Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience
Abstract
:1. Introduction
2. Materials and Methods
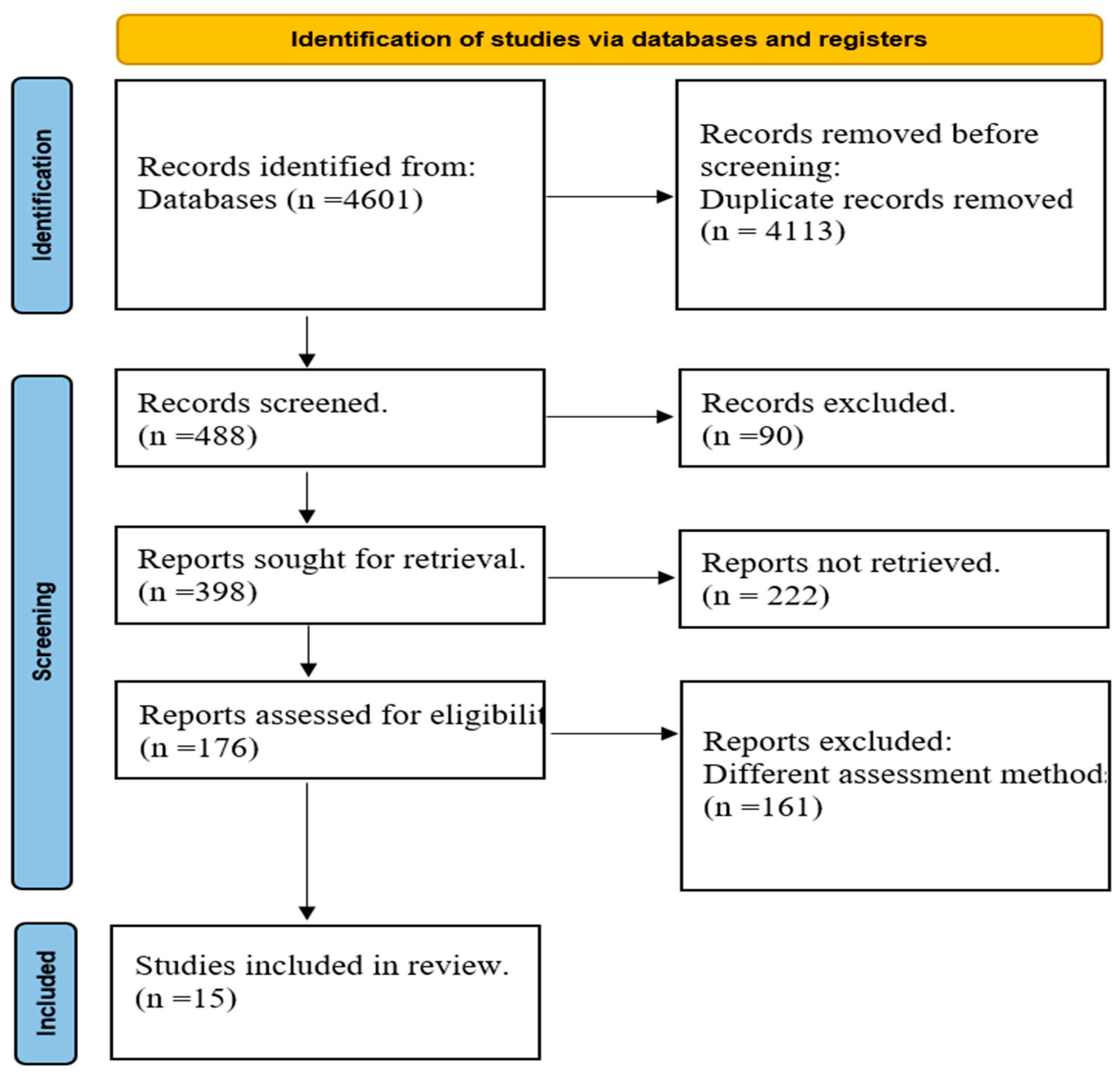
2.1. Search Strategy and Selection Criteria
2.2. Eligibility Screening
2.3. Data Extraction
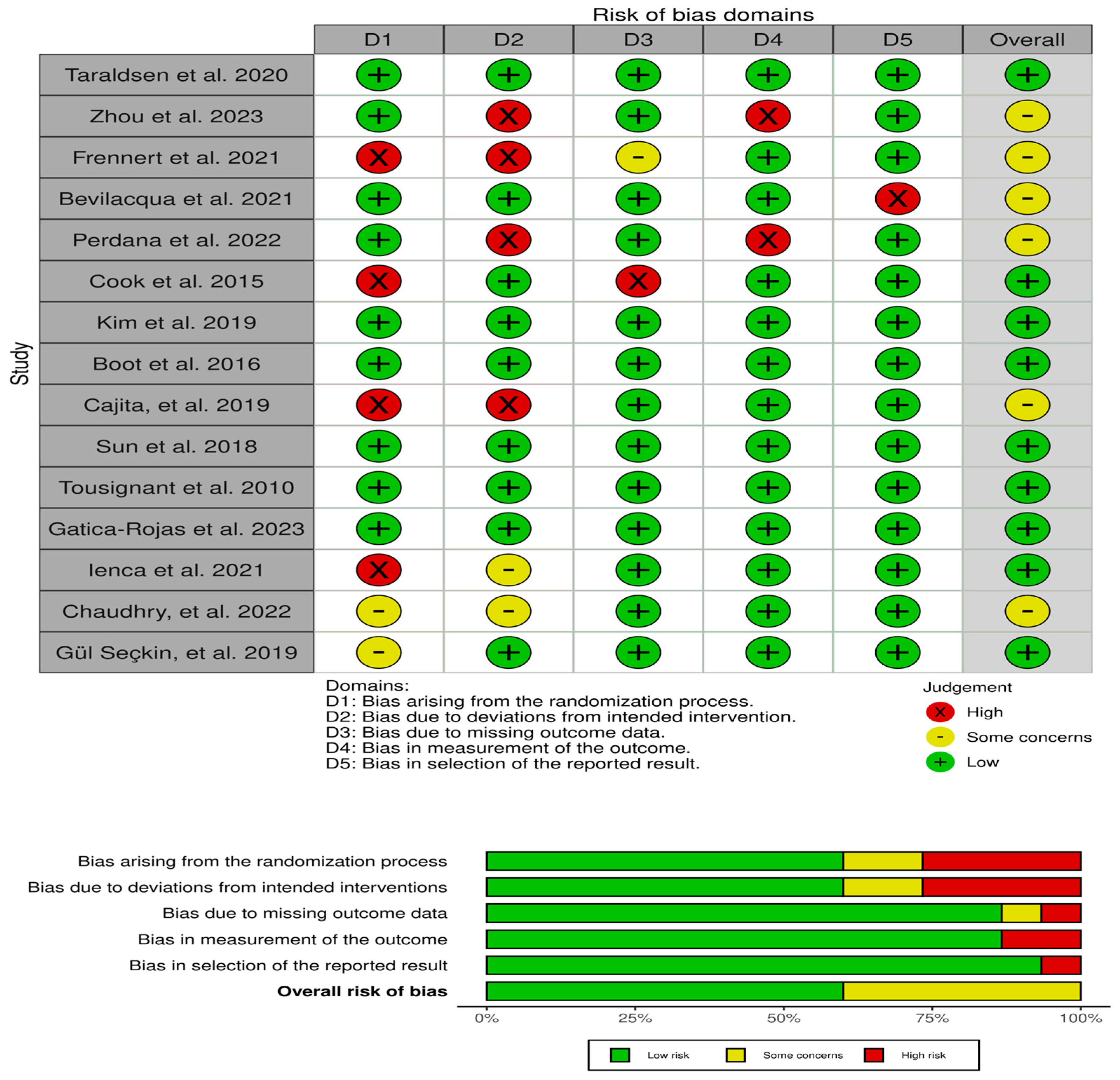
2.4. Assessment of Methodological Quality and Bias
2.5. Data Analysis
- The data analysis methods of this systematic review include the following methods: Narrative Synthesis: The proposed qualitative technology will include the synthesis and analysis of data from selected studies relating to adoption rates, effectiveness and user perception of digital health treatments in the context of promoting healthy aging. The utilization of narrative synthesis will facilitate a comprehensive comprehension of the implications for both users and healthcare providers.
- The thematic analysis: is used to get and systematically classify similar themes, patterns, and effects observed in a particular study. The present procedure will entail the coding of research outcomes pertaining to the domains of adoption, efficacy, and user experiences in the context of digital health interventions. This study aims to enable a comprehensive examination of the interconnections and diversities within these overarching concepts, thereby offering valuable perspectives on the efficacy and obstacles linked to various digital health interventions in the context of promoting optimal aging.
3. Results
3.1. The Quality Assessment
3.2. Main Outcomes
- Digital Health Adoption Patterns in the Elderly
- Efficacy of Digital Health Interventions for the Elderly and the Health Team
- Implementing Digital Health in Healthcare Systems
- Ethical Considerations for Patient-Centric Solutions
4. Discussion
4.1. Adoption Rates of Digital Health Interventions
4.2. Efficacy of Digital Health Interventions
4.3. User Experience of Digital Health Interventions
4.4. Digital Health Adoption Patterns
4.5. Efficacy of Digital Health Interventions
4.6. Implementing Digital Health in Healthcare Systems
4.7. Ethical Considerations for Patient-Centric Solutions
4.8. Methodological Considerations and Limitations
4.9. Future Research and Recommendations:
- Conduct more rigorous randomized controlled trials to establish efficacy evidence for different types of digital health interventions in promoting healthy aging. Outcomes should include clinically meaningful measures of health, functioning, quality of life, healthcare utilization and costs;
- Longitudinal research is needed to evaluate long-term impacts, effectiveness over time as technologies and needs change, and sustainability of adoption into routine care and lifestyles;
- Comparative effectiveness research can elucidate which digital solutions work best for specific conditions, populations and healthcare systems/models.
