The Important Role of Carbohydrates in the Flavor, Function, and Formulation of Oral Nutritional Supplements
Abstract
1. Introduction
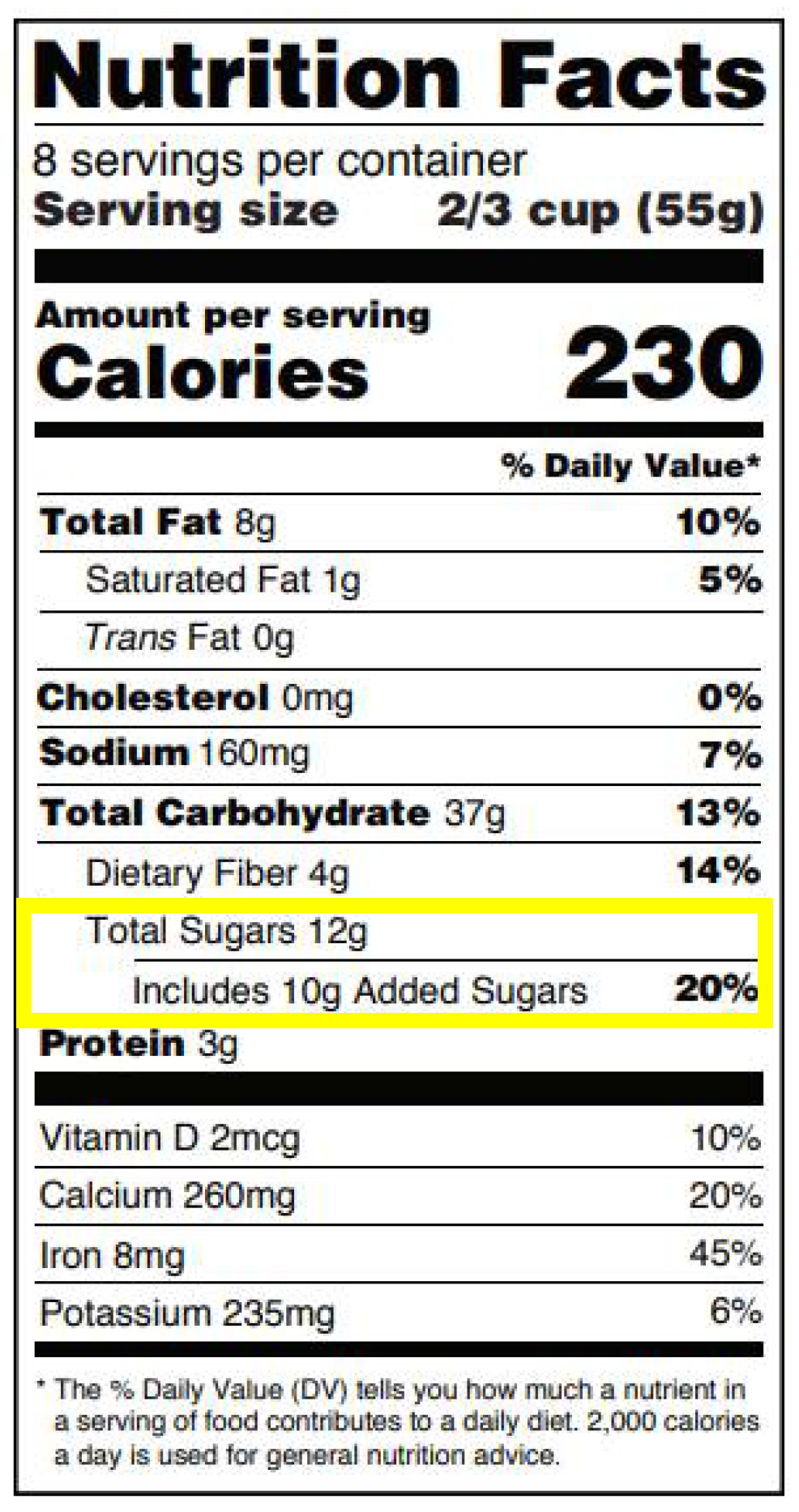
2. Health Policy Framework for Added Sugars
3. Added Carbohydrate in ONS
4. Taste and Flavor Roles of Carbohydrate in ONS
5. Functional Roles of Carbohydrate in ONS
5.1. Energy
5.2. Preventing the Utlization of Endogenous Energy Sources during Prolonged Fasting
6. Formulation Roles of Carbohydrate in ONS
6.1. Flavor Enhancement and Masking
6.2. Color and Flavor Formation
6.3. Texture
7. Summary
Author Contributions
Conflicts of Interest
References
- Stratton, R.J.; Elia, M. A review of reviews: a new look at the evidence for oral nutritional supplements in clinical practice. Clin. Nutr. Suppl. 2007, 2, 5–23. [Google Scholar] [CrossRef]
- Engfer, M.; Green, C. Oral Nutritional Supplement to Tackle Malnutrition: Summary Booklet. Medical Nutrition International Industry. Available online: http://www.file:///C:/Users/bronsal/Downloads/MNIBookletFINAL2911%20(2).pdf (accessed on 6 March 2018).
