Health Impacts of Urban Environmental Parameters: A Review of Air Pollution, Heat, Noise, Green Spaces and Mobility
Abstract
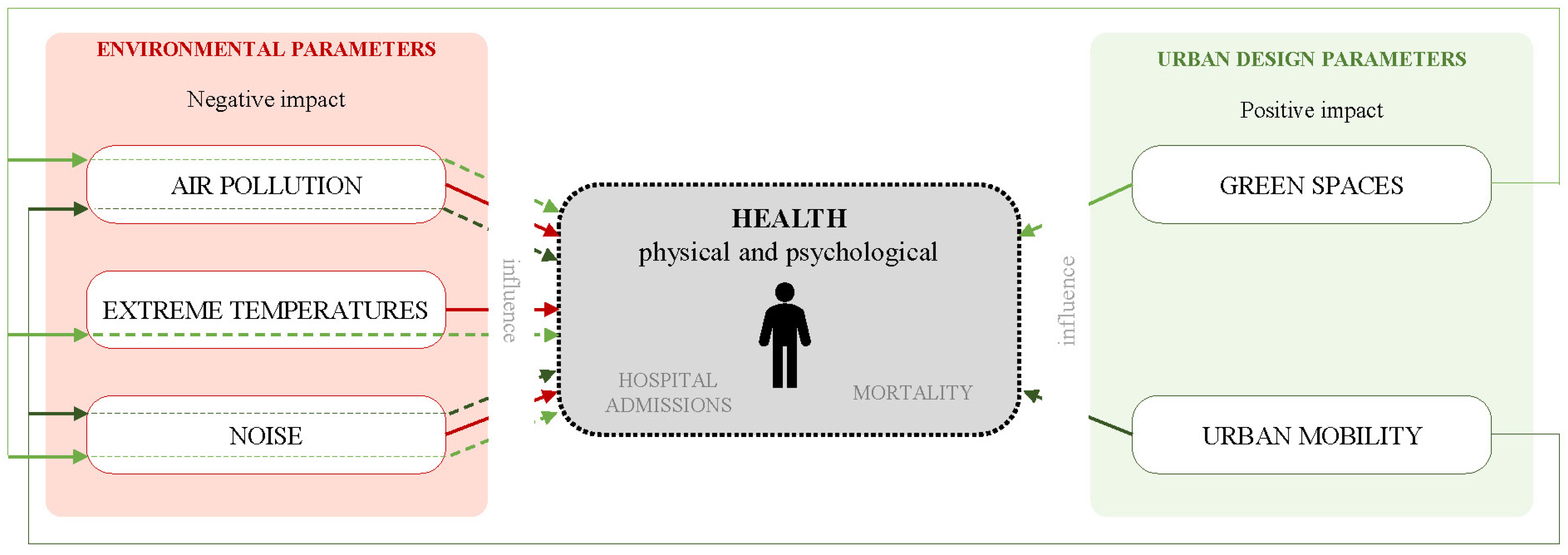
1. Introduction
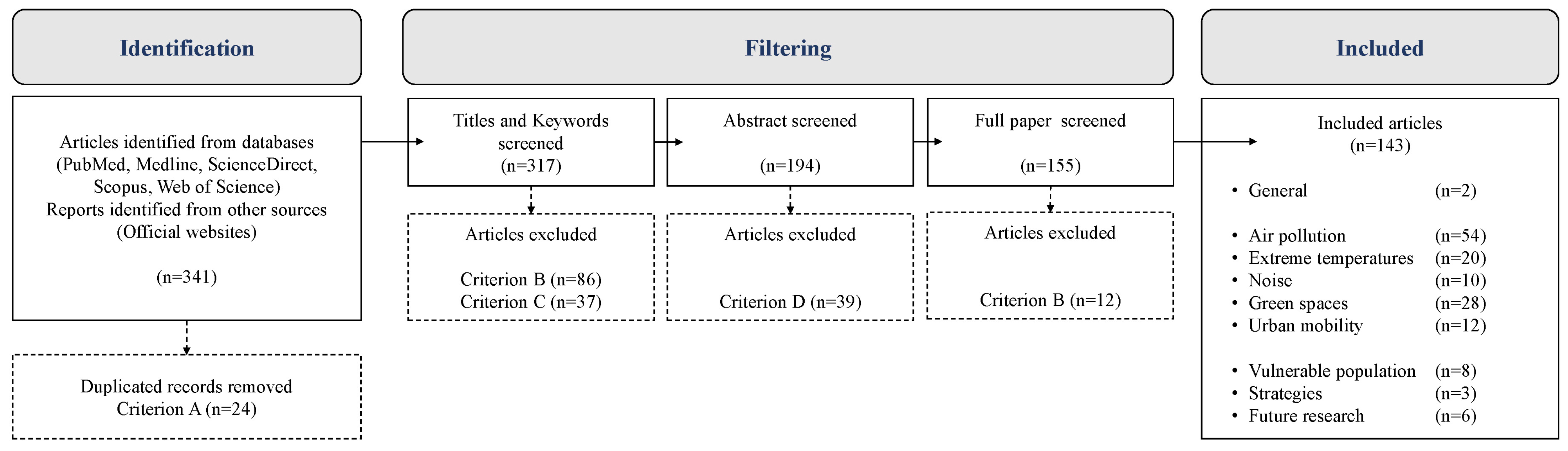
2. Materials and Methods
- Removal of duplicates
- Unavailability or incomprehension: publications that are inaccessible due to unavailability, language barriers, or incomprehensibility, as well as those removed due to plagiarism, are excluded.
- Thematic relevance: publications that analyze the impacts of the studied parameters on other fields but do not specifically focus on health were excluded.
- Type of results: studies reporting exclusively qualitative outcomes were excluded to maintain consistency in the assessment of health impacts across the different parameters. This criterion prioritizes studies that report quantifiable outcomes (e.g., morbidity rates, mortality rates, hospital admissions), facilitating comparative synthesis and supporting data-driven urban planning and health policy development.
