A Holistic View on the Adoption and Cost-Effectiveness of Technology-Driven Supply Chain Management Practices in Healthcare
Abstract
1. Introduction
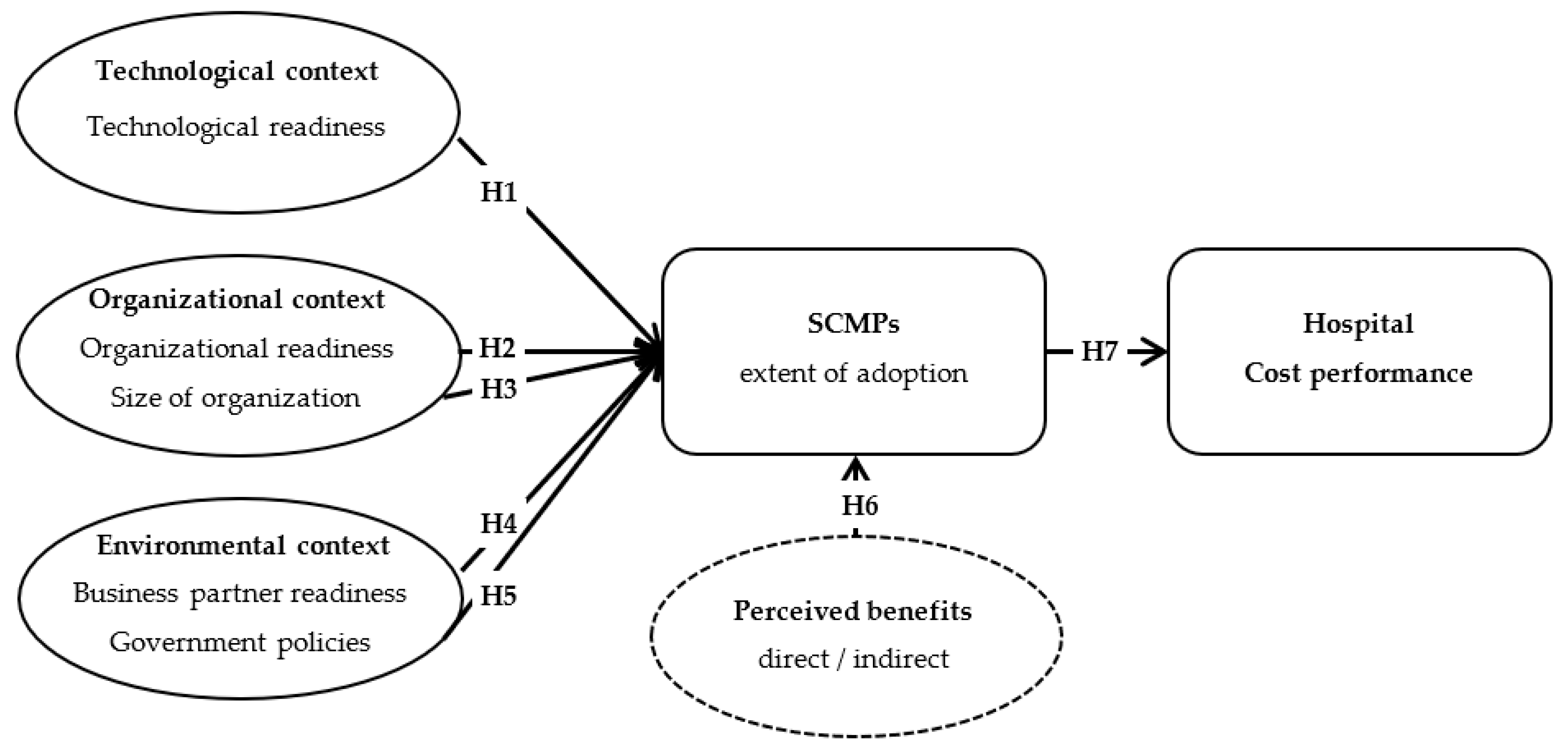
2. Research Framework and Hypotheses Development
2.1. Extent of Hospital SCMPs Adoption
2.2. Technological Context of a Hospital’s Adoption of SCMPs
2.3. Organizational Context of a Hospital’s Adoption of SCMPs
2.4. Environmental Context of a Hospital’s Adoption of SCMPs
2.5. Perceived Benefits as an Influencing Factor for the Extent of SCMP Adoption in Hospitals
2.6. Effect of the Extent of SCMP Adoption on the Cost Performance of Hospitals
3. Research Methodology
4. Data Analysis and Results
