Effect of Educational Interventions on Understanding and Use of Nutrition Labels: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
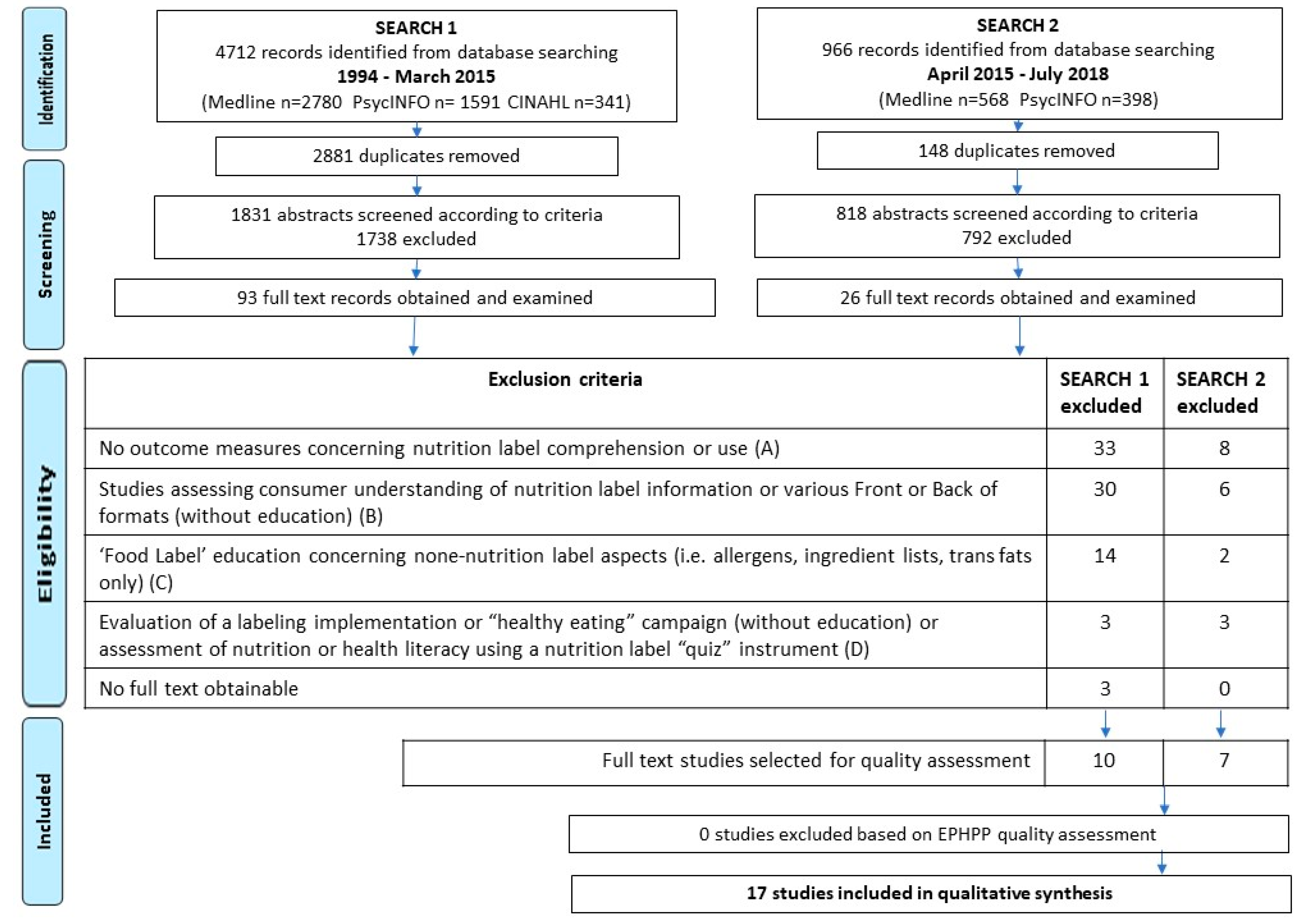
2.1. Search Strategy and Study Selection
2.2. Quality Assessment and Data Extraction
3. Results
3.1. Intervention Participants and Programs
3.2. Effect on Understanding of Nutrition Labels
3.3. Effect on Usage of Nutrition Labels
4. Discussion
4.1. Design Features of Effective Interventions
4.2. Outcome Measures
4.3. Strengths and Limitations of the Review
4.4. Implications for Practice and Research
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Campos, S.; Doxey, J.; Hammond, D. Nutrition labels on pre-packaged foods: A systematic review. Public Health Nutr. 2011, 14, 1496–1506. [Google Scholar] [CrossRef] [PubMed]
- Grunert, K.G.; Wills, J.M.; Fernández-Celemín, L. Nutrition knowledge, and use and understanding of nutrition information on food labels among consumers in the UK. Appetite 2010, 55, 177–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murimi, M.W. Healthy literacy, nutrition education, and food literacy. J. Nutr. Educ. Behav. 2013, 45, 195. [Google Scholar] [CrossRef]
- Malloy-Weir, L.; Cooper, M. Health literacy, literacy, numeracy and nutrition label understanding and use: A scoping review of the literature. J. Hum. Nutr. Diet. 2016, 30, 309–325. [Google Scholar] [CrossRef] [PubMed]
- Cowburn, G.; Stockley, L. Consumer understanding and use of nutrition labelling: A systematic review. Public Health Nutr. 2005, 8, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, S.; Hammond, D.; Goodman, S. Research Brief: Sociodemographic Differences in the Comprehension of Nutritional Labels on Food Products. J. Nutr. Educ. Behav. 2013, 45, 767–772. [Google Scholar] [CrossRef] [PubMed]
