1. Introduction
Digital technologies are transforming healthcare systems worldwide. The Digitalization of Healthcare, known as Health 4.0, with the application of powerful technologies such as Artificial Intelligence (AI), telemedicine, and the Internet of Medical Things (IoMT) [
1], is transforming the delivery of healthcare. These advancements are likely to introduce enormous changes in healthcare accessibility, performance, and responsiveness [
2]. Saudi Arabia, within the scope of its Vision 2030, is adopting Health 4.0 to transform its healthcare ecosystem and address decades-long issues of geographical limitations, resource limitations, and the demand for individually tailored healthcare services [
3]. In this transformation, Saudi Arabia is focusing on the development of e-health services, including telemedicine, electronic health records, and mobile health applications, to improve the accessibility and quality of medical care in the country.
DHL refers specifically to an individual’s ability to effectively use digital health tools, such as telemedicine platforms, mobile health applications, and wearable devices. On the other hand, digital environmental literacy focuses on understanding and managing the environmental impacts of digital health technologies, including energy consumption, e-waste, and carbon emissions. The effective penetration of e-health services, however, is dependent on the population’s capability to access and effectively use these technologies [
4]. In this context, DHL has emerged as a defining factor in the progress of Health 4.0, shaping how individuals engage with and benefit from digital health innovations. However, with the growing integration of technology, it is increasingly important to broaden the scope of Digital Health Literacy (DHL) to include two critical components: digital environmental literacy, which enables individuals to understand and reduce the environmental impact of their digital health behaviors, and digital stewardship, which promotes responsible and sustainable use of digital technologies in health contexts. This integrated perspective ensures that citizens are not only equipped to use digital health technologies effectively but also do so in environmentally conscious ways that align with long-term sustainability goals [
5]. The lack of adequate DHL, particularly in these expanded dimensions, may limit individuals’ ability to navigate and benefit fully from e-health services. This underscores the importance of addressing DHL as a core strategy for promoting healthcare sustainability and equity, especially as Saudi Arabia accelerates its transition toward a digital health ecosystem under Vision 2030.
The DHL readiness of the Saudi Arabian adult population has a significant gap, despite the increasing availability of digital health technologies within the country. The lack of e-health accessibility skills has continued to leave many people unskilled in using e-health services [
6], making it difficult for them to fully utilize the digital health tools offered. Several factors also contribute to this readiness gap, including age, level of education, access to technologies, and societal and cultural influences. Such obstacles raise particular concern, considering the rapid pace of healthcare digitalization in Saudi Arabia and the nation’s efforts to reduce its overall dependence on unsustainable and inaccessible e-health [
7]. DHL is a significant gap that needs to be addressed to realize the potential of Health 4.0 and make the digital healthcare revolution accessible to all segments of the population, benefiting them.
The primary objective of this study is to assess the preparedness of Saudi adults for DHL and to investigate the key factors influencing their ability to utilize e-health services. The study aims to specifically assess the population’s current levels of DHL, identify the technological and socioeconomic factors influencing preparedness, and examine the implications of DHL for the long-term utilization of e-health services in Saudi Arabia within the context of the health 4.0 framework. By investigating these areas, the study will provide valuable insights that can inform the development of strategies to enhance DHL among diverse populations, ultimately improving the sustainability and integration of e-health services. While this study focuses on assessing DHL and readiness as enablers for Health 4.0, including AI-driven tools, IoMT, and clinical decision support systems (CDSS), it lays the necessary behavioral and social foundation for their effective deployment and sustained adoption.
This study is significant for the successful implementation of e-health services in Saudi Arabia and for achieving the broader goals of Vision 2030. As the Kingdom continues to invest in the digitalization of healthcare through Health 4.0, ensuring that the population is digitally literate in the use of healthcare technologies is crucial. Improving DHL will not only enhance the adoption of e-health tools but also contribute to reducing healthcare disparities and improving overall health outcomes. By identifying the barriers to DHL and addressing them, this research will inform policymakers, healthcare providers, and educators in designing effective interventions to increase DHL across Saudi Arabia. This, in turn, will help ensure the sustainability and success of e-health services, benefiting all citizens and contributing to a more inclusive healthcare system.
This study is structured as follows:
Section 2 presents the conceptual and empirical literature on DHL;
Section 3 details the methodology, including survey design and analytical models.
Section 4 presents the results and discussion.
Section 5 concludes with policy implications and limitations.
3. Methodology
3.1. Study Design and Rationale
The proposal research employs a multi-phase, cross-sectional quantitative design, as presented in
Figure 1, to evaluate the DHL readiness of Saudi adults and analyze essential predictors of the use of Health 4.0 technologies. The study is designed to provide both a population-level and network-derived understanding of behavioral diffusion through the application of sophisticated statistical methods. Based on the application of science frameworks, including RE-AIM and CFIR, and utilizing SNA and NBDA, the design enables addressing both individual readiness and social impact on digital health engagement.
3.1.1. Study Design
The study method is rigorous and practically applicable, incorporating pilot testing, scale validation, and reliability assessment prior to full deployment. The methodology follows these phases:
Phase I: Stakeholder analysis and expert consultation are performed to establish the conceptual frameworks.
Phase II: A comprehensive survey is designed based on adapted and validated scales, and pilot testing is conducted to ensure item clarity, cultural appropriateness, and reliability.
Phase III: Data collection occurs using stratified random sampling.
Phase IV: CFA is applied to validate the factor structure of the adapted scales, ensuring construct reliability and factorial invariance across demographic groups.
3.1.2. Statistical Software Usage
The statistical analysis is performed using SPSS 29 for descriptive and inferential statistics (e.g., t-tests, ANOVA, multiple regression), and R is used for structural equation modeling (SEM) and network analysis (SNA and NBDA). These tools are selected based on their suitability for handling the specific analyses conducted in the study.
3.2. Conceptual Framework and Phase Overview
The study adopts a multi-phase design, comprising a cross-sectional baseline survey followed by a prospective longitudinal follow-up in Phase V. This integrated approach captures both the current state of DHL readiness and subsequent changes in adoption patterns over time, ensuring methodological rigor and alignment with research objectives.
3.2.1. Phase I: Conceptualization and Stakeholder Analysis
This stage establishes the conceptual framework of the study. A literature review and expert consultation are conducted to compile a logic model that demonstrates the hypothetical pathway from DHL to effective Health 4.0 engagement, encompassing the use of eHealth and improved confidence, decision-making, and health outcomes [
10]. Stakeholder feedback is obtained through expert surveys or Delphi methods to secure contextually relevant information. Furthermore, to ensure ecological integration within the DHL framework, environmental indicators, such as reductions in carbon emissions, life-cycle sustainability of digital devices, and renewable energy usage, are incorporated. Additionally, feedback is gathered from key stakeholders, including ICT suppliers with a focus on sustainability practices, NGOs advocating for sustainable digital rights, and international agencies monitoring progress towards SDG targets, thereby contributing to a comprehensive and inclusive framework.
