Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score
Abstract
:1. Introduction
2. Materials and Methods
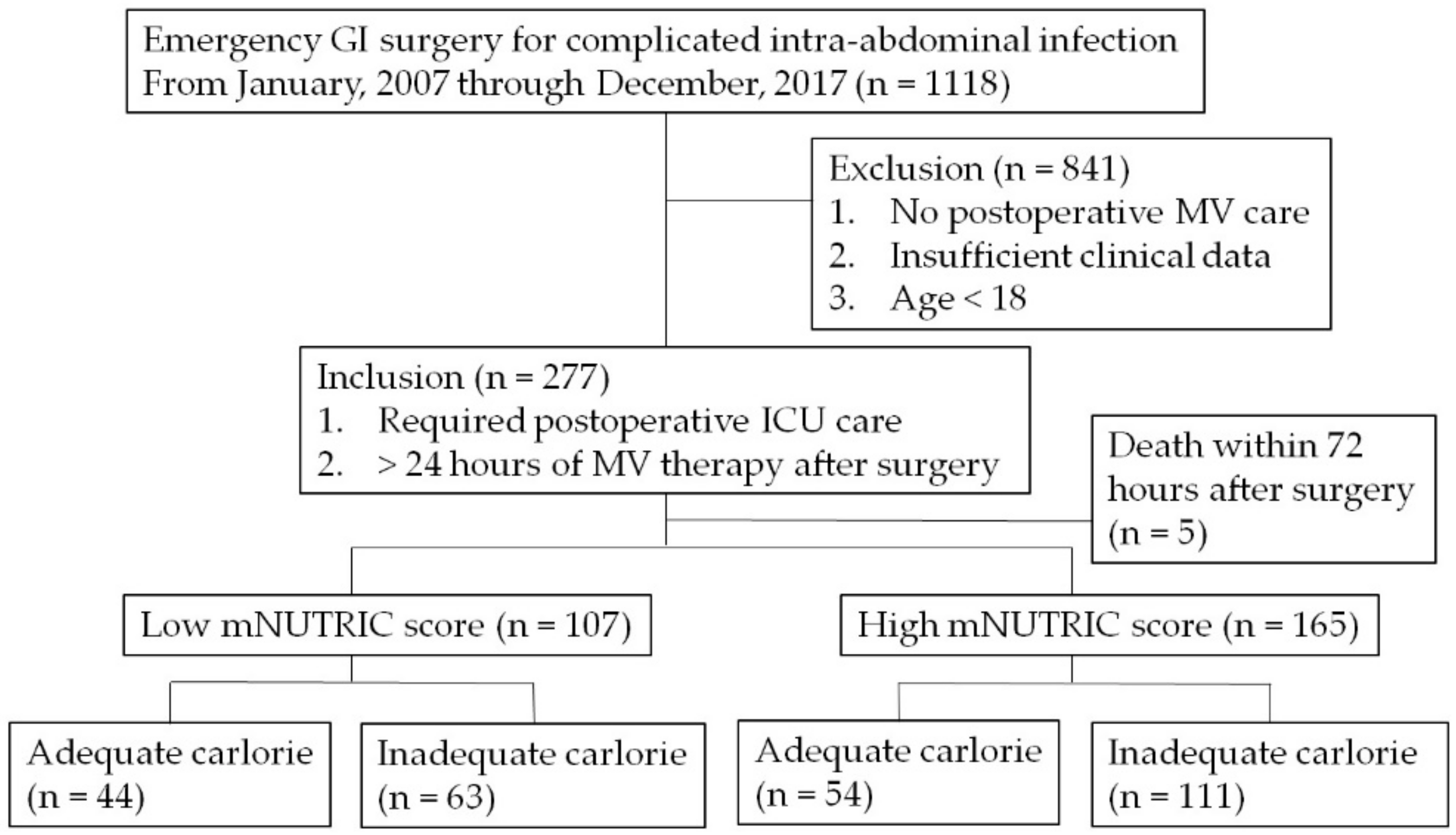
2.1. Study Population
2.2. Data Collection and Definition
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Perioperative Parameters
3.3. Calorie Requirement and Adequacy
3.4. Clinical Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alberda, C.; Gramlich, L.; Jones, N.; Jeejeebhoy, K.; Day, A.G.; Dhaliwal, R.; Heyland, D.K. The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. Intensive Care Med. 2009, 35, 1728–1737. [Google Scholar] [CrossRef] [PubMed]
- Faisy, C.; Lerolle, N.; Dachraoui, F.; Savard, J.F.; Abboud, I.; Tadie, J.M.; Fagon, J.Y. Impact of energy deficit calculated by a predictive method on outcome in medical patients requiring prolonged acute mechanical ventilation. Br. J. Nutr. 2009, 101, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Heyland, D.K.; Cahill, N.; Day, A.G. Optimal amount of calories for critically ill patients: Depends on how you slice the cake! Crit. Care Med. 2011, 39, 2619–2626. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. (Edinb. Scotl.) 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Hill, A.A.; Plank, L.D.; Finn, P.J.; Whalley, G.A.; Sharpe, N.; Clark, M.A.; Hill, G.L. Massive nitrogen loss in critical surgical illness: Effect on cardiac mass and function. Ann. Surg. 1997, 226, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Detsky, A.S.; McLaughlin, J.R.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? 1987. Classical article. Nutr. Hosp. 2008, 23, 400–407. [Google Scholar] [PubMed]
- Lim, S.L.; Tong, C.Y.; Ang, E.; Lee, E.J.; Loke, W.C.; Chen, Y.; Ferguson, M.; Daniels, L. Development and validation of 3-Minute Nutrition Screening (3-MinNS) tool for acute hospital patients in Singapore. Asia Pac. J. Clin. Nutr. 2009, 18, 395–403. [Google Scholar] [PubMed]
- Anthony, P.S. Nutrition screening tools for hospitalized patients. Nutr. Clin. Pract. 2008, 23, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, N.; Plank, L.D.; Sando, K.; Hill, G.L. Optimal protein requirements during the first 2 weeks after the onset of critical illness. Crit. Care Med. 1998, 26, 1529–1535. [Google Scholar] [CrossRef] [PubMed]