- Levy, A.S.; Fein, S.B. Consumers’ ability to perform tasks using nutrition labels. J. Nutr. Educ. 1998, 30, 210–217. [Google Scholar] [CrossRef]
- Pelletier, A.L.; Chang, W.W.; Delzell, J.E.; McCall, J.W. Patients’ Understanding and Use of Snack Food Package Nutrition Labels. J. Am. Board Fam. Pract. 2004, 17, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Roberto, C.A.; Khandpur, N. Improving the design of nutrition labels to promote healthier food choices and reasonable portion sizes. Int. J. Obes. 2014, 38 (Suppl. 1), S25–S33. [Google Scholar] [CrossRef] [Green Version]
- Malam, S.; Clegg, S.; Kirwan, S.; Mcginigal, S. Comprehension and Use of UK Nutrition Signpost Schemes; Food Standards Agency: London, UK, 2009. [Google Scholar]
- Food and Drug Administration. Labeling & Nutrition—Changes to the Nutrition Facts Label. Available online: https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm385663.htm (accessed on 29 August 2018).
- Khandpur, N.; Graham, D.J.; Roberto, C.A. Simplifying mental math: Changing how added sugars are displayed on the nutrition facts label can improve consumer understanding. Appetite 2017, 38. [Google Scholar] [CrossRef] [PubMed]
- Buttriss, J.L. The role of nutritional labelling and signposting from a European perspective. Proc. Nutr. Soc. 2018, 77, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration, Office of Regulatory Affairs. Nutritional Labeling and Education Act (NLEA) Requirements (8/94–2/95). Available online: https://www.fda.gov/iceci/inspections/inspectionguides/ucm074948.htm (accessed on 29 August 2018).
- European Union. Regulation (EU) No 1169/2011 of the European Parliament and of the Council of 25 October 2011 on the Provision of Food Information to Consumers. Available online: https://eur-lex.europa.eu/legal-content/en/ALL/?uri=CELEX%3A32011R1169 (accessed on 29 August 2018).