3. Results
3.1. Negative Impact of Environmental Parameters on Health
3.1.1. Air Pollution
3.1.2. High Temperature
3.1.3. Noise
| Parameter | Respiratory System | Cardiovascular System | Nervous System | Reproductive System | Excretory System | Others |
|---|---|---|---|---|---|---|
| Air pollution | Respiratory infections, cystic fibrosis, emphysema, and lung cancer [6,7,8]. Carcinogenesis, teratogenesis, and mutagenesis [9]. Intracellular calcium and inflammatory processes that may result in apoptosis or necrosis [10]. COPD, asthma, and complications in lung development in children [12,13]. | Myocardial infarctions [14]. Endothelial dysfunction, platelet activation, and systemic inflammation, which are associated with a wide range of cardiovascular diseases, such as arrhythmias, ischemia, hypertension, and atherosclerosis [7]. | Oxidative stress and neuroinflammation [15,16]. Stroke [15,19]. Neurodegeneration [29,30,35,36]. Declines in cognitive function in older adults [20,21]. | Decreased fertility [37,38,40,41]. Decreased sperm quality [30,31]. Increased birthing complications [7,34]. Reducing pregnancy rates in the in vitro treatments [28,32,33]. Altering the placental exchange, impacting umbilical blood flow and the transport of oxygen and essential nutrients for fetal growth and development [34,35]. Cleft palate, cleft lip, and congenital heart defects have been observed in newborns exposed to high levels of pollutants like O3 [39,40]. Decrease in respiratory volume by up to 2.7% with a 10 µg/m3 increase in NO2 concentration (children at 4.5 years of age) [41]. | Kidney damage, including tubular dysfunction, reduced glomerular filtration rate, and an increased risk of kidney stones and renal cancer [10]. Developing ulcers and cancer in this system in older individuals [42]. | Depressive behaviors [22]. Increasingly triggering a variety of allergies [43]. |
| High temperatures | - | Heat stroke, cardiovascular problems and decompensation [55]. Increased heart rate and blood pressure [57]. | - | - | - | Confusion, dizziness, nausea, red and hot skin, rapid pulse, and loss of consciousness, as well as minor ailments like cramps or dehydration [56]. Impact sleep quality, causing difficulty falling asleep and less restorative sleep, leading to long-term negative health consequences [58]. Mental performance, decreasing attention, memory, and decision-making ability during periods of extreme heat [59]. |
| Noise | - | Temporary increases in blood pressure, heart rate, and vasoconstriction (above 65 dB) [77]. | - | - | - | Loss of sensory cells in the cochlea, which do not regenerate (>85 dB) [72]. |
3.2. Positive Impact of Urban Design Parameters on Health
3.2.1. Green Spaces
3.2.2. Sustainable Urban Mobility
| Parameter | Direct Impact | Indirect | ||
|---|---|---|---|---|
| Air Pollution | High Temperatures | Noise | ||
| Green areas | Reduced stress [84,85]. Reduced anxiety and depression [86,87]. Improved mood [88,89]. Fostering social interactions, especially among older adults [90] and children [91,92]. Encourage physical activities [93]; therefore, reducing obesity [94] and lowering risks associated with type 2 diabetes [95]. Reduced cardiovascular mortality [96,97]. Reduction in stroke [98]. | Decrease primary PM10 concentrations by 10% by increasing vegetation coverage from 3.5% to 16.5% in an urban area [100]. Population in city areas with more green space had 1.68% fewer hospital admissions than the downtown population, linking these results to a reduction in PM10 (21 major US cities) [103]. Each 10 μm/m3 increase in PM2.5 was associated with a 0.99% increase in total hospitalizations for cardiovascular diseases, while in areas with more green space, the increase in hospitalizations for cardiovascular diseases was 0.45% (Wuhan, China) [104]. | Increasing urban vegetation coverage from 15% to 33% could reduce heat-related mortality rates by between 5% and 28% (Central Melbourne, Australia) [106]. 2644 premature deaths could be prevented by increasing city tree cover to 30% (93 European cities) [108]. | Natural barriers can disperse and mitigate traffic noise, improving environmental quality and the livability of urban spaces [110]. |
| Sustainable urban mobility | Can increase weekly physical activity minutes per person by more than 16%, leading to notable improvements in cardiovascular health and reduced obesity [116]. Lower stress levels and better psychological well-being [118]. | Reducing CO2 emissions: the motor vehicle traffic was reduced by 30.1% in the city and 70% in the city center, show that walking has increased by 67% and emissions have been reduced to 500 kg of CO2 per person per year (Pontevedra, Spain) [120]. | - | Reduces the number of private vehicles on the roads and, therefore, noise [121]. Promotion of electric and autonomous vehicles offers a notable reduction in noise, as these vehicles are much quieter than internal combustion vehicles [122]. |
4. Discussion
| Pollutant | European Regulation [124] | WHO Guidelines [123] |
|---|---|---|
| Sulfur dioxide (SO2) | 125 μg/m3 24-h concentration | 40 µg/m3 24-h concentration (i.e., 3–4 exceedance days per year) |
| Nitrogen dioxide (NO2) | 40 μg/m3 annual concentration | 10 µg/m3 annual concentration 25 µg/m3 24-h concentration (i.e., 3–4 exceedance days per year) |
| Ozone (O3) | 120 μg/m3 24-h concentration | 100 µg/m3 8-h concentration (i.e., 3–4 exceedance days per year) |
| Carbon monoxide (CO) | 10 μg/m3 24-h concentration | 4 µg/m3 24-h concentration (i.e., 3–4 exceedance days per year) |
| Particulate matter (PM10 y PM2.5) | PM10: 40 μg/m3 annual concentration PM2.5: 20 μg/m3 annual concentration | PM10: 15 µg/m3 annual concentration 45 µg/m3 24-h concentration (i.e., 3–4 exceedance days per year) PM2.5: 5 µg/m3 annual concentration 15 µg/m3 24-h concentration (i.e., 3–4 exceedance days per year) |
| Metals (Pb, As, Cd, Ni) | Pb: 10 μg/m3; As: 6 ng/m3; Cd: 5 ng/m3; Ni: 20 ng/m3 | - |
| Organic gases (C6H6, B(a)P) | C6H6: 5 μg/m3 | - |
- The first action is to renaturalize cities. This involves transforming unused urban spaces, such as courtyards or squares, into green areas and parks, promoting green roofs, reducing the use of asphalt and concrete, and implementing sustainable drainage systems. Additionally, it encourages planting trees, developing river parks, and creating green corridors for pedestrians and cyclists. It is essential to select tree species that are appropriate for the local climate, avoiding issues like allergies or excessive water demands, and promoting biodiversity to enhance ecological resilience.
- For example, the Montreal (Canada) case study where the 3-30-300 rule is evaluated [133].
- The second action is to promote sustainable mobility. This can be achieved by encouraging active transportation through the concept of “15-min cities,” where essential services are within walking or cycling distance. It also includes pedestrianizing streets, developing bicycle lanes, reducing speed for traffic in some urban zones, investing in efficient and sustainable public transport, improving traffic management, and promoting the use of sustainable vehicles. This can be supported by offering incentives for the purchase of electric vehicles, developing charging infrastructure, and establishing low-emission zones with restrictions for polluting vehicles.
- For Example, the Plan Vélo in Paris, which has implemented more than 1000 km of bike lanes, has achieved a significant reduction in car use and an improvement in active mobility in the city [134]. And the superblock plan in Barcelona, an innovative urban planning and transport strategy aimed at reclaiming public space for people, has reduced motorized traffic and improved both health and urban quality of life [135].
- The third action focuses on promoting management and education tools. This includes the development of a geographic information system (GIS)-based tool, to diagnose specific urban problems and apply solutions effectively. It also involves monitoring air pollution and temperatures to evaluate and adjust the implemented measures. Promoting epidemiological studies to assess the impact of these actions on public health is also crucial. Finally, educating and raising awareness among all stakeholders, from policymakers to citizens, about the benefits of these measures for public health is essential for their success.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Organización Mundial de la Salud Cada Año Mueren 12,6 Millones de Personas a Causa de La Insalubridad Del Medio Ambiente. Available online: https://www.who.int/es/news/item/15-03-2016-an-estimated-12-6-million-deaths-each-year-are-attributable-to-unhealthy-environments (accessed on 23 May 2024).
