Assessment of Muscle Wasting in Long-Stay ICU Patients Using a New Ultrasound Protocol
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Healthy Controls
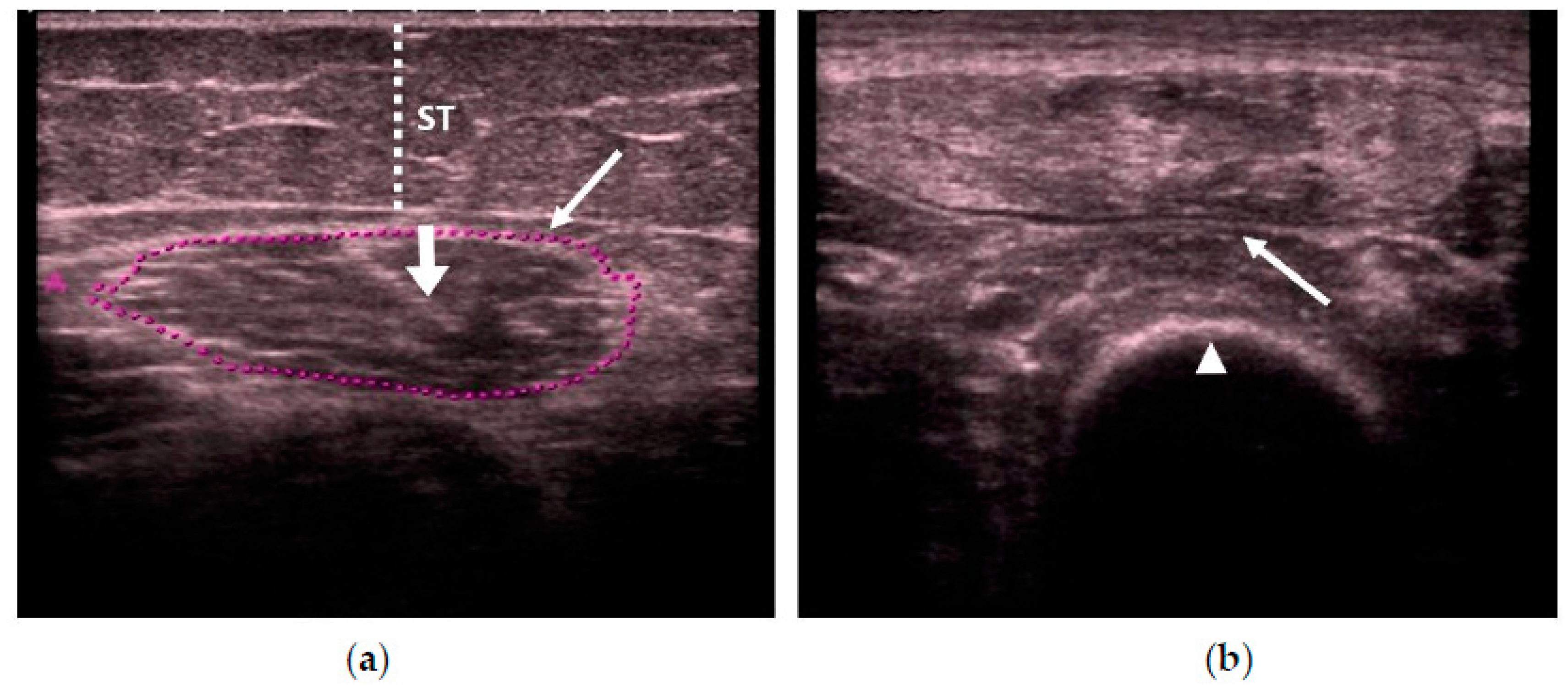
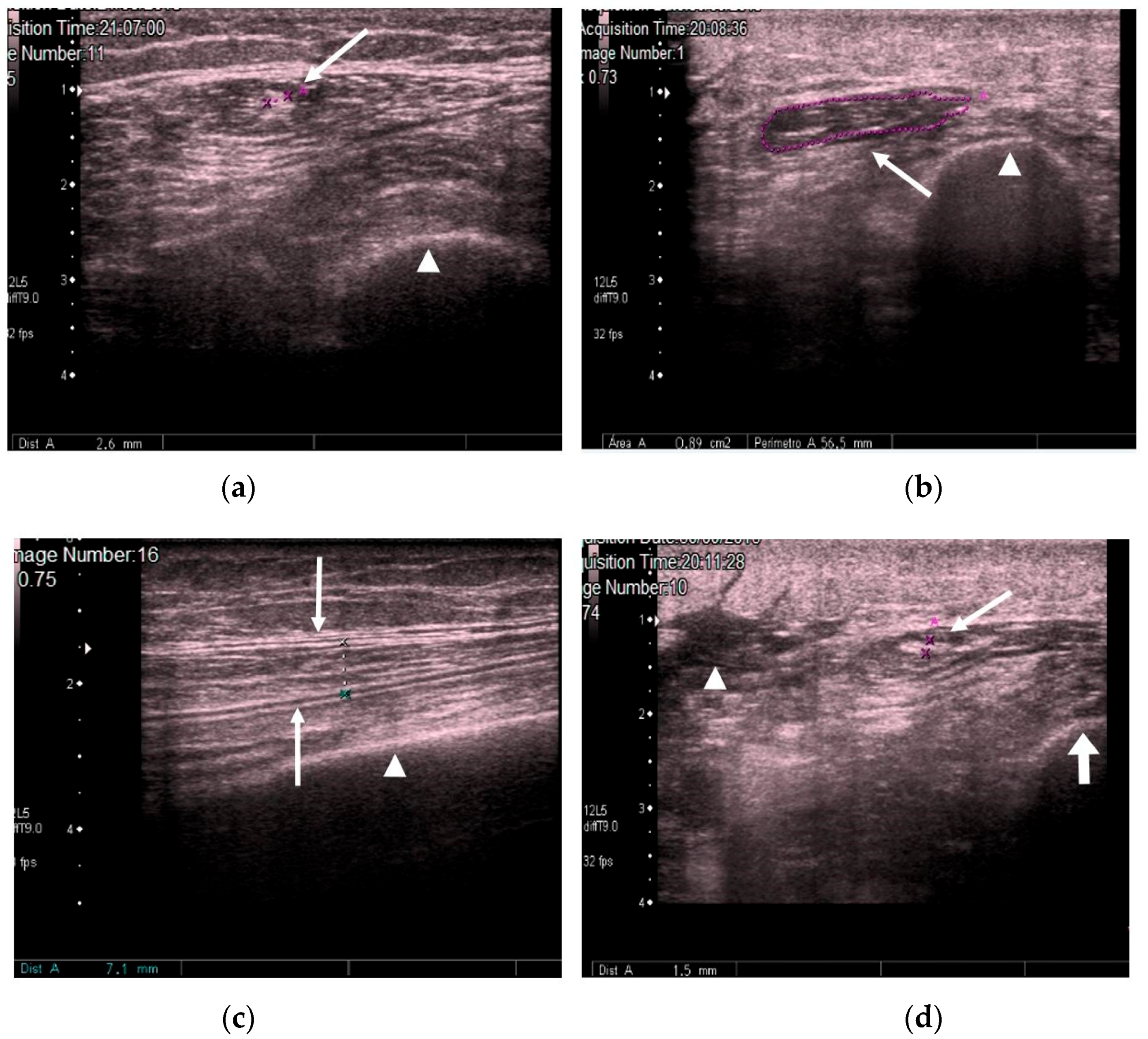
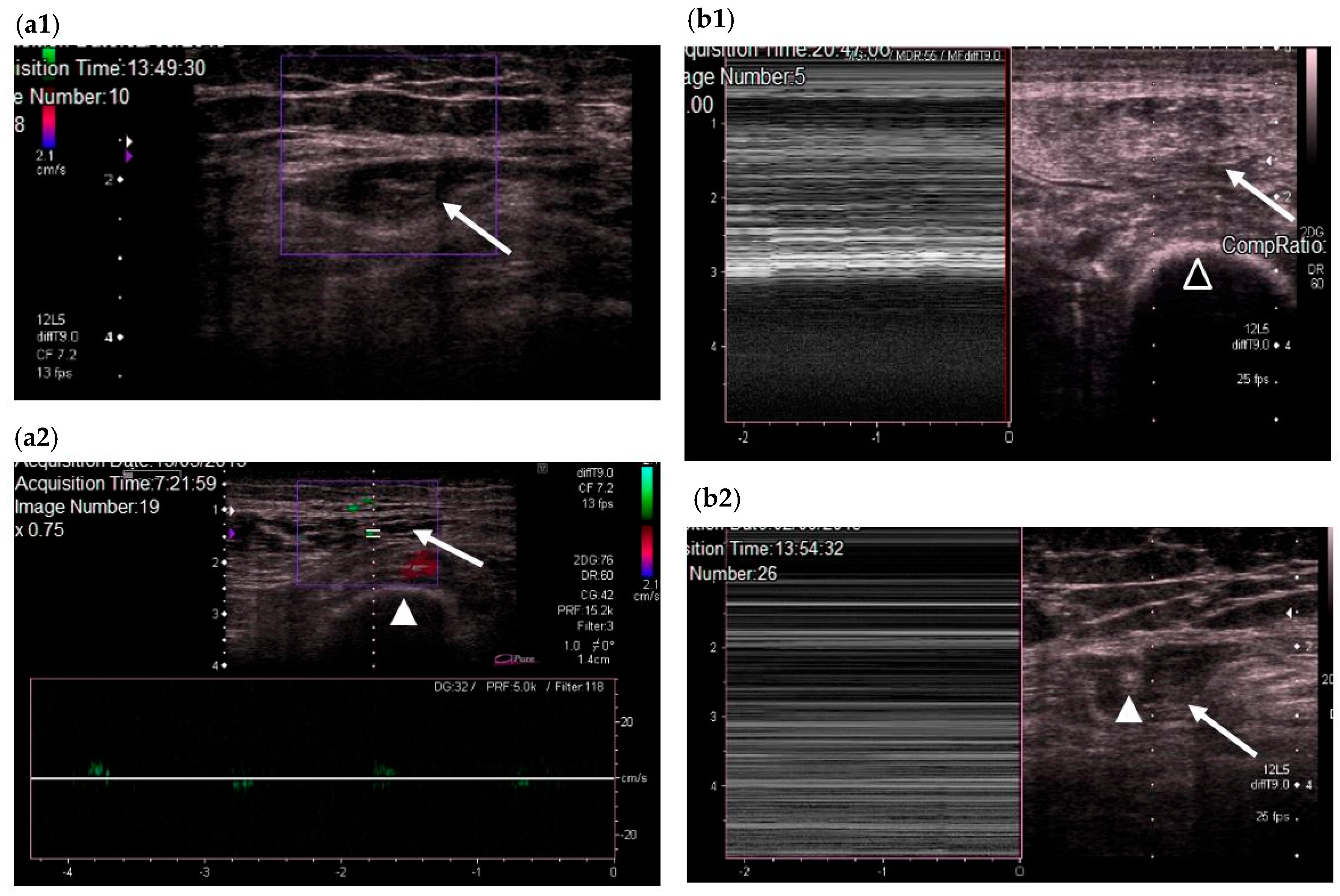
2.2. New Quadriceps Rectus Femoris Ultrasonography Assessment Protocol
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Coelho-Júnior, H.J.; Rodrigues, B.; Uchida, M.; Marzetti, E. Low protein intake is associated with frailty in older adults: A systematic review and meta-analysis of observational studies. Nutrients 2018, 10, 1334. [Google Scholar] [CrossRef] [PubMed]
- Wischmeyer, P.E.; Puthucheary, Z.; San Millán, I.; Butz, D.; Grocott, M.P.W. Muscle mass and physical recovery in ICU: Innovations for targeting of nutrition and exercise. Curr. Opin. Crit. Care 2017, 23, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Casaer, M.P. Muscle weakness and nutrition therapy in ICU. Curr. Opin. Nutr. Metab. Care 2015, 18, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Ahn, S.; Kim, Y.J.; Ji, M.J.; Kim, K.M.; Choi, S.H.; Jang, H.C.; Lim, S. Comparison between dual-energy X-ray absorptiometry and bioelectrical impedance analyses for accuracy in measuring whole body muscle mass and appendicular skeletal muscle mass. Nutrients 2018, 10, 738. [Google Scholar] [CrossRef] [PubMed]
- Schepens, T.; Verbrugghe, W.; Dams, K.; Corthouts, B.; Parizel, P.M.; Jorens, P.G. The course of diaphragm atrophy in ventilated patients assessed with ultrasound: A longitudinal cohort study. Crit. Care 2015, 19, 422. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.M.; Heymsfield, S.B. Lean tissue imaging: A new era for nutritional assessment and intervention. JPEN J. Parenter. Enter. Nutr. 2014, 38, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Weijs, P.J.; Looijaard, W.G.; Dekker, I.M.; Stapel, S.N.; Girbes, A.R.; Oudemans-van Straaten, H.M.; Beishuizen, A. Low skeletal muscle area is a risk factor for mortality in mechanically ventilated critically ill patients. Crit. Care 2014, 18, R12. [Google Scholar] [CrossRef] [PubMed]
