Abstract
The 2020–2022 period of the global COVID-19 pandemic exposed the fact that many countries health systems had inadequate health workforce availability. This is despite sustainable health workforces being critical to health service and healthcare delivery, an acknowledgement that drove the significant investment and focus on health workforce development over the previous two decades. As such, this review article discusses health workforce governance and planning, notes its weaknesses, and identifies some of the barriers to the implementation of health workforce policy making and planning and the achievement of sustainable health workforces. Important is the recognition that health workforce planning is long-term in nature, while health workforce decision-making processes are dominated by political processes that have much shorter time frames. The article concludes by offering the approach of backcasting to overcome this dichotomy.
1. Introduction
With the declaration of a global pandemic in March 2020 [1], countries were required to respond to reduce the viral spread and the treatment of the infected through a variety of actions that included restricting movement and gatherings, social distancing, mask wearing, personal hygiene routines, testing, redeploying health resources and implementing vaccination programs [2]. The pandemic and the responses to it also impacted health workforces through health worker illness and deaths [3], increased workloads, stress and burnout [4,5,6], changes to service provision [7,8] and by revealing existing workforce shortages and skill maldistributions [9].
Faced with these challenging situations, many countries post-COVID-19 have acknowledged and begun to address weaknesses in their health services and workforces, with some applying reactive policies such as importing workers from other countries [10]. These reactions occur despite the considerable focus on improving the capacity of country and regional health workforce planning and development over the previous two decades [11,12,13,14]. These activities have been redoubled by a global commitment to improving health workforces through the World Health Organization’s Health Workforce Strategy 2030 [15], which acknowledges that “without health workers, there can be no health services” (p. 11) [16] casting further light on the required health workforce improvement, and which is assisting to undo previous policy neglect and issue invisibility [17]. The WHO 2030 strategy aligns with the wider goals for global wellbeing, including the UN’s Sustainable Development Goals through action (3c), which is to “substantially increase health financing, and the recruitment, development and training and retention of the health workforce in developing countries, especially in least developed countries and small island developing States” [18].
In the context of health systems, sustainability represents the continuation or maintenance of changes or innovations to improve the delivery or practice of care [19]. Yet, the field is far from clear, as there is no formal agreed definition of sustainability in the health system context [20]. Nonetheless, there is a general sense that a sustainable health workforce is one where its policies and programs enable the governance, planning and delivery of health workforces, which are both fit for purpose and fit for practice [16,21] and ensure that the right people receive the right services at the right place, at the right time, from those with the right skills [22]. This definition occurs in the context of health workforce governance and planning’s long-term nature, from the preparation of workers, through their training, entry into the workforce, their continuous professional development and increasing role specialization.
As such, this review article aims to address the concept of a sustainable health workforce considering what has been revealed by the pandemic and identifies health workforce planning’s strengths and weaknesses to better understand how sustainable workforces are likely to be achieved. Therefore, we examine the concept of sustainable health workforces and highlight some of the key issues that emerge for health workforce governance; an activity that requires long-term commitment but occurs in a political environment of short-term decision-making. We then discuss the implications of this dichotomy and propose a complementary approach to relieve the persistent constrictions that inhibit more gainful policy and planning implementation.
2. Sustainable Health, Care and Workforces
The sustainability of improvements in the health context has been a challenge for some time and its importance is related to the risk of wasting valuable resources and losing significant progress and patient outcome improvements [23]. Part of the problem of defining sustainable practices in health is the lack of an agreed definition, which is partly due to many studies not including a working definition [20]. This lack of a commonly held definition has led to a multitude of tools or frameworks to measure healthcare sustainability improvement activities. Most of these tools or frameworks are used to evaluate sustainability, a smaller number are used to support sustainability planning, while others are applied to a range of uses, such as providing guidance and strategies, influencing sustainability actions, or as a mix of evaluation, planning and guidance [23]. However, progress over finding a suitable definition has occurred with Moore et al. [19] proposing a comprehensive definition that covers several constructs in common with the range of definitions found in the literature. This comprehensive definition consists of five constructs that are summarized in Table 1.

Table 1.
Comprehensive sustainability definition.
While this comprehensive definition can be applied for determining the sustainability of health workforce interventions, the evidence for consistent sustainable workforce gain is inconsistent. This is despite the significant focus that has been placed on programs and strategies to improve health workforces across regions and countries over the past two decades. For example, Godue et al. [12] reviewed the Pan American Health Organization’s (PAHO) Human Resources for Health 2007–2015 strategy’s five challenges and 20 regional goals and found that over the strategy’s timeframe particular areas of the health workforce milieu were especially resistant to change. These were identified as: low planning capability, including lack of strategic health workforce units; workforce distribution, composition and competencies of the workforce, including distortions of nurse-doctor ratios; the international migration of health workers, particularly those from English-speaking countries; and low remuneration and poor working conditions, leading to worker unrest and workplace instability. Likewise, Dal Poz et al. [24] indicate that there are similar reasons for poor improvement and the health workforce challenges across countries, for which they recommend that more common programs be developed to identify and address the lack of sustainability of health workforce development initiatives.
