Impaired Glucose Tolerance in Adults with Duchenne and Becker Muscular Dystrophy
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Anthropometric Measurements
2.4. Bioelectrical Impedance
2.5. Vastus Lateralis Anatomical cross Sectional Area
2.6. Oral Glucose Tolerance Test
2.7. Physical Activity Questionnaires
2.8. Statistics
3. Results
3.1. Anthropometry and Body Composition
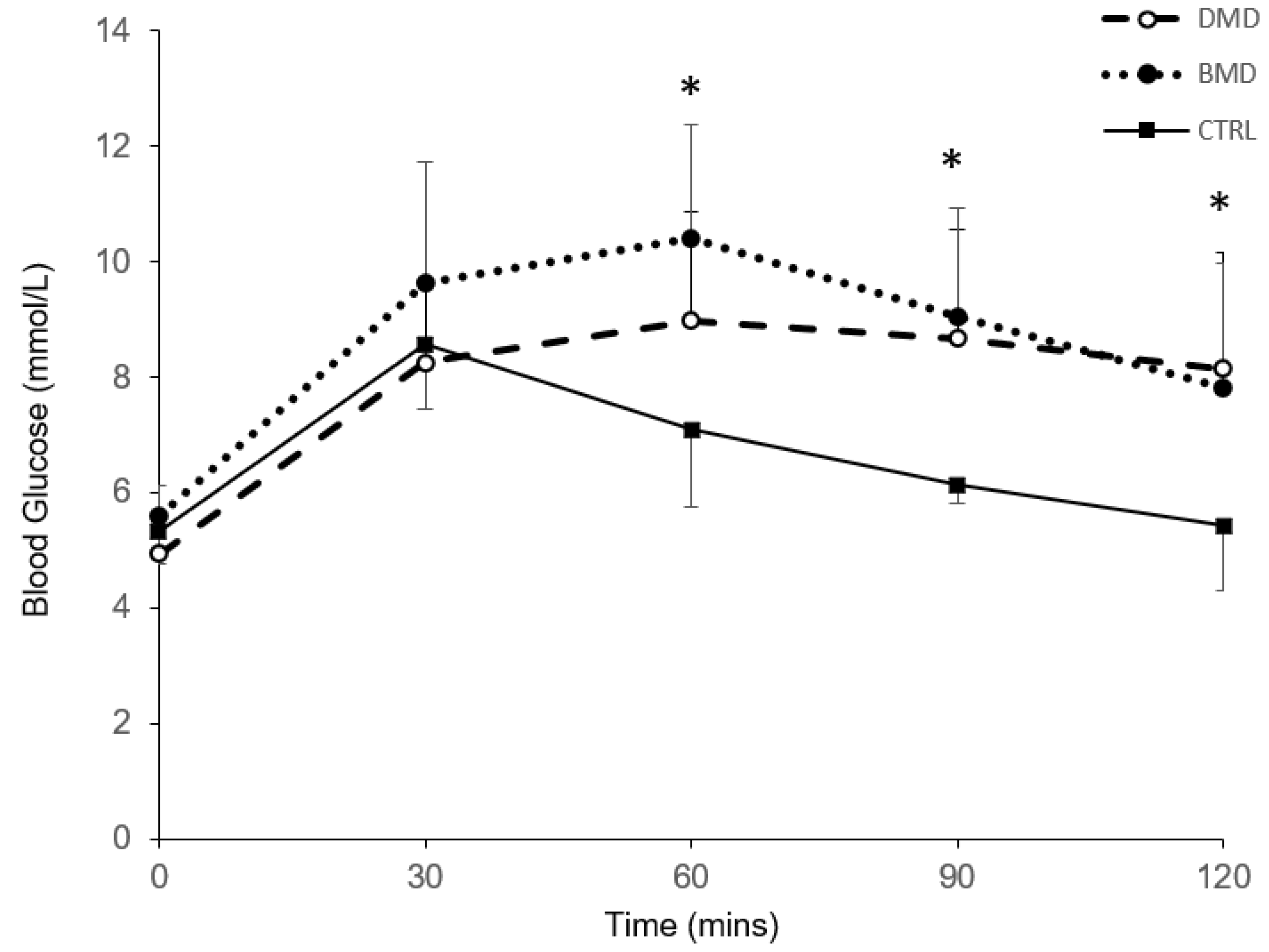
3.2. Oral Glucose Tolerance Test
3.3. Physical Activity Questionnaires
3.4. Correlations
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Huml, R.A. Muscular Dystrophy: A Concise Guide; Springer International Publishing: Basel, Switzerland, 2015. [Google Scholar]
- Emery, A.E. The muscular dystrophies. Lancet 2002, 359, 687–695. [Google Scholar] [CrossRef]
- Bushby, K.; Finkel, R.; Birnkrant, D.J.; Case, L.E.; Clemens, P.R.; Cripe, L.; Kaul, A.; Kinnett, K.; McDonald, C.; Pandya, S.; et al. Diagnosis and management of duchenne muscular dystrophy, part 1: Diagnosis, and pharmacological and psychosocial management. Lancet Neurol. 2010, 9, 77–93. [Google Scholar] [CrossRef]
- Hoffman, E.P.; Brown, R.H., Jr.; Kunkel, L.M. Dystrophin: The protein product of the duchenne muscular dystrophy locus. Cell 1987, 51, 919–928. [Google Scholar] [CrossRef]
- Deenen, J.C.; Horlings, C.G.; Verschuuren, J.J.; Verbeek, A.L.; van Engelen, B.G. The epidemiology of neuromuscular disorders: A comprehensive overview of the literature. J. Neuromuscul. Dis. 2015, 2, 73–85. [Google Scholar] [PubMed]
- Emery, A.E. Population frequencies of inherited neuromuscular diseases—A world survey. Neuromuscul. Disord. 1991, 1, 19–29. [Google Scholar] [CrossRef]
- Flanigan, K.M. Duchenne and becker muscular dystrophies. Neurol. Clin. 2014, 32, 671–688. [Google Scholar] [CrossRef]
- Birnkrant, D.J.; Bushby, K.; Bann, C.M.; Apkon, S.D.; Blackwell, A.; Brumbaugh, D.; Case, L.E.; Clemens, P.R.; Hadjiyannakis, S.; Pandya, S.; et al. Diagnosis and management of duchenne muscular dystrophy, part 1: Diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018, 17, 251–267. [Google Scholar] [CrossRef]
- Morse, C.I.; Smith, J.; Denny, A.; Tweedale, J.; Searle, N.D. Gastrocnemius medialis muscle architecture and physiological cross sectional area in adult males with duchenne muscular dystrophy. J. Musculoskelet. Neuronal. Interact. 2015, 15, 154–160. [Google Scholar]
- Morse, C.I.; Smith, J.; Denny, A.; Tweedale, J.; Searle, N.D.; Winwood, K.; Onambele-Pearson, G.L. Bone health measured using quantitative ultrasonography in adult males with muscular dystrophy. J. Musculoskelet. Neuronal. Interact. 2016, 16, 339–347. [Google Scholar]
