The Feasibility and Acceptability of Two Methods of Snack Portion Control in United Kingdom (UK) Preschool Children: Reduction and Replacement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Design
2.3. Procedure
2.4. Materials and Measures
2.4.1. Anthropometrics
2.4.2. Screening Questionnaire
2.4.3. Food Frequency Questionnaire (FFQ)
2.4.4. Parent and Child Characteristics
2.4.5. Acceptability Questionnaire
2.4.6. Follow-Up Questionnaire
2.4.7. Food Diary
2.5. Data Analysis
2.5.1. Qualitative
2.5.2. Quantitative
3. Results
3.1. Demographics
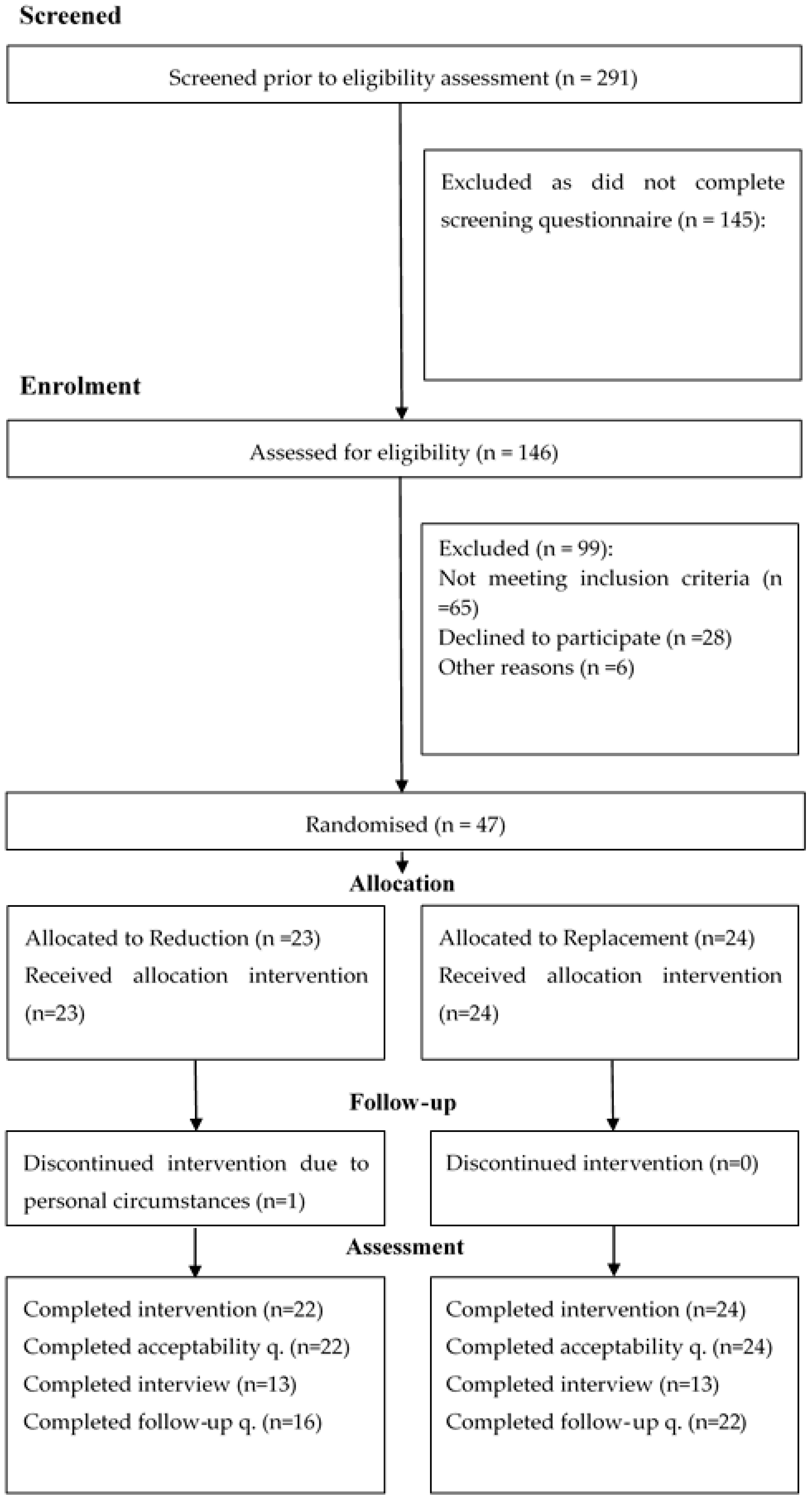
3.2. Participant Recruitment and Retention
3.3. Feasibility
3.3.1. Theme 1: In the Care of Others
3.3.2. Theme 2: Children’s Health and Behaviour
3.3.3. Theme 3: Maternal Organisation
3.4. Acceptability
3.4.1. Recording in the Food Diary
3.4.2. Week 2 Snacks
3.4.3. Week 3 Snacks
3.4.4. Sustainability of the Intervention
3.4.5. Theme 1: Recording in the Food Diary
3.4.6. Theme 2: Snack Type
3.4.7. Theme 3: Snack Preparation and Serving Method
3.4.8. Theme 4: Willingness to Continue with the Intervention
3.5. Preliminary Effects of the Intervention
3.5.1. Vegetable Intake
3.5.2. Fruit Intake
3.5.3. Energy (Mean Intake kcal/day)
3.5.4. Sugar Intake
3.5.5. Fat Intake
3.5.6. Mean Number of Snacks (LED and HED) Consumed per Day
3.5.7. Predictors of Nutritional Intake
3.6. Longer Term Effects of the Intervention on Snack Frequency (4–6 Weeks Follow-Up)
3.6.1. Theme 1: Change to Habitual Feeding Practices
3.6.2. Theme 2: Impact on Consumption
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix
| 1. Please circle the group you were assigned to in the study | ||||
| Reduction | Replacement | |||
| THINK ABOUT THE SECOND WEEK OF THE STUDY WHEN WE PROVIDED THE SNACKS FOR YOUR CHILD | ||||
| 2. The type of snacks provided in the snack pack for week two were appropriate for my child | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 3. My child liked the snacks in week two | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 4. The snacks offered during this week were similar to the snacks my child would normally eat | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| THINK ABOUT THE THIRD WEEK OF THE STUDY WHEN WE ASKED YOU TO REPLACE OR REDUCE YOUR CHILD’S SNACKS | ||||
| 5. My child’s hunger was satisfied by the snacks in week three | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 6. My child was happy with the snacks in week three | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 7. My child noticed the changes to his/her snacks | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 8. My child noticed the changes to his/her drinks | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 9. Keeping the food diary was inconvenient | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 10. Keeping the food diary was difficult | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 11. Keeping the food diary was helpful | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 12. Whilst keeping the food diary I chose different foods in order to make record keeping easier | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 13. How willing would you be to use this method to reduce your child’s portion sizes? | ||||
| Very unwilling | Unwilling | Neither willing nor unwilling | Willing | Very willing |
| 14. How likely is this method to make permanent changes to your child’s eating habits? | ||||
| Very unlikely | Unlikely | Neither likely nor unlikely | Likely | Very likely |
| 15. I found it easy to change my child’s snacks | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| 16. I found it easy to change my child’s drinks | ||||
| Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly Agree |
| Theme | Sub Theme | Supporting Quotations |
|---|---|---|
| 1: Reasons for non-compliance | 1.1 In the care of others | “Nursery aren’t going to follow the plan as the management aren’t happy with the snacks” (P190, Reduction, male, 22 months) |
| “some days at nursery she didn’t want what she was having in her bag but I told them that she’s not meant to be isolated with it” (P77, Replacement, female, 49 months) | ||
| “I felt like sometimes I didn’t want to put too much imposition on them, I felt sorry for my mother-in-law having to deal with him screaming” (P214, Replacement, male, 30 months) | ||
| “My mum and dad are terrible with him, giving him chocolate and things like that and my husbands a nightmare, like he gave him a mars bar from a celebration pack yesterday morning for breakfast and I was fuming because he knows that he can’t have that” (P74, Replacement, male, 30 months) | ||