- Sassi, F.; Cecchini, M.; Lauer, J.; Chisholm, D. Improving Lifestyles, Tackling Obesity: The Health and Economic Impact of Prevention Strategies; OECD Health Working Papers, No. 48; OECD Publishing: Paris, France, 2009. [Google Scholar] [CrossRef]
- Storcksdieck Genannt Bonsmann, S.; Wills, J.M. Nutrition Labeling to Prevent Obesity: Reviewing the Evidence from Europe. Curr. Obes. Rep. 2012, 1, 134–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van ’t Riet, J. Sales effects of product health information at points of purchase: A systematic review. Public Health Nutr. 2013, 16, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Cecchini, M.; Warin, L. Impact of food labelling systems on food choices and eating behaviours: A systematic review and meta-analysis of randomized studies. Obes. Rev. 2015, 17, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.J.; Lucas-Thompson, R.G.; Mueller, M.P.; Jaeb, M.; Harnack, L. Impact of explained v. unexplained front-of-package nutrition labels on parent and child food choices: A randomized trial. Public Health Nutr. 2017, 20, 774–785. [Google Scholar] [CrossRef] [PubMed]
- Alessandro, L.; Douglas, G.A.; Jennifer, T.; Cynthia, M.; Peter, C.G.; John, P.; Ioannidis, A.; Mike, C.; Devereaux, P.J.; Jos, K.; et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Lindhorst, K.; Corby, L.; Roberts, S.; Zeiler, S. Rural consumers’ attitudes towards nutrition labelling. Can. J. Diet. Pract. Res. 2007, 68, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Dukeshire, S.; Nicks, E.; Ferguson, J. Pilot Evaluation of an In-Store Nutrition Label Education Program. Can. J. Diet. Pract. Res. 2014, 75, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.K.; Jensen, G.L.; Achterberg, C.L. Evaluation of food label nutrition intervention for women with type 2 diabetes mellitus. J. Am. Diet. Assoc. 1999, 99, 323–328. [Google Scholar] [CrossRef]
- Treu, J.A.; Doughty, K.; Reynolds, J.S.; Njike, V.Y.; Katz, D.L. Advancing School and Community Engagement Now for Disease Prevention (ASCEND): A quasi-experimental trial of school-based interventions to prevent childhood obesity. Am. J. Health Promot. 2017, 31, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.K.; Edwards, L.; Kissling, G.; Sanville, L. Evaluation of a theory-based nutrition intervention for older adults with diabetes mellitus. J. Am. Diet. Assoc. 2002, 102, 1069–1081. [Google Scholar] [CrossRef]
- Pennings, M.; Striano, T.; Oliverio, S. A picture tells a thousand words: Impact of an educational nutrition booklet on nutrition label gazing. Mark. Lett. 2014, 25, 355–360. [Google Scholar] [CrossRef]
- Miller, L.M.S.; Beckett, L.A.; Bergman, J.J.; Wilson, M.D.; Applegate, E.A.; Gibson, T.N. Developing Nutrition Label Reading Skills: A Web-Based Practice Approach. J. Med. Internet Res. 2017, 19, e16. [Google Scholar] [CrossRef] [PubMed]
- Katz, D.L.; Treu, J.A.; Ayettey, R.G.; Kavak, Y.; Katz, C.S.; Njike, V. Testing the Effectiveness of an Abbreviated Version of the Nutrition Detectives Program. Prev. Chronic Dis. 2014, 11, E57. [Google Scholar] [CrossRef] [PubMed]
- Gavaravarapu, S.M.; Saha, S.; Vemula, S.R.; Mendu, V.V.R. Read-B4-U-Eat: A multicomponent communication module to promote food label reading skills among adolescents in India. J. Nutr. Educ. Behav. 2016, 48, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, W.S.; Scott-Pierce, M.; Dollahite, J. Research Brief: Choose Health: Food, Fun, and Fitness Youth Curriculum Promotes Positive Behaviors. J. Nutr. Educ. Behav. 2017, S1499–S4046. [Google Scholar] [CrossRef]
- Hawthorne, K.M.; Moreland, K.; Griffin, I.J.; Abrams, S.A. Research: An Educational Program Enhances Food Label Understanding of Young Adolescents. J. Am. Diet. Assoc. 2006, 106, 913–916. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.L.; Reardon, R.; Hammond, E.; Parrett, A.; Gebbie-Diben, A. Evaluation of the “Eat Better Feel Better” Cooking Programme to Tackle Barriers to Healthy Eating. Int. J. Environ. Res. Public Health 2017, 14, 380. [Google Scholar] [CrossRef] [PubMed]