3.2.2. Phase II: Survey Design and Instrument Development
At this stage, a comprehensive web-based questionnaire is designed based on validated measurements, including eHEALS for DHL, TRI 2.0 for technology readiness, and selected UTAUT construct performance expectancy, effort expectancy, social influence, and facilitating conditions as predictors of behavioral intention. EQ-5D is employed to measure health-related quality of life [
28]. The instrument also includes items to capture social connections, such as trusted health advisors and sources of digital health information, to support SNA. Tools are translated into Arabic and back-translated for accuracy. Internal consistency is evaluated post-deployment using Cronbach’s alpha, with a threshold of 0.70 or higher considered acceptable.
A conceptual distinction is maintained between Technology Readiness (TRI 2.0) and eHealth Readiness (eHEALS-based DHL). Technology Readiness reflects a general predisposition toward adopting or resisting new technologies, including optimism, innovativeness, discomfort, and insecurity. In contrast, eHealth Readiness captures domain-specific competencies and confidence in engaging with digital health platforms for informed health decision-making. This distinction ensures that both general and context-specific readiness are systematically assessed.
3.2.3. Phase III: Nationwide Data Collection
The finalized questionnaire is deployed in a nationwide cross-sectional survey targeting Saudi adults aged 18 and above. Stratified random sampling ensures representation across age, gender, education, and geographic region. The survey is distributed digitally, and informed consent is obtained electronically. Social network questions collect relational data (e.g., frequency of interaction and trust ties) for subsequent SNA. This phase generates a robust dataset for identifying DHL trends, predictors of eHealth readiness, and patterns of interpersonal influence on technology adoption across social structures.
3.2.4. Phase IV: Data Analysis and Social Network Mapping
Quantitative data are analyzed using SPSS or R. Descriptive and inferential statistics (e.g.,
t-tests, ANOVA, multivariate regression) are applied to examine DHL levels and their determinants. SEM tests relationships among variables, including UTAUT constructs. SNA is conducted using relational data to map peer networks, identify central influencers (via degree and betweenness centrality), and analyze subgroup structures [
29]. Comparing DHL levels across network positions offers insights into how social position correlates with digital readiness and trust in eHealth technologies.
3.2.5. Phase V: Network-Based Diffusion and Implementation Evaluation
To examine how the adoption of DHL and eHealth spreads socially, a subset of participants completes a follow-up survey approximately 3–6 months after the baseline. NBDA is applied to model whether adoption behaviors cluster around influential individuals within the social network [
30]. Where available, behavioral data such as app usage or portal login frequency are collected. The RE-AIM framework is used to evaluate program reach, effectiveness, adoption, implementation fidelity, and maintenance. Together, NBDA and RE-AIM provide insights into both individual outcomes and system-level sustainability and equity of digital health engagement. All phases; from Phase 1 to Phase 5 are depicted in
Table 1.
3.3. Population and Sampling
A priori sample size calculation for multiple regression and SEM was conducted using G*Power. Assuming a medium effect size (f2 = 0.15), significance level α = 0.05, and statistical power = 0.95 with 10 predictors, the estimated minimum sample size was 172 participants. However, given the study’s use of advanced multivariate techniques including SEM, SNA, and Network-Based Diffusion Analysis (NBDA), a target sample of 430 participants was selected. This larger sample ensures adequate power for structural modeling, enhances subgroup comparisons, and improves the robustness of behavioral and network-based inferences. The minimum sample size required to achieve adequate statistical power for multivariate analyses across regression analyses, SEM, SNA, and NBDA is 430 participants. It enables the collection of sufficient amounts of relational and behavioral data to facilitate trustworthy interpretation and modeling of adoption patterns.
Inclusion and Exclusion Criteria
Saudi adults aged 18 years and above from both urban and rural regions were included using stratified random sampling to ensure representativeness. Participants who submitted incomplete responses or failed to meet the age or residency criteria were excluded to maintain the quality and reliability of the data.
3.4. Data Collection
The data collection consists of a self-administered online questionnaire, based on a structured questionnaire, to obtain a comprehensive profile of the participants’ digital health reading habits. Some validated scales adapted to the Saudi context are incorporated into the instrument. The degree of DHL is assessed using the eHealth Literacy Scale (eHEALS), which comprises eight questions evaluated on a 5-point Likert-type scale. The Technology Readiness Index (TRI 2.0) with its 16-item structure is employed to assess technology readiness using a 7-point Likert scale. Behavioral intention to adopt eHealth is evaluated through selected constructs from the Unified Theory of Acceptance and Use of Technology (UTAUT). At the same time, self-reported health-related quality of life has been measured using the EQ-5D. Additional items collect demographic data, including age, gender, and education, income, and internet access. Social network-related questions explore peer interactions, trust in digital health advisors, and frequency of health-related communication. The questionnaire is available in both Arabic and English, and electronic informed consent has been obtained before participation.
The Arabic versions of the eHEALS and TRI 2.0 instruments undergo a rigorous translation and back-translation process to ensure linguistic and conceptual accuracy. Prior to full deployment, pilot testing is conducted to assess clarity and cultural appropriateness. Reliability testing demonstrates strong internal consistency, with Cronbach’s α of 0.89 for eHEALS and 0.86 for TRI 2.0, both exceeding the recommended 0.70 threshold. Multi-group confirmatory factor analysis confirms configural and metric invariance across gender, education, and urban/rural groups, indicating consistent factor structure and loadings as shown in
Table 2. These steps collectively substantiate the reliability and validity of the adapted tools for use in Saudi Arabia.
3.5. Data Analysis
Data analysis will be conducted using SPSS and R, applying a range of statistical and network modeling techniques to examine DHL, technology readiness, behavioral intention, and adoption patterns. The following analytical procedures will be used:
Descriptive analysis will summarize demographic characteristics (e.g., age, gender, education, region) and core variables (e.g., eHEALS, TRI 2.0, UTAUT constructs, EQ-5D). Continuous variables will be reported as means ± standard deviations (SD), and categorical variables will be presented as frequencies and percentages, to provide a profile of the sample and trends in the distribution of digital health indicators. In addition, Pearson’s correlation coefficients (r) will be used to examine linear relationships between continuous variables, such as eHEALS, TRI scores, EQ-5D, and behavioral intention scores. The p-value of <0.05 will be considered statistically significant.
