Abstract
Healthcare supply chain management operates amid fluctuating patient demand, rapidly advancing biotechnologies, and unpredictable supply disruptions pose high risks and create an imperative for sustainable resource optimization. This study investigates the underlying mechanisms through which digital intelligence drives strategic decision optimization in healthcare supply chains. Drawing on the Resource-Based View and Dynamic Capabilities Theory, we develop a chain-mediated model, defined as the multistage indirect path whereby digital intelligence first bolsters innovation capability, which then activates supply chain resilience (absorptive, response, and restorative capability), to improve decision optimization. Data were collected from 360 managerial-level respondents working in healthcare supply chain organizations in China, and the proposed model was tested using structural equation modeling. The results indicate that digital intelligence enhances innovation capability, which in turn activates all three dimensions of resilience, producing a synergistic effect that promotes sustained decision optimization. However, the direct effect of digital intelligence on decision optimization was not statistically significant, suggesting that its impact is primarily mediated through organizational capabilities, particularly supply chain resilience. Practically, the findings suggest that in the process of deploying digital intelligence systems and platforms, healthcare organizations should embed technological advantages into organizational processes, emergency response mechanisms, and collaborative operations, so that digitalization moves beyond the technical system level and is truly internalized as organizational innovation capability and resilience, thereby leading to sustained improvement in decision-making performance.
1. Introduction
With the continuous increase in healthcare service demand, accelerated population aging, and frequent public health emergencies, healthcare supply systems are under unprecedented pressure. On the one hand, the global demand for pharmaceuticals and medical services continues to grow rapidly, placing increasing pressure on resource allocation and supply efficiency [1]. According to the IQVIA Institute [2], global medicine usage rose by 14% over the past five years and is projected to grow another 12% by 2028, with China leading in both consumption volume and expenditure. On the other hand, population aging and the rising prevalence of chronic diseases have driven a long-term and diversified demand for healthcare services. By 2040, individuals aged 60 and above are expected to account for 28% of China’s population [3], with a sharp increase in patients requiring long-term treatment for diabetes, cardiovascular conditions, and other chronic illnesses. These developments have accelerated the integration of digital healthcare services such as telemedicine, e-prescriptions, and online pharmaceutical distribution into existing healthcare systems [4]. As noted by Srivastava et al. [5], the Healthcare Supply Chain (HSC) is a dynamic system involving multiple stakeholders, complex processes, and high risks, encompassing the entire flow of critical resources such as pharmaceuticals, medical devices, and consumables from raw material procurement to the end user. Systematic review studies have consistently shown that digital technologies such as artificial intelligence (AI), blockchain, and big data analytics can enhance data-driven decision-making, rapid response mechanisms, and resource allocation efficiency within supply chains, particularly in hospital operations, pharmaceutical distribution, and emergency medical resource assurance [6,7].
Accordingly, to address the rapidly growing demand for healthcare products and services, healthcare supply systems must undergo Digital Intelligence (DI) driven transformation. Unlike the mere adoption of general digital tools, DI refers to the integration, sensing, intelligent processing, and platform-based coordination of digital technologies across supply chain functions, leading to a fundamental improvement in managerial models and capability structures. In the pharmaceutical and healthcare context, DI typically manifests through the integration of smart digital technologies with enterprise systems such as Enterprise Resource Planning (ERP), Manufacturing Execution Systems (MESs), Warehouse Management Systems (WMSs), Electronic Health Records (EHRs), and Hospital Information Systems (HISs). These integrations enable end-to-end process digitalization and data interoperability, facilitating intelligent analytics and optimal decision-making at each organizational node [8,9,10,11].
In the HSC, Innovation Capability (IC) is indispensable for deepening and broadening the application of digital technologies, serving as a critical driver for platform collaboration, smart operations, and Decision Optimization (DO) [12]. Today, emerging models such as personalized medicine, smart healthcare, remote services, and precision medicine are reshaping patient-centered service delivery. HSCs are evolving beyond traditional drug logistics and inventory systems into collaborative networks that integrate hospitals, pharmaceutical manufacturers, digital platforms, and end users [6]. Digital technologies including AI, predictive analytics, smart inventory control, and multi-stakeholder collaboration platforms, are playing a pivotal role in enhancing responsiveness, operational efficiency, and patient satisfaction [13,14]. Mittal and Mantri [15] highlight that HSCs have evolved into dynamic network systems centered on patient needs, grounded in cross-organizational collaboration, and supported by digital tools. Therefore, viewing DI as an advanced technical resource and IC as a dynamic organizational competence, this study adopts the Resource-Based View (RBV) as a macro-theoretical framework to construct a chain-based logic of ‘technical resources → organizational capabilities → decision performance’ within HSCs [16].
Moreover, the outbreak of COVID-19 revealed the structural vulnerabilities of traditional supply chains and underscored the critical importance of resilience in healthcare systems. The ability to sense disruptions, respond rapidly, and recover systematically has become a fundamental requirement for the sustainable performance of HSCs [7,17]. To further address environmental uncertainty, this study introduces Dynamic Capabilities Theory (DCT) to investigate how healthcare organizations can adapt to external changes and make optimal decisions by enhancing Supply Chain Resilience (SCR), specifically Absorptive Capabilities (AC), Response Capabilities (RPC), and Restorative Capabilities (RTC) [18].
Therefore, this study develops a theoretical framework by integrating the RBV and the DCT. RBV emphasizes the strategic value of firm-specific resources in achieving competitive advantage, with DI conceptualized as a high-potential strategic resource. DCT explains how firms absorb, reconfigure, and dynamically deploy such resources under environmental uncertainty to develop adaptive organizational capabilities, IC, and SCR. Building on this perspective, this study proposes that DI influences DO in the HSC indirectly and profoundly through the capability-building pathways of IC and SCR.
Several previous studies have investigated the application of individual technologies such as AI or blockchain in HSCs [19,20,21], while others have conducted broader reviews on the DI transformation of supply chains [22,23,24]. While these studies demonstrate the potential of digital technologies to enhance supply chain decision-making and performance, several limitations remain. First, many lack robust theoretical support and fail to integrate multiple theoretical perspectives. Second, the research context is often overly broad, with limited focus on the specific characteristics and constraints of healthcare supply chains. Third, empirical studies tend to simplify the mechanisms of influence, overlooking the complex interrelationships among multidimensional variables. Therefore, unlike prior studies that enhance decision accuracy through standalone IT solutions or improve supply system performance via operations research methods [25], this study takes an operational perspective to explore the mechanisms driving decision optimization in HSCs. Grounded in RBV and DCT, and contextualized within the demand volatility and service complexity characteristic of healthcare, this research is the first to explore a parallel and sequential mediation mechanism composed of IC and the three dimensions of SCR (AC, RPC, and RTC). It aims to reveal how digital technology resources can be transformed into DO advantages through the collaborative functioning of organizational capabilities. By investigating how DI enhances organizational learning, innovation, and dynamic responsiveness, this study provides a new perspective on the deep-level impact of digital transformation on HSC management.
In summary, to address the current lack of system-level integration and the unclear mechanism pathways in the digital transformation of HSCs, this study aims to develop a theory-driven analytical framework that systematically explores how DI enhances DO through the mediating roles of IC and SCR. On the one hand, this research integrates the RBV, which frames DI as a firm-specific strategic resource that drives IC, and DCT, which emphasizes an organization’s capacity to sense, seize, and reconfigure competences to build SCR. This integration directly uncovers how these theoretical lenses explain the sequential mediating pathways through which digital resources translate into optimized strategic decision outcomes in HSCs. On the other hand, the study provides empirical evidence and practical guidance for healthcare organizations to strengthen resilient operations and improve decision-making efficiency under conditions of high uncertainty.
This study aims to explore the key drivers influencing DO in the HSC, with the goal of providing both theoretical support and practical guidance for the sustainable development of the healthcare industry. The structure of the study is as follows. Section 2 provides a comprehensive review of the relevant literature on DI, IC, and SCR, including AC, RPC, and RTC, as well as DO, and identifies the theoretical foundation and knowledge gaps addressed in this study. Section 3 presents the conceptual model and research hypotheses, along with a detailed explanation of the research methodology, variable development, and measurement approach. Section 4 reports the empirical findings based on Structural Equation Modeling (SEM) and interprets the statistical significance of the results. Section 5 discusses the research outcomes, highlights the theoretical and practical implications, outlines the study’s limitations, and proposes directions for future research.
2. Literature Review
2.1. Digital Intelligence
With the continuous penetration of advanced digital technologies such as AI, big data analytics, and the Internet of Things (IoT), digital transformation has become a critical force in reshaping core organizational capabilities and promoting high-quality development [26]. In the context of HSCs, digital transformation is regarded as a systemic innovation process driven by data, aiming to optimize resource allocation, enhance service effectiveness, and ensure medical quality [27]. In this transformation, organizations urgently need to build intelligent systems capable of sensing, analyzing, learning, and forecasting to cope with highly uncertain external environments.
Among the various technological attributes encompassed by digital transformation, DI has increasingly drawn scholarly attention due to its deep impact on supply chain responsiveness and decision-making capabilities [28]. DI primarily relies on advanced technologies such as AI, machine learning, and big data analytics to restructure supply chain processes through intelligent sensing, intelligent analysis, and intelligent decision-making. Empirical studies have shown that intelligent algorithms can significantly improve the efficiency of key supply chain functions, such as route optimization, demand forecasting, and inventory scheduling in healthcare systems [29,30]. In practice, the integration of AI with Vendor Managed Inventory (VMI) systems has enhanced information flow between hospitals and pharmaceutical firms, enabling automated replenishment and data visualization [31], while AI-based platforms have improved order responsiveness and production planning accuracy in pharmaceutical enterprises [32].
However, existing research largely treats DI as a technical tool, lacking structured modeling and theoretical interpretation of its role as an independent variable. In particular, studies exploring how DI influences strategic decision-making through organizational capability pathways in the HSC context remain scarce. For example, in pharmaceutical supply chain management, AI has bolstered inventory management capabilities by enabling timely and accurate capture of patient demand fluctuations, thereby mitigating stockouts and distribution disruptions and enhancing decision-making foresight, agility, and efficiency [33,34]. To address this gap, this study conceptualizes DI as a key driving force that reflects a digital system’s capacity for autonomous cognition, intelligent analysis, and data-driven decision-making.
2.2. Innovation Capability
IC in HSC management is widely recognized as a critical driver for organizations to gain competitive advantage in dynamic environments. It encompasses not only the adoption of emerging technologies, but also process optimization, service model restructuring, and rapid responsiveness to external changes [35]. From various theoretical perspectives, IC can be further specified as follows: from the perspective of technological resource integration, it reflects an organization’s ability to identify, absorb, and deploy advanced digital technologies such as AI, blockchain, and the IoT to support efficient coordination and service execution [36]. From the perspective of process redesign, it involves continuous improvement of operational mechanisms, reduction of redundancies, and enhancement of system flexibility [37]. From the service model restructuring lens, IC enables the transformation of traditional linear supply models into patient-centered, multi-point coordinated intelligent networks [38].
Additionally, the synergistic accumulation of organizational learning, data-driven capabilities, and cross-functional integration is considered a core component of IC [39], while dynamic responsiveness to environmental disruptions also entails the reconfiguration of processes and strategic plans [40]. Overall, IC is not only essential for the deep application of digital technologies, but also serves as a driving force for platform-based coordination, smart operations, and DO in HSCs [12].
Despite this, studies have applied the RBV to examine the role of AI capabilities in promoting product innovation [41]; some studies have drawn on DCT to investigate how DI transformation affects firm performance via IC [42]; and some studies have leveraged information processing theory and dynamic capabilities perspectives to explore the moderating role of open innovation between AI technologies and SCR [43]. However, existing research has not yet sufficiently examined how IC functions as a dynamic organizational capability that mediates the relationship between DI and DO via SCR. To address this gap, the present study incorporates IC as a core mediating variable to explore its role in converting DI into strategic value, thereby extending theoretical insights into capability building and performance enhancement in HSC management.
