A Place-Based County-Level Study of Air Quality and Health in Urban Communities
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Sociodemographic Data
2.3. Air Quality Data
2.4. Health Data
2.5. Correlation Analyses, Geospatial, and Geostatistical Modeling
3. Results
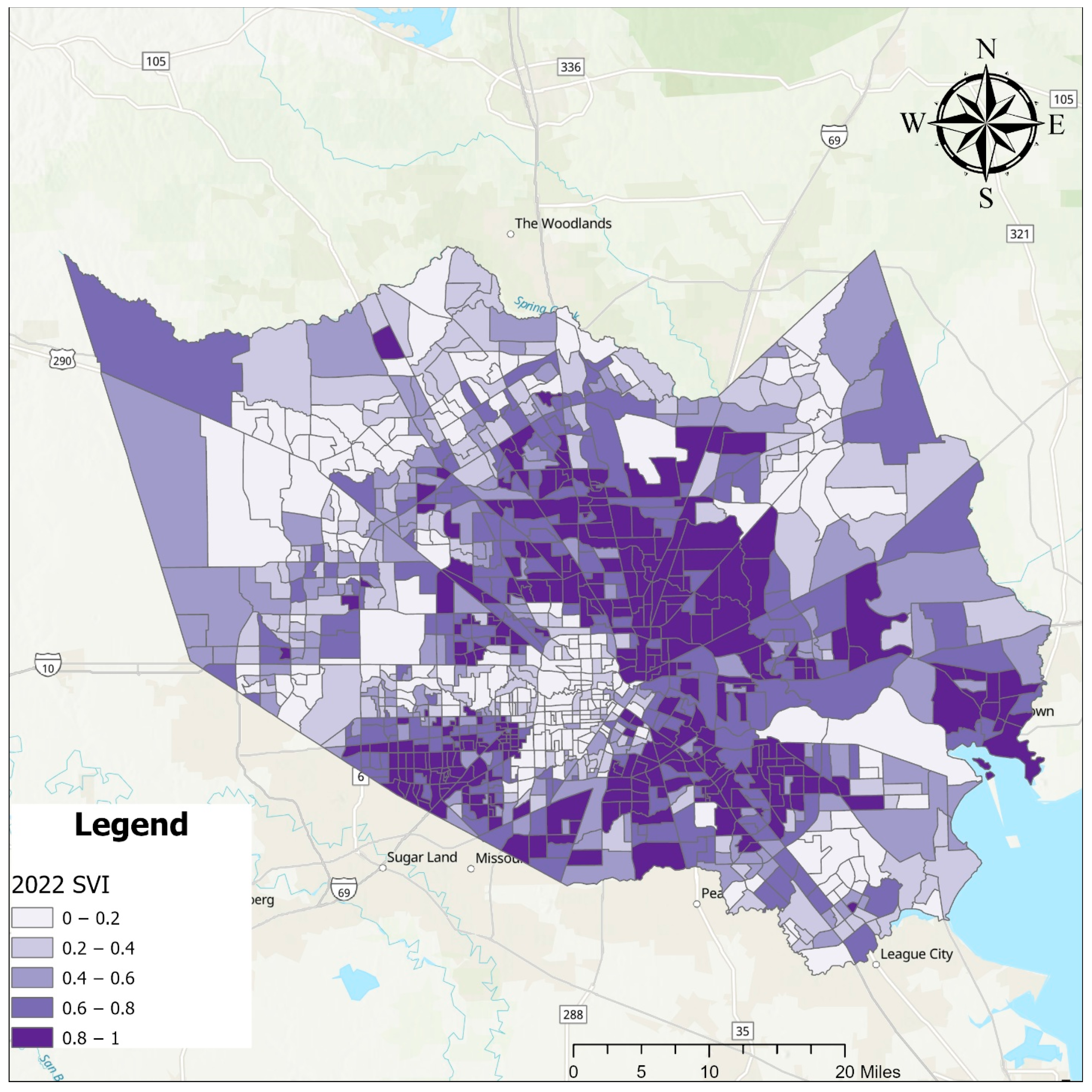
3.1. Geospatial Sociodemographic Analysis
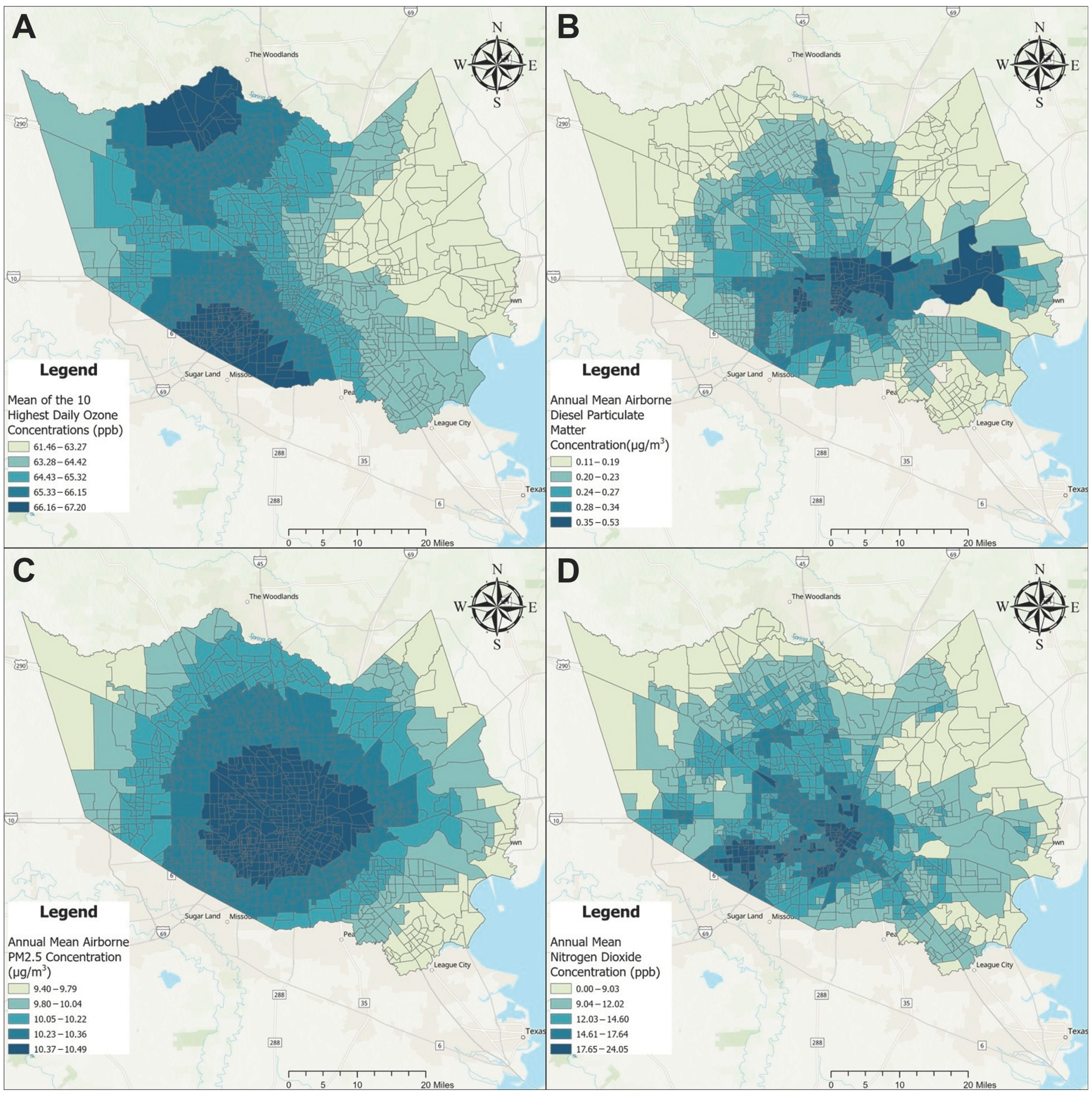
3.2. Geospatial Air Quality Measures
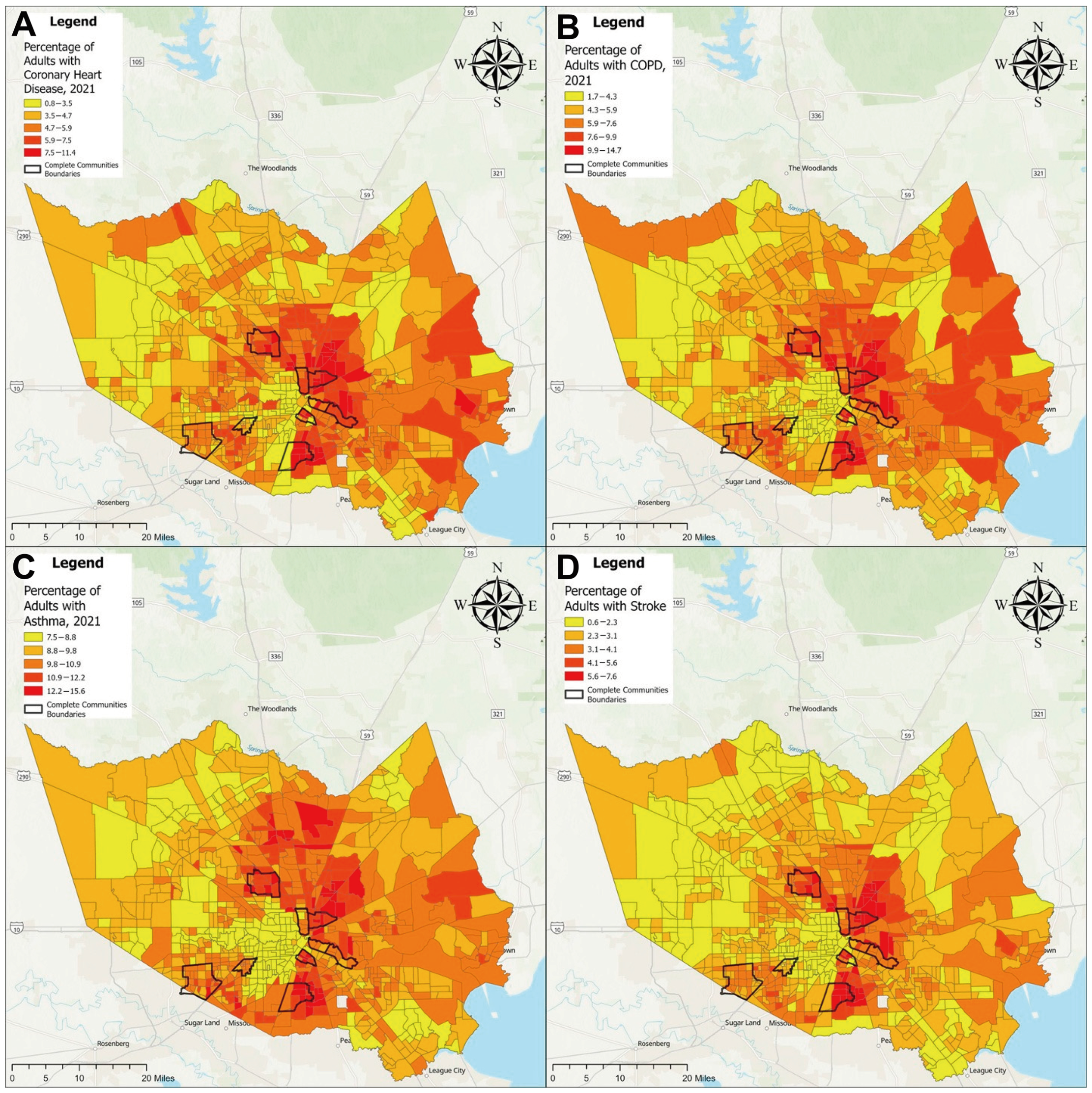
3.3. Geospatial Health Measures
3.4. Correlation Analyses
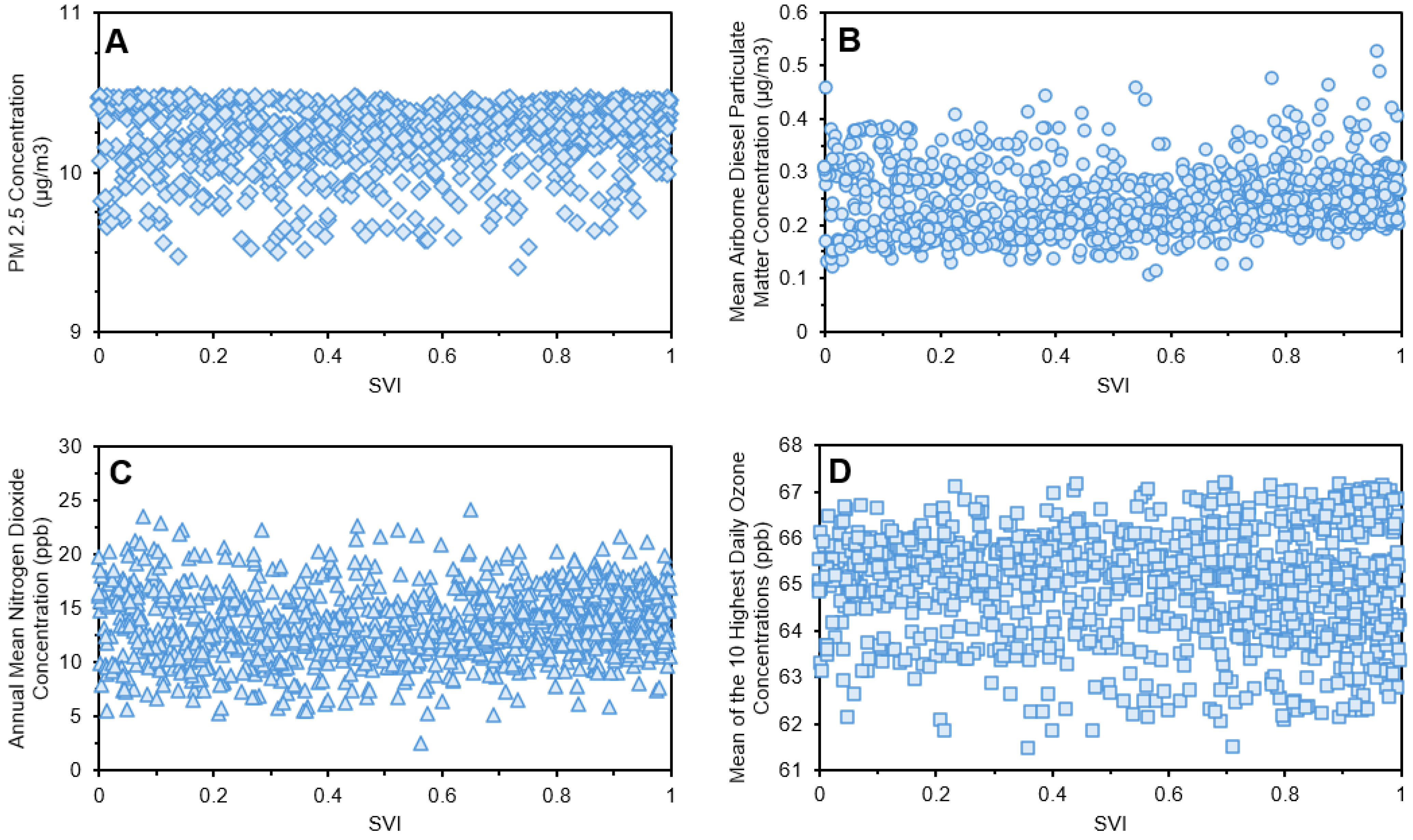
3.4.1. Air Quality and SVI
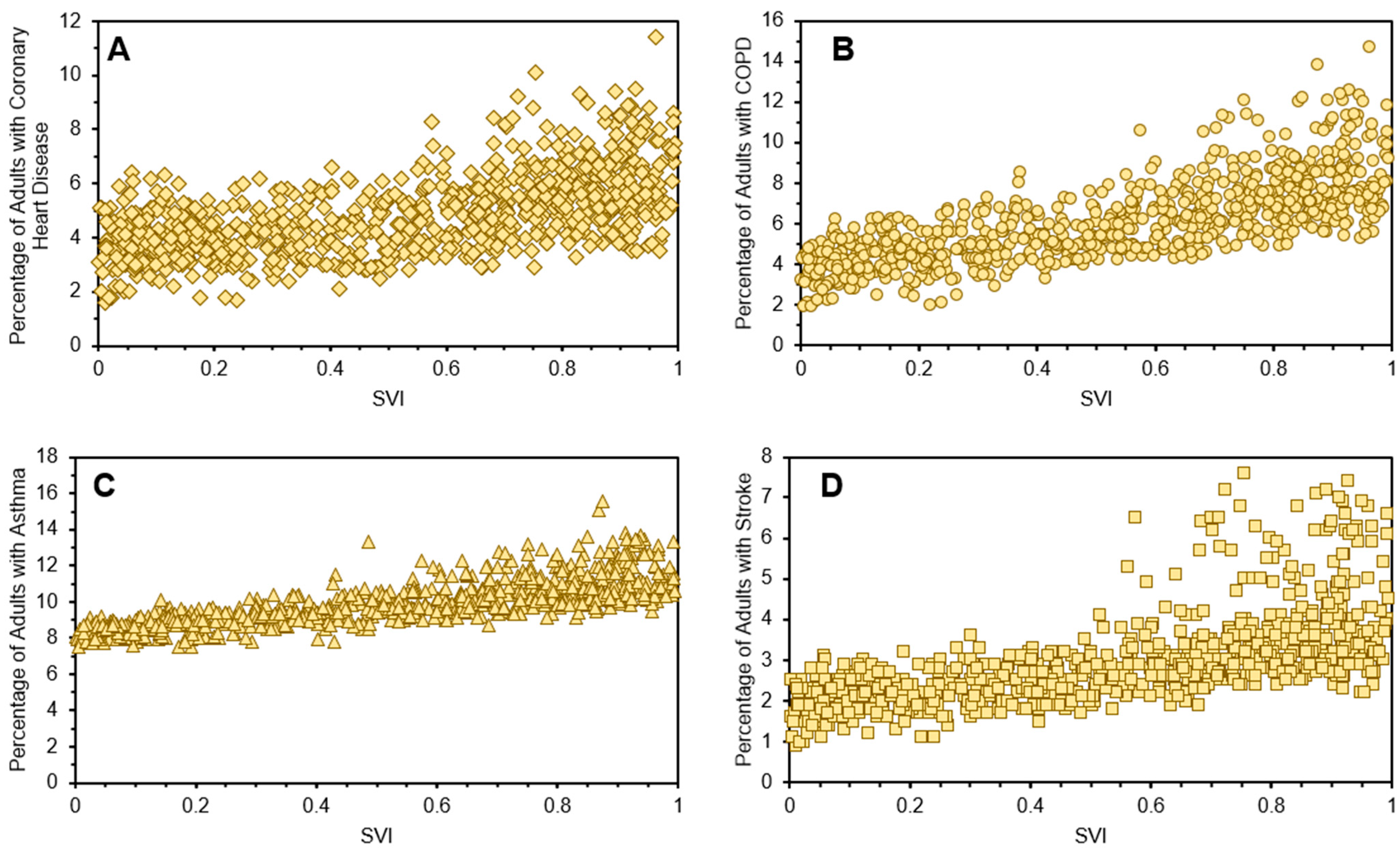
3.4.2. Health and SVI
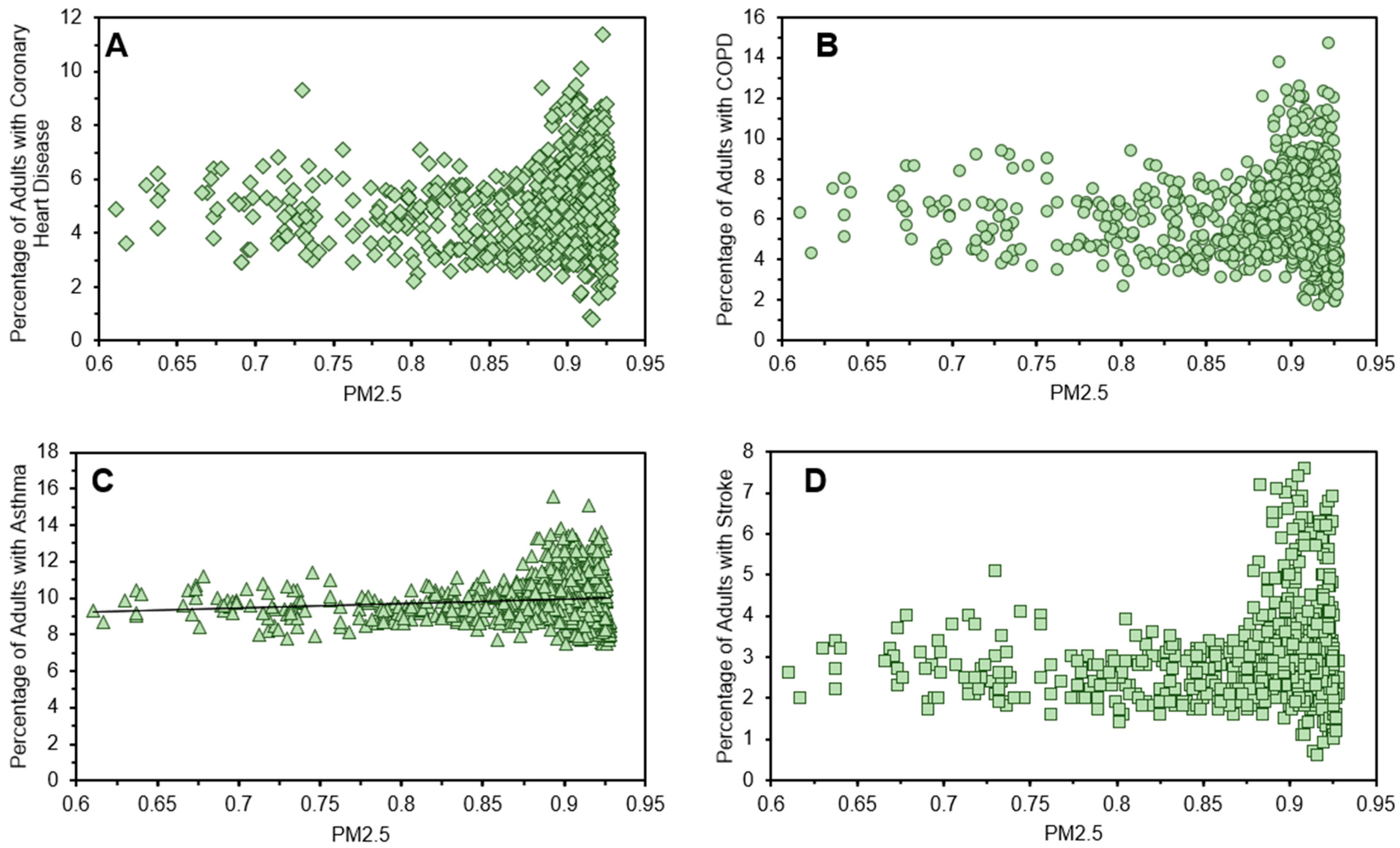
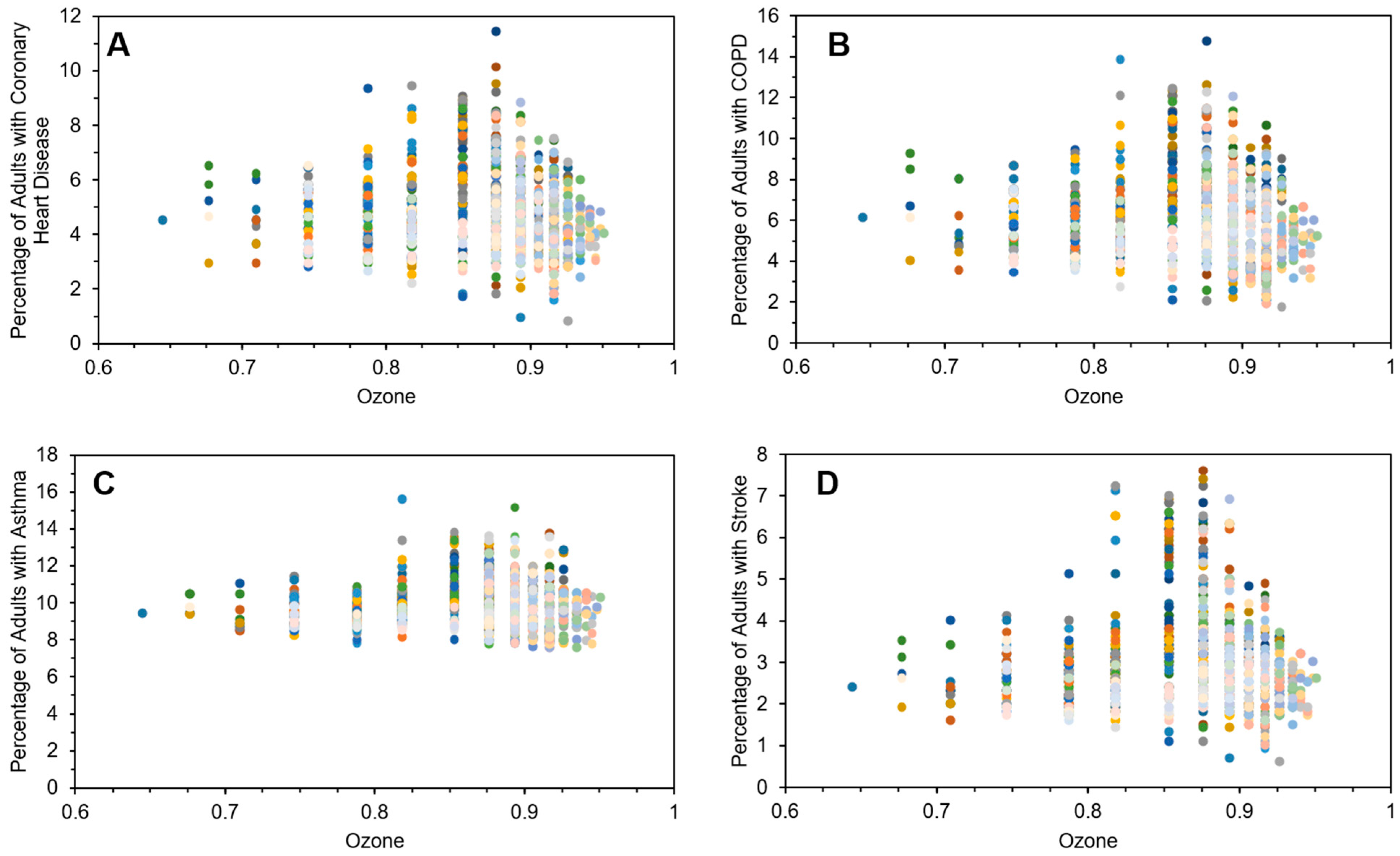
3.4.3. Health and Air Quality
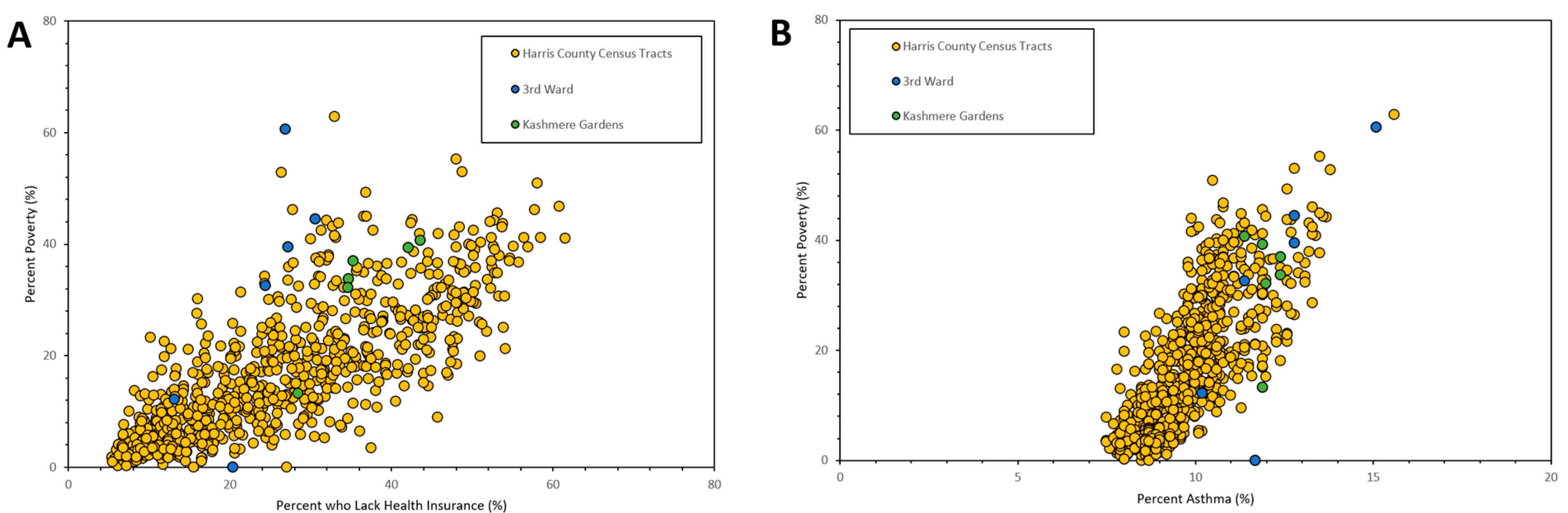
3.5. Community-Based Geospatial and Temporal Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242. [Google Scholar] [CrossRef] [PubMed]
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Hamanaka, R.B.; Mutlu, G.M. Particulate matter air pollution: Effects on the cardiovascular system. Front. Endocrinol. 2018, 9, 680. [Google Scholar] [CrossRef] [PubMed]
- Gómez-García, M.; Pitchon, V.; Kiennemann, A. Pollution by nitrogen oxides: An approach to NOx abatement by using sorbing catalytic materials. Environ. Int. 2005, 31, 445–467. [Google Scholar] [CrossRef]
- Amoatey, P.; Omidvarborna, H.; Baawain, M.S.; Al-Mamun, A. Emissions and exposure assessments of SOX, NOX, PM10/2.5 and trace metals from oil industries: A review study (2000–2018). Process Saf. Environ. Prot. 2019, 123, 215–228. [Google Scholar] [CrossRef]