- Oral Nutritional Supplements. The British Association for Parenteral and Enteral Nutrition Website. Available online: http://www.bapen.org.uk/nutrition-support/nutrition-by-mouth/oral-nutritional-supplements (accessed on 10 May 2018).
- Absorption of Monosaccharides. Vivo Pathophysiology Website. Available online: http://www.vivo.colostate.edu/hbooks/pathphys/digestion/smallgut/absorb_sugars.html (accessed on 11 May 2018).
- Tierney, M.; Gallagher, A.; Giotis, E.S.; Pentieva, K. An online survey on consumer knowledge and understanding of added sugars. Nutrients 2017, 9, 37. [Google Scholar] [CrossRef] [PubMed]
- Know Your Limit for Added Sugars. Center for Disease Control and Prevention Website. Available online: http://www.cdc.gov/nutrition/data-statistics/know-your-limit-for-added-sugars.html (accessed on 9 May 2018).
- Clemens, R.A.; Jones, J.M.; Lee, S.Y.; Mayhew, E.J.; Slavin, J.; Zivanovic, S. Functionality of sugars in foods and health. Compr. Rev. Food Sci. Food Saf. 2016, 15, 433–470. [Google Scholar] [CrossRef]
- Dennis, B. FDA Says Consumers Should Have More Details about ‘Added Sugars’ in Foods. Washington Post. Available online: https://www.washingtonpost.com/news/to-your-health/wp/2015/07/24/should-consumers-have-details-about-added-sugar-in-foods-fda-says-yes/ (accessed on 9 May 2018).
- US Department of Health and Human Services; US Department of Agriculture. 2010 Dietary Guidelines for Americans, 7th ed.; US Department of Health and Human Services: Washington, DC, USA, 2010. Available online: https://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf (accessed on 2 April 2018).
- World Health Organization. WHO Calls on Countries to Reduce Sugars Intake among Adults and Children. Available online: http://www.who.int/mediacentre/news/releases/2015/sugar-guideline/en/ (accessed on 2 March 2018).
- US Department of Health and Human Services; US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; US Department of Health and Human Services: Washington, DC, USA, 2015. Available online: http://www.health.gov/DietaryGuidelines (accessed on 16 May 2018).
- Guideline: Sugar Intake for Adults and Children. World Health Organization. Available online: https://public.eblib.com/choice/publicfullrecord.aspx?p=2033879 (accessed on 10 May 2018).
- Changes to the Nutrition Facts Label. U.S. Food and Drug Administration Website. Available online: https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm385663.htm (accessed on 10 May 2018).
- Terrie, Y.C. Medical Food and Meal Replacement Nutritional Supplements. Pharmacy Times Website. Available online: http://www.pharmacytimes.com/publications/issue/2015/january2015/medical-food-and-meal-replacement-nutritional-supplements?p=2 (accessed on 10 May 2018).