4.1. Measurement Model Results
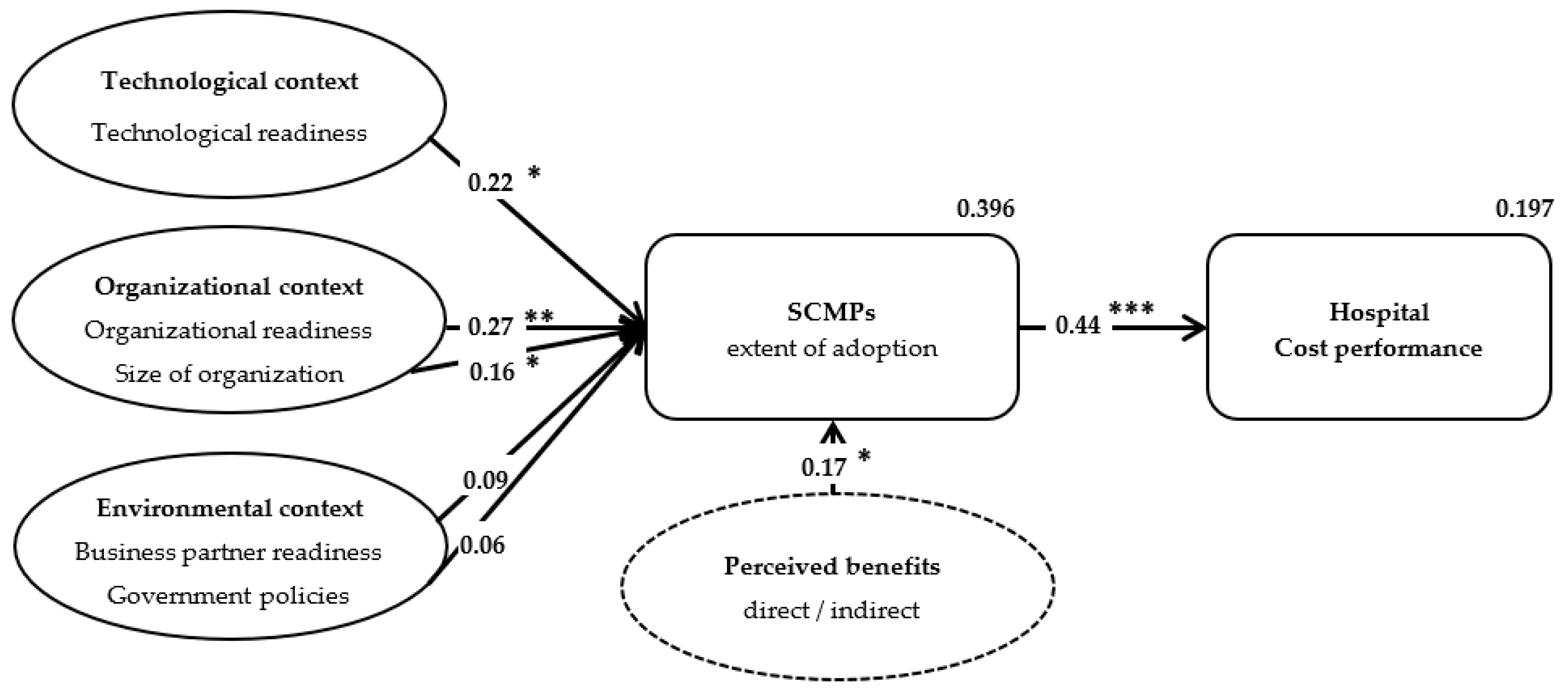
4.2. Structural Model Results
4.3. Endogeneity and Robustness
5. Conclusions
5.1. Scholarly Implications
5.2. Managerial Implications
6. Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hwang, J.; Christensen, C.M. Disruptive innovation in health care delivery: A framework for business-model innovation. Health Aff. 2008, 27, 1329–1335. [Google Scholar] [CrossRef]
- Gartner Research. The Gartner Healthcare Supply Chain Top 25 for 2021. 2020. Available online: https://www.gartner.com/en/webinars/4006369/the-2021-gartner-healthcare-supply-chain-top-25 (accessed on 17 February 2022).
