Healthcare Waste and Sustainability: Implications for a Circular Economy
Abstract
1. Introduction
- To identify the challenges to implementing a CE in HCW.
- Develop a hierarchal framework to evaluate these challenges.
- Create a foundation for future research in HCW management in the context of a circular economy.
2. Literature Review
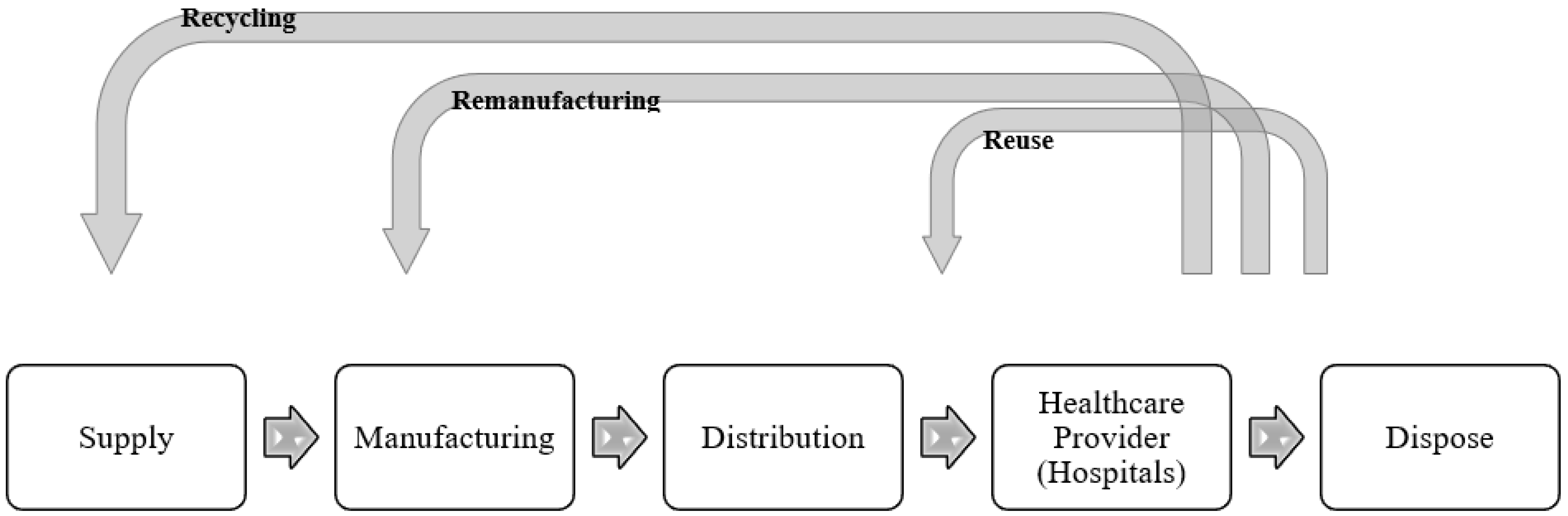
2.1. Circular Economy in Healthcare Waste Management
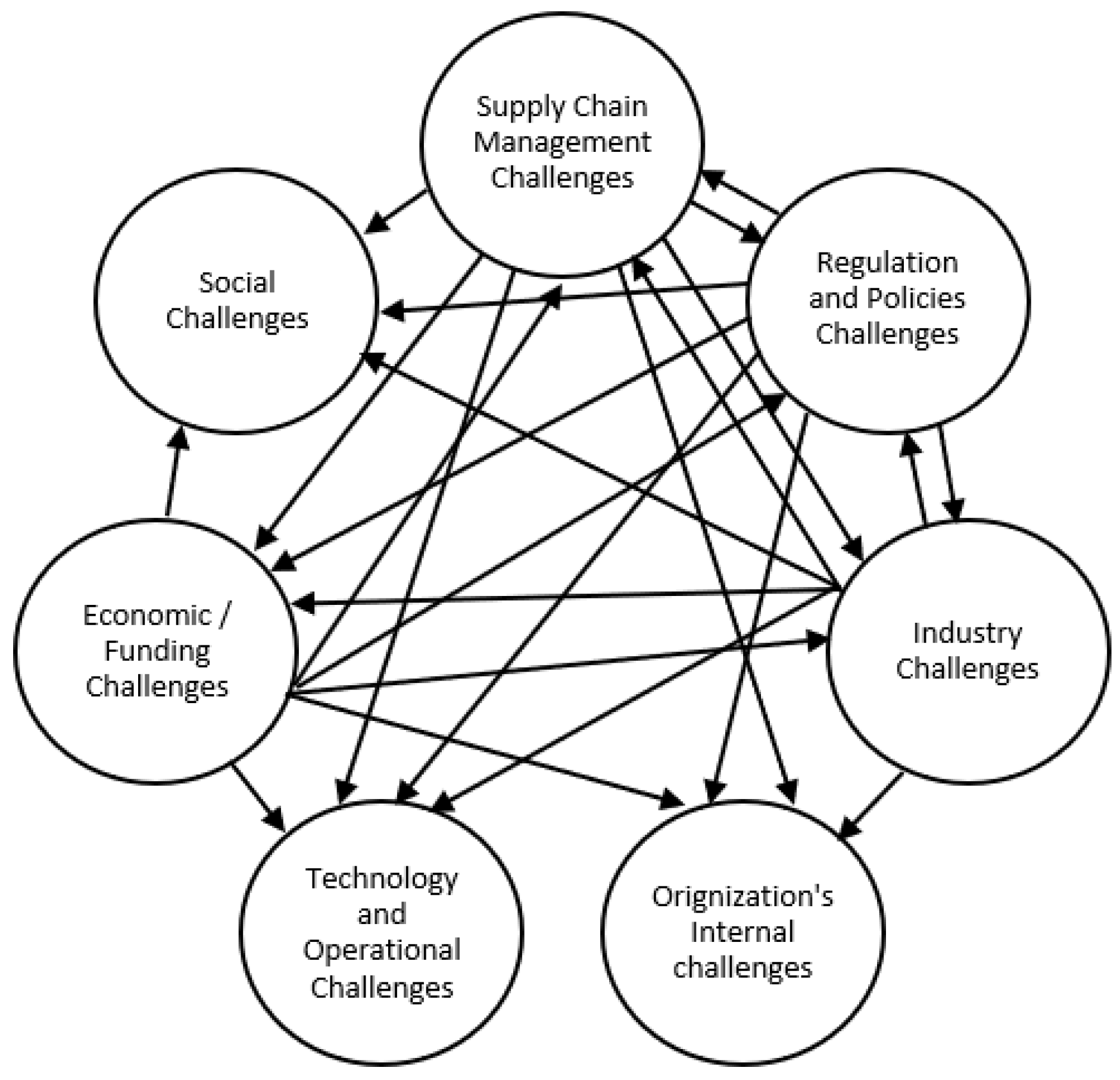
2.2. Challenges of Circular Economy
2.2.1. Supply Chain Management Challenges (C1)
2.2.2. Regulations and Policies Challenges (C2)
2.2.3. Industry Challenges (C3)
2.2.4. Organizations Internal Challenges (C4)
2.2.5. Technology and Operational Challenges (C5)
2.2.6. Economic/Funding Challenges (C6)
2.2.7. Social Challenges (C7)
2.3. Recent Literature Related to Healthcare Waste Sustainability