- Heyland, D.K.; Dhaliwal, R.; Jiang, X.; Day, A.G. Identifying critically ill patients who benefit the most from nutrition therapy: The development and initial validation of a novel risk assessment tool. Crit. Care (Lond. Engl.) 2011, 15, R268. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Hasan, R.M.; Agarwala, R.; Martin, C.; Day, A.G.; Heyland, D.K. Identifying critically-ill patients who will benefit most from nutritional therapy: Further validation of the “modified NUTRIC” nutritional risk assessment tool. Clin. Nutr. (Edinb. Scotl.) 2016, 35, 158–162. [Google Scholar] [CrossRef] [PubMed]
- de Vries, M.C.; Koekkoek, W.K.; Opdam, M.H.; van Blokland, D.; van Zanten, A.R. Nutritional assessment of critically ill patients: Validation of the modified NUTRIC score. Eur. J. Clin. Nutr. 2018, 72, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hubner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.; et al. ESPEN guideline: Clinical nutrition in surgery. Clin. Nutr. (Edinb. Scotl.) 2017, 36, 623–650. [Google Scholar] [CrossRef] [PubMed]
- McClave, S.A.; Taylor, B.E.; Martindale, R.G.; Warren, M.M.; Johnson, D.R.; Braunschweig, C.; McCarthy, M.S.; Davanos, E.; Rice, T.W.; Cresci, G.A.; et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J. Parenter. Enter. Nutr. 2016, 40, 159–211. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Jang, J.Y.; Kim, H.W.; Jung, M.J.; Lee, J.G. Effects of early enteral nutrition on patients after emergency gastrointestinal surgery: A propensity score matching analysis. Medicine 2014, 93, e323. [Google Scholar] [CrossRef] [PubMed]
- Woodcock, N.P.; Zeigler, D.; Palmer, M.D.; Buckley, P.; Mitchell, C.J.; MacFie, J. Enteral versus parenteral nutrition: A pragmatic study. Nutrition 2001, 17, 1–12. [Google Scholar] [CrossRef]
- Casaer, M.P.; Mesotten, D.; Hermans, G.; Wouters, P.J.; Schetz, M.; Meyfroidt, G.; Van Cromphaut, S.; Ingels, C.; Meersseman, P.; Muller, J.; et al. Early versus late parenteral nutrition in critically ill adults. N. Engl. J. Med. 2011, 365, 506–517. [Google Scholar] [CrossRef] [PubMed]
- Heidegger, C.P.; Berger, M.M.; Graf, S.; Zingg, W.; Darmon, P.; Costanza, M.C.; Thibault, R.; Pichard, C. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: A randomised controlled clinical trial. Lancet (Lond. Engl.) 2013, 381, 385–393. [Google Scholar] [CrossRef]