- Jacques, M.F.; Orme, P.; Smith, J.; Morse, C.I. Resting energy expenditure in adults with becker’s muscular dystrophy. PLoS ONE 2017, 12, e0169848. [Google Scholar] [CrossRef]
- Løkken, N.; Hedermann, G.; Thomsen, C.; Vissing, J. Contractile properties are disrupted in becker muscular dystrophy, but not in limb girdle type 2i. Ann. Neurol. 2016, 80, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Duboc, D.; Meune, C.; Pierre, B.; Wahbi, K.; Eymard, B.; Toutain, A.; Berard, C.; Vaksmann, G.; Weber, S.; Becane, H.M. Perindopril preventive treatment on mortality in duchenne muscular dystrophy: 10 years’ follow-up. Am. Heart J. 2007, 154, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Simonds, A.K.; Muntoni, F.; Heather, S.; Fielding, S. Impact of nasal ventilation on survival in hypercapnic duchenne muscular dystrophy. Thorax 1998, 53, 949–952. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.S. Low skeletal muscle mass is associated with insulin resistance, diabetes, and metabolic syndrome in the korean population: The korea national health and nutrition examination survey (knhanes) 2009–2010. Endocr. J. 2014, 61, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Srikanthan, P.; Karlamangla, A.S. Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third national health and nutrition examination survey. J. Clin. Endocrinol. Metab. 2011, 96, 2898–2903. [Google Scholar] [CrossRef] [PubMed]
- Sinacore, D.R.; Gulve, E.A. The role of skeletal muscle in glucose transport, glucose homeostasis, and insulin resistance: Implications for physical therapy. Phys. Ther. 1993, 73, 878–891. [Google Scholar] [CrossRef] [PubMed]
- DePirro, R.; Lauro, R.; Testa, I.; Ferretti, I.; De Martinis, C.; Dellatonio, R. Decreased insulin receptors but normal glucose metabolism in duchenne muscular dystrophy. Science 1982, 216, 311–313. [Google Scholar] [CrossRef] [PubMed]
- Freidenberg, G.R.; Olefsky, J.M. Dissociation of insulin resistance and decreased insulin receptor binding in duchenne muscular dystrophy. J. Clin. Endocrinol. Metab. 1985, 60, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Haymond, M.W.; Strobel, K.E.; DeVivo, D.C. Muscle wasting and carbohydrate homeostasis in duchenne muscular dystrophy. Neurology 1978, 28, 1224–1231. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Cruz, M.; Sanchez, R.; Escobar, R.E.; Cruz-Guzman Odel, R.; Lopez-Alarcon, M.; Bernabe Garcia, M.; Coral-Vazquez, R.; Matute, G.; Velazquez Wong, A.C. Evidence of insulin resistance and other metabolic alterations in boys with duchenne or becker muscular dystrophy. Int. J. Endocrinol. 2015, 2015, 867273. [Google Scholar] [CrossRef] [PubMed]
