A New Model for a Sustainable Healthcare Supply Chain Prioritizes Patient Safety: Using the Fuzzy Delphi Method to Identify Healthcare Workers’ Perspectives
Abstract
1. Introduction
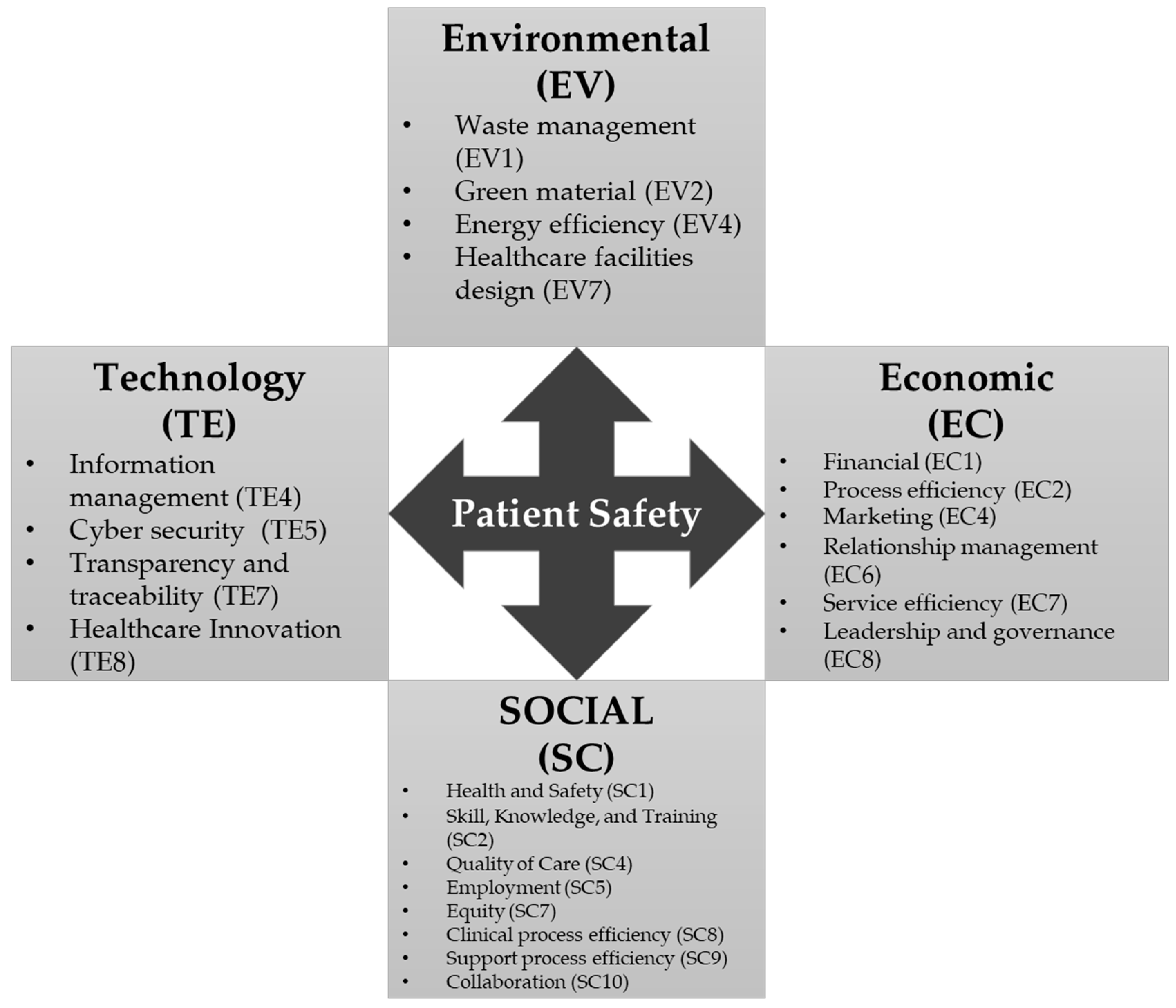
- To identify the attributes of an SHSC across four dimensions, those being the environmental, social, economic, and technological dimensions, so as to accelerate progress towards safety and to increase the quality of care from the perspective of healthcare workers.
- To develop and introduce a new pillar to the SHSC model, thus integrating technology with the three classical pillars of sustainability, while taking the perspective of healthcare workers.
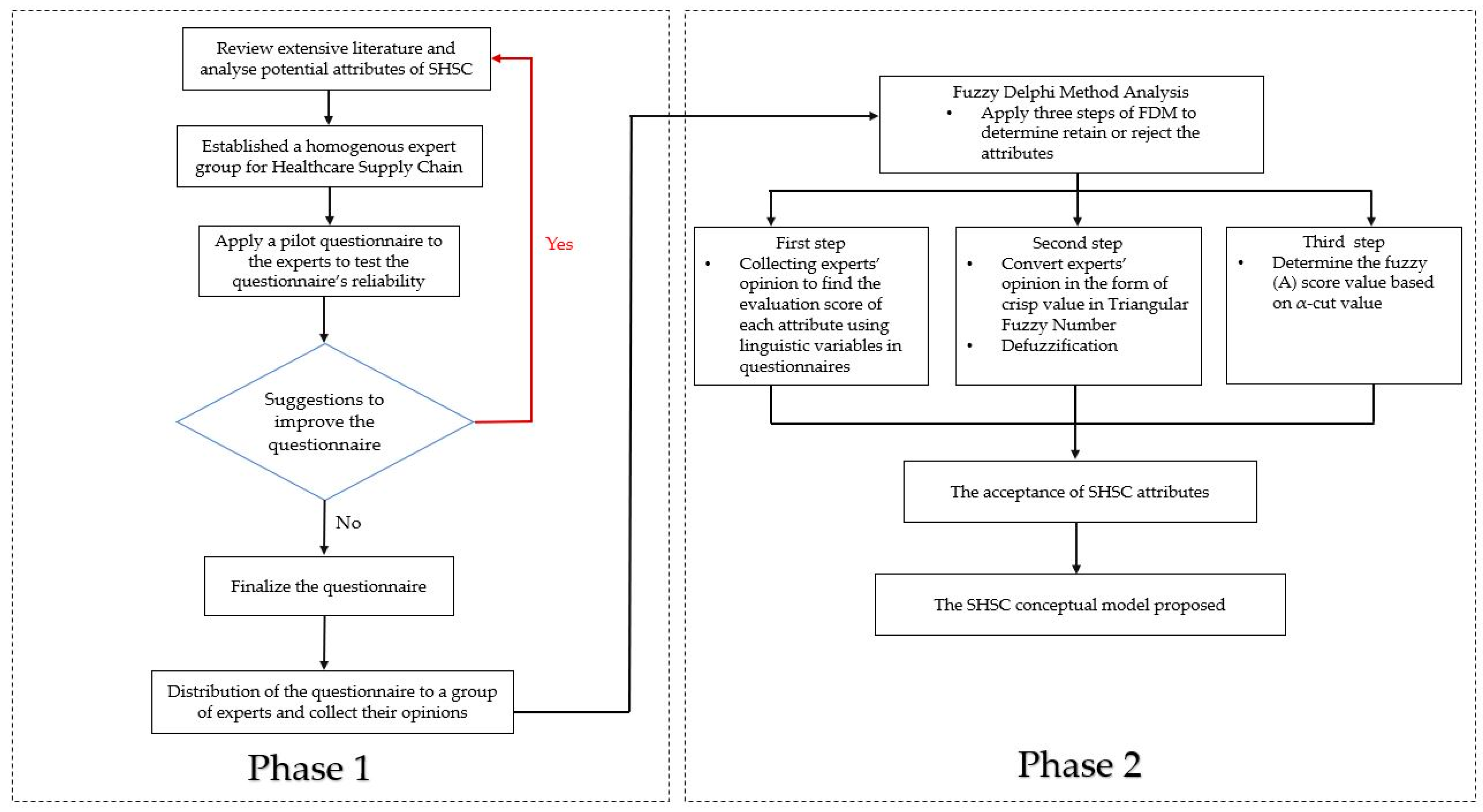
2. Research Methodology
2.1. Literature Review
- Identification stage. We studied key attributes of the sustainable healthcare supply chain as they relate to the three pillars of sustainability (environmental, social, and economic). We searched for articles in SCOPUS, IEEE, ResearchGate, Google Scholar, Science Direct, and the Web of Science, using the search terms “healthcare”, “supply chain”, “supply chain management”, “sustainability”, “technology”, “patient safety”, and “pandemic”, considering only those that had been published in the previous 20 years (2002–2023). Non-English and duplicate articles were eliminated at this stage.
- Screening stage. The screening process for the abstract review was conducted. The articles that were irrelevant to the healthcare supply chain and patient safety were excluded at this stage.
- Included stage. The remaining articles were conducted for the final full-text review. The researcher reviewed the SHSC attributes; then, the potential technological pillar was found and studied, including its key attributes. This step yielded a new SHSC model that features the integration of those four pillars.