3. Methodology
3.1. Data Collection
3.2. Expert Selection
3.3. Decision Making Trial and Evaluation Laboratory Method (DEMATEL) Steps
4. Results and Discussion
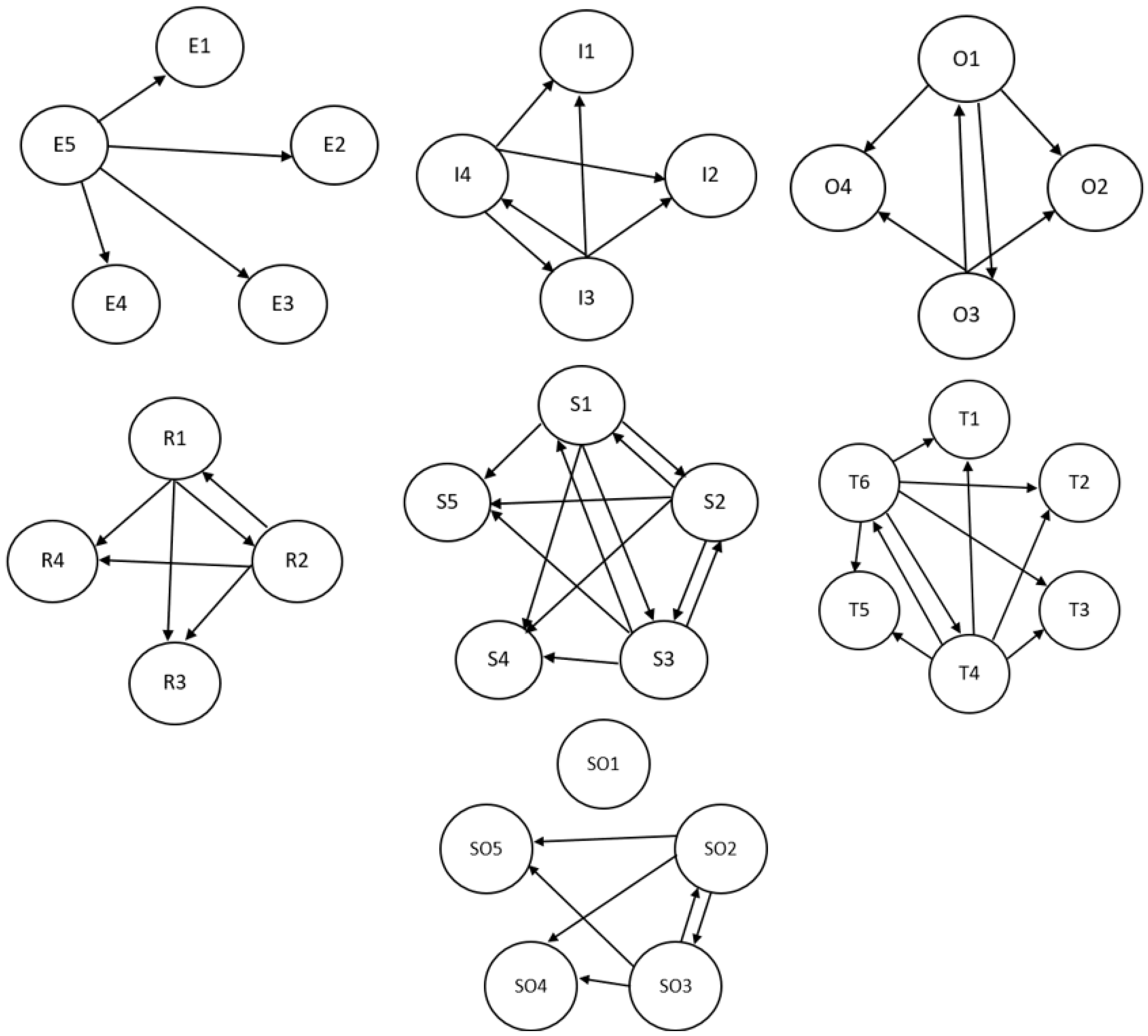
4.1. Supply Chain Management Challenges
4.2. Regulation and Policies Challenges
4.3. Industry Challenges
4.4. Organization’s Internal Challenges
4.5. Technology and Operational Challenges
4.6. Economic/Funding Challenges
4.7. Social Challenges
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yeoh, E.; Othman, K.; Ahmad, H. Understanding medical tourists: Word-of-mouth and viral marketing as potent marketing tools. Tour. Manag. 2013, 34, 196–201. [Google Scholar] [CrossRef]
- WHO. Global Spending on Health: Weathering the Storm. Available online: https://www.who.int/publications/i/item/9789240017788 (accessed on 1 January 2020).