- Varghese, V.; Rossetti, M.; Pohl, E.; Apras, S.; Marek, D. Applying actual usage inventory management best practice in a health care supply chain. Int. J. Supply Chain. Manag. 2012, 1, 1–10. [Google Scholar]
- Habib, M.M.; Chowdhury, F.; Sabah, S.; Debnath, D. A Study on Hospital Supply Chain Management. Am. J. Ind. Bus. Manag. 2022, 12, 806–823. [Google Scholar] [CrossRef]
- Schneller, E.S.; Smeltzer, L.R. Strategic Management of the Health Care Supply Chain; Jossey-Bass: San Francisco, CA, USA, 2006. [Google Scholar]
- Dobrzykowski, D.D.; McFadden, K.L.; Vonderembse, M.A. Examining pathways to safety and financial performance in hospitals: A study of lean in professional service operations. J. Oper. Manag. 2016, 42, 39–51. [Google Scholar] [CrossRef]
- Shi, M.; Yu, W. Supply chain management and financial performance: Literature review and future directions. Int. J. Oper. Prod. Manag. 2013, 33, 1283–1317. [Google Scholar] [CrossRef]
- De Vries, J.; Huijsman, R. Supply chain management in health services: An overview. Supply Chain. Manag. Int. J. 2011, 16, 159–165. [Google Scholar] [CrossRef]
- Damali, U.; Kocakulah, M.; Ozkul, A.S. Investigation of Cloud ERP Adoption in the Healthcare Industry Through Technology-Organization-Environment (TOE) Framework: Qualitative Study. Int. J. Healthc. Inf. Syst. Inform. 2021, 16, 1–4. [Google Scholar] [CrossRef]
- Venkatesh, V.; Bala, H. Technology acceptance model 3 and a research agenda on interventions. Decis. Sci. 2008, 39, 273–315. [Google Scholar] [CrossRef]
- Tornatzky, L.G.; Fleischer, M.; Chakrabarti, A.K. Processes of Technological Innovation; Lexington Books: Lanham, MD, USA, 1990. [Google Scholar]
- Thong, J.Y. An integrated model of information systems adoption in small businesses. J. Manag. Inf. Syst. 1999, 15, 187–214. [Google Scholar] [CrossRef]
- Chau, P.Y.; Hui, K.L. Determinants of small business EDI adoption: An empirical investigation. J. Organ. Comput. Electron. Commer. 2001, 11, 229–252. [Google Scholar] [CrossRef]
- Gibbs, J.L.; Kraemer, K.L. A cross-country investigation of the determinants of scope of e-commerce use: An institutional approach. Electron. Mark. 2004, 14, 124–137. [Google Scholar] [CrossRef]
- Hwang, B.-N.; Huang, C.-Y.; Wu, C.-H. A TOE Approach to Establish a Green Supply Chain Adoption Decision Model in the Semiconductor Industry. Sustainability 2016, 8, 168. [Google Scholar] [CrossRef]
- Lutfi, A.; Alshira’h, A.F.; Alshirah, M.H.; Al-Okaily, M.; Alqudah, H.; Saad, M.; Ibrahim, N.; Abdelmaksoud, O. Antecedents and Impacts of Enterprise Resource Planning System Adoption among Jordanian SMEs. Sustainability 2022, 14, 3508. [Google Scholar] [CrossRef]
- Gangwar, H.; Date, H.; Ramaswamy, R. Understanding determinants of cloud computing adoption using an integrated TAM-TOE model. J. Enterp. Inf. Manag. 2015, 28, 107–130. [Google Scholar] [CrossRef]
- Malik, S.; Chadhar, M.; Vatanasakdakul, S.; Chetty, M. Factors Affecting the Organizational Adoption of Blockchain Technology: Extending the Technology–Organization–Environment (TOE) Framework in the Australian Context. Sustainability 2021, 13, 9404. [Google Scholar] [CrossRef]
- Fiaz, M.; Ikram, A.; Ilyas, A. Enterprise resource planning systems: Digitization of healthcare service quality. Adm. Sci. 2018, 8, 38. [Google Scholar] [CrossRef]
- Kalchschmidt, M. Best practices in demand forecasting: Tests of universalistic, contingency and configurational theories. Int. J. Prod. Econ. 2012, 140, 782–793. [Google Scholar] [CrossRef]
- Morita, M.; Flynn, E.J. The linkage among management systems, practices and behaviour in successful manufacturing strategy. Int. J. Oper. Prod. Manag. 1997, 17, 967–993. [Google Scholar] [CrossRef]
- Blanchard, D. Supply Chain Management Best Practices; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar]
- Cai, J.; Liu, X.; Xiao, Z.; Liu, J. Improving supply chain performance management: A systematic approach to analyzing iterative KPI accomplishment. Decis. Support Syst. 2009, 46, 512–521. [Google Scholar] [CrossRef]
- Wyatt, J. Scorecards, dashboards, and KPIs keys to integrated performance measurement. Healthc. Financ. Manag. 2004, 58, 76–81. [Google Scholar]
- Beier, F.J. The management of the supply chain for hospital pharmacies: A focus on inventory management practices. J. Bus. Logist. 1995, 16, 153–173. [Google Scholar]
