Multilevel Structural Equation Modeling of Students’ Dietary Intentions/Behaviors, BMI, and the Healthfulness of Convenience Stores
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Young Adults’ Eating and Activity for the Health Sample
2.3. Young Adults’ Eating and Activity for Health Measures
2.3.1. Dietary Attitudes
2.3.2. Dietary Intake
2.3.3. Demographics
2.3.4. Anthropometrics
2.4. Environmental Audit Food Store Sample
2.5. Environmental Audit Food Store Measures
2.6. Analysis
3. Results
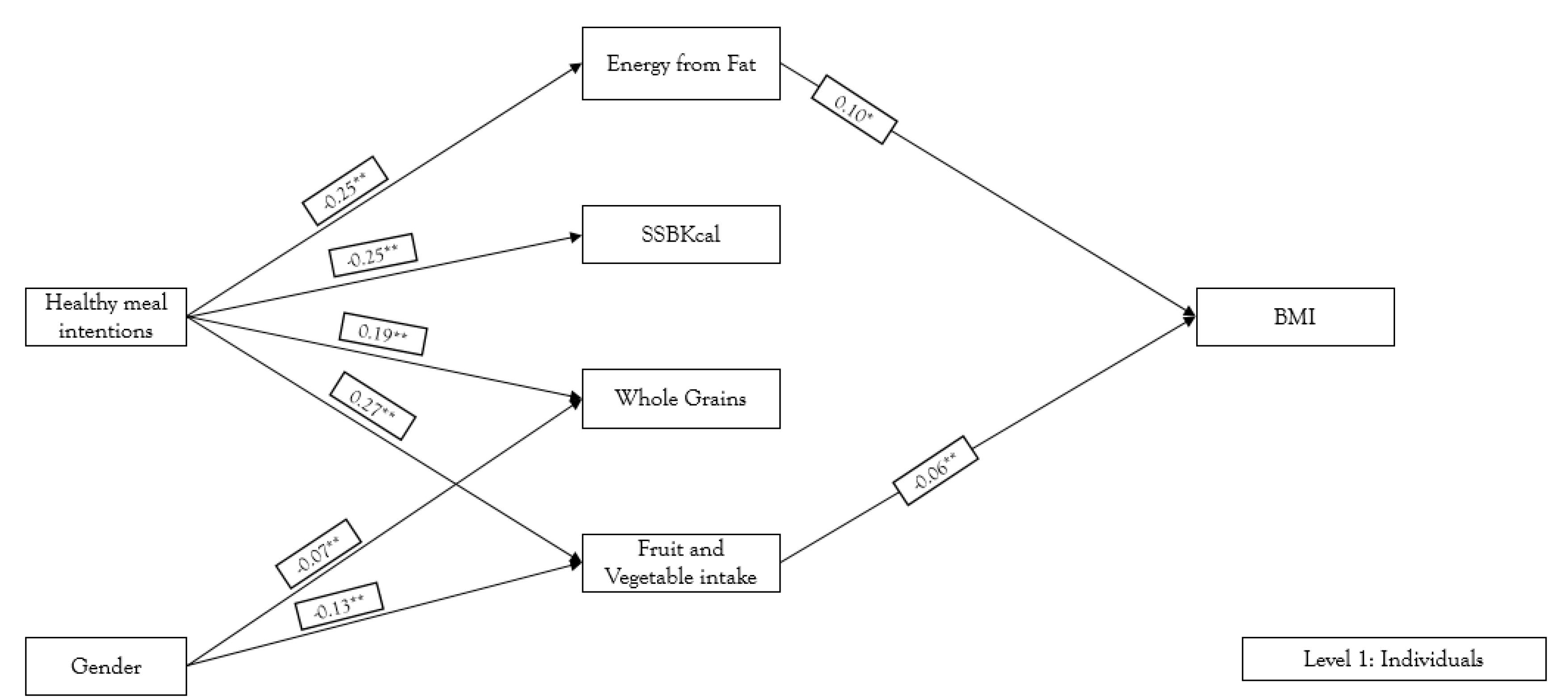
3.1. Individual Level Analysis
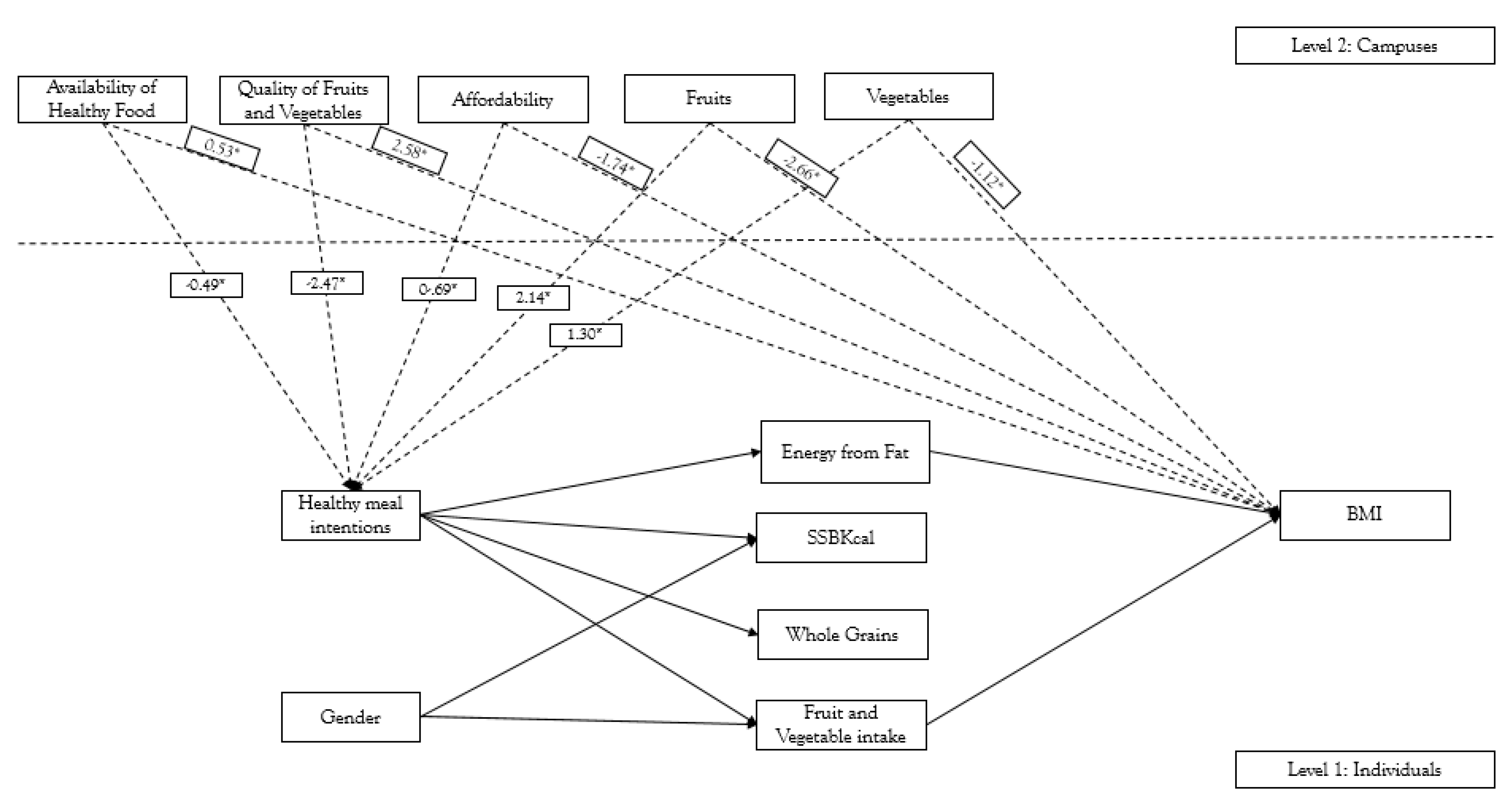
3.2. Campus Level Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cerin, E.; Frank, L.D.; Sallis, J.F.; Saelens, B.E.; Conway, T.L.; Chapman, J.E.; Glanz, K. From neighborhood design and food options to residents’ weight status. Appetite 2011, 56, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Diez-Roux, A.V.; Nettleton, J.A.; Lazo, M.; Brancati, F.; Caballero, B.; Glass, T.; Moore, L.V. Availability of healthy foods and dietary patterns: The Multi-Ethnic Study of Atherosclerosis. Am. J. Clin. Nutr. 2009, 89, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, A.; Hankins, S.; Jilcott, S. Measures of the consumer food store environment: a systematic review of the evidence 2000–2011. J. Community Health 2011, 37, 897–911. [Google Scholar] [CrossRef] [PubMed]
- Izumi, B.T.; Zenk, S.N.; Schulz, A.J.; Mentz, G.B.; Wilson, C. Associations between neighborhood availability and individual consumption of dark-green and orange vegetables among ethnically diverse adults in detroit. J. Am. Diet. Assoc. 2011, 111, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Hermstad, A.K.; Swan, D.W.; Kegler, M.C.; Barnette, J.K.; Glanz, K. Individual and environmental correlates of dietary fat intake in rural communities: a structural equation model analysis. Soc. Sci. Medicine 2010, 71, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Bodor, J.N.; Rose, D.; Farley, T.A.; Swalm, C.; Scott, S.K. Neighbourhood fruit and vegetable availability and consumption: The role of small food stores in an urban environment. Public Health Nutr. 2008, 11. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, E.M.; Miller, K.M.; DuBow, W.M.; Wytinck, S.M. Perceived access to fruits and vegetables associated with increased consumption. Public Health Nutr. 2009, 12, 1743–1750. [Google Scholar] [CrossRef] [PubMed]
