1. Introduction
Medical technology has advanced dramatically throughout the centuries, but none has been as transformational as digital technology. Networking and computing advancements have not only improved medical decision making but also revolutionized how physicians practice medicine. Today, healthcare organizations have access to massive datasets that have the potential to improve their operations and practices, but deriving valuable insights can be difficult. Cloud computing, blockchain, and AI powered by machine learning provide tools for uncovering patterns in massive datasets while assuring security and manageability. These tools help healthcare professionals improve performance, improve system integration, and manage expenses as they face new problems. Medical technology, with its ability to automate processes and optimize operations, is becoming indispensable for meeting rising expectations, but it is crucial that medical personnel receive training in effective communication techniques, especially in caring for elderly patients [
1,
2,
3].
The definition of “elderly” or “older adults” can vary depending on the context and the purpose for which it is being defined. There is no universally agreed-upon age that categorizes someone as elderly, as it can differ across cultures, healthcare systems, and research studies. The WHO defines “elderly” as individuals aged 65 years and above. This definition is widely used in many countries and for various health-related purposes. Saudi society gives a lot of attention to the elderly. From an organizational and cultural context, the government of the Kingdom of Saudi Arabia (KSA) is concerned with this group. It is possible that older adult carers do not always have simple access to this type of communication’s instructive possibilities. A strong qualification in nursing can facilitate interactions between healthcare professionals and older people, as well as those who provide care for them. Effective communication techniques help older patients and allow medical professionals to provide better patient care. They can assist patients in achieving better health outcomes and provide carers with the confidence that their patients are receiving the finest care available. Nurses provide support and guidance to elderly patients while maintaining professional objectivity and distance. Nurses with experience encourage older patients to engage with challenges on their own by using open-ended questions, the repetition of information, or even just silence. Therapeutic collaboration is proven to be important for healthcare and continues to demonstrate important advantages backed by research [
3,
4,
5].
Effective communication is critical in healthcare, not only between nursing personnel but also when working with colleagues from other disciplines. Furthermore, it is critical in providing patient-centered care, especially in the case of older patients. Nurses who can listen to and thoroughly appreciate the concerns of older patients are more prepared to address emergent challenges, resulting in better patient outcomes. In contrast, poor or non-existent communication in healthcare can lead to elderly people misinterpreting instructions and refusing therapeutic interventions. This breakdown in communication has the potential to interrupt team workflows and potentially result in pharmaceutical errors. According to the Cooperative Commission, inadequate communication during senior patient transfers is responsible for a significant proportion (80 percent) of major medical failures. Hence, the significance of this topic lies in its potential to address these critical issues and improve patient care outcomes through effective communication [
5,
6].
The interaction between nurses and elderly patients is crucial, not only for fostering a strong rapport between the nursing staff and elderly patients but also for improving elderly patients’ understanding of the treatment process and its implementation. Furthermore, efficient communication abilities are critical for health professionals’ practice, as well as their capacity to comprehend their elderly patients’ disease manifestations and their mental and physiological necessities. Elderly-patient-centered interaction allows for the development of therapeutic communication, which also allows healthcare providers to interact with elderly patients regarding their treatments in an intelligent, delicate, and collaborative manner [
5,
6,
7]. Efficient communication in nursing care necessitates a thorough evaluation of each interaction with elderly patients, aiming to grasp their conditions, perspectives, and viewpoints. This encompasses the utilization of both verbal and nonverbal communication skills, as well as proficient listening and the employment of strategies for ensuring that elderly patients fully comprehend the information provided.
Practitioners need to be aware of their nonverbal interactions in different situations so that they can recognize highly risky body language as well as deliberately change it. For instance, seeing a complicated elderly patient, trying to manage an elderly patient’s grievance, or coping with stress can all cause negative nonverbal responses. The use of advanced technologies can also produce nonverbal signals that can infuriate or demotivate elderly patients. Professionals should eliminate habits affiliated with electronic health records (EHRs) that create obstacles to elderly patient participation, like turning one’s back on the elderly patient whilst also typing details, looking at the desktop during sensitive conversations, or struggling to address what is included in the documentation. Describing the EHR and many of its advantages to the elderly patient, trying to set the desktop aside during conversations with the elderly patient, and using a scribe to record diagnostic and therapeutic encounters are some methods that may be useful.