More recently, the WHO Regional Office for Europe’s report on European health workforces [25], indicates similar findings to Godue et al., signaling that many of these problems are persistent despite locations, system differences and country histories. Similarly, a mid-term review report of the WHO South East Asia Region’s the Decade for Health Workforce Strengthening 2015–2024 strategy found that while doctor, nurse and midwife numbers in the region have increased since 2014 and that health workforce data quality across the regions had also improved, health worker density gains were not being achieved equally across the region, significant differences in nursing graduate numbers were observed across countries, and that while ten of the 11 member states reported having strategic health workforce units, these had varying capabilities and capacities impacting on their ability to play a more deliberate and effective role in improving their respective country’s health workforce [14]. Also, the mid-term monitoring review of PAHO’s Plan of Action on Human Resources for universal access to health and Universal Health Coverage 2018–2023 found variations across member states for meeting this strategy’s targets, with progress being described as low despite some countries evidencing substantive gains [26,27].
Taking the pandemic into account, PAHO’s progress report [27] suggests strengthening responses to emergencies, as well as actions such as better intersectoral coordination, planning agreements and mechanisms, a focus on primary care and interprofessional teams and improving working conditions as areas to focus on post-pandemic. Bourgeault, et al. [28] expands on this, suggesting that new pandemic response plans should include workforce-specific elements that improve physical and emotional safety, along with planning that uses all health workers to ensure high-quality care, supported by appropriate leadership and being mindful of those countries with weak health systems and with health workforce shortages, i.e., taking pandemic workforce lessons as a template for developing more sustainable health workforces. These suggested post-pandemic foci imply that health workforce governance is indeed an important element of health workforce improvement initiatives.
3. Health Workforce Governance and Planning
3.1. Health Workforce Governance
As achieving sustainable health workforces has become increasingly difficult, health workforce governance has been rising in importance [29]. Thus, more focus is being placed on this emergent field and its role in developing sustained improvements in health system delivery and workforce quality [30]. Health workforce governance consists of system oversight and steering functions achieved through a range of processes and tools such as policies and procedures related to health workforce planning, education and ongoing training, evaluation, certification and recertification, clinical guidelines, and the involvement of actors that can influence policy [31].
Taking a strategic view of the health workforce enables countries to be able to address gaps between policy and implementation and thereby be able to steer workforce distributions to overcome specialty, geographic and facility shortages, to have adequate centralized data that is also accurate at the regional and local levels, to assure worker capacity, quality and motivation and enabling delivery, and to be in collaboration with stake-holding organizations such as local authorities [32]. Thus, policy and decision makers require the capacity and willingness to engage with their stakeholders, to support future health service visions, to collaborate with the system’s regulatory and professional organizations and to maintain a general attractiveness of the sector to be able to realize the benefits of a longer-term view [33]. Supporting this requires a long-term perspective by governments to systematically address persistent health workforce problems, in contrast to the many and piecemeal solutions that abound [34]. Achieving it requires those responsible for health workforce governance to be able to project their leadership through the identification of priorities, provision of strategic direction to the health system’s multiple actors, and the creation of commitment across the health sector to address the identified health service improvement priorities [35]. In addition, it has been found that high-level leadership, organizational support, timely HRH data and clear ownership by a country’s ministry of health are important factors contributing to the credibility of a governments’ coordination mechanism, which is shown to aid actor participation [36].
Leadership is considered to be one of the most important factors for supporting workforce change and achieving the desired outcomes [37]. Leadership actions that produce positive outcomes for health workers are building trust, clearly articulating goals and considering the workforce throughout the planning, implementation, and evaluation phases of any changes [37]. Thus, the ability to create, sustain, and improve relationships and integration across professional groups and healthcare sectors is an important aspect of health workforce governance [38].
For countries wishing to strengthen their workforce policies and programs, its governance function should have health workforce units which are correctly placed within a country’s unique institutional and governance framework and with sufficient capacity and capability to perform or well coordinate three key policy processes: problem identification, solution development and policy building [39]. Correct placement of health workforce units is important due to the influence the state and its governance traditions will have on a health workforce unit’s ability to effect fundamental changes (or not) in policy and to develop responses to the country’s health workforce challenges [40]. This is particularly so where a country may have federated systems, where health and care may be funded and/or planned nationally but the country’s states or provinces are responsible for its operational planning and delivery. Without strong links or coordination between national and state health workforce governance responsibilities, tensions between funding, planning and delivery requirements are likely to occur and act to misalign training numbers, worker types and skill mixes [41].
3.2. Health Workforce Planning
Health workforce planning is a key governance tool [31] used by countries to achieve a balance between the supply and demand for health workers in both the long and short term [42]. This dual view is also reflected in the future paradigms of planning proposed by Snowden Hopkins [43], which are on the one hand a future we might expect by letting events run their course, or on the other a future we wish to achieve or desire through planned effort. Both dichotomies, short-long and unplanned-planned, act to emphasize a country’s orientation concerning the types of workforce planning activities that they may undertake.
To sustain workforce planning, its processes must be able to incorporate a range of data above basic workforce numbers and be able to consider productivity, skill mixes, and task substitutions in a way that is responsive to system needs and care design [44]. However, the models that support workforce planning have advanced little in the past decade or so, not through reasons of data, but more due to a lack of substantive model development, for while there have been marginal gains in supply estimation techniques, there have been few gains on modelling workforce demand [45].
