The Role of Evidence-Based Management in Driving Sustainable Innovation in Saudi Arabian Healthcare Systems
Abstract
1. Introduction
1.1. Background
1.2. Significance of the Study
1.3. Literature Review
1.4. Research Gap
1.4.1. Research Hypothesis
1.4.2. Research Objectives
- Research the level of influence EBM has on healthcare cost-efficiency throughout Saudi Arabia.
- Analyze EBM’s influence on healthcare access fairness along with the population group’s latest techniques.
- Conduct statistical analysis explores the connection between the implementation of EBM along with sustainability of healthcare services.
- Create a framework for EBM implementation according to Saudi Arabia’s existing healthcare operational challenges.
1.5. Contribution
2. Materials and Methods
2.1. Study Design
2.2. Population and Sampling
2.2.1. Population
2.2.2. Sample Characteristics
- Region: The participants were mainly from Riyadh (43.8%), with the rest coming from other areas of the Kingdom (31.3%). The Eastern Province accounted for 12.5%, while Medina and Mecca accounted for 6.3% each.
- Workplace Settings: The participants were employed in hospitals (31.3%), health centers (18.8%), and other medical facilities (50%), so it is reasonable to expect a variety of organizational cultures.
- Job Positions: The highest proportion of respondents (56.3%) fell under the “other” roles; 25% were department heads, and 18.8% were managers.
- Gender: 62.5% of the sample were male, while 37.5% were female.
- Age Distribution: The largest age group was between 41 and 50 (56.3%), 25% of the participants were between 31 and 40, and 18.8% were 51 years and above.
2.2.3. Sampling Technique
2.3. Variables and Measurement Instruments
2.3.1. Independent Variables (EBM Practices)
- Integration of research findings into clinical decisions.
- Medical institutions employ data analytics for resource management purposes.
- The role of evidence in strategic decision-making.
2.3.2. Dependent Variables
- Cost efficiency is a measurement tool that uses resource utilization rates and cost-savings metrics for evaluation.
- Equity is measured through the Equity in Healthcare Index (EHI) to determine how equal accessibility to healthcare affects different socioeconomic and demographic groups.