| “In the morning he asked for snack and his dad gave the whole pack of jaffa cakes” (P2, Reduction, male, 39 months) | ||
| 1.2 Children’s health and behaviour | “He’s been ill; it has been really quite tricky because his appetite is not right. I want him to eat so I am more like have whatever you want. I was like you want crisps go get crisps” (P2, Reduction, male, 39 months) | |
| “The only problems I guess was when he was ill because it was hard to, because he wasn’t eating as normal. Trying to get him to eat, because he just didn’t want to” (P202, Replacement, male, age 29 months) | ||
| “She’s been crying, not happy, upset, so I’ve been giving her more tasty or unhealthy snack to be able to manage her behaviour. I gave her cookie at the doctors as she was upset” (P84, Reduction, female, 37 months) | ||
| “I just gave it to him. I said this is what you’ve got we are going to V club in half an hour, you either eat it or you don’t” (P104, Replacement, male, age 50 months | ||
| “I just stuck to my guns and said no you’re not having it. I mean it’s hard at the time but I stuck to my guns” (P34, Replacement, female, 48 months) | ||
| 1.3 Organisation | “it was okay because I just did it all at the beginning of the week, it felt a bit strange obviously getting rid of half of it, but mm it was okay. I was just more organised. I think by this stage I had cracked it” (P148, Reduction, female, 26 months) | |
| “It was kind of helpful to be prompted to be organised. so I would get everything ready the night before, so sometimes I would split one thing into two bags and then I would have another days bag full all ready to go, and that was really convenient” (P205, Reduction, female, 29 months) | ||
| “I was quite often forgetting to give half. With pom bears I gave her the pack forgetting that it should be half.” (P84, Reduction, female, 37 months) | ||
| 2: Acceptability | 2.1 Recording in the food diary | “I found it absolutely fine, it was just a case of remembering to weigh everything, but the instructions on how to do it was clear” (P199, Reduction, female, 34 months) |
| “easy, it was easy peasy. I just got it into my routine. I just wrote it every time, every meal, I wrote everything straight away, I weighed it, wrote it down, served it and then weighed what was left” (P33, Reduction, female, 39 months) | ||
| “it was just obviously when out and about when I didn’t have the scales it became a bit trickier because I realised I have no idea about how much things weigh at all” (P143, Replacement, male, 46 months) | ||
| 2.2 Snack Type | “I think that was fairly standard but then I think this week wasn’t all that dissimilar to what I would have been doing anyway” (P291, Replacement, female, 26 months) | |
| “I don’t think she cared really actually as long as she likes it she’ll eat it. She wasn’t asking for anything any different”. (P160, Replacement, female, 28 months) | ||
| “Pear, he wouldn’t touch pear, I tried him with the skin on, without the skin, I did all that with him”. (P74, Replacement, boy, age 30 months). | ||
| 2.3 Snack preparation and serving method | “it was obviously a little bit more faffy than the other one because you have to weigh it, erm, washing it and prepping it before you go out and stuff like that” (P132, Replacement, male, 45 months) | |
| “Like the crisps maybe I put them in a bowl or something like that so maybe that’s why she didn’t notice as much” (P20, Reduction, female, 52 months) | ||
| “I kind of tried to serve the half serving in the packet although she did question to where the other half was erm, I took half of them out and she knew then, she was like ‘I want more, there’s more’ so I gave her another one and she was okay” (P199, Reduction, female, 34 months). | ||
| 2.4 willingness to continue the intervention | “I will be carrying on and giving her, I’ll mix it all up and make sure I am offering more fruit and veg snacks definitely” (P77, Replacement, female, 49 months) | |
| “if you said you could give him anything as long as you give him half portions that would be fine with me, but giving him just these snacks (in the schedule), I don’t think I’d be able to do it” (P190, Reduction, male, 22 months) | ||
| 3. Longer term effects of the intervention | 3.1 Changes to habitual feeding practices | “The study helped me think more about what he was eating and whether he needed snacks. Also it has made me focus on his main meals more to keep them more balanced and healthy” (P261, Reduction, male, 56 months) |