2.3. Supply Chain Resilience
In contemporary supply chain research, resilience is widely defined as an organization’s ability to maintain core functions and rapidly recover in the face of external disruptions [44]. Zhao et al. [45] further conceptualize resilience as a dynamic process encompassing AC, RPC, and RTC, highlighting the full cycle of sensing, reacting, and rebuilding in turbulent environments. Building on this, Senna et al. [46] propose a systemic framework in which resilience in HSCs is not merely reactive, but represents a structured, multi-layered, and dynamic set of capabilities embedded within a cyclical mechanism linking antecedents, mediators, and outcomes.
In the healthcare context, the ongoing disruptions caused by pandemics, large-scale disasters, and population aging necessitate supply chains that are capable of rapid adaptation, diversified responses, and effective recovery [47]. In response, recent studies have begun integrating DCT into resilience research, emphasizing the relevance of sensing, seizing, and reconfiguring mechanisms in uncertain environments [18]. Specifically, AC corresponds to the sensing dimension, emphasizing an organization’s ability to identify, acquire, and internalize external signals of risk and change, thereby serving as the foundational layer of resilience [48]. RPC aligns with the seizing mechanism, highlighting the judgment, decision-making, and resource allocation processes that enable organizations to act effectively during disruptions, functioning as the intermediate layer of the resilience mechanism [49]. RTC reflects the reconfiguring dimension, focusing on the recovery, repair, and upgrading of system processes and competencies after disruption, which represents the final stage in sustaining long-term resilience and post-crisis optimization [13]. This mapping not only clarifies the internal structure of SCR but also provides a theoretical foundation for constructing the subsequent mediation effects and causal pathways in this study.
Although some studies have highlighted the positive roles of agility, adaptability, and flexibility in mitigating supply chain disruptions [50], the integration mechanism between SCR and DCT remains underexplored, particularly from the perspective of the dynamic and complex environment of healthcare supply systems. To address this gap, the present study adopts a DCT informed approach and constructs a three-dimensional structure of AC, RPC, and RTC as mediating variables, aiming to systematically assess how resilience bridges the relationship between DI and DO in complex HSCs.
2.3.1. Absorptive Capability
AC is commonly defined as an organization’s ability to sense, identify, and integrate external information, early-warning signals, and potential disruptions in the pre-disruption phase [51]. Zhao et al. [45] identify AC as a critical starting point for resilient operations, enabling supply chains to detect disturbance sources and proactively consolidate relevant information resources at an early stage. In an empirical study of emerging economies, Tortorella et al. [52] emphasize that, in the context of healthcare, AC also reflects the system’s sensitivity to heterogeneous and multi-source data, such as pandemic forecasts, fluctuations in patient demand, and policy shifts, which indicates its predictive and preemptive capacity.
Wright et al. [53] argue that establishing preemptive mechanisms for information perception and integration enhances the HSC’s ability to anticipate crises and avoid delayed responses. In addition, Kumar et al. [54] highlight that AC relies heavily on the support of AI, big data, and other digital technologies, which accelerate information sensing and improve data processing quality, thereby creating an intelligent link between information and decision-making.
Although its preemptive role in resilience management has been widely recognized, the conceptual boundaries, operational mechanisms, and quantitative measurement of AC in HSCs remain underdeveloped. Therefore, this study defines AC as the ability of an organization to integrate, recognize, and internalize heterogeneous information from multiple sources prior to disruptions. It emphasizes its core role in forecasting, early warning, and risk prevention, and conceptualizes it as the first stage dimension of SCR.
2.3.2. Response Capability
Unlike AC, which emphasizes the identification and anticipation of risks before disruptions occur, RPC focuses on an organization’s ability to rapidly mobilize critical resources and make effective decisions during the occurrence of disruptions [55]. This capability is reflected in how quickly identified risk signals are translated into concrete actions such as activating alternative routes, adjusting inventory strategies, and reallocating resources in a timely and efficient manner [56].
In healthcare systems, the response window to disruptions is extremely narrow. In time-sensitive areas such as vaccine distribution, emergency drug delivery, and surgical supply provision, response efficiency is directly linked to patient safety and continuity of care [46]. Developing such capability requires not only refined internal process management but also support from digital technologies such as AI and machine learning, which enable real-time feedback, rapid scenario modeling, and intelligent path optimization [54]. Tortorella et al. [52], in their study of emerging economies, found that healthcare institutions with standardized, platform-based, and modularized response systems are better equipped to translate disruption signals into swift operational actions.
However, most existing studies treat resilience as a single aggregated construct, overlooking the phase-specific nature and structured mechanisms of RPC within supply chain disruption scenarios. Therefore, this study conceptualizes RPC as the operational competence of healthcare organizations to respond immediately, mobilize resources, and implement strategic actions at the point of disruption. It is positioned as the second stage dimension of the SCR mechanism and is empirically examined in the proposed research model.
2.3.3. Restorative Capability
RTC refers to an organization’s ability to effectively reorganize resources, rebuild disrupted processes, restructure operational systems, and even regenerate capabilities following a supply chain disruption, thereby enabling the system to return to its original or an even more optimal state [57]. It represents the final and most decisive stage of SCR, determining whether the system can fully recover or even achieve post-disruption performance improvement [58].
From the perspective of dynamic capabilities, RTC is essentially the strategic integration and reconstruction of prior absorptive and response efforts. It reflects not only operational recovery but also the organization’s transformative capacity for structural renewal and capability realignment [59]. Healthcare organizations with strong RTC can resume essential services, optimize critical nodes, and maximize operational efficiency even under resource constraints [60]. In complex, multi-stakeholder HSCs operating in dynamic environments, restoration also requires cross-system coordination of economic, environmental, and social resources to ensure a stable and efficient restart, which is vital for the long-term sustainability of pharmaceutical and medical operations [61].
However, in the context of HSC management, how digital technologies can enhance organizational coordination and resource reconfiguration during the recovery stage remains an underexplored area. Therefore, this study further investigates RTC as a critical component of resilience and empirically examines its mediating role in the digital transformation DO pathway.
2.4. Decision Optimization
DO in the HSC has increasingly emerged as a central focus for ensuring operational efficiency, service safety, and long-term sustainability [62]. As a multidimensional process, DO involves comprehensive coordination across various supply chain stages, including resource procurement, inventory allocation, and patient end service delivery [63,64].
With the accelerated integration of AI into healthcare systems, DO is evolving beyond static, rule-based models. It now entails the dynamic configuration of decision paths and resource structures, based on multi-source data and advanced analytics. Emerging technologies, particularly large language models (LLMs), support semantic interpretation, trend forecasting, and complex judgment, thus improving the quality and agility of strategic decisions [65,66].
To further explore the internal mechanisms through which HSCs achieve optimized decision-making, this study adopts the RBV to address how organizations can build efficient and intelligent decision systems based on internal resources, in response to increasing complexity and frequent external disruptions in HSCs [67]. RBV posits that sustained competitive advantage stems from the possession of core resources that are rare, inimitable, and deeply embedded within organizational processes [68]. In the context of supply chain management, RBV has been widely employed to explain how firms leverage key resources, such as technology, processes, and information, to develop unique operational capabilities that lead to superior performance outcomes [16]. Guided by RBV, this study constructs a theoretical framework grounded in the logic of technological resources → organizational capabilities → decision performance. DI is conceptualized as a core strategic resource within healthcare organizations, whose value is realized through the development of two critical capabilities: IC and SCR [69]. Accordingly, this study proposes a pathway of influence from DI to decision optimization, mediated sequentially by IC and resilience, to explain how technical resources are transformed into sustainable decision-making advantages.
However, existing research remains primarily focused on static reasoning, with limited exploration of how decision-making structures operate in dynamic environments shaped by AI, edge computing, and platform governance. Therefore, this study defines DO as a context adaptive mechanism that combines technological intelligence, dynamic organizational capabilities, and resource reconfiguration to support strategic decision-making. This conceptualization is further tested through empirical investigation.
2.5. Summary of Existing Studies and Research Gap
To further clarify the positioning of this study within the existing literature, a systematic review of recent representative studies was conducted, covering their theoretical foundations, research contexts, key findings, and identified limitations in Table 1. This table not only helps elucidate the theoretical underpinnings and empirical content of prior research, but also highlights existing gaps regarding chain mediation mechanisms, the dimensional construction of SCR, and the contextual applicability to HSCs. These insights provide a solid foundation for the development of this study’s research model and hypothesis formulation.

Table 1.
Summary of existing studies and research gaps.
In summary, prior research has yielded substantial insights into how digital technologies such as AI, blockchain, and the IoT enable supply chain management, drawing upon a variety of theoretical lenses including the RBV, Dynamic Resource-Based View (DRBV), DOI, Context Intervention Mechanism Outcome (CIMO), Multi-Criteria Decision Making (MCDM), and Organizational Information Processing Theory (OIPT). These studies have explored the links between digital capabilities, resilience mechanisms, and operational performance. However, several research gaps remain. First, existing studies predominantly focus on single technologies (e.g., blockchain, AI, IoT) or isolated mechanisms (e.g., resilience, visibility), lacking a comprehensive framework that conceptualizes DI as an integrated, multidimensional construct with explanatory power. Second, limited attention has been given to the sequential mechanism through which digital technologies via IC activate the three dimensions of SCR (AC, RPC, and RTC) and ultimately contribute to DO. Third, although the HSC has increasingly attracted scholarly attention, empirical studies grounded in the Chinese context remain scarce. To address these gaps, this study adopts a multi-theoretical perspective and proposes a chain mediation model linking DI → IC → SCR → DO. Using empirical data from the Chinese HSC sector, this study systematically examines how digital transformation facilitates DO under dynamic environments, thereby enriching the theoretical depth and practical value of digital supply chain research.
3. Hypotheses Development and Research Methodology
3.1. Research Hypotheses
To articulate the comprehensive logic of our model, we propose nine sets of interrelated hypotheses. First, we posit that DI exerts a positive influence on DO (H1), IC (H2), and each dimension of SCR including AC, RPC, and RTC (H3-1, H3-2, H3-3). Second, we anticipate that IC further enhances DO (H4) and drives each resilience dimension (H5-1, H5-2, H5-3). Third, we expect that AC, RPC, and RTC each contribute positively to DO (H6-1, H6-2, H6-3). Finally, we examine how IC and resilience mediate DI’s effects on DO in parallel (H7, H8-1, H8-2, H8-3) and sequentially through innovation and each resilience dimension (H9-1, H9-2, H9-3).
3.1.1. Digital Intelligence and Decision Optimization
In the highly uncertain environment of healthcare, organizations are required to make high-quality decisions that balance real-time responsiveness, efficient resource allocation, and patient satisfaction [27,78]. As a key technological attribute of digital transformation, DI refers to the organization’s ability to leverage AI, big data analytics, and machine learning to enable predictive analysis, route optimization, and intelligent decision-making [79]. Particularly in the context of HSCs, organizations must navigate complex trade-offs among compliance, safety, and timely delivery, necessitating a highly structured decision system that relies on advanced information processing and cross-functional coordination [80]. The integration of intelligent technologies allows healthcare organizations to identify risk signals, simulate intervention strategies, and rapidly generate optimal decision paths, especially in areas such as inventory allocation, demand forecasting, and service flow management [81]. From the perspective of the RBV, DI represents a distinctive and inimitable strategic resource that enhances the agility, precision, and sustainability of decision-making systems [67,82]. Therefore, this study proposes the following hypothesis:
H1.
Digital Intelligence has a positive effect on Decision Optimization.