- Kenny, C.; Priyadarshini, A. Review of Current Healthcare Waste Management Methods and Their Effect on Global Health. Healthcare 2021, 9, 284. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.C.; Rodic, L.; Modak, P.; Soos, R.; Carpintero, A.; Velis, K.; Iyer, M.; Simonett, O. Global Waste Management Outlook; United Nation Environment Programme, UNEP: Leeds, UK, 2015. [Google Scholar]
- McPhail, S.M. Multimorbidity in chronic disease: Impact on health care resources and costs. Risk Manag. Healthc. Policy 2016, 9, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Eckelman, V.; Sherman, J.D. Estimated Global Disease Burden From US Health Care Sector Greenhouse Gas Emissions. Am. J. Public Health 2018, 108, S120–S122. [Google Scholar] [CrossRef]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.J.; Campbell-Lendrum, D.; Capstick, S.; et al. The 2019 report of The Lancet Countdown on health and climate change: Ensuring that the health of a child born today is not defined by a changing climate. Lancet 2019, 394, 1836–1878. [Google Scholar] [CrossRef]
- MacNeill, A.J.; Hopf, H.; Khanuja, A.; Alizamir, S.; Bilec, M.; Eckelman, M.J.; Hernandez, L.; McGain, F.; Simonsen, K.; Thiel, C.; et al. Transforming The Medical Device Industry: Road Map To A Circular Economy. Health Affair. 2020, 39, 2088–2097. [Google Scholar] [CrossRef]
- Michelini, G.; Moraes, R.N.; Cunha, R.N.; Costa, J.M.H.; Ometto, A.R. From linear to circular economy: PSS conducting the transition. Proc. Cirp. 2017, 64, 2–6. [Google Scholar] [CrossRef]
- MacArthur, E. Towards the circular economy. J. Ind. Ecol. 2013, 2, 23–44. [Google Scholar]
- Reike, D.; Vermeulen, W.J.V.; Witjes, S. The circular economy: New or Refurbished as CE 3.0?—Exploring Controversies in the Conceptualization of the Circular Economy through a Focus on History and Resource Value Retention Options. Resour. Conserv. Recycl. 2018, 135, 246–264. [Google Scholar] [CrossRef]
- van Boerdonk, P.J.M.; Krikke, H.R.; Lambrechts, W. New business models in circular economy: A multiple case study into touch points creating customer values in health care. J. Clean. Prod. 2021, 282, 125375. [Google Scholar] [CrossRef]
- Chauhan, A.; Jakhar, S.K.; Chauhan, C. The interplay of circular economy with industry 4.0 enabled smart city drivers of healthcare waste disposal. J. Clean. Prod. 2021, 279, 123854. [Google Scholar] [CrossRef] [PubMed]
- Ranjbari, M.; Saidani, M.; Esfandabadi, Z.S.; Peng, W.X.; Lam, S.S.; Aghbashlo, M.; Quatraro, F.; Tabatabaei, M. Two decades of research on waste management in the circular economy: Insights from bibliometric, text mining, and content analyses. J. Clean. Prod. 2021, 314, 128009. [Google Scholar] [CrossRef]
- Kane, G.M.; Bakker, C.A.; Balkenende, A.R. Towards design strategies for circular medical products. Resour. Conserv. Recycl. 2018, 135, 38–47. [Google Scholar] [CrossRef]
- Di Foggia, G.; Beccarello, M. Designing waste management systems to meet circular economy goals: The Italian case. Sustain. Prod. Consump. 2021, 26, 1074–1083. [Google Scholar] [CrossRef]
- Bocken, N.M.; De Pauw, I.; Bakker, C.; Van Der Grinten, B. Product design and business model strategies for a circular economy. J. Ind. Prod. Eng. 2016, 33, 308–320. [Google Scholar] [CrossRef]
- Geissdoerfer, M.; Savaget, P.; Bocken, N.M.P.; Hultink, E.J. The Circular Economy A new sustainability paradigm? J. Clean Prod. 2017, 143, 757–768. [Google Scholar] [CrossRef]
- Overcash, M. A Comparison of Reusable and Disposable Perioperative Textiles: Sustainability State-of-the-Art 2012 (vol 114, pg 1055, 2012). Anesth. Analg. 2012, 115, 733. [Google Scholar] [CrossRef]
- AMDR. Available online: https://amdr.org/ (accessed on 2 January 2020).
- Ranjbari, M.; Esfandabadi, Z.S.; Shevchenko, T.; Chassagnon-Haned, N.; Peng, W.; Tabatabaei, M.; Aghbashlo, M. Mapping healthcare waste management research: Past evolution, current challenges, and future perspectives towards a circular economy transition. J. Hazard. Mater. 2022, 422, 126724. [Google Scholar] [CrossRef]
- IHI. Available online: https://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx (accessed on 2 January 2020).