- Therapeutic. Abbott Nutrition Website. Available online: https://abbottnutrition.com/therapeutic (accessed on 10 May 2018).
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Institute of Medicine. Available online: http://www.nationalacademies.org/hmd/Reports/2002/Dietary-Reference-Intakes-for-Energy-Carbohydrate-Fiber-Fat-Fatty-Acids-Cholesterol-Protein-and-Amino-Acids.aspx (accessed on 10 May 2018).
- Jensen, G. Oral nutritional supplementation. Am. J. Manag. Care 2013, 19, 119–120. [Google Scholar] [PubMed]
- Wilson, M.; Purushothaman, R.; Morley, J. Effect of liquid dietary supplements on energy intake. Am. J. Clin. Nutr. 2002, 75, 944–947. [Google Scholar] [CrossRef] [PubMed]
- Ruxton, C. Compliance with Oral Nutritional Supplements and the Role of Taste. CN Focus 2014, 6. Available online: https://www.nutrition2me.com/images/free-view-articles/free-downloads/ONSjuneCNFocus14.pdf (accessed on 8 December 2017).
- Hubbard, G.P.; Elia, M.; Holdoway, A.; Stratton, R.J. A systematic review of compliance to oral nutritional supplements. Clin. Nutr. Edinb. Scotl. 2012, 31, 293–312. [Google Scholar] [CrossRef] [PubMed]
- Darmon, P.; Karsegard, V.L.; Nardo, P.; Dupertuis, Y.M.; Pichard, C. Oral nutritional supplements and taste preferences: 545 days of clinical testing in malnourished in-patients. Clin. Nutr. 2008, 27, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Breslin, P.A.S. An evolutionary perspective on food and human taste. Curr. Biol. 2013, 23, R409–R418. [Google Scholar] [CrossRef] [PubMed]
- How Does Our Sense of Taste Work? PubMed Health Website. Available online: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072592/ (accessed on 9 May 2018).
- Hardy, K.; Brand-Miller, J.; Brown, K.D.; Thomas, M.G.; Copeland, L. The importance of dietary carbohydrate in human evolution. Q. Rev. Biol. 2015, 90, 251–268. [Google Scholar] [CrossRef] [PubMed]
- Tastes Differ: How Taste Preferences Develop. The European Food Information Council (EUFIC). Available online: http://www.eufic.org/en/food-today/article/tastes-differ-how-taste-preferences-develop (accessed on 30 August 2018).
- Auvray, M.; Spence, C. The multisensory perception of flavor. Conscious. Cogn. 2008, 17, 1016–1031. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, G.K.; Cowart, B.J. Congenital and experiential factors in the development of human flavor preferences. Appetite 1985, 6, 357–372. [Google Scholar] [CrossRef]
- Hoffman, J.; Ishii, E.; Macturk, R. Age-related changes in the prevalence of smell/taste problems among the United States adult population. Ann. N. Y. Acad. Sci. 1998, 855, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.M.; Bilash, I.; Zubek, J.P. The effect of age on taste sensitivity. J. Gerontol. 1959, 14, 56–58. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.C.; Cain, W.S.; Demarque, A.; Ruthruff, A.M. On the discrimination of missing ingredients: Aging and salt flavor. Appetite 1991, 16, 129–140. [Google Scholar] [CrossRef]
- Stevens, J.C. Detection of tastes in mixture with other tastes: Issues of masking and aging. Chem. Sens. 1996, 21, 211–221. [Google Scholar] [CrossRef]
