Technology-Based Dietary Assessment in Youth with and Without Developmental Disabilities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Measures
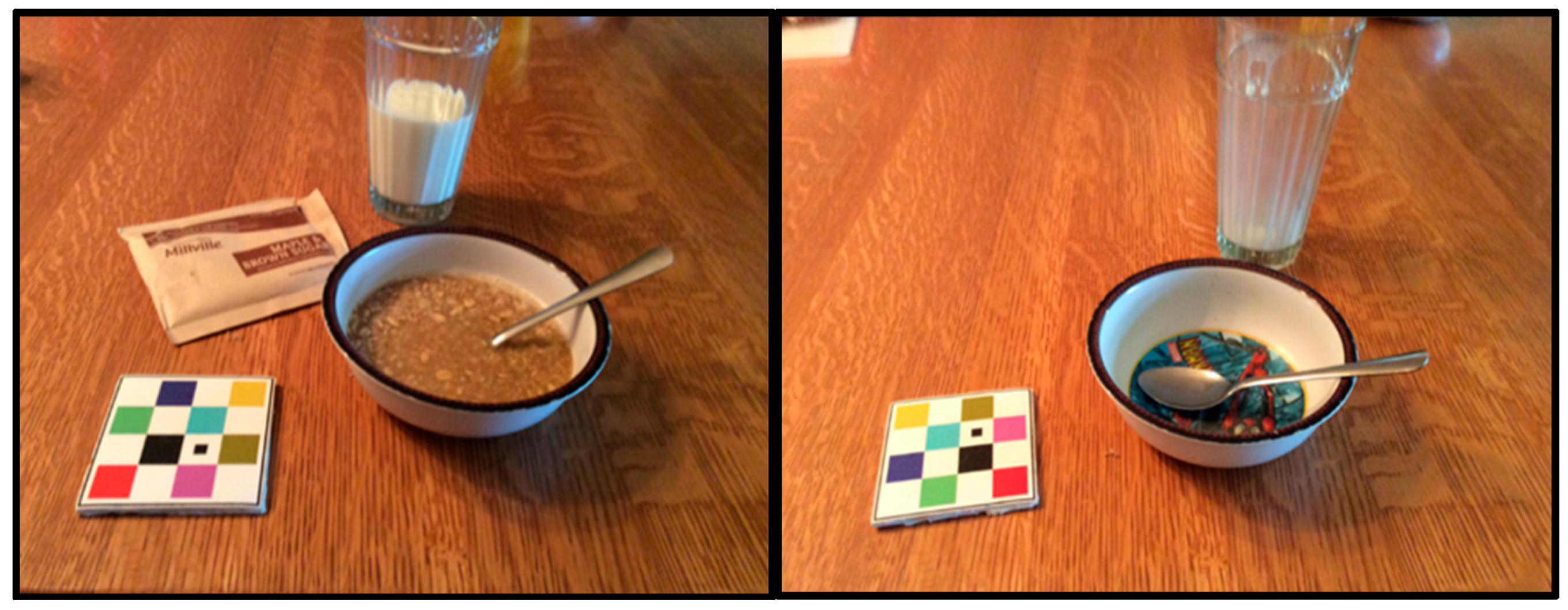
2.2.1. Dietary Assessment (mFR™)
2.2.2. Dietary Assessment (24 HR-FT)
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Feasibility and Acceptability
3.3. Energy and Dietary Macronutrients
3.4. Post Hoc Observations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Walker, J.; Ardouin, S.; Burrows, T. The validity of dietary assessment methods to accurately measure energy intake in children and adolescents who are overweight or obese: A systematic review. Eur. J. Clin. Nutr. 2017, 72, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Naska, A.; Lagiou, A.; Lagiou, P. Dietary assessment methods in epidemiological research: Current state of the art and future prospects. F1000 Res. 2017, 6, 926. [Google Scholar] [CrossRef] [PubMed]
- Ptomey, L.; Willis, E.; Goetz, J.; Lee, J.; Sullivan, D.; Donnelly, J. Digital photography improves estimates of dietary intake in adolescents with intellectual and developmental disabilities. Disabil. Health J. 2015, 8, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Bandini, L.; Danielson, M.; Esposito, L.E.; Foley, J.T.; Fox, M.H.; Frey, G.C.; Fleming, R.K.; Krahn, G.L.; Must, A.; Porretta, D.L.; et al. Obesity in children with developmental and/or physical disabilities. Disabil. Health J. 2015, 8, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.-S.; Oh, K.; Kim, H. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 2014, 36, e2014009. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.J.; Kerr, D.A.; Wright, J.; Lutes, K.D.; Ebert, D.S.; Delp, E.J. Use of technology in children’s dietary assessment. Eur. J. Clin. Nutr. 2009, 63, S50–S57. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.; Subar, A.; Loria, C.M.; Reedy, J.; Baranowski, T. Need for technological innovation in dietary assessment. J. Am. Diet. Assoc. 2010, 110, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.; Spoden, M.; Delp, E.; Zhu, F.; Bosch, M.; Ahmad, Z.; Shvetsov, Y.; DeLany, J.; Kerr, D. Reported energy intake accuracy compared to doubly labeled water and usability of the mobile food record among community dwelling adults. Nutrients 2017, 9, 312. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.J.; Harray, A.J.; Kerr, D.A.; Schap, T.E.; Paterson, S.; Aflague, T.; Bosch Ruiz, M.; Ahmad, Z.; Delp, E.J. How willing are adolescents to record their dietary intake? The mobile food record. JMIR mHealth uHealth 2015, 3, e47. [Google Scholar] [CrossRef] [PubMed]
- Kerr, D.; Dhaliwal, S.; Pollard, C.; Norman, R.; Wright, J.; Harray, A.; Shoneye, C.; Solah, V.; Hunt, W.; Zhu, F.; et al. BMI is associated with the willingness to record diet with a mobile food.record among adults participating in dietary interventions. Nutrients 2017, 9, 244. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Bosch, M.; Woo, I.; Kim, S.; Boushey, C.; Ebert, D.; Delp, E. The use of mobile devices in aiding dietary assessment and evaluation. IEEE J. Sel. Top. Signal Process. 2010, 4, 756–766. [Google Scholar] [PubMed]