- Michimi, A.; Wimberly, M.C. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous united states. Int. J. Heal. Geogr. 2010, 9, 49. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Lachance, L.L.; Schulz, A.J.; Mentz, G.; Kannan, S.; Ridella, W. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am. J. Heal. Promot. 2009, 23, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Boone-Heinonen, J.; Gordon-Larsen, P.; Kiefe, C.I.; Shikany, J.M.; Lewis, C.E.; Popkin, B.M. Fast food restaurants and food stores: Longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch. Intern. Med. 2011, 171, 1162–1170. [Google Scholar] [CrossRef] [PubMed]
- Caspi, C.E.; Sorensen, G.; Subramanian, S.V.; Kawachi, I. The local food environment and diet: a systematic review. Health Place 2012, 18, 1172–1187. [Google Scholar] [CrossRef] [PubMed]
- Cummins, S.; Flint, E.; Matthews, S.A. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Heal. Aff. 2014, 33, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, A.A.; Sharkey, J.; Samuel-Hodge, C.D.; Jones-Smith, J.; Folds, M.C.; Cai, J.; Ammerman, A.S. Perceived and objective measures of the food store environment and the association with weight and diet among low-income women in north carolina. Public Heal. Nutr. 2011, 14, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Hickson, D.A.; Diez Roux, A.V.; Smith, A.E.; Tucker, K.L.; Gore, L.D.; Zhang, L.; Wyatt, S.B. Associations of fast food restaurant availability with dietary intake and weight among african americans in the jackson heart study, 2000–2004. Am. J. Public Heal. 2011, 101, S301–S309. [Google Scholar] [CrossRef] [PubMed]
- Hollands, S.; Campbell, M.K.; Gilliland, J.; Sarma, S. A spatial analysis of the association between restaurant density and body mass index in Canadian adults. Prev. Med. 2013, 57, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Reitzel, L.R.; Regan, S.D.; Nguyen, N.; Cromley, E.K.; Strong, L.L.; Wetter, D.W.; McNeill, L.H. Density and proximity of fast food restaurants and body mass index among african americans. Am. J. Public Heal. 2014, 104, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Yan, R.; Bastian, N.D.; Griffin, P.M. Association of food environment and food retailers with obesity in us adults. Heal. Place 2015, 33, 19–24. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Tucker, P.; Gilliland, J.; Irwin, J.D.; Larsen, K.; Hess, P. The influence of local food environments on adolescents' food purchasing behaviors. Int. J. Environ. Res. Public Health 2012, 9, 1458–1471. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.A.; Boone-Heinonen, J.; Duffey, K.J.; Rodriguez, D.A.; Kiefe, C.I.; Lewis, C.E.; Gordon-Larsen, P. Combined measure of neighborhood food and physical activity environments and weight-related outcomes: the cardia study. Health Place 2015, 33, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Farley, T.A.; Rice, J.; Bodor, J.N.; Cohen, D.A.; Bluthenthal, R.N.; Rose, D. Measuring the food environment: shelf space of fruits, vegetables, and snack foods in stores. J. Urban Heal. 2009, 86, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Snyder, T.D.; Dillow, S.A. Digest of Education Statistics 2013 (NCES 2015-011); N.C.f.E. Statistics, Ed.; Institute of Education Sciences: Washington, DC, USA, 2015. [Google Scholar]
- Horacek, T.M.; Erdman, M.B.; Reznar, M.M.; Olfert, M.; Brown-Esters, O.N.; Kattelmann, K.K.; Kidd, T.; Koenings, M.; Phillips, B.; Quick, V.; et al. Evaluation of the food store environment on and near the campus of 15 postsecondary institutions. Am. J. Heal. Promot. 2013, 27, e81–e90. [Google Scholar] [CrossRef] [PubMed]
- Kapinos, K.A.; Yakusheva, O. Environmental influences on young adult weight gain: evidence from a natural experiment. J. Adolesc. Heal. 2011, 48, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Kapinos, K.A.; Yakusheva, O.; Eisenberg, D. Obesogenic environmental influences on young adults: evidence from college dormitory assignments. Econ. Hum. Biol. 2014, 12, 98–109. [Google Scholar] [CrossRef] [PubMed]
- LaCaille, L.; Dauner, K.N.; Krambeer, R.; Pedersen, J. Psychosocial and environmental determinants of eating behaviors, physical activity, and weight change among college students: a qualitative analysis. J. Am. Coll. Heal. 2011, 59, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, S.K. Development of the University Health Index to Examine the Interface between Campus Environment and Nutrition, Physical Activity, and Weight in College Students. Virginia Polytechnic Institute and State University: Blacksburg, VA, USA, 2011. [Google Scholar]
- Laska, M.N.; Hearst, M.O.; Forsyth, A.; Pasch, K.E.; Lytle, L. Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? Public Heal. Nutr. 2010, 13, 1757–1763. [Google Scholar] [CrossRef] [PubMed]
- Lowry, R.; Galuska, D.A.; Fulton, J.E.; Wechsler, H.; Kann, L.; Collins, J.L. Physical activity, food choice, and weight management goals and practices among US college students. Am. J. Prev. Med. 2000, 18, 18–27. [Google Scholar] [CrossRef]