- Mitsiopoulos, N.; Baumgartner, R.N.; Heymsfield, S.B.; Lyons, W.; Gallagher, D.; Ross, R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J. Appl. Physiol. 1998, 85, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Reeves, N.D.; Maganaris, C.N.; Narici, M.V. Ultrasonographic assessment of human skeletal muscle size. Eur. J. Appl. Physiol. 2004, 91, 116–118. [Google Scholar] [CrossRef] [PubMed]
- Bear, D.E.; Parry, S.M.; Puthucheary, Z.A. Can the critically ill patient generate sufficient energy to facilitate exercise in the ICU? Curr. Opin. Clin. Nutr. Metab. 2018, 21, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Spiegl, M.; Altmann, K.; Winkler, A.; Salamon, A.; Themessl-Huber, M.; Mouhieddine, M.; Strasser, E.M.; Schiferer, A.; Paternostro-Sluga, T.; et al. Muscle mass, strength and functional outcomes in critically ill patients after cardiothoracic surgery: Does neuromuscular electrical stimulation help? The Catastim 2 randomized controlled trial. Crit. Care 2016, 20, 30. [Google Scholar] [CrossRef] [PubMed]
- Mourtzakis, M.; Parry, S.; Connolly, B.; Puthucheary, Z. Skeletal muscle ultrasound in critical care: A tool in need of translation. Ann. Am. Thorac. Soc. 2017, 14, 1495–1503. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, A.; Regolisti, G.; Bozzoli, L.; Fani, F.; Antoniotti, R.; Maggiore, U.; Fiaccadori, E. Reliability of bedside ultrasound for measurement of quadriceps muscle thickness in critically ill patients with acute kidney injury. Clin. Nutr. 2016, 36, 1710–1715. [Google Scholar] [CrossRef] [PubMed]