- Ritchie, H.; Roser, M. Urbanization-Our World in Data. Available online: https://ourworldindata.org/urbanization#what-share-of-people-will-live-in-urban-areas-in-the-future (accessed on 20 February 2024).
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- WHO. Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease; Inis Communication: Geneva, Switzerland, 2016; ISBN 9783241511353. [Google Scholar]
- Lelieveld, J.; Klingmüller, K.; Pozzer, A.; Pöschl, U.; Fnais, M.; Daiber, A.; Münzel, T. Cardiovascular Disease Burden from Ambient Air Pollution in Europe Reassessed Using Novel Hazard Ratio Functions. Eur. Heart J. 2019, 40, 1590–1596. [Google Scholar] [CrossRef] [PubMed]
- Goss, C.H.; Newsom, S.A.; Schildcrout, J.S.; Sheppard, L.; Kaufman, J.D. Effect of Ambient Air Pollution on Pulmonary Exacerbations and Lung Function in Cystic Fibrosis. Am. J. Respir. Crit. Care Med. 2004, 169, 816–821. [Google Scholar] [CrossRef] [PubMed]
- Rückerl, R.; Schneider, A.; Breitner, S.; Cyrys, J.; Peters, A. Health Effects of Particulate Air Pollution: A Review of Epidemiological Evidence. Inhal. Toxicol. 2011, 23, 555–592. [Google Scholar] [CrossRef]
- Xing, Y.F.; Xu, Y.H.; Shi, M.H.; Lian, Y.X. The Impact of PM2.5 on the Human Respiratory System. J. Thorac. Dis. 2016, 8, E69–E74. [Google Scholar] [CrossRef]
- Greenwell, L.L.; Moreno, T.; Jones, T.P.; Richards, R.J. Particle-Induced Oxidative Damage Is Ameliorated by Pulmonary Antioxidants. Free Radic. Biol. Med. 2002, 32, 898–905. [Google Scholar] [CrossRef]
- Kampa, M.; Castanas, E. Human Health Effects of Air Pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef]
- Anderson, J.O.; Thundiyil, J.G.; Stolbach, A. Clearing the Air: A Review of the Effects of Particulate Matter Air Pollution on Human Health. J. Med. Toxicol. 2012, 8, 166–175. [Google Scholar] [CrossRef]
- Gauderman, J.; Avol, E.; Gilliland, F.; Vora, H.; Thomas, D.; Berhane KMcConnell, R.; Kuenzli, N.; Lurmann, F.; Rappaport, E.; Margolis, H. The Effect of Air Pollution on Lung Development from 10 to 18 Years of Age. N. Engl. J. Med. 2004, 352, 687–696. [Google Scholar] [CrossRef]
- Barraza-Villarreal, A.; Sunyer, J.; Hernandez-Cadena, L.; Escamilla-Nunñez, M.C.; Sienra-Monge, J.J.; Ramírez-Aguilar, M.; Cortez-Lugo, M.; Holguin, F.; Diaz-Sánchez, D.; Olin, A.C.; et al. Air Pollution, Airway Inflammation, and Lung Function in a Cohort Study of Mexico City Schoolchildren. Environ. Health Perspect. 2008, 116, 832–838. [Google Scholar] [CrossRef]
- Rajagopalan, S.; Al-Kindi, S.G.; Brook, R.D. Air Pollution and Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 2054–2070. [Google Scholar] [CrossRef] [PubMed]
- Genc, S.; Zadeoglulari, Z.; Fuss, S.H.; Genc, K. The Adverse Effects of Air Pollution on the Nervous System. J. Toxicol. 2012, 2012, 782462. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Feng, W.Y.; Wang, M.; Shi, J.W.; Zhang, F.; Ouyang, H.; Zhao, Y.L.; Chai, Z.F.; Huang, Y.Y.; Xie, Y.N.; et al. Transport of Intranasally Instilled Fine Fe2O3 Particles into the Brain: Micro-Distribution, Chemical States, and Histopathological Observation. Biol. Trace Elem. Res. 2007, 118, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Migliore, L.; Coppedè, F. Environmental-Induced Oxidative Stress in Neurodegenerative Disorders and Aging. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2009, 674, 73–84. [Google Scholar] [CrossRef]
- Jomova, K.; Vondrakova, D.; Lawson, M.; Valko, M. Metals, Oxidative Stress and Neurodegenerative Disorders. Mol. Cell Biochem. 2010, 345, 91–104. [Google Scholar] [CrossRef]
- Lisabeth, L.D.; Escobar, J.D.; Dvonch, J.T.; Sánchez, B.N.; Majersik, J.J.; Brown, D.L.; Smith, M.A.; Morgenstern, L.B. Ambient Air Pollution and Risk for Ischemic Stroke and Transient Ischemic Attack. Ann. Neurol. 2008, 64, 53–59. [Google Scholar] [CrossRef]
- Ranft, U.; Schikowski, T.; Sugiri, D.; Krutmann, J.; Krämer, U. Long-Term Exposure to Traffic-Related Particulate Matter Impairs Cognitive Function in the Elderly. Environ. Res. 2009, 109, 1004–1011. [Google Scholar] [CrossRef]
- Power, M.C.; Weisskopf, M.G.; Alexeeff, S.E.; Coull, B.A.; Spiro, A., III; Schwartz, J. Traffic-Related Air Pollution and Cognitive Function in a Cohort of Older Men. Environ. Health Perspect. 2017, 119, 682–687. [Google Scholar] [CrossRef]
- Fonken, L.K.; Xu, X.; Weil, Z.M.; Chen, G.; Sun, Q.; Rajagopalan, S.; Nelson, R.J. Air Pollution Impairs Cognition, Provokes Depressive-like Behaviors and Alters Hippocampal Cytokine Expression and Morphology. Mol. Psychiatry 2011, 16, 987–995. [Google Scholar] [CrossRef]
- Ballard, C.; Gauthier, S.; Corbett, A.; Brayne, C.; Aarsland, D.; Jones, E. Alzheimer’s Disease. Lancet 2011, 377, 1019–1031. [Google Scholar] [CrossRef]
- Shulman, J.M.; De Jager, P.L.; Feany, M.B. Parkinson’s Disease: Genetics and Pathogenesis. Annu. Rev. Pathol. Mech. Dis. 2011, 6, 193–222. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, M.J.; Basagaña, X.; Dadvand, P.; Martinez, D.; Cirach, M.; Beelen, R.; Jacquemin, B. Air Pollution and Human Fertility Rates. Environ. Int. 2014, 70, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Mahalingaiah, S.; Hart, J.E.; Laden, F.; Farland, L.V.; Hewlett, M.M.; Chavarro, J.; Aschengrau, A.; Missmer, S.A. Adult Air Pollution Exposure and Risk of Infertility in the Nurses’ Health Study II. Hum. Reprod. 2016, 31, 638–647. [Google Scholar] [CrossRef] [PubMed]
- Brauer, M.; Lencar, C.; Tamburic, L.; Koehoorn, M.; Demers, P.; Karr, C.; Brauer, M.; Lencar, C.; Tamburic, L.; Koehoorn, M.; et al. A Cohort Study of Traffic-Related Air Pollution Impacts on Birth Outcomes. Environ. Health 2018, 116, 680–686. [Google Scholar] [CrossRef]
- Checa Vizcaíno, M.A.; González-Comadran, M.; Jacquemin, B. Outdoor Air Pollution and Human Infertility: A Systematic Review. Fertil. Steril. 2016, 106, 897–904.e1. [Google Scholar] [CrossRef]