- Despeisse, M.; Baumers, M.; Brown, P.; Charnley, F.; Ford, S.J.; Garmulewicz, A.; Knowles, S.; Minshall, T.H.W.; Mortara, L.; Reed-Tsochas, F.P.; et al. Unlocking value for a circular economy through 3D printing: A research agenda. Technol. Forecast. Soc. Chang. 2017, 115, 75–84. [Google Scholar] [CrossRef]
- Kirchherr, J.; Piscicelli, L.; Bour, R.; Kostense-Smit, E.; Muller, J.; Huibrechtse-Truijens, A.; Hekkert, M. Barriers to the Circular Economy: Evidence From the European Union (EU). Ecol. Econ. 2018, 150, 264–272. [Google Scholar] [CrossRef]
- Barquet, A.P.B.; de Oliveira, M.G.; Amigo, C.R.; Cunha, V.P.; Rozenfeld, H. Employing the business model concept to support the adoption of product-service systems (PSS). Ind. Market Manag. 2013, 42, 693–704. [Google Scholar] [CrossRef]
- Agrawal, R.; Wankhede, V.A.; Kumar, A.; Luthra, S. Analysing the roadblocks of circular economy adoption in the automobile sector: Reducing waste and environmental perspectives. Bus. Strategy Environ. 2021, 30, 1051–1066. [Google Scholar] [CrossRef]
- Ormazabal, M.; Prieto-Sandoval, V.; Puga-Leal, R.; Jaca, C. Circular Economy in Spanish SMEs: Challenges and opportunities. J. Clean. Prod. 2018, 185, 157–167. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, W.; Wang, T.; Xu, Y.; Du, H. Impact of subsidies on innovations of environmental protection and circular economy in China. J. Environ. Manag. 2021, 289, 112385. [Google Scholar] [CrossRef]
- Masi, D.; Day, S.; Godsell, J. Supply Chain Configurations in the Circular Economy: A Systematic Literature Review. Sustainability 2017, 9, 1602. [Google Scholar] [CrossRef]
- Tingley, D.D.; Cooper, S.; Cullen, J. Understanding and overcoming the barriers to structural steel reuse, a UK perspective. J. Clean. Prod. 2017, 148, 642–652. [Google Scholar] [CrossRef]
- Devi, A.; Ravindra, K.; Kaur, M.; Kumar, R. Evaluation of biomedical waste management practices in public and private sector of health care facilities in India. Environ. Sci. Pollut. Res. 2019, 26, 26082–26089. [Google Scholar] [CrossRef]
- Tukker, A. Product services for a resource-efficient and circular economy—A review. J. Clean. Prod. 2015, 97, 76–91. [Google Scholar] [CrossRef]
- Bressanelli, G.; Perona, M.; Saccani, N. Challenges in supply chain redesign for the Circular Economy: A literature review and a multiple case study. Int. J. Prod. Res. 2019, 57, 7395–7422. [Google Scholar] [CrossRef]
- Tabash, M.I.; Hussein, R.A.; Mahmoud, A.H.; El-Borgy, M.D.; Abu-Hamad, B.A. Impact of an intervention programme on knowledge, attitude and practice of healthcare staff regarding pharmaceutical waste management, Gaza, Palestine. Public Health 2016, 138, 127–137. [Google Scholar] [CrossRef]
- Bang, J.Y.; Hawes, R.; Varadarajulu, S. Equivalent performance of single-use and reusable duodenoscopes in a randomised trial. Gut 2021, 70, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Dhagarra, D.; Goswami, M.; Sarma, P.R.S.; Choudhury, A. Big Data and blockchain supported conceptual model for enhanced healthcare coverage The Indian context. Bus Process Manag. J. 2019, 25, 1612–1632. [Google Scholar] [CrossRef]
- Kumar, P.; Singh, R.K.; Kumar, V. Managing supply chains for sustainable operations in the era of industry 4.0 and circular economy: Analysis of barriers. Resour. Conserv. Recycl. 2021, 164, 105215. [Google Scholar] [CrossRef]
- Govindan, K.; Hasanagic, M. A systematic review on drivers, barriers, and practices towards circular economy: A supply chain perspective. Int. J. Prod. Res. 2018, 56, 278–311. [Google Scholar] [CrossRef]
- Abdelsalam, M.K.; Egdair, I.M.M.; Begum, H.; Jadi, D.M.; Al Issa, H.E.; Abrika, O.S.S.; Alam, A.S.A.F. The Key Organizational Factors in Healthcare Waste Management Practices of Libyan Public Hospitals. Sustainability 2021, 13, 2785. [Google Scholar] [CrossRef]
- Ranta, V.; Aarikka-Stenroos, L.; Ritala, P.; Makinen, S.J. Exploring institutional drivers and barriers of the circular economy: A cross-regional comparison of China, the US, and Europe. Resour. Conserv. Recycl. 2018, 135, 70–82. [Google Scholar] [CrossRef]
- Kandasamy, J.; Kinare, Y.P.; Pawar, M.T.; Majumdar, A.; Vimal, K.E.K.; Agrawal, R. Circular economy adoption challenges in medical waste management for sustainable development: An empirical study. Sustain. Dev. 2022, 30, 958–975. [Google Scholar] [CrossRef]
- Selvaranjan, K.; Navaratnam, S.; Rajeev, P.; Ravintherakumaran, N. Environmental challenges induced by extensive use of face masks during COVID-19: A review and potential solutions. Environ. Chall. 2021, 3, 100039. [Google Scholar] [CrossRef]