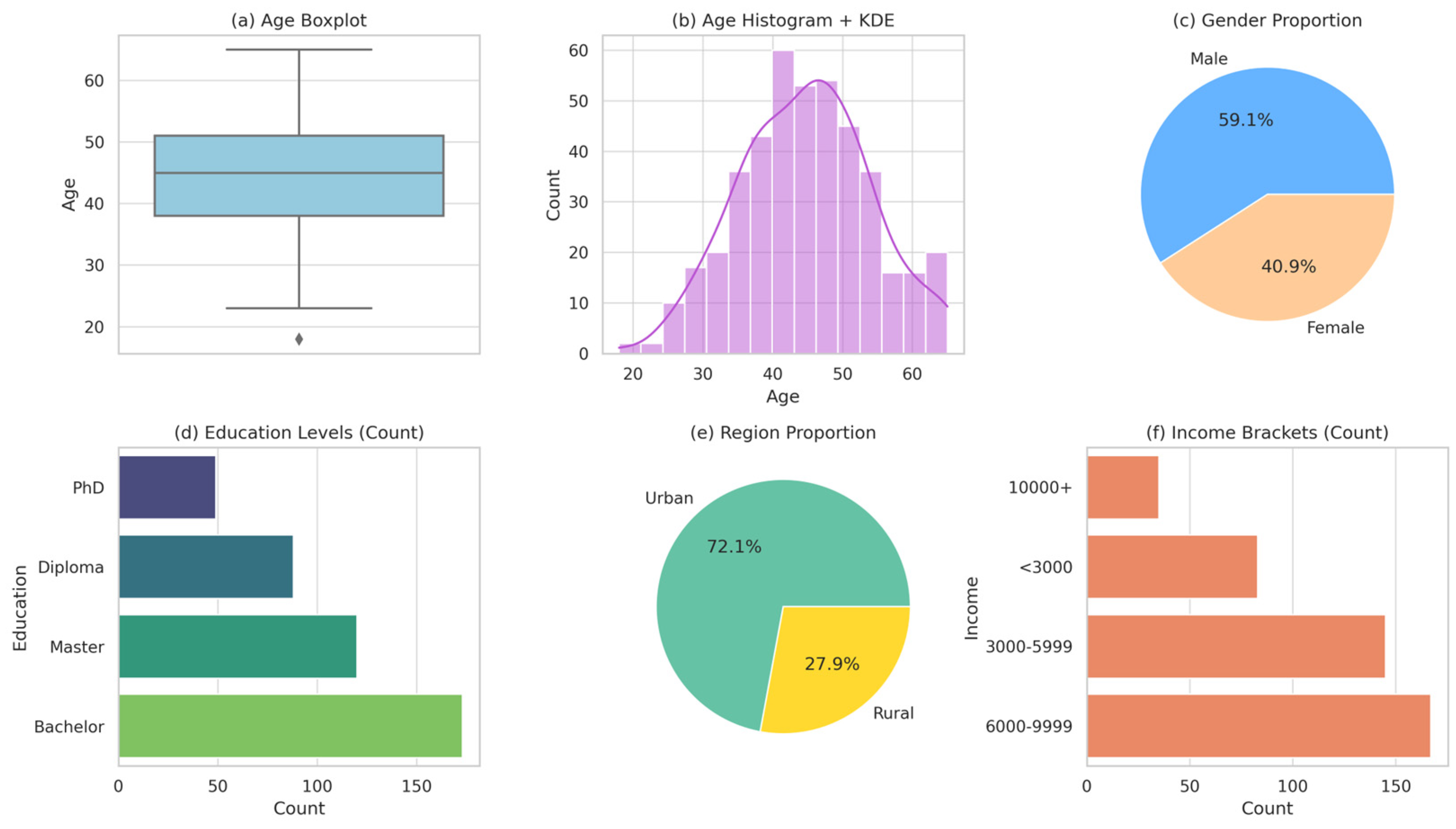
Figure 2 provides a detailed representation of the study participants. The age distribution shows a balanced age spread, with a median age of approximately 42 years, indicating that respondents in their midlife dominate the sample. The gender representation is quite good but skewed towards males (54.2%). The education level is varied, but most participants hold bachelor’s degrees, which means they could be referred to in digital health studies. There is a concentration in the income distribution, with the 3000–9999 SAR category indicating a moderate socioeconomic standing. In terms of region, 70.6% of residents are in urban areas, despite biases in digital involvement. These attributes are critical because known characteristics affecting digital health readiness and adoption, such as education, income, and living in urban areas, are likely to impact the evaluation of eHealth equity, warranting them as appropriate attributes of contextual validity and representativeness of the sample.
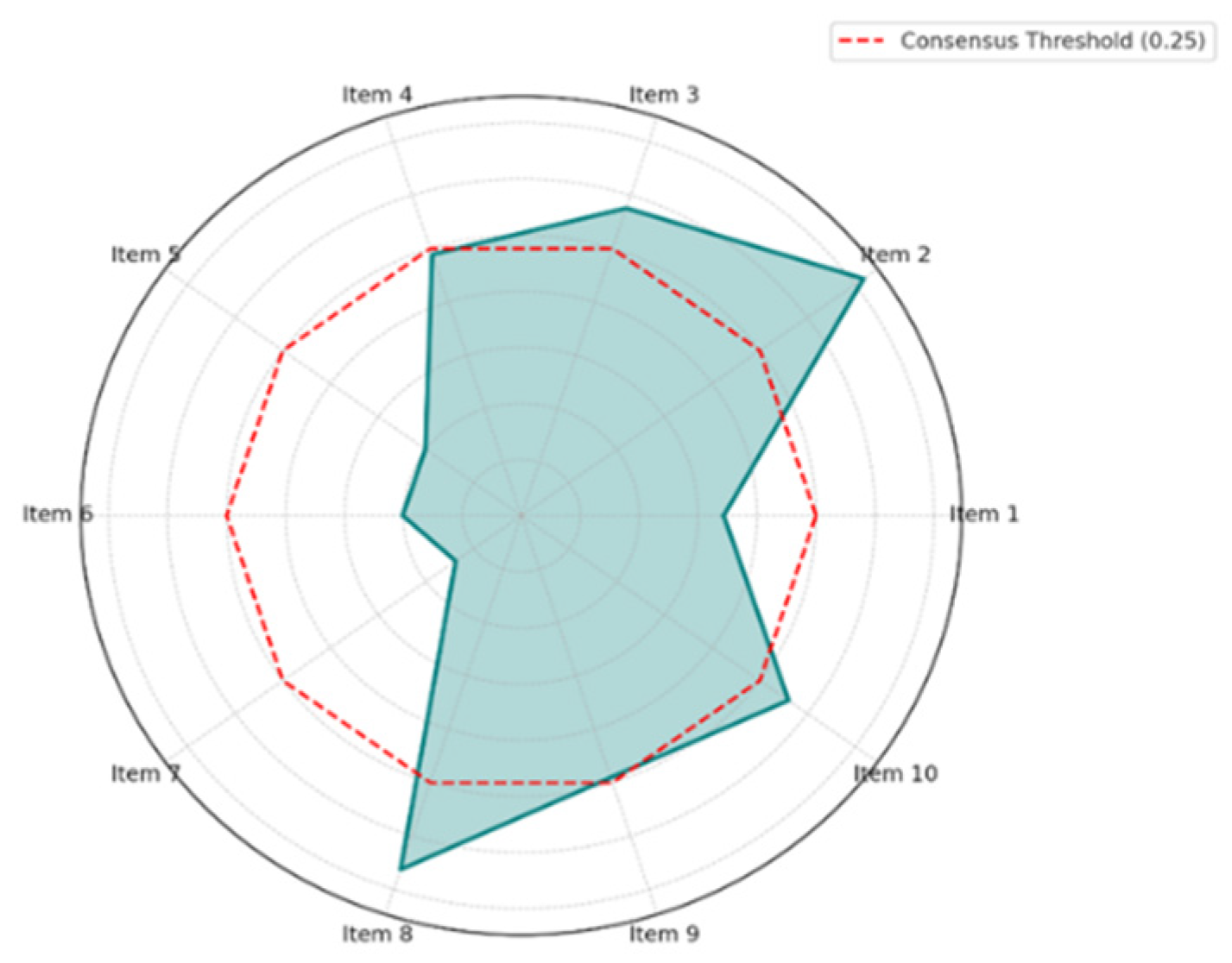
Digital environmental literacy and stewardship were incorporated into the DHL Equity Framework based on input from an international Delphi panel of 31 experts in digital health, sustainability, and health equity. While only Item 6 met the consensus threshold (CI ≤ 0.25), related items on stewardship and literacy came close (CI 0.26–0.30). Experts highlighted the rising importance of user responsibility and carbon-aware practices, especially with the growth of IoMT and telehealth. Thematic synthesis of qualitative feedback underscored concerns around device lifecycle impacts and energy efficiency, shaping the final domain definitions. To identify predictors of DHL and intention to adopt digital tools, multiple linear regression models will be used. The equation for the model is:
where
Y: Dependent variable (e.g., DHL score or behavioral intention)
β0: Intercept
Independent variables (age, gender, education, income, TRI, UTAUT scores, EQ-5D)
Regression coefficients
ε = Error term.