- Ramanathan, R. ABC inventory classification with multiple-criteria using weighted linear optimization. Comput. Oper. Res. 2006, 33, 695–700. [Google Scholar] [CrossRef]
- Danas, K.; Roudsari, A.; Ketikidis, P.H. The applicability of a multi-attribute classification framework in the healthcare industry. J. Manuf. Technol. Manag. 2006, 17, 772–785. [Google Scholar] [CrossRef]
- Van Wassenhove, L.N.; Pedraza Martinez, A.J. Using OR to adapt supply chain management best practices to humanitarian logistics. Int. Trans. Oper. Res. 2012, 19, 307–322. [Google Scholar] [CrossRef]
- Mettler, T.; Rohner, P. Supplier relationship management: A case study in the context of health care. J. Theor. Appl. Electron. Commer. Res. 2009, 4, 58–71. [Google Scholar] [CrossRef]
- Kannan, V.R.; Tan, K.C. Supplier selection and assessment: Their impact on business performance. J. Supply Chain Manag. 2002, 38, 11–21. [Google Scholar] [CrossRef]
- Tan, K.C.; Kannan, V.R.; Handfield, R.B. Supply chain management: Supplier performance and firm performance. J. Supply Chain. Manag. 1998, 34, 2. [Google Scholar]
- Puschmann, T.; Alt, R. Successful use of e-procurement in supply chains. Supply Chain. Manag. Int. J. 2005, 10, 122–133. [Google Scholar] [CrossRef]
- Smith, A.D.; Flanegin, F.R. E-procurement and automatic identification: Enhancing supply chain management in the healthcare industry. Int. J. Electron. Healthc. 2004, 1, 176–198. [Google Scholar] [CrossRef]
- Yao, W.; Chu, C.H.; Li, Z. The adoption and implementation of RFID technologies in healthcare: A literature review. J. Med. Syst. 2012, 36, 3507–3525. [Google Scholar] [CrossRef]
- Lee, C.P.; Shim, J.P. An exploratory study of radio frequency identification (RFID) adoption in the healthcare industry. Eur. J. Inf. Syst. 2007, 16, 712–724. [Google Scholar] [CrossRef]
- Zhu, K.; Kraemer, K.L.; Xu, S. The process of innovation assimilation by firms in different countries: A technology diffusion perspective on e-business. Manag. Sci. 2006, 52, 1557–1576. [Google Scholar] [CrossRef]
- Spina, D.; Di Serio, L.C.; Brito, L.A.; Duarte, A.L. The Influence of Supply Chain Management Practices in the Enterprise Performance. Am. J. Manag. 2015, 15, 54–63. [Google Scholar]
- Greco, S.; Ishizaka, A.; Tasiou, M.; Torrisi, G. On the methodological framework of composite indices: A review of the issues of weighting, aggregation, and robustness. Soc. Indic. Res. 2017, 141, 61–94. [Google Scholar] [CrossRef]
- Spetz, J.; Baker, L.C. Has Managed Care Affected the Availability of Medical Technology? Public Policy Institute of California: San Francisco, CA, USA, 1999. [Google Scholar]
- Autry, C.W.; Grawe, S.J.; Daugherty, P.J.; Richey, R.G. The effects of technological turbulence and breadth on supply chain technology acceptance and adoption. J. Oper. Manag. 2010, 28, 522–536. [Google Scholar] [CrossRef]
- Oliveira, T.; Martins, M.F. Understanding e-business adoption across industries in European countries. Ind. Manag. Data Syst. 2010, 110, 1337–1354. [Google Scholar] [CrossRef]
- Zhu, K.; Kraemer, K.L. Post-adoption variations in usage and value of e-business by organizations: Cross-country evidence from the retail industry. Inf. Syst. Res. 2005, 16, 61–84. [Google Scholar] [CrossRef]
- Lin, H.F.; Lin, S.M. Determinants of e-business diffusion: A test of the technology diffusion perspective. Technovation 2008, 28, 135–145. [Google Scholar] [CrossRef]
- Sanja, M.M. Impact of enterprise resource planning system in health care. Int. J. Acad. Res. Bus. Soc. Sci. 2013, 3, 404. [Google Scholar] [CrossRef]
- Ruivo, P.; Johansson, B.; Oliveira, T.; Neto, M. Commercial ERP systems and user productivity: A study across European SMEs. Procedia Technol. 2013, 9, 84–93. [Google Scholar] [CrossRef]
- Pan, M.J.; Jang, W.Y. Determinants of the adoption of enterprise resource planning within the technology-organization-environment framework: Taiwan’s communications industry. J. Comput. Inf. Syst. 2008, 48, 94–102. [Google Scholar]
- Zhen, Z.; Yousaf, Z.; Radulescu, M.; Yasir, M. Nexus of digital organizational culture, capabilities, organizational readiness, and innovation: Investigation of SMEs operating in the digital economy. Sustainability 2021, 13, 720. [Google Scholar] [CrossRef]
- Chwelos, P.; Benbasat, I.; Dexter, A.S. Empirical test of an EDI adoption model. Inf. Syst. Res. 2001, 12, 304–321. [Google Scholar] [CrossRef]