| “The combinations of food I give as snacks has changed. I think it has introduced more variety. I now buy crackers, rather than crisps so often, and I give more vegetable snacks than before” (P104, Replacement, male, 50 months) | ||
| 3.2 Impact on consumption | “He is more willing to try other items, but that could be because I’ll offer different options over favourites” (P234, Replacement, male, 24 months) | |
| “She is tending to finish snacks and meals more often and waste less food” (P142, Reduction, female, 39 months) | ||
| “My 6year old now eats more fruit as a snack too” (P291, Replacement, female, 26 months) | ||
| “His sister now eats similar snacks to him and will ask for things like peppers rather than fruit” (P104, Replacement, male, 50 months) | ||
| “no, we have a food routine which we went back to” (P208, Replacement, male, 26 months) | ||
| ”No, she’s continued to have the same amount of snacks” (P199, Reduction, female, 34 months) |
References
- NDNS. National Diet and Nutrition Survey—GOV.U. 2016. Available online: https://www.gov.uk/government/collections/national-diet-and-nutrition-survey (accessed on 25 June 2018).
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Nicklaus, S.; Boggio, V.; Chabanet, C.; Issanchou, S. A prospective study of food variety seeking in childhood, adolescence and early adult life. Appetite 2005, 44, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Maher, J.; Fraser, S.; Lindsay, J. Between provisioning and consuming?: Children, mothers and “childhood obesity”. Heal. Sociol. Rev. 2010, 19, 304–316. [Google Scholar] [CrossRef]
- Wroten, K.C.; O’Neil, C.E.; Stuff, J.E.; Liu, Y.; Nicklas, T.A. Resemblance of dietary intakes of snacks, sweets, fruit, and vegetables among mother-child dyads from low income families. Appetite 2012, 59, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.L.; Hughes, S.O.; Cui, X.; Li, X.; Allison, D.B.; Liu, Y.; Goodell, S.L.; Nicklas, T.; Power, T.G.; Vollrath, K. Portion sizes for children are predicted by parental characteristics and the amounts parents serve themselves. Am. J. Clin. Nutr. 2014, 99, 763–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, N.; Story, M. A Review of Snacking Patterns among Children and Adolescents: What Are the Implications of Snacking for Weight Status? Child. Obes. 2013, 9, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Dunford, E.K.; Popkin, B.M. 37 year snacking trends for US children 1977–2014. Pediatr. Obes. 2018, 13, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Piernas, C.; Popkin, B.M. Trends In Snacking Among, U.S. Children. Health Aff. 2010, 29, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Samuelson, G. Dietary habits and nutritional status in adolescents over Europe. An overview of current studies in the Nordic countries. Eur. J. Clin. Nutr. 2000, 154, S21–S28. [Google Scholar] [CrossRef]
- Albar, S.A.; Alwan, N.A.; Evans, C.E.; Cade, J.E. Is there an association between food portion size and BMI among British adolescents? Br. J. Nutr. 2014, 112, 841–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davison, K.K.; Blake, C.E.; Blaine, R.E.; Younginer, N.A.; Orloski, A.; Hamtil, H.A.; Ganter, C.; Bruton, Y.P.; Vaughn, A.E.; Fisher, J.O. Parenting around child snacking: Development of a theoretically-guided, empirically informed conceptual model. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 109. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, R.W.; Rydell, S.; Dunn, C.L.; Harnack, L.J.; Levine, A.S.; Pentel, P.R.; Baxter, J.E.; Walsh, E.M. Effects of portion size on chronic energy intake. Int. J. Behav. Nutr. Phys. Act. 2007, 4, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pearson, N.; Ball, K.; Crawford, D. Predictors of changes in adolescents’ consumption of fruits, vegetables and energy-dense snacks. Br. J. Nutr. 2011, 105, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Evans, E.W.; Jacques, P.F.; Dallal, G.E.; Sacheck, J.; Must, A. The role of eating frequency on total energy intake and diet quality in a low-income, racially diverse sample of schoolchildren. Public Health Nutr. 2015, 18, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Infant and Toddler Forum. Healthy Eating for Toddlers. Available online: https://www.infantandtoddlerforum.org/toddlers-to-preschool/portionsizes/portion-sizes-survey (accessed on 30 October 2017).
