Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology
Abstract
:1. Introduction
1.1. Research Objective and Hypothesis
- To assess the short- and medium-term effect of nutrition-related and lifestyle-related education program on nutrition knowledge, attitudes toward nutrition, diet quality, lifestyle, and body composition of Polish teenagers in a socio-demographic context.
- To determine the association between teenagers’ nutrition knowledge, attitudes toward nutrition, dietary and lifestyle behaviours, body composition, and socio-demographic factors.
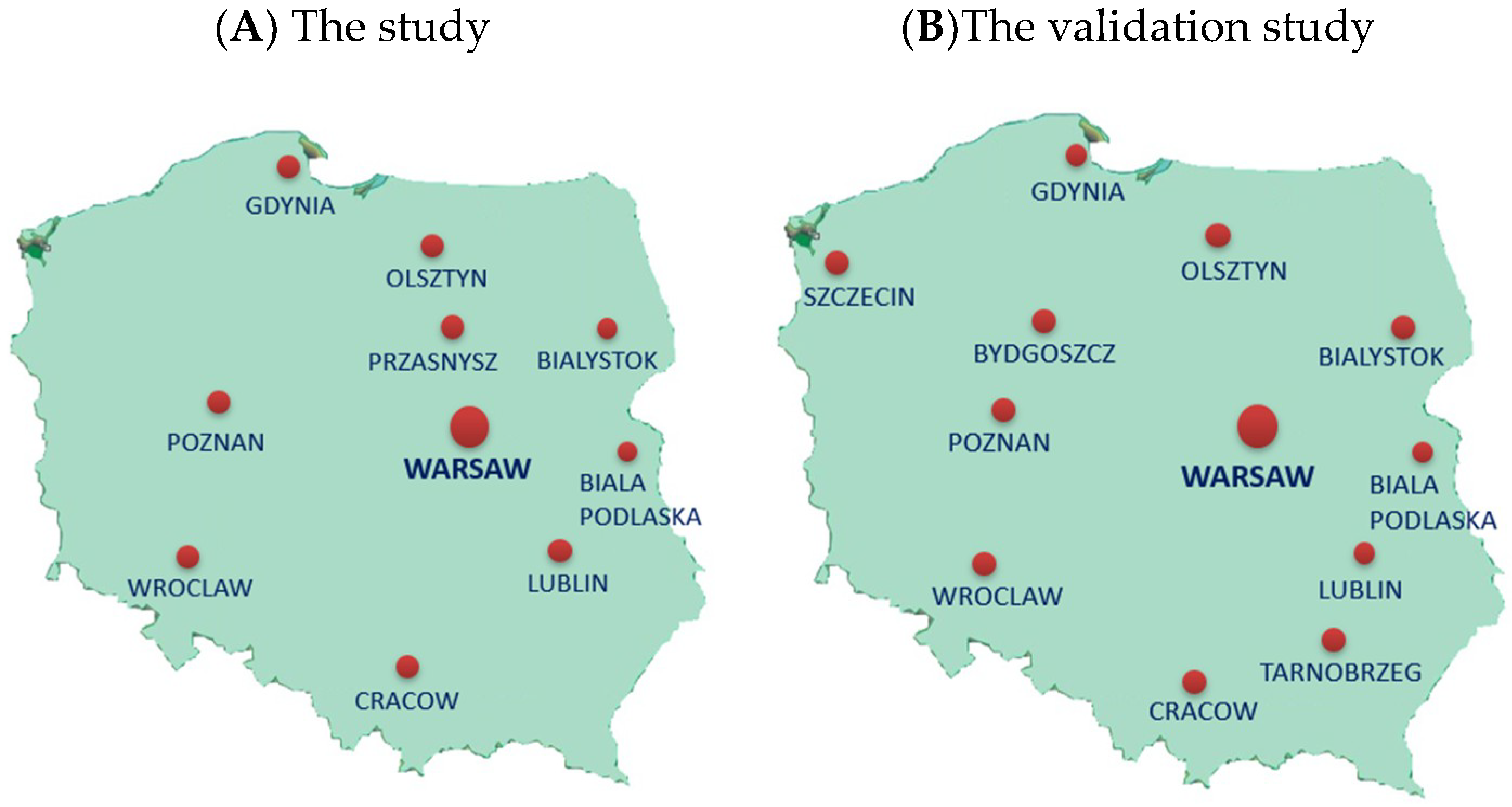
1.2. Study Design
- A national multicenter “ABC of Healthy Eating” project—the 1st edition in 2015–2016 (“ABC of Healthy Nutrition”) and the 2nd edition in 2016 (“ABC of Kids’ Nutrition”) (Figure S1).
- The own research of academic centers involved in the study, carried out in parallel with those two editions of the project.