3.1.2. Digital Intelligence and Innovation Capability
The intelligent attributes of digital technologies and organizational innovation capabilities are increasingly becoming key drivers of transformation in the HSC. Through DI, healthcare organizations are able to collect, share, and integrate data more effectively, which in turn facilitates knowledge creation, accelerates cross-departmental integration, and supports new product development, process optimization, organizational restructuring, as well as the development of novel services and business models suited to complex medical environments [83,84,85]. For example, the deployment of the IoT and RFID technologies across the supply chain enables real-time collection of product data from production through transportation to final delivery. These data are then securely shared among all stakeholders via cloud storage and blockchain platforms, promoting cross-functional collaboration. Big data analytics and AI tools further refine and integrate these vast datasets, allowing precise product development and optimized production allocation in response to market demand [86,87]. In particular, the embedded application of AI within healthcare networks demonstrates strong cross-organizational innovation potential, especially in terms of knowledge integration, process coordination, and service automation [88,89]. For instance, AI can assist in diagnostic interpretation in oncology, accelerate drug discovery, and enable personalized patient care pathways [90]. Empirical findings by Belhadi et al. [59] further indicate that under highly dynamic supply chain conditions, AI-driven innovation mechanisms significantly enhance organizational innovation performance. Therefore, this study proposes the following hypothesis:
H2.
Digital Intelligence has a positive effect on Innovation Capability.
3.1.3. Digital Intelligence and Supply Chain Resilience
Resilience capability, defined as a process-based capacity comprising absorptive, response, and restorative functions, requires the integrated support of digital technologies, organizational resources, and structural mechanisms [49]. Among various digital transformation features, DI provides healthcare organizations with enriched information flows, more efficient resource allocation methods, and accelerated task execution mechanisms, thereby enabling dynamic adaptability [45,52]. DI enhances AC by enabling proactive and predictive mechanisms. Through AI and big data analytics, healthcare organizations can detect abnormal patterns in large-scale datasets, helping decision makers identify potential sources of disruption and forecast future risks or demand fluctuations. This allows a shift from passive information reception to proactive early-warning systems [91]. For example, omnichannel healthcare platforms supported by big data and AI technologies integrate online consultations, e-prescriptions, online medicine ordering, and payment settlement services to build an end-to-end, fully traceable pharmaceutical distribution network. Through AI-driven data integration and analysis, manufacturers and suppliers can swiftly detect market demand fluctuations, thereby enhancing the AC of HSC resilience [92]. Regarding RPC, digital intelligent systems facilitate rapid scenario analysis, identify resource bottlenecks and task priorities, and enable route optimization, resource reallocation, and automatic task initiation via intelligent algorithms, significantly improving real-time responsiveness [29,93]. For example, during the COVID-19 vaccine rollout, AI-driven predictive models integrated with real-time IoT and RFID data enabled health authorities to forecast regional demand spikes, optimize cold-chain logistics routes through dynamic routing algorithms, and automatically trigger replenishment orders to vaccination sites [94]. Finally, DI empowers RTC by enabling organizations to self-repair and reconfigure operations. AI-based systems can predict recovery bottlenecks based on failure points and dynamically optimize recovery paths, thereby enhancing the efficiency of system reconstruction and the quality of service resumption [79]. For example, following a major healthcare supply disruption, an AI-driven digital twin leveraged reinforcement learning algorithms to analyze past interruption events and autonomously generate optimized recovery workflows, such as reprioritizing orders, adjusting batch sizes, and reallocating transport resources. Through this self-learning process of reengineering, the system significantly improved post-disruption service levels [49]. Therefore, this study proposes the following hypotheses:
H3-1.
Digital Intelligence has a positive effect on Absorptive Capability.
H3-2.
Digital Intelligence has a positive effect on Response Capability.
H3-3.
Digital Intelligence has a positive effect on Restorative Capability.
3.1.4. Innovation Capability and Decision Optimization
IC is considered a critical enabler for strategic and intelligent decision-making. Organizations with strong innovation capabilities are better positioned to leverage advanced digital technologies, optimize operational structures, and develop adaptive decision frameworks [95]. IC fosters the integration of new technologies into decision processes, enabling real-time data utilization, predictive modeling, and scenario planning [82]. Moreover, innovation serves as a mediating mechanism that translates digital and big data competencies into enhanced strategic decisions and sustainable outcomes [96]. Kumar & Raj [97] further emphasize that IC strengthens supply chain performance by bridging data capabilities and DO, particularly through enhanced supply chain integration and resilience. Therefore, this study proposes the following hypothesis:
H4.
Innovation Capability has a positive effect on Decision Optimization.
3.1.5. Innovation Capability and Supply Chain Resilience
Although SCR can enhance an organization’s ability to adapt and recover, without sufficient support from IC, its role may be limited to passive defense rather than proactive optimization [76]. IC enables the transformative application of digital technologies within HSCs, allowing organizations to more effectively absorb external information, respond to disruptions, and reconfigure service processes, thus facilitating a shift from risk response to system evolution [7].
First, IC enhances AC by fostering agile learning mechanisms and cross-boundary information integration. Tetteh et al. [98] noted that innovation-oriented healthcare organizations can leverage data analytics and knowledge recombination to increase sensitivity to potential risks and improve the efficiency of information absorption. Second, IC strengthens the structural flexibility of RPC by supporting process modularization, platform-based collaboration, and algorithmic optimization. Fernando et al. [99] emphasized that technological IC is a critical enabler for rapid adjustment and efficient resource allocation, especially in multi-organizational responses to sudden disruptions. Finally, innovation facilitates RTC by enabling organizations to implement structural optimization and system reconfiguration following a crisis, allowing not only a return to the previous state but also the achievement of superior performance [80]. Therefore, this study proposes the following hypotheses:
H5-1.
Innovation Capability has a positive effect on Absorptive Capability.
H5-2.
Innovation Capability has a positive effect on Response Capability.
H5-3.
Innovation Capability has a positive effect on Restorative Capability.
3.1.6. Supply Chain Resilience and Decision Optimization
Resilience capability in the HSC refers to an integrative process capability constructed through embedded workflows, sensing systems, and feedback mechanisms, which collectively support timely, precise, and coordinated decision-making [69]. First, AC acts as a precondition for DO by enabling risk perception, data assimilation, and early warning, which help organizations form accurate cognitive assessments in the face of uncertainty or volatility [100]. Second, RPC determines the feasibility of organizational decisions. From the perspective of decentralized decision-making, strong responsiveness allows for rapid command deployment and real-time resource reallocation [101]. In the healthcare context, explainable AI enhances decision transparency and controllability, improves inventory turnover, and prevents resource mismatch [102]. Finally, RTC reflects the organization’s ability to recover from disruptions, serving as a foundation for decision system stability and continuity [103]. As shown by Vega et al. [104], recovery capability influences how swiftly an organization can learn from interruptions, repair processes, and optimize its decision structure. Therefore, this study proposes the following hypotheses:
H6-1.
Absorptive Capability has a positive effect on Decision Optimization.
H6-2.
Response Capability has a positive effect on Decision Optimization.
H6-3.
Restorative Capability has a positive effect on Decision Optimization.
3.1.7. The Mediated Effects of Innovation Capability and Supply Chain Resilience
In the highly dynamic context of HSCs, DI, enabled by technologies such as AI and big data analytics, empowers organizations to develop systematic capabilities for data sensing, analysis, and intelligent judgment. This forms a critical foundation for the development of innovation mechanisms and the activation of SCR [83,88]. Recent research in the context of Industry 4.0 emphasizes the strategic role of digital technologies in fostering process innovation as a key enabler of supply chain performance. For instance, Qureshi et al. [105] demonstrate that the integration of advanced technologies such as the IoT, AI, and automation not only improves operational efficiency but also stimulates innovation in processes, workflows, and organizational routines. These innovation-driven transformations strengthen the firm’s adaptive capacity and decision rationality. IC plays a pivotal role in amplifying the positive effects of resilience mechanisms, enabling organizations to engage in process redesign, system reconfiguration, and service innovation in response to external disruptions or resource adjustments. These innovation-driven actions contribute to more rational, efficient, and sustainable decision-making processes [92,106].
First, DI-driven IC strengthens the value realization of AC. Innovation mechanisms improve the efficiency of information filtering, knowledge transformation, and solution generation, allowing resilience systems to more effectively convert external inputs into strategic decisions. As Belhadi et al. [59] observed, in AI-assisted environments, highly innovative organizations are more capable of transforming data insights into forward-looking strategies, thereby improving predictive accuracy and decision quality in pharmaceutical supply chains. Second, IC enhances the operational flexibility of RPC. When resilience mechanisms trigger emergency responses, innovation facilitates the development of modular processes and platform-based coordination mechanisms. These innovations support algorithmic modeling and task synchronization based on DI systems, improving the feasibility and effectiveness of crisis response decision-making. Finally, the real-time feedback and simulation functions provided by DI technologies require IC to enable process restart, recovery, and structural optimization. Through innovation, organizations can reconfigure operations in a way that not only restores but also improves upon pre-crisis performance [76].
In summary, in the healthcare sector, supply system disruptions, drug shortages, and policy shifts are commonplace, so the effectiveness of DI technologies in driving proactive DO depends on an organization’s innovation mechanisms and resilient adaptive capacities [107]. By integrating the IoT connectivity, AI-driven analytics, and cloud platforms, DI fortifies innovation mechanisms that improve the efficiency of information filtering and knowledge conversion under demand volatility, thereby amplifying AC and enabling proactive strategy formulation [108]. Intelligent digital capabilities, such as AI and predictive algorithms, can then merge with existing operations in innovation-oriented healthcare organizations to establish knowledge-driven rapid response mechanisms, yielding more rational, efficient, and sustainable decision outcomes. For example, intelligent algorithms can map infectious disease transmission pathways and swiftly trigger targeted supply and service deployments [109]. Finally, the use of digital twin simulations and automated feedback loops as innovation-driven reengineering tools supports self-learning and self-restorative processes, guiding rapid operational recovery and reconstructing supply chain workflows, which enhances RTC and enables decision pathways that outperform prior system states [110].
Therefore, DI activates IC, which in turn enhances the three sequential stages of resilience, AC, RPC, and RTC to jointly form an intelligence-driven pathway for organizational adaptation and DO. Therefore, this study proposes the following hypotheses:
H7.
Innovation Capability mediates the relationship between Digital Intelligence and Decision Optimization.
H8-1.
Absorptive Capability mediates the relationship between Digital Intelligence and Decision Optimization.
H8-2.
Response Capability mediates the relationship between Digital Intelligence and Decision Optimization.
H8-3.
Restorative Capability mediates the relationship between Digital Intelligence and Decision Optimization.
H9-1.
Innovation Capability and Absorptive Capability sequentially mediate the relationship between Digital Intelligence and Decision Optimization.
H9-2.
Innovation Capability and Response Capability sequentially mediate the relationship between Digital Intelligence and Decision Optimization.
H9-3.
Innovation Capability and Restorative Capability sequentially mediate the relationship between Digital Intelligence and Decision Optimization.
3.2. Research Model
This study develops a conceptual model and research hypotheses based on the RBV and DCT. The RBV provides a foundational theoretical lens for understanding how firms formulate strategic decisions to achieve sustainable competitive advantage [111]. In particular, for HSC systems undergoing digital transformation, it is essential to leverage internal digital technology resources in conjunction with the dynamic capabilities framework to enhance organizational processes [112]. By enabling supply chain innovation through digital technologies, organizations can enhance their SCR to effectively respond to external changes [18]. This process ultimately supports optimal decision-making, strengthens organizational competitiveness, and contributes to sustainable performance in HSC [113,114]. Therefore, this study proposes a research model in which intelligence, derived from digital transformation, serves as the independent variable. Its impact on DO, the dependent variable, is examined through the mediating roles of supply chain IC and SCR. The latter is conceptualized as consisting of AC, RPC, and RTC. The full model is presented in Figure 1.