- Studies should include broader populations from diverse settings and backgrounds to ensure equitable representation beyond current high-income-focused research;
- Further qualitative research can deepen understanding of user experiences, needs, perspectives on ethics/trust and optimization of technologies based directly on end-user feedback;
- Implementation science studies are warranted to evaluate real-world integration into care delivery, identify barriers/facilitators, and test strategies for scalable adoption addressing organizational factors;
- Health economic analyses can strengthen the case for investment and reimbursement by quantifying cost offsets from reduced hospitalizations, complications and informal caregiving needs;
- Policy research should explore approaches for addressing digital and health literacy divides, accessibility standards, data governance frameworks, and workforce training/skills.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yumiko, Y.; Lai, N.M.S..; Schmid, K. World Population Ageing; United Nations: New York, NY, USA, 2020; ISBN 9789211483475. [Google Scholar]
- Dobriansky, P.J.; Suzman, R.M.; Hodes, R.J. Why Population Aging Matters-A Global Perspective; US Department of State: Washington, DC, USA, 2007; pp. 1–32. [Google Scholar]
- Jaul, E.; Barron, J. Age-Related Diseases and Clinical and Public Health Implications for the 85 Years Old and Over Population. Front. Public Health 2017, 5, 335. [Google Scholar] [CrossRef] [PubMed]
- Noto, S. Perspectives on Aging and Quality of Life. Healthcare 2023, 11, 2131. [Google Scholar] [CrossRef] [PubMed]
- Kurjak, A.; Jakovljevic, M.; Masic, I.; Stanojevic, M. Healthy Ageing in the Time of Corona Pandemic. Med. Arch. 2021, 75, 4. [Google Scholar] [CrossRef]
- Kasoju, N.; Remya, N.S.; Sasi, R.; Sujesh, S.; Soman, B.; Kesavadas, C.; Muraleedharan, C.V.; Varma, P.R.H.; Behari, S. Digital Health: Trends, Opportunities and Challenges in Medical Devices, Pharma and Bio-Technology. CSI Trans. ICT 2023, 11, 11–30. [Google Scholar] [CrossRef]
- Senbekov, M.; Saliev, T.; Bukeyeva, Z.; Almabayeva, A.; Zhanaliyeva, M.; Aitenova, N.; Toishibekov, Y.; Fakhradiyev, I. The Recent Progress and Applications of Digital Technologies in Healthcare: A Review. Int. J. Telemed. Appl. 2020, 2020, 8830200. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Pratap Singh, R.; Suman, R. Medical 4.0 Technologies for Healthcare: Features, Capabilities, and Applications. Internet Things Cyber-Phys. Syst. 2022, 2, 12–30. [Google Scholar] [CrossRef]
- Marcum, Z.A.; Hanlon, J.T.; Murray, M.D. Improving Medication Adherence and Health Outcomes in Older Adults: An Evidence-Based Review of Randomized Controlled Trials. Drugs Aging 2017, 34, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Kwame, A.; Petrucka, P.M. A Literature-Based Study of Patient-Centered Care and Communication in Nurse-Patient Interactions: Barriers, Facilitators, and the Way Forward. BMC Nurs. 2021, 20, 158. [Google Scholar] [CrossRef]
- Ienca, M.; Schneble, C.; Kressig, R.W.; Wangmo, T. Digital Health Interventions for Healthy Ageing: A Qualitative User Evaluation and Ethical Assessment. BMC Geriatr. 2021, 21, 412. [Google Scholar] [CrossRef]
- Dermody, G.; Fritz, R.; Glass, C.; Dunham, M.; Whitehead, L. Factors Influencing Community-dwelling Older Adults’ Readiness to Adopt Smart Home Technology: A Qualitative Exploratory Study. J. Adv. Nurs. 2021, 77, 4847–4861. [Google Scholar] [CrossRef]
- Hunter, I.; Elers, P.; Lockhart, C.; Guesgen, H.; Singh, A.; Whiddett, D. Issues Associated With the Management and Governance of Sensor Data and Information to Assist Aging in Place: Focus Group Study With Health Care Professionals. JMIR mHealth uHealth 2020, 8, e24157. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.T.; Campbell, K.L.; Gong, E.; Scuffham, P. The Internet of Things: Impact and Implications for Health Care Delivery. J. Med. Internet Res. 2020, 22, e20135. [Google Scholar] [CrossRef] [PubMed]
- Maguire, D.; Et, A. Shaping the Future of Digital Technology in Health and Social Care. King’s Fund 2021, 84. [Google Scholar]
- Haque, M.D.R.; Rubya, S. An Overview of Chatbot-Based Mobile Mental Health Apps: Insights From App Description and User Reviews. JMIR mHealth uHealth 2023, 11, e44838. [Google Scholar] [CrossRef] [PubMed]
- Abernethy, A.; Adams, L.; Barrett, M.; Bechtel, C.; Brennan, P.; Butte, A.; Faulkner, J.; Fontaine, E.; Friedhoff, S.; Halamka, J.; et al. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect. 2022, 2022, 6. [Google Scholar] [CrossRef] [PubMed]
- Fortuna, K.L.; Venegas, M.; Umucu, E.; Mois, G.; Walker, R.; Brooks, J.M. The Future of Peer Support in Digital Psychiatry: Promise, Progress, and Opportunities. Curr. Treat. Options Psychiatry 2019, 6, 221–231. [Google Scholar] [CrossRef]