The short-term management of workforce supply is usually conducted through actions such as managing education inflows or improving workforce stability through recruitment and retention and are usually implemented as reactions to perceived shortages, which inadvertently create a ‘yo-yo’ effect of cyclical over and undersupplies [42]. More long-term or structural interventions for supply relate to workforce shaping or redesign policies enacted by understanding the overall mix of the workforce and through such actions as extending professional roles or scopes of practice and reviewing staff-mixes and skill-mixes [46], which are largely about how the health system will be, rather than how it is at present [47]. Workforce changes in the long-term can be delivered by vertical integration, which is the understanding of cadre interactions and transfer of tasks across different occupational groups e.g., doctors, nurses, physician assistants or care workers or through horizontal integration, where tasks or interactions are transferred within the same professional grouping, e.g., the strengthening primary care doctors to take on roles or tasks that are normally undertaken by hospital doctors [42]. As such, a country’s social, economic and political situation will uniquely affect its health system, meaning that its health workforce planning is quite context specific.
3.3. Health Workforce Planning Types
The two complementary forces we have identified as active in the health workforce planning ecosystem, short-long term and unplanned-planned, are markers that help to typify the active planning in a country’s health system. Figure 1 plots these planning forces as two horizontal continua, with four distinct planning types that have different attributes and contributions to health workforce sustainability.
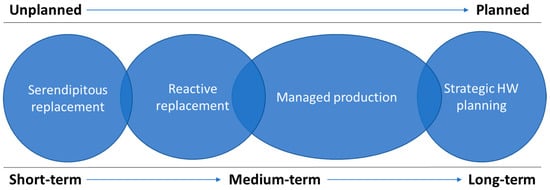
Figure 1.
The four health workforce planning types.
Following Figure 1 from left to right, Serendipitous replacement is typified by few, if any, planning efforts. Rather countries that have this workforce planning type tend to let their education institutions produce the workforces they can, responding to demand signals from employers and offering education and training for those roles that are perceived as being more attractive by the prospective students. Here the workforce entering the health system are mismatched with the health needs of the country, with some services failing as they are unable to attract sufficient entrants as workers retire. Reactive replacement has governments responding to perceived or real over or under-supplies, which end up producing Ono et al.’s [42] “yo-yo” (p. 13) effect of periodic worker surpluses and deficits. In this planning type, governments may increase or restrict access to health education or influence the attractiveness of different fields of study and occupations, location, retention rates and retirement patterns, such as by using wage rates [42] to manage the worker numbers and placements, which tend to be based on the health system’s existing positions or roles. Managed production uses health workforce data to implement a more controlled approach to workforce sustainability than replacement. This planning type is characterized by systematized workforce data collection, the use of projection or estimates produced by mathematical models, often including stock and flow models that use strategic analysis and scenarios to factor in a range of economic, political, social, technological, legal and environmental influences and proactive policy making to better control worker numbers and direct skills. Lastly, is the strategic approach to health workforce planning, where a more sophisticated approach to the health workforces’ relationship with the health system and the determinants of health that drive a country’s health needs are used. This planning type requires strong health workforce governance and significant involvement of health workforce actors in setting directions and working towards achieving the strategic objectives of the health system and associated strategies.
These planning types have differing levels of planning and governance complexity associated with them. This can be represented in a continuum, where the types are arranged with increasing complexity (see Figure 2).
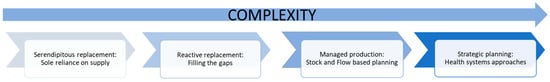
Figure 2.
The health workforce planning continuum.
Figure 2′s continuum shows that countries can progress in their planning type, by adding competencies, capacities, and learning from experience and by establishing governance process to support the relationships required to optimize and grow a country’s health workforce planning responses. However, with rising complexity also comes weaknesses. Increasing complexity requires different infrastructures in terms of increasingly current and reliable health workforce data. Without this data it is difficult to know which cadres require strengthening, the relative density of the workforces and geographical and medical specialty maldistributions, which are persistent problems that prevent many countries from attaining sustainability of their workforces. Likewise, both planning and governance capabilities are required to be strengthened. Table 2 lays out the characteristics of these planning types, their weaknesses, and example countries employing the planning type.

Table 2.
Descriptions of the four health workforce planning types.
4. Discussion
The limited successes of health workforce planning and sustainable implementation have been attributed to various institutional causes such as poor planning capability or processes, the lack of suitable planning tools, the lack of appropriate data, low levels of stakeholder involvement and the insufficiency of financial and capability building resources [55]. The effects of not making progress on these issues leads to the persistence of workforce shortages, maldistributions and skill-mix imbalances, poor collaboration and working conditions, lopsided gender distributions, and incomplete health workforce data [15]. These limitations have led to emphasis on improving institutional policy capacity and capability and towards examining the broader influences on the health workforce and system [33], in effect a focus on strengthening health workforce governance.
This brings up the issue of the need for a long-term view of health workforce planning. However, this issue also tends to be affected by the political environment riven by short-term solutions and sectoral interests [34,56]. The temporal issue of short versus long-term is pointed to by Padilha et al. [34], who emphasize that governments should not be swayed into enacting short-term solutions; an assessment reiterated by the WHO workforce strategy 2030 through its multiple underscoring of the necessity for political will and the time it will take for strategy realization [15].
Similarly, the environment of political cycles tends to orientate policy decisions towards a short-term view, due to policy reversal risks that stem from changing governments, ministers, and functionaries. However, this risk can be minimized by broad-based actor support for policy agendas that also acts to reduce the influence of vested interests [55]. Thus, political cycles seem to have a dampening effect on health workforce policy development. This would be largely due to many governments existing for only one or two cycles, when health workforce policies and strategies may take considerably longer than this to be realized. This milieu tends to result in a multitude of short-term policies and actions that appear to address the workforce problems, but have little or no impact in the long-term [34]. This short-circuiting of the policy process results in what is referred to as a policy soup, where the problems and solutions of a policy issue are in constant flux and may never be adequately dealt with [57].