2.2. Selection of Experts
2.3. Reliability of Questionnaire
2.4. Fuzzy Delphi Method
- Step 1: Collect expert opinions by distributing a questionnaire to 15 experts in the healthcare industry who meet the criteria as mentioned in Section 2.2. The questionnaire was divided into three main parts. The first part contained questions about respondents’ demographic. In the second part, the participants were asked to determine the importance of SHSC attributes via a questionnaire which employed linguistic preferences listed in Table 1: Not important, Slightly important, Moderately important, Very important, and Extremely important.
| Linguistic Variable | Triangular Fuzzy Numbers | ||
|---|---|---|---|
| a | b | C | |
| Not important | 0 | 0 | 0.25 |
| Slightly important | 0 | 0.25 | 0.5 |
| Moderately important | 0.25 | 0.5 | 0.75 |
| Very important | 0.5 | 0.75 | 1 |
| Extremely important | 0.75 | 1 | 1 |
- Step 2: This research calculated the importance value of each SHSC attribute, which were determined by the healthcare experts using triangular fuzzy numbers. The linguistic preferences were converted into triangular numbers, as mentioned in Table 1. Then, the computing formula is applied as follows to calculate the importance value of each SHSC attribute given by experts:
- Step 3: Determine whether to accept or reject SHSC attributes, according to the threshold γ. The equation is applied for the purpose of calculating the threshold values to screen out any unnecessary SHSC attributes. If the crisp value of is greater than the threshold value γ, attribute j is accepted; conversely, if the crisp value of is lower than the threshold value γ, attribute j is rejected.
3. Results
3.1. Literature Review
3.2. Selection of Experts
3.3. Reliability of Questionnaire
3.4. Fuzzy Delphi Method
3.5. A New Model of a Sustainable Healthcare Supply Chain (SHSC) Optimized for Patient Safety
3.5.1. Social Dimension
- Health and Safety (SC1) is an important attribute that relates to the safety of patients and healthcare workers, both physically and mentally. A safe environment in a healthcare facility can mitigate many harms that may occur. Safety for healthcare workers also leads to safety for patients and the wider society. The experts suggested that a healthcare organization must build a culture of health and safety within a society—for example, by providing basic life support and dental care programs to poor communities in developing countries. Therefore, healthcare executives should emphasize this attribute as part of a sustainability strategy.
- Skill, Knowledge, and Training (SC2) was observed to have the highest defuzzified score. The experts expressed that skill, knowledge, and training comprise a crucial factor for healthcare personnel. Effective skills and knowledge and adequate training can ensure that safe treatment and medical services are provided to patients.
- Quality of Care (SC4) focuses on improving health outcomes. The ultimate goals in healthcare are ensuring patient safety and enhancing the quality of care. The experts suggested that quality of care is a process in which the safest care is provided to the patient, while avoiding misuse of care, and that care is provided in a timely manner, while enhancing the efficiency of the equipment, supplies, and energy used in the healthcare setting. Furthermore, providing care equitably is a goal of implementing sustainability in healthcare.
- Employment (SC5) focuses on the improvement of healthcare worker efficiency, satisfaction, work–life balance (which is related to the proportion of working hours), employee privacy, and benefits provided to employees. The healthcare experts suggested that healthcare organizations can promote sustainability through employee well-being and satisfaction. Then, the outcome will be reflected in the high-quality care provided by the healthcare workers.
- Equity (SC7) in healthcare focuses on providing equal opportunities to all for attaining their health potential. Providing health services that everyone can access is a goal of sustainability in healthcare. Accelerating supply chain management in healthcare to cope with health inequities, especially in developing countries, plays a key role in the success of a SHSC.
- Clinical Process Efficiency (SC8) addresses the processes underlying the provision of medical services to patients, including patient admission, investigation, care delivery, patient discharge, and patient transfer. The efficiency of the clinical process establishes the possibility of a good clinical outcome. The experts noted that the efficiency of the clinical process ensures that the requirements of patients and healthcare workers are fulfilled in a timely manner, as well as providing adequate value for money spent.
- Support Process Efficiency (SC9) focuses on the processes required to accomplish support activities in healthcare, such as imaging diagnoses, laboratory services, inventory management, medical equipment preparedness, and preparing medical supplies. Support process efficiency aims to ensure the safety of the supply chain from upstream to downstream. One expert mentioned that, if the support process is effectively managed by stakeholders, healthcare workers can dedicate more time to patient care, resulting in good clinical outcomes. In addition, the implementation of efficiency throughout a sustainable supply chain can improve patient and practitioner safety.
- Collaboration (SC10) reflects the quality of the relationships among supply chain stakeholders. Collaboration in the HSC improves the timeliness of treatment, enhances patient and practitioner safety, and strengthens trust between the patient and the care provider. Collaboration drives communication throughout the supply chain. It creates consistency, reduces errors, develops strong partnerships among supply chain members, and builds long-term resilience. The outcome of good collaboration is that the healthcare organization can maintain and improve the quality of patient care.
3.5.2. Environmental Dimension
- Waste Management (EV1) focuses on ensuring that medical waste generated by healthcare facilities is properly managed. Ineffective medical waste management can pose serious health and environmental risks, including the spread of infectious diseases, pollution, and contamination of water, air, and soil. Therefore, the experts suggested that effective waste management is essential for the healthcare system, in order to ensure the safety and health of patients, staff, and the environment. Furthermore, it can help to minimize costs and reduce the environmental impact of healthcare operations.
- Green Material (EV2) is the attribute that ensures that healthcare products are produced from environmentally friendly materials. The experts suggested that, in order to reduce the environmental impact of medical waste, these products should be designed to be biodegradable and recyclable, thus reducing waste and preventing pollution or natural contamination. In addition, medical products should made from natural, nontoxic materials that are safe for patients, healthcare workers, and the environment.
- Energy Efficiency (EV4) refers to the optimization of energy consumption in healthcare activities. The healthcare experts recommended that promoting energy efficiency can be achieved in various ways, such as by using renewable energy sources (e.g., solar, wind, and geothermal power) to reduce the use of fossil fuels and decrease the carbon footprint of healthcare activities. Furthermore, healthcare organizations can optimize transportation through the use of electric vehicles, managing routes, and scheduling deliveries effectively.
- Healthcare Facility Design (EV7) can promote sustainable practices in the HSC, such as the use of sustainable materials in the construction of buildings and furnishings, using recyclable materials, reducing the use of nonrenewable energy in the construction phase, and promoting construction-waste recycling. For patient and healthcare worker safety, healthcare facilities should be designed with concern for safety and security, including fall prevention, infection control, the reduction of injuries from sharp objects, accessibility for vulnerable groups, and emergency preparedness planning.
3.5.3. Economic Dimension
- Financial (EC1): The experts suggested that, in terms of patient safety, ensuring adequate financial resources for investing in technology, equipment, staffing, training, facility infrastructure, and quality improvement initiatives can lead to sustainability. In addition, the ability to reduce the total cost of the HSC, which includes purchasing costs, administrative costs, supply expenses, inventory holding costs, transportation costs, and maintenance costs, while maximizing the revenue growth, profitability, net profits, and cash flow rate, can drive healthcare organizations in a sustainable manner.
- Process Efficiency (EC2) reflects the ability of a healthcare organization to transform various resources into value-added outputs. Process efficiency can improve patient and healthcare worker safety by mitigating the risk of supply chain disruptions, which might cause delays in treatment, as well as other adverse events that could harm either patients or healthcare workers. The experts suggested that process efficiency can minimize the cost, as well as ensuring that the right product is delivered to the right person in the right place at the right time. Achieving process efficiency in healthcare organizations can improve patient outcomes and stakeholder satisfaction, while sustainably delivering the highest quality of care.
- Marketing (EC4) refers to the ability of the firm to develop a unique, competitive profile, increase market growth, and build strong brand awareness and reputation. In terms of the expert opinions, a marketing strategy may indirectly relate to the safety aspect in HSC management through relationships with suppliers that have established brands that are associated with high safety and quality standards. Marketing can play an important role in the HSC, by promoting healthcare products and services that improve patient safety, while maintaining environmentally friendly and economical operations.
- Relationship Management (EC6) focuses on the involvement of additional parties and the opportunities that that affords for learning more from each other. Relationship-building is highly important in conveying reliability to customers. The experts indicated that the ability to communicate effectively and build a strong relationship among stakeholders can lead to meaningful improvements, not only in relation to safety, but also for the whole healthcare system.
- Service Efficiency (EC7) refers to the ability of the healthcare organization to respond to patient demand and deliver healthcare services, products, and equipment to the patient in a timely manner. Improving service efficiency in the healthcare supply chain results in improved patient outcomes, while optimizing costs and increasing the profitability of the firm.
- Leadership and Governance (EC8) tends to provide essential direction, oversight, and accountability to the HSC system, while a lack of leadership and governance in decision-making can lead to vagueness, resulting in excessive costs to the firm in the long run. The healthcare experts put forward the opinion that the policies and direction of the upper management are factors that are directly relevant to a SHSC.