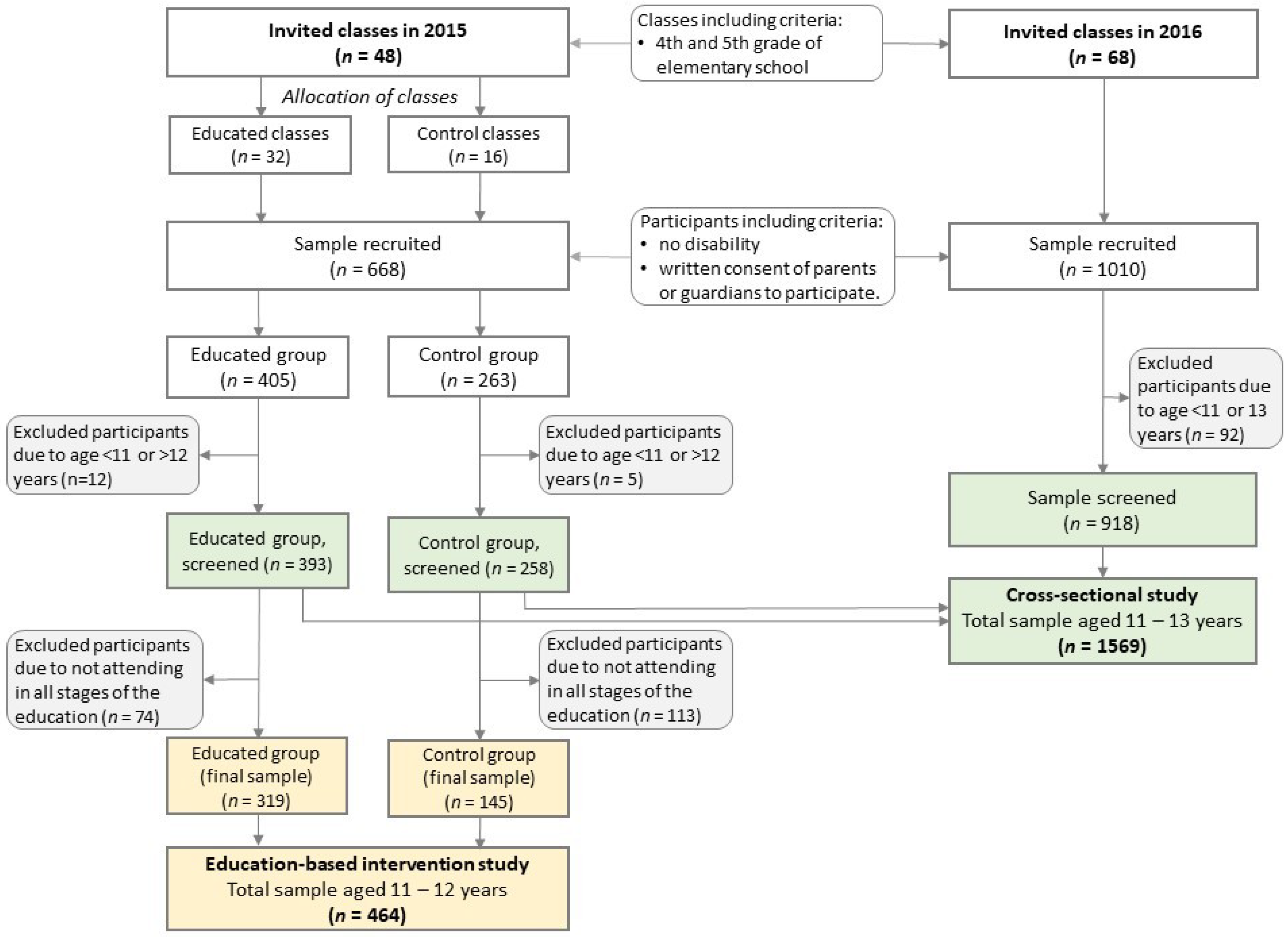
1.3. The Education-Based Intervention Study
1.4. The Cross-Sectional Study
2. Materials and Methods
2.1. Ethical Aspects
2.2. Participant Selection
2.3. Questionnaire for Data Collection
2.4. Nutrition Knowledge
2.5. Attitudes toward Nutrition
- Q12 to Q20: respondents could choose one of four answers: “definitely yes” (3 points), “rather yes” (2 points), “rather not” (1 point), “definitely not” (0 points),
- Q21: respondents could choose one of eight points on the graphical scale: 1 or 2 (0 points), 3 or 4 (1 point), 5 or 6 with (2 points), 7 or 8 (3 points).
2.6. Diet Quality
- A posteriori approach—three levels of each diet quality score based on tertile distribution:
- pHDI: bottom tertile (<20.625% points), middle tertile (20.625–32.125% points), upper tertile (≥32.125% points).
- nHDI: bottom tertile (<7.875% points), middle tertile (7.875–16.000% points), upper tertile (≥16.000% points).
- A priori approach—three levels of each diet quality score: low (<33.33% points), moderate (33.33–66.66% points), and high (≥66.66% points).
2.7. Lifestyle
2.8. Body Composition
2.9. Socio-Demographic Data
- Q44: “Does your family own a car, van or truck?” Answers: no (0 points); yes, one (1 point); yes, two or more (2 points).
- Q45: “During the past year, how many times did you travel away on holiday with your family?” (necessary examples were given) Answers: not at all (0 points); once (1 point); twice (2 points); more than twice (2 points).
- Q46: “Do you have your own bedroom for yourself?” Answers: no (0 points); yes (1 point).
- Q47: “How many computers, laptops or tablets do your family own?” Answers: none (0 points); one (1 point); two (2 points); more than two (2 points).
2.10. Sample Size Calculation
2.11. Statistical Analysis
- Eleven dietary, i.e., frequency consumption of breakfast, school meal and nine food items such as dairy products, fish, vegetables, fruit, fruit or vegetable juices, fast foods, sweetened drinks, energy drinks, sweets (in times/day).
- Three lifestyles, i.e., screen time, physical activity at school, physical activity at leisure time (in scores).
- For the education-based intervention study: (i) a chance to fall in the modeled category after 3- or 9-month follow-up in respect to baseline as reference, (ii) the chance to fall in the modeled category in the educated group in respect to the control group as reference,
- For the cross-sectional study: (iii) adherence to chosen DLP by nutrition knowledge, attitudes toward nutrition and sociodemographic factors in respect to referent DLP, (iv) the chance to fall in the modeled category of body composition in respect to normal body composition category as reference.