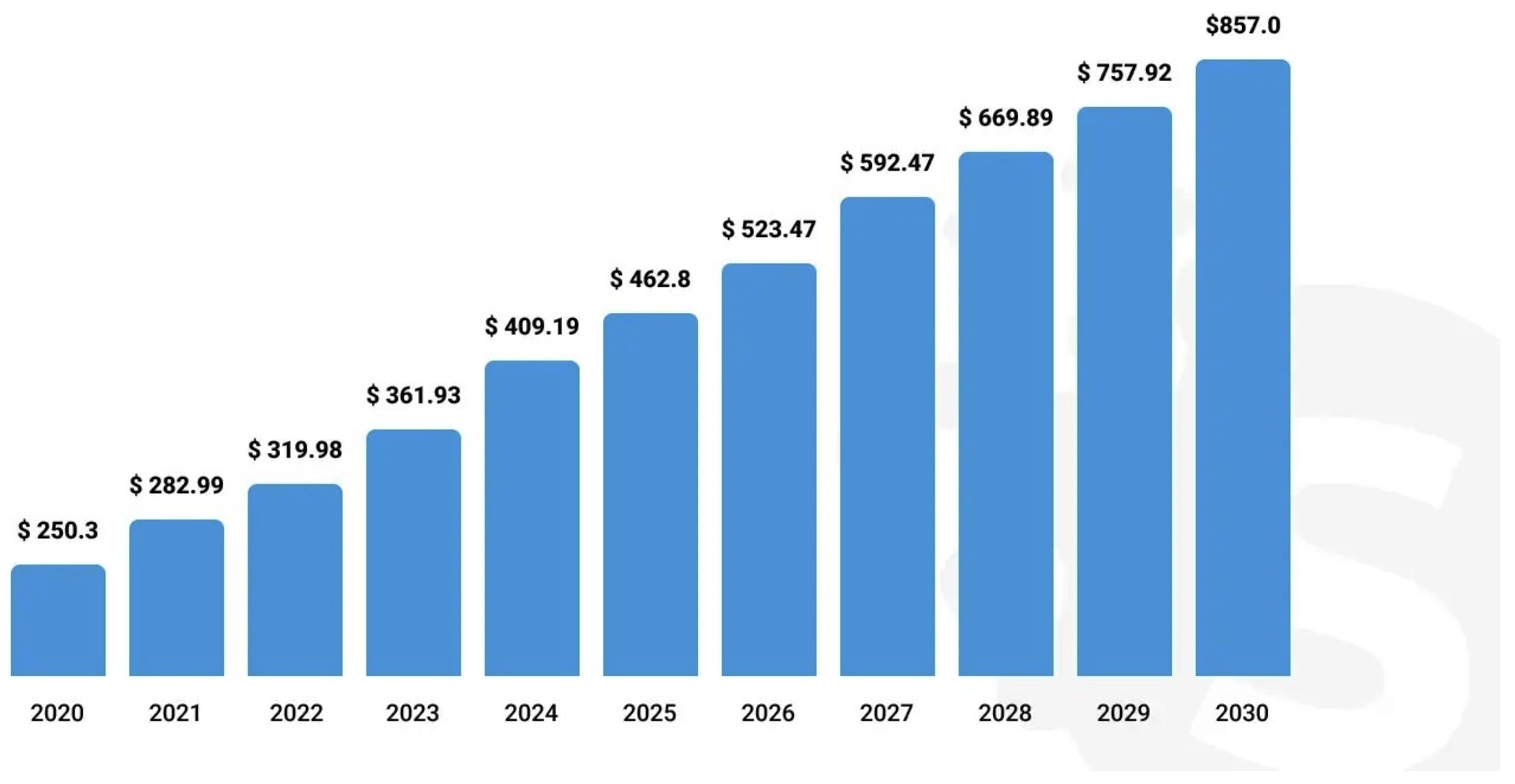
The market for healthcare services worldwide nearly reached USD 7.5 trillion in 2022 and is expected to keep expanding, topping USD 9 trillion in 2026. In addition, the healthcare IT market is expanding significantly. It reached USD 320 billion in 2022, surpassing Precedence Research, and is anticipated to reach USD 857.6 billion by 2030. The need for remote monitoring, cooperation among healthcare facilities, and readily available and safe care is expanding, according to a new Deloitte analysis. Thus, in order to meet this need and have the intended influence on patient care, healthcare experts look for new medical technology [
8].