Model fit will be evaluated using the R-squared statistics R2, Adjusted R-squared R2, and F-statistics. Multicollinearity will be assessed via the Variance Inflation Factor (VIF < 5). Residual plots will be used to confirm linearity and homoscedasticity.
3.5.1. Delphi Method Validation
In Phase I, a Delphi method will be employed to achieve expert consensus on the logic model and core domains of DHL. A panel of 10–15 subject matter experts will participate in 2–3 iterative rounds of structured rating using a 5-point Likert scale.
The Consensus Index (CI) will be calculated as:
where
C: Average consensus score
Interquartile range of item i
k: Total number of items
Range: Likert scale span (e.g., 1 to 5 = 4)
Consensus will be considered acceptable when CI ≤ 0.25 or when ≥80% of items have IQR ≤ 1, indicating high agreement and content validity for the constructs selected.
3.5.2. Structural Equation Modeling (SEM)
To validate hypothesized relationships between DHL, technology readiness, and adoption intention, SEM will be performed using the lavaan package in R.
η = endogenous latent variables (e.g., intention to adopt)
ξ = exogenous latent variables (e.g., DHL, TRI)
B = matrix of coefficients among endogenous variables
Γ = regression weights from exogenous to endogenous
ζ = error term.
Goodness-of-fit indices such as CFI (>0.90), RMSEA (<0.08), and χ2/df (<3) will be used to assess model fit.
3.5.3. Social Network Analysis (SNA)
To analyze digital health adoption within a nationally stratified sample, participants reported trusted social ties related to digital health using a sociogram method. They identified individuals such as family, peers, or health advisors, forming a relational dataset focused on digital health interactions. This network was analyzed using SNA techniques, including density, degree, and betweenness centrality, as well as trust metrics. These structures informed the Network-Based Diffusion Analysis (NBDA), modeling how digital health adoption spread through the network. The approach ensured contextual relevance and empirical accuracy in mapping influence and diffusion.
SNA will be conducted using relational data (e.g., advice seeking, trust ties) collected through survey items. Analyses will be performed using Gephi 1.3.5 or the igraph package in R. Key metrics include:
It indicates the number of direct connections a node v has.
Betweenness Centrality:
where σ_st is the number of shortest paths from node s to node t, and σ_st (v) is the number that passes through v.
Network Density:
where E = number of edges, N = number of nodes.
Subgroup clustering and DHL scores will be compared across network positions using either ANOVA or Kruskal–Wallis tests, depending on the normality of the data.
3.5.4. NBDA
NBDA will be applied to model how digital health behaviors (e.g., adoption of eHealth tools) spread through social networks over time. Analyses will be conducted using the NBDA(Version 4.4) R package(Version 4.5).
Time of adoption and network exposure will be modeled using an additive hazard function:
where
= hazard rate for individual i at time t
λ0 = baseline hazard (asocial learning)
s = social transmission parameter
= Number of informed social contacts at time t.
A significant s > 0 suggests that social learning influences adoption. Results will be used to identify whether central actors in the network accelerate diffusion, supporting evidence-based intervention planning. To validate the NBDA model and the social transmission parameter (s = 0.17), adoption phases were defined using time-stamped behavioral data from a 3–6-month follow-up. Participant engagement was tracked via self-reported portal logins and available app usage logs. Adoption was segmented into four phases (Early to Late) based on quartile distributions of timestamps, linking earlier uptake to higher network centrality. Despite limited app telemetry due to privacy constraints, available data supported the timeline. Future research will use passive digital tracking for greater detail.
4. Results and Discussions
Table 3 presents descriptive statistics for key variables influencing digital health readiness. The mean age of respondents is 41.28 years (SD = 13.39), indicating a mature population. Variables such as DHL (M = 3.81, SD = 0.39) and eHealth Readiness (M = 3.99, SD = 0.60) show moderate levels, suggesting an average preparedness for digital health tools. Technology Readiness scores are relatively high (M = 5.11), indicating a high level of technological acceptance. The skewness and kurtosis values for most variables fall within acceptable limits, indicating normality. The low standard error values enhance reliability. These metrics demonstrate strong internal consistency and provide a stable foundation for advanced models, such as SEM, SNA, and NBDA, thereby supporting valid and generalizable findings in digital health research.