- Ghaleb, E.A.A.; Dominic, P.D.D.; Fati, S.M.; Muneer, A.; Ali, R.F. The Assessment of Big Data Adoption Readiness with a Technology–Organization–Environment Framework: A Perspective towards Healthcare Employees. Sustainability 2021, 13, 8379. [Google Scholar] [CrossRef]
- Lee, G.; Xia, W. Organizational size and IT innovation adoption: A meta-analysis. Inf. Manag. 2006, 43, 975–985. [Google Scholar] [CrossRef]
- Hung, S.Y.; Hung, W.H.; Tsai, C.A.; Jiang, S.C. Critical factors of hospital adoption on CRM system: Organizational and information system perspectives. Decis. Support Syst. 2010, 48, 592–603. [Google Scholar] [CrossRef]
- Giancotti, M.; Guglielmo, A.; Mauro, M. Efficiency and optimal size of hospitals: Results of a systematic search. PLoS ONE 2017, 12, e0174533. [Google Scholar] [CrossRef]
- Saeed, M.A.; Kersten, W. Drivers of sustainable supply chain management: Identification and classification. Sustainability 2019, 11, 1137. [Google Scholar] [CrossRef]
- Mitropoulos, P.; Mitropoulos, I.; Sissouras, A. Managing for efficiency in health care: The case of Greek public hospitals. Eur. J. Health Econ. 2013, 14, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Truman, G.E. Integration in electronic exchange environments. J. Manag. Inf. Syst. 2000, 17, 209–244. [Google Scholar]
- Soares-Aguiar, A.; Palma-Dos-Reis, A. Why do firms adopt e-procurement systems. Using logistic regression to empirically conceptual model. IEEE Trans. Eng. Manag. 2008, 55, 120–133. [Google Scholar] [CrossRef]
- Global Healthcare Exchange. Applying Supply Chain Best Practices from Other Industries to Healthcare; Global Healthcare Exchange: Louisville, CO, USA, 2011. [Google Scholar]
- Friday, D.; Savage, D.A.; Melnyk, S.A.; Harrison, N.; Ryan, S.; Wechtler, H. A collaborative approach to maintaining optimal inventory and mitigating stockout risks during a pandemic: Capabilities for enabling health-care supply chain resilience. J. Humanit. Logist. Supply Chain. Manag. 2021, 11, 248–271. [Google Scholar] [CrossRef]
- Lin, C.Y.; Ho, Y.H. RFID technology adoption and supply chain performance: An empirical study in China’s logistics industry. Supply Chain. Manag. Int. J. 2009, 14, 369–378. [Google Scholar] [CrossRef]
- Lee, S.; Jung, K. A meta-analysis of determinants of RFID adoption around the world: Organization, technology, and public policy. Asia Pac. J. Innov. Entrep. 2016, 10, 67–90. [Google Scholar] [CrossRef]
- Ramanathan, R.; Ramanathan, U.; Ko, L.W. Adoption of RFID technologies in UK logistics: Moderating roles of size, barcode experience and government support. Expert Syst. Appl. 2014, 41, 230–236. [Google Scholar] [CrossRef]
- Pateli, A.; Mylonas, N.; Spyrou, A. Organizational Adoption of Social Media in the Hospitality Industry: An Integrated Approach Based on DIT and TOE Frameworks. Sustainability 2020, 12, 7132. [Google Scholar] [CrossRef]
- Hong, W.; Zhu, K. Migrating to internet-based e-commerce: Factors affecting e-commerce adoption and migration at the firm level. Inf. Manag. 2006, 43, 204–221. [Google Scholar] [CrossRef]
- Iacovou, C.L.; Benbasat, I.; Dexter, A.S. Electronic data interchange and small organizations: Adoption and impact of technology. MIS Q. 1995, 19, 465–485. [Google Scholar] [CrossRef]
- Avgar, A.C.; Litwin, A.S.; Pronovost, P.J. Drivers and barriers in health IT adoption: A proposed framework. Appl. Clin. Inform. 2012, 3, 488–500. [Google Scholar] [PubMed]
- Menachemi, N.; Saunders, C.; Chukmaitov, A.; Matthews, M.C.; Brooks, R.G. Hospital adoption of information technologies and improved patient safety: A study of 98 hospitals in Florida. J. Healthc. Manag. 2007, 52, 398–411. [Google Scholar] [CrossRef]
- McCullough, J.S.; Casey, M.; Moscovice, I.; Prasad, S. The effect of health information technology on quality in US hospitals. Health Aff. 2010, 29, 647–654. [Google Scholar] [CrossRef]
- Sharma, L.; Chandrasekaran, A.; Boyer, K.K.; McDermott, C.M. The impact of health information technology bundles on hospital performance: An econometric study. J. Oper. Manag. 2016, 41, 25–41. [Google Scholar] [CrossRef]
- McCone, B. Terminology and Applications: Hospital Performance Measures. In Measurement and Analysis in Transforming Healthcare Delivery; Springer International Publishing: Cham, Switzerland, 2017; pp. 7–23. [Google Scholar]
- BI-Health. Business Intelligence Portal of National Healthcare System. 2017. Available online: https://portal.bi.moh.gov.gr/el (accessed on 23 March 2017).