- Zacharias, T.; Ferreira, N. Nutritional risk screening 2002 and ASA score predict mortality after elective liver resection for malignancy. Arch. Med. Sci. AMS 2017, 13, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Hackett, N.J.; De Oliveira, G.S.; Jain, U.K.; Kim, J.Y. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int. J. Surg. (Lond. Engl.) 2015, 18, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Costa, R.T.; Nassar, A.P., Jr.; Caruso, P. Accuracy of SOFA, qSOFA, and SIRS scores for mortality in cancer patients admitted to an intensive care unit with suspected infection. J. Crit. Care 2018, 45, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Al-Dorzi, H.M.; Albarrak, A.; Ferwana, M.; Murad, M.H.; Arabi, Y.M. Lower versus higher dose of enteral caloric intake in adult critically ill patients: A systematic review and meta-analysis. Crit. Care (Lond. Engl.) 2016, 20, 358. [Google Scholar] [CrossRef] [PubMed]
- Tian, F.; Wang, X.; Gao, X.; Wan, X.; Wu, C.; Zhang, L.; Li, N.; Li, J. Effect of initial calorie intake via enteral nutrition in critical illness: A meta-analysis of randomised controlled trials. Crit. Care (Lond. Engl.) 2015, 19, 180. [Google Scholar] [CrossRef] [PubMed]
- Petros, S.; Horbach, M.; Seidel, F.; Weidhase, L. Hypocaloric vs Normocaloric Nutrition in Critically Ill Patients: A Prospective Randomized Pilot Trial. JPEN J. Parenter. Enter. Nutr. 2016, 40, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Gramlich, L.; Kichian, K.; Pinilla, J.; Rodych, N.J.; Dhaliwal, R.; Heyland, D.K. Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition 2004, 20, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Braunschweig, C.L.; Levy, P.; Sheean, P.M.; Wang, X. Enteral compared with parenteral nutrition: A meta-analysis. Am. J. Clin. Nutr. 2001, 74, 534–542. [Google Scholar] [CrossRef] [PubMed]
- Peter, J.V.; Moran, J.L.; Phillips-Hughes, J. A metaanalysis of treatment outcomes of early enteral versus early parenteral nutrition in hospitalized patients. Crit. Care Med. 2005, 33, 213–220. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total PopulationHigh Risk (mNUTRIC ≥ 5) (n = 165) | Matched PopulationHigh Risk (mNUTRIC ≥ 5) (n = 108) | ||||
|---|---|---|---|---|---|---|
| Inadequate Nutrition (n = 111) | Adequate Nutrition (n = 54) | p Value | Inadequate Nutrition (n = 54) | Adequate Nutrition (n = 54) | p Value | |
| Age, n | 71.02 ± 10.97 | 69.52 ± 11.48 | 0.418 | 69.96 ± 11.52 | 69.52 ± 11.48 | 0.841 |
| Sex, M/F, n (%) | 66 (59.5)/45 (40.5) | 23 (42.6)/31 (57.4) | 0.041 | 23 (42.6)/31 (57.4) | 23 (42.6)/31 (57.4) | 1.000 |
| BMI, kg/m2 | 23.17 ± 4.15 | 21.03 ± 3.11 | <0.001 | 21.02 ± 4.47 | 21.03 ± 3.11 | 0.603 |
| Weight, kg | 60.65 ± 12.80 | 53.11 ± 8.96 | <0.001 | 54.65 ± 11.32 | 53.11 ± 8.96 | 0.435 |
| Height, m | 1.62 ± 0.09 | 1.59 ± 0.08 | 0.081 | 1.60 ± 0.10 | 1.59 ± 0.08 | 0.679 |