4.1. Towards Sustainable Workforces
Much of health workforce planning relies on the ability to successfully estimate needs and to respond with a sustainable and fit-for-purpose workforce [21]. Typically, health workforce planners use quantitative forecasts, with many of these only estimating replacement needs and often focusing on specific professional groups, such as physicians and nurses rather than including the wider health workforce such as allied health professionals [42]. These quantitative forecasts tend to ignore the overarching political economy and health system interactions, focusing on the problem size rather than cost-effective solutions, and consider different health workforces in isolation [58]. These limitations tend to entrench the status quo’s institutions and structures, and so will therefore impede the ability of planners to view the future as it will or may be and therefore, to express the values and structures of this future health system [47]. A resolution to this is to understand forecasting’s limitations and be able to also apply appropriate models or tools to address the problem being faced. As Dunn [57] presents, while forecasting can be improved in terms of error reduction or forecast efficacy, better results can be achieved with a mix of theoretical models and expert judgements than by extrapolative forecasts alone. As such, an appreciation and the use of different forecasting or future preparation methods is advocated to complement the health workforce planning’s present techniques [58,59] and in wider public policy development [57,60,61,62,63].
This advocacy involves the use of qualitative research in health workforce planning to better understand needs, deal with uncertainty, and to take a longer-term view of the future. The various techniques that the authors propose aim to assist planners to understand what is important to health workforce actors, including health workers and the end-users, how futures may unfold and how policy options or actions can be sequenced to meet proposed strategic aims. These enablers are important features to be able to successfully align a health workforce plan with a corresponding national health strategy. As van der Steen [62] states, these types of techniques “draw attention to the role of time in policy” (p. 246) and by this means, policymaking can be deemed to be successful when it accounts for the dynamics of interactions that change over time, sometimes due to the policy itself.
A key benefit of the use of a wider range of forecasting or future preparation tools is the ability to study the future to identify its problems, and solutions and to imagine the possible or preferable future conditions. These future conditions may be represented by a nation’s strategic health plans and will point to the future that is desired and dictate a set of actions to achieve this state. Governments, by setting national health strategies and plans are therefore explicitly delineating a future for the nation’s health system and expressing what should happen to achieve it and, as such, are prescribing a future. Dunn [57] identifies three types of societal futures that relate to planning and policy development (see Table 3).

Table 3.
The three types of societal futures.
These future types represent the range of future states that a health system may experience. The plausible future group relate most to the first two health workforce planning types, Serendipitous replacement and Reactive replacement, in that there is little steering or intervention by governments to shape the future state of the health workforce. While for Managed replacement and Strategic health workforce planning, governments exert increasing control and actions to determine how the future will eventuate. Figure 3 represents the three societal futures over time, with the range of futures becoming fewer as health workforce planning becomes more influential.
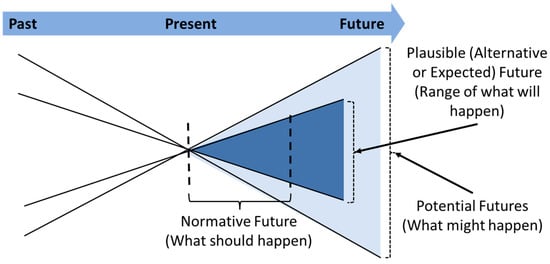
Figure 3.
The three societal futures over time. Source: Dunn [57].
For a government to be able to influence its health workforce’s makeup, it needs to be able to take the end state of its strategic health plans (a normative future) and align it with a sustainable workforce by steering the present workforce towards this goal by matching education and training, skill sets, quantity, and distributions appropriately. The consideration and inclusion of the health workforce in national health strategies or reforms are therefore essential to realize the strategy’s goals or to enable the system improvements [64]. Therefore, the question for governments seems to be: How can a health workforce plan’s actions and activities be aligned and sequenced with the national health plan or strategy? In essence, this is what we see as a central challenge for achieving sustainable workforces.
4.2. Introducing Backcasting
As we have discussed previously, political cycles and frequent turnover of planning staff are a barrier to long-term decisions. Responding to crises or urgent situations leads to increasing numbers of short-term solutions, so that longer-term view is less likely to enter decision making. This barrier can be likened to a bottleneck, preventing the long-term view or plans from being approved or adopted and perhaps the more politically expedient short-term solutions being preferred. This pattern of behavior further perpetuates the persistence of common health workforce problems by failing to address the problems with solutions that address root causes.
To alleviate this policy bottleneck (see Figure 4), we propose the use of a futures planning technique called backcasting. Backcasting is a normative approach to futures planning that literally means looking back from the future. It can be applied to situations to assess the feasibility of desired futures rather than exploring plausible or potential futures [65]. It is applicable when trying to understand how something can unfold and through balancing creativity and evidence, the technique assists planners to navigate through uncertainty [62].
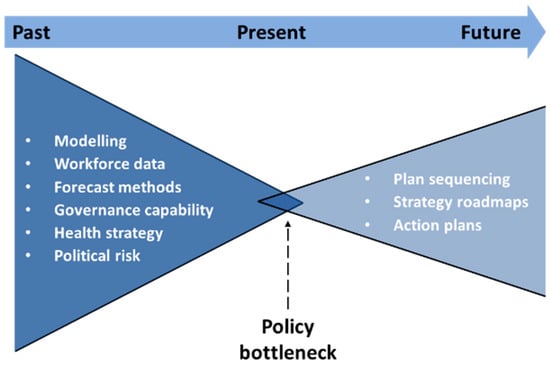
Figure 4.