3.5.4. Technological Dimension
- Information Management (TE4) refers to the usefulness, accuracy, reliability, and availability of data in the HSC that can be exchanged between stakeholders effectively. Furthermore, effective information management allows stakeholders to identify and mitigate risks that may cause supply chain disruptions. In terms of patient safety, providing data tracking and traceability, along with communication among stakeholders, can improve patient safety and minimize the risk of any adverse events.
- Cybersecurity (TE5) focuses on the ability of healthcare organizations to prevent cyberattacks and ensure patient safety. Cybersecurity measures must be prioritized and put in place. A lack of cybersecurity protocols can pose risks to healthcare operations, such as the data hacking of patients’ electronic medical records (EMRs), viral attacks on medical devices, and the loss, or leaking, of hospital financial and other confidential data. The implementation of strong access controls and building awareness throughout the supply chain can help to prevent cybercrime and ensure safe and healthy supply chain processes.
- Transparency and Traceability (TE7) are key attributes for ensuring patient safety in healthcare. They allow stakeholders to immediately identify and address potential safety issues, such that they can mitigate the risks and harm to patients that might occur. Transparency refers to the accessibility of information throughout the supply chain process, from the point of production to the point of consumption (i.e., from upstream to downstream). Traceability involves the ability to track the movement of material and healthcare products. Transparency and traceability also help to build trust and credibility among stakeholders of the HSC.
- Healthcare Innovation (TE8) involves the use of new technologies to improve safety and efficiency. Some examples of health innovations, according to the experts’ suggestions, include the following: (1) Blockchain technology can be used, which allows for secure and transparent supply chain transactions. This technology helps to prevent fraud and improve tracking and traceability in a supply chain. (2) The use of artificial intelligence (AI) plays a crucial role in healthcare services. AI can be used to enable imaging analysis in medical diagnoses and help in correct decision-making for healthcare professionals. (3) Robotics and automation can be included in the HSC to streamline both clinical and nonclinical processes, helping to reduce human errors and improving accuracy in healthcare processes. (4) Internet of Things (IoT) devices, which can be applied for a variety of purposes, such as wearable medical devices, sensor systems for supply chain management, and clinical care management, can be implemented. Adopting healthcare innovations in the supply chain in a healthcare setting can help to improve safety and efficiency, while reducing costs and minimizing the impact on the environment, leading to improvements in overall sustainability.
4. Discussion
5. Conclusions
Limitations and Future Research
- The presented SHSC is an integrated model that was developed for improving patient safety in healthcare from the perspective of healthcare experts in developing countries in Southeast Asia. As such, the experience of the HSC experts covers only the context of Southeast Asia. Therefore, the applicability of this model to other industries or other regions may be limited. Future studies in different contexts or focused on other industries or regions are required.
- As we analyzed and identified the key attributes based on a systematic literature review, some aspects relevant to an SHSC optimized for patient safety might have been overlooked.
- This research only presents a new conceptual model, lacking application to a real-world case. Future research may apply structural equation modeling to generate a model and apply the model to the Multi-Criteria Decision Making (MCDM) method as an assessment tool for healthcare organizations.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Dimension | Attributes | Definition |
|---|---|---|
| Social | SC1 Health and Safety | Ensure the safety of employees in physical and mental health. Promote a safe environment at the workplace to avoid any harm that may occur. Reduce the hazard incident from unqualified medical products. |
| SC2 Skills, Knowledge, and Training | Improve essential skills and knowledge, and promote training to the healthcare practitioners to enhance work efficiency, which can lead to safe treatment and avoid life-threatening complications that may occur to patients. | |
| SC3 Community | Building a strong engagement with local communities, increasing well-being of the population, provide healthcare services accessible to local communities. | |
| SC4 Quality of Care | Avoiding misuse of care, providing care in a timely manner, and providing care equitably. | |
| SC5 Employment | Focuses on healthcare workers efficiency, employee satisfaction, work-life balance, employee well-being, and benefits provided to employees. | |
| SC6 Stakeholder Engagement | A measurement of stakeholders’ involvement in an organization. The perceptions of stakeholders in the program, project, or initiative with the organization. | |
| SC7 Equity | Focuses on providing equal opportunities, promoting diversity, fairness, and basic needs to maintain an acceptable quality of life, eliminating gender bias, and reduce incidents of discrimination. | |
| SC8 Clinical Process Efficiency | Ensure the requirement of patients and healthcare workers are fulfilled in a timely manner and adequate value for the money spent on clinical activities. | |
| SC9 Support Process Efficiency | Focuses on the processes required to accomplish support activities in healthcare; for instance, imaging diagnoses, laboratory service, and inventory management. | |
| SC10 Collaboration | Driving communication throughout the supply chain among stakeholders to maintain and improve the quality of patient care. | |
| Environmental | EV1 Waste Management | Ensuring medical waste management in healthcare facilities is properly managed to reduce environmental impact. |
| EV2 Green Material | Promoting the use of biodegradable and recyclable products in medical products to help reduce waste and prevent pollution or natural contamination. | |
| EV3 Green Procurement | Promoting the environmentally friendly procurement of medical products by selecting suppliers that use products and packaging material which support green manufacturing. | |
| EV4 Energy Efficiency | Promoting the use of renewable energy (e.g., solar, wind, and geothermal power), reducing fossil fuel use, and decreasing the carbon footprint from healthcare activities. | |
| EV5 Emissions | Reducing carbon emission and pollution from energy consumption in healthcare systems. Optimizing the use of medical equipment to reduce greenhouse gas emissions. | |
| EV6 Transportation | Reducing the air emissions/pollution from healthcare business travelling and patient/product/staff transportation, by promoting pool vehicles with renewable energy. | |
| EV7 Healthcare Facility Design | Promoting the use of recyclable material in construction of building and furnishing. Reducing the use of non-renewable energy in the construction phase. Promoting the design of healthcare facility concerning for the safety and security for patients and practitioners. | |
| EV8 Legal | The importance of the government laws of energy efficiency regulations on environmental waste, the regulations on waste reduction and waste management in healthcare setting. | |
| EV9 Environmental Certification | Promoting the selection of suppliers that are in the compliance with certification standard, e.g., ISO 14000 standard. | |
| Economic | EC1 Financial | The ability to ensure adequate financial resources, reducing the total cost, while maximizing the revenue growth for the organization. |
| EC2 Process Efficiency | The ability of the firm to transform various resources into value-added output and improve patient and healthcare worker safety by mitigating the risks of supply chain disruptions. | |
| EC3 Investment | The ability to upgrade, invest, and utilize in infrastructure, technology, and service support in healthcare supply chain to enhance efficiency of the firm. | |