- The research used the Healthcare Access Index for accessibility measurements because it includes waiting time data and examines service availability alongside coverage for marginalized populations.
- The evaluation of sustainable practices involves environmental impact assessment in addition to resource conservation programs that follow Sustainable Development Goals (SDGs) in healthcare.
2.4. Data Collection Methods
2.4.1. Hybrid Surveys
- Professionals responded to EBM adoption questions through Likert-type survey items. The full list of survey items is provided in Appendix A.
- The survey includes open-ended questions that ask for qualitative data about the obstacles and opportunities related to EBM implementation and strategic decision-making effects. The research method enabled the collection of statistical and narrative data to be analyzed afterward.
2.4.2. AI-Moderated Focus Groups
2.4.3. Digital Ethnography
2.4.4. Experience Sampling Method (ESM)
2.5. Data Analysis Techniques
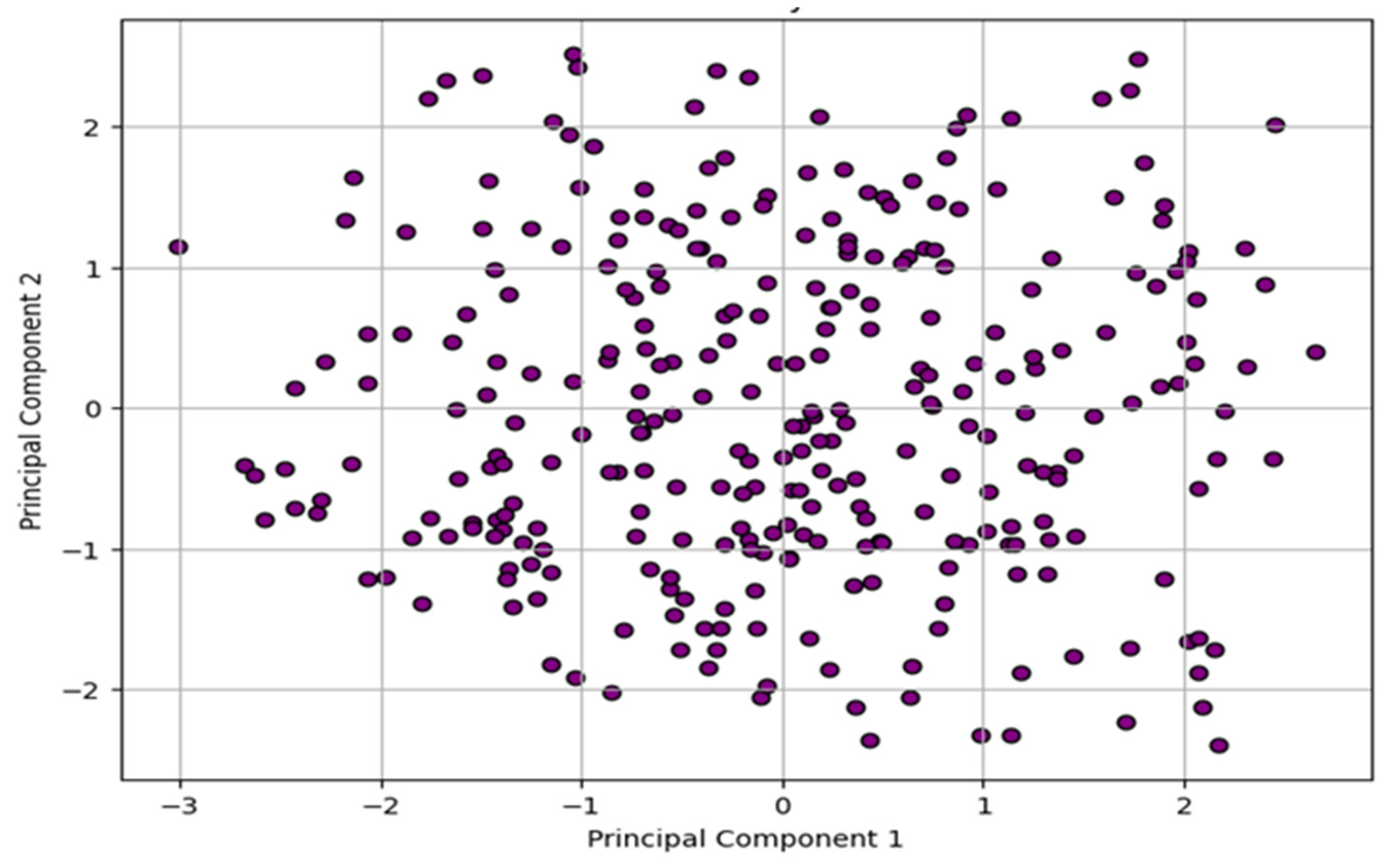
2.5.1. Latent Semantic Analysis (LSA)
2.5.2. Structural Equation Modeling (SEM)
2.5.3. Predictive Models (XGBoost and Explainable AI)
2.5.4. Multivariate Statistical Analysis: Dynamic Network Analysis (DNA)
2.5.5. Time-Series Analysis
2.6. Ethical Considerations
- Informed Consent: The participants were informed of the study’s purpose, told they would be assigned a code number, and told their details would not be disclosed to any other party.
- Data Security: All the collected data, including completed survey questionnaires, focus group recordings, and field notes, were kept secure and de-identified.
2.7. Validity and Reliability
2.7.1. Reliability
2.7.2. Validity
3. Results and Discussions
4. Discussion
5. Conclusions
6. Limitations
7. Future Research Directions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- Survey Questionnaire
- The following items were used in the survey, grouped by construct:
- Evidence-Based Management Practices
- Our organization integrates published research into managerial decisions.
- We use data analytics to support strategic choices.
- Managers receive training in evidence-based approaches.
- There is a culture of relying on facts and evidence over intuition.
- Cost Efficiency
- Our organization regularly reviews operations to minimize waste.
- We have implemented cost-saving technologies or practices.
- Equity
- Services are equally accessible to all socioeconomic groups.