3. Discussion
3.1. Strengths and Limitations in General
3.2. Strengths and Limitations of the Education-Based Intervention Study
3.3. Strengths and Limitations of the Cross-Sectional Study
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Lobstein, T.; Jackson-Leach, R. Planning for the worst: Estimates of obesity and comorbidities in school-age children in 2025. Pediatr. Obes. 2016, 11, 321–325. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Nutrition Monitoring Framework: Operational guidance for tracking progress in meeting targets for 2025. Geneva, Switzerland. 2017. Available online: http://apps.who.int/iris/bitstream/handle/10665/259904/9789241513609-eng.pdf;jsessionid=004DBB115D5F666C3EE9F022BFD99D86?sequence=1 (accessed on 20 July 2018).
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Suder, A.; Gomula, A.; Koziel, S. Central overweight and obesity in Polish schoolchildren aged 7–18 years: Secular changes of waist circumference between 1966 and 2012. Eur. J. Pediatr. 2017, 176, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Olds, T.; Maher, C.; Zumin, S.; Péneau, S.; Lioret, S.; Castetbon, K.; Bellisle, F.; de Wilde, J.; Hohepa, M.; Maddison, R.; et al. Evidence that the prevalence of childhood overweight is plateauing: Data from nine countries. Int. J. Pediatr. Obes. 2011, 6, 342–360. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Family Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Blössner, M.; Borghi, E. Prevalence and trends of stunting among pre-school children, 1990–2020. Public Health Nutr. 2012, 15, 142–148. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. European Food and Nutrition Action Plan 2015–2020, REGIONAL COMMITTEE FOR EUROPE 64th SESSION. Copenhagen, Denmark. 2014. Available online: http://www.euro.who.int/__data/assets/pdf_file/0008/253727/64wd14e_FoodNutAP_140426.pdf (accessed on 28 July 2018).
- Mazur, J. (Ed.) Zdrowie i Zachowania Zdrowotne Młodzieży Szkolnej w Polsce na tle Wybranych Uwarunkowań Socjodemograficznych. Wyniki. Badań HBSC 2014 [Health and Health Behaviour of School Children in Poland against the Background of Selected Sociodemographic Conditions. HBSC 2014 Results]; IMiD: Warsaw, Poland, 2015. [Google Scholar]
- Chobot, A.; Górowska-Kowolik, K.; Sokołowska, M.; Jarosz-Chobot, P. Obesity and diabetes-Not only a simple link between two epidemics. Diabetes Metab. Res. Rev. 2018, 21, e3042. [Google Scholar] [CrossRef] [PubMed]
- Kowalkowska, J.; Wadolowska, L.; Wuenstel, J.W.; Słowińska, M.A.; Niedźwiedzka, E. Socioeconomic status and overweight prevalence in polish adolescents: The impact of single factors and a complex index of socioeconomic status in respect to age and sex. Iran J. Public Health 2014, 43, 913–925. [Google Scholar] [PubMed]
- Wadolowska, L.; Kowalkowska, J.; Czarnocinska, J.; Jezewska-Zychowicz, M.; Babicz-Zielinska, E. Comparing dietary patterns derived by two methods and their associations with obesity in Polish girls aged 13–21 years: The cross-sectional GEBaHealth study. Perspect. Public Health 2017, 137, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Faienza, M.F.; Wang, D.Q.; Frühbeck, G.; Garruti, G.; Portincasa, P. The dangerous link between childhood and adulthood predictors of obesity and metabolic syndrome. Intern. Emerg Med. 2016, 11, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Prevention of Cardiovascular Disease. Geneva, Switzerland. 2007. Available online: http://www.who.int/cardiovascular_diseases/guidelines/en/ (accessed on 2 August 2018).
- Vucenik, I.; Stains, J.P. Obesity and cancer risk: Evidence, mechanisms, and recommendations. Ann. N.Y. Acad. Sci. 2012, 1271, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, A.; Simmonds, M.; Owen, C.G.; Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Pérez, A.; Wu, L.T.; Ranjit, N.; Brown, H.S.; Kelder, S.H. Cardiometabolic Risk Factors among Severely Obese Children and Adolescents in the United States, 1999–2012. Child Obes. 2016, 12, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Estrada, E.; Eneli, I.; Hampl, S.; Mietus-Snyder, M.; Mirza, N.; Rhodes, E.; Sweeney, B.; Tinajero-Deck, L.; Woolford, S.J.; Pont, S.J.; Children’s Hospital Association. Children’s Hospital Association consensus statements for comorbidities of childhood obesity. Child Obes. 2014, 10, 304–317. [Google Scholar] [CrossRef] [PubMed]
- Sbruzzi, G.; Eibel, B.; Barbiero, S.M.; Petkowicz, R.O.; Ribeiro, R.A.; Cesa, C.C.; Martins, C.C.; Marobin, R.; Schaan, C.W.; Souza, W.B.; et al. Educational interventions in childhood obesity: A systematic review with meta-analysis of randomized clinical trials. Prev. Med. 2013, 56, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P.; Pérusse, L.; Després, J.P.; Tremblay, A.; Bouchard, C. Findings from the quebec family study on the etiology of obesity: Genetics and environmental highlights. Curr. Obes. Rep. 2014, 3, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Bautista-Castaño, I. Etiology of obesity: Two ‘key issues’ and other emerging factors. Nutr. Hosp. 2013, 28 (Suppl. 5), 32–43. [Google Scholar] [CrossRef] [PubMed]
- Wadolowska, L.; Kowalkowska, J.; Lonnie, M.; Czarnocinska, J.; Jezewska-Zychowicz, M.; Babicz-Zielinska, E. Associations between physical activity patterns and dietary patterns in a representative sample of Polish girls aged 13–21 years: A cross-sectional study (GEBaHealth Project). BMC Public Health 2016, 16, 698. [Google Scholar] [CrossRef] [PubMed]