- Kollannoor-Samuel, G.; Shebl, F.M.; Segura-Pérez, S.; Chhabra, J.; Vega-López, S.; Pérez-Escamilla, R. Effects of Food Label Use on Diet Quality and Glycemic Control Among Latinos With Type 2 Diabetes in a Community Health Worker-Supported Intervention. Am. J. Public Health 2016, 106, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Pettigrew, S.; Moore, S.; Pratt, I.S.; Jongenelis, M. Evaluation outcomes of a long-running adult nutrition education programme. Public Health Nutr. 2016, 19, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Neuenschwander, L.M.; Abbott, A.; Mobley, A.R. Research: Comparison of a Web-Based vs In-Person Nutrition Education Program for Low-Income Adults. J. Acad. Nutr. Diet. 2013, 113, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Jay, M.; Adams, J.; Herring, S.J.; Gillespie, C.; Ark, T.; Feldman, H.; Jones, V.; Zabar, S.; Stevens, D.; Kalet, A. A randomized trial of a brief multimedia intervention to improve comprehension of food labels. Prev. Med. 2009, 48, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Chapman-Novakofski, K.; Karduck, J. Research: Improvement in Knowledge, Social Cognitive Theory Variables, and Movement through Stages of Change after a Community-Based Diabetes Education Program. J. Am. Diet. Assoc. 2005, 105, 1613–1616. [Google Scholar] [CrossRef] [PubMed]
- Murimi, M.W.; Kanyi, M.; Mupfudze, T.; Amin, M.R.; Mbogori, T.; Aldubayan, K. Systematic Review: Factors Influencing Efficacy of Nutrition Education Interventions: A Systematic Review. J. Nutr. Educ. Behav. 2017, 49, 142–165.e1. [Google Scholar] [CrossRef] [PubMed]
- Alberti, T.L.; Morris, N.J. Health literacy in the urgent care setting: What factors impact consumer comprehension of health information? J. Am. Assoc. Nurse Pract. 2017, 29, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Mackert, M.; Champlin, S.E.; Pasch, K.E.; Weiss, B.D. Understanding Health Literacy Measurement Through Eye Tracking. J. Health Commun. 2013, 18, 185–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharif, M.Z.; Rizzo, S.; Prelip, M.L.; Glik, D.C.; Belin, T.R.; Langellier, B.A.; Kuo, A.A.; Garza, J.R.; Ortega, A.N. The association between nutrition facts label utilization and comprehension among Latinos in two east Los Angeles neighborhoods. J. Acad. Nutr. Diet. 2014, 114, 1915–1922. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.M.S.; Cassady, D.L. Making healthy food choices using nutrition facts panels. The roles of knowledge, motivation, dietary modifications goals, and age. Appetite 2012, 59, 129–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kliemann, N.; Kraemer, M.; Scapin, T.; Rodrigues, V.; Fernandes, A.; Bernardo, G.; Uggioni, P.; Proença, R. Serving Size and Nutrition Labelling: Implications for Nutrition Information and Nutrition Claims on Packaged Foods. Nutrients 2018, 891. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.M.S.; Cassady, D.L. The effects of nutrition knowledge on food label use. A review of the literature. Appetite 2015, 92, 207–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Contento, I.R.; Randell, J.S.; Basch, C.E. Review and Analysis of Evaluation Measures Used in Nutrition Education Intervention Research. J. Nutr. Educ. Behav. 2002, 34, 2–25. [Google Scholar] [CrossRef]
- Sharf, M.; Sela, R.; Zentner, G.; Shoob, H.; Shai, I.; Stein-Zamir, C. Figuring out food labels. Young adults’ understanding of nutritional information presented on food labels is inadequate. Appetite 2012, 58, 531–534. [Google Scholar] [CrossRef] [PubMed]
| Ref (Country) | Sample Characteristics (Size) | Intervention Program Description, Aims, and Delivery Format | Study Design, Follow-up (Control Group) | Setting | Session Duration | Theory | Nutrition Label Use | Nutrition label Understanding | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Measure | Impact | Outcome Measure | Impact | |||||||
| [27] U.S. | Older adults with type 2 diabetes. 53% women. ≥65 years old. (n = 93) | Nutrition labeling education program to improve food label knowledge and skills in diabetes management. Delivered in-person by dietitians. | Randomized controlled trial. Pre-posttest. (Control group: no contact other than mailed questionnaire) | Outpatient | 10 weekly group sessions (each 1.5 h) | SCT. IP | Confidence in using food labels. i.e., “I can choose foods high in fiber” | Significantly increased in experimental not control group (p < 0.001) | Total, procedural and declarative knowledge of the food label and decision-making skills. | Procedural, declarative and total knowledge scores and decision-making skills increased significantly for intervention group but not for control group (all p < 0.01). |