- Nelson, M.C.; Story, M.; Larson, N.I.; Neumark-Sztainer, D.; Lytle, L.A. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity 2008, 16, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Arnett, J. Conceptions of the Transition to Adulthood: Perspectives from Adolescence through Midlife. J. Adult Develop. 2011, 8, 133–143. [Google Scholar] [CrossRef]
- Park, M.J.; Scott, J.T.; Adams, S.H.; Brindis, C.D.; Irwin, C.E. Adolescent and young adult health in the united states in the past decade: little improvement and young adults remain worse off than adolescents. J. Adolesc. Health 2014, 55, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Fedewa, M.V.; Das, B.M.; Evans, E.M.; Dishman, R.K. Change in weight and adiposity in college students: A systematic review and meta-analysis. Am. J. Prev. Med. 2014, 47, 641–652. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.S.; Simmons, K.P.; Connell, L.J.; Ulrich, P.V. Weight and Body Composition Changes during the First Three Years of College. J. Obes. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.S.; Simmons, K.P.; Connell, L.J.; Ulrich, P.V. Changes in body weight, composition, and shape: a 4-year study of college students. Appl. Physiol. Nutr. Metab. 2012, 37, 1118–1123. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Richardson, E.E.; Bailey, S.; Fava, J.L.; Wing, R.; Tobacco Etiology Research Network (TERN). A prospective study of weight gain during the college freshman and sophomore years. Prev. Med. 2009, 48, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Racette, S.B.; et al. Weight changes, exercise, and dietary patterns during freshman and sophomore years of college. J. Am. Coll. Health 2005, 53, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Racette, S.B.; Deusinger, S.S.; Strube, M.J.; Highstein, G.R.; Deusinger, R.H. Changes in weight and health behaviors from freshman through senior year of college. J. Nutr. Educ. Behav. 2008, 40, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Boek, S.; Bianco-Simeral, S.; Chan, K.; Goto, K. Gender and race are significant determinants of students’ food choices on a college campus. J. Nutr. Educ. Behav. 2012, 44, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Greene, G.W.; Schembre, S.M.; White, A.A.; Hoerr, S.L.; Lohse, B.; Shoff, S.; Horacek, T.; Riebe, D.; Patterson, J.; Phillips, B.W.; et al. Identifying clusters of college students at elevated health risk based on eating and exercise behaviors and psychosocial determinants of body weight. J. Am. Diet. Assoc. 2011, 111, 394–400. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.S.; Oliver, M.; Simnadis, T.; Beck, E.J.; Coltman, T.; Iverson, D.; Caputi, P.; Sharma, R. The theory of planned behaviour and dietary patterns: A systematic review and meta-analysis. Prev. Med. 2015, 81, 150–156. [Google Scholar] [CrossRef] [PubMed]