- Popkin, M.P.; Adair, L.S.; Ng, S.W. The Global Nutrition Transition: The pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Wen, L.M.; Rissel, C. Associations of parental influences with physical activity and screen time among young children: A systematic review. J. Obes. 2015, 2015, 546925. [Google Scholar] [CrossRef] [PubMed]
- Van Hecke, L.; Loyen, A.; Verloigne, M.; van der Ploeg, H.P.; Lakerveld, J.; Brug, J.; De Bourdeaudhuij, I.; Ekelund, U.; Donnelly, A.; Hendriksen, I.; et al. Variation in population levels of physical activity in European children and adolescents according to cross-European studies: A systematic literature review within DEDIPAC. Int. J. Behav. Nutr. Phys. Act. 2016, 28, 13–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumith, S.C.; Gigante, D.P.; Domingues, M.R.; Kohl, H.W. Physical activity change during adolescence: A systematic review and a pooled analysis. Int. J. Epidemiol. 2011, 40, 685–698. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Kubik, M.Y.; Lytle, L.A.; Hannan, P.J.; Perry, C.L.; Story, M. The association of the school food environment with dietary behaviors of young adolescents. Am. J. Public Health 2003, 93, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Fox, M.K.; Dodd, A.H.; Wilson, A.; Gleason, P.M. Association between school food environment and practices and body mass index of US public school children. J. Am. Diet Assoc. 2009, 109 (Suppl. 2), 108–117. [Google Scholar] [CrossRef] [PubMed]
- Singh, R. Childhood obesity: An epidemic in waiting? Int. J. Med. Public Health 2013, 3, 2–7. [Google Scholar] [CrossRef]
- Trude, A.C.B.; Kharmats, A.Y.; Jones-Smith, J.C.; Gittelsohn, J. Exposure to a multi-level multi-component childhood obesity prevention community-randomized controlled trial: Patterns, determinants, and implications. Trials 2018, 19, 287. [Google Scholar] [CrossRef] [PubMed]
- Ryan, P. Integrated theory of health behavior change: Background and intervention development. Clin. Nurse Spec. 2009, 23, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Jezewska-Zychowicz, M.; Wadolowska, L.; Kowalkowska, J.; Lonnie, M.; Czarnocinska, J.; Babicz-Zielinska, E. Perceived Health and Nutrition Concerns as Predictors of Dietary Patterns among Polish Females Aged 13–21 Years (GEBaHealth Project). Nutrients 2017, 9, 613. [Google Scholar] [CrossRef] [PubMed]
- Alkaed, D.; Ibrahim, N.; Ismail, F.; Barake, R. Validity and Reliability of a Nutrition Knowledge Questionnaire in an Adult Student Population. J. Nutr. Educ. Behav. 2018, 50, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.; Jennifer, S.; Savage, J.S.; Ventura, A. Influences on the development of children’s eating behaviours: From infancy to adolescence. Can. J. Diet Pract. Res. 2007, 68, S51–S56. [Google Scholar]
- Spronk, I.; Kullen, C.; Burdon, C.; O’Connor, H. Relationship between nutrition knowledge and dietary intake. Br. J. Nutr. 2014, 111, 1713–1726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baxter, S.D. Cognitive processes in children’s dietary recalls: Insight from methodological studies. Eur. J. Clin. Nutr. 2009, 63 (Suppl. 1), 19–32. [Google Scholar] [CrossRef] [PubMed]
- Story, M.; Kaphingst, K.M.; French, S. The role of schools in obesity prevention. Future Child 2006, 16, 109–142. [Google Scholar] [CrossRef] [PubMed]
- Hung, L.S.; Tidwell, D.K.; Hall, M.E.; Lee, M.L.; Briley, C.A.; Hunt, B.P. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr. Res. 2015, 35, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Worsley, A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pac. J Clin. Nutr. 2002, 11, S579–S585. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Grammatikaki, E.; Androutsos, O.; Chinapaw, M.J.; Gibson, E.L.; Buijs, G.; Iotova, V.; Socha, P.; Annemans, L.; Wildgruber, A.; et al. A systematic approach for the development of a kindergarten-based intervention for the prevention of obesity in preschool age children: The ToyBox-study. Obes. Rev. 2012, 13, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Androutsos, O.; Katsarou, C.; Iotova, V.; Socha, P.; Geyer, C.; Moreno, L.; Koletzko, B.; De Bourdeaudhuij, I.; on behalf of the ToyBox-study group. Designing and implementing a kindergarten-based, family-involved intervention to prevent obesity in early childhood: The ToyBox-study. Obes. Rev. 2014, 15, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Myszkowska-Ryciak, J.; Harton, A. Eating Healthy, Growing Healthy: Impact of a Multi-Strategy Nutrition Education on the Assortments of Beverages Served in Preschools, Poland. Int. J. Environ. Res. Public Health 2018, 15, 1355. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cancer Control: Knowledge into Action. Geneva, Switzerland. 2007. Available online: http://www.who.int/cancer/modules/en/ (accessed on 2 August 2018).
- World Health Organization. Framework for Care and Control of Tuberculosis and Diabetes. Geneva. 2011. Available online: https://www.worlddiabetesfoundation.org/files/collaborative-framework-care-and-control-tuberculosis-and-diabetes (accessed on 27 July 2018).
- Available online: http://www.zachowajrownowage.pl/pl/o-projekcie/ (accessed on 11 September 2018).