| ASA, n (%) | 0.049 | 0.627 | ||||
| 1 | 9 (8.1) | 12 (22.2) | 7 (13.0) | 12 (22.2) | ||
| 2 | 9 (8.1) | 8 (14.8) | 7 (13.0) | 8 (14.8) | ||
| 3 | 50 (45.0) | 18 (33.3) | 25 (46.3) | 18 (33.3) | ||
| 4 | 39 (35.1) | 14 (25.9) | 13 (24.1) | 14 (25.9) | ||
| 5 | 4 (3.6) | 2 (3.7) | 2 (3.7) | 2 (3.7) | ||
| APACHE II, n | 30.48 ± 6.85 | 29.43 ± 5.78 | 0.332 | 29.41 ± 5.81 | 29.43 ± 5.78 | 0.987 |
| SOFA, n | 7.86 ± 3.07 | 6.56 ± 3.04 | 0.011 | 6.89 ± 3.17 | 6.56 ± 3.04 | 0.578 |
| NUTRIC, n | 6.03 ± 1.07 | 5.94 ± 0.98 | 0.632 | 5.80 ± 0.88 | 5.94 ± 0.98 | 0.409 |
| HTN, n (%) | 67 (60.4) | 28 (51.9) | 0.299 | 29 (53.7) | 28 (51.9) | 0.847 |
| DM, n (%) | 35 (31.5) | 13 (24.1) | 0.322 | 13 (24.1) | 13 (24.1) | 1.000 |
| CRF, n (%) | 13 (11.7) | 7 (13.0) | 0.817 | 5 (9.3) | 7 (13.0) | 0.540 |
| Cancer, n (%) | 60 (54.1) | 26 (48.1) | 0.476 | 37 (68.5) | 26 (48.1) | 0.032 |
| Variable | Total PopulationHigh Risk (mNUTRIC ≥ 5) (n = 165) | Matched PopulationHigh Risk (mNUTRIC ≥ 5) (n = 108) | ||||
|---|---|---|---|---|---|---|
| Inadequate Nutrition (n = 111) | Adequate Nutrition (n = 54) | p Value | Inadequate Nutrition (n = 54) | Adequate Nutrition (n = 54) | p Value | |
| SBP < 100, n (%) | 96 (86.5) | 42 (77.8) | 0.156 | 45 (83.3) | 42 (77.8) | 0.466 |
| Vasopressors use, n (%) | 79 (71.2) | 31 (57.4) | 0.078 | 35 (64.8) | 31 (57.4) | 0.430 |
| CRRT, n (%) | 41 (36.9) | 12 (22.2) | 0.058 | 12 (22.2) | 12 (22.2) | 1.000 |
| Diagnosis, n (%) | 0.894 | 0.940 | ||||
| Perforation | 80 (72.1) | 40 (74.1) | 41 (75.9) | 40 (74.1) | ||
| Strangulation | 18 (16.2) | 9 (16.7) | 9 (16.7) | 9 (16.7) | ||
| Ischemia | 13 (11.7) | 5 (9.3) | 4 (7.4) | 5 (9.3) | ||
| Primary infection source, n (%) | 0.769 | 0.818 | ||||
| Stomach | 19 (17.1) | 9 (16.7) | 9 (16.7) | 9 (16.7) | ||
| Small bowel | 41 (36.9) | 23 (42.6) | 20 (37.0) | 23 (42.6) | ||
| Colorectal | 51 (45.9) | 22 (40.7) | 25 (46.3) | 22 (40.7) | ||
| Laparoscopy/Open, n (%) | 8 (7.2)/103 (92.8) | 4 (7.4)/50 (92.6) | 0.963 | 4 (7.4)/50 (92.6) | 4 (7.4)/50 (92.6) | 1.000 |
| Variable | Total PopulationHigh Risk (mNUTRIC ≥ 5) (n = 165) | Matched PopulationHigh Risk (mNUTRIC ≥ 5) (n = 108) | ||||
|---|---|---|---|---|---|---|
| Inadequate Nutrition (n = 111) | Adequate Nutrition (n = 54) | p Value | Inadequate Nutrition (n = 54) | Adequate Nutrition (n = 54) | p Value | |
| Required calorie, kcal | 1513.45 ± 321.64 | 1327.87 ± 223.92 | <0.001 | 1366.34 ± 282.91 | 1327.87 ± 223.92 | 0.435 |