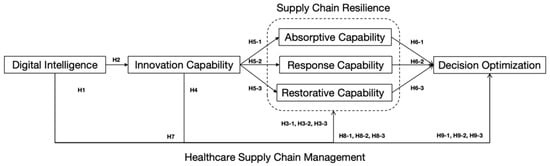
Figure 1.
Research model.
3.3. Measurement
Based on the theoretical model and hypotheses proposed in this study, a structured questionnaire was designed. All measurement items were adapted from well-established and validated scales in prior literature. Five items were used to measure each of the core constructs DI, IC, and DO while three items were assigned to each of the mediating variables: AC, RPC, and RTC. The full list of measurement items is presented in Table 2. A 5 Likert scale was adopted for all items [114], capturing participants’ level of agreement with each statement, ranging from 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, to 5 = strongly agree.

Table 2.
Variable measurement.
3.4. Demographics
This study targeted managerial-level respondents within organizations that constitute the HSC in China. The DI HSC is defined as one in which pharmaceutical or healthcare-related organizations have integrated one or more advanced digital technologies into their supply chain operations to enhance data-driven decision-making, system connectivity, and adaptive responsiveness. Specifically, qualifying digital technologies include: (1) integrated information systems, such as ERP, WMSs, and Transportation Management Systems (TMSs); (2) the IoT and sensor technologies for temperature control in cold chains, product tracking, and real-time inventory monitoring; (3) AI and advanced analytics for demand forecasting, intelligent replenishment, and emergency scenario simulation; (4) blockchain and traceability technologies for ensuring the integrity and authenticity of pharmaceutical data; and (5) mobile and visualization platforms for cross-organizational coordination, status monitoring, and real-time feedback [115,116]. Data were collected through an online survey using the platform wjx.cn, employing a random sampling method. The survey was conducted over a five-month period, from 7 October 2024, to 7 March 2025. A total of 381 questionnaires were collected. After removing 21 invalid responses due to missing or illogical information, 360 valid responses were retained, resulting in an effective response rate of 94.48%. General demographic characteristics of the respondents are presented in Table 3. Among the respondents, 69.2% were aged under 35, and 29.4% were aged between 35 and 50, indicating that most participants were young or mid-level managers within HSC organizations. This age group is typically characterized by being energetic and open to adopting new technologies and ideas, although their managerial experience may be relatively limited. In terms of education, 62.2% of the respondents held a bachelor’s degree, 15% held a master’s degree, and 8.1% had obtained a doctoral degree. Meanwhile, only 14.7% had an associate degree. These figures indicate that although the sample primarily consisted of middle-aged and younger professionals, the overall educational level of the respondents was generally above average. Regarding work experience, 54.4% of respondents had less than 5 years of experience, 37.8% had 5 to 15 years, and 7.8% had over 15 years, representing junior, mid-level, and senior managers, respectively. The distribution of managerial experience aligns with the age profile of the respondents, as most participants were under the age of 50, and their management experience typically fell within the 15-year range. As for the annual revenue of the respondents’ organizations, 54.7% were from small enterprises (less than CNY 40 million), 31.4% from medium-sized enterprises (CNY 40 million to 400 million), and 13.9% from large enterprises (over CNY 400 million). In terms of ownership type, 61.9% of the enterprises were domestic, 31.1% were Sino-foreign joint ventures, and 6.9% were wholly foreign-owned enterprises.

Table 3.
Demographic characteristics of the respondents.
4. Data Analysis and Results
4.1. Exploratory Factor Analysis
Exploratory factor analysis (EFA) was conducted using SPSS 26.0, and the results are presented in Table 4. To assess the suitability of the data for factor analysis, the Kaiser–Meyer–Olkin (KMO) measure and Bartlett’s test of sphericity were performed. The KMO value for this study was 0.914. According to Kaiser and Rice [117], a KMO value close to 1 indicates strong correlations among variables and a high degree of factorability; values above 0.9 suggest that the data are “marvelous” for factor analysis. Bartlett’s test yielded a Chi-square value of 6574.182 with 276 degrees of freedom, and the result was statistically significant (p < 0.001), indicating the presence of common factors among the items and supporting the appropriateness of conducting factor analysis [118]. In the HSC context, characterized by complex and interrelated latent constructs such as DI, IC, SCR, and DO, these results specifically confirm that the measured items share substantial common variance and sufficient inter-item correlations. This ensures that the EFA solution reliably captures meaningful underlying structures, thus enhancing the methodological rigor and validity of this analysis. Using the principal component analysis method, the cumulative variance explained by the extracted factors was 76.565%, exceeding the commonly accepted threshold of 50% [119], indicating a high level of explanatory power. The Varimax rotation was applied, and the rotated component matrix showed that all factor loadings had absolute values above 0.60, indicating good convergent validity between the items and their corresponding factors [120]. Additionally, the Cronbach’s alpha coefficients for each construct exceeded 0.80, meeting the criteria for excellent to good internal consistency [121], demonstrating that the measurement scales have high reliability. The high Cronbach’s alpha values obtained indicate strong internal consistency among measurement items for each specific construct, DI, IC, SCR, and DO, thus verifying that the selected scales reliably capture the intended theoretical dimensions and provide stable measurements within the HSC context.

Table 4.
Exploratory factor analysis results.
4.2. Confirmatory Factor Analysis
Confirmatory factor analysis (CFA) was conducted using AMOS 24.0 to evaluate the consistency between the latent constructs and their corresponding measurement items, and to verify the validity of the measurement scales. The results are presented in Table 5. All constructs demonstrated Composite Reliability (CR) values greater than 0.80 and Average Variance Extracted (AVE) values above 0.50. According to conventional criteria (CR > 0.70; AVE > 0.50), these findings indicate good convergent validity [122]. Additionally, all standardized factor loadings exceeded 0.70, suggesting strong associations between each latent construct and its observed indicators. Model fit indices were also satisfactory, with Chi-square/df = 1.737 (<3), GFI = 0.916, AGFI = 0.893, NFI = 0.939, RFI = 0.929, IFI = 0.973, TLI = 0.969, and CFI = 0.973. Most indices were close to or exceeded the recommended threshold of 0.90, indicating a good overall model fit and a well-structured measurement model. Specifically, the incremental fit indices including GFI, IFI, TLI, and CFI, all exceeded the recommended threshold of 0.90, indicating that the proposed theoretical model offers a substantial improvement over the baseline model and demonstrates strong explanatory power. Furthermore, the Chi-square/df ratio was below 3, and the RMSEA value was below 0.08, suggesting that the model achieves an acceptable level of absolute fit, with minimal discrepancy between the hypothesized structure and the observed data. The high values of GFI and AGFI further confirm the structural coherence and adequacy of the model. Collectively, these favorable fit statistics confirm that the measurement model aligns closely with the empirical data, thereby reinforcing the reliability and validity of the latent constructs. More importantly, the robustness of the model structure provides a solid methodological foundation for subsequent structural path analysis, enhancing the credibility and scientific rigor of the study’s hypothesis testing and conclusions.

Table 5.
Confirmatory factor analysis results.
4.3. Correlation Analysis
Pearson correlation analysis was conducted using SPSS 26.0, and the results are presented in Table 6. According to the classification proposed by Schober et al. [123], the absolute magnitude of the observed correlation coefficients can be interpreted as follows: 0.90~1.00 = very strong, 0.70~0.89 = strong, 0.40~0.69 = moderate, 0.10~0.39 = weak, and 0.00~0.10 = negligible correlation. The results of this study indicated that the correlation coefficients among variables ranged from 0.307 to 0.613 and were all statistically significant at the 0.01 level (p < 0.01), suggesting significant positive correlations among the key constructs. In addition, the results of the discriminant validity test showed that the square roots of the AVEs for all constructs were greater than the absolute values of the interconstruct correlations, indicating that the measurement model possesses satisfactory discriminant validity.

Table 6.
Descriptive statistics and bivariate correlations results.
4.4. Path Analysis
Path analysis was conducted using AMOS 24.0, and the results are presented in Table 7 [124]. The effect of DI on DO was not statistically significant (β = 0.132, p > 0.05); thus, Hypothesis H1 was rejected. DI had a significant positive effect on IC (β = 0.308, p < 0.001), supporting Hypothesis H2. In addition, DI had significant positive effects on all three resilience capabilities: AC (β = 0.482, p < 0.001), supporting H3-1; RPC (β = 0.538, p < 0.001), supporting H3-2; and RTC (β = 0.518, p < 0.001), supporting H3-3. However, IC had a significant negative effect on DO (β = −0.420, p < 0.001); thus, H4 was rejected. IC positively influenced AC (β = 0.314, p < 0.001), supporting H5-1; RPC (β = 0.362, p < 0.001), supporting H5-2; and RTC (β = 0.417, p < 0.001), supporting H5-3. All three resilience capabilities showed significant positive effects on DO (β = 0.351, p < 0.001), supporting H6-1; RPC (β = 0.341, p < 0.001), supporting H6-2; and RTC (β = 0.666, p < 0.001), supporting H6-3.

Table 7.
Path analysis results.
4.5. Test of Mediating Effect
Mediation analysis was conducted using AMOS 24.0 with 5000 bootstrap samples, and the results are presented in Table 8. The total effect of DI on DO was found to be significantly positive (p < 0.001), while the direct effect was not statistically significant (p > 0.05). In contrast, the indirect effect was significantly positive (p < 0.001), indicating that IC and SCR function as full mediators in the relationship between DI and DO. Specifically, the indirect effect of DI → IC → DO was significantly negative (p < 0.001); thus, Hypothesis H7 was rejected. Meanwhile, the indirect effects of DI → AC → DO, DI → RPC → DO, and DI → RTC → DO were all significant (p < 0.001), supporting Hypotheses H8-1, H8-2, and H8-3, respectively. Furthermore, the results of the serial mediation analysis revealed that the three paths DI → IC → AC → DO, DI → IC → RPC → DO, DI → IC → RTC → DO were also statistically significant (p < 0.001), thereby supporting Hypotheses H9-1, H9-2, and H9-3 [125].

Table 8.
Mediating effect test results.
5. Discussion
5.1. Conclusions
To deepen the understanding of how strategic DO can be achieved in the context of DI-driven transformation of HSCs, this study empirically tested the causal relationships among DI, IC, SCR (AC, RPC, and RTC), and DO using SEM.
First, the path analysis results indicate that DI does not exert a statistically significant direct effect on DO in HSCs, and Hypothesis H1 is rejected. This finding contrasts with those of Senapati et al. [126] and Ivanov et al. [67]. One plausible explanation is that digital technologies, when implemented as isolated tools without deep integration into management processes, may fail to directly enhance decision performance. As Tiwari et al. [127] argue, digital infrastructure must be effectively aligned with network operations and process management to foster system autonomy and generate strategic advantages such as resilience, coordination, and efficiency. The results of the mediation analysis in this study further support this view. This also responds to a growing academic recognition that the ‘technology → performance’ pathway requires deeper theoretical interpretation. While previous studies primarily evaluated the direct impact of technology usage behaviors on performance outcomes, this study focuses on the value generated when DI technologies are integrated, absorbed, reconfigured, and embedded into organizational operations [126]. This reflects a capability-oriented pathway more consistent with the logic of the RBV and DCT, rather than a simplistic linear assumption that ‘technology equals value’.
DI was found to have a significant direct positive effect on both IC and SCR, supporting hypotheses H2, H3-1, H3-2, and H3-3, consistent with findings by Apell & Eriksson [84] and Abourokbah et al. [83]. The findings validate the RBV-based partial framework in which technological resources drive organizational capabilities, confirming that DI in HSCs can indeed function as a strategic resource that enhances IC and strengthens SCR.