The health workforce policy bottleneck.
Backcasting enables plans to pass through the policy bottleneck by making the extensive and uncertain paths towards nation’s health strategy objectives more achievable. It does this by reducing uncertainty about the future. As the normative future is stated as the health strategy’s goals, this acts to place the government in the driving seat to attain the future state, rather being at the whim of planning variables or being forced to choose a path towards a plausible or expected future.
Backcasting is also useful for sectioning national health strategies into time phases that may match political cycles. Thus, an appropriate model of care can be devised for each strategy goal and for this model of care an appropriate workforce can be described and quantified. The planner then applies backcasting to look back from this desired state to identify how this came about, to identify the sequences of small but critical steps and to ensure that these will have the sufficient resources for the strategy or plan’s realization. Following this exercise, regular action planning or roadmap development can take place, with the uncertainties and hidden issues now clarified through the backcasting process.
As such, Quist [65] outlines the implementation of backcasting through his framework of five steps, a number of tools and the involvement of relevant stakeholders. His steps begin with identifying the strategic problem, for example the issues being addressed by a government’s health strategy, followed by the step of developing the future vision, which here is the desired future expressed by the strategy and the changes that comprise the strategy’s implementation. The third step is backcasting itself, which features two sub-stages, where the first is to identify the changes and the second is to determine the what, how and who of the changes and actions. Identifying change drivers and barriers is also part of this backcasting step. The fourth step is to define the change-based activities along with their associated budgets and timeframes by producing strategy-based action plans based on the backcasting’s results. The fifth and final step is to ensure that these actions are followed up and the results are embedded.
The involvement of stakeholders in backcasting assists to provide increased legitimacy, accountability and expertise to address the issues being faced [65]. Thus, backcasting supports sustainability by involving health workforce actors to contribute to the identification of priorities, provision of strategic direction, and the creation of commitment to address the identified improvement priorities -that is for stakeholders to be more involved in the health workforce governance process. Actor involvement can also improve intervention design as knowledge of the system’s actors influences and an understanding of their behaviors interactions and decisions allows for better collaboration and health system enhancement opportunities [66,67].
As such, backcasting addresses the twofold problem of the attraction of short-term decision-making and the political risks of more long-term policy decisions by providing clarity for future cost and supply requirements and to adjust for any shorter-term service requirements. These benefits can provide governments with an early opportunity to demonstrate positive progress of their strategy and to better frame the appropriate workforce supply as a plan objective that is being delivered.
5. Conclusions
In this review article, we aimed to address the global issue of sustainable health workforces by identifying present problems and to further understand the health workforce policymaking and planning process. Persistent problems encountered by many countries consist of worker and skill shortages or maldistributions, poor working conditions, and limited health workforce data to build strong models to assist planning. Countries may find themselves, due to limited health workforce governance capabilities, unable to maintain and project leadership, involve policy actors and agree on common priorities, leading to their workforce planning being replacement focused or simply left to the market. However, as Table 2 reveals, several countries do exhibit stronger abilities and have health workforce planning that is of the managed or strategic types.
From our analysis, we identified two overarching issues that impede the implementation of strategies and plans that would lead to sustainable health workforces. These issues consist of the temporal view and political uncertainty. The temporal view relates to health workforce planning and policy needing to a have a long-term orientation, but many times countries are mired in short-term activities and interventions that do not lead to sustainable solutions for the problem or that will result in lasting improvements. For political uncertainty, we observe that political cycles and government changes lead to the long-term view being undermined through political pressures and vested interests, further entrenching the short-term view.
To alleviate this, we propose adding backcasting to the health workforce planning toolbox. Backcasting enables countries with national health strategies to envisage this normative future and to look backwards to be able to see how this future was achieved. As a technique, it is not commonly used in health policy development [68], but as indicated above, the appreciation and advocacy of the use of such complementary planning and policy development techniques in health workforce and wider public policy is increasing [57,59,60,61,62,63].
In conclusion, sustainable health workforces require three key abilities to become a reality for many countries. First, improved governance capabilities are required, second, the adoption of longer-term planning perspectives and third, the use of a wider range of planning tools. With these, we believe sustainable health workforces are possible.
Author Contributions
Conceptualization, G.H.R. and C.S.; Literature collection, G.H.R., C.S. and R.J.; Formal Analysis, G.H.R. and C.S.; Writing—Original Draft Preparation, G.H.R.; Writing—Review, Editing & Finalization, G.H.R., C.S., R.J. and L.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to acknowledge Graham Willis for his insightful comments that encouraged the authors to develop this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 3 July 2022).
- European Observatory on Health Systems and Policies COVID-19 Health System Response Monitor (HSRM). Available online: https://eurohealthobservatory.who.int/monitors/hsrm/overview (accessed on 3 July 2022).
