MOSH Syndrome (Male Obesity Secondary Hypogonadism): Clinical Assessment and Possible Therapeutic Approaches
Abstract
1. Introduction
2. Materials and Methods
2.1. Analysis of Blood Samples
2.2. Anthropometric Measurements
2.3. Dual-Energy X-ray Absorptiometry
2.4. Questionnaires
2.5. Nutritional Intervention
2.6. Physical Activity Program
2.7. Statistical Analysis
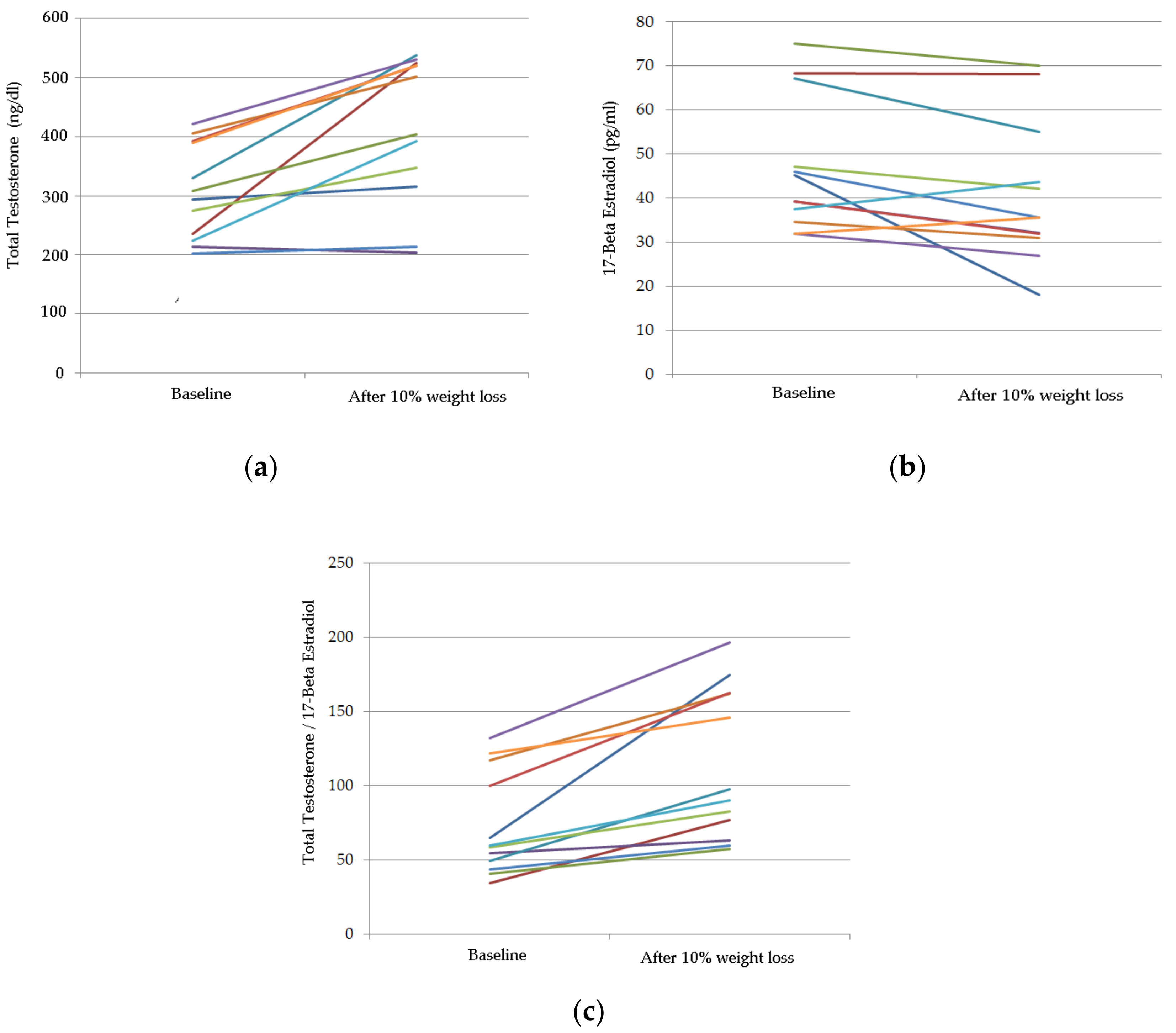
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- De Lorenzo, A.; Soldati, L.; Sarlo, F.; Calvani, M.; Di Lorenzo, N.; Di Renzo, L. New obesity classification criteria as a tool for bariatric surgery indication. World J. Gastroenterol. 2016, 22, 681–703. [Google Scholar] [CrossRef] [PubMed]
- Di Daniele, N.; Noce, A.; Vidiri, M.F.; Moriconi, E.; Marrone, G.; Annicchiarico-Petruzzelli, M.; D’Urso, G.; Tesauro, M.; Rovella, V.; De Lorenzo, A. Impact of Mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget 2017, 8, 8947–8979. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Nieschlag, E.; Hermann, M.; Nieschlag, S. Andrology: Male Reproductive Health and Dysfunction, 3rd ed.; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Hall, S.A.; Esche, G.R.; Araujo, A.B.; Travison, T.G.; Clark, R.V.; Williams, R.E.; McKinlay, J.B. Correlates of low testosterone and symptomatic androgen deficiency in a population-based sample. J. Clin. Endocrinol. Metab. 2008, 93, 3870–3877. [Google Scholar] [CrossRef] [PubMed]
- Gore, A.C.; Chappell, V.A.; Fenton, S.E.; Flaws, J.A.; Nadal, A.; Prins, G.S.; Toppari, J.; Zoeller, R.T. Edc-2: The endocrine society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev. 2015, 36, E1–E150. [Google Scholar] [CrossRef] [PubMed]
- Mihalca, R.; Fica, S. The impact of obesity on the male reproductive axis. J. Med. Life 2014, 7, 296–300. [Google Scholar] [PubMed]
- Skakkebaek, N.E.; Rajpert-De Meyts, E.; Buck Louis, G.M.; Toppari, J.; Andersson, A.M.; Eisenberg, M.L.; Jensen, T.K.; Jorgensen, N.; Swan, S.H.; Sapra, K.J.; et al. Male reproductive disorders and fertility trends: Influences of environment and genetic susceptibility. Physiol. Rev. 2016, 96, 55–97. [Google Scholar] [CrossRef] [PubMed]
- Canale, M.P.; Manca di Villahermosa, S.; Martino, G.; Rovella, V.; Noce, A.; De Lorenzo, A.; Di Daniele, N. Obesity-related metabolic syndrome: Mechanisms of sympathetic overactivity. Int. J. Endocrinol. 2013, 2013, 865965. [Google Scholar] [CrossRef] [PubMed]
- Caprio, M.; Isidori, A.M.; Carta, A.R.; Moretti, C.; Dufau, M.L.; Fabbri, A. Expression of functional leptin receptors in rodent leydig cells. Endocrinology 1999, 140, 4939–4947. [Google Scholar] [CrossRef] [PubMed]