- Bathgate, K.; Sherriff, J.; Leonard, H.; Dhaliwal, S.; Delp, E.; Boushey, C.; Kerr, D. Feasibility of assessing diet with a mobile food record for adolescents and young adults with down syndrome. Nutrients 2017, 9, 273. [Google Scholar] [CrossRef] [PubMed]
- Polfuss, M.; Sawin, K.J.; Papanek, P.E.; Bandini, L.; Forseth, B.; Moosreiner, A.; Zvara, K.; Schoeller, D.A. Total energy expenditure and body composition of children with developmental disabilities. Disabil. Health J. 2017, 3, 442–446. [Google Scholar] [CrossRef] [PubMed]
- University of Minnesota. Nutrition Data System for Research-Nutritional Analysis Software. Available online: http://license.umn.edu/technologies/ndsr87072_nutrition-data-system-for-research-nutritional-analysis-software (accessed on 26 July 2017).
| Mobile Food Record (mFR™) | |
| Willing to use TADA mFR™ in future | 12/12 (100%) |
| Ease of use (1-very easy; 10-very difficult) | 1 (75%); 3 (8.3%); 4 (8.3%); 9 (8.3%) |
| Screen easy to read | 10 (83.3%) strongly agree and 2 (16.7%) agree |
| Easy to enter information | 8 (66.7%) strongly agree and 4 (33.3%) agree |
| Information provided was accurate | 10 (83.3%) strongly agree and 2 (16.7%) agree |
| Interfered with daily activities | 4 (33.3%) strongly disagree; 7 (33.3%) disagree and 1 (8.3%) agree |
| 24-h Recall by FaceTime (24 HR-FT) | |
| Willing to use 24 HR-FT in future | 12/12 (100%) |
| Ease of use (1-very easy; 10 very difficult) | 1 (83.3%); 2 (8.3%); 4 (8.3%) |
| Easy to recall food | 4 (33.3%) strongly agree and 8 (66.7%) agree |
| Information provided was accurate | 7 (58.3%) strongly agree and 5 (41.7%) agree |
| Interfered with daily activities | 5 (41.7%) strongly disagree; 6 (50%) disagree and 1 (8.3%) agree |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polfuss, M.; Moosreiner, A.; Boushey, C.J.; Delp, E.J.; Zhu, F. Technology-Based Dietary Assessment in Youth with and Without Developmental Disabilities. Nutrients 2018, 10, 1482. https://doi.org/10.3390/nu10101482
Polfuss M, Moosreiner A, Boushey CJ, Delp EJ, Zhu F. Technology-Based Dietary Assessment in Youth with and Without Developmental Disabilities. Nutrients. 2018; 10(10):1482. https://doi.org/10.3390/nu10101482
Chicago/Turabian StylePolfuss, Michele, Andrea Moosreiner, Carol J. Boushey, Edward J. Delp, and Fengqing Zhu. 2018. "Technology-Based Dietary Assessment in Youth with and Without Developmental Disabilities" Nutrients 10, no. 10: 1482. https://doi.org/10.3390/nu10101482
APA StylePolfuss, M., Moosreiner, A., Boushey, C. J., Delp, E. J., & Zhu, F. (2018). Technology-Based Dietary Assessment in Youth with and Without Developmental Disabilities. Nutrients, 10(10), 1482. https://doi.org/10.3390/nu10101482