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob. Health 2020, 5, e003097. [Google Scholar] [CrossRef] [PubMed]
- De Raeve, P.; Adams, E.; Xyrichis, A. The impact of the COVID-19 pandemic on nurses in Europe: A critical discussion of policy failures and opportunities for future preparedness. Int. J. Nurs. Stud. Adv. 2021, 3, 100032. [Google Scholar] [CrossRef]
- Huffman, A. COVID-19 Surges Then Crickets and the Impact on the Emergency Department Workforce. Ann. Emerg. Med. 2022, 79, A11–A14. [Google Scholar] [CrossRef]
- Hamouche, S. COVID-19 and employees’ mental health: Stressors, moderators and agenda for organizational actions. Emerald Open Res. 2020, 2, 15. [Google Scholar] [CrossRef]
- López-Cabarcos, M.A.; López-Carballeira, A.; Ferro-Soto, C. New ways of working and public healthcare professionals’ well-being: The response to face the COVID-19 pandemic. Sustainability 2020, 12, 8087. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Wherton, J.; Shaw, S.; Morrison, C. Video consultations for COVID-19. BMJ 2020, 368, m998. [Google Scholar] [CrossRef]
- Buchan, J.; Williams, G.A.; Zapata, T. Governing health workforce responses during COVID-19. Eurohealth 2021, 27, 41–48. [Google Scholar]
- Neilson, M. Immigration health Green List: Top Health Official Urges Ministers to Take Action on Healthcare Workforce Shortages. Available online: https://www.nzherald.co.nz/nz/politics/immigration-health-green-list-top-health-official-urges-ministers-take-action-on-healthcare-workforce-shortages/W3M7FEZRBVFXNDNT2TROWRDN4U/ (accessed on 20 November 2022).
- Afzal, M.; Cometto, G.; Rosskam, E.; Sheikh, M. Global Health Workforce Alliance: Increasing the momentum for health workforce development. Rev. Peru. Med. Exp. Salud Publica 2011, 28, 298–307. [Google Scholar] [CrossRef]
- Godue, C.; Cameron, R.; Borrell, R.M. Capacity building in human resources for health: The experience of the region of the Americas. Can. J. Public Health 2016, 107, e347–e354. [Google Scholar] [CrossRef]
- Pan American Health Organization. Strategy on Human Resources for Universal Access to Health and Universal Health Coverage; Pan American Health Organization: Washington DC, USA, 2017; Available online: https://iris.paho.org/handle/10665.2/53838 (accessed on 15 December 2022).
- Zapata, T.; Zakoji, M.; Kanda, M.; Travis, P.; Tangcharoensathien, V.; Buchan, J.; Jhalani, M. Implementing a decade of strengthening the health workforce in the WHO South-East Asia Region: Achievements and way forward for primary health care. WHO South-East Asia J. Public Health 2021, 10, S76–S86. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; World Health Organization: Geneva, Switzerland, 2016; ISBN 9789241511131. [Google Scholar]
- Global Health Workforce Alliance, World Health Organization. A Universal Truth: No Health without a Workforce; Global Health Workforce Alliance, World Health Organization: Geneva, Switzerland, 2014; ISBN 9789241506762. [Google Scholar]
- Dussault, G. Bringing the health workforce challenge to the policy agenda. In The Palgrave International Handbook of Healthcare Policy and Governance; Kuhlmann, E., Blank, R.H., Bourgeault, I.L., Wendt, C., Eds.; Palgrave Macmillan: London, UK, 2015; pp. 273–288. ISBN 978-1-137-38493-5. [Google Scholar]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015; Available online: https://sdgs.un.org/sites/default/files/publications/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf (accessed on 13 December 2022).
- Moore, J.E.; Mascarenhas, A.; Bain, J.; Straus, S.E. Developing a comprehensive definition of sustainability. Implement. Sci. 2017, 12, 110. [Google Scholar] [CrossRef] [PubMed]
- Stirman, S.W.; Kimberly, J.; Cook, N.; Calloway, A.; Castro, F.; Charns, M. The sustainability of new programs and innovations: A review of the empirical literature and recommendations for future research. Implement. Sci. 2012, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Gorman, D.F. Towards a sustainable and fit-for-purpose health workforce-lessons from New Zealand. Med. J. Aust. 2012, 1 (Suppl. 3), 32–36. [Google Scholar] [CrossRef]
- Birch, S. Health human resource planning for the new millennium: Inputs in the production of health, illness, and recovery in populations. Can. J. Nurs. Res. 2002, 33, 109–114. [Google Scholar]
- Lennox, L.; Maher, L.; Reed, J. Navigating the sustainability landscape: A systematic review of sustainability approaches in healthcare. Implement. Sci. 2018, 3, 27. [Google Scholar] [CrossRef]
- Dal Poz, M.R.; Sepulveda, H.R.; Costa Couto, M.H.; Godue, C.; Padilla, M.; Cameron, R.; de Andrade Vidaurre Franco, T. Assessment of human resources for health programme implementation in 15 Latin American and Caribbean countries. Hum. Resour. Health 2015, 13, 24. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. Health and Care Workforce in Europe: Time to Act; WHO Regional Office for Europe: Copenhagen, Denmark, 2022. [Google Scholar]
- Cho, M.; Levin, R. Implementación del plan de acción de recursos humanos en salud y la respuesta a la pandemia por la COVID-19. Rev. Panam. Salud Publica 2022, 46, e52. [Google Scholar] [CrossRef]
- Pan American Health Organization. Plan de Acción Sobre Recursos Humanos Para el Acceso Universal a la Salud y Cobertura Universal de Salud 2018–2023: Progress Report to the 59th Directing Council of PAHO. CD59/INF/16; PAHO: Washington, DC, USA, 2021; Available online: https://www.paho.org/es/documentos/cd59inf16-plan-accion-sobre-recursos-humanos-para-acceso-universal-salud-cobertura (accessed on 15 December 2022).