- Morse, C.I.; Bostock, E.L.; Twiss, H.M.; Kapp, L.H.; Orme, P.; Jacques, M.F. The cardiorespiratory response and physiological determinants of the assisted 6-minute handbike cycle test in adult males with muscular dystrophy. Muscle Nerve 2018, 58, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Shimokata, H.; Muller, D.C.; Fleg, J.L.; Sorkin, J.; Ziemba, A.W.; Andres, R. Age as independent determinant of glucose tolerance. Diabetes 1991, 40, 44–51. [Google Scholar] [CrossRef] [PubMed]
- World Medical, A. World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
- Reeves, S.L.; Varakamin, C.; Henry, C.J. The relationship between arm-span measurement and height with special reference to gender and ethnicity. Eur. J. Clin. Nutr. 1996, 50, 398–400. [Google Scholar] [PubMed]
- Menke, A.; Casagrande, S.; Geiss, L.; Cowie, C.C. Prevalence of and trends in diabetes among adults in the united states, 1988–2012. JAMA 2015, 314, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Twig, G.; Afek, A.; Derazne, E.; Tzur, D.; Cukierman-Yaffe, T.; Gerstein, H.C.; Tirosh, A. Diabetes risk among overweight and obese metabolically healthy young adults. Diabetes Care 2014, 37, 2989–2995. [Google Scholar] [CrossRef] [PubMed]
- Okasora, K.; Takaya, R.; Tokuda, M.; Fukunaga, Y.; Oguni, T.; Tanaka, H.; Konishi, K.; Tamai, H. Comparison of bioelectrical impedance analysis and dual energy x-ray absorptiometry for assessment of body composition in children. Pediatr. Int. 1999, 41, 121–125. [Google Scholar] [CrossRef]
- Sun, G.; French, C.R.; Martin, G.R.; Younghusband, B.; Green, R.C.; Xie, Y.G.; Mathews, M.; Barron, J.R.; Fitzpatrick, D.G.; Gulliver, W.; et al. Comparison of multifrequency bioelectrical impedance analysis with dual-energy x-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am. J. Clin. Nutr. 2005, 81, 74–78. [Google Scholar] [CrossRef]
- Mok, E.; Letellier, G.; Cuisset, J.M.; Denjean, A.; Gottrand, F.; Hankard, R. Assessing change in body composition in children with duchenne muscular dystrophy: Anthropometry and bioelectrical impedance analysis versus dual-energy x-ray absorptiometry. Clin. Nutr. 2010, 29, 633–638. [Google Scholar] [CrossRef]
- Di Iorio, B.R.; Terracciano, V.; Bellizzi, V. Bioelectrical impedance measurement: Errors and artifacts. J. Ren. Nutr. 1999, 9, 192–197. [Google Scholar] [CrossRef]