- Patel, S.P.; Sun, E.; Reinhardt, A.; Geevarghese, S.; He, S.; Gazmararian, J.A. Social Determinants of Digital Health Adoption: Pilot Cross-Sectional Survey. JMIR Form. Res. 2022, 6, e39647. [Google Scholar] [CrossRef]
- Wang, T.; Giunti, G.; Melles, M.; Goossens, R. Digital Patient Experience: Umbrella Systematic Review. J. Med. Internet Res. 2022, 24, e37952. [Google Scholar] [CrossRef]
- Benson, T. Digital Innovation Evaluation: User Perceptions of Innovation Readiness, Digital Confidence, Innovation Adoption, User Experience and Behaviour Change. BMJ Health Care Inform. 2019, 26, e000018. [Google Scholar] [CrossRef]
- Flemming, K.; Booth, A.; Garside, R.; Tunçalp, Ö.; Noyes, J. Qualitative Evidence Synthesis for Complex Interventions and Guideline Development: Clarification of the Purpose, Designs and Relevant Methods. BMJ Glob. Health 2019, 4, e000882. [Google Scholar] [CrossRef]
- Ambeskovic, M.; Roseboom, T.J.; Metz, G.A.S. Transgenerational Effects of Early Environmental Insults on Aging and Disease Incidence. Neurosci. Biobehav. Rev. 2020, 117, 297–316. [Google Scholar] [CrossRef] [PubMed]
- Short, S.E.; Mollborn, S. Social Determinants and Health Behaviors: Conceptual Frames and Empirical Advances. Curr. Opin. Psychol. 2015, 5, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Hong, A.; Welch-Stockton, J.; Kim, J.Y.; Canham, S.L.; Greer, V.; Sorweid, M. Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 2554. [Google Scholar] [CrossRef]
- Grady, P.A.; Gough, L.L. Self-Management: A Comprehensive Approach to Management of Chronic Conditions. Am. J. Public Health 2014, 104, e25–e31. [Google Scholar] [CrossRef]
- Friberg-Felsted, K.; Caserta, M. Essentials to Improve the Effectiveness of Healthy Aging Programming: Consideration of Social Determinants and Utilization of a Theoretical Model. Int. J. Environ. Res. Public Health 2023, 20, 6491. [Google Scholar] [CrossRef] [PubMed]
- van Hoof, J.; Marston, H.R.; Kazak, J.K.; Buffel, T. Ten Questions Concerning Age-Friendly Cities and Communities and the Built Environment. Build. Environ. 2021, 199, 107922. [Google Scholar] [CrossRef]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef]
- Reynolds, C.F.; Jeste, D.V.; Sachdev, P.S.; Blazer, D.G. Mental Health Care for Older Adults: Recent Advances and New Directions in Clinical Practice and Research. World Psychiatry 2022, 21, 336–363. [Google Scholar] [CrossRef]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using Social and Behavioural Science to Support COVID-19 Pandemic Response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Won, C.W.; Ha, E.; Jeong, E.; Kim, M.; Park, J.; Baek, J.E.; Kim, S.; Kim, S.B.; Roh, J.; Choi, J.H.; et al. World Health Organization Integrated Care for Older People (ICOPE) and the Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) Study in Korea. Ann. Geriatr. Med. Res. 2021, 25, 10–16. [Google Scholar] [CrossRef]
- Wilson, J.; Heinsch, M.; Betts, D.; Booth, D.; Kay-Lambkin, F. Barriers and Facilitators to the Use of E-Health by Older Adults: A Scoping Review. BMC Public Health 2021, 21, 1556. [Google Scholar] [CrossRef]
- Davenport, T.; Kalakota, R. The Potential for Artificial Intelligence in Healthcare. Futur. Healthc. J. 2019, 6, 94–98. [Google Scholar] [CrossRef]
- Taraldsen, K.; Mikolaizak, A.S.; Maier, A.B.; Mellone, S.; Boulton, E.; Aminian, K.; Becker, C.; Chiari, L.; Follestad, T.; Gannon, B.; et al. Digital Technology to Deliver a Lifestyle-Integrated Exercise Intervention in Young Seniors—The PreventIT Feasibility Randomized Controlled Trial. Front. Digit. Health 2020, 2, 10. [Google Scholar] [CrossRef]
- Sun, X.; Yan, W.; Zhou, H.; Wang, Z.; Zhang, X.; Huang, S.; Li, L. Internet Use and Need for Digital Health Technology among the Elderly: A Cross-Sectional Survey in China. BMC Public Health 2020, 20, 1386. [Google Scholar] [CrossRef] [PubMed]
- Tousignant, M.; Moffet, H.; Boissy, P.; Corriveau, H.; Cabana, F.; Marquis, F. A Randomized Controlled Trial of Home Telerehabilitation for Post-Knee Arthroplasty. J. Telemed. Telecare 2011, 17, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Gatica-Rojas, V.; Cartes-Velásquez, R. Telerehabilitation in Low-Resource Settings to Improve Postural Balance in Older Adults: A Non-Inferiority Randomised Controlled Clinical Trial Protocol. Int. J. Environ. Res. Public Health 2023, 20, 6726. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, B.M.; Dasgupta, D.; Chawla, N.V. Successful Aging for Community-Dwelling Older Adults: An Experimental Study with a Tablet App. Int. J. Environ. Res. Public Health 2022, 19, 13148. [Google Scholar] [CrossRef] [PubMed]
- Seçkin, G.; Hughes, S.; Yeatts, D.; Degreve, T. Digital Pathways to Positive Health Perceptions: Does Age Moderate the Relationship Between Medical Satisfaction and Positive Health Perceptions Among Middle-Aged and Older Internet Users? Innov. Aging 2019, 3, igy039. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Cho, Y.; Shang, S.; Jiang, Y. Use of Digital Health Technology Among Older Adults With Cancer in the United States: Findings From a National Longitudinal Cohort Study (2015–2021). J. Med. Internet Res. 2023, 25, e46721. [Google Scholar] [CrossRef]