Figure 1 shows the healthcare IT market size from 2020 to 2030 in USD Billion.
In the realm of mental nursing care for elderly patients, the use of advanced healthcare technologies and therapeutic communication techniques has revolutionized the quality of care provided. Advanced healthcare technologies, such as telemedicine platforms and wearable devices, have greatly improved accessibility and convenience for elderly patients in need of mental health support. Telemedicine enables remote consultations, allowing elderly patients to receive timely care from the comfort of their homes. Moreover, wearable devices, such as smartwatches, can monitor vital signs and track activity levels, providing healthcare professionals with valuable insights into patients’ well-being. These technologies not only enhance the efficiency of care but also promote patient autonomy and independence.
In conjunction with advanced technologies, therapeutic communication plays a vital role in mental nursing care for elderly patients. The elderly population often faces unique challenges, such as loneliness, isolation, and cognitive decline, which can significantly impact their mental health. Therapeutic communication involves establishing a rapport with patients, actively listening to their concerns, and providing empathetic support. It creates a safe and trusting environment where elderly patients feel comfortable expressing their emotions and fears. Effective communication empowers healthcare professionals to tailor treatment plans to the individual needs of elderly patients, ensuring that their mental health is addressed holistically [
9,
10,
11]. The integration of advanced healthcare technologies and therapeutic communication in mental nursing care for elderly patients signifies a transformative approach that prioritizes individualized care, accessibility, and overall well-being. By harnessing the power of technology and compassionate communication, healthcare professionals can deliver comprehensive mental health support to the elderly population, improving their quality of life and promoting mental well-being. Nonverbal communication accounts for two-thirds of all communication systems, according to some researchers [
8,
9]. Nonverbal communication can convey information both vocally and through the use of appropriate body cues or expressions. Body signals include physical characteristics, conscious as well as unconscious expressions and signals, and personal space intervention. If the facial expression communicated does not complement the verbal message, a false impression can be developed. Nonverbal communication improves first perceptions in everyday situations, such as encouraging a person or in a business question-and-answer session: perceptions are formed within the first four seconds of interaction in ordinary circumstances. The KSA is experiencing a fundamental national evolution, designated as Saudi Vision 2030. The purpose is to minimize economic reliance on the oil industry as well as on foreign labor, as well as to modernize and professionalize public institutions and to resurrect private sector investment. This corresponds to a system-wide transition in the medical sector, encompassing corporate takeovers, the growth of the medical system, and efficiency improvements, with a concentration on value-based health coverage. The initiatives are a response to rising requirements for the Saudi healthcare system as a result of a rapidly aging population, as well as rising preconceptions of enhanced health coverage for all citizens [
9,
10].
The objective of this research article is to investigate the practice of therapeutic communication between nurses and senior patients, with a specific emphasis on mental healthcare. While the significance of effective communication in nursing is widely acknowledged, a systematic approach to strengthening therapeutic communication is required. This study aims to fill that need by presenting an innovative way of evaluating and improving therapeutic communication via fuzzy-based multi-criteria decision making (MCDM). According to current research, studies emphasize the importance of therapeutic communication, which includes empathy, trust-building, and accurate information exchange. However, research on the specific challenges of nurse–elderly patient communication, particularly in mental health contexts, is lacking. In the unique context of Saudi Arabia, this study tackled the challenges posed by linguistic, cultural, and religious differences in nurse–elderly patient interactions. The assessment framework includes seven criteria, namely, Verbal Communication, Nonverbal Communication, Patient Satisfaction, Trust and Rapport, Understanding and Clarity, Emotional Support, and Cultural Sensitivity, designed to measure the effectiveness of therapeutic communication methods. Six therapeutic communication approaches for mental health nurses, namely, Traditional Communication Training, Simulation-Based Training, Technology-Assisted Communication, Interdisciplinary Training, Communication Assessment Tools, and Feedback and Coaching, were evaluated based on these criteria. However, an investigation was performed on the special intricacies of nurse–elderly patient communication, especially in mental health situations. In the particular setting of Saudi Arabia, this study addresses the complex difficulties brought on by linguistic, cultural, and religious distinctions in nurse–elderly patient contact [
8,
9,
10].
