.; Sandige, H.; Ndekha, M.J.; Ashorn, P.; Briend, A.; Ciliberto, H.M.; Manary, M.J. Comparison of home-based therapy with ready-to-use therapeutic food with standard therapy in the treatment of malnourished Malawian children: A controlled, clinical effectiveness trial. Am. J. Clin. Nutr. 2005, 81, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Manary, M.J.; Ndkeha, M.J.; Ashorn, P.; Maleta, K.; Briend, A. Home based therapy for severe malnutrition with ready-to-use food. Arch. Dis. Child. 2004, 89, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Manary, M.; Chang, C.Y. Comparing Milk Fortified Corn-SoyBlend (CSB++), Soy Ready-to-Use Supplementary Food (RUSF), and Soy/Whey RUSF (Supplementary Plumpy®) in the Treatment of Moderate Acute Malnutrition; FANTA-2 BRIDGE/FHI 360: Washington, DC, USA, 2012.
- LaGrone, L.N.; Trehan, I.; Meuli, G.J.; Wang, R.J.; Thakwalakwa, C.; Maleta, K.; Manary, M.J. A novel fortified blended flour, corn-soy blend “plus-plus”, is not inferior to lipid-based ready-to-use supplementary foods for the treatment of moderate acute malnutrition in Malawian children. Am. J. Clin. Nutr. 2012, 95, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Sandige, H.; Ndekha, M.J.; Briend, A.; Ashorn, P.; Manary, M.J. Home-based treatment of malnourished Malawian children with locally produced or imported ready-to-use food. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Linneman, Z.; Matilsky, D.; Ndekha, M.; Manary, M.J.; Maleta, K.; Manary, M.J. A large-scale operational study of home-based therapy with ready-to-use therapeutic food in childhood malnutrition in Malawi. Matern. Child Nutr. 2007, 3, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Ndekha, M.J.; Manary, M.J.; Ashorn, P.; Briend, A. Home-based therapy with ready-to-use therapeutic food is of benefit to malnourished, HIV-infected Malawian children. Acta Paediatr. Int. J. Paediatr. 2005, 94, 222–225. [Google Scholar] [CrossRef]
- Bahwere, P.; Banda, T.; Sadler, K.; Nyirenda, G.; Owino, V.; Shaba, B.; Dibari, F.; Collins, S. Effectiveness of milk whey protein-based ready-to-use therapeutic food in treatment of severe acute malnutrition in Malawian under-5 children: A randomised, double-blind, controlled non-inferiority clinical trial. Matern. Child Nutr. 2014, 10, 436–451. [Google Scholar] [CrossRef] [PubMed]
- Nackers, F.; Broillet, F.; Oumarou, D.; Djibo, A.; Gaboulaud, V.; Guerin, P.J.; Rusch, B.; Grais, R.F.; et al. Effectiveness of ready-to-use therapeutic food compared to a corn/soy-blend-based pre-mix for the treatment of childhood moderate acute malnutrition in Niger. J. Trop. Pediatr. 2010, 56, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Gaboulaud, V.; Dan-Bouzoua, N.; Brasher, C.; Fedida, G.; Gergonne, B.; Brown, V. Could nutritional rehabilitation at home complement or replace centre-based therapeutic feeding programmes for severe malnutrition? J. Trop. Pediatr. 2007, 53, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Ashworth, A. Efficacy and effectiveness of community-based treatment of severe malnutrition. Food Nutr. Bull. 2006, 27, 24–48. [Google Scholar] [CrossRef] [PubMed]