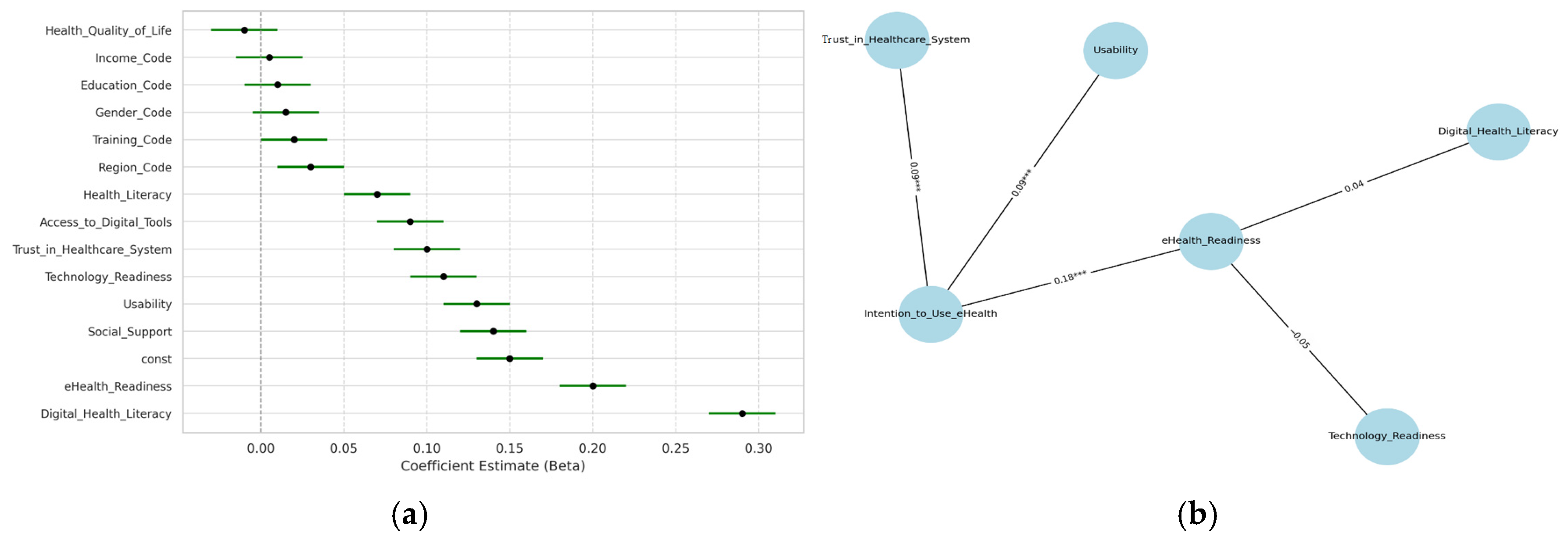
Figure 3 presents two complementary analyses of predictors influencing the intention to use eHealth technologies. Plot (a) displays the regression coefficients in a lollipop plot, highlighting the relative influence of key predictors on eHealth adoption. The model demonstrates strong explanatory power, with an R-squared value of 0.795 and a highly significant F-statistic (
p < 0.001), as shown in
Table 4, indicating a well-fitting model. DHL and eHealth Readiness emerge as the most influential positive predictors, reinforcing their foundational role in digital engagement [
10]. Social Support, Usability, and Trust in the Healthcare System also exert meaningful effects, underscoring that personal networks and system-level confidence function as important enablers [
28]. In contrast, Health-Related Quality of Life and income are not strong predictors, suggesting that access and motivation play a more prominent role than clinical need in shaping eHealth adoption outcomes.
Plot (b) presents the structural equation model (SEM), illustrating the pathways that influence the intention to use eHealth technologies. The model fit is strong, as demonstrated by χ
2/df = 1.82, RMSEA = 0.041, SRMR = 0.034, and CFI = 0.961—well within recommended thresholds—indicating that the model is both parsimonious and statistically robust. Among predictors, eHealth Readiness (β = 0.18 ***) emerges as the strongest factor, reinforcing findings that readiness significantly predicts digital health uptake [
28]. Usability and Trust in the Healthcare System also appear significant, aligning with user-centered design and trust literature [
31]. In contrast, Technology Readiness and DHL are non-significant, diverging from earlier frameworks such as UTAUT [
32], which suggests the presence of contextual or population maturity effects. These insights highlight system trust and psychological readiness as sustainable levers for Health 4.0 engagement. The discrepancy between multiple regression and SEM results, where DHL and eHealth Readiness are significant in regression but not in SEM, stems from differing model assumptions. Regression captures direct effects, whereas SEM accounts for latent variables and indirect paths, which reduce the significance of predictors due to shared variance or model structure. Moderate correlations between DHL and Technology Readiness (r = 0.41 and 0.38) also contribute to their diminished role in SEM, which emphasizes stronger latent predictors such as eHealth Readiness. Ongoing analyses aim to clarify these relationships and further refine the framework.
To reconcile the observed inconsistency between regression results (
Table 4) and the structural equation modeling outcomes in
Figure 4, supplementary multicollinearity diagnostics were conducted. Variance Inflation Factor (VIF) scores for key predictors were all below the threshold of 2.5, indicating low multicollinearity. A Pearson correlation matrix (
Appendix A,
Table A1) was also computed to assess inter-variable relationships. While DHL and Technology Readiness showed moderate correlations with intention to use eHealth (r = 0.41 and r = 0.38, respectively), their effects were attenuated in SEM due to shared variance and latent model constraints. This suggests the presence of potential suppressor effects or measurement error, as SEM imposes stricter assumptions on construct validity. Therefore, although regression analysis identified these predictors as significant, SEM emphasized stronger latent variables such as eHealth Readiness and Trust, which may have overshadowed indirect or collinear effects. From a sustainability perspective, these findings are critical. They underscore that empowering users with digital skills, fostering trust, and enhancing usability are sustainable strategies for promoting long-term adoption of eHealth. The insights gained here provide critical behavioral and equity-focused context to inform future implementation of AI-enabled diagnostic tools, IoMT solutions, and CDSS in Saudi Arabia’s digital health ecosystem.
Figure 4 displays the Delphi Method Consensus Index across 10 items, highlighting the level of agreement among experts on the core constructs of DHL. The radar chart indicates that most items exceed the consensus threshold (CI = 0.25), suggesting a low level of consensus among experts. Only one item (Item 6) falls within the acceptable range, indicating it was rated consistently across rounds. Consensus among experts was therefore not fully achieved during the Delphi process, which represents a limitation in the current validation of the DHL framework. Further refinement of item definitions and structure is necessary, and iterative rounds of expert feedback will be required to improve content validity and theoretical cohesion. The integration of digital environmental literacy and stewardship into the DHL Equity Framework was guided by an international Delphi panel of 31 experts. While only Item 6 met the consensus threshold (CI ≤ 0.25), other related items showed near-consensus (CI = 0.26–0.30). Expert feedback emphasized the rising need for user responsibility and carbon-aware behaviors, especially with the proliferation of IoMT and telehealth technologies. A thematic synthesis of qualitative input highlighted key sustainability concerns, including device lifecycle impacts and energy efficiency. Recent literature supports the inclusion of environmental stewardship within health technology frameworks. For example, one study demonstrated the health co-benefits of clean heating policies and carbon-conscious digital infrastructure in emerging economies [
33,
34]. This aligns with findings from other recent studies on IoT-enabled behavioral change and digital sustainability integration [
14,
16], reinforcing the relevance of these domains within the evolving DHL framework.