- Conforti, A.; Mascia, M.; Cioffi, G.; De Angelis, C.; Coppola, G.; De Rosa, P.; Pivonello, R.; Alviggi, C.; De Placido, G. Air Pollution and Female Fertility: A Systematic Review of Literature. Reprod. Biol. Endocrinol. 2018, 16, 117. [Google Scholar] [CrossRef]
- Selevan, S.G.; Borkovec, L.; Slott, V.L.; Zudová, Z.; Environmental, S.; Perspectives, H.; Sep, N.; Selevan, S.G.; Borkovec, L.; Slott, V.L.; et al. Semen Quality and Reproductive Health of Young Czech Men Exposed to Seasonal Air Pollution. Environ. Health Perspect. 2000, 108, 887. [Google Scholar] [CrossRef]
- Agarwal, A.; Makker, K.; Sharma, R. Clinical Relevance of Oxidative Stress in Male Factor Infertility: An Update. Am. J. Reprod. Immunol. 2008, 59, 2–11. [Google Scholar] [CrossRef]
- Slama, R.; Bottagisi, S.; Solansky, I.; Lepeule, J.; Giorgis-Allemand, L.; Sram, R. Short-Term Impact of Atmospheric Pollution on Fecundability. Epidemiology 2013, 24, 871–879. [Google Scholar] [CrossRef]
- Legro, R.S.; Sauer, M.V.; Mottla, G.L.; Richter, K.S.; Li, X.; Dodson, W.C.; Liao, D. Effect of Air Quality on Assisted Human Reproduction. Hum. Reprod. 2010, 25, 1317–1324. [Google Scholar] [CrossRef]
- Slama, R.; Morgestern, V.; Cyrys, J.; Zutavern, A.; Herbarth, O.; Wichmann, H.E.; Heinrich, J. Traffic-Related Atmospheric Pollutants Levels during Pregnancy and Offspring’s Term Birth Weight: A Study Relying on a Land-Use Regression Exposure Model. Environ. Health Perspect. 2007, 115, 1283–1292. [Google Scholar] [CrossRef] [PubMed]
- Kaaja, R.J.; Greer, I.A. Manifestations of Chronic Disease during Pregnancy. JAMA 2005, 294, 2751–2757. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, V.; Díaz, J.; Salvador, P.; Linares, C. Impact of Air Pollution on Low Birth Weight in Spain: An Approach to a National Level Study. Environ. Res. 2019, 171, 69–79. [Google Scholar] [CrossRef]
- Mohorovic, L.; Petrovic, O.; Haller, H.; Micovic, V. Pregnancy Loss and Maternal Methemoglobin Levels: An Indirect Explanation of the Association of Environmental Toxics and Their Adverse Effects on the Mother and the Fetus. Int. J. Environ. Res. Public Health 2010, 7, 4203–4212. [Google Scholar] [CrossRef]
- Faiz, A.S.; Rhoads, G.G.; Demissie, K.; Kruse, L.; Lin, Y.; Rich, D.Q. Ambient Air Pollution and the Risk of Stillbirth. Am. J. Epidemiol. 2012, 176, 308–316. [Google Scholar] [CrossRef]
- Hwang, B.; Jaakkola, J.J.K. Ozone and Other Air Pollutants and the Risk of Oral Clefts. Environ. Health Perspect. 2008, 116, 1411–1415. [Google Scholar] [CrossRef]
- Gilboa, S.M.; Mendola, P.; Olshan, A.F.; Langlois, P.H.; Savitz, D.A.; Loomis, D.; Herring, A.H.; Fixler, D.E. Relation between Ambient Air Quality and Selected Birth Defects, Seven County Study, Texas, 1997–2000. Am. J. Epidemiol. 2005, 162, 238–252. [Google Scholar] [CrossRef]
- Morales, E.; Garcia-Esteban, R.; De La Cruz, O.A.; Basterrechea, M.; Lertxundi, A.; Martinez López de Dicastillo, M.D.; Zabaleta, C.; Sunyer, J. Intrauterine and Early Postnatal Exposure to Outdoor Air Pollution and Lung Function at Preschool Age. Thorax 2015, 70, 64–73. [Google Scholar] [CrossRef]
- Tian, L.; Qiu, H.; Sun, S.; Tsang, H.; Chan, K.P.; Leung, W.K. Association between Emergency Admission for Peptic Ulcer Bleeding and Air Pollution: A Case-Crossover Analysis in Hong Kong’s Elderly Population. Lancet Planet. Health 2017, 1, e74–e81. [Google Scholar] [CrossRef]
- Bosson, J.A.; Mudway, I.S.; Sandström, T. Traffic-Related Air Pollution, Health, and Allergy: The Role of Nitrogen Dioxide. Am. J. Respir. Crit. Care Med. 2019, 200, 523–524. [Google Scholar] [CrossRef]
- Khaniabadi, Y.O.; Sicard, P.; Takdastan, A.; Hopke, P.K.; Taiwo, A.M.; Khaniabadi, F.O.; De Marco, A.; Daryanoosh, M. Mortality and Morbidity Due to Ambient Air Pollution in Iran. Clin. Epidemiol. Glob. Health 2019, 7, 222–227. [Google Scholar] [CrossRef]
- Scarinzi, C.; Alessandrini, E.R.; Chiusolo, M.; Galassi, C.; Baldini, M.; Serinelli, M.; Pandolfi, P.; Bruni, A.; Biggeri, A.; De Togni, A.; et al. Air Pollution and Urgent Hospital Admissions in 25 Italian Cities: Results from the EpiAir2 Project. Epidemiol. Prev. 2013, 37, 230–241. [Google Scholar] [PubMed]
- Qiu, H.; Yu, H.; Wang, L.; Zhu, X.; Chen, M.; Zhou, L.; Deng, R.; Zhang, Y.; Pu, X.; Pan, J. The Burden of Overall and Cause-Specific Respiratory Morbidity Due to Ambient Air Pollution in Sichuan Basin, China: A Multi-City Time-Series Analysis. Environ. Res. 2018, 167, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Bell, E.M.; Liu, W.; Walker, R.J.; Kim, N.K.; Hwang, S.A. Ambient Ozone Concentration and Hospital Admissions Due to Childhood Respiratory Diseases in New York State, 1991–2001. Environ. Res. 2008, 108, 42–47. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, S.G.; Ma, Y.X.; Shang, K.Z.; Cheng, Y.F.; Li, X.; Ning, G.C.; Zhao, W.J.; Li, N.R. Association between Ambient Air Pollution and Hospital Emergency Admissions for Respiratory and Cardiovascular Diseases in Beijing: A Time Series Study. Biomed. Environ. Sci. 2015, 28, 352–363. [Google Scholar] [CrossRef]
- Pope, C.A.; Ezzati, M.; Dockery, D.W. Fine-Particulate Air Pollution and Life Expectancy in the United States. N. Engl. J. Med. 2009, 360, 376–386. [Google Scholar] [CrossRef]
- Hoek, G.; Krishnan, R.M.; Beelen, R.; Peters, A.; Ostro, B.; Brunekreef, B.; Kaufman, J.D. Long-Term Air Pollution Exposure and Cardio-Respiratory Mortality: A Review. Environ. Health 2013, 1, 43. [Google Scholar] [CrossRef]
- Beelen, R.; Raaschou-Nielsen, O.; Stafoggia, M.; Andersen, Z.J.; Weinmayr, G.; Hoffmann, B.; Wolf, K.; Samoli, E.; Fischer, P.; Nieuwenhuijsen, M.; et al. Effects of Long-Term Exposure to Air Pollution on Natural-Cause Mortality: An Analysis of 22 European Cohorts within the Multicentre ESCAPE Project. Lancet 2014, 383, 785–795. [Google Scholar] [CrossRef]
- World Health Organization. Heat and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-heat-and-health (accessed on 11 March 2024).