However, in contrast to Al-Surmi et al. [82], this study reveals that IC has a significant negative effect on DO, and Hypothesis H4 is rejected. A potential explanation lies in the fact that innovation in intelligent systems often entails high initial investment and operational complexity, which may hinder internal collaboration and decision efficiency in the short term [80]. The value of IC can only be fully realized when supported by resilience capabilities; organizations lacking sufficient absorptive and restorative mechanisms may struggle to accommodate the process changes and cognitive shifts introduced by innovation. This is further corroborated by the mediation analysis, which suggests that in the absence of adequate resilience mechanisms, innovation may act as a disruptive force rather than an enabling one.
In addition, the study confirms that IC positively influences all three dimensions of resilience (AC, RPC, and RTC), supporting Hypotheses H5-1, H5-2, and H5-3, which aligns with the findings of Mehmood et al. [76] and Adana et al. [101]. The empirical results suggest that sustained IC within the supply chain system provides critical support and momentum for resilience, enabling organizations to better withstand environmental changes and external risks. Moreover, each of the three resilience dimensions was shown to significantly enhance DO, supporting Hypotheses H6-1, H6-2, and H6-3, and aligning with the findings of Vega et al. [104] and Revilla et al. [69]. These results confirm that the three-dimensional structure of SCR, grounded in DCT, can collectively facilitate DO in HSC systems.
Secondly, the mediation analysis results reveal that, consistent with the findings of Junaid et al. [106], SCR (AC, RPC, and RTC) plays a full mediating role between DI and DO in HSCs. This supports Hypotheses H8-1, H8-2, and H8-3, and further confirms the applicability of the RBV-based pathway of digital resources → organizational capabilities → decision performance in HSC management. Furthermore, the chain mediation formed by IC and SCR (AC, RPC, and RTC) also shows a full mediating effect between DI and DO, supporting Hypotheses H9-1, H9-2, and H9-3, and aligning with the findings of Belhadi et al. [59] and Zhang et al. [128]. The empirical results suggest that in HSCs with DI, IC and SCR function as two distinct yet synergistic organizational trends that jointly facilitate the continuous optimization of decision-making.
Notably, however, IC exhibits a significant negative full mediation effect between DI and DO, leading to the rejection of Hypothesis H7, which contradicts the findings of Jum’a et al. [96]. This raises the possibility that a non-linear mechanism, such as a U-shaped mediation or moderation effect, may exist in this relationship [129]. In the early stages, low levels of IC, characterized by underdeveloped platform integration and insufficient information sharing, may disrupt supply chain coordination and diminish decision efficiency. However, as IC matures and collaborative mechanisms improve, it may strengthen the adaptive responsiveness of the resilience system and enhance intelligent decision-making support, ultimately leading to substantial improvements in decision performance [130]. The effectiveness of IC in supporting decision optimization may depend not only on its maturity but also on its dynamic alignment with resilience capabilities. That is, the degree of coupling between innovation and resilience mechanisms. Without sufficient absorptive and restorative mechanisms, even high IC may lead to misaligned objectives or overcomplexity [92].
5.2. Theoretical Contribution
This study establishes a theoretical foundation for future research on digital intelligent transformation in HSCs, grounded in an integrated perspective of the RBV and DCT. It deepens the theoretical understanding of how DI influences supply chain DO, contributing significantly to theoretical development within this domain.
Firstly, this research systematically integrates RBV and DCT within the context of digital intelligent transformation in HSC management. Previous studies predominantly emphasized the technological dimension, lacking theoretical and empirical exploration of how resources translate into capabilities, and how capabilities support strategic decision-making. Due to inherent complexities, demand uncertainty, and high risk characteristics, HSCs require a dual theoretical perspective involving strategic resource identification and dynamic capability construction. By integrating RBV and DCT, this study theoretically clarifies how healthcare organizations leverage DI as a strategic resource, transforming it through dynamic pathways involving IC and SCR into strategic advantages for DO.
Secondly, this research develops a novel structured path analysis framework by conducting a refined three-dimensional structural decomposition (AC, RPC, and RTC) of HSC resilience. Furthermore, it proposes a chain-mediated mechanism between IC and SCR. This mechanism specifies that digital technological resources, when encountering environmental disruptions and resource constraints, do not operate in isolation. Instead, they require the activation of internal organizational innovation mechanisms and dynamic responsiveness via resilience mechanisms to systematically enhance resource allocation efficiency, risk management, and strategic decision-making capability. Consequently, this study provides a fresh theoretical perspective and solid foundation for future fine-grained theoretical construction and multi-level research in supply chain management.
5.3. Practical Implications
This study provides forward-looking and practical managerial implications for achieving the sustainable and healthy development of HSCs in the context of DI transformation.
First, this study empirically validates a theoretical framework grounded in the RBV and DCT, which illustrates how DI resources can drive IC and coordinate dynamic SCR to DO. In the process of implementing DI initiatives, HSCs must consider not only the adoption of smart technologies but also their integration with platform systems, which serve as the operational foundation for enhancing organizational capabilities, particularly innovation and resilience. For upstream HSC stakeholders such as pharmaceutical manufacturers, it is essential to complement technologies like the IoT, AI, and blockchain with enterprise-level platforms such as ERP, MESs, and WMSs. This integration strengthens traceability, supports interdepartmental collaboration, streamlines development processes, and enhances drug safety across the product lifecycle [131]. For midstream logistics and distribution providers, decision timeliness can be enhanced by adopting blockchain-based drug traceability platforms and IoT-enabled status tracking systems for visualization [132], alongside real-time inventory management systems, robotic process automation (RPA), and intelligent scheduling tools. These solutions are particularly suitable for managing urgent logistics, vaccine distribution, and high-turnover inventory items [133,134]. For downstream actors such as hospital pharmacies, the deployment of AI-based predictive analytics, machine learning decision support systems, EHRs, HISs, demand forecasting models, and intelligent replenishment tools is especially critical in managing chronic medications, personalized prescriptions, and remote drug delivery [135]. Nevertheless, the deployment of DI technologies still faces several challenges, including high upfront investment requirements, shortages of skilled technical personnel, and uneven development levels across emerging economies. To address these issues, it is recommended to adopt dynamic assessment frameworks such as the Digital Maturity Model proposed by The Lancet and other authoritative medical publications. This model can guide pharmaceutical producers, distributors, and platform-based service providers in evaluating and advancing their digital capabilities at different stages [136].
Second, strengthening organizational capabilities in HSCs should not be limited to the allocation and integration of DI system resources. It is equally important to embed these technological advantages into organizational workflows, emergency response mechanisms, and inter-organizational collaboration processes, thereby internalizing them into actionable resilience, decision power, and execution capability. In practice, this necessitates the enhancement of process mechanisms. Hospitals, pharmaceutical firms, and logistics providers should collaboratively establish early-warning systems that consolidate anomaly signals across HIS, ERP, and TMS platforms via standardized application programming interfaces (APIs), enabling real-time data collection and integration [46,137]. Furthermore, contingency plans for redundant pharmaceutical resources should be prearranged, with established agreements involving alternative suppliers, third-party logistics providers, and emergency inventory facilities [138]. These measures transform the HSC from a static, linear structure into a dynamic and elastic network, enabling organizational agility and enhancing the system’s overall resilience and recovery capabilities. However, the implementation of DI technologies for organizational coordination is not without risk. Concerns such as data privacy breaches, cybersecurity threats, and internal resistance must be addressed. Accordingly, appropriate policy-level governance is essential. For instance, China’s HSCs, particularly in the pharmaceutical sector, should establish a phased and tiered digital transformation roadmap. This roadmap should define the pace and priorities of process reengineering, system deployment, and capability development across different organizational types, thereby improving structural efficiency [139]. Through such multi-level and collaborative advancement, China’s pharmaceutical supply chain can realize systemic improvement and continuous optimization of operational decision-making amid digital transformation.
Finally, this study also contributes to the sustainable management of HSCs by clarifying how the DI → IC → SCR → DO mechanism enhances both resilience and long-term adaptability. While resilience emphasizes recovery and robustness, sustainability underscores inclusiveness, adaptability, and responsible resource allocation. For example, AI-enabled inventory optimization and intelligent scheduling can reduce drug waste and energy consumption in logistics. Integrated early-warning systems and cross-platform collaboration promote equitable access to medications during emergencies [140]. Moreover, embedding resilience into the digital transformation process facilitates sustainable procurement practices, circular supply systems, and real-time transparency across the pharmaceutical lifecycle. These outcomes align closely with global health objectives by ensuring availability, accessibility, and affordability, particularly in under-resourced and marginalized regions [141]. Thus, the findings of this study not only advance the resilience and efficiency of HSCs, but also offer strategic insights into balancing DI with sustainable development in healthcare ecosystems.
5.4. Limitations and Future Research
Despite offering valuable theoretical and practical insights into the digital transformation and continuous optimization of HSCs, this study is subject to several limitations that warrant further exploration.
First, the empirical analysis is based on cross-sectional data. Given the progressive and phased nature of digital transformation, future research could benefit from longitudinal or panel data to more systematically examine how the development of digital capabilities influences the long-term stability and sustainability of decision-making performance.
Second, the data collected in this study are primarily drawn from HSC organizations in mainland China. While representative to a certain extent, the findings may be limited by region-specific institutional settings, healthcare system structures, and technological adoption environments. Thus, future studies should extend the research scope to other countries or regions, particularly those with different regulatory frameworks or levels of digital infrastructure, in order to enable cross-country comparisons and enhance the external validity and global relevance of the results.
Third, this study did not investigate the temporally sequential nature of SCR in the healthcare context, particularly how AC, RPC, and RTC affect DO over time. Future research could explore how DI dynamically supports the evolution of these resilience capabilities across different stages, thereby offering deeper insights into its phased and adaptive role in DO.
Lastly, as emerging technologies such as generative AI, the IoT, and biometric systems become increasingly integrated into the healthcare sector, the scope of digital transformation continues to expand. Future research could incorporate these developments to re-examine their impact on SCR, organizational innovation behavior, and complex decision-making processes, thereby providing more forward-looking theoretical frameworks and strategic recommendations.