- Tadesse, A.W.; Tadesse, E.; Berhane, Y.; Ekström, E.C. Choosing anthropometric indicators to monitor the response to treatment for severe acute malnutrition in rural southern Ethiopia—Empirical evidence. Nutrients 2017, 9, 8–10. [Google Scholar] [CrossRef] [PubMed]
- Amthor, R.E.; Cole, S.M.; Manary, M.J. The Use of Home-Based Therapy with Ready-to-Use Therapeutic Food to Treat Malnutrition in a Rural Area during a Food Crisis. J. Am. Diet. Assoc. 2009, 109, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Schoonees, A.; Lombard, M.; Musekiwa, A.; Nel, E.; Volmink, J. Ready-to-use therapeutic food for home-based treatment of severe acute malnutrition in children from six months to five years of age (Review). Cochrane Database Syst. Rev. 2013, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yebyo, H.G.; Kendall, C.; Nigusse, D.; Lemma, W. Outpatient Therapeutic Feeding Program Outcomes and Determinants in Treatment of Severe Acute Malnutrition in Tigray, Northern Ethiopia: A Retrospective Cohort Study. PLoS ONE 2013, 8, e65840. [Google Scholar] [CrossRef] [PubMed]
- Forsén, E.; Tadesse, E.; Berhane, Y.; Ekström, E. Predicted implications of using percentage weight gain as single discharge criterion in management of acute malnutrition in rural southern Ethiopia. Matern. Child Nutr. 2015, 11, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Myatt, M.; Khara, T.; Collins, S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr. Bull. 2006, 27, 7–23. [Google Scholar] [CrossRef] [PubMed]
- Mwangome, M.K.; Fegan, G.; Mbunya, R.; Prentice, A.M.; Berkley, J.A. Reliability and accuracy of anthropometry performed by community health workers among infants under 6 months in rural Kenya. Trop. Med. Int. Health 2012, 17, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Dale, N.M.; Myatt, M.; Prudhon, C. Using Mid-Upper Arm Circumference to End Treatment of Severe Acute Malnutrition Leads to Higher Weight Gains in the Most Malnourished Children. PLoS ONE 2013, 8, e55404. [Google Scholar] [CrossRef] [PubMed]
- Laillou, A.; Prak, S.; De Groot, R.; Whitney, S.; Conkle, J.; Horton, L.; Un, S.O.; Dijkhuizen, M.A.; Wieringa, F.T. Optimal Screening of Children with Acute Malnutrition Requires a Change in Current WHO Guidelines as MUAC and WHZ Identify Different Patient Groups. PLoS ONE 2014, 9, e101159. [Google Scholar] [CrossRef] [PubMed]
- Tadesse, A.W.; Tadesse, E.; Berhane, Y.; Ekström, E.C. Comparison of mid-upper arm circumference and weight-for-height to diagnose severe acute malnutrition: A study in Southern Ethiopia. Nutrients 2017, 9, 267. [Google Scholar] [CrossRef] [PubMed]
- Walters, T.; Sibson, V.; McGrath, M. Mid Upper Arm Circumference and Weight-for-Height Z-Score as Indicators of Severe Acute Malnutrition: A Consultation of Operational Agencies and Academic Specialists to Understand the Evidence, Identify Knowledge Gaps and to Inform Operational Guidance. Available online: http://files.ennonline.net/attachments/1398/muac-wfh-reportweb.pdf (accessed on 20 June 2018).