- Balius, R.; Maestro, A.; Pedret, C.; Estruch, A.; Mota, J.; Rodríguez, L.; García, P.; Mauri, E. Central aponeurosis tears of the rectus femoris: Practical sonographic prognosis. Br. J. Sports Med. 2009, 43, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Hermans, G.; Van den Berghe, G. Clinical review: Intensive care unit acquired weakness. Crit. Care 2015, 19, 274. [Google Scholar] [CrossRef] [PubMed]
- Witteveen, E.; Sommers, J.; Wieske, L.; Doorduin, J.; van Alfen, N.; Schultz, M.J.; van Schaik, I.N.; Horn, J.; Verhamme, C. Diagnostic accuracy of quantitative neuromuscular ultrasound for the diagnosis of intensive care unit-acquired weakness: A cross-sectional observational study. Ann. Intensive Care 2017, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Hough, C.L.; Lieu, B.K.; Caldwell, E.S. Manual muscle strength testing of critically ill patients: Feasibility and interobserver agreement. Crit. Care 2011, 15, R43. [Google Scholar] [CrossRef] [PubMed]
- Mayans, D.; Cartwright, M.S.; Walker, F.O. Neuromuscular ultrasonography: Quantifying muscle and nerve measurements. Phys. Med. Rehabil. Clin. N. Am. 2012, 23, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.; Low, G.; Mourtzakis, M.; Zenith, L.; Myers, R.P.; Abraldes, J.G.; Shaheen, A.A.; Qamar, H.; Mansoor, N.; Carbonneau, M.; et al. A Model to Identify Sarcopenia in Patients with Cirrhosis. Clin. Gastroenterol. Hepatol. 2016, 14, 1473–1480. [Google Scholar] [CrossRef] [PubMed]
- Strasse, E.M.; Draskovits, T.; Praschak, M.; Quittan, M.; Graf, A. Association between ultrasound measurements of muscle thickness, pennation angle, echogenicity and skeletal muscle strength in the elderly. Age 2013, 35, 2377–2388. [Google Scholar] [CrossRef] [PubMed]