- We track service provision across diverse population segments.
- Accessibility
- Patients can easily access services without long delays.
- We offer services via remote and telehealth platforms.
- Sustainability
- We implement green and environmentally friendly healthcare practices.
- Sustainability is a key factor in organizational planning.
- (All items rated on a 5-point Likert scale: 1 = Strongly Disagree to 5 = Strongly Agree.)
References
- Janati, A.; Hasanpoor, E.; Hajebrahimi, S.; Sadeghi-Bazargani, H.; Khezri, A. An Evidence-Based Framework for Evidence-Based Management in Healthcare Organizations: A Delphi Study. Ethiop. J. Health Sci. 2018, 28, 305–314. [Google Scholar] [CrossRef]
- Viswanadham, N. Ecosystem model for healthcare platform. Sādhanā 2021, 46, 188. [Google Scholar] [CrossRef]
- Dusin, J.; Melanson, A.; Mische-Lawson, L. Evidence-based practice models and frameworks in the healthcare setting: A scoping review. BMJ Open 2023, 13, e071188. [Google Scholar] [CrossRef] [PubMed]
- Hulpke, J.F.; Fronmueller, M.P. What’s not to like about evidence-based management: A hyper-rational fad? Int. J. Organ. Anal. 2022, 30, 95–123. [Google Scholar] [CrossRef]
- Kraus, S.; Schiavone, F.; Pluzhnikova, A.; Invernizzi, A.C. Digital transformation in healthcare: Analyzing the current state-of-research. J. Bus. Res. 2021, 123, 557–567. [Google Scholar] [CrossRef]
- Välimäki, M.; Hu, S.; Lantta, T.; Hipp, K.; Varpula, J.; Chen, J.; Liu, G.; Tang, Y.; Chen, W.; Li, X. The impact of evidence-based nursing leadership in healthcare settings: A mixed methods systematic review. BMC Nurs. 2024, 23, 452. [Google Scholar] [CrossRef]
- Huebner, C.; Flessa, S. Strategic Management in Healthcare: A Call for Long-Term and Systems-Thinking in an Uncertain System. Int. J. Environ. Res. Public Health 2022, 19, 8617. [Google Scholar] [CrossRef]
- Alfahad, A.H.; Alabbas, Y.S.; ALabbas, H.S.M.; Abukhashbah, T.H.; Alabdali, A.A.; Alfatieh, Q.M.H.; Bashawri, E.A.; Hadidi, H.T.H.; Junaid, R.M.A.; Alhazmi, K.M.A. Evaluating the Impact of Saudi Vision 2030 on Healthcare Investment: A Comprehensive Review of Progress and Future Directions. J. Ecohumanism 2024, 3, 870–880. [Google Scholar] [CrossRef]
- Kujala, J.; Sachs, S.; Leinonen, H.; Heikkinen, A.; Laude, D. Stakeholder Engagement: Past, Present, and Future. Bus. Soc. 2022, 61, 1136–1196. [Google Scholar] [CrossRef]