- Bourgeault, I.L.; Maier, C.B.; Dieleman, M.; Ball, J.; MacKenzie, A.; Nancarrow, S.; Nigenda, G.; Sidat, M. The COVID-19 pandemic presents an opportunity to develop more sustainable health workforces. Hum. Resour. Health 2020, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, E.; Batenburg, R.; Dussault, G. Where health workforce governance research meets health services management. Health Serv. Manag. Res. 2016, 29, 21–24. [Google Scholar] [CrossRef]
- Kuhlmann, E.; Batenburg, R.; Dussault, G. Health workforce governance in Europe. Health Policy 2015, 119, 1515–1516. [Google Scholar] [CrossRef]
- Barbazza, E.; Langins, M.; Kluge, H.; Tello, J. Health workforce governance: Processes, tools and actors towards a competent workforce for integrated health services delivery. Health Policy 2015, 119, 1645–1654. [Google Scholar] [CrossRef] [PubMed]
- Fritzen, S.A. Strategic management of the health workforce in developing countries: What have we learned? Hum. Resour. Health 2007, 5, 4. [Google Scholar] [CrossRef] [PubMed]
- Dussault, G.; Buchan, J.; Sermeus, W.; Padaiga, Z. Assessing Future Health Workforce Needs; World Health Organisation: Copenhagen, Denmark, 2010; ISSN 2077-1584. [Google Scholar]
- Padilha, A.; Kasonde, J.; Mukti, G.; Crisp, N.; Takemi, K.; Buch, E. Human resources for universal health coverage: Leadership needed. Bull. World Health Organ. 2013, 91, 800–800A. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, C.A.; Harrison, R.; Chauhan, A.; Meyer, L. Priorities and challenges for health leadership and workforce management globally: A rapid review. BMC Health Serv. Res. 2019, 19, 239. [Google Scholar] [CrossRef] [PubMed]
- Martineau, T.; Ozano, K.; Raven, J.; Mansour, W.; Bay, F.; Nkhoma, D.; Badr, E.; Baral, S.; Regmi, S.; Caffrey, M. Improving health workforce governance: The role of multi-stakeholder coordination mechanisms and human resources for health units in ministries of health. Hum. Resour. Health 2022, 20, 47. [Google Scholar] [CrossRef]
- Hastings, S.E.; Armitage, G.D.; Mallinson, S.; Jackson, K.; Suter, E. Exploring the relationship between governance mechanisms in healthcare and health workforce outcomes: A systematic review. BMC Health Serv. Res. 2014, 14, 479. [Google Scholar] [CrossRef]
- Kuhlmann, E.; Burau, V. Strengthening stakeholder involvement in health workforce governance: Why we need to talk about power. J. Health Serv. Res. Policy 2018, 23, 66–68. [Google Scholar] [CrossRef]
- Cometto, G.; Nartey, E.; Zapata, T.; Kanda, M.; Md, Y.; Narayan, K.; Pritasari, K.; Irufa, A.; Lamichhane, R.; De Silva, D.; et al. Analysing public sector institutional capacity for health workforce governance in the South-East Asia region of WHO. Hum. Resour. Health 2019, 17, 43. [Google Scholar] [CrossRef]
- Voorberg, W.; Bekkers, V.; Flemig, S.; Timeus, K.; Tonurist, P.; Tummers, L. Does co-creation impact public service delivery? The importance of state and governance traditions. Public Money Manag. 2017, 37, 365–372. [Google Scholar] [CrossRef]
- Imison, C.; Buchan, J.; Xavier, S. NHS Workforce Planning: Limitations and Possibilities; King’s Fund: London, UK, 2009; Available online: https://www.kingsfund.org.uk/sites/files/kf/NHS-Workforce-Planning-Candace-Imison-James-Buchan-Su-Xavier-Kings-Fund-November-2009.pdf (accessed on 16 January 2023).
- Ono, T.; Lafortune, G.; Schoenstein, M. Health Workforce Planning in OECD Countries: A Review of 26 Projection Models from 18 Countries; OECD Health Working Papers, No. 62; OECD Publishing: Paris, France, 2013. [Google Scholar] [CrossRef]
- Snowden Hopkins, F. The planning mission before us. In Handbook of Futures Research; Folwes, J., Ed.; Greenwood Press: Westport, CT, USA, 1978; pp. 779–790. ISBN 0837198852. [Google Scholar]
- Bloor, K.; Maynard, A. Planning Human Resources in Health Care: Towards an Economic Approach—An International Comparative Review; CHSRF: Ottawa, ON, Canada, 2003. [Google Scholar]
- Birch, S. Health Workforce Planning: Australia and Canada. In Proceedings of the International Workshop on Health and Social Care Workforce Planning, Dublin, Ireland, 7 June 2022; Available online: https://www.youtube.com/watch?v=HAAfyUUhr90 (accessed on 13 December 2022).
- Bohmer, R.M.J.; Imison, C. Lessons from England’s health care workforce redesign: No quick fixes. Health Aff. 2013, 3, 2025–2031. [Google Scholar] [CrossRef]
- Gorman, D.F. Developing health care workforces for uncertain futures. Acad. Med. 2015, 90, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Richardson, E.; Nino, B. Georgia: Health system review. Health Syst. Transit. 2017, 19, 1–90. Available online: https://eurohealthobservatory.who.int/publications/i/georgia-health-system-review-2017 (accessed on 12 December 2022).