- James, P.T.; Van den Briel, N.; Rozet, A.; Israël, A.-D.; Fenn, B.; Navarro-Colorado, C. Low-dose RUTF protocol and improved service delivery lead to good programme outcomes in the treatment of uncomplicated SAM: A programme report from Myanmar. Matern. Child Nutr. 2015, 11, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Burza, S.; Mahajan, R.; Marino, E.; Sunyoto, T.; Shandilya, C.; Tabrez, M.; Kumari, K.; Mathew, P.; Jha, A.; Salse, N.; Mishra, K.N. Community-based management of severe acute malnutrition in Indiaë: New evidence from Bihar 1–3. Am. J. Clin. Nutr. 2015, 101, 847–859. [Google Scholar] [CrossRef] [PubMed]
- Tharkur, G.S.; Singh, H.P.; Patel, C. Locally-prepared ready-to-use therapeutic food for children with severe acute malnutrition: A controlled trial. Indian Pediatr. 2013, 50, 295–299. [Google Scholar] [CrossRef]
- Ciliberto, M.; Manary, M.; Ndekha, M.; Briend, A.; Ashorn, P. Home-based therapy for oedematous malnutrition with ready-to-use therapeutic food. Acta Paediatr. Int. J. Paediatr. 2006, 95, 1012–1015. [Google Scholar] [CrossRef] [PubMed]
- Maust, A.; Koroma, A.S.; Abla, C.; Molokwu, N.; Ryan, K.N.; Singh, L.; Manary, M.J. Severe and Moderate Acute Malnutrition Can Be Successfully Managed with an Integrated Protocol in Sierra Leone. J. Nutr. 2015, 145, 2604–2609. [Google Scholar] [CrossRef] [PubMed]
- Collins, S. Treating severe acute malnutrition seriously. Arch. Dis. Child. 2007, 92, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Homann, A.M.; Ayieko, M.A.; Konyole, S.O.; Roos, N. Acceptability of biscuits containing 10% cricket (Acheta domesticus) compared to milk biscuits among 5-10-year-old Kenyan schoolchildren. J. Insects Food Feed 2017, 1, 1–9. [Google Scholar] [CrossRef]
- Som, S.; Prak, S.; Laillou, A.; Gauthier, L.; Berger, J.; Poirot, E.; Wieringa, F. Diets and Feeding Practices during the First 1000 Days Window in the Phnom Penh and North Eastern Districts of Cambodia. Nutrients 2018, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.P.; Barker, M. Why is changing health-related behaviour so difficult? Public Health 2016, 136, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Corace, K.; Garber, G. When knowledge is not enough: Changing behavior to change vaccination results. Hum. Vaccines Immunother. 2014, 10, 2623–2624. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.G.; Higgins, P.D.R.; Waljee, A.K. A primer on effectiveness and efficacy trials. Clin. Transl. Gastroenterol. 2014, 5, 1–4. [Google Scholar] [CrossRef] [PubMed]
| NumTrey Paste Only | NumTrey Paste and Wafer | BP-100™ | UN Requirements | |
|---|---|---|---|---|
| Macronutrients | ||||
| Energy (Kcal) | 531 | 506 | 529 | 520–550 |
| Protein/Total energy (%) | 11.3 | 9.7 | 11.1 | 10–12 |
| Fat/Total energy (%) | 56.2 | 49.6 | 51.6 | 45–60 |
| Omega-6/Energy ratio (%) | 15 | - | - | 3–10 |
| Omega-3/Energy ratio (%) | 3.6 | - | - | 0.3–2.5 |
| Vitamins | ||||
| Vitamin A (mg) | 1.1 | 0.8 | 0.9 | 0.8–1.1 |
| Vitamin D (µg) | 16.7 | 11.7 | 18 | 15–20 |
| Vitamin E (mg) | 19 | 13.3 | 27 | ≥20 |
| Vitamin K (µg) | 24.9 | 17.4 | 21 | 15–30 |