- Chen, T.-M.; Kuschner, W.G.; Gokhale, J.; Shofer, S. Outdoor air pollution: Nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am. J. Med. Sci. 2007, 333, 249–256. [Google Scholar] [CrossRef]
- Chen, T.-M.; Kuschner, W.G.; Gokhale, J.; Shofer, S. Outdoor air pollution: Ozone health effects. Am. J. Med. Sci. 2007, 333, 244–248. [Google Scholar] [CrossRef]
- Geer, L.A.; Weedon, J.; Bell, M.L. Ambient air pollution and term birth weight in Texas from 1998 to 2004. J. Air Waste Manag. Assoc. 2012, 62, 1285–1295. [Google Scholar] [CrossRef]
- Zora, J.E.; Sarnat, S.E.; Raysoni, A.U.; Johnson, B.A.; Li, W.-W.; Greenwald, R.; Holguin, F.; Stock, T.H.; Sarnat, J.A. Associations between urban air pollution and pediatric asthma control in El Paso, Texas. Sci. Total Environ. 2013, 448, 56–65. [Google Scholar] [CrossRef]
- Montone, R.A.; Rinaldi, R.; Bonanni, A.; Severino, A.; Pedicino, D.; Crea, F.; Liuzzo, G. Impact of air pollution on ischemic heart disease: Evidence, mechanisms, clinical perspectives. Atherosclerosis 2023, 366, 22–31. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Hajat, S.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. Effects of air pollution on the incidence of myocardial infarction. Heart 2009, 95, 1746–1759. [Google Scholar] [CrossRef] [PubMed]
- Raziani, Y.; Raziani, S. The effect of air pollution on myocardial infarction. J. Chem. Rev. 2021, 3, 83–96. [Google Scholar]
- Lee, K.K.; Miller, M.R.; Shah, A.S. Air pollution and stroke. J. Stroke 2018, 20, 2. [Google Scholar] [CrossRef] [PubMed]
- Ljungman, P.L.; Mittleman, M.A. Ambient air pollution and stroke. Stroke 2014, 45, 3734–3741. [Google Scholar] [CrossRef]