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 7, 348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hörnell, A.; Berg, C.; Forsum, E.; Larsson, C.; Sonestedt, E.; Åkesson, A.; Lachat, C.; Hawwash, D.; Kolsteren, P.; Byrnes, G.; et al. Perspective: An Extension of the STROBE Statement for Observational Studies in Nutritional Epidemiology (STROBE-nut): Explanation and Elaboration. Adv. Nutr. 2017, 8, 652–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reporting Guidelines for Main Study Types. Available online: http://www.equator-network.org (accessed on 23 July 2018).
- Piramida Zdrowego Zywienia i Aktywnosci Fizycznej. Available online: http://www.izz.waw.pl/pl/zasady-prawidowego-ywienia (accessed on 23 July 2018).
- Whati, L.H.; Senekal, M.; Steyn, N.P.; Nel, J.H.; Lombard, C.; Norris, S. Development of a reliable and valid nutritional knowledge questionnaire for urban South African adolescents. Nutrition 2005, 21, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Dzielska, A.; Mazur, J.; Małkowska-Szkutnik, A.; Kołoło, H. Adaptation of the Three-Factor Eating Questionnaire (TFEQ-13) for school-aged adolescents in a population study. Probl. Hig. Epidemiol. 2009, 90, 362–369. [Google Scholar]
- Rampersaud, G.C.; Pereira, M.A.; Girard, B.L.; Adams, J.; Metzl, J.D. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J. Am. Diet. Assoc. 2005, 105, 743–760. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.A.; Erickson, E.; McKee, P.; Schrankler, K.; Raatz, S.K.; Lytle, L.A.; Pellegrini, A.D. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J. Nutr. 2011, 141, 163–168. [Google Scholar] [CrossRef] [PubMed]
- AAP Council on communications and media. Media Use in School-Aged Children and Adolescents. Pediatrics 2016, 138, e20162592. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health. Geneva, Switzerland. 2010. Available online: http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/ (accessed on 29 July 2018).
- ISAK. International Standards for Anthropometric Assessment. Potchefstroom, South Africa: International Society for the Advancement of Kinanthropometry. 2001. Available online: http://www.ceap.br/material/MAT17032011184632.pdf (accessed on 17 July 2018).
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Mazur, J. Family Affluence Scale—validation study and suggested modification. Hygeia Pub. Health 2013, 48, 211–217. [Google Scholar]
- Armitage, P.; Berry, G.; Matthews, J.N.S. Statistical Methods in Medical Research, 4th ed.; Blackwell Science: Oxford, UK, 2008. [Google Scholar]
- Centeio, E.E.; McCaughtry, N.; Moore, E.W.G.; Kulik, N.; Garn, A.; Martin, J.; Shen, B.; Somers, C.L.; Fahlman, M. Building healthy communities: A comprehensive school health program to prevent obesity in elementary schools. Prev. Med. 2018, 111, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Sobol-Goldberg, S.; Rabinowitz, J.; Gross, R. School-based obesity prevention programs: A meta-analysis of randomized controlled trials. Obesity 2013, 21, 2422–2428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lycett, K.; Miller, A.; Knox, A.; Dunn, S.; Kerr, J.A.; Sung, V.; Wake, M. ‘Nudge’ interventions for improving children’s dietary behaviors in the home: A. systematic review. Obes. Med. 2017, 7, 21–33. [Google Scholar] [CrossRef]
- Zielińska, M.; Hamułka, J.; Gajda, K. Family influences on breakfast frequency and quality among primary school pupils in Warsaw and its surrounding areas. Rocz. Panstw. Zakl. Hig. 2015, 66, 143–149. [Google Scholar] [PubMed]
- Inchley, J.; Currie, D.; Young, T.; Samdal, O.; Torsheim, T.; Augustson, L.; Mathison, F.; Aleman-Diaz, A.; Molcho, M.; Weber, M.; et al. Growing up unequal: Gender and socioeconomic differences in young people’s health and wellbeing. Health Behaviour in School-aged Children (HBSC) study: International report from the 2013/2014 survey. WHO Regional Office for Europe: Copenhagen, Denmark, 2016. Available online: http://www.euro.who.int/en/hbsc-report-2016 (accessed on 9 September 2018).
- Wunstel, J.W.; Kowalkowska, J.; Wadolowska, L.; Slowinska, M.A.; Niedzwiedzka, E.; Kurp, L. Habitual eating breakfast consumption. Dev. Period Med. 2015, 19, 193–201. [Google Scholar]
- Kollataj, W.; Sygit, K.; Sygit, M.; Karwat, I.D.; Kollataj, B. Eating habits of children and adolescents from rural regions depending on gender, education, and economic status of parents. Ann. Agric. Environ. Med. 2011, 18, 393–397. [Google Scholar]
- Zakrzewski, J.K.; Gillison, F.B.; Cumming, S.; Church, T.S.; Katzmarzyk, P.T.; Broyles, S.T.; Champagne, C.M.; Chaput, J.P.; Denstel, K.D.; Fogelholm, M.; et al. Associations between breakfast frequency and adiposity indicators in children from 12 countries. Int. J. Obes. 2015, 5 (Suppl. 2), 80–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brug, J.; van Stralen, M.M.; te Velde, S.J.; Chinapaw, M.J.M.; De Bourdeaudhuij, I.; Lien, N.; Bere, E.; Maskini, V.; Singh, A.S.; Maes, L. Differences in weight status and energy-balance related behaviors among schoolchildren across europe: The energy-project. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hallstrom, L.; Vereecken, C.A.; Labayen, I.; Ruiz, J.R.; Le Donne, C.; Garcia, M.C.; Gilbert, C.C.; Martínez, S.G.; Grammatikaki, E.; Huybrechts, I. Breakfast habits among European adolescents and their association with sociodemographic factors: The HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Public Health Nutr. 2012, 15, 1879–1889. [Google Scholar] [CrossRef] [PubMed]
- Gubbels, J.S.; Kremers, S.P.; Stafleu, A.; Goldbohm, A.; Vries, N.K.; Thijs, C. Clustering of energy balance-related behaviors in 5-year-old children: Lifestyle patterns and their longitudinal association with weight status development in early childhood. Int. J. Behav. Nutr. 2012, 9, 77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Food and Agriculture Organization. Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings. Rome. 2018. Available online: http://www.fao.org/3/i9940en/I9940EN. (accessed on 17 July 2018).