- Deming, D.M.; Reidy, K.C.; Fox, M.K.; Briefel, R.R.; Jacquier, E.; Eldridge, A.L. Cross-sectional analysis of eating patterns and snacking in the US Feeding Infants and Toddlers Study 2008. Public Health Nutr. 2017, 20, 1584–1592. [Google Scholar] [CrossRef] [PubMed]
- Kachurak, A.; Davey, A.; Bailey, R.L.; Fisher, J.O. Daily Snacking Occasions and Weight Status Among US Children Aged 1 to 5 Years. Obesity 2018, 26, 1034–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Public Health England. 2018 Change4Life Nutrition Campaign | Campaign Resource Centre. 2018. Available online: https://campaignresources.phe.gov.uk/resources/campaigns/66-2018-change4life-nutrition-campaign/overview (accessed on 5 February 2018).
- World Health Organization. WHO Calls on Countries to Reduce Sugars Intake among Adults and Children. 2016. Available online: http://www.who.int/mediacentre/news/releases/2015/sugar-guideline/en/ (accessed on 5 February 2018).
- United States Department of Agriculture. Center for Nutrition Policy and Promotion. Dietary Guidelines for Americans 2015–2020. Available online: https://www.cnpp.usda.gov/2015-2020-dietary-guidelines-americans (accessed on 1 June 2018).
- Scientific Advisory Committee on Nutrition. Carbohydrates and Health. 2015. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf (accessed on 1 June 2018).
- Blake, C.E.; Fisher, J.O.; Ganter, C.; Younginer, N.; Orloski, A.; Blaine, R.E.; Bruton, Y.; Davison, K.K. A qualitative study of parents’ perceptions and use of portion size strategies for preschool children’s snacks. Appetite 2015, 88, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J. The Psychology of Eating: From Healthy to Disordered Behavior, 2nd ed.; Wiley-Blackwell: Chichester, UK, 2010; p. 378, ISBN: 978-1-405-19120-3. [Google Scholar]
- Ogden, J. Health Psychology, 5th ed.; McGraw-Hill: Maidenhead, UK, 2012; p. 565, ISBN-10: 0-335-243835. [Google Scholar]
- Roe, L.S.; Meengs, J.S.; Birch, L.L.; Rolls, B.J. Serving a variety of vegetables and fruit as a snack increased intake in preschool children. Am. J. Clin. Nutr. 2013, 98, 693–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute for Health Research. Feasibility and pilot studies in NIHR NETSCC Glossary. 2013. Available online: https://www.nihr.ac.uk/glossary?letter=F&postcategory=-1 (accessed on 4 June 2018).
- Kazdin, A.E. Acceptability of child treatment techniques: The influence of treatment efficacy and adverse side effects. Behav. Ther. 1981, 12, 493–506. [Google Scholar] [CrossRef]
- Cocks, K.; Torgersonm, D.J. Sample size calculations for pilot randomized trials: A confidence interval approach. J. Clin. Epidemiol. 2013, 66, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Powell, H.; Mihalas, S.; Onwuegbuzie, A.J.; Suldo, S.; Daley, C.E. Mixed methods research in school psychology: A mixed methods investigation of trends in the literature. Psychol. Sch. 2008, 45, 291–309. [Google Scholar] [CrossRef]
- Sedgwick, P. Treatment allocation in trials: Block randomisation. BMJ 2014, 348, g2409. [Google Scholar] [CrossRef]
- McGuire, W.J. Theory-Oriented Research in Natural Settings: The Best of Both Worlds for Social Psychology. 2017. Available online: https://www.taylorfrancis.com/books/e/9781351512022/chapters/10.4324%2F9780203788363-2 (accessed on 12 July 2018).
- Whitehead, A.L.; Sully, B.G.; Campbell, M.J. Pilot and feasibility studies: Is there a difference from each other and from a randomised controlled trial? Contemp. Clin. Trials 2014, 38, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Glaser, B.G.; Strauss, A.L. Discovery of Grounded Theory, 1st ed.; Routledge: New York, NY, USA, 2017; p. 282, ISBN: 978-0-202-30260-7. [Google Scholar]
- Hammond, J.; Nelson, M.; Chinn, S.; Rona, R.J. Validation of a food frequency questionnaire for assessing dietary intake in a study of coronary heart disease risk factors in children. Eur. J. Clin. Nutr. 1993, 47, 242–250. [Google Scholar] [PubMed]
- Musher-Eizenman, D.; Holub, S. Comprehensive Feeding Practices Questionnaire: Validation of a New Measure of Parental Feeding Practices. J. Pediatr. Psychol. 2007, 32, 960–972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wardle, J.; Guthrie, C.A.; Sanderson, S.; Rapoport, L. Development of the Children’s Eating Behaviour Questionnaire. J. Child. Psychol. Psychiatr. Allied Discip. 2001, 42, 963–970. [Google Scholar] [CrossRef]
- Pliner, P. Development of measures of food neophobia in children. Appetite 1994, 23, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Kral, T.V.E. Food Neophobia and Its Association with Diet Quality and Weight Status in Children. In Food Neophobia; Woodhead Publishing: Cambridge, UK, 2018; Available online: https://www.sciencedirect.com/science/article/pii/B9780081019313000148 (accessed on 12 July 2018).