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., III; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Guarnieri, M.; Balmes, J.R. Outdoor air pollution and asthma. Lancet 2014, 383, 1581–1592. [Google Scholar] [CrossRef]
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong-Neto, H.J.; Novakova, S.; Steiropoulos, P.; Kowal, K. Impact of air pollution on asthma outcomes. Int. J. Environ. Res. Public Health 2020, 17, 6212. [Google Scholar] [CrossRef]
- Ko, F.W.; Hui, D.S. Air pollution and chronic obstructive pulmonary disease. Respirology 2012, 17, 395–401. [Google Scholar] [CrossRef]
- Duan, R.-R.; Hao, K.; Yang, T. Air pollution and chronic obstructive pulmonary disease. Chronic Dis. Transl. Med. 2020, 6, 260–269. [Google Scholar] [CrossRef]
- Peters, R.; Peters, J.; Booth, A.; Mudway, I. Is air pollution associated with increased risk of cognitive decline? A systematic review. Age Ageing 2015, 44, 755–760. [Google Scholar] [CrossRef]
- Schikowski, T.; Altuğ, H. The role of air pollution in cognitive impairment and decline. Neurochem. Int. 2020, 136, 104708. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.-J.; Heinrich, J.; Bloom, M.S.; Zhao, T.-Y.; Shi, T.-X.; Feng, W.-R.; Sun, Y.; Shen, J.-C.; Yang, Z.-C.; Yang, B.-Y. Ambient air pollution and depression: A systematic review with meta-analysis up to 2019. Sci. Total Environ. 2020, 701, 134721. [Google Scholar] [CrossRef]
- Borroni, E.; Pesatori, A.C.; Bollati, V.; Buoli, M.; Carugno, M. Air pollution exposure and depression: A comprehensive updated systematic review and meta-analysis. Environ. Pollut. 2022, 292, 118245. [Google Scholar] [CrossRef] [PubMed]