- Kostova Neda, M.; Snezhana, C.; Ponce Ninez, A.; van Ginneken, E.; Winkelmann, J. The former Yugoslav Republic of Macedonia: Health System review. Health Syst. Transit. 2017, 19, 1–160. Available online: https://eurohealthobservatory.who.int/publications/i/the-former-yugoslav-republic-of-macedonia-health-system-review-2017 (accessed on 12 December 2022).
- Onvlee, O.; Kaitelidou, D.; Scotter, C.; Dieleman, M. Navigating the political and technical challenges of developing a national HRH strategy: A case study in Greece. Health Policy 2021, 125, 1574–1579. [Google Scholar] [CrossRef] [PubMed]
- Kroneman, M.; Boerma, W.; van den Berg, M.; Groenewegen, P.; de Jong, J.; van Ginneken, E. The Netherlands: Health system review. Health Syst. Transit. 2016, 18, 1–239. Available online: https://eurohealthobservatory.who.int/publications/i/netherlands-health-system-review-2016 (accessed on 12 December 2022).
- Van Greuningen, M.; Batenburg, R.S.; Van der Velden, L.F.J. Ten years of health workforce planning in the Netherlands: A tentative evaluation of GP planning as an example. Hum. Resour. Health 2012, 10, 21. [Google Scholar] [CrossRef]
- Pearse, J.; Robertson, E.; Brownwood, I.; Cho, O.; Mitchell, S. Building a sustainable health workforce: Using clinical data to inform workforce planning. In Proceedings of the 35th Patient Classification Systems International Conference, Reykjavík, Iceland, 27–30 September 2022; Available online: http://www.pcsinternational.org/conference/PCSI2022/assets/PCSI2022_abstract_74.html (accessed on 12 December 2022).
- Willis, G. Robust Workforce Planning Framework: An Introduction; CfWI Technical Paper Series No. 0001; Centre for Workforce Intelligence: London, UK, 2014; Available online: http://www.cfwi.org.uk/publications/robust-workforce-planning-an-introduction (accessed on 12 December 2022).
- World Health Organization. Models and Tools for Health Workforce Planning and Projections; World Health Organization: Geneva, Switzerland, 2010; pp. 1–16. ISBN 978 92 4 159901 6. [Google Scholar]
- World Health Organization. Health Workforce 2030: Towards a Global Strategy on Human Resources for Health; World Health Organization: Geneva, Switzerland, 2015; ISBN 978 92 4 150862 9. [Google Scholar]
- Dunn, W.N. Public Policy Analysis: An Introduction, 6th ed.; Routledge: New York, NY, USA, 2018; ISBN 9781315181226. [Google Scholar]
- National Health Workforce Planning and Research Collaboration. Alternative Approaches to Health Workforce Planning: Final Report; Health Workforce Australia: Adelaide, Australia, 2011; pp. 1–56. [Google Scholar]
- Rees, G.H.; Crampton, P.; Gauld, R.; MacDonell, S. New Zealand’s health workforce planning should embrace complexity and uncertainty. N. Z. Med. J. 2018, 131, 109–115. Available online: https://journal.nzma.org.nz/journal-articles/new-zealand-s-health-workforce-planning-should-embrace-complexity-and-uncertainty (accessed on 12 December 2022).
- Liwanag, H.J.; Uy, J.; Politico, M.R.; Padilla, M.J.; Arzobal, M.C.; Manuel, K.; Cagouia, A.l.; Tolentino, P.; Frahsa, A.; Ronquillo, K. Cocreation in Health Workforce Planning to Shape the Future of the Health Care System in the Philippines. Glob. Health Sci. Pract. 2022, 10, e2200176. [Google Scholar] [CrossRef]
- Gariboldi, M.I.; Lin, V.; Bland, J.; Auplish, M.; Cawthorne, A. Foresight in the time of COVID-19. Lancet Reg. Health West. Pac. 2021, 6, 100049. [Google Scholar] [CrossRef]
- van der Steen, M. Scenario analysis, forecasting and backcasting as policy tools. In The Routledge Handbook of Policy Tools; Howlett, M., Ed.; Routledge: New York, NY, USA, 2022; pp. 245–256. [Google Scholar] [CrossRef]
- Schmidt, J.M. Policy, planning, intelligence and foresight in government organizations. Foresight 2015, 17, 489–511. [Google Scholar] [CrossRef]
- Rees, G.H. The evolution of New Zealand’s health workforce policy and planning system: A study of workforce governance and health reform. Hum. Resour. Health 2019, 17, 51. [Google Scholar] [CrossRef] [PubMed]
- Quist, J. Backcasting. In Foresight in Organizations: Methods and Tools, 1st ed.; van der Duin, P., Ed.; Routledge: New York, NY, USA, 2016; pp. 145–164. ISBN 9781138692862. [Google Scholar]
- Gilson, L. Introduction to health policy and systems research. Health Policy and Systems Research: A Methodology Reader; Alliance for Health Policy and System Research & World Health Organization: Geneva, Switzerland, 2012; pp. 19–39. ISBN 9789241503136. [Google Scholar]
- Rees, G.H.; Crampton, P.; Gauld, R.; MacDonell, S. Rethinking health workforce planning: Capturing health system social and power interactions through actor analysis. Futures 2018, 99, 16–27. [Google Scholar] [CrossRef]
- Veenman, S.A. Futures studies and uncertainty in public policy: A case study on the ageing population in the Netherlands. Futures 2013, 53, 42–52. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).