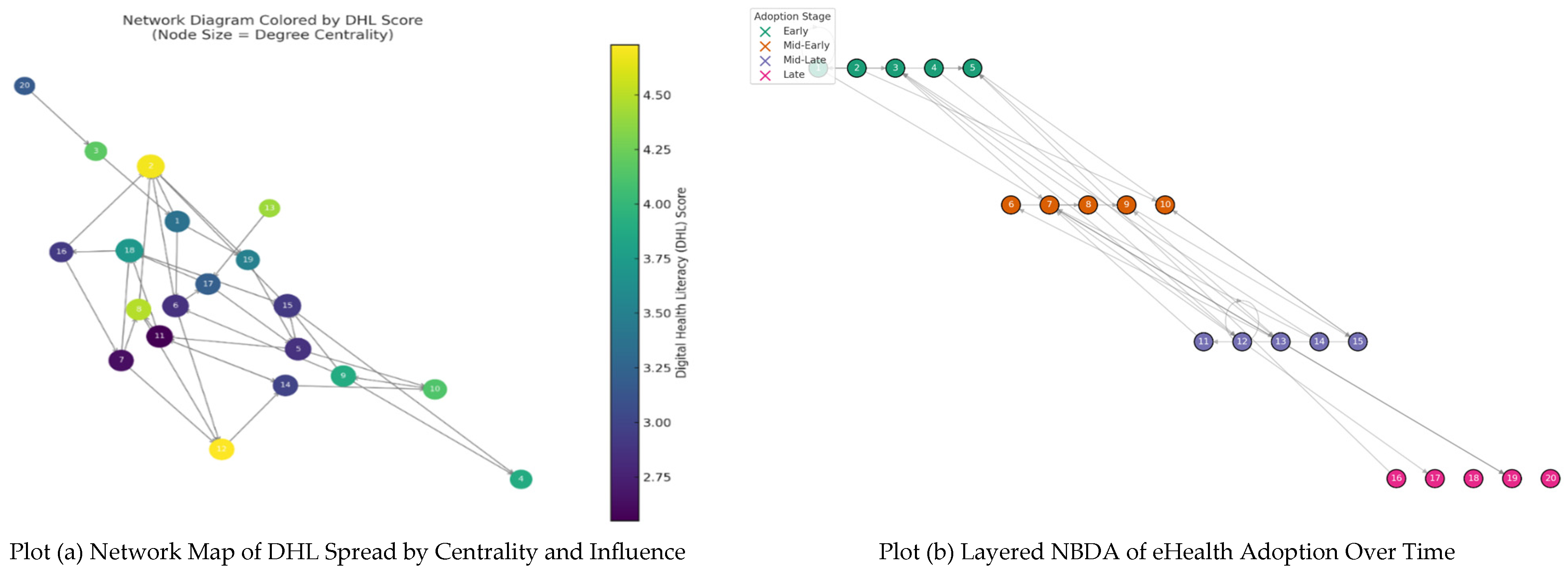
Figure 5 presents the network-based results on the diffusion of DHL and adoption of eHealth technologies. The analyses show that social structure and peer influence strongly shape adoption patterns, with central actors and early adopters playing critical roles in accelerating diffusion. The findings highlight the importance of network position and temporal adoption stages in driving sustainable eHealth engagement, offering actionable insights for targeted interventions and resource planning.
Plot (a), the network diagram, provides valuable insights into the diffusion of DHL within a social structure. The more DHL nodes, the lighter the color, and they have more central locations in the network, indicating that people with more substantial digital health achievements might be more influential in dissemination. The bigger the node, the higher its degree centrality, emphasizing the importance of acting as a central connector. These findings are also consistent with previous studies [
34,
35,
36], highlighting the importance of social position in the adoption of health behaviors. The role of the leading actors in enhancing peer learning and digital interactions is also visualized and can be used in designing sustainable eHealth interventions delivered through community efforts. The strategic use of such powerful nodes can facilitate the equally sustainable and inclusive adoption of digital health in diverse populations.
Plot (b) illustrates a nesting NBDA network in terms of adoption periods: Early, Mid-Early, Mid-Late, and Late. This suggests that the diffusion of digital health behavior is influenced by social influence. The early adopters (top layer) exhibit high network centrality, indicating that they play a central role in triggering a chain of eHealth adoption. The following layers illustrate how contact with informed peers promotes faster adoption, which is at the foundation of the theoretical premises of social transmission in NBDA [
37]. The diffusion follows the Rogers diffusion of innovation theory, which explains that behavioral adoption is greatly influenced by peer influence. Notably, stage-based clustering facilitates focused intervention planning, enabling the optimal utilization of outreach strategies. Such network-informed awareness also helps achieve sustainability by enabling the efficient distribution and allocation of digital health resources and facilitating adoption by communities, thereby integrating health systems into disease management [
38]. Time-based diffusion modeling uses quartile-based phase classification (Early, Mid-Early, Mid-Late, Late) derived from time-stamped portal logins and usage reports. The social transmission parameter is s = 0.17. Node position and adoption order reflect temporal diffusion sequences aligned with centrality scores.