- Reeves, N.D.; Maganaris, C.N.; Narici, M.V. Ultrasonographic assessment of human skeletal muscle size. Eur. J. Appl. Physiol. 2004, 91, 116–118. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes, A. (2) classification and diagnosis of diabetes. Diabetes Care 2015, 38, S8–S16. [Google Scholar] [CrossRef] [PubMed]
- Chilelli, N.C.; Cosma, C.; Ragazzi, E.; Burlina, S.; Zaninotto, M.; Plebani, M.; Lapolla, A. Screening with hba1c identifies only one in two individuals with diagnosis of prediabetes at oral glucose tolerance test: Findings in a real-world caucasian population. Acta Diabetol. 2014, 51, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Weeks, B.K.; Beck, B.R. The bpaq: A bone-specific physical activity assessment instrument. Osteoporos. Int. 2008, 19, 1567–1577. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.A.; Zhu, W.; McAuley, E.; Frogley, M.; Figoni, S.F. The physical activity scale for individuals with physical disabilities: Development and evaluation. Arch. Phys. Med. Rehabil. 2002, 83, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Van der Ploeg, H.P.; Streppel, K.R.; van der Beek, A.J.; van der Woude, L.H.; Vollenbroek-Hutten, M.; van Mechelen, W. The physical activity scale for individuals with physical disabilities: Test-retest reliability and comparison with an accelerometer. J. Phys. Act. Health 2007, 4, 96–100. [Google Scholar] [CrossRef]
- Son, J.W.; Lee, S.S.; Kim, S.R.; Yoo, S.J.; Cha, B.Y.; Son, H.Y.; Cho, N.H. Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: Findings from the koges. Diabetologia 2017, 60, 865–872. [Google Scholar] [CrossRef]
- Vohra, R.S.; Lott, D.; Mathur, S.; Senesac, C.; Deol, J.; Germain, S.; Bendixen, R.; Forbes, S.C.; Sweeney, H.L.; Walter, G.A.; et al. Magnetic resonance assessment of hypertrophic and pseudo-hypertrophic changes in lower leg muscles of boys with duchenne muscular dystrophy and their relationship to functional measurements. PLoS ONE 2015, 10, e0128915. [Google Scholar] [CrossRef]
- Beenakker, E.A.; de Vries, J.; Fock, J.M.; van Tol, M.; Brouwer, O.F.; Maurits, N.M.; van der Hoeven, J.H. Quantitative assessment of calf circumference in duchenne muscular dystrophy patients. Neuromuscul. Disord. 2002, 12, 639–642. [Google Scholar] [CrossRef]
- Forbes, S.C.; Walter, G.A.; Rooney, W.D.; Wang, D.J.; DeVos, S.; Pollaro, J.; Triplett, W.; Lott, D.J.; Willcocks, R.J.; Senesac, C.; et al. Skeletal muscles of ambulant children with duchenne muscular dystrophy: Validation of multicenter study of evaluation with mr imaging and mr spectroscopy. Radiology 2013, 269, 198–207. [Google Scholar] [CrossRef]