- Frennert, S.; Baudin, K. The Concept of Welfare Technology in Swedish Municipal Eldercare. Disabil. Rehabil. 2021, 43, 1220–1227. [Google Scholar] [CrossRef]
- Bevilacqua, R.; Strano, S.; Di Rosa, M.; Giammarchi, C.; Cerna, K.K.; Mueller, C.; Maranesi, E. EHealth Literacy: From Theory to Clinical Application for Digital Health Improvement. Results from the ACCESS Training Experience. Int. J. Environ. Res. Public Health 2021, 18, 11800. [Google Scholar] [CrossRef] [PubMed]
- Perdana, A.; Mokhtar, I.A. Seniors’ Adoption of Digital Devices and Virtual Event Platforms in Singapore during COVID-19. Technol. Soc. 2022, 68, 101817. [Google Scholar] [CrossRef] [PubMed]
- Cook, R.F.; Hersch, R.K.; Schlossberg, D.; Leaf, S.L. A Web-Based Health Promotion Program for Older Workers: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e82. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.K.; Choi, M. Older Adults’ Willingness to Share Their Personal and Health Information When Adopting Healthcare Technology and Services. Int. J. Med. Inform. 2019, 126, 86–94. [Google Scholar] [CrossRef]
- Boot, W.R.; Souders, D.; Charness, N.; Blocker, K.; Roque, N.; Vitale, T. The Gamification of Cognitive Training: Older Adults’ Perceptions of and Attitudes Toward Digital Game-Based Interventions; Springer: Berlin/Heidelberg, Germany, 2016; pp. 290–300. [Google Scholar]
- Cajita, M.I.; Hodgson, N.A.; Lam, K.W.; Yoo, S.; Han, H.-R. Facilitators of and Barriers to MHealth Adoption in Older Adults With Heart Failure. CIN Comput. Inform. Nurs. 2018, 36, 376–382. [Google Scholar] [CrossRef]
- Ahmad, N.A.; Mat Ludin, A.F.; Shahar, S.; Mohd Noah, S.A.; Mohd Tohit, N. Willingness, Perceived Barriers and Motivators in Adopting Mobile Applications for Health-Related Interventions among Older Adults: A Scoping Review. BMJ Open 2022, 12, e054561. [Google Scholar] [CrossRef]
- Harris, M.T.; Blocker, K.A.; Rogers, W.A. Older Adults and Smart Technology: Facilitators and Barriers to Use. Front. Comput. Sci. 2022, 4, 835927. [Google Scholar] [CrossRef]
- Schroeder, T.; Dodds, L.; Georgiou, A.; Gewald, H.; Siette, J. Older Adults and New Technology: Mapping Review of the Factors Associated With Older Adults’ Intention to Adopt Digital Technologies. JMIR Aging 2023, 6, e44564. [Google Scholar] [CrossRef]
- Morrison-Smith, S.; Ruiz, J. Challenges and Barriers in Virtual Teams: A Literature Review; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; Volume 2, ISBN 0123456789. [Google Scholar]
- Kavandi, H.; Jaana, M. Factors That Affect Health Information Technology Adoption by Seniors: A Systematic Review. Health Soc. Care Community 2020, 28, 1827–1842. [Google Scholar] [CrossRef]
- Zin, K.S.L.T.; Kim, S.; Kim, H.-S.; Feyissa, I.F. A Study on Technology Acceptance of Digital Healthcare among Older Korean Adults Using Extended Tam (Extended Technology Acceptance Model). Adm. Sci. 2023, 13, 42. [Google Scholar] [CrossRef]
- Anderson, J.T.; Bouchacourt, L.M.; Sussman, K.L.; Bright, L.F.; Wilcox, G.B. Telehealth Adoption during the COVID-19 Pandemic: A Social Media Textual and Network Analysis. Digit. Health 2022, 8, 205520762210900. [Google Scholar] [CrossRef]
- Agarwal, S.; Punn, N.S.; Sonbhadra, S.K.; Tanveer, M.; Nagabhushan, P.; Pandian, K.K.S.; Saxena, P. Unleashing the Power of Disruptive and Emerging Technologies amid COVID-19: A Detailed Review. arXiv 2020, arXiv:2005.11507. [Google Scholar]
- Felzmann, H.; Villaronga, E.F.; Lutz, C.; Tamò-Larrieux, A. Transparency You Can Trust: Transparency Requirements for Artificial Intelligence between Legal Norms and Contextual Concerns. Big Data Soc. 2019, 6, 205395171986054. [Google Scholar] [CrossRef]
- Jarva, E.; Oikarinen, A.; Andersson, J.; Tuomikoski, A.; Kääriäinen, M.; Meriläinen, M.; Mikkonen, K. Healthcare Professionals’ Perceptions of Digital Health Competence: A Qualitative Descriptive Study. Nurs. Open 2022, 9, 1379–1393. [Google Scholar] [CrossRef]
- Darling-Hammond, L.; Flook, L.; Cook-Harvey, C.; Barron, B.; Osher, D. Implications for Educational Practice of the Science of Learning and Development. Appl. Dev. Sci. 2020, 24, 97–140. [Google Scholar] [CrossRef]
- Conway, C.M.; Kelechi, T.J. Digital Health for Medication Adherence in Adult Diabetes or Hypertension: An Integrative Review. JMIR Diabetes 2017, 2, e20. [Google Scholar] [CrossRef] [PubMed]
- Lear, S.A.; Norena, M.; Banner, D.; Whitehurst, D.G.T.; Gill, S.; Burns, J.; Kandola, D.K.; Johnston, S.; Horvat, D.; Vincent, K.; et al. Assessment of an Interactive Digital Health–Based Self-Management Program to Reduce Hospitalizations Among Patients With Multiple Chronic Diseases. JAMA Netw. Open 2021, 4, e2140591. [Google Scholar] [CrossRef] [PubMed]