Author Contributions
Writing—original draft preparation and writing—review and editing, J.-Y.M.; conceptualization and data analysis, T.-W.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study by Institution Committee due to Legal Regulations (Administrative Measures for Ethical Review of Life Science and Medical Research Involving Human Subjects (2023, Document No. 4), https://www.gov.cn/zhengce/zhengceku/2023-02/28/content_5743658.htm, accessed on 20 July 2025).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets of this study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nguyen, A.; Lamouri, S.; Pellerin, R.; Tamayo, S.; Lekens, B. Data analytics in pharmaceutical supply chains: State of the art, opportunities, and challenges. Int. J. Prod. Res. 2022, 60, 6888–6907. [Google Scholar] [CrossRef]
- The IQVIA Institute. The Global Use of Medicines 2024: Outlook to 2028; The IQVIA Institute: Durham, NC, USA, 2024. [Google Scholar]
- Sun, X.; Li, X. Aging and chronic disease: Public health challenge and education reform. Front. Public Health 2023, 11, 1175898. [Google Scholar]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2022, 139, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, S.; Garg, D.; Agarwal, A. A step towards responsive healthcare supply chain management: An overview. In Advances in Manufacturing and Industrial Engineering: Select Proceedings of ICAPIE, Proceedings of the International Conference on Advanced Production and Industrial Engineering, Delhi, India, 21–22 December 2019; Springer: Singapore, 2021; pp. 431–443. [Google Scholar]
- Avinash, B.; Joseph, G. Reimagining healthcare supply chains: A systematic review on digital transformation with specific focus on efficiency, transparency and responsiveness. J. Health Organ. Manag. 2024, 38, 1255–1279. [Google Scholar] [CrossRef]
- Arji, G.; Ahmadi, H.; Avazpoor, P.; Hemmat, M. Identifying resilience strategies for disruption management in the healthcare supply chain during COVID-19 by digital innovations: A systematic literature review. Inform. Med. Unlocked 2023, 38, 101199. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Li, G.; Zheng, H. How does digital intelligence technology enhance supply chain resilience? Sustainable framework and agenda. Ann. Oper. Res. 2024, 1–23. [Google Scholar] [CrossRef]
- Paramasivan, A. Transforming healthcare supply chains: AI for efficient drug distribution and inventory management. IJSAT-Int. J. Sci. Technol. 2023, 14, 1–15. [Google Scholar]
- Naz, A.; Ali, M.; Cheema, S.M.; Pires, I.M. Cloud-Based Framework for Data Exchange to Enhance Global Healthcare. Procedia Comput. Sci. 2024, 241, 570–575. [Google Scholar] [CrossRef]
- Torab-Miandoab, A.; Samad-Soltani, T.; Jodati, A.; Akbarzadeh, F.; Rezaei-Hachesu, P. A unified component-based data-driven framework to support interoperability in the healthcare systems. Heliyon 2024, 10, e35036. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Shi, Y.; Yang, B. Open innovation in times of crisis: An overview of the healthcare sector in response to the COVID-19 Pandemic. J. Open Innov. Technol. Mark. Complex. 2022, 8, 21. [Google Scholar] [CrossRef]
- Ali, O.; Abdelbaki, W.; Shrestha, A.; Elbasi, E.; Alryalat, M.A.A.; Dwivedi, Y.K. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. J. Innov. Knowl. 2023, 8, 100333. [Google Scholar] [CrossRef]
- Mehedy, M.T.J.; Jalil, M.S.; Saeed, M.; Snigdha, E.Z.; Khan, N.; Hasan, M.M. Big Data and Machine Learning in Healthcare: A Business Intelligence Approach for Cost Optimization and Service Improvement. Am. J. Med. Sci. Pharm. Res. 2025, 7, 115–135. [Google Scholar] [CrossRef]
- Mittal, A.; Mantri, A. A literature survey on healthcare supply chain management. F1000Research 2023, 12, 759. [Google Scholar] [CrossRef]
- Madhani, P.M. Resource Based View (RBV) of Competitive Advantage: An Overview. Resource Based View: Concepts and Practices; Madhani, P., Ed.; Icfai University Press: Hyderabad, India, 2010; pp. 3–22. [Google Scholar]
- Gera, N.; Singh, R. Identifying key drivers of supply chain resilience in Indian pharmaceutical industry for enhanced export performance. Int. J. Pharm. Healthc. Mark. 2025. [Google Scholar] [CrossRef]
- Stadtfeld, G.M.; Gruchmann, T. Dynamic capabilities for supply chain resilience: A meta-review. Int. J. Logist. Manag. 2024, 35, 623–648. [Google Scholar] [CrossRef]
- Singh, G.; Singh, S.; Daultani, Y.; Chouhan, M. Measuring the influence of digital twins on the sustainability of manufacturing supply chain: A mediating role of supply chain resilience and performance. Comput. Ind. Eng. 2023, 186, 109711. [Google Scholar] [CrossRef]
- Charles, V.; Emrouznejad, A.; Gherman, T. A critical analysis of the integration of blockchain and artificial intelligence for supply chain. Ann. Oper. Res. 2023, 327, 7–47. [Google Scholar] [CrossRef] [PubMed]
- Armand, T.P.T.; Carole, K.S.; Bhattacharjee, S.; Mozumder, M.A.I.; Amaechi, A.O.; Kim, H.C. The benefits of integrating AI, IoT, and Blockchain in healthcare supply chain management: A multi-dimensional analysis with case study. In Proceedings of the 2024 26th International Conference on Advanced Communications Technology (ICACT), Pyeong Chang, Republic of Korea, 4–7 February 2024; pp. 300–304. [Google Scholar]
- Stroumpoulis, A.; Kopanaki, E. Theoretical perspectives on sustainable supply chain management and digital transformation: A literature review and a conceptual framework. Sustainability 2022, 14, 4862. [Google Scholar] [CrossRef]
- Sahoo, S.K.; Goswami, S.S.; Sarkar, S.; Mitra, S. A review of digital transformation and industry 4.0 in supply chain management for small and medium-sized enterprises. Spectr. Eng. Manag. Sci. 2023, 1, 58–72. [Google Scholar] [CrossRef]
- Al Mashalah, H.; Hassini, E.; Gunasekaran, A.; Bhatt, D. The impact of digital transformation on supply chains through e-commerce: Literature review and a conceptual framework. Transp. Res. Part E Logist. Transp. Rev. 2022, 165, 102837. [Google Scholar] [CrossRef]
- Koot, M.; Mes, M.R.; Iacob, M.E. A systematic literature review of supply chain decision making supported by the Internet of Things and Big Data Analytics. Comput. Ind. Eng. 2021, 154, 107076. [Google Scholar] [CrossRef]
- Uzhakova, N.; Fischer, S. Data-driven enterprise architecture for pharmaceutical R&D. Digital 2024, 4, 333–371. [Google Scholar] [CrossRef]
- Yadav, P. Digital transformation in the health product supply chain: A framework for analysis. Health Syst. Reform 2024, 10, 2386041. [Google Scholar] [CrossRef] [PubMed]
- Dadhich, A.; Dadhich, P. Artificial Intelligence from Vaccine Development to Pharmaceutical Supply Chain Management in Post-COVID-19 Period. In Blockchain, IoT, and AI Technologies for Supply Chain Management; Taylor and Francis: Abingdon, UK, 2023; pp. 143–161. [Google Scholar]
- Long, P.; Lu, L.; Chen, Q.; Chen, Y.; Li, C.; Luo, X. Intelligent selection of healthcare supply chain mode–an applied research based on artificial intelligence. Front. Public Health 2023, 11, 1310016. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, A.; Ebrahimpour, M.; Ramazanian, M.; Moradi, M. Intelligent distributed supply chain management in the pharmaceutical industry. J. Strateg. Manag. Stud. 2024, 14, 141–167. [Google Scholar]
- Shen, J.; Bu, F.; Ye, Z.; Zhang, M.; Ma, Q.; Yan, J.; Huang, T. Management of drug supply chain information based on “artificial intelligence+ vendor managed inventory” in China: Perspective based on a case study. Front. Pharmacol. 2024, 15, 1373642. [Google Scholar] [CrossRef] [PubMed]
- Al-Shboul, M.D.A. Do artificial intelligence system adoptions foster production management supply chain performance in pharmaceutical manufacturing firms? An empirical exploring study from the MENA region. Bus. Process Manag. J. 2024, 30, 2427–2455. [Google Scholar]
- Skowron-Grabowska, B.; Wincewicz-Bosy, M.; Dymyt, M.; Sadowski, A.; Dymyt, T.; Wąsowska, K. Healthcare supply chain reliability: The case of medical air transport. Int. J. Environ. Res. Public Health 2022, 19, 4336. [Google Scholar] [CrossRef] [PubMed]
- Ramos, E.; Patrucco, A.S.; Chavez, M. Dynamic capabilities in the “new normal”: A study of organizational flexibility, integration and agility in the Peruvian coffee supply chain. Supply Chain Manag. Int. J. 2023, 28, 55–73. [Google Scholar] [CrossRef]
- Tian, S.; Wu, L.; Ciano, M.P.; Ardolino, M.; Pawar, K.S. Enhancing innovativeness and performance of the manufacturing supply chain through datafication: The role of resilience. Comput. Ind. Eng. 2024, 188, 109841. [Google Scholar] [CrossRef]
- Moderno, O.B.D.S.; Braz, A.C.; Nascimento, P.T.D.S. Robotic process automation and artificial intelligence capabilities driving digital strategy: A resource-based view. Bus. Process Manag. J. 2024, 30, 105–134. [Google Scholar] [CrossRef]
- Wang, D.; Liu, W.; Liang, Y.; Wei, S. Decision optimization in service supply chain: The impact of demand and supply-driven data value and altruistic behavior. Ann. Oper. Res. 2023, 324, 971–992. [Google Scholar] [CrossRef]
- Martínez-Peláez, R.; Ochoa-Brust, A.; Rivera, S.; Félix, V.G.; Ostos, R.; Brito, H.; Mena, L.J. Role of digital transformation for achieving sustainability: Mediated role of stakeholders, key capabilities, and technology. Sustainability 2023, 15, 11221. [Google Scholar] [CrossRef]
- Adama, H.E.; Popoola, O.A.; Okeke, C.D.; Akinoso, A.E. Economic theory and practical impacts of digital transformation in supply chain optimization. Int. J. Adv. Econ. 2024, 6, 95–107. [Google Scholar] [CrossRef]
- Bahrami, M.; Shokouhyar, S.; Seifian, A. Big data analytics capability and supply chain performance: The mediating roles of supply chain resilience and innovation. Mod. Supply Chain Res. Appl. 2022, 4, 62–84. [Google Scholar] [CrossRef]
- Gao, Y.; Liu, Y.; Wu, W. How Does Artificial Intelligence Capability Affect Product Innovation in Manufacturing Enterprises? Evidence from China. Systems 2025, 13, 480. [Google Scholar] [CrossRef]
- Zhang, G.; Wang, X.; Xie, J.; Hu, Q. A mechanistic study of enterprise digital intelligence transformation, innovation resilience, and firm performance. Systems 2024, 12, 186. [Google Scholar] [CrossRef]
- Le, T.T.; Behl, A. Linking artificial intelligence and supply chain resilience: Roles of dynamic capabilities mediator and open innovation moderator. IEEE Trans. Eng. Manag. 2023, 71, 8577–8590. [Google Scholar] [CrossRef]
- Hendry, L.C.; Stevenson, M.; MacBryde, J.; Ball, P.; Sayed, M.; Liu, L. Local food supply chain resilience to constitutional change: The Brexit effect. Int. J. Oper. Prod. Manag. 2019, 39, 429–453. [Google Scholar] [CrossRef]
- Zhao, N.; Hong, J.; Lau, K.H. Impact of supply chain digitalization on supply chain resilience and performance: A multi-mediation model. Int. J. Prod. Econ. 2023, 259, 108817. [Google Scholar] [CrossRef] [PubMed]
- Senna, P.; Reis, A.; Dias, A.; Coelho, O.; Guimarães, J.; Eliana, S. Healthcare supply chain resilience framework: Antecedents, mediators, consequents. Prod. Plan. Control 2023, 34, 295–309. [Google Scholar] [CrossRef]