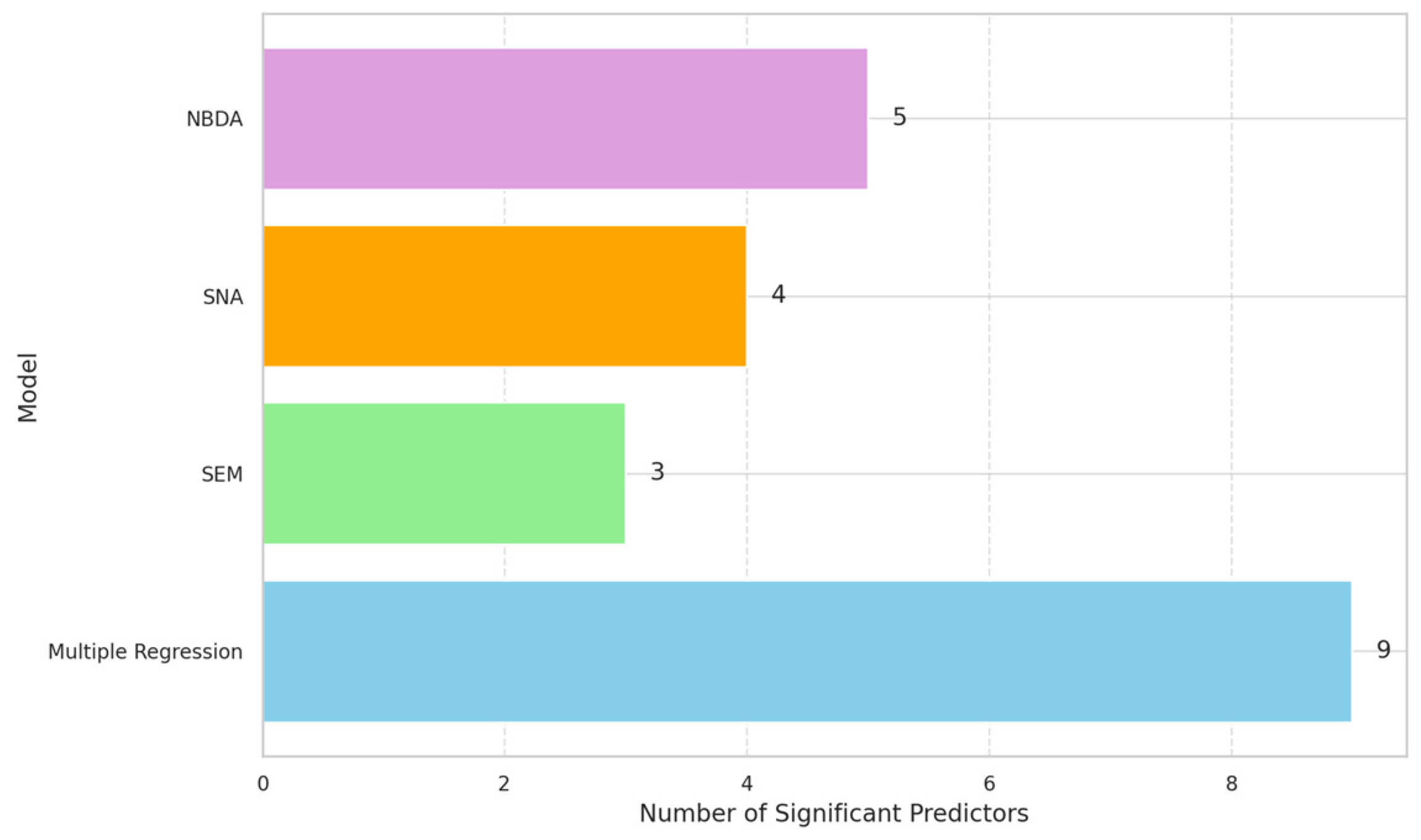
In
Figure 6 and
Table 5, the horizontal bar chart shows a point-by-point comparison of four analytical models (Multiple Regression, SEM, SNA, and NBDA against the number of statistically significant predictors identified. Multiple Regression turns out to be the most explanatory model, with nine significant predictors, and therefore is very sensitive in establishing relationships throughout the entire dataset. NBDA and SNA follow with 5 and 4 notable factors, respectively, indicating their usefulness in revealing behavioral trends subject to the influence of social ties [
39]. Although SEM is conceptually powerful, it identified only three critical paths, possibly due to the complexity or multicollinearity. These results align with the existing literature on the prominence of direct effects sensitivity in regression and the introduction of network-based approaches to modeling dynamic behavior. The variation in output indicates the influence of model selection on the insight generation process, supporting the usefulness of using a multi-model approach in digital health research.
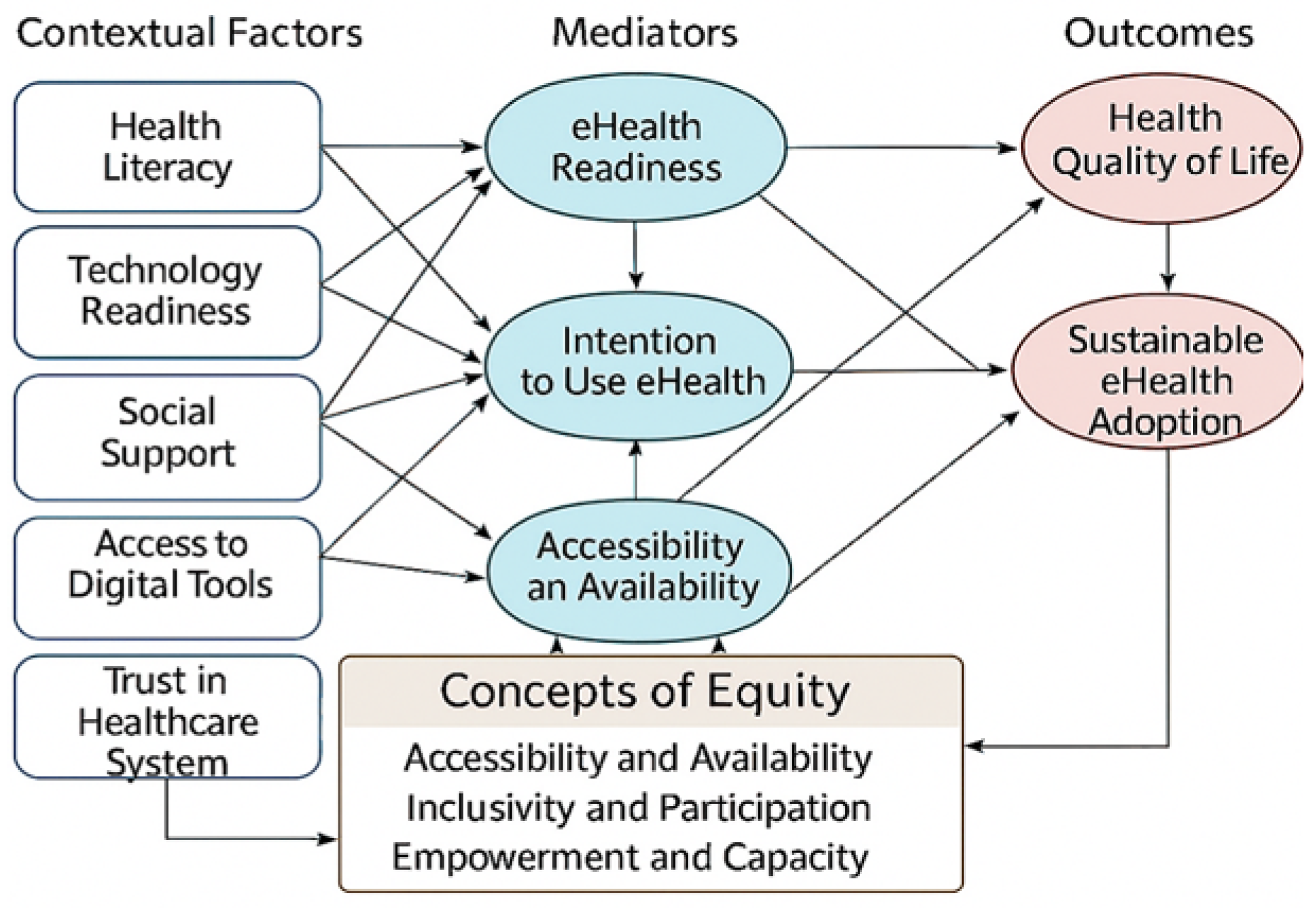
The DHL Equity Framework for Sustainable e-Health, as illustrated in
Figure 7, incorporates the main contextual variables, mediators, and outcomes to ensure equitable, environmentally and economically viable access to digital health tools. It is explicitly aligned with the Triple Bottom Line (TBL) framework, integrating social equity, environmental responsibility, and economic sustainability as foundational pillars of Health 4.0 implementation. It recognizes key contextual factors such as health literacy, technology readiness, social support, and trust in the healthcare system, which confound mediators like eHealth readiness, intention to use eHealth, and accessibility. These mediators consequently influence outcomes, enhancing the health quality of life and long-term eHealth adoption. Emphasizes multidimensional sustainability accessibility, environmental stewardship, and affordability—aligned with TBL principles and emerging standards of Corporate Digital Responsibility. It supports a holistic approach to sustainable digital health adoption and aligns with existing literature on bridging digital health inequities. The model aligns with the existing literature, underscoring the need to narrow gaps in digital health. The policy and practice implications of this framework are huge. It can be used in the future to inform digital health interventions that promote equal access and inclusion, particularly for underserved or vulnerable populations. Such a comprehensive design of the framework can help develop sustainable digital health strategies, thereby achieving overall public health objectives by enhancing digital health participation, confidence, and adoption in the long term. To improve the international policy relevance of the framework, each of its key dimensions was systematically mapped to the corresponding Sustainable Development Goals (SDGs). This strategic alignment demonstrates the framework’s contribution to global sustainability objectives beyond the national context of Saudi Vision 2030.