- Jayaraj, R.L.; Rodriguez, E.A.; Wang, Y.; Block, M.L. Outdoor ambient air pollution and neurodegenerative diseases: The neuroinflammation hypothesis. Curr. Environ. Health Rep. 2017, 4, 166–179. [Google Scholar] [CrossRef] [PubMed]
- Armas, F.V.; D’Angiulli, A. Neuroinflammation and neurodegeneration of the central nervous system from air pollutants: A scoping review. Toxics 2022, 10, 666. [Google Scholar] [CrossRef]
- Wu, M.-Y.; Lo, W.-C.; Chao, C.-T.; Wu, M.-S.; Chiang, C.-K. Association between air pollutants and development of chronic kidney disease: A systematic review and meta-analysis. Sci. Total Environ. 2020, 706, 135522. [Google Scholar] [CrossRef]
- Tsai, H.-J.; Wu, P.-Y.; Huang, J.-C.; Chen, S.-C. Environmental pollution and chronic kidney disease. Int. J. Med. Sci. 2021, 18, 1121. [Google Scholar] [CrossRef]
- Chen, Y.; Cao, F.; Xiao, J.-P.; Fang, X.-Y.; Wang, X.-R.; Ding, L.-H.; Wang, D.-G.; Pan, H.-F. Emerging role of air pollution in chronic kidney disease. Environ. Sci. Pollut. Res. 2021, 28, 52610–52624. [Google Scholar] [CrossRef]
- Wu, X.; Gao, M. Effects of different environmental regulations and their heterogeneity on air pollution control in China. J. Regul. Econ. 2021, 60, 140–166. [Google Scholar] [CrossRef]
- Jbaily, A.; Zhou, X.; Liu, J.; Lee, T.-H.; Kamareddine, L.; Verguet, S.; Dominici, F. Air pollution exposure disparities across US population and income groups. Nature 2022, 601, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Colmer, J.; Hardman, I.; Shimshack, J.; Voorheis, J. Disparities in PM2. 5 air pollution in the United States. Science 2020, 369, 575–578. [Google Scholar] [CrossRef]
- Marquès, M.; Domingo, J.L.; Nadal, M.; Schuhmacher, M. Health risks for the population living near petrochemical industrial complexes. 2. Adverse health outcomes other than cancer. Sci. Total Environ. 2020, 730, 139122. [Google Scholar] [CrossRef]