- Gong, Q.Y.; Phoenix, J.; Kemp, G.J.; Garcia-Finana, M.; Frostick, S.P.; Brodie, D.A.; Edwards, R.H.; Whitehouse, G.H.; Roberts, N. Estimation of body composition in muscular dystrophy by mri and stereology. J. Magn. Reson. Imaging 2000, 12, 467–475. [Google Scholar] [CrossRef]
- Monforte, M.; Mercuri, E.; Laschena, F.; Ricci, E.; Tasca, G. Calf muscle involvement in becker muscular dystrophy: When size does not matter. J. Neurol. Sci. 2014, 347, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Ryder, S.; Leadley, R.M.; Armstrong, N.; Westwood, M.; de Kock, S.; Butt, T.; Jain, M.; Kleijnen, J. The burden, epidemiology, costs and treatment for duchenne muscular dystrophy: An evidence review. Orphanet J. Rare Dis. 2017, 12, 79. [Google Scholar] [CrossRef]
- Hwang, J.L.; Weiss, R.E. Steroid-induced diabetes: A clinical and molecular approach to understanding and treatment. Diabetes Metab. Res. Rev. 2014, 30, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Takuya, I.; Yoshiyuki, K.; Yutaka, N.; Shigeki, K.; Michio, K. Steroid-induced diabetes mellitus and related risk factors in patients with neurologic diseases. Pharmacotherapy 2004, 24, 508–514. [Google Scholar]
- Burke, J.P.; Williams, K.; Gaskill, S.P.; Hazuda, H.P.; Haffner, S.M.; Stern, M.P. Rapid rise in the incidence of type 2 diabetes from 1987 to 1996: Results from the san antonio heart study. Arch. Intern. Med. 1999, 159, 1450–1456. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.I.; Flegal, K.M.; Cowie, C.C.; Eberhardt, M.S.; Goldstein, D.E.; Little, R.R.; Wiedmeyer, H.M.; Byrd-Holt, D.D. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in u.S. Adults. The third national health and nutrition examination survey, 1988-1994. Diabetes Care 1998, 21, 518–524. [Google Scholar] [CrossRef]
- King, H.; Aubert, R.E.; Herman, W.H. Global burden of diabetes, 1995–2025: Prevalence, numerical estimates, and projections. Diabetes Care 1998, 21, 1414–1431. [Google Scholar] [CrossRef]
- Van Dam, R.M.; Rimm, E.B.; Willett, W.C.; Stampfer, M.J.; Hu, F.B. Dietary patterns and risk for type 2 diabetes mellitus in u.S. Men. Ann. Intern. Med. 2002, 136, 201–209. [Google Scholar] [CrossRef]
- Boehme, M.W.; Buechele, G.; Frankenhauser-Mannuss, J.; Mueller, J.; Lump, D.; Boehm, B.O.; Rothenbacher, D. Prevalence, incidence and concomitant co-morbidities of type 2 diabetes mellitus in south western germany—A retrospective cohort and case control study in claims data of a large statutory health insurance. BMC Public Health 2015, 15, 855. [Google Scholar] [CrossRef]
- Tuomilehto, J.; Lindström, J.; Eriksson, J.G.; Valle, T.T.; Hämäläinen, H.; Ilanne-Parikka, P.; Keinänen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