| EC4 Marketing | The ability of the firm to develop a unique, competitive profile, and build strong brand awareness and reputation. | |
| EC5 Marketing Strategy | The capability to develop strategies to increase market growth, and execute the strategies to build trust of the firm among stakeholders. | |
| EC6 Relationship Management | The ability to communicate effectively and build a strong relationship among stakeholders that leads to improvement of supply chain by information-sharing and cooperation. | |
| EC7 Service Efficiency | The ability to respond to patient demand and deliver healthcare services, products, and equipment to the patient in a timely manner, that results in improved patient outcomes. | |
| EC8 Leadership and Governance | Providing essential direction, oversight, and accountability. Eliminating the vagueness in decision-making and providing clear direction of the firm. | |
| Technological | TE1 Smart, Wearable Devices | The devices that help in monitoring health status, e.g., smartwatch for monitoring body temperature, blood oxygen level, heart rate, sleep duration, etc. The use of smart devices promotes health awareness, as they are able to alert abnormal detection, such as cardiac arrest. |
| TE2 Health Application | Electronic healthcare applications, such as mobile health (mHealth) in mobile phones, are the tools that allow patients to track their symptoms and help them manage their condition. | |
| TE3 Telemedicine | The medical technology and equipment to conduct diagnosis and treatment plans for the patient in remote areas. It helps to increase medical accessibility during travel restrictions. | |
| TE4 Information Management | The ability to identify and mitigate the risk that may cause supply chain disruption. Promoting stakeholders to share and provide data for tracking and traceability among supply chain stakeholders. | |
| TE5 Cybersecurity | The ability of the healthcare organization to prevent cyber-attacks and ensure patient safety. Promote the measures to protect crucial data of the firm, such as patient information, Electronic Medical Record (EMR), and hospital financial and confidential data. | |
| TE6 Healthcare Robots | Robotics in healthcare aims to promote minimally invasive, fast recovery from the treatment, minimizing the risk of human errors, enhancing patient safety, and reducing the cost of poor quality from the treatment. The robotic in healthcare helps reduce exposure for healthcare workers and patients in case of high-risk infection. | |
| TE7 Transparency and Traceability | The ability to build trust and credibility among stakeholders of the supply chain. Promoting track and traceability to verify the supply chain from upstream to downstream, and mitigate the risks and harm to patients that might occur. | |
| TE8 Healthcare Innovation | Aims to help firms gain competitive advantage, by bringing innovation to support healthcare supply chain and improve safety and efficiency, in both clinical and non-clinical activities. |
Appendix B
| #1 | #2 | #3 | … … | #11 | #12 | #13 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a | b | c | a | b | c | a | b | c | … … | a | b | c | a | b | c | a | b | c | |
| SC1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 |
| SC2 | 0.75 | 0.5 | 1 | 0.75 | 1 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.75 | 1 | 1 | 0.75 | 1 | 1 |
| SC3 | 0.25 | 0.5 | 0.75 | 0.25 | 0.5 | 0.75 | 0.25 | 0.5 | 0.75 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 |
| SC4 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.75 | 1 | 1 | 0.75 | 1 | 1 |
| SC5 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 |
| SC6 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| SC7 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| SC8 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 |
| SC9 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 |
| SC10 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 |
| EV1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0 | 0 | 0.25 |
| EV2 | 0.5 | 0.5 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| EV3 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.25 | 0.5 | 0.75 | 0 | 0 | 0.25 |
| EV4 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 |
| EV5 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.25 | 0.5 | 0.75 | 0 | 0 | 0.25 |
| EV6 | 0.75 | 1 | 1 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 |
| EV7 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 |
| EV8 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0 | 0.25 | 0.5 |
| EV9 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0 | 0 | 0.25 |
| EC1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| EC2 | 0.75 | 0.75 | 1 | 0.25 | 0.5 | 0.75 | 0.75 | 1 | 1 | … … | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.75 | 1 | 1 |
| EC3 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | … … | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 |
| EC4 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| EC5 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 |
| EC6 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | … … | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| EC7 | 0.75 | 1 | 1 | 0.25 | 0.5 | 0.75 | 0.75 | 1 | 1 | … … | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 |
| EC8 | 0.75 | 1 | 1 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 |
| TE1 | 0.25 | 0.5 | 0.75 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.25 | 0.5 | 0.75 |
| TE2 | 0.5 | 0.5 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| TE3 | 0.25 | 0.5 | 0.75 | 0.25 | 0.5 | 0.75 | 0.75 | 1 | 1 | … … | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0 | 0.25 | 0.5 |
| TE4 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 |
| TE5 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 |
| TE6 | 0.5 | 0.75 | 1 | 0.25 | 0.5 | 0.75 | 0.25 | 0.5 | 0.75 | … … | 0.25 | 0.5 | 0.75 | 0.75 | 1 | 1 | 0 | 0.25 | 0.5 |
| TE7 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
| TE8 | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.75 | 1 | 1 | … … | 0.75 | 1 | 1 | 0.5 | 0.75 | 1 | 0.5 | 0.75 | 1 |
References
- Keeble, B.R. United Nations General Assembly. Report of the World Commission on Environment and Development: Our Common Future. Med. War 1988, 4, 17–25. [Google Scholar] [CrossRef]
- Johnston, R.B. Transforming Our World: The 2030 Agenda for Sustainable Development. In Proceedings of the 6th International Congress on Arsenic in the Environment—Arsenic Research and Global Sustainability (AS 2016), Stockholm, Sweden, 19–23 June 2016; pp. 12–14. [Google Scholar] [CrossRef]
- Zhao, W.; Yin, C.; Hua, T.; Meadows, M.E.; Li, Y.; Liu, Y.; Cherubini, F.; Pereira, P.; Fu, B. Achieving the Sustainable Development Goals in the Post-Pandemic Era. Hum. Soc. Sci. Commun. 2022, 9, 258. [Google Scholar] [CrossRef] [PubMed]
- De Aguiar Hugo, A.; da Lima, R.S. Healthcare Waste Management Assessment: Challenges for Hospitals in COVID-19 Pandemic Times. Waste Manag. Res. 2021, 39, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Woolen, S.A.; Kim, C.J.; Hernandez, A.M.; Becker, A.; Martin, A.J.; Kuoy, E.; Pevec, W.C.; Tutton, S. Radiology Environmental Impact: What Is Known and How Can We Improve? Acad. Radiol. 2022, 30, 625–630. [Google Scholar] [CrossRef]
- Wold Health Organization. WHO Timeline—COVID-19. 2020. Available online: https://www.who.int/news/item/27-04-2020-who-timeline---covid-19 (accessed on 1 March 2022).
- Kumar, S.; Raut, R.D.; Narkhede, B.E. A Proposed Collaborative Framework by Using Artificial Intelligence-Internet of Things (AI-IoT) in COVID-19 Pandemic Situation for Healthcare Workers. Int. J. Healthc. Manag. 2020, 13, 337–345. [Google Scholar] [CrossRef]
- Xu, Z.; Elomri, A.; Kerbache, L.; El Omri, A. Impacts of COVID-19 on Global Supply Chains: Facts and Perspectives. IEEE Eng. Manag. Rev. 2020, 48, 153–166. [Google Scholar] [CrossRef]
- Balfour, H. European Pharmaceutical Review. COVID-19 Update: Coronavirus and the Pharmaceutical Supply Chain. 2020. Available online: https://www.europeanpharmaceuticalreview.com/article/116145/covid-19-update-coronavirus-and-the-pharmaceutical-supply-chain/ (accessed on 15 March 2022).