- Hossain, M.S.; Balakrishnan, V.; Ab Rahman, N.N.N.; Sarker, M.Z.I.; Ab Kadir, M.O. Treatment of Clinical Solid Waste Using a Steam Autoclave as a Possible Alternative Technology to Incineration. Int. J. Environ. Res. Public Health 2012, 9, 855–867. [Google Scholar] [CrossRef]
- Bouzon, M.; Govindan, K.; Rodriguez, C.M.T. Evaluating barriers for reverse logistics implementation under a multiple stakeholders’ perspective analysis using grey decision making approach. Resour. Conserv. Recycl. 2018, 128, 315–335. [Google Scholar] [CrossRef]
- Patil, A.; Shardeo, V.; Dwivedi, A.; Madaan, J.; Varma, N. Barriers to sustainability in humanitarian medical supply chains. Sustain. Prod. Consump. 2021, 27, 1794–1807. [Google Scholar] [CrossRef]
- Kazancoglu, Y.; Sagnak, M.; Lafci, C.; Luthra, S.; Kumar, A.; Tacoglu, C. Big Data-Enabled Solutions Framework to Overcoming the Barriers to Circular Economy Initiatives in Healthcare Sector. Int. J. Environ. Res. Public Health 2021, 18, 7513. [Google Scholar] [CrossRef] [PubMed]
- Karuppiah, K.; Sankaranarayanan, B.; Ali, S.M.; Paul, S.K. Key Challenges to Sustainable Humanitarian Supply Chains: Lessons from the COVID-19 Pandemic. Sustainability 2021, 13, 5850. [Google Scholar] [CrossRef]
- Ghisellini, P.; Cialani, C.; Ulgiati, S. A review on circular economy: The expected transition to a balanced interplay of environmental and economic systems. J. Clean. Prod. 2016, 114, 11–32. [Google Scholar] [CrossRef]
- Sohrabi, M.; Zandieh, M.; Nadjafi, B.A. Dynamic demand-centered process-oriented data model for inventory management of hemovigilance systems. Healthc. Inform. Res. 2021, 27, 73–81. [Google Scholar] [CrossRef]
- Anand, A.; Agarwal, M.; Aggrawal, D. Multiple Criteria Decision-Making Methods: Applications for Managerial Discretion; Walter de Gruyter GmbH & Co KG: Berlin/Heidelberg, Germany, 2022; Volume 14. [Google Scholar]
- Vinodh, S.; Wankhede, V.A. Application of fuzzy DEMATEL and fuzzy CODAS for analysis of workforce attributes pertaining to Industry 4.0: A case study. Int. J. Qual. Reliab. Manag. 2020, 38, 1695–1721. [Google Scholar] [CrossRef]

| Main Challenges | Code | Sub-Challenges | Code |
|---|---|---|---|
| Supply Chain Management Challenges | C1 | Uncertainty in return flows | S1 |
| Lack of consideration for a CE supply chain | S2 | ||
| Inefficient resource utilization | S3 | ||
| Lack of flexibility in implementation of CE phases | S4 | ||
| Challenges in taking back products (4Rs) | S5 | ||
| Regulation and Policies Challenges | C2 | Lack of governmental legislation on CE healthcare policies | R1 |
| Lack of sustainability foundation practices, incentives and policies | R2 | ||
| Lack of R&D to reinforce sustainability practices and create/update new legislation | R3 | ||
| Lack of standards for existing CE | R4 | ||
| Industry Challenges | C3 | Resistance to improve existing practices to be sustainable | I1 |
| Minimal knowledge on training and expertise for sustainability practices | I2 | ||
| Lack of realistic CE business model | I3 | ||
| Lack of consumer interest in the environment | I4 | ||
| Organization’s Internal challenges | C4 | Carelessness in usage | O1 |
| Poor contribution by stakeholders (information exchange) | O2 | ||
| Strict requirements for advanced education and training | O3 | ||
| Conflict of interests among departments | O4 | ||
| Technology and Operational Challenges | C5 | Lack of environmentally friendly disposal practices | T1 |
| Challenges in reprocessing | T2 | ||
| Insufficient product traceability | T3 | ||
| The associated complexity with circular economy practices | T4 | ||
| Lack of key performance indexes to adequately measure “green” performance of hospitals | T5 | ||
| Minimal advocation to use medical informatics to reinforce sustainability | T6 | ||
| Economic/Funding Challenges | C6 | Low eco-efficiency of technological processes | E1 |
| Conflict of interests and poor communication among departments | E2 | ||
| High costs associated with circular economy disposal practices | E3 | ||
| Unwillingness to invest more | E4 | ||
| Inadequate allocation of funds | E5 | ||
| Social Challenges | C7 | Cultural barriers | SO1 |
| Minimal public incentives and interest regarding sustainability practices | SO2 | ||
| Lack of awareness about CE practices and resources | SO3 | ||
| The widespread use disposal of medical products/devices/supplies | SO4 | ||
| Lack of environmental impact awareness on public health | SO5 |
| Code | Description | References |
|---|---|---|
| S1 | Uncertainty in the quality, quantity, timing, and location of end-of-use returned products makes capacity planning challenging. | [23] |