- Williams, S.B.; Shan, Y.; Jazzar, U.; Kerr, P.S.; Okereke, I.; Klimberg, V.S.; Tyler, D.S.; Putluri, N.; Lopez, D.S.; Prochaska, J.D. Proximity to oil refineries and risk of cancer: A population-based analysis. JNCI Cancer Spectr. 2020, 4, pkaa088. [Google Scholar] [CrossRef] [PubMed]
- Danforth, C.G.; Portier, C.; Ensor, K.B.; Hopkins, L.; Evans, B.; Quist, A.J.; McGraw, K.E.; Craft, E. Development and demonstration of a data visualization platform of short-term guidelines for ambient air levels of benzene during disaster response in Houston, Texas. Integr. Environ. Assess. Manag. 2024, 20, 533–546. [Google Scholar] [CrossRef]
- Peckham-Gregory, E.C.; Ton, M.; Rabin, K.R.; Danysh, H.E.; Scheurer, M.E.; Lupo, P.J. Maternal residential proximity to major roadways and the risk of childhood acute leukemia: A population-based case-control study in Texas, 1995–2011. Int. J. Environ. Res. Public Health 2019, 16, 2029. [Google Scholar] [CrossRef]
- Siddiqua, A.; Hahladakis, J.N.; Al-Attiya, W.A.K. An overview of the environmental pollution and health effects associated with waste landfilling and open dumping. Environ. Sci. Pollut. Res. 2022, 29, 58514–58536. [Google Scholar] [CrossRef]
- Symanski, E.; Whitworth, K.W.; Han, I.; Rammah, A.; Alvarez, J.; Moussa, I.; Han, H.A.; Flores, J. Assessing Metal Exposures Among Children Living in Environmental Justice Communities Near Metal Recycling Facilities in Houston, Texas. Environ. Justice 2024, 17, 128–142. [Google Scholar] [CrossRef]