- Gubbels, J.S.; van Assema, P.; Kremers, S.P.J. Physical activity, sedentary behavior, and dietary patterns among children. Curr. Nutr. Rep. 2013, 2, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, P.; Friedenreich, C.; Matthews, C.E. The role of measurement error in estimating levels of physical activity. Am. J. Epidemiol. 2007, 166, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Saunders, T.J.; Prince, S.A.; Tremblay, M.S. Clustering of children’s activity behaviour: The use of self-report versus direct measures. Int. J. Behav. Nutr. Phys. Act. 2011, 8. [Google Scholar] [CrossRef] [PubMed]
- Verbestel, V.; De Henauw, S.; Bammann, K.; Barba, G.; Hadjigeorgiou, C.; Eiben, G.; Konstabel, K.; Kovács, E.; Pitsiladis, Y.; Reisch, L.; et al. Are context-specific measures of parental-reported physical activity and sedentary behaviour associated with accelerometer data in 2–9-year-old European children? Public Health Nutr. 2015, 18, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Martin-Calvo, N.; Moreno-Galarraga, L.; Martinez-Gonzalez, M.A. Association between body mass index, waist-to-height ratio and adiposity in children: A systematic review and meta-analysis. Nutrients 2016, 8, 512. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef] [PubMed]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. Clustering of diet, physical activity and sedentary behaviour among Australian children: Cross-sectional and longitudinal associations with overweight and obesity. Int. Obes. 2015, 39, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Rodrigo, C.; Gil, A.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G.; Aranceta-Bartrina, J. Clustering of Dietary Patterns, Lifestyles, and Overweight among Spanish Children and Adolescents in the ANIBES Study. Nutrients 2016, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Mandic, S.; Bengoechea, E.G.; Coppell, K.J.; Spence, J.C. Clustering of (Un) Healthy Behaviors in Adolescents from Dunedin, New Zealand. Am. J. Health Behav. 2017, 41, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Nuutinen, T.; Lehto, E.; Ray, C.; Roos, E.; Villberg, J.; Tynjälä, J. Clustering of energy balance-related behaviours, sleep, and overweight among Finnish adolescents. Int. J. Public Health 2017, 62, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Laxer, R.E.; Brownson, R.C.; Dubin, J.A.; Cooke, M.; Chaurasia, A.; Leatherdale, S.T. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health 2017, 17, 102. [Google Scholar] [CrossRef] [PubMed]
| Nutrition Topic | |
| Goal | Shaping pro-healthy dietary habits. |
| Scope | Nutrients important in the diet of young people. Health consequences of uncontrolled consumption of energy drinks and dietary supplements. A “Good snack” as an alternative to chips, sticks and sweets. A Pyramid of Healthy Nutrition and Physical Activity [52] and dietary guidelines for teenagers. |
| Methods | Talk; discussion; workshops. |
| Activities | Participants propose three various “healthy” breakfasts to take at school by selecting foods from a levels of the Pyramid of Healthy Nutrition and Physical Activity; Participants prepare an “ideal sandwich”. |
| Tools | Brochure; puzzles; crosswords; website. |
| Dietary topic | |
| Goal | Supporting well-being, physical, and intellectual development through a healthy lifestyle. |
| Scope | General recommendations for a healthy lifestyle (healthy eating and physical activity) at school age. The influence of nutrition and physical activity on physical and intellectual development and healthy well-being. The Student Menu—The brain cannot live only on chocolate—A discussion on the most important nutrients in the diet of young people. |
| Methods | Talk; discussion; workshops. |
| Activities | Using a pedometer to measure the number of calories consumed during the various activities. Determination of time needed to “burn” the calories contained in the selected product. “Nutrition detective”—measuring the amounts of oil, sugar and salt corresponding to fat, sucrose and salt content in various foods (three sets). |
| Tools | Brochure; puzzles; crosswords; website. |
| Sensory-consumer topic | |
| Goal | The world of senses. How to read the food labels? What is important when choosing food? |