| S2 | Minimal knowledge on adapting current supply chains: closing the supply loop to make it more efficient. | [24] |
| S3 | Inaccuracies in forecasting. Ordering items solely based on what is currently needed instead of for the future. | [25] |
| S4 | Inflexible infrastructure and processes to improve current methods to be more sustainable. (Segregation, transportation, disposal). | [15] |
| S5 | Reduce|Re-use|Recycle|Recover is challenging. | [26] |
| R1 | Governmental legislation is needed to enforce organizations transitions to CE to achieve advantages in terms of resource use efficiency. | [27] |
| R2 | Government should emphasize and incentivize hospitals to adopt CE practices to reduce public health impact. And, to save the hospitals money. | [8] |
| R3 | Lack of studies in the CE field emphasizing the importance of transitioning to a CE. | [28] |
| R4 | As CE is an emerging field, metrics for measuring a hospitals performance are generally archaic and not in line with sustainable technologies. | [29] |
| I1 | Changes to be more sustainable have implications (cost, time, effort, etc.) and thus there is a resistance to shift practices. | [30] |
| I2 | Not enough training programs in healthcare sustainability emphasizing CE waste management. | [31] |
| I3 | A business model would ease the process on hospitals. Unavailability of proper CE business models creates problems. | [24] |
| I4 | If consumers aren’t interested enough to protect the environment, implementation of CE is difficult. | [27] |
| O1 | Consuming items without considering consequences. Over-use without taking responsibility. | [25,32] |
| O2 | Information exchange between hospitals stakeholders and government representatives in order to adopt sustainable healthcare systems. | [8] |
| O3 | No incentives to educate and train extensively (financially, socially, etc.) | [33] |
| O4 | The easiest methods are generally the most attractive and least sustainable. | [34] |
| T1 | Poor responsiveness from hospitals to adapt more “green” waste management methods. | [3] |
| T2 | Hospitals avoid reprocessing due to the liability issues, maintenance, cost, approval for reprocessed products. | [35] |
| T3 | Information systems are generally insufficient, and the inability to trace products makes it difficult to collect and refurbish products. | [30] |
| T4 | Minimal technological product infrastructure. Current technological infrastructure is difficult to adapt to shifting towards CE practices. | [15] |
| T6 | A CE focus requires a shift from a solely volume drive economic approach to consider triple bottom line (economic, environmental, and social factors) | [29] |
| T7 | In general, current practices rely on vintage techniques to trace medical waste. The use of digital technology could be beneficial from a sustainability perspective. | [36] |
| E1 | Recycling operations may be expensive and inefficient, which result in material loss and cross contamination. | [37] |
| E2 | CE needs efficient coordination and information exchange throughout all departments, which is difficult to implement due to budgeting limitations. | [30] |
| E3 | Implementing CE increases manufacturing cost due to the urgency to reuse/recycle products. | [38] |
| E5 | Always the consumer-aim is to reduce cost when pricing is a key factor for profitability. There is a cost associated with CE due to reprocessing/reusing for some products | [31] |
| E6 | Poor financial planning leads to lack of investment in CE practices. Which is an area to focus on to reduce environmental impact. | [31] |
| SO1 | Conflict in medical waste management practices due to backgrounds and cultural differences. Some cultures are accustomed to disposing of things immediately, while others may not be. | [39] |
| SO2 | Not enough social incentive to be more “green” due to many factors: education, funding, and public awareness. | [40] |
| SO3 | Lack of education and resources available regarding the new trends in waste management to reinforce sustainability. | [41] |
| SO4 | Due to the pandemic, much research has been done in waste management practices to negate the problems associated with single use products. | [42] |
| SO5 | Lack of consumer interest in reducing environmental impact of improper waste management techniques. | [43] |
| Objectives | Methods | Outcomes | Limitations | Sources | Journal | |
|---|---|---|---|---|---|---|
| 1 | Investigate medical and pharmaceutical waste management | Fuzzy best-worse | Material issues are the largest barrier to sustainability. | Lack of diversity in respondents | [45] | Sustainable Production and Consumption |