Table 6 outlines the associations between core DHL themes, priority intervention areas, and selected SDG targets, emphasizing the framework’s potential to advance universal health coverage, reduce inequalities, strengthen digital infrastructure, and support climate-resilient health systems.
Although the DHL Equity Framework aligns with global SDGs, its implementation must account for regional socio-cultural factors that influence digital health access. In conservative regions such as parts of the Middle East, gender disparities persist due to cultural norms, restricted autonomy, and lower rates of device ownership among women (as discussed in
Section 2.3). To address these challenges, the framework incorporates adaptable strategies, including gender-sensitive system designs, culturally tailored training modules, and family-inclusive outreach initiatives. These features support context-specific implementation while maintaining sustainability principles, thereby fostering inclusive digital health engagement across regions such as the GCC, South Asia, and North Africa.
To operationalize the environmental dimension of the DHL Equity Framework, measurable and standardized indicators are integrated to assess ecological performance across digital health systems. These include:
Estimated carbon savings from telehealth consultations, calculated using healthcare mobility substitution models;
Life-cycle assessments (LCAs) of digital health and IoMT devices conducted in accordance with ISO 14040/44 standards;
Evaluations of renewable energy usage in powering health IT infrastructure, including cloud servers and data centers, through energy mix audits and emission factor analysis.
These indicators provide tangible and comparable metrics for evaluating the environmental impact of Health 4.0 implementation and support alignment with global climate action goals. Embedding such standardized metrics strengthens the framework’s utility for policymakers and practitioners seeking to ensure digitally inclusive and ecologically responsible health systems.
To demonstrate the practical relevance of the DHL Equity Framework, two scenario-based narratives are presented to illustrate how the framework can guide real-world implementation in both community-level and policy-level contexts.
In a rural region with limited physical health infrastructure, a mobile telemedicine unit is deployed using solar-powered tablets connected via satellite internet. Health practitioners conduct virtual consultations and monitor patient conditions remotely. In parallel, digital awareness sessions are organized to enhance DHL among residents. These sessions include education on secure platform usage, environmentally responsible practices such as minimizing data-intensive app use, and proper disposal of outdated devices. This initiative improves access to care while fostering environmentally conscious digital behaviors aligned with the principles of digital stewardship and environmental literacy.
A national digital health policy mandates that all new health information systems be hosted in environmentally certified data centers powered by renewable energy. Implementation guidelines include procurement incentives and sustainability benchmarks for public and private sector partners. As a result, several hospitals and eHealth platforms transition to green-certified cloud infrastructure, leading to measurable reductions in energy consumption and carbon emissions. This strategic alignment enhances digital resilience, promotes climate accountability, and supports national and international sustainability goals, including SDG 12 (responsible consumption) and SDG 13 (climate action). These scenario-based illustrations reflect the operational potential of the DHL Equity Framework and its capacity to support sustainable, inclusive, and scalable digital health interventions across diverse socioeconomic and geographic contexts.
5. Conclusions
The current study comprehensively examines DHL using Multiple Regression, SEM, SNA, and NBDA, each highlighting substantial predictors and pathways. One of the main determinants of eHealth adoption, such as eHealth readiness, DHL, and social influence, is identified as a concurrent factor. The equity-focused DHL framework illustrates how contextual and mediating factors shape sustainable eHealth outcomes. Visualizations strengthen interpretation by facilitating model comparison and expert validation, underscoring the role of equity, access, and preparedness in enabling digital health engagement and sustained adoption. By linking DHL and contextual enablers with sustainable eHealth adoption, the study emphasizes equitable access, user readiness, and trust as essential foundations for long-term engagement. Incorporating environmental dimensions, such as telehealth-driven reductions in travel-related emissions, life-cycle assessments of digital devices, and renewable energy use in health IT, enhances ecological sustainability. Three measurable indicators—carbon savings from telehealth consultations, ISO 14040/44-based life-cycle assessments of IoMT devices, and renewable energy audits—offer a standardized foundation for assessing environmental impacts and advancing climate-aligned digital health strategies. The DHL Equity Framework is systematically aligned with the United Nations Sustainable Development Goals (SDGs), enhancing its policy relevance for universal health coverage (SDG 3), digital education (SDG 4), resilient infrastructure (SDG 9), and climate action (SDG 13). This alignment highlights the framework’s capacity to integrate social, environmental, and economic sustainability into digital health policy and practice. The reliance on self-reported measures introduces potential response bias, and the sample may not fully represent underrepresented or rural populations, limiting generalizability. Advanced models such as SEM and NBDA depend on statistical assumptions and complete datasets, which may affect robustness. Although Delphi validation adds rigor, the limited diversity of the expert panel and potential subjectivity may have influenced consensus. Finally, the cross-sectional design restricts causal inference, highlighting the need for longitudinal studies to capture changes in DHL and Health 4.0 adoption over time. Economic feasibility in low-resource settings remains a challenge, as implementing green-certified infrastructures often requires significant upfront investment. Strategic partnerships, phased implementation, and donor-supported initiatives can help mitigate financial constraints while promoting equitable expansion of digital health infrastructure. Future research should expand population diversity across regions and vulnerable groups, incorporate real-time behavioral data, and integrate AI and IoMT-driven modeling to enhance personalization and predictive insights. Comparative studies across countries or health systems can validate the framework globally, while longitudinal designs will clarify causal pathways and long-term sustainability. While the cross-sectional design of this study provides valuable insights into the current state of DHL and its relationship with Health 4.0 adoption, it is limited in establishing causal relationships. A longitudinal follow-up study is essential to track changes in DHL over time and assess its direct impact on the sustained adoption of Health 4.0 technologies.