- Jazieh, A.R.; Kozlakidis, Z. Healthcare Transformation in the Post-Coronavirus Pandemic Era. Front. Med. 2020, 7, 429. [Google Scholar] [CrossRef] [PubMed]
- Jeannell, M. Mansur the Effect of Illicit Supply Chains on Patient Safety. Jt. Comm. Int. 2017, 2, 1–12. [Google Scholar]
- Chandra, D.; Kumar, D. Evaluating the Effect of Key Performance Indicators of Vaccine Supply Chain on Sustainable Development of Mission Indradhanush: A Structural Equation Modeling Approach. Omega 2021, 101, 102258. [Google Scholar] [CrossRef]
- WHO. Draft Global Patient Safety Action Plan 2021–2030. In Towards Eliminating Avoidable Harm in Health Care; Angewandte Chemie International Edition; WHO: Geneva, Switzerland, 2021; Volume 6, pp. 951–952. [Google Scholar]
- Supeekit, T.; Somboonwiwat, T.; Kritchanchai, D. Causal Relationship of Supply Chain Efficiency and Patient Safety in Measuring Internal Hospital Supply Chain Performance Applying DEMATEL. In Proceedings of the CIE 2014—44th International Conference on Computers and Industrial Engineering and IMSS 2014—9th International Symposium on Intelligent Manufacturing and Service Systems, Joint International Symposium on “The Social Impacts of Developments in Information, Istanbul, Turkey, 14–16 October 2014; pp. 988–1001. [Google Scholar]
- Supeekit, T.; Somboonwiwat, T.; Kritchanchai, D. DEMATEL-Modified ANP to Evaluate Internal Hospital Supply Chain Performance. Comput. Ind. Eng. 2016, 102, 318–330. [Google Scholar] [CrossRef]
- Duque-Uribe, V.; Sarache, W.; Gutiérrez, E.V. Sustainable Supply Chain Management Practices and Sustainable Performance in Hospitals: A Systematic Review and Integrative Framework. Sustainability 2019, 11, 5949. [Google Scholar] [CrossRef]
- Vali-Siar, M.M.; Roghanian, E. Sustainable, Resilient and Responsive Mixed Supply Chain Network Design under Hybrid Uncertainty with Considering COVID-19 Pandemic Disruption. Sustain. Prod. Consum. 2022, 30, 278–300. [Google Scholar] [CrossRef] [PubMed]
- Ben-Zvi, T.; Luftman, J. Post-Pandemic IT: Digital Transformation and Sustainability. Sustainability 2022, 14, 15275. [Google Scholar] [CrossRef]
- Chandra, M.; Kumar, K.; Thakur, P.; Chattopadhyaya, S.; Alam, F.; Kumar, S. Digital Technologies, Healthcare and COVID-19: Insights from Developing and Emerging Nations. Health Technol. 2022, 12, 547–568. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for Healthcare: Capabilities, Features, Barriers, and Applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Jamil, F.; Hang, L.; Kim, K.H.; Kim, D.H. A Novel Medical Blockchain Model for Drug Supply Chain Integrity Management in a Smart Hospital. Electronics 2019, 8, 505. [Google Scholar] [CrossRef]
- Alhasan, M.; Hasaneen, M. Digital Imaging, Technologies and Artificial Intelligence Applications during COVID-19 Pandemic. Comput. Med. Imaging Graph. 2021, 91, 101933. [Google Scholar] [CrossRef]
- Franchina, L.; Calabrese, A.; Inzerilli, G.; Scatto, E.; Brutti, G.; de los Ángeles Bonanni, M.V. Thinking Green: The Role of Smart Technologies in Transforming Cities’ Waste and Supply Chain’s Flow. Clean. Eng. Technol. 2021, 2, 100077. [Google Scholar] [CrossRef]
- Singh Yadav, A.; Pandey, G.; Kumar Arora, T.; Kumar Chaubey, P. Block-Chain Application Based Economic Impact of Coronavirus Pandemic on Medicine Industry Inventory System for Deteriorating Objects with Two-Warehouse and Wastewater Treatment Using PSO. Mater. Today Proc. 2021, 51, 939–946. [Google Scholar] [CrossRef]
- Subramanian, L. Effective Demand Forecasting in Health Supply Chains: Emerging Trend, Enablers, and Blockers. Logistics 2021, 5, 12. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-Compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, R.; Otero-Neira, C.; Svensson, G. Sustainability Endeavors and Sustainable Development in Spanish Public Hospitals: The Case for Upstream Social Marketing. J. Soc. Mark. 2020, 10, 215–242. [Google Scholar] [CrossRef]
- Serrou, D.; Abouabdellah, A.; Mharzi, H. Proposed an Approach for Measuring the Performance of Hospital Logistics Systems by Integrating Quality, Safety and Environment. Int. J. Sci. Eng. Technol. 2015, 4, 24–27. [Google Scholar] [CrossRef]
- El Farouk, I.I.; Frichi, Y.; Jawab, F. An Innovative Approach to Develop Performance Indicators for Medicines Supply Chain in Moroccan Public Hospitals. Int. J. Sci. Technol. Res. 2020, 9, 386–391. [Google Scholar]
- Tavakol, M.; Dennick, R. Making Sense of Cronbach’s Alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Santos, J.; Santos, A.D.L.; Santos-Mallet; Pinto, J.D.S.; Santos, J.; Santos, J.B.; Ramalho-Santos, J. Cronbach’s Alpha: A Tool for Assessing the Reliability of Scales. J. Ext. 1999, 37, 1–5. [Google Scholar]
- Ishikawa, A. The New Fuzzy Delphi Methods: Economization of GDS (Group Decision Support). In Proceedings of the Annual Hawaii International Conference on System Sciences, Hawaii, HI, USA, 8 January 1993. [Google Scholar]
- Gliem, J.A.; Gliem, R.R. Calculation, Interpreting, and Reporting Cronbach’s Alpha Reliability Coefficient for Likert-Type Scales. In Proceedings of the Midwest Research to Practice Conference in Adult, Continuing, and Community Education, Dublin, Ireland, 28–30 July 2003. [Google Scholar]
- Mohamed, H.A.E.; Eltohamy, A.I. Critical Success Factors for Competitiveness of Egyptian Construction Companies. Sustainability 2022, 14, 10460. [Google Scholar] [CrossRef]
- Kaur, K.; Zarin, I.; Chen, L.E.; Choong, Y.V.; Sze-Siong, C. Constructing a Stress Index for Teachers in Malaysia: A Fuzzy Delphi Approach. Asian J. Univ. Educ. 2022, 18, 606–624. [Google Scholar] [CrossRef]
- Ishikawa, A.; Amagasa, M.; Shiga, T.; Tomizawa, G.; Tatsuta, R.; Mieno, H. The Max-Min Delphi Method and Fuzzy Delphi Method via Fuzzy Integration. Fuzzy Sets Syst. 1993, 55, 241–253. [Google Scholar] [CrossRef]
- Rejeb, A.; Rejeb, K.; Keogh, J.G.; Zailani, S. Barriers to Blockchain Adoption in the Circular Economy: A Fuzzy Delphi and Best-Worst Approach. Sustainability 2022, 14, 3611. [Google Scholar] [CrossRef]
- Borelli, G.; Orrù, P.F.; Zedda, F. Performance Analysis of a Healthcare Supply Chain. A RFID System Implementation Design. In Proceedings of the Summer School Francesco Turco, Brescia, Italy, 11–13 September 2013; pp. 42–47. [Google Scholar]
- Swarnakar, V.; Bagherian, A.; Singh, A.R. Modeling Critical Success Factors for Sustainable LSS Implementation in Hospitals: An Empirical Study. Int. J. Qual. Reliab. Manag. 2022, 39, 1249–1280. [Google Scholar] [CrossRef]
- Rodríguez, R.; Svensson, G.; Otero-Neira, C. Future Direction of Sustainable Development in Private Hospitals: General Similarities and Specific Differences. J. Bus. Ind. Mark. 2020, 35, 537–550. [Google Scholar] [CrossRef]
- Hossain, M.K.; Thakur, V. Drivers of Sustainable Healthcare Supply Chain Performance: Multi-Criteria Decision-Making Approach under Grey Environment. Int. J. Qual. Reliab. Manag. 2022, 39, 859–880. [Google Scholar] [CrossRef]
- Esposito, M.; Kapoor, A.; Goyal, S. Enabling Healthcare Services for the Rural and Semi-Urban Segments in India: When Shared Value Meets the Bottom of the Pyramid. Corp. Gov. 2012, 12, 514–533. [Google Scholar] [CrossRef]
- Kantabutra, S. Sustainable Leadership in a Thai Healthcare Services Provider. Int. J. Health Care Qual. Assur. 2011, 24, 67–80. [Google Scholar] [CrossRef]
- Marimuthu, M.; Paulose, H. Emergence of Sustainability Based Approaches in Healthcare: Expanding Research and Practice. Procedia Soc. Behav. Sci. 2016, 224, 554–561. [Google Scholar] [CrossRef]
- Faezipour, M.; Ferreira, S. A System Dynamics Perspective of Patient Satisfaction in Healthcare. In Procedia Computer Science; Elsevier: Amsterdam, The Netherlands, 2013; Volume 16, pp. 148–156. [Google Scholar]
- Capolongo, S.; Gola, M.; di Noia, M.; Nickolova, M.; Nachiero, D.; Rebecchi, A.; Settimo, G.; Vittori, G.; Buffoli, M. Monographic Section Social Sustainability in Healthcare Facilities: A Rating Tool for Analysing and Improving Social Aspects in Environments of Care. Ann. Ist. Super Sanità 2016, 52, 15–23. [Google Scholar] [CrossRef]
- Meiling, L.; Yahya, F.; Waqas, M.; Shaohua, Z.; Ali, S.A.; Hania, A. Boosting Sustainability in Healthcare Sector through Fintech: Analyzing the Moderating Role of Financial and ICT Development. Inquiry 2021, 58, 00469580211028174. [Google Scholar] [CrossRef]