- Symanski, E.; Whitworth, K.W.; Mendez-Figueroa, H.; Aagaard, K.M.; Moussa, I.; Alvarez, J.; Chardon Fabian, A.; Kannan, K.; Walker, C.L.; Coarfa, C. The Maternal and Infant Environmental Health Riskscape study of perinatal disparities in greater Houston: Rationale, study design and participant profiles. Front. Reprod. Health 2024, 6, 1304717. [Google Scholar] [CrossRef]
- Park, K.; Jin, H.-G.; Baik, J.-J. Do heat waves worsen air quality? A 21-year observational study in Seoul, South Korea. Sci. Total Environ. 2023, 884, 163798. [Google Scholar] [CrossRef]
- Nnoli, N.C.; Linder, S.H.; Smith, M.A.; Gemeinhardt, G.L.; Zhang, K. The combined effect of ambient ozone exposure and toxic air releases on hospitalization for asthma among children in Harris County, Texas. Int. J. Environ. Health Res. 2018, 28, 358–378. [Google Scholar] [CrossRef] [PubMed]
- Rammah, A.; Whitworth, K.W.; Symanski, E. Particle air pollution and gestational diabetes mellitus in Houston, Texas. Environ. Res. 2020, 190, 109988. [Google Scholar] [CrossRef] [PubMed]
- Botlaguduru, V.S.; Kommalapati, R.R.; Huque, Z. Long-term meteorologically independent trend analysis of ozone air quality at an urban site in the greater Houston area. J. Air Waste Manag. Assoc. 2018, 68, 1051–1064. [Google Scholar] [CrossRef]
- Michael, R.; O’Lenick, C.R.; Monaghan, A.; Wilhelmi, O.; Wiedinmyer, C.; Hayden, M.; Estes, M. Application of geostatistical approaches to predict the spatio-temporal distribution of summer ozone in Houston, Texas. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 806–820. [Google Scholar] [CrossRef]
- Sofia, D.; Lotrecchiano, N.; Giuliano, A.; Barletta, D.; Poletto, M. Optimization of Number and Location of Sampling Points of an Air Quality Monitoring Network in an Urban Contest. Chem. Eng. Trans. 2019, 74, 277–282. [Google Scholar]