- Nieschlag, E.; Behre, H.M.; Bouchard, P.; Corrales, J.J.; Jones, T.H.; Stalla, G.K.; Webb, S.M.; Wu, F.C. Testosterone replacement therapy: Current trends and future directions. Hum. Reprod. Update 2004, 10, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.J. Beneficial health effects of modest weight loss. Int. J. Obes. Relat. Metab. Disord. 1992, 16, 397–415. [Google Scholar] [PubMed]
- Pasanisi, F.; Contaldo, F.; de Simone, G.; Mancini, M. Benefits of sustained moderate weight loss in obesity. Nutr. Metab. Cardiovasc. Dis. 2001, 11, 401–406. [Google Scholar] [PubMed]
- Cohen, P.G. The hypogonadal-obesity cycle: Role of aromatase in modulating the testosterone-estradiol shunt—A major factor in the genesis of morbid obesity. Med. Hypotheses 1999, 52, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Schulster, M.; Bernie, A.M.; Ramasamy, R. The role of estradiol in male reproductive function. Asian J. Androl. 2016, 18, 435–440. [Google Scholar] [PubMed]
- Tremellen, K. Gut endotoxin leading to a decline in gonadal function (GELDING)—A novel theory for the development of late onset hypogonadism in obese men. Basic Clin. Androl. 2016, 26, 7. [Google Scholar] [CrossRef] [PubMed]
- Shang, T.; Zhang, X.; Wang, T.; Sun, B.; Deng, T.; Han, D. Toll-like receptor-initiated testicular innate immune responses in mouse leydig cells. Endocrinology 2011, 152, 2827–2836. [Google Scholar] [CrossRef] [PubMed]
- Dohle, G.R.; Arver, S.; Bettocchi, C.; Jones, T.H.; Kliesch, S. EAU guidelines in male hypogonadism. Eur. Assoc. Urol. 2015, 3, 242–252. [Google Scholar]
- Volkow, N.D.; O’Brien, C.P. Issues for DSM-V: Should obesity be included as a brain disorder? Am. J. Psychiatry 2007, 164, 708–710. [Google Scholar] [CrossRef] [PubMed]
- Cota, D.; Tschop, M.H.; Horvath, T.L.; Levine, A.S. Cannabinoids, opioids and eating behavior: The molecular face of hedonism? Brain Res. Rev. 2006, 51, 85–107. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, L.; Zimmermann, T.; Vermeulen, A.; Thiel, C. A new “aging male’s symptoms” (AMS) rating scale. Aging Male 1999, 2, 105–114. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the yale food addiction scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Dandona, P.; Rosenberg, M.T. A practical guide to male hypogonadism in the primary care setting. Int. J. Clin. Pract. 2010, 64, 682–696. [Google Scholar] [CrossRef] [PubMed]
- Bhasin, S.; Woodhouse, L.; Casaburi, R.; Singh, A.B.; Bhasin, D.; Berman, N.; Chen, X.; Yarasheski, K.E.; Magliano, L.; Dzekov, C.; et al. Testosterone dose-response relationships in healthy young men. Am. J. Physiol. Endocrinol. Metab. 2001, 281, E1172–E1181. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.; Roche, A.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Press: Champaing, IL, USA, 1998. [Google Scholar]