- Guerrieri, R.; Nederkoorn, C.; Jansen, A. The interaction between impulsivity and a varied food environment: Its influence on food intake and overweight. Int. J. Obes. 2008, 32, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Graziano, P.A.; Calkins, S.D.; Keane, S.P. Toddler self-regulation skills predict risk for pediatric obesity. Int. J. Obes. 2010, 34, 633–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rothbart, M.K. Temperament, Development, and Personality. Curr. Dir. Psychol. Sci. 2007, 16, 207–212. [Google Scholar] [CrossRef]
- Fulkerson, J.A.; Rydell, S.; Kubik, M.Y.; Lytle, L.; Boutelle, K.; Story, M.; Neumark-Sztainer, D.; Dudovitz, B.; Garwick, A. Healthy Home Offerings via the Mealtime Environment (HOME): Feasibility, Acceptability, and Outcomes of a Pilot Study. Obesity 2010, 18, S69–74. [Google Scholar] [CrossRef] [PubMed]
- Wyse, R.; Wolfenden, L.; Campbell, E.; Campbell, K.; Brennan, L.; Fletcher, A.; Bowman, J.; Heard, T.; Wiggers, J. A pilot study of a telephone-based parental intervention to increase fruit and vegetable consumption in 3–5-year-old children. Public Health Nutr. 2011, 14, 2245–2253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Frith, H.; Gleeson, K. Clothing and Embodiment: Men Managing Body Image and Appearance. Psychol. Men Masc. 2004, 5, 40–48. [Google Scholar] [CrossRef]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage Publications: Thousand Oaks, CA, USA, 1998; p. 184. ISBN 0-7619-0960-5. [Google Scholar]
- Anzul, M.; Downing, M.; Ely, M.; Vinz, R. On Writing Qualitative Research, 1st ed.; Routledge: London, UK, 2003; p. 240. ISBN 9781135715427. [Google Scholar]
- Field, A. Discovering Statistics through SPSS: (And Sex and Drugs and Rock’n’Roll), 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2009; p. 821, ISBN: 978-1-84787-906-6. [Google Scholar]
- Cooke, L.J.; Wardle, J.; Gibson, E.; Sapochnik, M.; Sheiham, A.; Lawson, M. Demographic, familial and trait predictors of fruit and vegetable consumption by pre-school children. Public Health Nutr. 2004, 7, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Shohaimi, S.; Welch, A.; Bingham, S.; Luben, R.; Day, N.; Wareham, N.; Khaw, K. Residential area deprivation predicts fruit and vegetable consumption independently of individual educational level and occupational social class: A cross sectional population study in the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). J. Epidemiol. Commun. Health 2004, 58, 686–691. [Google Scholar]
- Yee, A.Z.H.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- ASHE. Annual Survey of Hours and Earnings—Office for National Statistics. 2017. Available online: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2017provisionaland2016revisedresults (accessed on 1 February 2018).
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef] [PubMed]
- Gersovitz, M.; Madden, J.P.; Smiciklas-Wright, H. Validity of the 24-hr. dietary recall and seven-day record for group comparisons. J. Am. Diet. Assoc. 1978, 73, 48–55. [Google Scholar] [PubMed]
- Martin, C.K.; Nicklas, T.; Gunturk, B.; Correa, J.B.; Allen, H.R.; Champagne, C. Measuring food intake with digital photography. J. Hum. Nutr. Diet. 2014, 27, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; Allen, H.R.; Martin, P.D.; Alfonso, A.; Gerald, B.; Hunt, A. Digital photography: A new method for estimating food intake in cafeteria settings. Eat. Weight Disord. 2004, 9, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; Allen, H.R.; Martin, P.D.; Alfonso, A.J.; Gerald, B.; Hunt, A. Comparison of digital photography to weighed and visual estimation of portion sizes. J. Am. Diet. Assoc. 2003, 103, 1139–1145. [Google Scholar] [CrossRef]
- Fisher, J.O.; Rolls, B.J.; Birch, L.L. Children’s bite size and intake of an entrée are greater with large portions than with age-appropriate or self-selected portions. Am. J. Clin. Nutr. 2003, 77, 1164–1170. [Google Scholar] [CrossRef] [PubMed]
- Sothern, M.S. Obesity prevention in children: Physical activity and nutrition. Nutrition 2004, 20, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Oldham, M.; Cuckson, I.; Brunstrom, J.M.; Rogers, P.J.; Hardman, C.A. Visual exposure to large and small portion sizes and perceptions of portion size normality: Three experimental studies. Appetite 2016, 98, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Kersbergen, I. Portion size and later food intake: Evidence on the “normalizing” effect of reducing food portion sizes. Am. J. Clin. Nutr. 2018, 107, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Kling, S.M.R.; Roe, L.S.; Keller, K.L.; Rolls, B.J. Double trouble: Portion size and energy density combine to increase preschool children’s lunch intake. Physiol. Behav. 2016, 162, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Leahy, K.E.; Birch, L.L.; Fisher, J.O.; Rolls, B.J. Reductions in Entrée Energy Density Increase Children’s Vegetable Intake and Reduce Energy Intake. Obesity 2008, 16, 1559–1565. [Google Scholar] [CrossRef] [PubMed]
- Newton, S.; Braithwaite, D.; Akinyemiju, T.F. Socio-economic status over the life course and obesity: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0177151. [Google Scholar] [CrossRef] [PubMed]
- Si Hassen, W.; Castetbon, K.; Péneau, S.; Tichit, C.; Nechba, A.; Lampuré, A.; Bellisle, F.; Hercberg, S.; Méjean, C. Socio-economic and demographic factors associated with snacking behavior in a large sample of French adults. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scottish Maternal and Infant Nutrition Survey 2017. Available online: http://www.gov.scot/Resource/0053/00531610.pdf (accessed on 13 July 2018).