- Ketokivi, M.; McIntosh, C.N. Addressing the endogeneity dilemma in operations management research: Theoretical, empirical, and pragmatic considerations. J. Oper. Manag. 2017, 52, 1–14. [Google Scholar] [CrossRef]
- Lian, J.W.; Yen, D.C.; Wang, Y.T. An exploratory study to understand the critical factors affecting the decision to adopt cloud computing in Taiwan hospital. Int. J. Inf. Manag. 2014, 34, 28–36. [Google Scholar] [CrossRef]
- Lumsden, J.R.I.; Anabel, G. Understanding the determinants of cloud computing adoption within the UK. In Proceedings of the European, Mediterranean and Middle Eastern Conference on Information Systems, Windsor, UK, 17–18 October 2013. [Google Scholar]
- Hsu, P.F.; Kraemer, K.L.; Dunkle, D. Determinants of e-business use in US firms. Int. J. Electron. Commer. 2006, 10, 9–45. [Google Scholar] [CrossRef]
- Teo, T.S.H.; Ranganathan, C. Adopters and non-adopters of business- to-business electronic commerce in Singapore. Inf. Manag. 2004, 42, 89–102. [Google Scholar] [CrossRef]
- Oliveira, T.; Thomas, M.; Espadanal, M. Assessing the determinants of cloud computing adoption: An analysis of the manufacturing and services sectors. Inf. Manag. 2014, 51, 497–510. [Google Scholar] [CrossRef]
- Premkumar, G.; Ramamurthy, K. The role of interorganizational and organizational factors on the decision mode for adoption of interorganizational systems. Decis. Sci. 1995, 26, 303–336. [Google Scholar] [CrossRef]
- Rogers, E.M. Diffusion of Innovations; Simon and Schuster: New York, NY, USA, 2010. [Google Scholar]
- Kimberly, J.R.; Evanisko, M.J. Organizational innovation: The influence of individual, organizational, and contextual factors on hospital adoption of technological and administrative innovations. Acad. Manag. J. 1981, 24, 689–713. [Google Scholar] [CrossRef]
- Wang, Y.M.; Wang, Y.S.; Yang, Y.F. Understanding the determinants of RFID adoption in the manufacturing industry. Technol. Forecast. Soc. Chang. 2010, 77, 803–815. [Google Scholar] [CrossRef]
- Low, C.; Chen, Y.; Wu, M. Understanding the determinants of cloud computing adoption. Ind. Manag. Data Syst. 2011, 111, 1006–1023. [Google Scholar] [CrossRef]
- Crow, M.M.; Nath, S. Technology strategy development in Japanese industry: An assessment of market and government influences. Technovation 1990, 10, 333–346. [Google Scholar] [CrossRef]
- Arunachalam, V. Electronic data interchange: Issues in adoption and management. Inf. Resour. Manag. J. 1997, 10, 22–31. [Google Scholar] [CrossRef]
- Pinsonneault, A.; Kraemer, K. Survey research methodology in management information systems: An assessment. J. Manag. Inf. Syst. 1993, 10, 75–105. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879. [Google Scholar] [CrossRef]
- Lin, I.F.; Schaeffer, N.C. Using survey participants to estimate the impact of nonparticipation. Public Opin. Q. 1995, 59, 236–258. [Google Scholar] [CrossRef]
- Arbuckle, J. IBM SPSS and AMOS (Version 22.0) User Guide; IBM: New York, NY, USA, 2015. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Zhang, H. Structural equation modeling. In Models and Methods for Management Science; Springer Nature: Singapore, 2022; pp. 363–381. [Google Scholar]
- Antonakis, J.; Bendahan, S.; Jacquart, P.; Lalive, R. Causality and endogeneity: Problems and solutions. Oxf. Handb. Leadersh. Organ. 2014, 1, 93–117. [Google Scholar]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Tatham, R.L. Multivariate Data Analysis; Prentice Hall: Upper Saddle River, NJ, USA, 1998; Volume 5, pp. 207–219. [Google Scholar]
- Bagozzi, R.P.; Yi, Y.; Phillips, L.W. Assessing Construct Validity in Organizational Research; Administrative Science Quarterly. Digital Society; Springer: New York, NY, USA, 1991; pp. 421–458. [Google Scholar]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 2003, 8, 23–74. [Google Scholar]
- Boyer, K.K.; Gardner, J.W.; Schweikhart, S. Process quality improvement: An examination of general vs. outcome-specific climate and practices in hospitals. J. Oper. Manag. 2012, 30, 325–339. [Google Scholar] [CrossRef]