- Zhang, S.; Liu, H.; Tang, N.; Ali, N.; Yu, J.; Ding, B. Highly Efficient, Transparent, and Multifunctional Air Filters Using Self-Assembled 2D Nanoarchitectured Fibrous Networks. ACS Nano 2019, 13, 13501–13512. [Google Scholar] [CrossRef] [PubMed]
- Lyu, C.; Zhao, P.; Xie, J.; Dong, S.; Liu, J.; Rao, C.; Fu, J. Electrospinning of Nanofibrous Membrane and Its Applications in Air Filtration: A Review. Nanomaterials 2021, 11, 1501. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Oh, S.; Park, J.-E.; Hwang, J.; Eom, H. Scalable, solvent-free transparent film-based air filter with high particulate matter 2.5 filtration efficiency. Sci. Total Environ. 2023, 895, 165197. [Google Scholar] [CrossRef]
- Mukherjee, F.; Singh, D. Detecting flood prone areas in Harris County: A GIS based analysis. GeoJournal 2020, 85, 647–663. [Google Scholar] [CrossRef]
- Dey, H.; Shao, W.; Haque, M.M.; VanDyke, M. Enhancing flood risk analysis in Harris County: Integrating flood susceptibility and social vulnerability mapping. J. Geovis. Spat. Anal. 2024, 8, 19. [Google Scholar] [CrossRef]
- Adepoju, O.E.; Han, D.; Chae, M.; Smith, K.L.; Gilbert, L.; Choudhury, S.; Woodard, L. Health disparities and climate change: The intersection of three disaster events on vulnerable communities in Houston, Texas. Int. J. Environ. Res. Public Health 2021, 19, 35. [Google Scholar] [CrossRef] [PubMed]
- City of Houston, Department of Neighborhoods, Super Neighborhoods. Available online: https://www.houstontx.gov/superneighborhoods/ (accessed on 12 May 2025).
- Houston Complete Communities. Available online: https://www.houstoncc.org/ (accessed on 12 May 2025).