| 2 | Identify barriers related to Circular Economy in Healthcare Sector. | Fuzzy best-worse and Fuzzy Vikor | High-cost requirement for circular technologies and implementations was found to be most important barrier. | Study conducted in a country with a developing economy. | [46] | International Journal of Environmental Research and Public Health |
| 3 | Identify and evaluate challenges hampering sustainable humanitarian supply chain management during COVID-19. | AHP and TODIM | Facility location problems, short lead times for supplies, spread of rumors, emergence of new clusters, doubt concerning vaccine are critical challenges. | Study conducted in India only and based on local expert feedback. | [47] | Sustainability |
| 4 | Investigate circular economy adoption challenges. | Fuzzy theory | Most significant group of challenges related to supply chain management and technology. | Study conducted in a country with a developing economy. | [41] | Wiley |
| 5 | Provide inclusive map of background of Waste Management and Circular Economy over the last two decades. | Mixed-Method Approach | Identified seven major research themes. | Research themes clustered based on bibliographic coupling of articles. | [14] | Journal of Cleaner Production |
| 6 | Provide review of literature on main CE features. | Literature Review | Future evaluation and monitoring needed on CE principles applied. | [48] | Journal of Cleaner Production | |
| 7 | Propose a dynamic demand-centered framework for managing a blood banks inventory. | Object Oriented and Integrated Computer Aided Manufacturing (ICAM). | Developed a model that captures top features of the inventory system to understand the systems elements and attributes. | Future research requires a mathematical optimization model alongside the framework, | [49] | Healthcare Informatics Research |
| Expert | Education Level | Position of the Participants | Years of Work Experience | Hospital Specialty |
|---|---|---|---|---|
| 1 | Bachelor’s degree | Environmental Director (Environmental services, EV) | More than 20 years | General hospital |
| 2 | Bachelor’s degree | Director of Facilities & Operations | More than 20 years | General hospital |
| 3 | Master’s degree | Assistant Vice President (AVP), Support Services | More than 10 years | Independent non-profit hospital |
| Intensity of Value | Interpretation |
|---|---|
| 0 | No influence |
| 1 | Very low influence (xi has very low influence over xi) |
| 2 | Low influence (xi has low influence over xi) |
| 3 | High influence (xi has high influence over xi) |
| 4 | Very high influence (xi has very high influence over xi) |
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | |
|---|---|---|---|---|---|---|---|
| C1 | 0 | 2 | 2 | 2 | 2 | 2 | 2 |
| C2 | 2 | 0 | 3 | 2 | 3 | 2 | 2 |
| C3 | 2 | 2 | 0 | 3 | 2 | 2 | 2 |
| C4 | 2 | 2 | 3 | 0 | 2 | 2 | 2 |
| C5 | 2 | 2 | 2 | 2 | 0 | 2 | 2 |
| C6 | 2 | 2 | 2 | 2 | 2 | 0 | 2 |
| C7 | 1 | 2 | 2 | 1 | 2 | 2 | 0 |
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | |
|---|---|---|---|---|---|---|---|
| C1 | 0 | 0.079 | 0.079 | 0.095 | 0.095 | 0.079 | 0.095 |
| C2 | 0.079 | 0 | 0.127 | 0.111 | 0.127 | 0.095 | 0.095 |
| C3 | 0.079 | 0.111 | 0 | 0.143 | 0.111 | 0.095 | 0.111 |
| C4 | 0.079 | 0.095 | 0.127 | 0 | 0.111 | 0.095 | 0.095 |
| C5 | 0.079 | 0.111 | 0.095 | 0.111 | 0 | 0.095 | 0.111 |
| C6 | 0.079 | 0.095 | 0.095 | 0.095 | 0.095 | 0 | 0.095 |
| C7 | 0.063 | 0.079 | 0.079 | 0.063 | 0.079 | 0.079 | 0 |
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | |
|---|---|---|---|---|---|---|---|
| C1 | 0.088 | 0.182 | 0.187 | 0.203 | 0.203 | 0.176 | 0.200 |
| C2 | 0.180 | 0.131 | 0.250 | 0.241 | 0.253 | 0.211 | 0.224 |
| C3 | 0.182 | 0.233 | 0.140 | 0.269 | 0.243 | 0.213 | 0.239 |
| C4 | 0.175 | 0.212 | 0.244 | 0.134 | 0.233 | 0.205 | 0.217 |
| C5 | 0.174 | 0.224 | 0.217 | 0.232 | 0.133 | 0.204 | 0.229 |
| C6 | 0.167 | 0.202 | 0.208 | 0.210 | 0.210 | 0.109 | 0.207 |
| C7 | 0.136 | 0.167 | 0.171 | 0.160 | 0.174 | 0.162 | 0.098 |
| Criteria (Main Groups of Challenges) | Ri | Ci | Ri + Ci | Ri − Ci | Identify |
|---|---|---|---|---|---|
| Supply Chain Management Challenges | 1.238 | 1.101 | 2.339 | 0.137 | Cause |
| Regulation and Policies Challenges | 1.490 | 1.349 | 2.839 | 0.140 | Cause |
| Industry Challenges | 1.518 | 1.418 | 2.936 | 0.100 | Cause |
| Organization’s Internal challenges | 1.420 | 1.449 | 2.869 | −0.029 | Effect |
| Technology and Operational Challenges | 1.413 | 1.448 | 2.861 | −0.035 | Effect |
| Economic/Funding Challenges | 1.312 | 1.279 | 2.591 | 0.033 | Cause |
| Social Challenges | 1.068 | 1.415 | 2.483 | −0.347 | Effect |