- Zhao, X.; Huo, B.; Selen, W.; Yeung, J.H.Y. The impact of internal integration and relationship commitment on external integration. J. Oper. Manag. 2011, 29, 17–32. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Sörbom, D. LISREL 8: Structural Equation Modeling with the SIMPLIS Command Language; Scientific Software International: Skokie, IL, USA, 1993. [Google Scholar]
- Steiger, J.H. Structural model evaluation and modification: An interval estimation approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with EQS and EQS/Windows: Basic Concepts, Applications, and Programming; Sage: Thousand Oaks, OK, USA, 1994. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Conley, T.G.; Hansen, C.B.; Rossi, P.E. Plausibly exogenous. Rev. Econ. Stat. 2012, 94, 260–272. [Google Scholar] [CrossRef]
- Schmidt, F.L.; Hunter, J.E. Methods of Meta-Analysis: Correcting Error and Bias in Research Findings; Sage Publications: Thousand Oaks, OK, USA, 2014. [Google Scholar]
- Bendig, D.; Strese, S.; Brettel, M. The link between operational leanness and credit ratings. J. Oper. Manag. 2017, 52, 46–55. [Google Scholar] [CrossRef]
- Chen, D.Q.; Preston, D.S.; Xia, W. Enhancing hospital supply chain performance: A relational view and empirical test. J. Oper. Manag. 2013, 31, 391–408. [Google Scholar] [CrossRef]
- Gorane, S.; Kant, R. Supply chain practices and organizational performance: An empirical investigation of Indian manufacturing organizations. Int. J. Logist. Manag. 2017, 28, 75–101. [Google Scholar] [CrossRef]
| SCMP Clusters | Description | Underlying Technologies | References | Saidin Index Weighting | |
|---|---|---|---|---|---|
| SCMP1 | Inventory management KPI tracking and reporting |
|
| Cai et al. [23] Wyatt [24] | 0.47 |
| SCMP2 | Inventory replenishment optimization |
|
| Varghese et al. [3] Beier [25] | 0.73 |
| SCMP3 | Data segmentation |
|
| Varghese et al. [3] Ramanathan [26] Danas et al. [27] | 0.27 |
| SCMP4 | Demand forecasting |
|
| Van Wassenhove [28] Kalchschmidt [20] Varghese et al. [3] | 0.45 |
| SCMP5 | Supplier evaluation |
|
| Mettler and Rohner [29] Kannan and Tan [30] Tan et al. [31] | 0.70 |
| SCMP6 | Web-based procurement |
|
| Puschmann and Alt [32] Smith and Flanegin [33] | 0.35 |
| SCMP7 | Asset tracking |
|
| Yao et al. [34] Blanchard [22] Lee and Shim [35] | 0.72 |
| SCMP8 | Supplier integration |
|
| Schneller and Smeltzer [5] Chau and Hui [13] | 0.79 |
| Construct | Adapted Sources for Constructs | Items | Item Descriptions | |
|---|---|---|---|---|
| Technological context | Technological readiness | Lian et al. [72] | TR1 | Sufficient IT infrastructure (HW/SW) |
| Lumsden and Anabel [73] | TR2 | IT resources with adequate expertise | ||
| Hsu et al. [74] Teo and Ranganathan [75] Chau and Hui [13] | TR3 TR4 TR5 TR6 TR7 | Level of integration of internal IT applications IT system adaptability to new requirements Adequate use of ERP system Level of spending on new technologies Integration capability with external systems | ||
| Organizational context | Organizational readiness | Oliveira et al. [76] | OR1 | Organization’s favorable attitude toward change |
| Lian et al. [72] | OR2 | Personnel competent with new technologies | ||
| Teo and Ranganathan [75] Premkumar and Ramamurthy [77] Rogers [78] | OR3 OR4 OR5 | Top management support Cross-departmental cooperation Regularity of personnel training | ||
| Organization size (single item) | Hung et al. [51] Kimberly and Evanisko [79] | SIZE | Classification of hospitals based on the number of beds | |
| Environmental context | Business partner readiness | Wang et al. [80] | BPI1 | Business partners’ capabilities |
| Chau and Hui [13] | BPI2 | Recommended by business partners | ||
| Hsu et al. [74] | BPI3 BPI4 | Requested by business partners Cooperation level with business partners | ||
| Government policies | Oliveira et al. (2014) | GPI1 | Supported by government policies | |
| Lian et al. [76] | GPI2 | Mandated by government policies | ||