- Rollins, K.E.; Javanmard-Emamghissi, H.; Awwad, A.; Macdonald, I.A.; Fearon, K.C.H.; Lobo, D.N. Body composition measurement using computed tomography: Does the phase of the scan matter? Nutrition 2017, 41, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Aubrey, J.; Esfandiari, N.; Baracos, V.E.; Buteau, F.A.; Frenette, J.; Putman, C.T.; Mazurak, V.C. Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiol. 2014, 210, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Miljkovic, I.; Zmuda, J.M. Epidemiology of myosteatosis. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, N.; Nakagawa, H.; Kudo, Y.; Tateishi, R.; Taguri, M.; Watadani, T.; Nakagomi, R.; Kondo, M.; Nakatsuka, T.; Minami, T.; et al. Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J. Hepatol. 2015, 63, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Mohseni-Bandpei, M.A.; Nakhaee, M.; Mousavi, M.E.; Shakourirad, A.; Safari, M.R.; Vahab Kashani, R. Application of ultrasound in the assessment of plantar fascia in patients with plantar fasciitis: A systematic review. Ultrasound Med. Biol. 2014, 40, 1737–1754. [Google Scholar] [CrossRef] [PubMed]
- Fan, E.; Cheek, F.; Chlan, L.; Gosselink, R.; Hart, N.; Herridge, M.S.; Hopkins, R.O.; Hough, C.L.; Kress, J.P.; Latronico, N.; et al. ATS Committee on ICU-acquired weakness in adults; American thoracic society. An official American thoracic society clinical practice guideline: The diagnosis of intensive care unit-acquired weakness in adults. Am. J. Respir. Crit. Care Med. 2014, 190, 1437–1446. [Google Scholar] [CrossRef] [PubMed]
- Grimm, A.; Teschner, U.; Porzelius, C.; Ludewig, K.; Zielske, J.; Witte, O.W.; Brunkhorst, F.M.; Axer, H. Muscle ultrasound for early assessment of critical illness neuromyopathy in severe sepsis. Crit. Care 2013, 17, R227. [Google Scholar] [CrossRef] [PubMed]