| Main Groups of Challenges | Sub- Challenges | Ri | Ci | Ri + Ci | Ri − Ci | Identify |
|---|---|---|---|---|---|---|
| Supply Chain Management Challenges | S1 | 13.09 | 12.70 | 25.79 | 0.38 | Cause |
| S2 | 13.20 | 12.70 | 25.90 | 0.50 | Cause | |
| S3 | 13.19 | 12.89 | 26.08 | 0.30 | Cause | |
| S4 | 12.21 | 12.24 | 24.45 | −0.03 | Effect | |
| S5 | 5.89 | 7.05 | 12.94 | −1.15 | Effect | |
| Regulation and Policies Challenges | R1 | 9.99 | 8.36 | 18.35 | 1.63 | Cause |
| R2 | 9.16 | 8.36 | 17.52 | 0.80 | Cause | |
| R3 | 7.96 | 8.77 | 16.73 | −0.81 | Effect | |
| R4 | 8.36 | 9.97 | 18.34 | −1.61 | Effect | |
| Industry Challenges | I1 | 11.13 | 12.59 | 23.72 | −1.46 | Effect |
| I2 | 10.80 | 11.99 | 22.79 | −1.20 | Effect | |
| I3 | 11.97 | 11.70 | 23.67 | 0.28 | Cause | |
| I4 | 12.30 | 9.92 | 22.22 | 2.38 | Cause | |
| Organization’s Internal challenges | O1 | 11.21 | 10.71 | 21.92 | 0.51 | Cause |
| O2 | 10.44 | 10.96 | 21.40 | −0.52 | Effect | |
| O3 | 11.21 | 10.71 | 21.92 | 0.51 | Cause | |
| O4 | 10.96 | 11.46 | 22.42 | −0.50 | Effect | |
| Technology and Operational Challenges | T1 | 11.32 | 11.69 | 23.01 | −0.37 | Effect |
| T2 | 10.97 | 12.13 | 23.10 | −1.16 | Effect | |
| T3 | 9.98 | 10.04 | 20.03 | −0.06 | Effect | |
| T4 | 11.83 | 10.80 | 22.63 | 1.03 | Cause | |
| T5 | 10.73 | 10.76 | 21.49 | −0.04 | Effect | |
| T6 | 10.81 | 10.21 | 21.02 | 0.59 | Cause | |
| Economic/Funding Challenges | E1 | 4.53 | 5.02 | 9.56 | −0.49 | Effect |
| E2 | 4.68 | 5.02 | 9.70 | −0.35 | Effect | |
| E3 | 5.70 | 5.97 | 11.67 | −0.27 | Effect | |
| E4 | 5.74 | 5.54 | 11.28 | 0.20 | Effect | |
| E5 | 5.87 | 4.97 | 10.84 | 0.90 | Cause | |
| Social Challenges | SO1 | 9.85 | 9.85 | 19.70 | 0.00 | N/A |
| SO2 | 10.48 | 9.48 | 19.96 | 0.99 | Cause | |
| SO3 | 10.18 | 9.48 | 19.66 | 0.70 | Cause | |
| SO4 | 9.50 | 11.14 | 20.64 | −1.64 | Effect | |
| SO5 | 10.17 | 10.22 | 20.39 | −0.05 | Effect |
| # | Main Challenges Group | Group Weight | # | Sub- Challenge Code | Local Weight | Local Ranking | Global Weight | Global Rank |
|---|---|---|---|---|---|---|---|---|
| 1 | Supply Chain Management Challenges | 0.131 | 1 | S1 | 0.2272 | 3 | 0.0298 | 18 |
| 2 | S2 | 0.2292 | 1 | 0.0300 | 14 | |||
| 3 | S3 | 0.2291 | 2 | 0.0300 | 16 | |||
| 4 | S4 | 0.2121 | 4 | 0.0278 | 19 | |||
| 5 | S5 | 0.1024 | 5 | 0.0134 | 33 | |||
| 2 | Regulation and Policies Challenges | 0.157 | 6 | R1 | 0.2816 | 1 | 0.0443 | 1 |
| 7 | R2 | 0.2582 | 2 | 0.0407 | 4 | |||
| 8 | R3 | 0.2244 | 4 | 0.0353 | 12 | |||
| 9 | R4 | 0.2358 | 3 | 0.0371 | 10 | |||
| 3 | Industry Challenges | 0.160 | 10 | I1 | 0.2409 | 3 | 0.0387 | 5 |
| 11 | I2 | 0.2337 | 4 | 0.0375 | 9 | |||
| 12 | I3 | 0.2592 | 2 | 0.0416 | 3 | |||
| 13 | I4 | 0.2662 | 1 | 0.0427 | 2 | |||
| 4 | Organization’s Internal challenges | 0.150 | 14 | O1 | 0.2559 | 1 | 0.0384 | 6 |
| 15 | O2 | 0.2382 | 4 | 0.0358 | 11 | |||
| 16 | O3 | 0.2559 | 1 | 0.0384 | 6 | |||
| 17 | O4 | 0.2501 | 3 | 0.0375 | 8 | |||
| 5 | Technology and Operational Challenges | 0.149 | 18 | T1 | 0.1725 | 2 | 0.0258 | 21 |
| 19 | T2 | 0.1671 | 3 | 0.0250 | 22 | |||
| 20 | T3 | 0.1521 | 6 | 0.0227 | 30 | |||
| 21 | T4 | 0.1802 | 1 | 0.0269 | 20 | |||
| 22 | T5 | 0.1634 | 5 | 0.0244 | 25 | |||
| 23 | T6 | 0.1646 | 4 | 0.0246 | 23 | |||
| 6 | Economic/Funding Challenges | 0.139 | 24 | E1 | 0.1710 | 5 | 0.0237 | 26 |
| 25 | E2 | 0.1763 | 4 | 0.0245 | 24 | |||
| 26 | E3 | 0.2149 | 3 | 0.0298 | 17 | |||
| 27 | E4 | 0.2164 | 2 | 0.0300 | 15 | |||
| 28 | E5 | 0.2213 | 1 | 0.0307 | 13 | |||
| 7 | Social Challenges | 0.113 | 29 | SO1 | 0.1963 | 4 | 0.0222 | 31 |
| 30 | SO2 | 0.2088 | 1 | 0.0236 | 27 | |||
| 31 | SO3 | 0.2029 | 2 | 0.0229 | 28 | |||
| 32 | SO4 | 0.1893 | 5 | 0.0214 | 32 | |||
| 33 | SO5 | 0.2027 | 3 | 0.0229 | 29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahjoob, A.; Alfadhli, Y.; Omachonu, V. Healthcare Waste and Sustainability: Implications for a Circular Economy. Sustainability 2023, 15, 7788. https://doi.org/10.3390/su15107788
Mahjoob A, Alfadhli Y, Omachonu V. Healthcare Waste and Sustainability: Implications for a Circular Economy. Sustainability. 2023; 15(10):7788. https://doi.org/10.3390/su15107788
Chicago/Turabian StyleMahjoob, Abrar, Yousef Alfadhli, and Vincent Omachonu. 2023. "Healthcare Waste and Sustainability: Implications for a Circular Economy" Sustainability 15, no. 10: 7788. https://doi.org/10.3390/su15107788
APA StyleMahjoob, A., Alfadhli, Y., & Omachonu, V. (2023). Healthcare Waste and Sustainability: Implications for a Circular Economy. Sustainability, 15(10), 7788. https://doi.org/10.3390/su15107788