This study also acknowledges the significance of creative solutions in removing obstacles to effective communication. An organized and methodical way to evaluate various interventions targeted at improving therapeutic communication is introduced through the implementation of a fuzzy-based MCDM approach. By utilizing this strategy, this research aids in the redesign of interventions that address the psychological and physiological requirements of elderly patients, as well as the reform of nursing practice. Given the changing nature of medical services and the growing significance of patient-centered care, this research is especially pertinent at this time. This research not only determines a promising path but also offers practical advice for healthcare institutions to improve the education and professional growth of their nursing staff by assessing and ranking different therapeutic communication approaches as a potential remedy for enhancing communication during therapy [
11,
12,
13].
The remainder of this article is organized as follows: The next section,
Section 2, explores some of the associated papers published, comprising a synopsis of research studies on therapeutic communication among mental health nurses.
Section 3 describes the therapeutic communication measurement approach that was developed to prioritize different mental health nurses.
Section 4 presents the investigation’s outcomes of the research. This investigation is deliberated in
Section 5. To conclude,
Section 6 discusses the conclusion, as well as suggestions for future research in this domain of research.
2. Literature Review
The literature review section of this paper explores existing research and studies related to therapeutic communication in mental nursing care for elderly patients in Saudi Arabia. This section aims to critically analyze and synthesize the available literature to identify the gaps and opportunities for improving therapeutic communication in this specific context. By utilizing a fuzzy-based MCDM approach, this paper seeks to provide valuable insights and recommendations to enhance the quality of care provided to elderly patients with mental health conditions in Saudi Arabia. Through an in-depth exploration of the relevant literature, this section lays the foundation for understanding the current state of therapeutic communication practices and highlights the significance of implementing a fuzzy-based MCDM approach to address the unique needs and challenges faced by elderly patients in mental nursing care.
Alshammari et al. [
11] conducted an evaluation study to recognize and synthesize statistical and observational substantiation of existing nurse–elderly patient interaction practice in Saudi Arabia, as well as its impact on the performance of care, security, and the satisfaction of support customers.
In a study conducted by Martin and Chanda [
12], a psychiatric simulation was introduced to encourage student nurses to apply therapeutic communication techniques when assisting elderly patients with mental illnesses in a healthcare environment. They employed a quasi-experimental approach with a one-group pre–post-test design as part of the mental health clinical orientation for students. Data analysis was carried out using dependent t-tests. Their findings underscore the need for further research and suggest the integration of a therapeutic communication psychiatric screening into the education of undergraduate nursing students before they embark on their medical training. This addition can better prepare students for effectively engaging with elderly patients suffering from mental illnesses, emphasizing the importance of strong communication skills in the nursing profession.
Arthur et al. [
13] presented a subjective study aimed at recognizing therapeutic communication techniques utilized by psychiatric nurses in Hong Kong with Chinese clients. Three case analysis vignettes with Chinese cultural attributes were created to obtain in-depth information regarding the therapeutic communication techniques used by survey participants. Ten admittance hospital nurses as well as ten public nurses from two different psychiatric facilities made up the purposive sample with a sample size of twenty. Everyone in the study had at least five years of post-registration expertise. For the nursing staff’s responses to the vignettes, information analysis showed communication classifications as well as theme groupings. The findings revealed that a distinct cultural influence appeared in communication trends.
Hammer et al. [
14] characterized an innovative teaching prototype that used simulation to instruct therapeutic communication techniques to pre-licensure student nurses. This innovative, philosophically centered teaching and learning approach is a repeatable framework that incorporates student as well as faculty preparation; pre- and post-assignments; techniques for the effective involvement of students as key actors or investigators using therapeutic communication technologies, as well as critical analysis regarding the therapeutic communication concept; techniques for self-assessment as well as peer assessment; and possibilities for inter-professional interaction for professional development. The prototype also worked as an alternative environment to the treatment center. A relatively short review of the literature offered a theoretical as well as a socioeconomic conceptual model.
Joung and Park [
15] described a study that included in-depth personal interviews that were recorded as well as translated as they transpired, and the data were analyzed by employing the content analysis method. The findings of their study suggested that therapeutic communication initiatives for mental health nurses should be developed and implemented. Guidance is needed to enhance therapeutic communication between many mental health nurses, and institutional assistance is required.