- Bärnreuther, S. Disrupting healthcare? Entrepreneurship as an “innovative” financing mechanism in India’s primary care sector. Soc. Sci. Med. 2023, 319, 115314. [Google Scholar] [CrossRef]
- Hussain, A.; Umair, M.; Khan, S.; Alonazi, W.B.; Almutairi, S.S.; Malik, A. Exploring sustainable healthcare: Innovations in health economics, social policy, and management. Heliyon 2024, 10, e33186. [Google Scholar] [CrossRef] [PubMed]
- Al Shahrani, A.M.; Rizwan, A.; Sánchez-Chero, M.; Rosas-Prado, C.E.; Salazar, E.B.; Awad, N.A. An internet of things (IoT)-based optimization to enhance security in healthcare applications. Math. Probl. Eng. 2022, 2022, 6802967. [Google Scholar] [CrossRef]
- Alghassab, M. A Computational Case Study on Sustainable Energy Transition in the Kingdom of Saudi Arabia. Energies 2023, 16, 5133. [Google Scholar] [CrossRef]
- Alasiri, A.A.; Mohammed, V. Healthcare Transformation in Saudi Arabia: An Overview Since the Launch of Vision 2030. Health Serv. Insights 2022, 15, 11786329221121214. [Google Scholar] [CrossRef]
- Ahmad Ghaus, M.G.; Tuan Kamauzaman, T.H.; Norhayati, M.N. Knowledge, Attitude, and Practice of Evidence-Based Medicine among Emergency Doctors in Kelantan, Malaysia. Int. J. Environ. Res. Public Health 2021, 18, 11297. [Google Scholar] [CrossRef]
- Gurajala, S. Healthcare System in the Kingdom of Saudi Arabia: An Expat Doctor’s Perspective. Cureus 2023, 15, e38806. [Google Scholar] [CrossRef] [PubMed]
- Alojail, M.; Alturki, M.; Bhatia Khan, S. An Informed Decision Support Framework from a Strategic Perspective in the Health Sector. Information 2023, 14, 363. [Google Scholar] [CrossRef]
- Shortell, S.M.; Rundall, T.G.; Hsu, J. Improving patient care by linking evidence-based medicine and evidence-based management. JAMA 2007, 298, 673–676. [Google Scholar] [CrossRef]
- Tomlinson, M.; Ward, C.L.; Marlow, M. Improving the efficiency of evidence-based interventions: The strengths and limitations of randomised controlled trials. S. Afr. Crime Q. 2015, 51. [Google Scholar] [CrossRef]
- Kochetkov, E.P.; Zabavina, A.A.; Gafarov, M.G. Digital Transformation of Companies as a Tool of Crisis Management: Ð N Empirical Research of The Impact on Efficiency. Strateg. Decis. Risk Manag. Real Econ. Publ. House 2021, 12, 68–81. [Google Scholar] [CrossRef]