- Nuttall, F.Q. Body mass index: Obesity, BMI, and health: A critical review. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Madden, A.M.; Smith, S. Body composition and morphological assessment of nutritional status in adults: A review of anthropometric variables. J. Hum. Nutr. Diet. 2016, 29, 7–25. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Bianchi, A.; Maroni, P.; Iannarelli, A.; Di Daniele, N.; Iacopino, L.; Di Renzo, L. Adiposity rather than BMI determines metabolic risk. Int. J. Cardiol. 2013, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, L.A.; Saad, F.; Zimmermann, T.; Novak, A.; Myon, E.; Badia, X.; Potthoff, P.; T’Sjoen, G.; Pollanen, P.; Goncharow, N.P.; et al. The aging males’ symptoms (AMS) scale: Update and compilation of international versions. Health Qual. Life Outcomes 2003, 1, 15. [Google Scholar] [CrossRef] [PubMed]
- Innamorati, M.; Imperatori, C.; Manzoni, G.M.; Lamis, D.A.; Castelnuovo, G.; Tamburello, A.; Tamburello, S.; Fabbricatore, M. Psychometric properties of the Italian yale food addiction scale in overweight and obese patients. Eat. Weight Disord. 2015, 20, 119–127. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Tagliabue, A.; Andreoli, A.; Testolin, G.; Comelli, M.; Deurenberg, P. Measured and predicted resting metabolic rate in Italian males and females, aged 18–59 y. Eur. J. Clin. Nutr. 2001, 55, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Wyatt, H.R.; Peters, J.C. Energy balance and obesity. Circulation 2012, 126, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Associazione Medici Diabetologi. Standard Italiani per la Cura del Diabete Mellito; Società Italiana di Diabetologia (SID): Roma, Italy, 2016. [Google Scholar]
- Kaur, J. A comprehensive review on metabolic syndrome. Cardiol. Res. Pract. 2014, 2014, 943162. [Google Scholar] [CrossRef] [PubMed]
- Donohoe, C.L.; Doyle, S.L.; Reynolds, J.V. Visceral adiposity, insulin resistance and cancer risk. Diabetol. Metab. Syndr. 2011, 3, 12. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.V.; Kolka, C.M.; Kim, S.P.; Bergman, R.N. Obesity, insulin resistance and comorbidities? Mechanisms of association. Arq. Bras. Endocrinol. Metabol. 2014, 58, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Toomey, C.M.; McCormack, W.G.; Jakeman, P. The effect of hydration status on the measurement of lean tissue mass by dual-energy X-ray absorptiometry. Eur. J. Appl. Physiol. 2017, 117, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Noce, A.; Vidiri, M.F.; Marrone, G.; Moriconi, E.; Bocedi, A.; Capria, A.; Rovella, V.; Ricci, G.; De Lorenzo, A.; Di Daniele, N. Is low-protein diet a possible risk factor of malnutrition in chronic kidney disease patients? Cell Death Discov. 2016, 2, 16026. [Google Scholar] [CrossRef] [PubMed]