| Thiamine (Vitamin B1) (mg) | 0.5 | 0.4 | 0.5 | ≥0.5 |
| Riboflavin (Vitamin B2) (mg) | 1.6 | 1.1 | 1.8 | ≥1.6 |
| Vitamin C (mg) | 56.1 | 39.3 | 54 | ≥50 |
| Vitamin B6 (mg) | 0.7 | 0.5 | 0.7 | ≥0.6 |
| Cobalamin (Vitamin B12) (µg) | 1.6 | 1.1 | 1.6 | ≥1.6 |
| Folic acid (µg) | 355 | 249 | 225 | ≥200 |
| Niacin (mg) | 5.8 | 4.1 | 5.8 | ≥5 |
| Pantothenic acid (mg) | 3.8 | 2.7 | 3 | ≥3 |
| Biotin (Vitamin B7) (µg) | 135 | 94.5 | 70 | ≥60 |
| Minerals | ||||
| Calcium (mg) | 313 | 219 | 470 | 300–600 |
| Sodium (mg) | 11.8 | 8.26 | <290 | ≤290 |
| Potassium (mg) | 1104 | 773 | 1100 | 1100–1400 |
| Phosphorus (mg) | 424 | 297 | 470 | 300–600 |
| Magnesium (mg) | 125 | 88 | 110 | 80–140 |
| Iron (mg) | 8.2 | 5.8 | 10 | 10–14 |
| Zinc (mg) | 10.8 | 7.6 | 12 | 11–14 |
| Copper (mg) | 1.6 | 1.1 | 1.5 | 1.4–1.8 |
| Selenium (µg) | 29.3 | 20.5 | 25 | 20–40 |
| Iodine (µg) | 112.8 | 79.0 | 110 | 70–140 |
| Weight (kg) | Wafers or Bars per Day | |
|---|---|---|
| BP-100TM | NumTrey | |
| Bar | Wafer | |
| 3.0–3.4 | 2 | 17 |
| 3.5–4.9 | 2.5 | 20 |
| 5.0–6.9 | 4 | 27 |
| 7.0–9.9 | 5 | 40 |
| 10.0–14.0 | 6 | 53 |
| 14.0–19.0 | 9.5 | 79 |
| 19.0–23.0 | 13 | 106 |
| 23.0–30.0 | 16 | 131 |
| >30.0 | 200 kcal/kg/day | 200 kcal/kg/day |
| BP-100™ (61) | NumTrey (60) * | All Patients (121) | |
|---|---|---|---|
| Socio-demographic parameters | |||
| Patient age, months | 19.7 (12.3) | 22.7 (15.1) | 21.2 (13.8) |
| Breastfeeding, % (n) | 49.2 (30) | 45.0 (27) | 47.1 (57) |
| Gender | |||
| Female, % (n) | 34.4 (21) | 48.3 (29) | 41.3 (50) |
| Male, % (n) | 65.6 (40) | 51.7 (31) | 58.6 (71) |
| Child living with family, % (n) | 96.7 (59) | 95.0 (57) | 95.9 (116) |
| Ethnicity | |||
| Khmer, % (n) | 73.8 (45) | 86.7 (52) | 80.2 (97) |
| Main caregiver | |||
| Biological mother, % (n) | 73.8 (45) | 75.0 (45) | 74.4 (90) |
| Nutrition parameters | |||
| Baseline weight, kg | 7.32 (1.61) | 7.71 (2.02) | 7.51 (1.83) |
| Baseline height, cm | 74.8 (9.2) | 77.3 (10.8) | 76.0 (10.0) |
| Baseline MUAC, mm | 118 (9.0) | 119 (7.3) | 118 (8.2) |
| Baseline weight-for-height, z-score | −2.9 (0.7) | −3.0 (0.6) | −3.0 (0.6) |
| Baseline weight-for-age, z-score | −3.3 (0.9) | −3.2 (0.8) | −3.3 (0.8) |
| Baseline height-for-age, z-score | −2.3 (1.3) | −2.1 (1.4) | −2.2 (1.4) |
| Infectious parameters | |||
| HIV positive, % (n) | 1.6 (1) | - | 0.8 (1) |
| Diarrhea, % (n)1 | 31.1 (19) | 25.0 (15) | 28.1 (34) |
| Fever, % (n)1 | 67.2 (41) | 60.0 (36) | 63.6 (77) |
| Lost appetite, % (n) 1 | 6.6 (4) | 13.3 (8) | 9.9 (12) |
| Effectiveness Analysis | Efficacy Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Follow-Up Visits | BP-100™ | NumTrey | Difference *,1 | p-Value | BP-100™ | NumTrey | Difference *,1 | p-Value | |
| Weight (kg) | Baseline | 7.51 ± 0.11 (61) | 7.64 ± 0.11 (60) | −0.14 ± 0.16 | 0.388 | 7.58 ± 0.91 (60) | 7.58 ± 0.90 (61) | 0.08 ± 0.09 | 0.927 |
| Week 2 follow-up | 7.62 ± 0.12 (43) | 7.78 ± 0.11 (45) | −0.02 ± 0.06 | 0.749 | 7.69 ± 0.94 (41) | 7.71 ± 0.91 (47) | 0.03 ± 0.06 | 0.584 | |