- Rapp, C.A.; Etzel-Wise, D.; Marty, D.; Coffman, M.; Carlson, L.; Asher, D.; Callaghan, J.; Holter, M. Barriers to evidence-based practice implementation: Results of a qualitative study. Community Ment. Health J. 2010, 46, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Molero, A.; Calabrò, M.; Vignes, M.; Gouget, B.; Gruson, D. Sustainability in Healthcare: Perspectives and Reflections Regarding Laboratory Medicine. Ann. Lab. Med. 2021, 41, 139–144. [Google Scholar] [CrossRef]
- Li, T.; Zhang, H.; Yuan, C.; Liu, Z.; Fan, C. PCA-Based Method for Construction of Composite Sustainability Indicators. Int. J. Life Cycle Assess. 2012, 17, 593–603. [Google Scholar] [CrossRef]
- Rathobei, K.E.; Ranängen, H.; Lindman, Å. Stakeholder integration in sustainable business models to enhance value delivery for a broader range of stakeholders. Bus. Strat. Environ. 2024, 33, 3687–3706. [Google Scholar] [CrossRef]
- Ajoud, M.E.K.; Ibrahim, A.I.H. The impact of Sustainability Practices on Healthcare Institutions: Evidence from Public Healthcare Institutions in Saudi Arabia. Eur. J. Sustain. Dev. 2024, 13, 379. [Google Scholar] [CrossRef]
- Ratnani, I.; Fatima, S.; Abid, M.M.; Surani, Z.; Surani, S. Evidence-Based Medicine: History, Review, Criticisms, and Pitfalls. Cureus 2023, 15, e35266. [Google Scholar] [CrossRef]
- Alsulami, H.; Serbaya, S.H.; Rizwan, A.; Saleem, M.; Maleh, Y.; Alamgir, Z. Impact of emotional intelligence on the stress and safety of construction workers’ in Saudi Arabia. Eng. Constr. Archit. Manag. 2023, 30, 1365–1378. [Google Scholar] [CrossRef]
- D’Adamo, I.; Gastaldi, M.; Morone, P. Economic sustainable development goals: Assessments and perspectives in Europe. J. Clean. Prod. 2022, 354, 131730. [Google Scholar] [CrossRef]
- McCaughey, D.; Bruning, N.S. Rationality versus reality: The challenges of evidence-based decision making for health policy makers. Implement. Sci. 2010, 5, 39. [Google Scholar] [CrossRef]
- Roshanghalb, A.; Lettieri, E.; Aloini, D.; Cannavacciuolo, L.; Gitto, S.; Visintin, F. What evidence on evidence-based management in healthcare? Manag. Decis. 2018, 56, 2069–2084. [Google Scholar] [CrossRef]
- Nurjono, M.; Shrestha, P.; Ang, I.Y.H.; Shiraz, F.; Eh, K.X.; Toh, S.-A.E.S.; Vrijhoef, H.J.M. Shifting care from hospital to community, a strategy to integrate care in Singapore: Process evaluation of implementation fidelity. BMC Health Serv. Res. 2020, 20, 452. [Google Scholar] [CrossRef] [PubMed]