- Blaine, R.E.; Fisher, J.O.; Taveras, E.M.; Geller, A.C.; Rimm, E.B.; Land, T.; Perkins, M.; Davison, K.K. Reasons Low-Income Parents Offer Snacks to Children: How Feeding Rationale Influences Snack Frequency and Adherence to Dietary Recommendations. Nutrients 2015, 7, 5982–5999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Younginer, N.A.; Blake, C.E.; Davison, K.K.; Blaine, R.E.; Ganter, C.; Orloski, A.; Fisher, J.O. “What do you think of when I say the word ‘snack’?” Towards a cohesive definition among low-income caregivers of preschool-age children. Appetite 2016, 98, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.D.; Brage, S.; Forouhi, N.G.; Griffin, S.J.; Wareham, N.J.; Monsivais, P. Does the importance of dietary costs for fruit and vegetable intake vary by socioeconomic position? Br. J. Nutr. 2015, 114, 1464–1470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehm, C.D.; Monsivais, P.; Drewnowski, A. Relation between diet cost and Healthy Eating Index 2010 scores among adults in the United States 2007–2010. Prev. Med. 2015, 73, 70–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kral, T.V.E.; Hetherington, M.M. Variability in children’s eating response to portion size. A biobehavioral perspective. Appetite 2015, 88, 5–10. [Google Scholar] [CrossRef] [PubMed]
| Weight/Portion (g) | Energy (kcal) | Energy Density (kcal/g) | Fat (g) | Carbohydrate (g) | Sugar (g) | Salt (g) | |
|---|---|---|---|---|---|---|---|
| Chocolate coated sponge cookie (Jaffa Cakes, McVitie’s ®) | 37 | 144 | 3.9 | 3.6 | 25.8 | 19.2 | 0.07 |
| Cookies (Digestives, McVitie’s ®) | 30 | 142 | 4.7 | 6.4 | 18.6 | 5 | 0.4 |
| Ritz Crackers (Mondelēz ©) | 32 | 146 | 4.6 | 5.7 | 20.5 | 2.9 | 0.7 |
| Oat-bar (Goodies, Organix ®) | 30 | 121 | 4.0 | 4.5 | 17 | 7.8 | 0.01 |
| Yoghurt coated raisins (Sunny Raisins, Whitworths) | 25 | 112 | 4.5 | 5.1 | 15.8 | 15.8 | 0 |
| Cheese flavoured crackers ( Mini Cheddars, Jacobs ®) | 25 | 128 | 5.1 | 7.3 | 12.5 | 1.3 | 0.6 |
| Salted potato chips (Pom-Bear, Intersnack ©) | 15 | 79 | 5.3 | 4.2 | 9.6 | 0.5 | 0.26 |
| Bell Pepper (Red, yellow and orange) | 40 | 11 | 0.3 | 0.08 | 2.53 | 0 | 0 |
| Grapes (White) | 40 | 28 | 0.7 | 0.06 | 7.24 | 6.2 | 0 |
| Apple (Gala) | 40 | 20 | 0.5 | 0.25 | 5.25 | 4 | 0 |
| Banana | 40 | 36 | 0.9 | 0.1 | 9 | 4.9 | 0 |
| Carrot | 40 | 16 | 0.4 | 0.1 | 3.8 | 1.8 | 0 |
| Cucumber | 40 | 6 | 0.2 | 0.04 | 1.45 | 0.7 | 0 |
| Pear | 40 | 23 | 0.6 | 0 | 6 | 4 | 0.05 |
| Tomato (cherry) | 40 | 7 | 0.2 | 0.08 | 1.57 | 1.1 | 0 |
| Rice cake (Kallø) | 7 | 30 | 4.3 | 0.2 | 6.3 | 0.1 | 0.1 |
| Breadstick (Tesco own brand) | 8.25 | 34.5 | 4.2 | 0.6 | 6 | 0.3 | 0.15 |
| Crackerbread (Ryvita ®) | 7.5 | 27 | 3.6 | 0.15 | 5.7 | 0.15 | 0.1 |
| Child | Total n = 46 | Reduction n = 22 | Replacement n = 24 |
|---|---|---|---|
| Gender | 52% male | 63% male | 39% male |
| Age (months) | 36.6 ± 9.5 | 35.8 ± 9.9 | 37.5 ± 8.9 |
| BMI Centile | 60.9 ± 26.7 | 56.0 ± 30.2 | 66.2 ± 21.8 |
| Mother | |||
| Age (years) | 35 ± 4 | 35 ± 3 | 35 ± 5 |
| * BMI (kg/m2) | 24.7 ± 5.2 | 23.2 ± 3.5 | 26.3 ± 6.2 |
| Ethnicity | White British, mixed or other 94% Chinese 4% Asian Indian 2% | White British, mixed or other 96% Chinese 4% | White British, mixed or other 92% Chinese 4% Asian Indian 4% |