| Week 4 follow-up | 7.61 ± 0.12 (33) | 7.84 ± 0.11 (37) | −0.09 ± 0.07 | 0.168 | 7.68 ± 0.95 (34) | 7.77 ± 0.94 (36) | 0.11 ± 0.07 | 0.110 | |
| Week 6 follow-up | 7.74 ± 0.12 (28) | 7.82 ± 0.11 (39) | 0.06 ± 0.07 | 0.399 | 7.80 ± 0.95 (29) | 7.75 ± 0.94 (38) | 0.04 ± 0.07 | 0.524 | |
| Endline | 7.79 ± 0.12 (38) | 7.94 ± 0.12 (37) | −0.01 ± 0.06 | 0.843 | 7.88 ± 0.94 (39) | 7.86 ± 0.94 (36) | 0.02 ± 0.07 | 0.779 | |
| MUAC (mm) | Baseline | 118 ± 1.0 (60) | 119 ± 0.1 (60) | −0.24 ± 1.4 | 0.862 | 118 ± 0.9 (60) | 119 ± 0.9 (60) | −0.11 ± 1.2 | 0.929 |
| Week 2 follow-up | 121 ± 1.1 (43) | 121 ± 1.0 (45) | 0.65 ± 1.2 | 0.574 | 121 ± 1.1 (41) | 121 ± 1.0 (47) | 0.86 ± 1.1 | 0.463 | |
| Week 4 follow-up | 122 ± 1.1 (33) | 121 ± 1.1 (37) | 1.19 ± 1.3 | 0.342 | 122 ± 1.1 (34) | 121 ± 1.1 (36) | 0.76 ± 1.3 | 0.549 | |
| Week 6 follow-up | 122 ± 1.2 (28) | 121 ± 1.1 (38) | 1.03 ± 1.3 | 0.429 | 122 ± 1.1 (28) | 121 ± 1.0 (38) | 1.25 ± 1.3 | 0.343 | |
| Endline | 123 ± 1.1 (38) | 121 ± 1.1 (36) | 2.10 ± 1.2 | 0.090 | 122 ± 1.0 (38) | 122 ± 1.1 (36) | 1.68 ±1.3 | 0.178 | |
| WHZ (z-score) | Baseline | −2.98 ± 0.09 (61) | −2.99 ± 0.09 (60) | 0.01 ± 0.12 | 0.905 | −2.97 ± 0.08 (60) | −3.00 ± 0.08 (61) | 0.04 ± 0.10 | 0.715 |
| Week 2 follow-up | −2.81 ± 0.09 (43) | −2.83 ± 0.09 (45) | 0.01 ± 0.09 | 0.952 | −2.82 ± 0.09 (41) | −2.82 ± 0.08 (47) | −0.04 ± 0.09 | 0.689 | |
| Week 4 follow-up | −2.92 ± 0.10 (33) | −2.75 ± 0.09 (37) | −0.19 ± 0.10 | 0.059 | −2.92 ± 0.09 (34) | −2.74 ± 0.09 (36) | −0.22 ± 0.10 | 0.028 | |
| Week 6 follow-up | −2.70 ± 0.10 (28) | −2.83 ± 0.09 (39) | 0.11 ± 0.10 | 0.255 | −2.73 ± 0.09 (29) | −2.81 ± 0.09 (38) | 0.04 ± 0.10 | 0.715 | |
| Endline | −2.68 ± 0.10 (38) | −2.55 ± 0.09 (37) | −0.14 ± 0.10 | 0.146 | −2.64 ± 0.09 (39) | −2.60 ± 0.09 (36) | −0.08 ± 0.10 | 0.424 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sigh, S.; Roos, N.; Chamnan, C.; Laillou, A.; Prak, S.; Wieringa, F.T. Effectiveness of a Locally Produced, Fish-Based Food Product on Weight Gain among Cambodian Children in the Treatment of Acute Malnutrition: A Randomized Controlled Trial. Nutrients 2018, 10, 909. https://doi.org/10.3390/nu10070909
Sigh S, Roos N, Chamnan C, Laillou A, Prak S, Wieringa FT. Effectiveness of a Locally Produced, Fish-Based Food Product on Weight Gain among Cambodian Children in the Treatment of Acute Malnutrition: A Randomized Controlled Trial. Nutrients. 2018; 10(7):909. https://doi.org/10.3390/nu10070909
Chicago/Turabian StyleSigh, Sanne, Nanna Roos, Chhoun Chamnan, Arnaud Laillou, Sophanneary Prak, and Frank T. Wieringa. 2018. "Effectiveness of a Locally Produced, Fish-Based Food Product on Weight Gain among Cambodian Children in the Treatment of Acute Malnutrition: A Randomized Controlled Trial" Nutrients 10, no. 7: 909. https://doi.org/10.3390/nu10070909
APA StyleSigh, S., Roos, N., Chamnan, C., Laillou, A., Prak, S., & Wieringa, F. T. (2018). Effectiveness of a Locally Produced, Fish-Based Food Product on Weight Gain among Cambodian Children in the Treatment of Acute Malnutrition: A Randomized Controlled Trial. Nutrients, 10(7), 909. https://doi.org/10.3390/nu10070909