- Gruther, W.; Benesch, T.; Zorn, C.; Paternostro-Sluga, T.; Quittan, M.; Fialka-Moser, V.; Spiss, C.; Kainberger, F.; Crevenna, R. Muscle wasting in intensive care patients: Ultrasound observation of the M. quadriceps femoris muscle layer. J. Rehabil. Med. 2008, 40, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Tillquist, M.; Kutsogiannis, D.J.; Wischmeyer, P.E.; Kummerlen, C.; Leung, R.; Stollery, D.; Karvellas, C.J.; Preiser, J.C.; Bird, N.; Kozar, R.; et al. Bedside ultrasound is a practical and reliable measurement tool for assessing quadriceps muscle layer thickness. J. Parenter. Enteral Nutr. 2014, 38, 886–890. [Google Scholar] [CrossRef] [PubMed]
- Puthucheary, Z.A.; Rawal, J.; McPhail, M.; Connolly, B.; Ratnayake, G.; Chan, P.; Hopkinson, N.S.; Phadke, R.; Dew, T.; Sidhu, P.S.; et al. Acute skeletal muscle wasting in critical illness. JAMA 2013, 16, 1591–1600. [Google Scholar] [CrossRef] [PubMed]
- Parry, S.M.; El-Ansary, D.; Cartwright, M.S.; Sarwal, A.; Berney, S.; Koopman, R.; Annoni, R.; Puthucheary, Z.; Gordon, I.R.; Morris, P.E.; et al. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J. Crit. Care 2015, 30, 1151. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.M.; Loenneke, J.P.; Jo, E.; Wilson, G.J.; Zourdos, M.C.; Kim, J.S. The effects of endurance, strength, and power training on muscle fiber type shifting. J. Strength Cond. Res. 2012, 26, 1724–1729. [Google Scholar] [CrossRef] [PubMed]
- Bierbrauer, J.; Koch, S.; Olbricht, C.; Hamati, J.; Lodka, D.; Schneider, J.; Luther-Schröder, A.; Kleber, C.; Faust, K.; Wiesener, S.; et al. Early type II fiber atrophy in intensive care unit patients with nonexcitable muscle membrane. Crit. Care Med. 2012, 40, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Ticinesi, A.; Meschi, T.; Narici, M.V.; Lauretani, F.; Maggio, M. Muscle Ultrasound and Sarcopenia in Older Individuals: A Clinical Perspective. J. Am. Med. Dir. Assoc. 2017, 18, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Berger, J.; Bunout, D.; Barrera, G.; de la Maza, M.P.; Henriquez, S.; Leiva, L.; Hirsch, S. Rectus femoris (RF) ultrasound for the assessment of muscle mass in older people. Arch. Gerontol. Geriatr. 