| Highest education | >A-level or equivalents 74% | >A-level or equivalents 88% | >A-level or equivalents 61% |
| Employment Status | 63% Employed full/part time or on maternity leave | 71% Employed full/part time or on maternity leave | 57% Employed full/ part time or on maternity leave |
| Residential Status | Own with or without mortgage 78% | Own with or without mortgage 88% | Own with or without mortgage 65% |
| Marital Status | 100% married or cohabiting | 100% married or cohabiting | 100% married or cohabiting |
| Income | £0–10,000 4% | £0–10,000 5% | £0–10,000 4% |
| £10–20,000 28% | £10–20,000 32% | £10–20,000 25% | |
| £20–30,000 22% | £20–30,000 23% | £20–30,000 21% | |
| £30–40,000 24% | £30–40,000 23% | £30–40,000 25% | |
| £40,000+ 22% | £40,000+ 18% | £40,000+ 25% |
| Reduction | Replacement | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Week1 | Week2 | Week3 | Week1 | Week2 | Week3 | Week1 | Week2 | Week3 | |
| Vegetable: Snacks (g) | 1.7 ± 3.9 | 1.3 ± 3.0 | 0.5 ± 1.8 | 0.2 ± 0.6 | 0.6 ± 2.3 | 21.0 ± 21.8 *# | 0.9 ± 2.8 | 0.9 ± 2.7 | 11.2 ± 18.8 *# |
| Vegetable: Meals (g) | 24.8 ± 19.1 | 19.6 ± 12.0 | 20.3 ± 17.0 | 28.5 ± 29.8 | 24.3 ± 23.6 | 24.9 ± 23.0 | 26.8 ± 25.0 | 22.0 ± 18.9 | 22.7 ± 20.3 |
| Vegetable: Total (g) | 26.5 ± 20.3 | 20.9 ± 12.5 | 20.8 ± 17.0 | 28.7 ± 29.8 | 24.9 ± 24.9 | 45.9 ± 35.1 *# | 27.7 ± 25.4 | 23.0 ± 19.8 | 33.9 ± 30.5 # |
| Fruit: Snacks (g) | 65.6 ± 75.7 | 45.1 ± 31.4 | 65.9 ± 50.8 | 42.0 ± 31.6 | 27.6 ± 31.1 | 65.4 ± 41.6 | 53.3 ± 57.7 | 36.0 ± 32.1 *# | 65.6 ± 45.7 |
| Fruit: Meals (g) | 34.4 ± 42.0 | 39.1 ± 33.3 | 37.1 ± 36.4 | 36.7 ± 28.1 | 36.7 ± 27.4 | 33.5 ± 31.3 | 35.6 ± 35.1 | 37.8 ± 30.0 | 35.2 ± 33.5 |
| Fruit: Total (g) | 100.0 ± 71.8 | 84.2 ± 40.4 | 102.9 ± 63.0 | 78.7 ± 46.5 | 64.3 ± 49.7 | 99.0 ± 51.8 | 88.9 ± 60.2 | 73.8 ± 46.1 | 100.9 ± 56.8 # |
| Energy (kcal) | 1052.1 ± 235.8 | 1077.8 ± 229.1 | 1063.5 ± 284.1 | 1116.3 ± 239.6 | 1058.5 ± 225.2 | 971.8 ± 188.3 *# | 1085.6 ± 37.3 | 1067.7 ± 224.7 | 1015.7 ± 240.7 |
| Total Sugar (g) | 71.1 ± 21.9 | 69.9 ± 19.6 | 67.5 ± 23.7 | 79.7 ± 28.2 | 69.8 ± 19.5 | 62.6 ± 26.6 | 75.6 ± 25.5 | 69.9 ± 19.3 | 65.0 ± 25.1 * |
| Free Sugar (g) | 29.2 ± 15.4 | 24.3 ± 17.0 | 20.8 ± 13.0 | 40.4 ± 26.7 | 27.2 ± 14.7 | 25.2 ± 24.6 | 35.1 ± 22.5 # | 25.8 ± 15.7 | 23.1 ± 19.8 * |
| Total Fat (g) | 38.2 ± 9.1 | 42.8 ± 10.2 | 41.9 ± 15.8 | 42.0 ± 11.5 | 42.4 ± 12.6 | 34.6 ± 9.2 *# | 40.2 ± 10.5 | 42.6 ± 11.4 | 38.1 ± 13.2 # |
| Mean number of snacks | 1.6 ± 0.6 | 2.1 ± 0.6 | 2.1 ± 0.6 | 2.0 ± 0.6 | 2.2 ± 0.5 | 2.1 ± 0.5 | 1.8 ± 0.6 # | 2.1 ± 0.5 | 2.1 ± 0.6 * |
| Vegetables | Fresh Fruit | Total Energy | Total Fat | Total Sugar | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | se | β | p | b | se | β | p | b | se | β | p | b | se | β | p | b | se | β | p | |
| Intervention Group | 23.91 | 6.34 | 0.39 | 0.001 | 23.81 | 12.42 | 0.22 | 0.06 | −125.83 | 58.49 | −0.26 | 0.04 | −10.44 | 3.28 | −0.40 | <0.01 | −16.09 | 6.05 | −0.31 | 0.01 |
| Baseline Intake | 0.72 | 0.13 | 0.58 | <0.001 | 0.72 | 0.13 | 0.63 | <0.001 | 0.71 | 0.13 | 0.72 | <0.001 | 0.71 | 0.15 | 0.58 | <0.001 | 0.66 | 0.12 | 0.66 | <0.001 |
| Child Neophobia | −1.59 | 0.62 | −0.27 | 0.01 | −7.99 | 2.21 | −0.77 | <0.01 | - | - | - | - | - | - | - | - | - | - | - | - |