| Scope | Recognition of the basic flavors in aqueous solutions. Discovering the different taste sensations in selected foods. “What kind of a consumer am I”—what do I like and why? Qualification of the consumer’s personality. |
| Methods | Talk; discussion; workshops. |
| Activities | Use of sensory memory to identify eight coded odor samples of natural spices, vegetables and fruits. Recognition of selected foods with masked/closed eyes, based on sensory perceptions in the mouth. Preparation of colorful, tasty and healthy snacks from provided foods according to one’s own ideas. |
| Tools | Brochure; recipes of ‘healthy’ snacks; website. |
| Hygiene topic | |
| Goal | Food safety. Hygiene during the preparation and consuming of meals. |
| Scope | The world of microorganisms, pathogens and probiotics. The rules of proper food storage and hygiene during meal preparation and consumption. |
| Methods | Talk; discussion; workshops. |
| Activities | Microscopic observation of selected microorganisms—Lactic acid bacteria (Lactobacillus) as an example of a microorganism with healthy properties, E. coli (Escherichia coli) as an example of a pathogen. Mapping the observed microorganisms’ cells in the prepared templates. Practicing proper hand washing according to instructions. Checking hand cleanness with a test indicator, before and after hand washing. |
| Tools | Brochure; microscope; test indicator of hand washing; puzzles; crosswords; website. |
| Culinary topic | |
| Goal | How to prepare healthy, cheap and tasty meals? |
| Scope | The impact of culinary processes on sensory quality, nutritional value and food safety. The phenomenon of enzymatic browning of fruit and vegetables and ways to prevent this process. |
| Methods | Talk; discussion; workshops. |
| Activities | Culinary experiments—preventing the darkening of fruits and vegetables. Checking the impact of storage temperature on the quality of frozen foods, e.g., vegetables. Preparing low-budget healthy meals and low-sweetened beverages. |
| Tools | A “healthy meals” recipe book; brochure; website. |
| Timing | Activities | Group | |
|---|---|---|---|
| Educated | Control | ||
| June 2015 Before education (Baseline) |
| A | A |
| A | A | |
| June 2015 Education program (lasting 3 weeks) |
| A | NA |
| June 2015 After education (3 weeks from baseline) |
| A | NA |
| September 2015 After 3 months from baseline (3-month follow-up) |
| A | A |
| March 2016 After 9 months from baseline (9-month follow-up) |
| A | A |
| A | A | |
| Timing | Activities | Group | |
|---|---|---|---|
| Educated | Control | ||
| June 2015 Before education |
| A | A |
| A | A | |
| June 2016 Before education |
| A | NA |
| A | NA | |
School inclusion criteria:
|
Participant inclusion criteria—in general:
|
Participant exclusion criteria—for the education-based intervention study:
|
Participant exclusion criteria—for the cross-sectional study:
|
| Physical Activity at School | Physical Activity at Leisure Time | ||
|---|---|---|---|
| Low | Moderate | Vigorous | |
| Low | Low (0) | Low (1) | Moderate (2) |
| Moderate | Low (1) | Moderate (3) | Moderate (4) |
| Vigorous | Moderate (2) | Moderate (4) | High (5) Adherence to WHO recommendation |
| Parameter (Units) | Procedure, Accuracy, and Equipment |
|---|---|
| Height (H) (cm) |
|
| Body weight (BW) (kg) |
|
| Waist circumference (WC) (cm) |
|
| Hand grip strength (HGS) (kg) |
|
| Parameters | Education-Based Intervention Study (At Baseline) | Cross-Sectional Study | ||||
|---|---|---|---|---|---|---|
| Total Sample | Boys | Girls | Total Sample | Boys | Girls | |
| Sample size | 464 | 216 | 248 | 1569 | 760 | 809 |
| Sample percentage | 100.0 | 46.6 | 53.4 | 100.0 | 48.4 | 51.6 |
| Age (years) | 11.9 (11.9, 12.0) | 11.9 (11.9, 12.0) | 11.9 (11.9, 11.9) | 11.9 (11.9, 12.0) | 11.9 (11.9, 12.0) | 11.9 (11.9, 12.0) |
| Age (categories) | ||||||
| 11 years | 7.1 | 5.1 | 8.9 | 16.6 | 15.3 | 17.9 |
| 12 years | 92.9 | 94.9 | 91.1 | 73.6 | 75.9 | 71.3 |
| 13 years | 0.0 | 0.0 | 0.0 | 9.8 | 8.8 | 10.8 |
| Residence | ||||||
| rural | 34.9 | 36.1 | 33.9 | 40.3 | 40.3 | 40.3 |
| urban | 65.1 | 63.9 | 66.1 | 59.7 | 59.7 | 59.7 |
| Family Affluence Scale (points) | 5.3 (5.1, 5.5) | 5.2 (4.9, 5.4) | 5.4 (5.2, 5.6) | 5.4 (5.3, 5.4) | 5.3 (5.2, 5.4) | 5.4 (5.3, 5.5) |