- Taylor, J.; McLeod, R.; Petrou, G.; Hopfe, C.; Mavrogianni, A.; Castaño-Rosa, R.; Pelsmakers, S.; Lomas, K. Ten Questions Concerning Residential Overheating in Central and Northern Europe. Build. Environ. 2023, 234, 110154. [Google Scholar] [CrossRef]
- Pörtner, H.-O.; Roberts, D.C.; Tignor, M.; Poloczanska, E.S.; Mintenbeck, K.; Alegría, A.; Craig, M.; Langsdorf, S.; Löschke, S.; Möller, V.; et al. IPCC, 2022: Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; IPCC: Geneva, Switzerland, 2022. [Google Scholar]
- Karimi, A.; Mohammad, P.; Gachkar, S.; Gachkar, D.; García-Martínez, A.; Moreno-Rangel, D.; Brown, R.D. Surface Urban Heat Island Assessment of a Cold Desert City: A Case Study over the Isfahan Metropolitan Area of Iran. Atmosphere 2021, 12, 1368. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Plan Nacional de Actuaciones Preventivas de Los Efectos Del Exceso de Temperaturas Sobre La Salud. 2023. Available online: https://www.sanidad.gob.es/areas/sanidadAmbiental/riesgosAmbientales/calorExtremo/publicaciones/planesAnteriores/docs/PlanNacionalExcesoTemperaturas_2022.pdf (accessed on 24 May 2024).
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-Related and Cold-Related Deaths in England and Wales: Who Is at Risk? Occup. Environ. Med. 2007, 64, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Chevance, G.; Minor, K.; Vielma, C.; Campi, E.; O’Callaghan-Gordo, C.; Basagaña, X.; Ballester, J.; Bernard, P. A Systematic Review of Ambient Heat and Sleep in a Warming Climate. Sleep Med. Rev. 2024, 75, 101915. [Google Scholar] [CrossRef] [PubMed]
- Malchaire, J. Human Thermal Environments: The Effects of Hot, Moderate and Cold Environments on Human Health—Comfort and Performance: The Principles and the Practice. Saf. Sci. 1994, 18, 67–68. [Google Scholar] [CrossRef]
- Linares, C.; Díaz, J. Impact of High Temperatures on Hospital Admissions: Comparative Analysis with Previous Studies about Mortality (Madrid). Eur. J. Public Health 2008, 18, 317–322. [Google Scholar] [CrossRef]
- Royé, D. The Effects of Hot Nights on Mortality in Barcelona, Spain. Int. J. Biometeorol. 2017, 61, 2127–2140. [Google Scholar] [CrossRef]
- Sohail, H.; Lanki, T.; Kollanus, V.; Tiittanen, P.; Schneider, A. Heat, Heatwaves and Cardiorespiratory Hospital Admissions in Helsinki, Finland. Int. J. Environ. Res. Public Health 2020, 17, 7892. [Google Scholar] [CrossRef]
- Brooks, K.; Landeg, O.; Kovats, S.; Sewell, M.; Oconnell, E. Heatwaves, Hospitals and Health System Resilience in England: A Qualitative Assessment of Frontline Perspectives from the Hot Summer of 2019. BMJ Open 2023, 13, e068298. [Google Scholar] [CrossRef]
- Leonardi, G.S.; Hajat, S.; Kovats, R.S.; Smith, G.E.; Cooper, D.; Gerard, E. Syndromic Surveillance Use to Detect the Early Effects of Heat-Waves: An Analysis of NHS Direct Data in England. Soz. Praventivmed 2006, 51, 194–201. [Google Scholar] [CrossRef]
- Turner, L.R.; Connell, D.; Tong, S. The Effect of Heat Waves on Ambulance Attendances in Brisbane, Australia. Prehospital Disaster Med. 2013, 28, 482–487. [Google Scholar] [CrossRef]
- Schaffer, A.; Muscatello, D.; Broome, R.; Corbett, S.; Smith, W. Emergency Department Visits, Ambulance Calls, and Mortality Associated with an Exceptional Heat Wave in Sydney, Australia, 2011: A Time-Series Analysis. Environ. Health 2012, 11, 3. [Google Scholar] [CrossRef]
- Brücker, G. Vulnerable Populations: Lessons Learnt from the Summer 2003 Heat Waves in Europe. Eurosurveillance 2005, 10, 1–2. [Google Scholar] [CrossRef]
- Hémon, D.; Jougla, E. The Heat Wave in France in August 2003. Rev. Epidemiol. Sante Publique 2004, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Ballester, J.; Quijal-zamorano, M.; Fernando, R.; Turrubiates, M.; Pegenaute, F.; Herrmann, F.R.; Robine, J.M.; Basagaña, X. Heat-Related Mortality in Europe during the Summer of 2022. Nat. Med. 2023, 29, 1857–1866. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, L.; Shen, L. Meteorology and Climate Influences on Tropospheric Ozone: A Review of Natural Sources, Chemistry, and Transport Patterns. Curr. Pollut. Rep. 2019, 5, 238–260. [Google Scholar] [CrossRef]
- Ruiz-Páez, R.; Díaz, J.; López-Bueno, J.A.; Navas, M.A.; Mirón, I.J.; Martínez, G.S.; Luna, M.Y.; Linares, C. Does the Meteorological Origin of Heat Waves Influence Their Impact on Health? A 6-Year Morbidity and Mortality Study in Madrid (Spain). Sci. Total Environ. 2023, 855, 158900. [Google Scholar] [CrossRef]
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and Non-Auditory Effects of Noise on Health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef]
- Tobías, A.; Recio, A.; Díaz, J.; Linares, C. Health Impact Assessment of Traffic Noise in Madrid (Spain). Environ. Res. 2015, 137, 136–140. [Google Scholar] [CrossRef]
- Goines, L.; Hagler, L. Noise Pollution: A Modern Plague. South. Med. J. 2007, 100, 287–294. [Google Scholar] [CrossRef]
- European Environment Agency. Environmental Noise in Europe; European Environment Agency: Copenhagen, Denmark, 2020. [Google Scholar]
- Eriksson, C.; Pershagen, G.; Nilsson, M. Biological Mechanisms Related to Cardiovascular and Metabolic Effects by Environmental Noise; European Commission Joint Research Centre: Brussels, Belgium, 2018; p. 19. [Google Scholar]