- van’t Riet, J.; Sijtsema, S.J.; Dagevos, H.; De Bruijn, G.J. The importance of habits in eating behaviour. An overview and recommendations for future research. Appetite 2011, 57, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.; Monsivais, P.; Cook, A.J.; Drewnowski, A. Positive attitude toward healthy eating predicts higher diet quality at all cost levels of supermarkets. J. Acad. Nutr. Diet. 2014, 114, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: a Social Cognitive Theory. Prentice Hall: Upper Saddle River, NJ, USA, 1986. [Google Scholar]
- Kattelmann, K.K.; Bredbenner, C.B.; White, A.A.; Greene, G.W.; Hoerr, S.L.; Kidd, T.; Colby, S.; Horacek, T.M.; Phillips, B.W.; Koenings, M.M.; et al. The effects of young adults eating and active for health (yeah): a theory-based web-delivered intervention. J. Nutr. Educ. Behav. 2014, 46, S27–S41. [Google Scholar] [CrossRef] [PubMed]
- Brown, O.; Quick, V.; Colby, S.; Greene, G.; Horacek, T.M.; Hoerr, S.; Koenings, M.; Kidd, T.; Morrell, J.; Olfert, M.; et al. Recruitment lessons learned from a tailored web-based health intervention project y.e.a.h. (Young Adults Eating and Active for Health). Heal. Educ. 2015, 115, 470–479. [Google Scholar] [CrossRef]
- Strong, K.A.; Parks, S.L.; Anderson, E.; Winett, R.; Davy, B.M. Weight gain prevention: identifying theory-based targets for health behavior change in young adults. J. Am. Diet. Assoc. 2008, 108, 1708–1715. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.E.; Midthune, D.; Subar, A.F.; Kahle, L.L.; Schatzkin, A.; Kipnis, V. Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage energy from fat and fibre. Public Heal. Nutr. 2004, 7. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.E.; Midthune, D.; Subar, A.F.; Kipnis, V.; Kahle, L.L.; Schatzkin, A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J. Am. Diet. Assoc. 2007, 107, 760–767. [Google Scholar] [CrossRef] [PubMed]
- West, D.S.; Bursac, Z.; Quimby, D.; Prewitt, T.E.; Spatz, T.; Nash, C.; Mays, G.; Eddings, K. Self-reported sugar-sweetened beverage intake among college students*. Obesity 2006, 14, 1825–1831. [Google Scholar] [CrossRef] [PubMed]
- ChooseMyPlate.gov. Available online: http://www.choosemyplate.gov/food-groups/grains-counts.html (accessed on 1 September 2008).