- Mohamad Taghvaee, V.; Assari Arani, A.; Nodehi, M.; Khodaparast Shirazi, J.; Agheli, L.; Neshat Ghojogh, H.M.; Salehnia, N.; Mirzaee, A.; Taheri, S.; Mohammadi Saber, R.; et al. Sustainable Development Goals: Transportation, Health and Public Policy. Rev. Econ. Political Sci. 2021, 8, 134–161. [Google Scholar] [CrossRef]
- Tejativaddhana, P.; Briggs, D.; Singhadej, O.; Hinoguin, R. Developing Primary Health Care in Thailand: Innovation in the Use of Socio-Economic Determinants, Sustainable Development Goals and the District Health Strategy. Public Adm. Policy 2018, 21, 36–49. [Google Scholar] [CrossRef]
- Faggini, M.; Cosimato, S.; Nota, F.D.; Nota, G. Pursuing Sustainability for Healthcare through Digital Platforms. Sustainability 2019, 11, 165. [Google Scholar] [CrossRef]
- Rejeb, A.; Rejeb, K. Blockchain and Supply Chain Sustainability. Logforum 2020, 16, 363–372. [Google Scholar] [CrossRef]
- Cheang, S.; Lee, J.-D. Evaluation Telecenter Performance in Social Sustainability Context: A Cambodia Case Study. In Proceedings of the 6th International Conference on Advanced Information Management and Service (IMS), Seoul, Republic of Korea, 30 November–2 December 2010. [Google Scholar]
- Garrido, A.; Ramírez López, L.J.; Álvarez, N.B. A Simulation-Based AHP Approach to Analyze the Scalability of EHR Systems Using Blockchain Technology in Healthcare Institutions. Inform. Med. Unlocked 2021, 24, 100576. [Google Scholar] [CrossRef]
- George, S.; Elrashid, S. The Role of Information Technology and Information Sharing in Pharmaceutical Supply Chain Performance: Private Hospitals’ Perspective. In Proceedings of the 2021 International Conference on Decision Aid Sciences and Application (DASA 2021), Online, 7–8 December 2021; Institute of Electrical and Electronics Engineers Inc.: New York, NY, USA, 2021; pp. 601–606. [Google Scholar]
- Rajak, M.; Shaw, K. Evaluation and Selection of Mobile Health (MHealth) Applications Using AHP and Fuzzy TOPSIS. Technol. Soc. 2019, 59, 101186. [Google Scholar] [CrossRef]
- Lee, C.K.M.; Na, C.M.; Kit, N.C. IoT-Based Asset Management System for Healthcare-Related Industries. Int. J. Eng. Bus. Manag. 2015, 2015, 7–19. [Google Scholar] [CrossRef]
- Tajbakhsh, A.; Hassini, E. Performance Measurement of Sustainable Supply Chains: A Review and Research Questions. Int. J. Product. Perform. Manag. 2015, 64, 744–783. [Google Scholar] [CrossRef]
- Nagariya, R.; Kumar, D.; Kumar, I. Enablers to Implement Sustainable Practices in the Service Only Supply Chain: A Case of an Indian Hospital. Bus. Process Manag. J. 2021, 27, 1463–1495. [Google Scholar] [CrossRef]
- Tseng, M.L.; Tan, P.A.; Wu, K.J.; Lin, R.C.W.; Todumrongkul, N.; Juladacha, P.; Christianti, G. Sustainable Total Resource Management in Thailand Healthcare Industry under Uncertain Situations. Sustainability 2020, 12, 9611. [Google Scholar] [CrossRef]
- Ritmak, N.; Rattanawong, W.; Vongmanee, V. A New Dimension of Health Sustainability Model after Pandemic Crisis Using Structural Equation Model. Sustainability 2023, 15, 1616. [Google Scholar] [CrossRef]
- Ritmak, N.; Rattanawong, W.; Vongmanee, V. The Dynamic Evaluation Model of Health Sustainability under MCDM Benchmarking Health Indicator Standards. Int. J. Environ. Res. Public Health 2023, 20, 259. [Google Scholar] [CrossRef]
- Ullah, Z.; Sulaiman, M.A.B.A.; Ali, S.B.; Ahmad, N.; Scholz, M.; Han, H. The Effect of Work Safety on Organizational Social Sustainability Improvement in the Healthcare Sector: The Case of a Public Sector Hospital in Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 6672. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Khan, M.; Ajmal, M.; Sheikh, K.S.; Ahamat, A. A Multi-Stakeholders View of the Barriers of Social Sustainability in Healthcare Supply Chains: Analytic Hierarchy Process Approach. Sustain. Account. Manag. Policy J. 2019, 10, 290–313. [Google Scholar] [CrossRef]
- Majumdar, A.; Shaw, M.; Sinha, S.K. COVID-19 Debunks the Myth of Socially Sustainable Supply Chain: A Case of the Clothing Industry in South Asian Countries. Sustain. Prod. Consum. 2020, 24, 150–155. [Google Scholar] [CrossRef]
- Eizenberg, E.; Jabareen, Y. Social Sustainability: A New Conceptual Framework. Sustainability 2017, 9, 68. [Google Scholar] [CrossRef]
- United Nations Thailand. Oxford Policy Management Social Impact COVID-19 in Thailand; United Nations Thailand: Bangkok, Thailand, 2020. [Google Scholar]
- Hussain, M.; Ajmal, M.M.; Gunasekaran, A.; Khan, M. Exploration of Social Sustainability in Healthcare Supply Chain. J. Clean. Prod. 2018, 203, 977–989. [Google Scholar] [CrossRef]
- D’Eusanio, M.; Zamagni, A.; Petti, L. Social Sustainability and Supply Chain Management: Methods and Tools. J. Clean. Prod. 2019, 235, 178–189. [Google Scholar] [CrossRef]
- Social Impact Assessment of COVID-19 in Thailand. Available online: https://www.unicef.org/thailand/media/5071/file/Social%20Impact%20Assessment%20of%20COVID-19%20in%20Thailand.pdf (accessed on 31 March 2022).
- Mani, V.; Agrawal, R.; Sharma, V. Social Sustainability in the Supply Chain: Analysis of Enablers. Manag. Res. Rev. 2015, 38, 1016–1042. [Google Scholar] [CrossRef]
- Lundin, B.Y.C. Making Sense of Social Sustainability, Agency and Resistance in Sihanoukville, Cambodia. Bachelor’s Thesis, The University of Gothenburg, Gothenburg, Sweden, 2019. [Google Scholar]
- Venkatesh, V.G.; Kang, K.; Wang, B.; Zhong, R.Y.; Zhang, A. System Architecture for Blockchain Based Transparency of Supply Chain Social Sustainability. Robot. Comput. Integr. Manuf. 2020, 63, 101896. [Google Scholar] [CrossRef]
- Khosravi, F.; Izbirak, G. A Stakeholder Perspective of Social Sustainability Measurement in Healthcare Supply Chain Management. Sustain. Cities Soc. 2019, 50, 101681. [Google Scholar] [CrossRef]
- Maghsoudi, T.; Cascón-Pereira, R.; Lara, A.B.H. The Role of Collaborative Healthcare in Improving Social Sustainability: A Conceptual Framework. Sustainability 2020, 12, 3195. [Google Scholar] [CrossRef]
- Rafiaani, P.; Dikopoulou, Z.; Van Dael, M.; Kuppens, T.; Azadi, H.; Lebailly, P.; Van Passel, S. Identifying Social Indicators for Sustainability Assessment of CCU Technologies: A Modified Multi-Criteria Decision Making. Soc. Indic. Res. 2020, 147, 15–44. [Google Scholar] [CrossRef]
- Sarker, M.R.; Moktadir, M.A.; Santibanez-Gonzalez, E.D.R. Social Sustainability Challenges Towards Flexible Supply Chain Management: Post-COVID-19 Perspective. Glob. J. Flex. Syst. Manag. 2021, 22, 199–218. [Google Scholar] [CrossRef]
- Zadeh, R.S.; Xuan, X.; Shepley, M.M. Sustainable Healthcare Design: Existing Challenges and Future Directions for an Environmental, Economic, and Social Approach to Sustainability. Facilities 2016, 34, 264–288. [Google Scholar] [CrossRef]
- Govindan, K.; Shaw, M.; Majumdar, A. Social Sustainability Tensions in Multi-Tier Supply Chain: A Systematic Literature Review towards Conceptual Framework Development. J. Clean. Prod. 2021, 279, 123075. [Google Scholar] [CrossRef]
- Huq, F.A.; Stevenson, M.; Zorzini, M. Social Sustainability in Developing Country Suppliers: An Exploratory Study in the Ready Made Garments Industry of Bangladesh. Int. J. Oper. Prod. Manag. 2014, 34, 610–638. [Google Scholar] [CrossRef]
- Mavridoglou, G.; Polyzos, N. Sustainability of Healthcare Financing in Greece: A Relation Between Public and Social Insurance Contributions and Delivery Expenditures. INQUIRY J. Health Care Organ. Provis. Financ. 2022, 59, 004695802210928. [Google Scholar] [CrossRef] [PubMed]
- Da Maynard, D.C.; Vidigal, M.D.; Farage, P.; Zandonadi, R.P.; Nakano, E.Y.; Botelho, R.B.A. Environmental, Social and Economic Sustainability Indicators Applied to Food Services: A Systematic Review. Sustainability 2020, 12, 1804. [Google Scholar] [CrossRef]
- Kumar, C.; Chaudhary, R. Environmental Sustainability Practices in Hospitals of Bihar. Curr. Res. Environ. Sustain. 2021, 3, 100106. [Google Scholar] [CrossRef]
- Singh, P. Lean in Healthcare Organization: An Opportunity for Environmental Sustainability. Benchmarking 2019, 26, 205–220. [Google Scholar] [CrossRef]
- King, N.R.; Project, P. Kingdom of Cambodia Ministry of Health Updated Environmental and Social. Balance 2020, 8, 2–126. [Google Scholar]