- Willis, V.C.; Thomas Craig, K.J.; Jabbarpour, Y.; Scheufele, E.L.; Arriaga, Y.E.; Ajinkya, M.; Rhee, K.B.; Bazemore, A. Digital Health Interventions to Enhance Prevention in Primary Care: Scoping Review. JMIR Med. Informatics 2022, 10, e33518. [Google Scholar] [CrossRef]
- Chrysi, M.S.; Michopoulos, I.; Dimitriadis, G.; Peppa, M. A Modern Web-Based Health Promotion Program for Patients in Greece with Diabetes 2 and Obesity: An Interventional Study. BMC Public Health 2023, 23, 639. [Google Scholar] [CrossRef]
- Monzani, D.; Pizzoli, S.F.M. The Prevention of Chronic Diseases Through EHealth: A Practical Overview. In P5 eHealth: An Agenda for the Health Technologies of the Future; Springer International Publishing: Cham, Switzerland, 2020; pp. 33–51. [Google Scholar]
- Fiani, B.; Siddiqi, I.; Lee, S.C.; Dhillon, L. Telerehabilitation: Development, Application, and Need for Increased Usage in the COVID-19 Era for Patients with Spinal Pathology. Cureus 2020, 12, 9. [Google Scholar] [CrossRef]
- Darekar, A.; McFadyen, B.J.; Lamontagne, A.; Fung, J. Efficacy of Virtual Reality-Based Intervention on Balance and Mobility Disorders Post-Stroke: A Scoping Review. J. Neuroeng. Rehabil. 2015, 12, 46. [Google Scholar] [CrossRef]
- Burton, L.; Rush, K.L.; Smith, M.A.; Davis, S.; Rodriguez Echeverria, P.; Suazo Hidalgo, L.; Görges, M. Empowering Patients Through Virtual Care Delivery: Qualitative Study With Micropractice Clinic Patients and Health Care Providers. JMIR Form. Res. 2022, 6, e32528. [Google Scholar] [CrossRef] [PubMed]
- Naslund, J.A.; Aschbrenner, K.A.; Marsch, L.A.; Bartels, S.J. The Future of Mental Health Care: Peer-to-Peer Support and Social Media. Epidemiol. Psychiatr. Sci. 2016, 25, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Cole, A.C.; Adapa, K.; Khasawneh, A.; Richardson, D.R.; Mazur, L. Codesign Approaches Involving Older Adults in the Development of Electronic Healthcare Tools: A Systematic Review. BMJ Open 2022, 12, e058390. [Google Scholar] [CrossRef]
- Borges do Nascimento, I.J.; Abdulazeem, H.; Vasanthan, L.T.; Martinez, E.Z.; Zucoloto, M.L.; Østengaard, L.; Azzopardi-Muscat, N.; Zapata, T.; Novillo-Ortiz, D. Barriers and Facilitators to Utilizing Digital Health Technologies by Healthcare Professionals. NPJ Digit. Med. 2023, 6, 161. [Google Scholar] [CrossRef] [PubMed]
- Brandenberger, I.A.; Hasu, M.A.; Nerland, M. Integrating Technology with Work Practices in Primary Care: Challenges to Sustainable Organizing “from Within”. Learn. Organ. 2023. [Google Scholar] [CrossRef]
- Mengiste, S.A.; Antypas, K.; Johannessen, M.R.; Klein, J.; Kazemi, G. EHealth Policy Framework in Low and Lower Middle-Income Countries; a PRISMA Systematic Review and Analysis. BMC Health Serv. Res. 2023, 23, 328. [Google Scholar] [CrossRef]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-Implementation Hybrid Designs. Med. Care 2012, 50, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Bashshur, R.L.; Shannon, G.W.; Smith, B.R.; Alverson, D.C.; Antoniotti, N.; Barsan, W.G.; Bashshur, N.; Brown, E.M.; Coye, M.J.; Doarn, C.R.; et al. The Empirical Foundations of Telemedicine Interventions for Chronic Disease Management. Telemed. e-Health 2014, 20, 769–800. [Google Scholar] [CrossRef]
- Rodriguez-Villa, E.; Torous, J. Regulating Digital Health Technologies with Transparency: The Case for Dynamic and Multi-Stakeholder Evaluation. BMC Med. 2019, 17, 226. [Google Scholar] [CrossRef]
- Data, H.; Age, I.; Donaldson, P.M.S.; Lohr, K.N.; Health, R.; Networks, D.; Isbn, M.; Pdf, T.; Press, N.A.; Press, N.A.; et al. Health Data in the Information Age; National Academies Press: Washington, DC, USA, 1994; ISBN 0309538211. [Google Scholar]
- Scheibner, J.; Ienca, M.; Kechagia, S.; Troncoso-Pastoriza, J.R.; Raisaro, J.L.; Hubaux, J.-P.; Fellay, J.; Vayena, E. Data Protection and Ethics Requirements for Multisite Research with Health Data: A Comparative Examination of Legislative Governance Frameworks and the Role of Data Protection Technologies. J. Law Biosci. 2020, 7, lsaa010. [Google Scholar] [CrossRef] [PubMed]
- Chopik, W.J. The Benefits of Social Technology Use Among Older Adults Are Mediated by Reduced Loneliness. Cyberpsychology Behav. Soc. Netw. 2016, 19, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
| Author and Year | Study Design | Title | Participants | Interventions | Results |
|---|---|---|---|---|---|
| Taraldsen et al., 2020 [35] | Randomized Controlled Trial | “Digital Technology to Deliver a Lifestyle-Integrated Exercise Intervention in Young Seniors—The Prevent IT Feasibility Randomized Controlled Trial” | 180 older adults (age 65+) | Evaluate the viability of implementing a Lifestyle-integrated Functional Exercise program and test its efficacy in preventing functional decline in individuals aged 61–70 through the use of digital technology (eLiFE). | Young seniors can safely and effectively participate in a fitness program that incorporates lifestyle changes through the use of information and communication technologies. |