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Nutrition environment measures survey in stores (NEMS-S): Development and evaluation. Am. J. Prev. Med. 2007, 32, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide; 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. Lisrel-VI User’s Guide; Scientific Software.: Mooresville, IN, USA, 1984. [Google Scholar]
- Bollen, K.A.; Long, J.S. Alternative ways of assessing model fit. In Testing Structural Equation Models; Sage: Beverly Hills, CA, USA, 1993. [Google Scholar]
- Cluskey, M.; Grobe, D. College weight gain and behavior transitions: Male and female differences. J. Am. Diet. Assoc. 2009, 109, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Adriaanse, M.A.; Vinkers, C.D.; De Ridder, D.T.; Hox, J.J.; De Wit, J.B. Do implementation intentions help to eat a healthy diet? A systematic review and meta-analysis of the empirical evidence. Appetite 2011, 56, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Cobb, L.K.; Appel, L.J.; Franco, M.; Jones-Smith, J.C.; Nur, A.; Anderson, C.A. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity (Silver Spring) 2015, 23, 1331–1344. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, S.S.; Franco, M.; Gittelsohn, J.; Zonderman, A.B.; Evans, M.K.; Fanelli Kuczmarski, M.; Gary-Webb, T.L. Healthy food availability and the association with BMI in Baltimore, Maryland. Public Health Nutr. 2011, 14, 1001–1007. [Google Scholar] [CrossRef] [PubMed]
- Ruff, R.R.; Akhund, A.; Adjoian, T. Small convenience stores and the local food environment: an analysis of resident shopping behavior using multilevel modeling. Am. J. Heal. Promot. 2016, 30, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Fennis, B.M.; Adriaanse, M.A.; Stroebe, W.; Pol, B. Bridging the intention–behavior gap: inducing implementation intentions through persuasive appeals. J. Consum. Psychol. 2011, 21, 302–311. [Google Scholar] [CrossRef]
- Freedman, M.R.; Connors, R. Point-of-purchase nutrition information influences food-purchasing behaviors of college students: a pilot study. J. Am. Diet. Assoc. 2010, 110, 1222–1226. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Zhao, Z.; Wang, Y. Food prices and fruit and vegetable consumption among young american adults. Heal. Place 2009, 15, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Pearson, T.; Russell, J.; Campbell, M.J.; Barker, M.E. Do ‘food deserts’ influence fruit and vegetable consumption?--A cross-sectional study. Appetite 2005, 45, 195–197. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.J.; Pelletier, J.E.; Neumark-Sztainer, D.; Lust, K.; Laska, M.N. Perceived social-ecological factors associated with fruit and vegetable purchasing, preparation, and consumption among young adults. J. Acad. Nutr. Diet. 2013, 113, 1366–1374. [Google Scholar] [CrossRef] [PubMed]
- Kothe, E.J.; Mullan, B.A. A randomised controlled trial of a theory of planned behaviour to increase fruit and vegetable consumption. Fresh Facts. Appetite 2014, 78, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Kersten, E.; Laraia, B.; Kelly, M.; Adler, N.; Yen, I. Small food stores and availability of nutritious foods: a comparison of database and in-store measures, northern california, 2009. Prev. Chronic Dis. 2012. [Google Scholar] [CrossRef]
- Gittelsohn, J.; Dennisuk, L.A.; Christiansen, K.; Bhimani, R.; Johnson, A.; Alexander, E.; Lee, M.; Lee, S.H.; Rowan, M.; Coutinho, A.J. Development and implementation of baltimore healthy eating zones: a youth-targeted intervention to improve the urban food environment. Heal. Educ. Res. 2013, 28, 732–744. [Google Scholar] [CrossRef] [PubMed]