2015, 61, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Puthucheary, Z.A.; Phadke, R.; Rawal, J.; McPhail, M.J.; Sidhu, P.S.; Rowlerson, A.; Moxham, J.; Harridge, S.; Hart, N.; Montgomery, H.E. Qualitative ultrasound in acute critical illness muscle wasting. Crit. Care Med. 2015, 43, 1603–1611. [Google Scholar] [CrossRef] [PubMed]
- Batt, J.; Mathur, S.; Katzberg, H.D. Mechanism of ICU-acquired weakness: Muscle contractility in critical illness. Intensive Care Med. 2017, 43, 584–586. [Google Scholar] [CrossRef] [PubMed]

| Controls (n = 19) | Cases (n = 29) | p | |
|---|---|---|---|
| Mean age in years (± SD) | 59.9 ± 18.4 | 62.9 ± 15.7 | 0.543 |
| Age 65 years, n (%) | 10 (52.6) | 14 (48.3) | 0.768 |
| Sex, n (%) | 0.049 | ||
| Male | 5 (26.3) | 16 (55.2) | |
| Female | 14 (73.7) | 13 (44.8) | |
| Body mass index, kg/m2, mean (±SD) | 25.4 ± 3.6 | 28.3 ± 5.4 | 0.068 |
| QRF muscle area, cm2, median (IQR) | 3.6 (3.0; 4.3) | 1.0 (0.5; 1.8) | <0.001 |
| QRF tendon thickness, mm, median (IQR) | 1.5 (1.4; 1.6) | 1.8 (1.3; 2.1) | 0.047 |
| QRF muscle thickness, mm, median (IQR) | 11.4 (7.5; 13.3) | 5.7 (3.5; 8.5) | 0.001 |
| Doppler color, n (%) | 19 (100) | 7 (24.1) | <0.001 |
| Fasciculations, n (%) | 19 (100) | 7 (24.1) | <0.001 |
| Subcutaneous edema, n (%) | 0 | 23 (88.5) | <0.001 |
| Intramuscular fluid, n (%) | 0 | 18 (69.2) | <0.001 |
| Echogenicity, n (%) | <0.001 | ||
| 1 | 19 (100.0) | 0 | |
| 2 | 0 | 4 (13.8) | |
| 3 | 0 | 15 (51.7) | |
| 4 | 0 | 10 (34.5) |
| n = 29 | |
|---|---|
| Apache-II median (IQR) | 26.5 (23.8; 29) |
| SOFA score at ICU admission, median (IQR) | 7 (6.2; 7.8) |
| GCS at ICU admission, median (IQR) | 4 (3; 14) |
| Time between ICU admission and QRF-US in days, median (IQR) | 28 (15.5; 48.5) |
| Multiorgan failure, n (%) | 25 (86.2) |