- Carrelli, A.; Bucovsky, M.; Horst, R.; Cremers, S.; Zhang, C.; Bessler, M.; Schrope, B.; Evanko, J.; Blanco, J.; Silverberg, S.J.; et al. Vitamin D storage in adipose tissue of obese and normal weight women. J. Bone Miner. Res. 2017, 32, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Annalisa, N.; Alessio, T.; Claudette, T.D.; Erald, V.; Antonino de, L.; Nicola, D.D. Gut microbioma population: An indicator really sensible to any change in age, diet, metabolic syndrome, and life-style. Mediators Inflamm. 2014, 2014, 901308. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K. Muscle as a secretory organ. Compr. Physiol. 2013, 3, 1337–1362. [Google Scholar] [PubMed]
- Mazur-Bialy, A.I.; Bilski, J.; Pochec, E.; Brzozowski, T. New insight into the direct anti-inflammatory activity of a myokine irisin against proinflammatory activation of adipocytes. Implication for exercise in obesity. J. Physiol. Pharmacol. 2017, 68, 243–251. [Google Scholar] [PubMed]
- Jastroch, M.; Oelkrug, R.; Keipert, S. Insights into brown adipose tissue evolution and function from non-model organisms. J. Exp. Biol. 2018, 221. [Google Scholar] [CrossRef] [PubMed]
- Armamento-Villareal, R.; Aguirre, L.E.; Qualls, C.; Villareal, D.T. Effect of lifestyle intervention on the hormonal profile of frail, obese older men. J. Nutr. Health Aging 2016, 20, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Stanik, S.; Dornfeld, L.P.; Maxwell, M.H.; Viosca, S.P.; Korenman, S.G. The effect of weight loss on reproductive hormones in obese men. J. Clin. Endocrinol. Metab. 1981, 53, 828–832. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Rastrelli, G.; Monami, M.; Saad, F.; Luconi, M.; Lucchese, M.; Facchiano, E.; Sforza, A.; Forti, G.; Mannucci, E.; et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: A systematic review and meta-analysis. Eur. J. Endocrinol. 2013, 168, 829–843. [Google Scholar] [CrossRef] [PubMed]
- Woodard, G.; Ahmed, S.; Podelski, V.; Hernandez-Boussard, T.; Presti, J., Jr.; Morton, J.M. Effect of roux-en-Y gastric bypass on testosterone and prostate-specific antigen. Br. J. Surg. 2012, 99, 693–698. [Google Scholar] [CrossRef] [PubMed]
| (1) Demographic and Anthropometrical Parameters: | |
| Age (years) | 46.6 ± 14 (min 25; max 63) |
| BMI (kg/m2) | 36.2 ± 7.6 (min 26.9; max 51.5) |
| (2) Blood Parameters: | |
| Total Testosterone (ng/dL) | 300.2 ± 79.5 |
| 17-Beta Estradiol (pg/mL) | 48.3 ± 14.9 |
| TT/E2 | 68.6 ± 32.6 |
| LH (mIU/mL) | 6.2 ± 1.2 |
| SHBG (nmol/L) | 21.5 ± 8.8 |
| Prolactin (ng/mL) | 11.9 ± 2.7 |
| HOMAi | 4.1 ± 2.3 |
| 25-OH vitamin D (ng/mL) | 11.3 ± 7.4 |
| ColT/HDL | 4.6 ± 1.2 |
| LDL/HDL | 3.1 ± 1.1 |
| TG/HDL | 2.7 ± 0.9 |
| Body Composition Parameters | Baseline | After 10% Weight Loss | p Value | 95% CI |