- Gittelsohn, J.; Rowan, M.; Gadhoke, P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Prev. Chronic Dis. 2012. [Google Scholar] [CrossRef]
- Gudzune, K.; Hutfless, S.; Maruthur, N.; Wilson, R.; Segal, J. Strategies to prevent weight gain in workplace and college settings: A systematic review. Prev. Med. 2013, 57, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Gebauer, H.; Laska, M.N. Convenience stores surrounding urban schools: an assessment of healthy food availability, advertising, and product placement. J. Urban Heal. 2011, 88, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, J.R.; Dean, W.R.; Nalty, C. Convenience stores and the marketing of foods and beverages through product assortment. Am. J. Prev. Medicine 2012, 43, S109–S115. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Powell, L.M.; Rimkus, L.; Isgor, Z.; Barker, D.C.; Ohri-Vachaspati, P.; Chaloupka, F. Relative and absolute availability of healthier food and beverage alternatives across communities in the united states. Am. J. Public Heal. 2014, 104, 2170–2178. [Google Scholar] [CrossRef] [PubMed]
- Blondin, S.A.; Mueller, M.P.; Bakun, P.J.; Choumenkovitch, S.F.; Tucker, K.L.; Economos, C.D. Cross-sectional associations between empirically-derived dietary patterns and indicators of disease risk among university students. Nutrients 2015, 8. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; Laska, M.N.; Story, M.; Neumark-Sztainer, D. Predictors of fruit and vegetable intake in young adulthood. J. Acad. Nutr. Diet. 2012, 112, 1216–1222. [Google Scholar] [CrossRef] [PubMed]
- Allan, J.L.; Johnston, M.; Campbell, N. Snack purchasing is healthier when the cognitive demands of choice are reduced: a randomized controlled trial. Heal. Psychol. 2015, 34, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Hartman, H.; Wadsworth, D.P.; Penny, S.; van Assema, P.; Page, R. Psychosocial determinants of fruit and vegetable consumption among students in a new zealand university. Results of focus group interviews. Appetite 2013, 65, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V.; Diez Roux, A.V.; Franco, M. Measuring availability of healthy foods: agreement between directly measured and self-reported data. Am. J. Epidemiology 2012, 175, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V.; Diez Roux, A.V.; Nettleton, J.A.; Jacobs, D.R. Associations of the local food environment with diet quality--a comparison of assessments based on surveys and geographic information systems: the multi-ethnic study of atherosclerosis. Am. J. Epidemiology 2008, 167, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Minaker, L.M.; Raine, K.D.; Wild, T.C.; Nykiforuk, C.I.; Thompson, M.E.; Frank, L.D. Objective food environments and health outcomes. Am. J. Prev. Med. 2013, 45, 289–296. [Google Scholar] [CrossRef] [PubMed]
| Variable | Statistics % (n) | χ2 | p |
|---|---|---|---|
| Age | Mean ± SD (19.33 ± 1.07) | ||
| BMI category | 803.77 (df = 2) | <0.001 | |
| Normal weight | 67.9% (951) | ||
| Overweight | 23.6% (330) | ||
| Obese | 8.4% (118) | ||
| Gender | 141.34 (df = 1) | <0.001 | |
| Male | 34.1% (478) | ||
| School Year | 935.58 (df = 4) | <0.001 | |
| Freshman | 38.7% (542) | ||
| Sophomore | 34.5% (484) | ||
| Junior | 23.9% (335) | ||
| Senior | 1.3% (18) | ||
| Residence | 2471.54 (df = 5) | <0.001 | |
| On campus residence hall | 63.4% (888) | ||
| On campus sorority or fraternity | 3.8% (53) | ||
| On campus-other college housing | 7.6% (107) | ||
| Off campus housing | 20.6% (289) | ||
| Off campus parent/guardian’s home | 2.4% (34) | ||