| Respiratory failure, n (%) | 25 (86.2) |
| Cardiovascular failure, n (%) | 21 (72.4) |
| Renal failure, n (%) | 20 (69.0) |
| Hepatic failure, n (%) | 2 (6.9) |
| Hematologic failure, n (%) | 1 (3.5) |
| Gastrointestinal failure, n (%) | 1 (3.5) |
| Septic at ICU admission, n (%) | 23 (80.1) |
| Corticosteroids, n (%) | 11 (37.9) |
| Neuromuscular blockers, n (%) | 12 (41.4) |
| Coefficient (SE) | p | OR (95% CI) | |
|---|---|---|---|
| (Intercept) | −4.533 (3.578) | 0.205 | - |
| QRF Muscle area, per cm2 | −2.641 (0.893) | 0.003 | 0.071 (0.012; 0.410) |
| QRF Tendon Thickness, per mm | 7.543 (3.349) | 0.024 | 1887 (2.661; 1,338,092) |
| Parameter | Estimation (%) | 95% CI |
|---|---|---|
| Sensitivity | 90.9 | 70.8; 98.9 |
| Specificity | 89.5 | 66.9; 98.7 |
| Negative predictive value | 89.5 | 69.2; 97.0 |
| Positive predictive value | 90.9 | 72.8; 97.4 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Socorro, C.R.; Saavedra, P.; López-Fernández, J.C.; Ruiz-Santana, S. Assessment of Muscle Wasting in Long-Stay ICU Patients Using a New Ultrasound Protocol. Nutrients 2018, 10, 1849. https://doi.org/10.3390/nu10121849
Hernández-Socorro CR, Saavedra P, López-Fernández JC, Ruiz-Santana S. Assessment of Muscle Wasting in Long-Stay ICU Patients Using a New Ultrasound Protocol. Nutrients. 2018; 10(12):1849. https://doi.org/10.3390/nu10121849
Chicago/Turabian StyleHernández-Socorro, Carmen Rosa, Pedro Saavedra, Juan Carlos López-Fernández, and Sergio Ruiz-Santana. 2018. "Assessment of Muscle Wasting in Long-Stay ICU Patients Using a New Ultrasound Protocol" Nutrients 10, no. 12: 1849. https://doi.org/10.3390/nu10121849
APA StyleHernández-Socorro, C. R., Saavedra, P., López-Fernández, J. C., & Ruiz-Santana, S. (2018). Assessment of Muscle Wasting in Long-Stay ICU Patients Using a New Ultrasound Protocol. Nutrients, 10(12), 1849. https://doi.org/10.3390/nu10121849