- Schiffman, S.S. Perception of taste and smell in elderly persons. Crit. Rev. Food Sci. Nutr. 1993, 33, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, S.S. Taste and smell losses in normal aging and disease. JAMA 1997, 278, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Duffy, V.B.; Backstrand, J.R.; Ferris, A.M. Olfactory dysfunction and related nutritional risk in free-living, elderly women. J. Am. Diet. Assoc. 1995, 95, 879–884. [Google Scholar] [CrossRef]
- Arcavi, L.; Shahar, A. Drug related taste disturbances: Emphasis on the elderly. Harefuah 2003, 142, 446–450. [Google Scholar] [PubMed]
- Schiffman, S.S.; Gatlin, C.A. Clinical physiology of taste and smell. Annu. Rev. Nutr. 1993, 13, 405–436. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, S.S.; Graham, B.G.; Suggs, M.S.; Sattely-Miller, E.A. Effect of psychotropic drugs on taste responses in young and elderly persons. Ann. N. Y. Acad. Sci. 1998, 855, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Douglass, R.; Heckman, G. Drug-related taste disturbance. Can. Fam. Phys. 2010, 56, 1142–1147. [Google Scholar]
- Seiberling, K.A.; Conley, D.B. Aging and olfactory and taste function. Otolaryngol. Clin. N. Am. 2004, 37, 1209–1228. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.E. Principles of geriatric dentistry and their application to the older adult with a physical disability. Clin. Geriatr. Med. 2006, 22, 413–434. [Google Scholar] [CrossRef] [PubMed]
- Wrobel, B.B.; Leopold, D.A. Clinical assessment of patients with smell and taste disorders. Otolaryngol. Clin. N. Am. 2004, 37, 1127–1142. [Google Scholar] [CrossRef] [PubMed]
- Imoscopi, A.; Inelmen, E.M.; Sergi, G.; Miotto, F.; Manzato, E. Taste loss in the elderly: Epidemiology, causes and consequences. Aging Clin. Exp. Res. 2012, 24, 570–579. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.B.; Mouridsen, H.T.; Bergmann, O.J.; Reibel, J.; Brünner, N.; Nauntofte, B. Oral mucosal lesions, microbial changes, and taste disturbances induced by adjuvant chemotherapy in breast cancer patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, S.S. Intensification of sensory properties of foods for the elderly. J. Nutr. 2000, 130, 927S–930S. [Google Scholar] [CrossRef] [PubMed]
- Mathey, M.F.; Siebelink, E.; de Graaf, C.; Van Staveren, W.A. Flavor enhancement of food improves dietary intake and nutritional status of elderly nursing home residents. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M200–M205. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.; Snow, B. The Functions of Carbohydrates in the Body. In An Introduction to Nutrition. pp. 188–193. Available online: https://2012books.lardbucket.org/pdfs/an-introduction-to-nutrition.pdf (accessed on 16 May 2018).
- How Many Calories Are in one Gram of Fat, Carbohydrate, or Protein? United States Department of Agriculture’s National Agricultural Library Website. Available online: https://www.nal.usda.gov/fnic/how-many-calories-are-one-gram-fat-carbohydrate-or-protein (accessed on 10 May 2018).
- American Society of Hematology. Blood Basics. Available online: http://www.hematology.org/Patients/Basics/ (accessed on 30 August 2018).