| [25] U.S. | Women with type 2 diabetes. 40–60 years old. (n = 40) | Nutrition labeling education program to facilitate the application of information on the food label to meet patient’s needs. Delivered in-person by dietitians | Pre-posttest control group design. (Control group: no contact other than mailed questionnaire). | Community centres | 9 weekly group sessions | TML | Confidence in skills using the food label. | Significantly increased in experimental, not control group (p < 0.01) | Nutrition and food label related knowledge: Total, procedural, and declarative. | Both total, procedural and declarative knowledge were significantly increased in experimental, not control group (p < 0.01). |
| [38] U.S. | Low-income adult patients. Mean age 50 years. 73% female. (n = 42) | Intervention to improve nutrition label comprehension. Brief interactive multi-media video and pocket card. Tutor delivered. | Randomized (controlled) trial, Pre-posttest. (Control group: received black and white reading materials only). | Healthcare center | 1 group session, 45 min total. | NS | Confidence in nutrition knowledge. | No significant difference between groups. | Nutrition label knowledge comprehension quiz score (%), including accurate interpretation of %DV and serving size information. | Quiz score pre-post gains were greater for the intervention group than the control group (p < 0.05). Sub group analysis of (n = 7) participants with low health literacy found no significant increase for either group. |
| [39] U.S. | U.S. older adults with diabetes. Mean age 63 years. 73% female. (n = 239) | Dining with Diabetes: Diabetes education program about healthy eating and food label components. Group taught sessions delivered in person. | Cohort using pre- posttests. | Community-based | 3-monthly group sessions, 2 h each. | SoC SCT | Confidence in ability to use labels | Significant pre-posttest improvement (p < 0.01). | Knowledge questions included the nutrition label items. Exact details NS | Knowledge scores were significantly better post, compared to pretest (p = 0.001). Knowledge scores were a significant factor for response to “Do you agree you know how to use food labels?” |
| [24] Canada | Adults. Aged 31–75 years. >90% female. (n = 19) | An in-store Nutrition Label Education Program designed to teach how to read nutrition facts panel. Delivered by a registered dietitian using a lecture with materials followed by a store tour | Cohort pre- postsurvey and one-month follow-up (n = 3). | Grocery Store | A 2-h group session. | NS | Self-confidence, awareness and ability to use nutrition labels | Self-confidence performing all seven activities were significantly increased posttest (p < 0.01). | Self-reported knowledge of the NFP assessed using two items (serving size and definition of the term “percent daily value”). | Increase in number of participants answering %DV question correct (15.8% to 57.9%). Smaller increase in number of participants correctly identifying serving size (26.3% to 36.8%). |
| [36] Australia | Disadvantaged adults. Age NS. 76% female. (n = 927) | FOODcents nutrition education program: aims to improve household food expenditure according to the healthy eating pyramid, includes food label reading. Delivered face-to-face with cooking sessions and supermarket tours. | Cohort comprising 54% of the FOODcent centers, includes different program durations. Pre-post survey and six-week online follow-up (n = 97). | Community-based | Single group session of 1–2 h or up to 8 sessions. | P&P. | Reading of the nutrition information panel (self-reported) | Significantly increased at six-week follow-up (p < 0.01). | Knowledge of interpreting food labels used three questions including one item on nutrition labels: “In 100 g of this product how many grams of sugar are there?” | Higher proportion of correct responses in post-session surveys. No significant differences by socioeconomic status. |