- Anozie, U.C.; Adewumi, G.; Obafunsho, O.E.; Toromade, A.S.; Olaluwoye, O.S. Leveraging advanced technologies in Supply Chain Risk Management (SCRM) to mitigate healthcare disruptions: A comprehensive review. World J. Adv. Res. Rev. 2024, 23, 1039–1045. [Google Scholar] [CrossRef]
- Gaudenzi, B.; Pellegrino, R.; Confente, I. Achieving supply chain resilience in an era of disruptions: A configuration approach of capacities and strategies. Supply Chain Manag. Int. J. 2023, 28, 97–111. [Google Scholar] [CrossRef]
- Furstenau, L.B.; Zani, C.; Terra, S.X.; Sott, M.K.; Choo, K.K.R.; Saurin, T.A. Resilience capabilities of healthcare supply chain and supportive digital technologies. Technol. Soc. 2022, 71, 102095. [Google Scholar] [CrossRef]
- Aslam, H.; Khan, A.Q.; Rashid, K.; Rehman, S.U. Achieving supply chain resilience: The role of supply chain ambidexterity and supply chain agility. J. Manuf. Technol. Manag. 2020, 31, 1185–1204. [Google Scholar] [CrossRef]
- Singh, R.K.; Modgil, S. Adapting to disruption: The impact of agility, absorptive capacity and ambidexterity on supply chain resilience. Int. J. Product. Perform. Manag. 2025, 74, 637–658. [Google Scholar] [CrossRef]
- Tortorella, G.; Prashar, A.; Samson, D.; Kurnia, S.; Fogliatto, F.S.; Capurro, D.; Antony, J. Resilience development and digitalization of the healthcare supply chain: An exploratory study in emerging economies. Int. J. Logist. Manag. 2023, 34, 130–163. [Google Scholar] [CrossRef]
- Wright, A.M.; Snowdon, A.; Saunders, M.; Trampas, D. The necessity of healthcare supply chain resilience for crisis preparedness. Healthc. Manag. Forum 2024, 37, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Naz, F.; Luthra, S.; Vashistha, R.; Kumar, V.; Garza-Reyes, J.A.; Chhabra, D. Digging DEEP: Futuristic building blocks of omni-channel healthcare supply chains resiliency using machine learning approach. J. Bus. Res. 2023, 162, 113903. [Google Scholar] [CrossRef]
- Saarinen, L.; Oddsdottir, H.; Rehman, O. Resilience through appropriate response: A simulation study of disruptions and response strategies–case COVID-19 and the grocery supply chain. Oper. Manag. Res. 2024, 17, 1078–1099. [Google Scholar] [CrossRef]
- Maheshwari, P.; Kamble, S.S.; Belhadi, A.; Gupta, S.; Mangla, S.K. Resilient healthcare network for simultaneous product allocations during supply chain disruptions. Supply Chain Forum Int. J. 2024, 25, 407–427. [Google Scholar] [CrossRef]
- Tetteh, F.K.; Nyamekye, B.; Williams, E.; Attah, J.; Degbe, F.D. Effect of Supply Chain Analytics on Healthcare Supply Chain Performance: The Relevance of Building Responsive, Resilience, Restoration (3rs) and Desorptive Capabilities. Resil. Restor. (3rs) Desorptive Capab. 2024. [Google Scholar] [CrossRef]
- Vanany, I.; Ali, M.H.; Tan, K.H.; Kumar, A.; Siswanto, N. A supply chain resilience capability framework and process for mitigating the COVID-19 pandemic disruption. IEEE Trans. Eng. Manag. 2021, 71, 10358–10372. [Google Scholar] [CrossRef]
- Belhadi, A.; Mani, V.; Kamble, S.S.; Khan, S.A.R.; Verma, S. Artificial intelligence-driven innovation for enhancing supply chain resilience and performance under the effect of supply chain dynamism: An empirical investigation. Ann. Oper. Res. 2024, 333, 627–652. [Google Scholar] [CrossRef] [PubMed]
- Tortorella, G.L.; Prashar, A.; Antony, J.; Fogliatto, F.S.; Gonzalez, V.; Godinho Filho, M. Industry 4.0 adoption for healthcare supply chain performance during COVID-19 pandemic in Brazil and India: The mediating role of resilience abilities development. Oper. Manag. Res. 2024, 17, 389–405. [Google Scholar] [CrossRef]
- Silva, A.C.; Marques, C.M.; de Sousa, J.P. A simulation approach for the design of more sustainable and resilient supply chains in the pharmaceutical industry. Sustainability 2023, 15, 7254. [Google Scholar] [CrossRef]
- Badejo, O.; Ierapetritou, M. Optimization of pharmaceutical supply chains: Navigating disruptions and operational uncertainty utilizing risk measures. AIChE J. 2025, 71, e18770. [Google Scholar] [CrossRef]
- Mahdavimanshadi, M.; Anaraki, M.G.; Mowlai, M.; Ahmadirad, Z. A multistage stochastic optimization model for resilient pharmaceutical supply chain in COVID-19 pandemic based on patient group priority. In Proceedings of the 2024 Systems and Information Engineering Design Symposium (SIEDS), Charlottesville, VA, USA, 3 May 2024; pp. 382–387. [Google Scholar]
- Li, Q.; Zhang, H.; Liu, K.; Zhang, Z.J.; Jasimuddin, S.M. Linkage between digital supply chain, supply chain innovation and supply chain dynamic capabilities: An empirical study. Int. J. Logist. Manag. 2024, 35, 1200–1223. [Google Scholar] [CrossRef]
- Aghaei, R.; Kiaei, A.A.; Boush, M.; Vahidi, J.; Barzegar, Z.; Rofoosheh, M. The Potential of Large Language Models in Supply Chain Management: Advancing Decision-Making, Efficiency, and Innovation. arXiv 2025, arXiv:2501.15411. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, J.; Zhang, H.; Song, J. Bridging Prediction and Decision: Advances and Challenges in Data-Driven Optimization. Nexus 2025, 2, 100057. [Google Scholar] [CrossRef]
- Ivanov, D.; Dolgui, A.; Das, A.; Sokolov, B. Digital supply chain twins: Managing the ripple effect, resilience, and disruption risks by data-driven optimization, simulation, and visibility. In Handbook of Ripple Effects in the Supply Chain; Springer: Cham, Switzerland, 2019; pp. 309–332. [Google Scholar]
- Barney, J.B. Resource-based theories of competitive advantage: A ten-year retrospective on the resource-based view. J. Manag. 2001, 27, 643–650. [Google Scholar] [CrossRef]
- Revilla, E.; Acero, B.; Sáenz, M.J. Resilience in the Supply Chain. In The Palgrave Handbook of Supply Chain Management; Palgrave Macmillan: Cham, Switzerland, 2024; pp. 601–625. [Google Scholar]
- Ning, L.; Yao, D. The impact of digital transformation on supply chain capabilities and supply chain competitive performance. Sustainability 2023, 15, 10107. [Google Scholar] [CrossRef]
- Wang, S.; Ghadge, A.; Aktas, E. Digital transformation in food supply chains: An implementation framework. Supply Chain Manag. Int. J. 2024, 29, 328–350. [Google Scholar] [CrossRef]
- Tiwari, M.; Bryde, D.J.; Stavropolou, F.; Dubey, R.; Kumari, S.; Foropon, C. Modelling supply chain Visibility, digital Technologies, environmental dynamism and healthcare supply chain Resilience: An organisation information processing theory perspective. Transp. Res. Part E Logist. Transp. Rev. 2024, 188, 103613. [Google Scholar] [CrossRef]
- Lima, B.; Ganga, G.M.D.; Godinho Filho, M.; De Santa-Eulalia, L.A.; Thürer, M.; Queiroz, M.M.; Moraes, K.K. Timing and interdependencies in blockchain capabilities development for supply chain management: A resource-based view perspective. Ind. Manag. Data Syst. 2025, 125, 1645–1685. [Google Scholar] [CrossRef]
- Tonsi, A.A.; Husain, K.S.; Yaqub, M.Z. IT Capabilities’ Impact on Postponement and Supply Chain Viability of Retail Manufacturers: A Dynamic Resource-Based View. Sustainability 2025, 17, 1437. [Google Scholar] [CrossRef]
- Moraes, K.K.; Ganga, G.M.D.; Godinho Filho, M.; Santa-Eulalia, L.A.; Tortorella, G.L. Overcoming technological barriers for blockchain adoption in supply chains: A diffusion of innovation (DOI)-informed framework proposal. Supply Chain Manag. Int. J. 2025, 30, 19–49. [Google Scholar] [CrossRef]
- Mehmood, S.; Nazir, S.; Fan, J.; Nazir, Z. Achieving supply chain sustainability: Enhancing supply chain resilience, organizational performance, innovation and information sharing: Empirical evidence from Chinese SMEs. Mod. Supply Chain Res. Appl. 2025, 7, 2–29. [Google Scholar] [CrossRef]
- Seifi, N.; Ghoodjani, E.; Majd, S.S.; Maleki, A.; Khamoushi, S. Evaluation and prioritization of artificial intelligence integrated block chain factors in healthcare supply chain: A hybrid Decision Making Approach. Comput. Decis. Mak. Int. J. 2025, 2, 374–405. [Google Scholar] [CrossRef]
- Kasparis, E.; Huang, Y.; Lin, W.; Vasilakis, C. Improving timeliness in the neglected tropical diseases preventive chemotherapy donation supply chain through information sharing: A retrospective empirical analysis. PLoS Neglected Trop. Dis. 2021, 15, e0009523. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Che Mat, C.R.; Ibrahim, A.; Zhang, Y.; Muzammil, S. Digital supply chain reshaping industrial ecology: A study from the Pharma Industry. In Industrial Ecology: A Fusion of Material and Energy in Green Supply Chain Context; Springer: Singapore, 2024; pp. 107–123. [Google Scholar]
- Adhikari, A.; Joshi, R.; Basu, S. Collaboration and coordination strategies for a multi-level AI-enabled healthcare supply chain under disaster. Int. J. Prod. Res. 2025, 63, 497–523. [Google Scholar] [CrossRef]
- Lee, K.L.; Wong, S.Y.; Alzoubi, H.M.; Al Kurdi, B.; Alshurideh, M.T.; El Khatib, M. Adopting smart supply chain and smart technologies to improve operational performance in manufacturing industry. Int. J. Eng. Bus. Manag. 2023, 15, 18479790231200614. [Google Scholar] [CrossRef]
- Al-Surmi, A.; Bashiri, M.; Koliousis, I. AI based decision making: Combining strategies to improve operational performance. Int. J. Prod. Res. 2022, 60, 4464–4486. [Google Scholar] [CrossRef]
- Abourokbah, S.H.; Mashat, R.M.; Salam, M.A. Role of absorptive capacity, digital capability, agility, and resilience in supply chain innovation performance. Sustainability 2023, 15, 3636. [Google Scholar] [CrossRef]
- Apell, P.; Eriksson, H. Artificial intelligence (AI) healthcare technology innovations: The current state and challenges from a life science industry perspective. Technol. Anal. Strateg. Manag. 2023, 35, 179–193. [Google Scholar] [CrossRef]
- Papalexi, M.; Bamford, D.; Breen, L. Key sources of operational inefficiency in the pharmaceutical supply chain. Supply Chain Manag. Int. J. 2020, 25, 617–635. [Google Scholar] [CrossRef]
- Chen, X.; He, C.; Chen, Y.; Xie, Z. Internet of Things (IoT)—Blockchain-enabled pharmaceutical supply chain resilience in the post-pandemic era. Front. Eng. Manag. 2023, 10, 82–95. [Google Scholar] [CrossRef]
- Kyeremeh, E.; Yamoah, E.E.; Yamoah, A. Enhancing pharmaceutical supply chain performance: The impact of technology integration, interorganizational trust, and collaboration in the digital age. Future Bus. J. 2025, 11, 98. [Google Scholar] [CrossRef]
- Gama, F.; Magistretti, S. Artificial intelligence in innovation management: A review of innovation capabilities and a taxonomy of AI applications. J. Prod. Innov. Manag. 2025, 42, 76–111. [Google Scholar] [CrossRef]
- Cannavale, C.; Esempio Tammaro, A.; Leone, D.; Schiavone, F. Innovation adoption in inter-organizational healthcare networks–the role of artificial intelligence. Eur. J. Innov. Manag. 2022, 25, 758–774. [Google Scholar] [CrossRef]
- Machucho, R.; Ortiz, D. The Impacts of Artificial Intelligence on Business Innovation: A Comprehensive Review of Applications, Organizational Challenges, and Ethical Considerations. Systems 2025, 13, 264. [Google Scholar] [CrossRef]