- Berglund, B.; Lindvall, T.; Schwela, D. Guidelines for Community Noise; World Health Organization: Geneva, Switzerland, 1995; Volume 31. [Google Scholar]
- Chang, T.Y.; Lai, Y.A.; Hsieh, H.H.; Lai, J.S.; Liu, C.S. Effects of Environmental Noise Exposure on Ambulatory Blood Pressure in Young Adults. Environ. Res. 2009, 109, 900–905. [Google Scholar] [CrossRef]
- World Health Organization. Environmental Noise Guidelines for the European Region; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Moebus, S.; Gruehn, D.; Poppen, J.; Sutcliffe, R.; Haselhoff, T.; Lawrence, B. Acoustic Quality and Urban Health—More than Just Noise and Silence. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2020, 63, 997–1003. [Google Scholar] [CrossRef]
- Foraster, M.; Esnaola, M.; López-Vicente, M.; Rivas, I.; Álvarez-Pedrerol, M.; Persavento, C.; Sebastian-Galles, N.; Pujol, J.; Dadvand, P.; Sunyer, J. Exposure to Road Traffic Noise and Cognitive Development in Schoolchildren in Barcelona, Spain: A Population-Based Cohort Study. PLoS Med. 2022, 19, e1004001. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Assessing the Value of Urban Green and Blue Spaces for Health and Well-Being; World Health Organization: Geneva, Switzerland, 2023; pp. 1–17. [Google Scholar]
- White, M.P.; Alcock, I.; Grellier, J.; Wheeler, B.W.; Hartig, T.; Warber, S.L.; Bone, A.; Depledge, M.H.; Fleming, L.E. Spending at Least 120 Minutes a Week in Nature Is Associated with Good Health and Wellbeing. Sci. Rep. 2019, 9, 7730. [Google Scholar] [CrossRef] [PubMed]
- Grahn, P.; Stigsdotter, U.K. The Relation between Perceived Sensory Dimensions of Urban Green Space and Stress Restoration. Landsc. Urban. Plan. 2010, 94, 264–275. [Google Scholar] [CrossRef]
- Mohammadzadeh, N.; Mohammadzadeh, R. The Assessment of Soundscape Quality in Historic Urban Parks: A Case Study of El-Goli Park of Tabriz, Iran. Noise Vib. Worldw. 2023, 54, 248–260. [Google Scholar] [CrossRef]
- Gascon, M.; Mas, M.T.; Martínez, D.; Dadvand, P.; Forns, J.; Plasència, A.; Nieuwenhuijsen, M.J. Mental Health Benefits of Long-Term Exposure to Residential Green and Blue Spaces: A Systematic Review. Int. J. Environ. Res. Public Health 2015, 12, 4354–4379. [Google Scholar] [CrossRef]
- Pearce, M.; Garcia, L.; Abbas, A.; Strain, T.; Schuch, F.B.; Golubic, R.; Kelly, P.; Khan, S.; Utukuri, M.; Laird, Y.; et al. Association between Physical Activity and Risk of Depression: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2022, 79, 550–559. [Google Scholar] [CrossRef]
- Vert, C.; Gascon, M.; Ranzani, O.; Márquez, S.; Triguero-Mas, M.; Carrasco-Turigas, G.; Arjona, L.; Koch, S.; Llopis, M.; Donaire-Gonzalez, D.; et al. Physical and Mental Health Effects of Repeated Short Walks in a Blue Space Environment: A Randomised Crossover Study. Environ. Res. 2020, 188, 109812. [Google Scholar] [CrossRef]
- White, M.P.; Elliott, L.R.; Grellier, J.; Economou, T.; Bell, S.; Bratman, G.N.; Cirach, M.; Gascon, M.; Lima, M.L.; Lõhmus, M.; et al. Associations between Green/Blue Spaces and Mental Health across 18 Countries. Sci. Rep. 2021, 11, 8903. [Google Scholar] [CrossRef]
- Enssle, F.; Kabisch, N. Urban Green Spaces for the Social Interaction, Health and Well-Being of Older People—An Integrated View of Urban Ecosystem Services and Socio-Environmental Justice. Environ. Sci. Policy 2020, 109, 36–44. [Google Scholar] [CrossRef]
- Tillmann, S.; Tobin, D.; Avison, W.; Gilliland, J. Mental Health Benefits of Interactions with Nature in Children and Teenagers: A Systematic Review. J. Epidemiol. Community Health 2018, 72, 958–966. [Google Scholar] [CrossRef]
- Zhang, Y.; Mavoa, S.; Zhao, J.; Raphael, D.; Smith, M. The Association between Green Space and Adolescents Mental Well-Being: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6640. [Google Scholar] [CrossRef] [PubMed]
- Kaczynski, A.T.; Potwarka, L.R.; Saelens, B.E. Association of Park Size, Distance, and Features with Physical Activity in Neighborhood Parks. Am. J. Public Health 2008, 98, 1451–1456. [Google Scholar] [CrossRef] [PubMed]
- Bedimo-Rung, A.L.; Mowen, A.J.; Cohen, D.A. The Significance of Parks to Physical Activity and Public Health: A Conceptual Model. Am. J. Prev. Med. 2005, 28, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.D.; Crippa, A.; Woodcock, J.; Brage, S. Physical Activity and Incident Type 2 Diabetes Mellitus: A Systematic Review and Dose–Response Meta-Analysis of Prospective Cohort Studies. Diabetologia 2016, 59, 2527–2545. [Google Scholar] [CrossRef]
- Ngom, R.; Gosselin, P.; Blais, C.; Rochette, L. Type and Proximity of Green Spaces Are Important for Preventing Cardiovascular Morbidity and Diabetes—A Cross-Sectional Study for Quebec, Canada. Int. J. Environ. Res. Public Health 2016, 13, 423. [Google Scholar] [CrossRef]
- Leng, H.; Li, S.; Yan, S.; An, X. Exploring the Relationship between Green Space in a Neighbourhood and Cardiovascular Health in the Winter City of China: A Study Using a Health Survey for Harbin. Int. J. Environ. Res. Public Health 2020, 17, 513. [Google Scholar] [CrossRef]