- Yang, X.; Lo, K. Environmental Health Research and the COVID-19 Pandemic: A Turning Point towards Sustainability. Environ. Res. 2021, 197, 111157. [Google Scholar] [CrossRef] [PubMed]
- Jæger, B.; Menebo, M.M.; Upadhyay, A. Identification of Environmental Supply Chain Bottlenecks: A Case Study of the Ethiopian Healthcare Supply Chain. Manag. Environ. Qual. Int. J. 2021, 32, 1233–1254. [Google Scholar] [CrossRef]
- Khalid, S.; Beattie, C.; Sands, J.; Hampson, V. Incorporating the Environmental Dimension into the Balanced Scorecard: A Case Study in Health Care. Meditari Account. Res. 2019, 27, 652–674. [Google Scholar] [CrossRef]
- Manika, D.; Gregory-Smith, D.; Wells, V.K.; Comerford, L.; Aldrich-Smith, L. Linking Environmental Sustainability and Healthcare: The Effects of an Energy Saving Intervention in Two Hospitals. Int. J. Bus. Sci. Appl. Manag. 2016, 11, 32–54. [Google Scholar]
- Wang, Q.; Huang, R. The Impact of COVID-19 Pandemic on Sustainable Development Goals—A Survey. Environ. Res. 2021, 202, 111637. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.R.; Usman, B.; Zaman, K.; Nassani, A.A.; Haffar, M.; Muneer, G. The Impact of Carbon Pricing, Climate Financing, and Financial Literacy on COVID-19 Cases: Go-for-Green Healthcare Policies. Environ. Sci. Pollut. Res. 2022, 29, 35884–35896. [Google Scholar] [CrossRef] [PubMed]
- Tudor, M.A.; Filimon Benea, A.; Bratosin, S.; Romero-Rodríguez, M. COVID-19 Pandemic Lockdown and Religious Mediatization of Social Sustainability. A Case Study of Romania. Int. J. Environ. Res. 2021, 18, 2287. [Google Scholar] [CrossRef]
- Hsu, L.H.; Hsiao, Y.H. Facilitating Green Supply Chain in Dental Care through Kansei Healthscape of Positive Emotions. Int. J. Environ. Res. Public Health 2019, 16, 3507. [Google Scholar] [CrossRef]
- O’mahony, L.; McCarthy, K.; O’donoghue, J.; Teeling, S.P.; Ward, M.; McNamara, M. Using Lean Six Sigma to Redesign the Supply Chain to the Operating Room Department of a Private Hospital to Reduce Associated Costs and Release Nursing Time to Care. Int. J. Environ. Res. Public Health 2021, 18, 11011. [Google Scholar] [CrossRef]
- Sudusinghe, J.I.; Seuring, S. Social Sustainability Empowering the Economic Sustainability in the Global Apparel Supply Chain. Sustainability 2020, 12, 2595. [Google Scholar] [CrossRef]
- Nematollahi, M.; Hosseini-Motlagh, S.M.; Heydari, J. Economic and Social Collaborative Decision-Making on Visit Interval and Service Level in a Two-Echelon Pharmaceutical Supply Chain. J. Clean. Prod. 2017, 142, 3956–3969. [Google Scholar] [CrossRef]
- Taqi, H.M.M.; Ahmed, H.N.; Paul, S.; Garshasbi, M.; Ali, S.M.; Kabir, G.; Paul, S.K. Strategies to Manage the Impacts of the COVID-19 Pandemic in the Supply Chain: Implications for Improving Economic and Social Sustainability. Sustainability 2020, 12, 9483. [Google Scholar] [CrossRef]
- Vuong, Q.H.; Vuong, T.T.; Ho, T.M.; Nguyen, H.V. Psychological and Socio-Economic Factors Affecting Social Sustainability through Impacts on Perceived Health Care Quality and Public Health: The Case of Vietnam. Sustainability 2017, 9, 1456. [Google Scholar] [CrossRef]
- Grundy-Warr, C.; Lin, S. COVID-19 Geopolitics: Silence and Erasure in Cambodia and Myanmar in Times of Pandemic. Eurasian Geogr. Econ. 2020, 61, 493–510. [Google Scholar] [CrossRef]
- Zamiela, C.; Hossain, N.U.I.; Jaradat, R. Enablers of Resilience in the Healthcare Supply Chain: A Case Study of U.S Healthcare Industry during COVID-19 Pandemic. Res. Transp. Econ. 2022, 93, 101174. [Google Scholar] [CrossRef]
- Rajak, S.; Mathiyazhagan, K.; Agarwal, V.; Sivakumar, K.; Kumar, V.; Appolloni, A. Issues and Analysis of Critical Success Factors for the Sustainable Initiatives in the Supply Chain during COVID-19 Pandemic Outbreak in India: A Case Study. Res. Transp. Econ. 2021, 93, 101114. [Google Scholar] [CrossRef]
- El Baz, J.; Ruel, S. Can Supply Chain Risk Management Practices Mitigate the Disruption Impacts on Supply Chains’ Resilience and Robustness? Evidence from an Empirical Survey in a COVID-19 Outbreak Era. Int. J. Prod. Econ. 2021, 233, 107972. [Google Scholar] [CrossRef] [PubMed]
- Dolgui, A.; Ivanov, D. Exploring Supply Chain Structural Dynamics: New Disruptive Technologies and Disruption Risks. Int. J. Prod. Econ. 2020, 229, 107886. [Google Scholar] [CrossRef]
- Alam, S.T.; Ahmed, S.; Ali, S.M.; Sarker, S.; Kabir, G.; Ul-Islam, A. Challenges to COVID-19 Vaccine Supply Chain: Implications for Sustainable Development Goals. Int. J. Prod. Econ. 2021, 239, 108193. [Google Scholar] [CrossRef]
- Joshi, S.; Sharma, M. Impact of Sustainable Supply Chain Management on Performance of SMEs amidst COVID-19 Pandemic: An Indian Perspective. Int. J. Logist. Econ. Glob. 2022, 9, 248. [Google Scholar] [CrossRef]
- Ioan, B.; Nestian, A.; Tiţă, S.-M. Relevance of Key Performance Indicators (KPIs) in a Hospital Performance Management Model. J. East. Eur. Res. Bus. Econ. 2012, 2012, 1. [Google Scholar] [CrossRef]
- Kerr, R.S. Surgery in the 2020s: Implications of Advancing Technology for Patients and the Workforce. Future Healthc. J. 2020, 7, 46. [Google Scholar] [CrossRef] [PubMed]
- What Is the Role of Technology in Strengthening the Healthcare Supply Chain? Available online: https://appinventiv.com/blog/technology-strengthening-healthcare-supply-chain/ (accessed on 22 January 2023).
- Tsarfati, B.; Cojocaru, D. The Importance of Receiving Training in Computerized Technology for Nurses to Maintain Sustainability in the Health System. Sustainability 2022, 14, 15958. [Google Scholar] [CrossRef]
- Musigmann, B.; Von Der Gracht, H.; Hartmann, E. Blockchain Technology in Logistics and Supply Chain Management—A Bibliometric Literature Review from 2016 to January 2020. IEEE Trans. Eng. Manag. 2020, 67, 988–1007. [Google Scholar] [CrossRef]
- Pennestrì, F.; Banfi, G. The Experience of Patients in Chronic Care Management: Applications in Health Technology Assessment (HTA) and Value for Public Health. Int. J. Environ. Res. Public Health 2022, 19, 9868. [Google Scholar] [CrossRef]
- Chen, T.-C.T.; Chiu, M.-C. Evaluating the Sustainability of Smart Technology Applications in Healthcare after the COVID-19 Pandemic: A Hybridising Subjective and Objective Fuzzy Group Decision-Making Approach with Explainable Artificial Intelligence. Digit. Health 2022, 8, 205520762211363. [Google Scholar] [CrossRef]
- Apostolopoulos, S.; Makris, I.; Stavroyiannis, S. Healthcare Innovation in Greece: The Views of Private Health Entrepreneurs on Implementing Innovative Plans. J. Open Innov. Technol. Mark. Complex. 2022, 8, 78. [Google Scholar] [CrossRef]
- Malleeswaran, B.; Uthayakumar, R. A Sustainable Pharmaceutical Supply Chain Model for Household Energy Consumption and Expiration Cost under Decision Making Approach. Clean. Eng. Technol. 2022, 11, 100568. [Google Scholar] [CrossRef]
- Burbano, A.; Rardin, R.; Pohl, E. Exploring the Factors Affecting the Identification Standards Adoption Process in the US Healthcare Supply Chain. In Proceedings of the 2011 PICMET’11: Technology Management in the Energy Smart World (PICMET), Portland, OR, USA, 31 July–4 August 2011. [Google Scholar]
- Stroumpoulis, A.; Kopanaki, E. Theoretical Perspectives on Sustainable Supply Chain Management and Digital Transformation: A Literature Review and a Conceptual Framework. Sustainability 2022, 14, 4862. [Google Scholar] [CrossRef]
| Title of Article | Sustainability Pillar | Reference | ||||
|---|---|---|---|---|---|---|
| EV | EC | SC | TE | Misc | ||
| Performance analysis of a healthcare supply chain. A RFID system implementation design | ✓ | ✓ | ✓ | [38] | ||
| Modeling critical success factors for sustainable LSS implementation in hospitals: an empirical study | ✓ | ✓ | ✓ | [39] | ||
| Future direction of sustainable development in private hospitals: general similarities and specific differences | ✓ | ✓ | ✓ | [40] | ||
| Drivers of sustainable healthcare supply chain performance: multi-criteria decision-making approach under grey environment | ✓ | ✓ | ✓ | [41] | ||
| Enabling healthcare services for the rural and semi-urban segments in India: When shared value meets the bottom of the pyramid | ✓ | ✓ | [42] | |||
| Sustainable leadership in a Thai healthcare services provider | ✓ | [43] | ||||
| Sustainability endeavors and sustainable development in Spanish public hospitals: The case for upstream social marketing | ✓ | ✓ | [27] | |||