| Zhou et al., 2023 [35] | Cohort Study | “Use of Digital Health Technology Among Older Adults with Cancer in the United States: Findings from a National Longitudinal Cohort Study (2015–2021)” | 1131 older adults (age 60+) | Investigate the patterns and variables linked to the utilization of digital health technologies by cancer patients in their later years. | An increasing number of elderly persons diagnosed with cancer are utilizing digital health technologies, and this trend has been more pronounced during the COVID-19 epidemic. Nonetheless, racial and socioeconomic inequalities persist among cancer survivors in their latter years. Furthermore, there may be some distinct characteristics of digital health technology use among older persons with cancer. |
| Frennert et al., 2021 [42] | Qualitative Analysis | “The concept of welfare technology in Swedish municipal eldercare” | 290 older adults | Talk about how the elderly view welfare technology and what they see as the benefits and drawbacks of using it. | There seems to be an internal struggle among municipal eldercare organizations to bring this goal to fruition, despite the fact that the individuals involved in welfare technology deployment and decision-making are typically rather enthusiastic about it. |
| Bevilacqua et al., 2021 [35] | Quasi experimental design | “eHealth Literacy: From Theory to Clinical Application for Digital Health Improvement. Results from the ACCESS Training Experience” | 58 older | Evaluate the Clinical Application for Digital Health for elderly people | Overall, digital health interventions in geriatric care showed positive outcomes, including reduced hospitalizations and better medication adherence. |
| Perdana et al., 2022 [44] | Cross-Sectional Survey | “Seniors’ adoption of digital devices and virtual event platforms in Singapore during COVID-19” | 144 older adults (age 60+) | Examine the use of technology by the elderly, employing the social exchange theory as a framework. Additionally, you should look into what drives elderly people to use online event platforms. | The perceived advantages are impacted by social factors and the perceived simplicity of use. When it comes to seniors’ plans to use virtual event platforms, these elements are crucial. |
| Cook et al., 2015 [44] | RCT | “A Web-based health promotion program for older workers: randomized controlled trial” | 278 employees aged 50 to 68 | Assess the efficacy of HealthyPast50, an entirely automated web-based health promotion program that targets employees aged 50 and up and is grounded in social cognitive theory. | Older working individuals’ short-term food and exercise habits could benefit greatly from an online health promotion program. According to gender impacts, the majority of the positive effects of the program on exercise have been shown in women. |
| Kim et al., 2019 [44] | Cross-sectional study | “Older adults’ willingness to share their personal and health information when adopting healthcare technology and services” | 170 elderly | investigate the variables affecting the openness of older persons to sharing their personal and health information through healthcare IT and services, particularly wearable tech and relevant services, with an emphasis on the kind of information requested and the organization making the request. | In order to maintain and improve their health, older persons are careful about the entities asked to share different types of personal and health information when using healthcare technologies and relevant services. |
| Boot et al., 2016 [47] | Randomized Controlled Trial | “The Gamification of Cognitive Training: Older Adults’ Perceptions of and Attitudes Toward Digital Game-Based Interventions” | 60 older adults (age 60+) | Investigated the views and feelings of seniors towards game-based interventions following a month of playing digital games (either experimental or control games). | The study’s findings emphasize the significance of game design and user experience in encouraging older adults to engage with digital interventions that aim to enhance their cognitive abilities. Specifically, it found that older adults were more motivated to play enjoyable control games rather than gamified brain training interventions, and they had more positive attitudes towards these games overall. |
| Cajita, et al., 2019 [48] | Descriptive, exploratory study | “Facilitators of and Barriers to mHealth Adoption in Older Adults with Heart Failure” | 10 older adults (age 65+) | Investigate how elderly individuals suffering from heart failure see the utilization of mobile devices and discover any variables that can encourage or discourage the uptake of mHealth. | Technology was one of the obstacles that were found. Despite their worries, older folks are open to using mobile health technologies. |