| [31] India | School children. Aged 12–15 years. Females: NS. (n = 175) | READ-B4-U-EAT multicomponent school module to promote use of food label information and informed food choices. Delivered using videos, handouts and presentations, by teachers. | Intervention group and comparison group using pre-post intervention questionnaires. (Comparison group received a lecture about food labels.) | School | 4 sessions of 45 min | SCT | Use of nutrition labels evaluated with 5 questions(self-reported) i.e., “Do you read the sugar content when buying chocolate?” | 1 question showed improvements in intervention compared to comparison group (p < 0.05), i.e., “Do you see the salt content when buying snacks?” | Knowledge of nutrition label assessed using item: “Is nutrition information present on this label”? | Significant improvement in intervention compared to control group (p < 0.05) |
| [37] U.S. | Low income U.S. adults Aged 18–50 years. 90% female. (n = 123) | Web based nutrition education program on healthy eating including nutrition label reading. | Randomized block equivalence (comparator group received in-person taught session). | Own home computer/community centre | 3 sessions each 30–40 min | KEL | Frequency of use of labels when shopping (self-reported). “When shopping do you use nutrition labels to decide what food to buy?” | Both groups significantly increased at post-intervention but in-person group showed greatest improvement. | NP | NP |
| [28] U.S. | College students. Aged 17–24 years. 63% females. (n = 32) | Thumbs Up Healthy Eating Nutrition Education booklet designed to promote attention focus on nutrition labels on product packaging. | Randomized controlled, pre-posttest. (Control group viewed a word puzzle). | University | A 10-min session. | IP | Eye gaze time on nutrition labels on cereal box packaging images. | Participants in the experimental group gazed longer at nutrition labels during post-test compared to the pre-test (p < 0.01) and at posttest compared to the control group (p < 0.001). | NP | NP |
| [35] U.S. | Latinos with Type II diabetes. Median age 57 years. 73% female. (n = 203) | Diabetes among Latinos Best Practices Trial (DIALBEST) on food labels and glycemic control. Includes nutrition education and how to interpret food labels. Delivered with individuals by community health workers. | Block-randomized to either intervention or control groups which were evaluated at baseline, 3,6,12,18 months (control group received standard care). | Home-based (and store visit) | 17 home-based sessions over a 12-month period. | NS | Frequency of use of food labels (self-reported). | Food label use significantly higher in the intervention vs control groups at 3, 12, and 18 months (p < 0.01). | NP | NP |
| [23] Canada | Adults. Aged 18–65 years. 81% female. (n = 259) | Healthy Eating is in Store for You—a nutrition labeling education program aiming to help consumers make food choices promoting healthy weight. Delivered by trained community health officers. | Cohort comprised of 18 workshops across the country. Pre-posttest and 3-month follow-up questionnaires. (n = 35) | Community-based | 1 session | NS | Nutrition label attitudes and behaviors (self-reported). i.e., “Is it important to you to review the nutrition information before buying that food”? | Data on 35 participants only available at 3-month follow-up. Increased proportions of participants selecting higher responses. | NP | NP |
| [34] UK | Vulnerable adults. Aged >45 years. 68% female. (n = 62) | Eat Better Feel Better community-based cooking program aimed at tackling barriers to cooking and healthy eating. Delivered by community-trained chefs. | Single group repeated measures. Pre and post intervention and 3–4 month follow-up (n = 17). | Community-based | 6-weekly sessions of 2 h. | NS | (1) Confidence reading food labels (self-reported). (2) Food label elements read (indicated using tick boxes) | (1) Significantly increased from baseline to post intervention (p < 0.01) (2) Reading of nutrition elements Significantly increased from baseline to post intervention and follow-up. | NP | NP |