- Brown, S.C.; Aitken, W.W.; Lombard, J.; Wang, K.; Rundek, T.; Byrne, M.M.; Toro, M.; Nardi, M.I.; Kardys, J.; Parrish, A.; et al. Precision Greenness and Stroke/Transient Ischemic Attack in 249,405 US Medicare Beneficiaries. J. Stroke 2023, 25, 173–176. [Google Scholar] [CrossRef]
- Wang, K.; Lombard, J.; Rundek, T.; Dong, C.; Gutierrez, C.M.; Byrne, M.M.; Toro, M.; Nardi, M.I.; Kardys, J.; Yi, L.; et al. Relationship of Neighborhood Greenness to Heart Disease in 249 405 US Medicare Beneficiaries. J. Am. Heart Assoc. 2019, 8, 21–29. [Google Scholar] [CrossRef]
- Diener, A.; Mudu, P. How Can Vegetation Protect Us from Air Pollution? A Critical Review on Green Spaces’ Mitigation Abilities for Air-Borne Particles from a Public Health Perspective-with Implications for Urban Planning. Sci. Total Environ. 2021, 796, 148605. [Google Scholar] [CrossRef]
- Chaparro, L.; Terrasdas, J. Ecological Services of Urban Forest in Barcelona. Shengtai Xuebao/Acta Ecol. Sin. 2009, 29, 103. [Google Scholar]
- Vilela, J. Distribución Del Arbolado Urbano En La Ciudad de Fuenlabrada y Su Contribución a La Calidad Del Aire. Ciudad. Y Territ. Estud. Territ. 2004, 36, 419–427. [Google Scholar]
- Heo, S.; Bell, M.L. The Influence of Green Space on the Short-Term Effects of Particulate Matter on Hospitalization in the U.S. for 2000–2013. Environ. Res. 2019, 174, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Liao, J.; Wang, J.; Yang, C.; Jiao, K.; Wang, X.; Huang, Z.; Ma, X.; Liu, X.; Liao, J.; et al. PM2.5-Associated Hospitalization Risk of Cardiovascular Diseases in Wuhan: Cases Alleviated by Residential Greenness. Int. J. Environ. Res. Public Health 2022, 20, 746. [Google Scholar] [CrossRef] [PubMed]
- Pereira, G.; Foster, S.; Martin, K.; Christian, H.; Boruff, B.J.; Knuiman, M.; Giles-Corti, B. The Association between Neighborhood Greenness and Cardiovascular Disease: An Observational Study. BMC Public Health 2012, 12, 466. [Google Scholar] [CrossRef]
- Chen, D.; Wang, X.; Thatcher, M.; Barnett, G.; Kachenko, A.; Prince, R. Urban Vegetation for Reducing Heat Related Mortality. Environ. Pollut. 2014, 192, 275–284. [Google Scholar] [CrossRef]
- Wang, G.; Yang, F.F.; Lin, G.; Wang, Z.; Zhang, X. Modification of Low Temperature-Related Hospital Admissions for Cardiovascular Diseases by Multiple Green Space Indicators at Multiple Spatial Scales: Evidence from Guangzhou, China. Int. J. Hyg. Environ. Health 2023, 251, 114193. [Google Scholar] [CrossRef]
- Iungman, T.; Cirach, M.; Marando, F.; Pereira Barboza, E.; Khomenko, S.; Masselot, P.; Quijal-Zamorano, M.; Mueller, N.; Gasparrini, A.; Urquiza, J.; et al. Cooling Cities through Urban Green Infrastructure: A Health Impact Assessment of European Cities. Lancet 2023, 401, 577–589. [Google Scholar] [CrossRef]
- Karimi, A.; Moreno-Rangel, D.; García-Martínez, A. Granular Mapping of UHI and Heatwave Effects: Implications for Building Performance and Urban Resilience. Build. Environ. 2025, 273, 112705. [Google Scholar] [CrossRef]
- Gallo, M.; Marinelli, M. Sustainable Mobility: A Review of Possible Actions and Policies. Sustainability 2020, 12, 7499. [Google Scholar] [CrossRef]
- Sugiyama, T.; Koohsari, M.J.; Oka, K. New Urban Mobility: A Catalyst to Enhance Population Health. Perspect. Public Health 2020, 140, 198–199. [Google Scholar] [CrossRef]
- Clínica Universidad de Navarra Caminar y Salud. Available online: https://www.cun.es/chequeos-salud/vida-sana/deporte/caminar-salud (accessed on 1 August 2024).
- Fundación Española del Corazón Caminar a Paso Rápido de Forma Regular Reduce Hasta Un 11% El Riesgo Cardiovascular. Available online: https://fundaciondelcorazon.com/prensa/notas-de-prensa/2604-caminar-a-paso-rapido-de-forma-regular-reduce-hasta-un11-riesgo-cardiovascular.html (accessed on 1 August 2024).
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Foster, S.; Lowe, M.; Sallis, J.F.; Stevenson, M.; et al. City Planning and Population Health: A Global Challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L.; et al. Physical Activity in Relation to Urban Environments in 14 Cities Worldwide: A Cross-Sectional Study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef] [PubMed]
- Handy, S.L.; Boarnet, M.G.; Ewing, R.; Killingsworth, R.E. How the Built Environment Affects Physical Activity: Views from Urban Planning. Am. J. Prev. Med. 2002, 23, 64–73. [Google Scholar] [CrossRef]
- Organización Mundial de la Salud Cada Movimiento Cuenta Para Mejorar La Salud. Available online: https://www.who.int/es/news/item/25-11-2020-every-move-counts-towards-better-health-says-who (accessed on 1 August 2024).
- Rojas-Rueda, D.; De Nazelle, A.; Tainio, M.; Nieuwenhuijsen, M.J. The Health Risks and Benefits of Cycling in Urban Environments Compared with Car Use: Health Impact Assessment Study. BMJ 2011, 343, d4521. [Google Scholar] [CrossRef]
- Evans, G.W.; Wener, R.E. Rail Commuting Duration and Passenger Stress. Health Psychol. 2006, 25, 408–412. [Google Scholar] [CrossRef]
- La Ciudad de Pontevedra, Referente de Movilidad Sostenible. Available online: https://ecopalabras.com/2020/09/08/la-ciudad-de-pontevedra-referente-de-movilidad-sostenible/ (accessed on 16 April 2024).