| Sun et al., 2018 [36] | Cross-sectional Survey | “Internet use and need for digital health technology among the elderly: a cross-sectional survey in China” | 669 older adults (age 60+) | Investigates the present situation of senior Internet use, the elements impacting it (including psychological, social, and physical aspects), and the desire for smart services among the aged. | There has to be a greater push to promote digital health technology and lower Internet access restrictions. To ensure that the elderly can enjoy the advantages of internet technology, society, equipment makers, and family members must collaborate. |
| Tousignant et al., 2010 [37] | Randomized Controlled Trial | “A randomized controlled trial of home telerehabilitation for post-knee arthroplasty” | 48 older adults (age 66+) | Comparing the efficacy of conventional rehabilitation after knee replacement surgery with home telerehabilitation | Home telerehabilitation is just as effective as traditional therapy and could open up more treatment options in places with fast Internet. |
| Gatica-Rojas et al., 2023 [38] | Randomized Controlled Trial | “Telerehabilitation in Low-Resource Settings to Improve Postural Balance in Older Adults: A Non-Inferiority Randomized Controlled Clinical Trial Protocol” | 60 older adults (age 60+) | Validate the viability and efficacy of a rehabilitation plan targeting the enhancement of postural balance in elderly individuals through the utilization of cost-effective virtual reality. Also, it aims to evaluate two ways of delivering low-cost VR: telerehabilitation (TR) in centers for the elderly and face-to-face (FtF) in rehabilitation facilities. | This study will examine the potential of a low-cost virtual reality (VR) rehabilitation program to enhance postural balance in older adults from a city in Chile that has a sizable rural and underprivileged population. The goal is to provide evidence to inform public health policy decisions. |
| Ienca et al., 2021 [19] | qualitative Study | “Digital health interventions for healthy ageing: a qualitative user evaluation and ethical assessment” | 19 older adults | Investigate the perspectives, requirements, and understandings of older persons residing in the community with reference to the utilization of digital health technology for the promotion of healthy aging. | Digital health technologies were generally well-received by participants, who held the belief that these tools may enhance their overall health, particularly when they were created with the patient in mind. Participants also highlighted safety risks and ethical issues connected to privacy, empowerment, and the absence of human interaction as important factors to consider. |
| Chaudhry et al., 2022 [39] | Experimental Study | “Successful Aging for Community-Dwelling Older Adults: An Experimental Study with a Tablet App” | 25 older adults (age 65+) | explore the viability of an eSenior Care tablet app using the Successful Ageing framework | Older persons from low-income backgrounds regarding the viability and potential influence of a mobile health tool on health-related quality of life. This demographic calls for mHealth support tools and follow-up studies to assess their efficacy. |
| Gül Seçkin, et al., 2019 [40] | Experimental Study | “Digital Pathways to Positive Health Perceptions: Does Age Moderate the Relationship Between Medical Satisfaction and Positive Health Perceptions Among Middle-Aged and Older Internet Users?” | 499 aged 40–93. | Find out how medical satisfaction and good health perceptions are impacted by e-trust, e-health literacy, e-health information seeking, and e-health information consumption. | There were two significant predictors: e-trust and e-health consumption. The positive health perception index was significantly predicted by the e-health literacy and e-trust measures in the OLS regression models. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alruwaili, M.M.; Shaban, M.; Elsayed Ramadan, O.M. Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability 2023, 15, 16503. https://doi.org/10.3390/su152316503
Alruwaili MM, Shaban M, Elsayed Ramadan OM. Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability. 2023; 15(23):16503. https://doi.org/10.3390/su152316503
Chicago/Turabian StyleAlruwaili, Majed M., Mostafa Shaban, and Osama Mohamed Elsayed Ramadan. 2023. "Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience" Sustainability 15, no. 23: 16503. https://doi.org/10.3390/su152316503
APA StyleAlruwaili, M. M., Shaban, M., & Elsayed Ramadan, O. M. (2023). Digital Health Interventions for Promoting Healthy Aging: A Systematic Review of Adoption Patterns, Efficacy, and User Experience. Sustainability, 15(23), 16503. https://doi.org/10.3390/su152316503