|---|---|---|---|---|
| Weight (kg) | 109.3 ± 20.5 | 100.8 ± 19.6 | 0.0001 | 0.6; 8.0 |
| BMI (kg/m2) | 36.2 ± 7.6 | 33.4 ± 7.4 | 0.0001 | 0.5; 1.7 |
| WHR | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.052 | 0.01; 0.00 |
| Total FM% | 39.2 ± 6.4 | 36.2 ± 5.8 | 0.0001 | 22.5; 62.3 |
| Android FM% | 51.5 ± 6.8 | 47.6 ± 6.8 | 0.001 | 0.6; 1.8 |
| Gynoid FM% | 39.2 ± 6.2 | 36.5 ± 6.3 | 0.0001 | 0.9; 2.0 |
| FM L2-L5 (kg) | 7.33 ± 2.7 | 6.0 ± 2.4 | 0.0001 | 0.4; 1.8 |
| Total FM (kg) | 42.3 ± 11.8 | 36.8 ± 9.9 | 0.0001 | 0.1; −0.3 |
| Total FFM (kg) | 62.3 ± 8.2 | 60.3 ± 7.7 | 0.002 | 45.0; 93.0 |
| A/G | 1.29 ± 0.08 | 1.31 ± 0.09 | 0.784 | 22.1; 86.9 |
| BMD (g/cm2) | 1.4 ± 0.5 | 1.4 ± 0.4 | 0.359 | 0.1; −0.3 |
| Patient Group | |||
|---|---|---|---|
| Baseline (%) | After 10% Weight Loss (%) | p (McNemar’s Test) | |
| Prevalence of food addiction | 54.5 | 9.1 | 0.063 |
| Prevalence of every symptom: | |||
| A. Substance taken in larger amount and for a longer period than intended | 36.4 | 0 | 0.125 |
| B. Persistent desire or repeated unsuccessful attempt to quit | 36.4 | 54.5 | 0.500 |
| C. Much time/activity required to obtain, use, and recover | 18.2 | 27.3 | 0.500 |
| D. Important social, occupational, or recreational activities given up or reduced | 54.5 | 18.2 | 0.250 |
| E. Use continues despite knowledge of adverse consequences | 27.3 | 9.1 | 0.063 |
| F. Tolerance | 18.2 | 0 | 0.500 |
| G. Withdrawal | 9.1 | 0 | 1 |
| H. Clinically significant impairment | 36.4 | 9.1 | 0.250 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Lorenzo, A.; Noce, A.; Moriconi, E.; Rampello, T.; Marrone, G.; Di Daniele, N.; Rovella, V. MOSH Syndrome (Male Obesity Secondary Hypogonadism): Clinical Assessment and Possible Therapeutic Approaches. Nutrients 2018, 10, 474. https://doi.org/10.3390/nu10040474
De Lorenzo A, Noce A, Moriconi E, Rampello T, Marrone G, Di Daniele N, Rovella V. MOSH Syndrome (Male Obesity Secondary Hypogonadism): Clinical Assessment and Possible Therapeutic Approaches. Nutrients. 2018; 10(4):474. https://doi.org/10.3390/nu10040474
Chicago/Turabian StyleDe Lorenzo, Antonino, Annalisa Noce, Eleonora Moriconi, Tiziana Rampello, Giulia Marrone, Nicola Di Daniele, and Valentina Rovella. 2018. "MOSH Syndrome (Male Obesity Secondary Hypogonadism): Clinical Assessment and Possible Therapeutic Approaches" Nutrients 10, no. 4: 474. https://doi.org/10.3390/nu10040474
APA StyleDe Lorenzo, A., Noce, A., Moriconi, E., Rampello, T., Marrone, G., Di Daniele, N., & Rovella, V. (2018). MOSH Syndrome (Male Obesity Secondary Hypogonadism): Clinical Assessment and Possible Therapeutic Approaches. Nutrients, 10(4), 474. https://doi.org/10.3390/nu10040474