| Chau and Hui [13] Low et al. [81] Crow [82] | GPI3 GPI4 | Sufficient regulatory environment Government incentives | ||
| Perceived Benefits | Perceived benefits | Low et al. [81] | PB1 | Reduced supply chain costs |
| (direct & indirect) | Wang et al. [80] | PB2 | Improved supply chain process efficiency | |
| Arunachalam [83] Iacovou et al. [64] | PB3 PB4 | Improved quality of care Other resulting indirect benefits |
| Goodness-of-Fit Indices | Recommended Value (Source) | Measurement Model Result |
|---|---|---|
| Absolute fit | ||
| χ2/df Chi-square/Degrees of freedom | <3.00 (Jöreskog and Sörbom) [97] | 1.047 |
| GFI Goodness-of-Fit Index | >0.90 (Jöreskog and Sörbom) [97] | 0.901 |
| AGFI Adjusted Goodness-of-Fit Index | >0.85 (Jöreskog and Sörbom) [97] | 0.851 |
| RMSEA Root Mean Square Error of Approximation | <0.05 (Steiger) [98] | 0.022 |
| Incremental fit | ||
| IFI Incremental Fit Index | >0.95 (Hu and Bentler) [99] | 0.993 |
| NFI Normed Fit Index | >0.90 (Byrne,) [100] | 0.864 |
| TLI (NNFI) Tucker Lewis Index | >0.95 (Hu and Bentler) [99] | 0.990 |
| CFI Comparative Fit Index | >0.95 (Hu and Bentler) [99] | 0.993 |
| CR | AVE | TR | OR | BR | PB | GP | |
|---|---|---|---|---|---|---|---|
| TR | 0.829 | 0.618 | 0.786 | ||||
| OR | 0.749 | 0.508 | 0.589 | 0.713 | |||
| BR | 0.754 | 0.511 | 0.127 | 0.369 | 0.715 | ||
| PB | 0.768 | 0.529 | 0.059 | 0.104 | 0.411 | 0.727 | |
| GP | 0.849 | 0.654 | 0.602 | 0.554 | 0.410 | 0.368 | 0.809 |
| Goodness-of-Fit Indices | Recommended Value (Source) | Structural Model Result |
|---|---|---|
| Absolute fit | ||
| χ2/df Chi-square/Degrees of freedom | <3.00 (Jöreskog and Sörbom) [97] | 1.108 |
| GFI Goodness-of-Fit Index | >0.90 (Jöreskog and Sörbom) [97] | 0.984 |
| AGFI Adjusted Goodness-of-Fit Index | >0.85 (Jöreskog and Sörbom) [97] | 0.904 |
| RMSEA Root Mean Square Error of Approximation | <0.05 (Steiger) [98] | 0.033 |
| Incremental fit | ||
| IFI Incremental Fit Index | >0.95 (Hu and Bentler) [99] | 0.997 |
| NFI Normed Fit Index | >0.90 (Byrne) [100] | 0.966 |
| TLI (NNFI) Tucker Lewis Index | >0.95 (Hu and Bentler) [99] | 0.982 |
| CFI Comparative Fit Index | >0.95 (Hu and Bentler) [99] | 0.996 |
| Hypotheses | Path from | Path to | r2 | t-Value | Path Coeff. | p-Value | Supported |
|---|---|---|---|---|---|---|---|
| H1 | Technological readiness | 2.069 | 0.22 * | 0.039 | Yes | ||
| H2 | Organizational readiness | 2.721 | 0.27 ** | 0.007 | Yes | ||
| H3 | Organization size | The extent of SCMP adoption | 0.396 | 2.052 | 0.16 * | 0.040 | Yes |
| H4 | Business partner readiness | 1.076 | 0.09 | 0.282 | No | ||
| H5 | Government policies | 0.640 | 0.06 | 0.522 | No | ||
| H6 | Perceived benefits | 2.040 | 0.17 * | 0.041 | Yes | ||
| H7 | SCMP extent of adoption | Hospital cost performance | 0.197 | 4.931 | 0.44 *** | <0.001 | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bialas, C.; Bechtsis, D.; Aivazidou, E.; Achillas, C.; Aidonis, D. A Holistic View on the Adoption and Cost-Effectiveness of Technology-Driven Supply Chain Management Practices in Healthcare. Sustainability 2023, 15, 5541. https://doi.org/10.3390/su15065541
Bialas C, Bechtsis D, Aivazidou E, Achillas C, Aidonis D. A Holistic View on the Adoption and Cost-Effectiveness of Technology-Driven Supply Chain Management Practices in Healthcare. Sustainability. 2023; 15(6):5541. https://doi.org/10.3390/su15065541
Chicago/Turabian StyleBialas, Christos, Dimitrios Bechtsis, Eirini Aivazidou, Charisios Achillas, and Dimitrios Aidonis. 2023. "A Holistic View on the Adoption and Cost-Effectiveness of Technology-Driven Supply Chain Management Practices in Healthcare" Sustainability 15, no. 6: 5541. https://doi.org/10.3390/su15065541
APA StyleBialas, C., Bechtsis, D., Aivazidou, E., Achillas, C., & Aidonis, D. (2023). A Holistic View on the Adoption and Cost-Effectiveness of Technology-Driven Supply Chain Management Practices in Healthcare. Sustainability, 15(6), 5541. https://doi.org/10.3390/su15065541