| Off campus -other | 0.8% (11) | ||
| Race | 2777.61 (df = 5) | <0.001 | |
| White | 64.6% (905) | ||
| Black or African American | 12.9% (181) | ||
| Asian | 9.0% (126) | ||
| American Indian or Alaska Native | 0.8% (11) | ||
| Native Hawaiian or Other Pacific Islander | 0.5% (7) | ||
| Other | 4.0% (56) | ||
| Ethnicity | |||
| Hispanic | 5.7% (80) | ||
| Convenience Store Variables | Mean ± SD | ||
| Healthy food affordability | 8.11 ± 0.09 | ||
| Healthy food availability | 9.75 ± 2.91 | ||
| Fruit/vegetable quality | 2.19 ± 1.85 | ||
| Fruit availability | 1.63 ± 0.64 | ||
| Vegetable availability | 1.05 ± 0.65 |
| Individual Variables | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | Mean | ± SD |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | 1.0 | |||||||||
| 2. BMI | −0.059 ** | 1.0 | 24.13 | 4.31 | ||||||
| 3. Healthful meal intentions | 0.212 ** | −0.043 | 1.0 | 3.19 | 0.77 | |||||
| 4. Healthful meal behaviors | 0.145 ** | −0.127 ** | 0.681 ** | 1.0 | 3.32 | 0.77 | ||||
| 5. % kcal/ Fat/day | −0.019 | 0.125 ** | −0.244 ** | −0.300 ** | 1.0 | 31.18 | 5.06 | |||
| 6. SSB kcal/day | −0.134 ** | 0.054 * | −0.263 ** | −0.284 ** | 0.300 ** | 1.0 | 157.45 | 243.28 | ||
| 7. Whole grain/day | −0.026 | −0.037 | 0.171 ** | 0.231 ** | −0.115 ** | −0.101 ** | 1.0 | 2.07 | 1.48 | |
| 8. F/V intake/day | −0.075 * | −0.065 * | 0.2420 ** | 0.373 ** | −0.098 ** | −0.003 | 0.168 ** | 1.0 | 2.72 | 2.33 |
| Individual Variables | Male | Female | t-Value (df = 1399) | p | ||
|---|---|---|---|---|---|---|
| Mean | ± SD | Mean | ± SD | |||
| BMI | 24.48 | ± 3.97 | 23.95 | ± 4.47 | 2.273 | <0.05 |
| Healthful meal intentions | 2.97 | ± 0.82 | 3.31 | ± 0.72 | −7.672 | <0.001 |
| Healthful meal behaviors | 3.17 | ± 0.79 | 3.40 | ± 0.74 | −5.300 | <0.001 |
| % kcal/fat/day | 31.31 | ± 4.74 | 31.11 | ± 5.22 | 0.686 | NS |
| SSB/kcal/day | 202.90 | ± 276.74 | 134.21 | ± 220.84 | 4.614 | <0.001 |
| Whole grain servings/day | 2.12 | ± 2.12 | 2.04 | ± 1.44 | 0.926 | NS |
| Fruit and vegetable intake cups/day | 2.97 | ± 2.97 | 2.60 | ± 2.27 | 2.651 | <0.05 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horacek, T.; Dede Yildirim, E.; Kattelmann, K.; Byrd-Bredbenner, C.; Brown, O.; Colby, S.; Greene, G.; Hoerr, S.; Kidd, T.; Koenings, M.; et al. Multilevel Structural Equation Modeling of Students’ Dietary Intentions/Behaviors, BMI, and the Healthfulness of Convenience Stores. Nutrients 2018, 10, 1569. https://doi.org/10.3390/nu10111569
Horacek T, Dede Yildirim E, Kattelmann K, Byrd-Bredbenner C, Brown O, Colby S, Greene G, Hoerr S, Kidd T, Koenings M, et al. Multilevel Structural Equation Modeling of Students’ Dietary Intentions/Behaviors, BMI, and the Healthfulness of Convenience Stores. Nutrients. 2018; 10(11):1569. https://doi.org/10.3390/nu10111569
Chicago/Turabian StyleHoracek, Tanya, Elif Dede Yildirim, Kendra Kattelmann, Carol Byrd-Bredbenner, Onikia Brown, Sarah Colby, Geoffrey Greene, Sharon Hoerr, Tandalayo Kidd, Mallory Koenings, and et al. 2018. "Multilevel Structural Equation Modeling of Students’ Dietary Intentions/Behaviors, BMI, and the Healthfulness of Convenience Stores" Nutrients 10, no. 11: 1569. https://doi.org/10.3390/nu10111569
APA StyleHoracek, T., Dede Yildirim, E., Kattelmann, K., Byrd-Bredbenner, C., Brown, O., Colby, S., Greene, G., Hoerr, S., Kidd, T., Koenings, M., Morrell, J., Olfert, M. D., Phillips, B., Shelnutt, K., & White, A. (2018). Multilevel Structural Equation Modeling of Students’ Dietary Intentions/Behaviors, BMI, and the Healthfulness of Convenience Stores. Nutrients, 10(11), 1569. https://doi.org/10.3390/nu10111569