| Deprivation Score * | 2.06 | 0.98 | 0.21 | 0.04 | - | - | - | - | - | - | - | - | 0.88 | 0.51 | 0.22 | 0.09 | 1.95 | 0.95 | 0.24 | <0.05 |
| Food Fussiness | - | - | - | - | 5.84 | 2.56 | 0.53 | 0.03 | - | - | - | - | - | - | - | - | 1.04 | 0.61 | 0.19 | 0.10 |
| Modelling | - | - | - | - | −10.25 | 2.38 | −0.53 | < 0.001 | - | - | - | - | - | - | - | - | - | - | - | - |
| Food Responsiveness | - | - | - | - | −3.06 | 1.70 | −0.22 | 0.08 | −18.05 | 7.85 | −0.29 | 0.03 | −0.83 | 0.41 | −0.25 | 0.05 | - | - | - | - |
| Satiety Responsiveness | - | - | - | - | −4.78 | 2.38 | −0.31 | 0.05 | - | - | - | - | - | - | - | - | - | - | - | - |
| * BMI Centile | - | - | - | - | −0.41 | 0.23 | −0.21 | 0.08 | - | - | - | - | - | - | - | - | - | - | - | - |
| Child Age | - | - | - | - | - | - | - | - | - | - | - | - | 0.33 | 0.16 | 0.25 | < 0.05 | - | - | - | - |
| Food Item | Pre-Intervention | Post Intervention | ||||
|---|---|---|---|---|---|---|
| Reduction | Replacement | Total | Reduction | Replacement | Total | |
| Cookies | 5.68 ± 4.98 | 2.96 ± 2.03 | 4.26 ± 3.95 | 3.55 ± 2.32 | 2.92 ± 2.59 | 3.18 ± 2.47 |
| Cake | 2.36 ± 2.75 | 1.49 ± 2.06 | 1.91 ± 2.43 | 1.66 ± 1.70 | 1.14 ± 1.07 | 1.36 ± 1.37 |
| Pastries | 0.34 ± 0.47 | 0.28 ± 0.31 | 0.31 ± 0.39 | 0.30 ± 0.32 | 0.16 ± 0.24 | 0.22 ± 0.28 |
| Sweets | 3.64 ± 3.11 | 2.52 ± 2.88 | 3.03 ± 3.00 | 3.38 ± 3.64 | 2.09 ± 1.95 | 2.63 ± 2.82 |
| Potato Chips | 3.56 ± 2.69 | 2.40 ± 2.07 | 2.93 ± 2.42 | 3.13 ± 2.18 | 2.76 ± 2.97 | 2.91 ± 2.64 |
| Green cooked vegetables | 6.61 ± 4.97 | 4.78 ± 3.01 | 5.66 ± 4.12 | 6.27 ± 5.13 | 5.50 ± 4.60 | 5.82 ± 4.78 |
| Other Vegetables | 4.59 ± 3.30 | 4.06 ± 3.04 | 4.32 ± 3.14 | 4.66 ± 3.13 | 3.98 ± 2.24 | 4.26 ± 2.64 |
| Salad | 4.69 ± 4.07 | 2.68 ± 2.24 | 3.64 ± 3.37 | 4.20 ± 3.42 | 3.86 ± 4.45 | 4.01 ± 4.00 |
| Fruit | 13.14 ± 8.59 | 11.42 ± 5.32 | 12.24 ± 7.05 | 13.69 ± 6.79 | 14.73 ± 7.62 | 14.29 ± 7.21 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reale, S.; Kearney, C.M.; Hetherington, M.M.; Croden, F.; Cecil, J.E.; Carstairs, S.A.; Rolls, B.J.; Caton, S.J. The Feasibility and Acceptability of Two Methods of Snack Portion Control in United Kingdom (UK) Preschool Children: Reduction and Replacement. Nutrients 2018, 10, 1493. https://doi.org/10.3390/nu10101493
Reale S, Kearney CM, Hetherington MM, Croden F, Cecil JE, Carstairs SA, Rolls BJ, Caton SJ. The Feasibility and Acceptability of Two Methods of Snack Portion Control in United Kingdom (UK) Preschool Children: Reduction and Replacement. Nutrients. 2018; 10(10):1493. https://doi.org/10.3390/nu10101493
Chicago/Turabian StyleReale, Sophie, Colette M. Kearney, Marion M. Hetherington, Fiona Croden, Joanne E. Cecil, Sharon A. Carstairs, Barbara J. Rolls, and Samantha J. Caton. 2018. "The Feasibility and Acceptability of Two Methods of Snack Portion Control in United Kingdom (UK) Preschool Children: Reduction and Replacement" Nutrients 10, no. 10: 1493. https://doi.org/10.3390/nu10101493
APA StyleReale, S., Kearney, C. M., Hetherington, M. M., Croden, F., Cecil, J. E., Carstairs, S. A., Rolls, B. J., & Caton, S. J. (2018). The Feasibility and Acceptability of Two Methods of Snack Portion Control in United Kingdom (UK) Preschool Children: Reduction and Replacement. Nutrients, 10(10), 1493. https://doi.org/10.3390/nu10101493