- Nelms, M. Starvation, Underweight, Malnutrition and Eating Disorders. Lecture Presentation Slides; The Ohio State University: Columbus, OH, USA, 2017. [Google Scholar]
- Bonnans, S.; Noble, A.C. Effect of sweetener type and of sweetener and acid levels on temporal perception of sweetness, sourness and fruitiness. Chem. Sens. 1993, 18, 273–283. [Google Scholar] [CrossRef]
- Valdes, R.; Hinreiner, E.; Simone, M. Effect of sucrose and organic acids on apparent flavor intensity. Food Technol. 1956, 10, 282–285. [Google Scholar]
- VonSydow, E.; Moskowitz, H.; Jacobs, H.; Meiselman, H. Odor-taste interaction in fruit juices. Lebensm. Wiss. Technol. 1974, 7, 9–16. [Google Scholar]
- Chen, S.-D.; Ofoli, R.Y.; Scott, E.P.; Asmussen, J. Volatile retention in microwave freeze-dried model foods. J. Food Sci. 1993, 58, 1157–1161. [Google Scholar] [CrossRef]
- Sugisawa, H.; Kobayashi, N.; Sakagami, A. The retention of volatile flavors in food. Jpn. Soc. Food Sci. Technol. 1973, 20, 364–368. [Google Scholar] [CrossRef]
- Ehler, K.F.; Bernhard, R.A.; Nickerson, T.A. Heats of adsorption of small molecules on various forms of lactose, sucrose, and glucose. J. Agric. Food Chem. 1979, 27, 921–927. [Google Scholar] [CrossRef]
- Schifferstein, H.N.; Verlegh, P.W. The role of congruency and pleasantness in odor-induced taste enhancement. Acta Psychol. 1996, 94, 87–105. [Google Scholar] [CrossRef]
- Green, B.G.; Nachtigal, D.; Hammond, S.; Lim, J. Enhancement of retronasal odors by taste. Chem. Sens. 2012, 37, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Keast, R.S.J.; Breslin, P.A.S. An overview of binary taste–taste interactions. Food Qual. Prefer. 2003, 14, 111–124. [Google Scholar] [CrossRef]
- Goldfein, K.R.; Slavin, J.L. Why sugar is added to food: Food science 101. Compr. Rev. Food Sci. Food Saf. 2015, 14, 644–656. [Google Scholar] [CrossRef]
- Kerler, J.; Winkel, C.; Davidek, T.; Blank, I. Chapter 3: Basic chemistry and process conditions for reaction flavours with particular focus on maillard-type reactions. In Food Flavour Technology, 2nd ed.; Taylor, A.J., Linforth, R.S., Eds.; John Wiley & Sons, Inc.: Chichester, West Sussex, UK, 2010. [Google Scholar]
- Monte, W.; Maga, J. Flavor chemistry of sucrose. Sugar Technol. Rev. 1982, 8, 181–204. [Google Scholar]
- Colonna, W.; Samaraweera, U.; Clarke, M.; Cleary, M.; Godshall, M.; White, J.S. Sugar. In Kirk-Othmer Encyclopedia of Chemical Technology; John Wiley & Sons, Inc.: New York, NY, USA, 2006. [Google Scholar] [CrossRef]
- Billaud, C.; Adrian, J. Louis-camille maillard, 1878–1936. Food Rev. Int. 2003, 19, 345–374. [Google Scholar] [CrossRef]
- Reineccius, G. Flavor Chemistry and Technology, 2nd ed.; Taylor and Francis Group: Boca Raton, FL, USA, 2005. [Google Scholar]
- Chattopadhyay, S.; Raychaudhuri, U.; Chakraborty, R. Artificial sweeteners—A review. J. Food Sci. Technol. 2014, 51, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Dhartiben, B.K.; Aparnathi, K.D. Chemistry and use of artificial intense sweeteners. Int. J. Curr. Microbiol. App. Sci. 2017, 6, 1283–1296. [Google Scholar]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kokkinidou, S.; Peterson, D.; Bloch, T.; Bronston, A. The Important Role of Carbohydrates in the Flavor, Function, and Formulation of Oral Nutritional Supplements. Nutrients 2018, 10, 742. https://doi.org/10.3390/nu10060742
Kokkinidou S, Peterson D, Bloch T, Bronston A. The Important Role of Carbohydrates in the Flavor, Function, and Formulation of Oral Nutritional Supplements. Nutrients. 2018; 10(6):742. https://doi.org/10.3390/nu10060742
Chicago/Turabian StyleKokkinidou, Smaro, Devin Peterson, Tama Bloch, and Ashley Bronston. 2018. "The Important Role of Carbohydrates in the Flavor, Function, and Formulation of Oral Nutritional Supplements" Nutrients 10, no. 6: 742. https://doi.org/10.3390/nu10060742
APA StyleKokkinidou, S., Peterson, D., Bloch, T., & Bronston, A. (2018). The Important Role of Carbohydrates in the Flavor, Function, and Formulation of Oral Nutritional Supplements. Nutrients, 10(6), 742. https://doi.org/10.3390/nu10060742