| [32] U.S. | School children in grades 3–5 and 6–8. ~50% female. (n = 1334) | Choose Health: Food, Fun, and Fitness Youth Curriculum aimed at enhancing knowledge and skills building. Incudes label reading. Delivered by community health educators. | 2 cohort sub-samples, across age groups and settings evaluated using pre-post surveys (which featured nutrition label items) | School, clubs, summer camp | 6-weekly lessons 45–90 min each. | SCT EL | Reading of nutrition information (self-reported) i.e., “I read nutrition facts labels on food packages” | Significantly increased post-survey (p <0.01) | NP | NP |
| [26] U.S. | School children in grade 3. Mean age 8.7 years. 52% female. (n = 1487) | Nutrition Detectives and ABC for Fitness programs (standard intervention), alongside family, home, and supermarket sessions (enhanced intervention). | Quasi-experimental 3 group design. Schools randomized on district. Pre-posttests. (Control group received normal curriculum and no pre-posttests.) | School | 90-min class session. 3-month follow-up, 30-min booster. | NS | NP | NP | Food Literacy and Label Nutrition Knowledge (FLLANK) test to evaluate knowledge of healthful food choices. | Both groups increased FLLANK scores compared to baseline values after first and booster sessions (p < 0.01). No significant difference in this improvement between the two intervention groups. |
| [29] U.S. | College students. Mean age 20.7 years. 60% female. (n = 140) | Web-based label-reading training tool to improve individuals’ ability to use labels to select more healthful foods. Training tasks required individuals to compare 3 × 24 different pairs of nutrition labels to select the healthiest. | Randomized to 2 groups. Prior knowledge group received short presentation. Basic group did not. | University | One session of 60–90 min. | Skill | NP | NP | Accuracy (of selecting correct answer in training tasks) | Accuracy increased with practice, across each of the three training blocks (p < 0.01). In block 3, the odds of a correct answer for the prior-knowledge group were 79% higher than those in the basic group (p = 0.02). |
| [33] U.S. | Young adolescents. Aged 11–14 years. 47% female. (n = 34) | How to read and use a nutrition facts label education program. Delivered by a registered dietitian. | Single cohort using pre-posttests. | NS | 1 group session of 1 h. | NS | NP | NP | Nutrition Facts Label knowledge pre- posttests developed by author (calculating %DV with differing serving sizes and defining DV). | Overall test score improved significantly pre-posttest (p < 0.01) Correct answers to the questions concerning %DV definition improved significantly (p = 0.03) from 38% to 74%, as did correct answers to question concerning serving size modification calculations (p = 0.003). No difference in boys or girls scores. |
| [30] U.S. | Grade 5 school children. Age NS. 58% female. (n = 212) | Nutrition Detectives educational program on how to read food labels aimed at developing food-literacy skills. Taught by teacher within class (presentation and practical) | Cohort comprising of classes across 5 schools, using pre -posttests. | School class | 1 session of 45 min | NS | NP | NP | Food label literacy (quiz) evaluating ability to distinguish between healthy and unhealthy foods using the Nutrition Facts panel. | Quiz scores increased significantly pre-posttest by 16.2% (ranging from 4.3%–23.6% among schools) (p < 0.01). Girls score improved significantly more than boys (p = 0.04) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moore, S.G.; Donnelly, J.K.; Jones, S.; Cade, J.E. Effect of Educational Interventions on Understanding and Use of Nutrition Labels: A Systematic Review. Nutrients 2018, 10, 1432. https://doi.org/10.3390/nu10101432
Moore SG, Donnelly JK, Jones S, Cade JE. Effect of Educational Interventions on Understanding and Use of Nutrition Labels: A Systematic Review. Nutrients. 2018; 10(10):1432. https://doi.org/10.3390/nu10101432
Chicago/Turabian StyleMoore, Sally G., Judy K. Donnelly, Steve Jones, and Janet E. Cade. 2018. "Effect of Educational Interventions on Understanding and Use of Nutrition Labels: A Systematic Review" Nutrients 10, no. 10: 1432. https://doi.org/10.3390/nu10101432
APA StyleMoore, S. G., Donnelly, J. K., Jones, S., & Cade, J. E. (2018). Effect of Educational Interventions on Understanding and Use of Nutrition Labels: A Systematic Review. Nutrients, 10(10), 1432. https://doi.org/10.3390/nu10101432