- U.S. Census Bureau. (n.d.). American Community Survey 5-Year Estimates U.S. Department of Commerce 2025. Available online: https://catalog.data.gov/dataset/american-community-survey-5-year-estimates-detailed-tables-5-year-155db (accessed on 12 May 2025).
- Centers for Disease Control and Prevention (CDC). Available online: https://www.atsdr.cdc.gov/place-health/php/svi/index.html (accessed on 12 May 2025).
- EPA AirData Air Quality Monitors. Available online: https://epa.maps.arcgis.com/apps/webappviewer/index.html?id=5f239fd3e72f424f98ef3d5def547eb5&extent=-146.2334,13.1913,-46.3896,56.5319 (accessed on 12 May 2025).
- Centers for Disease Control and Prevention. PLACES: Local Data for Better Health. U.S. Department of Health and Human Services. 2024. Available online: https://www.cdc.gov/places (accessed on 12 May 2025).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khalili, A.; Vines, W.E.; Rifai, H.S. A Place-Based County-Level Study of Air Quality and Health in Urban Communities. Sustainability 2025, 17, 5368. https://doi.org/10.3390/su17125368
Khalili A, Vines WE, Rifai HS. A Place-Based County-Level Study of Air Quality and Health in Urban Communities. Sustainability. 2025; 17(12):5368. https://doi.org/10.3390/su17125368
Chicago/Turabian StyleKhalili, Ainaz, William E. Vines, and Hanadi S. Rifai. 2025. "A Place-Based County-Level Study of Air Quality and Health in Urban Communities" Sustainability 17, no. 12: 5368. https://doi.org/10.3390/su17125368
APA StyleKhalili, A., Vines, W. E., & Rifai, H. S. (2025). A Place-Based County-Level Study of Air Quality and Health in Urban Communities. Sustainability, 17(12), 5368. https://doi.org/10.3390/su17125368