- Johnston, B.M.; Burke, S.; Kavanagh, P.M.; O’Sullivan, C.; Thomas, S.; Parker, S. Moving beyond formulae: A review of international population-based resource allocation policy and implications for Ireland in an era of healthcare reform. HRB Open Res. 2021, 4, 121. [Google Scholar] [CrossRef]










| Count | Mean | Std | Min | 25% | 50% | 75% | Max | |
|---|---|---|---|---|---|---|---|---|
| Cost Efficiency | 300 | 2.883567 | 1.177682 | 1 | 1.78 | 2.87 | 3.895 | 5 |
| Equity | 300 | 2.9966 | 1.17267 | 1 | 2.085 | 2.885 | 4.1225 | 5 |
| Accessibility | 300 | 2.9479 | 1.07037 | 1.03 | 2.0575 | 3.025 | 3.8 | 5 |
| Sustainability | 300 | 3.057 | 1.158002 | 1.01 | 2.1425 | 3.18 | 3.9925 | 4.99 |
| Implementation Challenges | 300 | |||||||
| Stakeholder Engagement | 300 | 2.926967 | 1.173807 | 1 | 1.9875 | 2.885 | 4.0125 | 4.99 |
| Decision Outcome Rating | 300 | 2.976 | 1.179587 | 1.03 | 1.8925 | 2.92 | 3.9875 | 4.97 |
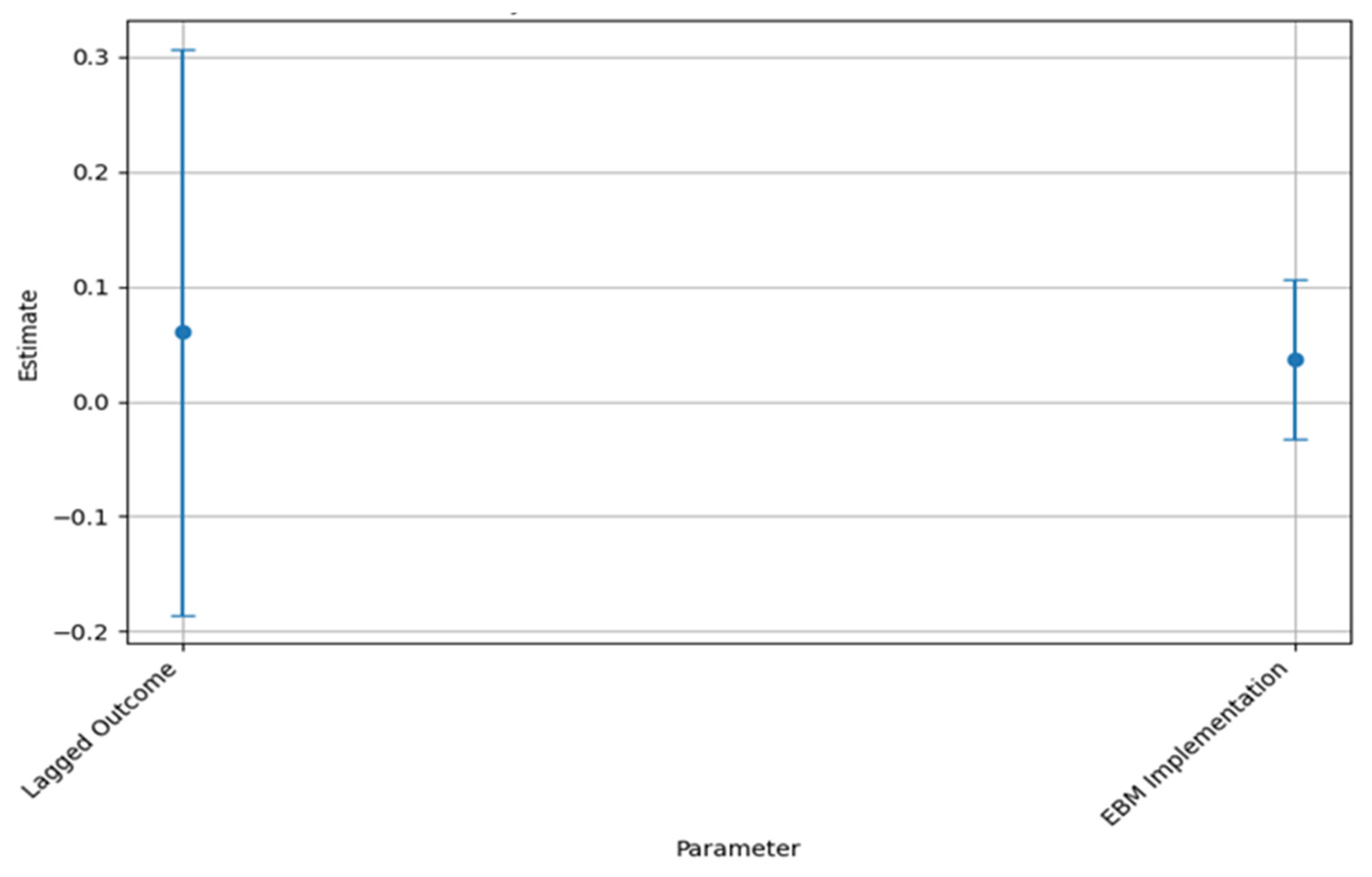
| Local | rval | Estimate | Std. Err | z-Value | p-Value |
|---|---|---|---|---|---|
| Equity | EBMAdoption | 0.001156 | 0.056963 | 0.020302 | 0.02838 |
| Accessibility | EBMAdoption | 0.002668 | 0.057501 | 0.046391 | 0.0163 |
| CostEfficiency | EBMAdoption | 0.022284 | 0.056522 | 0.394259 | 0.029339 |
| Sustainability | Equity | −0.0592 | 0.059105 | −1.00167 | 0.016504 |
| Sustainability | Accessibility | −0.06328 | 0.058551 | −1.08069 | 0.027984 |
| Accessibility | Accessibility | 1.340408 | 0.109444 | 12.24745 | 0 |
| Equity | Equity | 1.315428 | 0.107404 | 12.24745 | 0 |
| CostEfficiency | CostEfficiency | 1.295144 | 0.105748 | 12.24745 | 0 |
| Sustainability | Sustainability | 1.37858 | 0.112561 | 12.24745 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almoajel, A.M. The Role of Evidence-Based Management in Driving Sustainable Innovation in Saudi Arabian Healthcare Systems. Sustainability 2025, 17, 4352. https://doi.org/10.3390/su17104352
Almoajel AM. The Role of Evidence-Based Management in Driving Sustainable Innovation in Saudi Arabian Healthcare Systems. Sustainability. 2025; 17(10):4352. https://doi.org/10.3390/su17104352
Chicago/Turabian StyleAlmoajel, Alia Mohammed. 2025. "The Role of Evidence-Based Management in Driving Sustainable Innovation in Saudi Arabian Healthcare Systems" Sustainability 17, no. 10: 4352. https://doi.org/10.3390/su17104352
APA StyleAlmoajel, A. M. (2025). The Role of Evidence-Based Management in Driving Sustainable Innovation in Saudi Arabian Healthcare Systems. Sustainability, 17(10), 4352. https://doi.org/10.3390/su17104352