| Calorie adequacy, % | 44.07 ± 14.82 | 88.12 ± 17.37 | <0.001 | 46.50 ± 13.39 | 88.12 ± 17.37 | <0.001 |
| EN within 5 days, n (%) | 26 (23.4) | 11 (20.4) | 0.659 | 13 (24.1) | 11 (20.4) | 0.643 |
| PN supplement within 5 days, n (%) | 54 (48.6) | 47 (87.0) | <0.001 | 26 (48.1) | 47 (87.0) | <0.001 |
| Variables | Total PopulationHigh Risk (mNUTRIC ≥ 5) (n = 165) | Matched PopulationHigh Risk (mNUTRIC ≥ 5) (n = 108) | ||||
|---|---|---|---|---|---|---|
| Inadequate Nutrition (n = 111) | Adequate Nutrition (n = 54) | p Value | Inadequate Nutrition (n = 54) | Adequate Nutrition (n = 54) | p Value | |
| In-hospital mortality, n (%) | 48 (43.2) | 13 (24.1) | 0.017 | 21 (38.9) | 13 (24.1) | 0.097 |
| 30-day mortality, n (%) | 38 (34.2) | 6 (11.1) | 0.002 | 17 (31.5) | 6 (11.1) | 0.010 |
| MV-free day, median (Q1, Q3), d | 27 (12.0, 29.0) | 26 (18.0, 29.0) | 0.993 | 25 (17.0, 28.0) | 28 (21.0, 29.0) | 0.131 |
| ICU-free day, (Q1, Q3), d | 22 (1.5, 26.0) | 22.5 (9.0, 26.0) | 0.747 | 20.5(6.0, 26.0) | 24 (7.0, 26.0) | 0.535 |
| HLOS, median (Q1, Q3), d | 22 (14.0, 36.0) | 24 (16.0, 50.0) | 0.227 | 23.5 (15.0, 39.0) | 24 (16.0, 50.0) | 0.645 |
| IAI, n (%) | 31 (27.9) | 13 (24.1) | 0.599 | 13 (24.1) | 13 (24.1) | 1.000 |
| Pulmonary complication, n (%) | 60 (54.1) | 31 (57.4) | 0.684 | 31 (57.4) | 33 (61.1) | 0.695 |
| Wound complication, n (%) | 36 (32.4) | 19 (35.2) | 0.725 | 15 (27.8) | 19 (35.2) | 0.407 |
| Postoperative leak, n (%) | 19 (17.1) | 6 (11.1) | 0.313 | 6 (11.1) | 6 (11.1) | 1.000 |
| Infection, n (%) | 64 (57.7) | 28 (51.9) | 0.481 | 27 (50.0) | 28 (51.9) | 0.847 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, Y.T.; Park, J.Y.; Jeon, J.; Kim, M.J.; Lee, S.H.; Lee, J.G. Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score. Nutrients 2018, 10, 1589. https://doi.org/10.3390/nu10111589
Jung YT, Park JY, Jeon J, Kim MJ, Lee SH, Lee JG. Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score. Nutrients. 2018; 10(11):1589. https://doi.org/10.3390/nu10111589
Chicago/Turabian StyleJung, Yun Tae, Jung Yun Park, Jiyeon Jeon, Myung Jun Kim, Seung Hwan Lee, and Jae Gil Lee. 2018. "Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score" Nutrients 10, no. 11: 1589. https://doi.org/10.3390/nu10111589
APA StyleJung, Y. T., Park, J. Y., Jeon, J., Kim, M. J., Lee, S. H., & Lee, J. G. (2018). Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score. Nutrients, 10(11), 1589. https://doi.org/10.3390/nu10111589