| Nutrition knowledge | ||||||
| Nutrition knowledge score (points) | 6.0 (5.7, 6.2) | 5.5 (5.2, 5.9) | 6.3 (6.0, 6.7) | 6.1 (5.9, 6.2) | 5.7 (5.5, 5.9) | 6.5 (6.3, 6.6) |
| Nutrition knowledge (categories) | ||||||
| the lowest | 30.6 | 35.6 | 26.2 | 30.9 | 35.7 | 26.3 |
| moderately low | 41.4 | 42.1 | 40.7 | 39.3 | 40.1 | 38.6 |
| higher | 28.0 | 22.2 | 33.1 | 29.8 | 24.2 | 35.1 |
| Attitudes toward nutrition | ||||||
| Emotional Eating (points) | 1.3 (1.2, 1.5) | 1.3 (1.1, 1.5) | 1.4 (1.2, 1.5) | 1.3 (1.3, 1.4) | 1.3 (1.2, 1.3) | 1.4 (1.3, 1.5) |
| Uncontrolled Eating (points) | 5.3 (5.0, 5.5) | 5.5 (5.1, 5.9) | 5.1 (4.8, 5.4) | 5.3 (5.2, 5.4) | 5.3 (5.1, 5.5) | 5.3 (5.1, 5.5) |
| Cognitive Restraint of Eating (points) | 4.2 (4.0, 4.4) | 4.0 (3.7, 4.3) | 4.3 (4.1, 4.6) | 4.3 (4.2, 4.4) | 4.3 (4.1, 4.4) | 4.4 (4.2, 4.5) |
| Diet quality | ||||||
| Every day consumption of | ||||||
| breakfast | 71.0 | 70.7 | 71.3 | 70.0 | 72.7 | 67.4 |
| school meal | 67.5 | 59.8 | 74.2 | 69.0 | 64.7 | 72.9 |
| pHDI (% points) | 27.7 (26.4, 29.0) | 24.4 (22.8, 26.1) | 30.5 (28.6, 32.4) | 28.4 (27.7, 29.1) | 27.4 (26.3, 28.4) | 29.4 (28.4, 30.4) |
| pHDI (categories) | ||||||
| low | 71.0 | 81.8 | 61.7 | 69.2 | 72.9 | 65.8 |
| moderate | 28.6 | 17.8 | 37.9 | 29.8 | 25.9 | 33.5 |
| high | 0.4 | 0.5 | 0.4 | 1.0 | 1.2 | 0.7 |
| nHDI (% points) | 14.3 (13.3, 15.3) | 15.1 (13.8, 16.4) | 13.6 (12.2, 15.1) | 14.1 (13.5, 14.7) | 15.0 (14.1, 15.9) | 13.3 (12.5, 14.0) |
| nHDI (categories) | ||||||
| low | 93.9 | 94.0 | 92.7 | 93.8 | 93.8 | 93.8 |
| moderate | 6.7 | 6.0 | 7.3 | 5.9 | 5.5 | 6.2 |
| high | 0.0 | 0.0 | 0.0 | 0.3 | 0.7 | 0.0 |
| Lifestyle | ||||||
| Screen time (points) | 0.84 (0.74, 0.94) | 0.91 (0.76, 1.06) | 0.78 (0.65, 0.91) | 0.86 (0.81, 0.92) | 0.98 (0.89, 1.06) | 0.76 (0.69, 0.82) |
| Screen time (categories) | ||||||
| <2 h/day | 46.5 | 41.1 | 51.2 | 46.3 | 42.1 | 50.3 |
| 2 to 4 h/day | 34.7 | 40.7 | 29.4 | 34.4 | 35.2 | 33.6 |
| ≥4 h/day | 18.8 | 18.2 | 19.4 | 19.3 | 22.7 | 16.1 |
| Total physical activity (points) | 3.65 (3.53, 3.78) | 3.66 (3.48, 3.85) | 3.65 (3.49, 3.81) | 3.68 (3.61, 3.74) | 3.73 (3.63, 3.82) | 3.63 (3.54, 3.71) |
| Total physical activity (categories) | ||||||
| low | 12.3 | 13.4 | 11.3 | 9.8 | 10.0 | 9.5 |
| moderate | 54.6 | 49.5 | 59.1 | 58.9 | 53.3 | 58.9 |
| high | 33.0 | 37.0 | 29.6 | 31.3 | 36.7 | 26.3 |
| Body composition | ||||||
| Waist circumference (cm) | 64.4 (63.5, 65.3) | 65.7 (64.3, 67.0) | 63.3 (62.2, 64.5) | 66.1 (65.6, 66.5) | 67.8 (67.1, 68.6) | 64.4 (63.8, 65.0) |
| z-Waist circumference >1 SD | 13.5 | 18.5 | 9.2 | 15.1 | 20.1 | 10.4 |
| WHtR | 0.42 (0.42, 0.43) | 0.43 (0.42, 0.44) | 0.42 (0.41, 0.42) | 0.43 (0.43, 0.43) | 0.44 (0.44, 0.45) | 0.42 (0.42, 0.42) |
| Central obesity a | 10.0 | 11.4 | 8.8 | 12.2 | 15.9 | 8.7 |
| BMI (kg/m2) | 19.6 (19.2, 19.9) | 19.7 (19.1, 20.2) | 19.5 (19.0, 20.0) | 19.4 (19.2, 19.6) | 19.5 (19.2, 19.7) | 19.3 (19.1, 19.6) |
| BMI category b | ||||||
| underweight | 10.2 | 9.0 | 11.3 | 9.8 | 8.4 | 11.1 |
| normal weight | 63.4 | 62.3 | 64.4 | 65.6 | 64.8 | 66.2 |
| overweight | 26.4 | 28.8 | 24.3 | 24.7 | 26.8 | 22.7 |
| Hand grip strength c (kg) | 20.1 (19.5, 20.8) | 20.7 (19.8, 21.6) | 19.6 (18.7, 20.5) | 20.8 (20.4, 21.1) | 21.4 (20.9, 21.8) | 20.2 (19.7, 20.6) |
| z-Hand grip strength c >1 SD | 10.0 | 11.9 | 8.3 | 12.5 | 14.6 | 10.4 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamulka, J.; Wadolowska, L.; Hoffmann, M.; Kowalkowska, J.; Gutkowska, K. Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology. Nutrients 2018, 10, 1439. https://doi.org/10.3390/nu10101439
Hamulka J, Wadolowska L, Hoffmann M, Kowalkowska J, Gutkowska K. Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology. Nutrients. 2018; 10(10):1439. https://doi.org/10.3390/nu10101439
Chicago/Turabian StyleHamulka, Jadwiga, Lidia Wadolowska, Monika Hoffmann, Joanna Kowalkowska, and Krystyna Gutkowska. 2018. "Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology" Nutrients 10, no. 10: 1439. https://doi.org/10.3390/nu10101439
APA StyleHamulka, J., Wadolowska, L., Hoffmann, M., Kowalkowska, J., & Gutkowska, K. (2018). Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology. Nutrients, 10(10), 1439. https://doi.org/10.3390/nu10101439