- Saha, R. Empowering Absorptive Capacity in Healthcare Supply Chains Through Big Data Analytics and AI-Driven Collaborative Platforms: A Prisma-Based Systematic Review. Innov. Eng. J. 2024, 1, 10–70937. [Google Scholar] [CrossRef]
- Bag, S.; Dhamija, P.; Singh, R.K.; Rahman, M.S.; Sreedharan, V.R. Big data analytics and artificial intelligence technologies based collaborative platform empowering absorptive capacity in health care supply chain: An empirical study. J. Bus. Res. 2023, 154, 113315. [Google Scholar] [CrossRef]
- Kazancoglu, I.; Ozbiltekin-Pala, M.; Mangla, S.K.; Kazancoglu, Y.; Jabeen, F. Role of flexibility, agility and responsiveness for sustainable supply chain resilience during COVID-19. J. Clean. Prod. 2022, 362, 132431. [Google Scholar] [CrossRef]
- Addy, A.L.F.R.E.D. Artificial intelligence in the supply chain management for vaccine distribution in the West Africa n healthcare sector with a focus on Ghana. Int. J. Leg. Sci. Innov. 2023, 10, 1–25. [Google Scholar]
- Makarevic, M.; Tas, P.G. Strategic decision-making in process optimization of healthcare technology manufacturing. J. Supply Chain. Manag. Sci. 2024, 5, 117–142. [Google Scholar] [CrossRef]
- Jum’a, L.; Zimon, D.; Madzik, P. Impact of big data technological and personal capabilities on sustainable performance on Jordanian manufacturing companies: The mediating role of innovation. J. Enterp. Inf. Manag. 2024, 37, 329–354. [Google Scholar] [CrossRef]
- Kumar, R.R.; Raj, A. Big data adoption and performance: Mediating mechanisms of innovation, supply chain integration and resilience. Supply Chain Manag. Int. J. 2025, 30, 67–85. [Google Scholar] [CrossRef]
- Tetteh, F.K.; Amoako, D.K.; Kyeremeh, A.; Atiki, G.; Degbe, F.D.; Nyame, P.E.D. Unraveling the interplay between supply chain analytics and healthcare supply chain performance: Establishing an underlying mechanism and a boundary condition. Int. J. Qual. Reliab. Manag. 2025, 42, 752–783. [Google Scholar] [CrossRef]
- Fernando, Y.; Tseng, M.L.; Nur, G.M.; Ikhsan, R.B.; Lim, M.K. Practising circular economy performance in Malaysia: Managing supply chain disruption and technological innovation capability under industry 4.0. Int. J. Logist. Res. Appl. 2023, 26, 1704–1727. [Google Scholar] [CrossRef]
- Javan-Molaei, B.; Tavakkoli-Moghaddam, R.; Ghanavati-Nejad, M.; Asghari-Asl, A. A data-driven robust decision-making model for configuring a resilient and responsive relief supply chain under mixed uncertainty. Ann. Oper. Res. 2024, 1–38. [Google Scholar] [CrossRef]
- Adana, S.; Manuj, I.; Herburger, M.; Cevikparmak, S.; Celik, H.; Uvet, H. Linking decentralization in decision-making to resilience outcomes: A supply chain orientation perspective. Int. J. Logist. Manag. 2024, 35, 256–280. [Google Scholar] [CrossRef]
- Sadeghi, K.; Ojha, D.; Kaur, P.; Mahto, R.V.; Dhir, A. Explainable artificial intelligence and agile decision-making in supply chain cyber resilience. Decis. Support Syst. 2024, 180, 114194. [Google Scholar] [CrossRef]
- Xiang, Y.; Li, X.; Liu, W.; Luo, F.; Wang, M. Enhancing chromium supply chain security through resilience strategies: Decision support based on system dynamics simulations. J. Clean. Prod. 2025, 493, 144981. [Google Scholar] [CrossRef]
- Vega, D.; Arvidsson, A.; Saiah, F. Resilient supply management systems in times of crisis. Int. J. Oper. Prod. Manag. 2023, 43, 70–98. [Google Scholar] [CrossRef]
- Qureshi, K.M.; Mewada, B.G.; Kaur, S.; Alghamdi, S.Y.; Almakayeel, N.; Almuflih, A.S.; Qureshi, M.R.N.M. Sustainable manufacturing supply chain performance enhancement through technology utilization and process innovation in industry 4.0: A SEM-PLS approach. Sustainability 2023, 15, 15388. [Google Scholar] [CrossRef]
- Junaid, M.; Zhang, Q.; Cao, M.; Luqman, A. Nexus between technology enabled supply chain dynamic capabilities, integration, resilience, and sustainable performance: An empirical examination of healthcare organizations. Technol. Forecast. Soc. Change 2023, 196, 122828. [Google Scholar] [CrossRef]
- Olaleye, B.R.; Lekunze, J.N.; Sekhampu, T.J.; Khumalo, N.; Ayeni, A.A.W. Leveraging innovation capability and organizational resilience for business sustainability among small and medium enterprises: A PLS-SEM approach. Sustainability 2024, 16, 9201. [Google Scholar] [CrossRef]
- Taghizadeh, S.K.; Rahman, S.A.; Nikbin, D.; Radomska, M.; Maleki Far, S. Dynamic capabilities of the SMEs for sustainable innovation performance: Role of environmental turbulence. J. Organ. Eff. People Perform 2024, 11, 767–787. [Google Scholar] [CrossRef]
- Atieh Ali, A.A.; Sharabati, A.A.A.; Allahham, M.; Nasereddin, A.Y. The relationship between supply chain resilience and digital supply chain and the impact on sustainability: Supply chain dynamism as a moderator. Sustainability 2024, 16, 3082. [Google Scholar] [CrossRef]
- Su, X.; Mou, C.; Zhou, S. Institutional environment, technological innovation capability and service-oriented transformation. PLoS ONE 2023, 18, e0281403. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, N.C.; Ferreira, J.J. The field of resource-based view research: Mapping past, present and future trends. Manag. Decis. 2025, 63, 1124–1153. [Google Scholar] [CrossRef]
- Tyagi, S. Analytics in healthcare supply chain management in the new normal era: A review and future research agenda. Benchmarking Int. J. 2024, 31, 2151–2175. [Google Scholar] [CrossRef]
- Hussain, M.; Ajmal, M.; Subramanian, G.; Khan, M.; Anas, S. Challenges of big data analytics for sustainable supply chains in healthcare–a resource-based view. Benchmarking Int. J. 2024, 31, 2897–2918. [Google Scholar] [CrossRef]
- Joshi, A.; Kale, S.; Chandel, S.; Pal, D.K. Likert scale: Explored and explained. Br. J. Appl. Sci. Technol. 2015, 7, 396. [Google Scholar] [CrossRef]
- Le, T.V.; Fan, R. Digital twins for logistics and supply chain systems: Literature review, conceptual framework, research potential, and practical challenges. Comput. Ind. Eng. 2024, 187, 109768. [Google Scholar] [CrossRef]
- Wu, C.H.; Tsang, Y.P.; Lee, C.K.M.; Ching, W.K. A blockchain-IoT platform for the smart pallet pooling management. Sensors 2021, 21, 6310. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, H.F.; Rice, J. Little Jiffy, Mark Iv. Educ. Psychol. Meas. 1974, 34, 111–117. [Google Scholar] [CrossRef]
- Arsham, H.; Lovric, M. Bartlett’s Test. Int. Encycl. Stat. Sci. 2011, 2, 20–23. [Google Scholar]
- Suhr, D.D. Principal component analysis vs. exploratory factor analysis. SUGI 30 Proc. 2005, 203, 1–11. [Google Scholar]
- Fabrigar, L.R.; Wegener, D.T.; MacCallum, R.C.; Strahan, E.J. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods 1999, 4, 272. [Google Scholar] [CrossRef]
- Babbie, E.; Wagner-Huang, W.E.; Zaino, J. Adventures in Social Research: Data Analysis Using IBM SPSS Statistics; Sage Publications: Thousand Oaks, CA, USA, 2022. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation coefficients: Appropriate use and interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef] [PubMed]
- Alwin, D.F.; Hauser, R.M. The decomposition of effects in path analysis. Am. Sociol. Rev. 1975, 40, 37–47. [Google Scholar] [CrossRef]
- Wen, Z.; Ye, B. Analyses of mediating effects: The development of methods and models. Adv. Psychol. Sci. 2014, 22, 731. [Google Scholar] [CrossRef]
- Senapati, T.; Sarkar, A.; Chen, G. Enhancing healthcare supply chain management through artificial intelligence-driven group decision-making with Sugeno–Weber triangular norms in a dual hesitant q-rung orthopair fuzzy context. Eng. Appl. Artif. Intell. 2024, 135, 108794. [Google Scholar] [CrossRef]
- Tiwari, M.K.; Bidanda, B.; Geunes, J.; Fernandes, K.; Dolgui, A. Supply chain digitisation and management. Int. J. Prod. Res. 2024, 62, 2918–2926. [Google Scholar] [CrossRef]
- Zhang, W.; Xu, H.; Grebinevych, O.; Chen, M. Sustainable development with Artificial Intelligence: Examining the absorptive capacity pathways to green innovation. J. Environ. Manag. 2025, 381, 125219. [Google Scholar] [CrossRef] [PubMed]
- Kalnins, A. Should moderated regressions include or exclude quadratic terms? Present both! Then apply our linear algebraic analysis to identify the preferable specification. Organ. Res. Methods 2024, 27, 29–63. [Google Scholar] [CrossRef]
- Xiao, J.; Bao, Y. Partners’ knowledge utilization and exploratory innovation: The moderating effect of competitive and collaborative relationships. Int. J. Oper. Prod. Manag. 2022, 42, 1356–1383. [Google Scholar] [CrossRef]
- Tank, Y.T. Research Report on the Current Status and Capabilities of Digital Transformation of China’s Medical Industry in 2023. 2023. Available online: https://www.iyiou.com/research/202308141255 (accessed on 20 July 2025).
- Nanda, S.K.; Panda, S.K.; Dash, M. Medical supply chain integrated with blockchain and IoT to track the logistics of medical products. Multimed. Tools Appl. 2023, 82, 32917–32939. [Google Scholar] [CrossRef] [PubMed]
- Roosevelt, S.C.; Veemaraj, E.; Kirubakaran, S. Real Time Stock Inventory Management System. In Proceedings of the 2024 8th International Conference on Inventive Systems and Control (ICISC), Coimbatore, India, 29–30 July 2024; pp. 156–162. [Google Scholar]
- Tayab, A.; Li, Y. The contribution of the RPA technology in enhancing better business performance in Warehouse management. IEEE Access 2024, 12, 142419–142426. [Google Scholar] [CrossRef]
- Mousa, B.A.; Al-Khateeb, B. Predicting medicine demand using deep learning techniques: A review. J. Intell. Syst. 2023, 32, 20220297. [Google Scholar] [CrossRef]
- Cresswell, K.; Sheikh, A.; Krasuska, M.; Heeney, C.; Franklin, B.D.; Lane, W.; Williams, R. Reconceptualising the digital maturity of health systems. Lancet Digit. Health 2019, 1, e200–e201. [Google Scholar] [CrossRef] [PubMed]
- Rehman, O.U.; Ali, Y. Enhancing healthcare supply chain resilience: Decision-making in a fuzzy environment. Int. J. Logist. Manag. 2022, 33, 520–546. [Google Scholar] [CrossRef]
- Contreras, N.A.; Guerrero, W.; Besiou, M. Pharmaceutical Inventory Management Using Industry 4.0 Technologies Based on Collaborative Demand: A System Dynamics Approach. In Proceedings of the 7th European Conference on Industrial Engineering and Operations Management, Augsburg, Germany, 16–18 July 2024; pp. 957–973. [Google Scholar]
- Beaulieu, M.; Bentahar, O. Digitalization of the healthcare supply chain: A roadmap to generate benefits and effectively support healthcare delivery. Technol. Forecast. Soc. Change 2021, 167, 120717. [Google Scholar] [CrossRef]
- Anthony, O.C.; Oluwagbade, E.; Bakare, A.; Animasahun, B. Evaluating the economic and clinical impacts of pharmaceutical supply chain centralization through AI-driven predictive analytics: Comparative lessons from large-scale centralized procurement systems and implications for drug pricing, availability, and cardiovascular health outcomes in the US. Int. J. Res. Publ. Rev. 2024, 5, 5148–5161. [Google Scholar]
- Asa, K.J.; Zosu, S.J. Enhancing procurement and supply chain management for sustainable development through digital transformation. Int. J. Afr. Res. Sustain. Stud. 2023, 2, 62–76. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).