| Emergence of Sustainability Based Approaches in Healthcare: Expanding Research and Practice | ✓ | ✓ | ✓ | [44] | ||
| Sustainable, resilient and responsive mixed supply chain network design under hybrid uncertainty with considering COVID-19 pandemic disruption | ✓ | ✓ | ✓ | [17] | ||
| A system dynamics perspective of patient satisfaction in healthcare | ✓ | [45] | ||||
| Monographic section social sustainability in healthcare facilities: a rating tool for analyzing and improving social aspects in environments of care | ✓ | [46] | ||||
| Boosting Sustainability in Healthcare Sector through Fintech: Analyzing the Moderating Role of Financial and ICT Development | ✓ | ✓ | [47] | |||
| Sustainable development goals: transportation, health and public policy | ✓ | ✓ | ✓ | [48] | ||
| Developing primary healthcare in Thailand: Innovation in the use of socio-economic determinants, Sustainable Development Goals and the district health strategy | ✓ | ✓ | [49] | |||
| Pursuing sustainability for healthcare through digital platforms | ✓ | ✓ | [50] | |||
| Blockchain and supply chain sustainability | ✓ | ✓ | ✓ | ✓ | [51] | |
| Evaluation Tele-center Performance in Social Sustainability Context: A Cambodia Case Study | ✓ | ✓ | [52] | |||
| Telemedicine for healthcare: Capabilities, features, barriers, and applications | ✓ | [20] | ||||
| A simulation-based AHP approach to analyze the scalability of EHR systems using blockchain technology in healthcare institutions | ✓ | [53] | ||||
| The Role of Information Technology and Information Sharing in Pharmaceutical Supply Chain Performance: Private hospitals’ perspective | ✓ | ✓ | [54] | |||
| Evaluation and selection of mobile health (mHealth) applications using AHP and fuzzy TOPSIS | ✓ | [55] | ||||
| IoT-based asset management system for healthcare-related industries | ✓ | ✓ | ✓ | [56] | ||
| Performance measurement of sustainable supply chains: A review and research questions | ✓ | ✓ | ✓ | [57] | ||
| Enablers to implement sustainable practices in the service only supply chain: a case of an Indian hospital | ✓ | ✓ | ✓ | [58] | ||
| Sustainable total resource management in Thailand healthcare industry under uncertain situations | ✓ | ✓ | ✓ | [59] | ||
| A New Dimension of Health Sustainability Model after Pandemic Crisis Using Structural Equation Model | ✓ | ✓ | ✓ | ✓ | [60] | |
| The Dynamic Evaluation Model of Health Sustainability under MCDM Benchmarking Health Indicator Standards | ✓ | ✓ | ✓ | ✓ | [61] | |
| The effect of work safety on organizational social sustainability improvement in the healthcare sector: The case of a public sector hospital in Pakistan | ✓ | [62] | ||||
| Dimension | Attributes | Reference |
|---|---|---|
| Social | SC1 Health and Safety | [27,52,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80] |
| SC2 Skills, Knowledge, and Training | ||
| SC3 Community | ||
| SC4 Quality of Care | ||
| SC5 Employment | ||
| SC6 Stakeholder Engagement | ||
| SC7 Equity | ||
| SC8 Clinical Process Efficiency | ||
| SC9 Support Process Efficiency | ||
| SC10 Collaboration | ||
| Environmental | EV1 Waste Management | [5,81,82,83,84,85,86,87,88,89,90,91,92,93] |
| EV2 Green Material | ||
| EV3 Green Procurement | ||
| EV4 Energy Efficiency | ||
| EV5 Emissions | ||
| EV6 Transportation | ||
| EV7 Healthcare Facility Design | ||
| EV8 Legal | ||
| EV9 Environmental Certification | ||
| Economic | EC1 Financial | [24,48,49,77,81,94,95,96,97,98,99,100,101] |
| EC2 Process Efficiency | ||
| EC3 Investment | ||
| EC4 Marketing | ||
| EC5 Marketing Strategy | ||
| EC6 Relationship Management | ||
| EC7 Service Efficiency | ||
| EC8 Leadership and Governance | ||
| Technological | TE1 Smart, Wearable Devices | [18,22,41,42,43,102,103,104,105,106,107,108,109,110,111,112,113,114] |
| TE2 Health Application | ||
| TE3 Telemedicine | ||
| TE4 Information Management | ||
| TE5 Cybersecurity | ||
| TE6 Healthcare Robots | ||
| TE7 Transparency and Traceability | ||
| TE8 Healthcare Innovation |
| Expert No. | Title | Expertise | Years of Work Experience |
|---|---|---|---|
| 1 | Professor | Healthcare Innovation and Technology | >20 years |
| 2 | Professor, M.D. | Medical Doctor, professional in Radiology | >20 years |
| 3 | - | Chief of Finance and Accounting in healthcare organization | 15 years |
| 4 | M.D. | Medical Doctor, specialty in occupational health | >20 years |
| 5 | - | Director of healthcare supply chain | 18 years |
| 6 | Professor, M.D. | Medical Doctor, professional in Urology | >20 years |
| 7 | M.D. | Chief of medical affairs organization | >20 years |
| 8 | M.D. | Medical Director of private healthcare organization | >20 years |
| 9 | M.D. | Chief Executive Officer of private healthcare organization | >20 years |
| 10 | Doctor | Academician and Director of Logistics Research and Institute | >20 years |
| 11 | Professor, M.D. | Medical Doctor, professional in Medical Imaging and Radiation Science | >20 years |
| 12 | M.D. | Medical Doctor, Director of Department of Dentistry | 15 years |
| 13 | Doctor | Professional level, Academician and Expert in International Atomic Energy Agency (IAEA) | >20 years |
| Dimension | Attribute | Triangular Fuzzy Value | Crisp Value | Expert Consensus |
|---|---|---|---|---|
| Social | SC1 | (0.64, 0.89, 1.00) | 0.840 | Accepted |
| SC2 | (0.73, 0.94, 1.00) | 0.891 | Accepted | |
| SC3 | (0.48, 0.73, 0.92) | 0.712 | Rejected | |
| SC4 | (0.67, 0.92, 1.00) | 0.865 | Accepted | |
| SC5 | (0.62, 0.86, 1.00) | 0.827 | Accepted | |
| SC6 | (0.52, 0.75, 0.96) | 0.743 | Rejected | |
| SC7 | (0.54, 0.79, 0.96) | 0.763 | Accepted | |
| SC8 | (0.60, 0.85, 0.98) | 0.808 | Accepted | |
| SC9 | (0.64, 0.89, 1.00) | 0.840 | Accepted | |
| SC10 | (0.65, 0.87, 1.00) | 0.827 | Accepted | |
| Environmental | EV1 | (0.58, 0.80, 0.92) | 0.769 | Accepted |
| EV2 | (0.56, 0.79, 0.98) | 0.776 | Accepted | |
| EV3 | (0.46, 0.69, 0.89) | 0.679 | Rejected | |
| EV4 | (0.56, 0.76, 0.94) | 0.756 | Accepted | |
| EV5 | (0.42, 0.65, 0.83) | 0.635 | Rejected | |
| EV6 | (0.44, 0.69, 0.90) | 0.679 | Rejected | |
| EV7 | (0.56, 0.81, 0.98) | 0.782 | Accepted | |
| EV8 | (0.48, 0.73, 0.90) | 0.705 | Rejected | |
| EV9 | (0.46, 0.73, 0.87) | 0.705 | Rejected | |
| Economic | EC1 | (0.60, 0.85, 1.00) | 0.814 | Accepted |
| EC2 | (0.60, 0.83, 0.98) | 0.801 | Accepted | |
| EC3 | (0.52, 0.73, 0.96) | 0.736 | Rejected | |
| EC4 | (0.48, 0.73, 0.94) | 0.781 | Accepted | |
| EC5 | (0.50, 0.79, 0.94) | 0.743 | Rejected | |
| EC6 | (0.58, 0.83, 1.00) | 0.801 | Accepted | |
| EC7 | (0.62, 0.87, 0.98) | 0.821 | Accepted | |
| EC8 | (0.64, 0.89, 0.98) | 0.833 | Accepted | |
| Technological | TE1 | (0.39, 0.64, 0.87) | 0.628 | Rejected |
| TE2 | (0.50, 0.73, 0.96) | 0.731 | Rejected | |
| TE3 | (0.44, 0.69, 0.89) | 0.673 | Rejected | |
| TE4 | (0.56, 0.81, 0.98) | 0.782 | Accepted | |
| TE5 | (0.56, 0.85, 0.98) | 0.808 | Accepted | |
| TE6 | (0.35, 0.60, 0.83) | 0.590 | Rejected | |
| TE7 | (0.58, 0.83,1.00) | 0.801 | Accepted | |
| TE8 | (0.62, 0.87, 1.00) | 0.827 | Accepted |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanokphanvanich, C.; Rattanawong, W.; Vongmanee, V. A New Model for a Sustainable Healthcare Supply Chain Prioritizes Patient Safety: Using the Fuzzy Delphi Method to Identify Healthcare Workers’ Perspectives. Sustainability 2023, 15, 7123. https://doi.org/10.3390/su15097123
Kanokphanvanich C, Rattanawong W, Vongmanee V. A New Model for a Sustainable Healthcare Supply Chain Prioritizes Patient Safety: Using the Fuzzy Delphi Method to Identify Healthcare Workers’ Perspectives. Sustainability. 2023; 15(9):7123. https://doi.org/10.3390/su15097123
Chicago/Turabian StyleKanokphanvanich, Chayada, Wanchai Rattanawong, and Varin Vongmanee. 2023. "A New Model for a Sustainable Healthcare Supply Chain Prioritizes Patient Safety: Using the Fuzzy Delphi Method to Identify Healthcare Workers’ Perspectives" Sustainability 15, no. 9: 7123. https://doi.org/10.3390/su15097123
APA StyleKanokphanvanich, C., Rattanawong, W., & Vongmanee, V. (2023). A New Model for a Sustainable Healthcare Supply Chain Prioritizes Patient Safety: Using the Fuzzy Delphi Method to Identify Healthcare Workers’ Perspectives. Sustainability, 15(9), 7123. https://doi.org/10.3390/su15097123