| Control | DMD | BMD | |
|---|---|---|---|
| N | 12 | 15 | 13 |
| Ambulatory | 12 | 0 | 4 |
| Current corticosteroid use (n) | 0 | 6 | 0 |
| Age (Years) | 27.1 ± 7.4 | 24.6 ± 4.3 | 43.7 ± 7.3 *,# |
| Height (m) | 1.80 ± 0.08 | 1.68 ± 0.07 *,# | 1.76 ± 0.07 |
| Body Mass (Kg) | 79.7 ± 11.9 | 71.5 ± 13.8 | 96.5 ± 20.6 *,# |
| BMI (Kg/m2) | 24.6 ± 2.5 | 25.2 ± 4.1 | 31.1 ± 6.7 *,# |
| Fat Mass (Kg) | 13.9 ± 6.4 | 22.6 ± 6.2 * | 36.9 ± 17.6 *,# |
| Body Fat% | 16.4 ± 5.5 | 31.3 ± 3.8 * | 35.4 ± 8.2 * |
| FFM (Kg) | 65.7 ± 7.4 | 48.9 ± 8.6 *,# | 59.5 ± 13.4 |
| Relative FFM (%) | 83.1 ± 5.5 | 68.7 ± 3.8 * | 62.9 ± 12.7 * |
| VL ACSA (cm2) | 32.2 ± 8.6 | 16.3 ± 9.5 * | 16.9 ± 6.9 * |
| n with IGT | 0 | 8 | 6 |
| PASIPD | - | 7.2 ± 7.1 | 12.9 ± 7.8 |
| BPAQ | 49.7 ± 48.0 | 5.9 ± 8.2 * | 10.1 ± 10.2 * |
| Glucose 120 min | Glucose AUC | |||||
|---|---|---|---|---|---|---|
| Control | DMD | BMD | Control | DMD | BMD | |
| Body Mass | 0.228 | 0.105 | 0.318 | 0.189 | 0.087 | −0.107 |
| BMI | 0.193 | 0.086 | 0.394 | 0.305 | 0.046 | 0.017 |
| Fat Mass | 0.350 | 0.209 | 0.463 | 0.049 | 0.173 | 0.132 |
| Body Fat% | 0.322 | 0.148 | 0.554 * | −0.238 | 0.199 | 0.217 |
| FFM | 0.063 | 0.118 | −0.268 | 0.224 | 0.041 | −0.286 |
| Relative FFM | −0.434 | −0.148 | −0.557 * | 0.028 | −0.199 | −0.203 |
| VL ACSA | 0.434 | −0.032 | 0.168 | −0.224 | 0.279 | −0.269 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bostock, E.L.; Edwards, B.T.; Jacques, M.F.; Pogson, J.T.S.; Reeves, N.D.; Onambele-Pearson, G.L.; Morse, C.I. Impaired Glucose Tolerance in Adults with Duchenne and Becker Muscular Dystrophy. Nutrients 2018, 10, 1947. https://doi.org/10.3390/nu10121947
Bostock EL, Edwards BT, Jacques MF, Pogson JTS, Reeves ND, Onambele-Pearson GL, Morse CI. Impaired Glucose Tolerance in Adults with Duchenne and Becker Muscular Dystrophy. Nutrients. 2018; 10(12):1947. https://doi.org/10.3390/nu10121947
Chicago/Turabian StyleBostock, Emma L., Bryn T. Edwards, Matthew F. Jacques, Jake T.S. Pogson, Neil D. Reeves, Gladys L. Onambele-Pearson, and Christopher I. Morse. 2018. "Impaired Glucose Tolerance in Adults with Duchenne and Becker Muscular Dystrophy" Nutrients 10, no. 12: 1947. https://doi.org/10.3390/nu10121947
APA StyleBostock, E. L., Edwards, B. T., Jacques, M. F., Pogson, J. T. S., Reeves, N. D., Onambele-Pearson, G. L., & Morse, C. I. (2018). Impaired Glucose Tolerance in Adults with Duchenne and Becker Muscular Dystrophy. Nutrients, 10(12), 1947. https://doi.org/10.3390/nu10121947