- Pucher, J.; Buehler, R. Cycling for Everyone: Lessons from Europe. Transp. Res. Rec. 2008, 2074, 58–65. [Google Scholar] [CrossRef]
- Kovačić, M.; Mutavdžija, M.; Buntak, K. New Paradigm of Sustainable Urban Mobility: Electric and Autonomous Vehicles—A Review and Bibliometric Analysis. Sustainability 2022, 14, 9525. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Air Quality Guidelines; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Consejo de la Unión Europea. Directiva 2008/50/CE Del Parlamento Europeo y Del Consejo Relativa a La Calidad Del Aire Ambiente y a Una Atmósfera Más Limpia En Europa; World Health Organization. Regional Office for Europe: Geneva, Switzerland, 2008; pp. 1–44. [Google Scholar]
- Konijnendijk, C.C. Evidence-Based Guidelines for Greener, Healthier, More Resilient Neighbourhoods: Introducing the 3–30–300 Rule. J. For. Res. 2023, 34, 821–830. [Google Scholar] [CrossRef]
- Ministerio de Salud de España. Impacto Sobre La Salud de La Calidad Del Aire En España. 2019, 1–93. Available online: https://www.sanidad.gob.es/ciudadanos/saludAmbLaboral/docs/PLAN_AIRE_Medida_5_19_12_27.pdf (accessed on 31 March 2024).
- Cadot, E.; Rodwin, V.G.; Spira, A. In the Heat of the Summer: Lessons from the Heat Waves in Paris. J. Urban Health 2007, 84, 466–468. [Google Scholar] [CrossRef]
- Monge-Barrio, A.; Sánchez-Ostiz Gutierrez, A. Passive Energy Strategies for Mediterranean Residential Buildings Facing the Challenges of Climate Change and Vulnerable Populations; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Mayrhuber, E.A.S.; Dückers, M.L.A.; Wallner, P.; Arnberger, A.; Allex, B.; Wiesböck, L.; Wanka, A.; Kolland, F.; Eder, R.; Hutter, H.P.; et al. Vulnerability to Heatwaves and Implications for Public Health Interventions—A Scoping Review. Environ. Res. 2018, 166, 42–54. [Google Scholar] [CrossRef]
- Wright, F. Old and Cold: Older People and Policies Failing to Address Fuel Poverty. Soc. Policy Adm. 2004, 38, 488–503. [Google Scholar] [CrossRef]
- Plan Nacional de Actuaciones Preventivas Por Bajas Temperaturas. 2022. Available online: https://www.sanidad.gob.es/areas/sanidadAmbiental/riesgosAmbientales/frioExtremo/publicaciones/docs/Plan_Frio_23-24.pdf (accessed on 31 March 2024).
- Van Daalen, K.R.; Tonne, C.; Semenza, J.C.; Rocklöv, J.; Markandya, A.; Dasandi, N.; Jankin, S.; Achebak, H.; Ballester, J.; Bechara, H.; et al. The 2024 Europe Report of the Lancet Countdown on Health and Climate Change: Unprecedented Warming Demands Unprecedented Action. Lancet Public Health 2024, 9, e495–e522. [Google Scholar] [CrossRef] [PubMed]
- Robitaille, É.; Douyon, C. Using the 3-30-300 Indicator to Evaluate Green Space Accessibility and Inequalities: A Case Study of Montreal, Canada. Geographies 2025, 5, 6. [Google Scholar] [CrossRef]
- Natterer, E.; Loder, A.; Bogenberger, K. Effects of the Plan Velo I and II on Vehicular Flow in Paris—An Empirical Analysis. arXiv 2024, arXiv:2408.09836. [Google Scholar]
- Mueller, N.; Rojas-Rueda, D.; Khreis, H.; Cirach, M.; Andrés, D.; Ballester, J.; Bartoll, X.; Daher, C.; Deluca, A.; Echave, C.; et al. Changing the Urban Design of Cities for Health: The Superblock Model. Environ. Int. 2020, 134, 105132. [Google Scholar] [CrossRef]
- Gascon, M.; Zijlema, W.; Vert, C.; White, M.P.; Nieuwenhuijsen, M.J. Outdoor Blue Spaces, Human Health and Well-Being: A Systematic Review of Quantitative Studies. Int. J. Hyg. Environ. Health 2017, 220, 1207–1221. [Google Scholar] [CrossRef]
- Li, D.; Bou-Zeid, E. Synergistic Interactions between Urban Heat Islands and Heat Waves: The Impact in Cities Is Larger than the Sum of Its Parts. J. Appl. Meteorol. Climatol. 2013, 52, 2051–2064. [Google Scholar] [CrossRef]
- Zhao, L.; Lee, X.; Smith, R.B.; Oleson, K. Strong Contributions of Local Background Climate to Urban Heat Islands. Nature 2014, 511, 216–219. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.J. Urban and Transport Planning Pathways to Carbon Neutral, Liveable and Healthy Cities; A Review of the Current Evidence. Environ. Int. 2020, 140, 105661. [Google Scholar] [CrossRef]
- Mahdavi Estalkhsari, B.; Mohammad, P.; Karimi, A. Land Use and Land Cover Change Dynamics and Modelling Future Urban Growth Using Cellular Automata Model over Isfahan Metropolitan Area of Iran. In Ecological Footprints of Climate Change. Adaptive Adaptive Approaches and Sustainability; Springer Climate: Cham, Switzerland, 2022; ISBN 978-3-031-15500-0. [Google Scholar]
- Stewart, I.D.; Oke, T.R. Local Climate Zones for Urban Temperature Studies. Bull. Am. Meteorol. Soc. 2012, 93, 1879–1900. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arriazu-Ramos, A.; Santamaría, J.M.; Monge-Barrio, A.; Bes-Rastrollo, M.; Gutierrez Gabriel, S.; Benito Frias, N.; Sánchez-Ostiz, A. Health Impacts of Urban Environmental Parameters: A Review of Air Pollution, Heat, Noise, Green Spaces and Mobility. Sustainability 2025, 17, 4336. https://doi.org/10.3390/su17104336
Arriazu-Ramos A, Santamaría JM, Monge-Barrio A, Bes-Rastrollo M, Gutierrez Gabriel S, Benito Frias N, Sánchez-Ostiz A. Health Impacts of Urban Environmental Parameters: A Review of Air Pollution, Heat, Noise, Green Spaces and Mobility. Sustainability. 2025; 17(10):4336. https://doi.org/10.3390/su17104336
Chicago/Turabian StyleArriazu-Ramos, Ainhoa, Jesús Miguel Santamaría, Aurora Monge-Barrio, Maira Bes-Rastrollo, Sonia Gutierrez Gabriel, Nuria Benito Frias, and Ana Sánchez-Ostiz. 2025. "Health Impacts of Urban Environmental Parameters: A Review of Air Pollution, Heat, Noise, Green Spaces and Mobility" Sustainability 17, no. 10: 4336. https://doi.org/10.3390/su17104336
APA StyleArriazu-Ramos, A., Santamaría, J. M., Monge-Barrio, A., Bes-Rastrollo, M., Gutierrez Gabriel, S., Benito Frias, N., & Sánchez-Ostiz, A. (2025). Health Impacts of Urban Environmental Parameters: A Review of Air Pollution, Heat, Noise, Green Spaces and Mobility. Sustainability, 17(10), 4336. https://doi.org/10.3390/su17104336