Rnning and Brkly [
16] conducted an evaluation study to look for research results from both subjective and quantification investigations. Ovid (MEDLINE, PsycInfo), Cochrane, ScienceDirect, Cinahl, SweMed, Norart, Google Scholar, and ProQuest were used to obtain comprehensive literature search results. According to their study, role playing in monitored groups appeared to promote reflection as well as perspective not only for trainees acting the part of elderly patients as well as therapists but also for a peer group monitoring the group meetings. Clinical role playing, according to the included research, promotes helper–user fairness, as well as increases students’ active participation, self-efficacy, and empathic skills in psychiatric care.
According to Rosenberg and Gallo-Silver [
17], the nurse practitioner should be guided through a procedure of coordinating with elderly patients that includes role playing, intellectual strategies, and particular didactic details on how to perceive elderly patient obstacles to care. During their two-year clinical placements, attempting to teach therapeutic relationships with the help of this prototype may help students react to distressed elderly patients, depersonalize negative messages, and form goal-driven associations.
According to Webster [
18], there has been little investigation into the efficacy of standardized elderly patient experiences (SPEs) in teaching therapeutic communication abilities to undergrad psychiatric nurse practitioners. The efficiency of using SPEs to instruct therapeutic communication techniques in psychiatric nursing was investigated using a quasi-experimental, one-group, pre–post-evaluation strategy. Eighty-nine senior medical students enrolled in a mental health clinical nursing curriculum in an undergraduate nursing program took part in the study.
Canales [
19] investigated the influence of an ethnic presence on the nurse–patient interaction through the eyes of Chicanas, females of Mexican origin. However, the concerns raised for Chicanas are relevant to associates of several additional traditional communities, participants whose individuality is frequently crafted from typecasts as well as mythologies that their presence inspires. Ethnic-minority women frequently feel a sense of a double risk as a result of existing in a society that debases both women and representatives of particular races and ethnicities. Nursing, counseling psychology, and sociology studies provided the foundation for an investigation of the psychological effects of this double bind. As a therapeutic method of interaction, storytelling interaction, or the distribution of information through stories, was indeed provided.
Levy-Storms [
20] presented a comprehensive review to challenge current exploratory studies and also to suggest recommendations for future research initiatives on nursing assistants’ therapeutic relationships with older individuals in organizational long-term care configurations who have impaired cognitive and/or mental illnesses. The research results of the studies included in this assessment demonstrated that the respective therapeutic communication methods can be learned and benefit employees as well as older adults’ standard of living: open-ended questionnaires, positive declarations, eye contact, efficacious touch, and smiling.
After conducting an extensive examination of the existing literature, it is clear that there is a significant demand for assessing the various therapeutic communication methods utilized by nurses in their dealings with elderly patients. This requirement arises from the recognition of the essential role that proficient communication plays in achieving the best possible healthcare results and elevating the contentment of geriatric patients. The complexity of therapeutic communication in this context is influenced by various factors, including age-related cognitive changes, diverse health conditions, and varying cultural backgrounds. Because of its capacity to cope with the inherent subjectivity as well as uncertainty frequently associated with assessing qualitative factors like communication, fuzzy TOPSIS (Technique for Order of Preference by Similarity to Ideal Solution) stands out as an ideal method for assessing several therapeutic communication strategies. Fuzzy TOPSIS excels in capturing variations by allowing for levels of preference and imprecision in decision making, resulting in a more realistic and robust evaluation framework. Furthermore, it allows for the incorporation of expert opinions and varied perspectives, making it a versatile instrument for a thorough evaluation of therapeutic communication strategies in healthcare. Consequently, this research endeavored to address this need by undertaking a systematic evaluation of different therapeutic communication approaches to ascertain their efficacy in enhancing patient outcomes and satisfaction. Specifically, this evaluation entailed a comparative analysis of various training methods to identify the most advantageous approaches for nurses engaged in mental nursing care for elderly patients.
3. Materials and Methods
The main objective of this study is to appraise and analyze the effectiveness of different therapeutic communication methods employed by mental health nurses when caring for elderly patients in Saudi Arabia. The study seeks to provide suggestions for how to improve the quality of nurse–patient interactions in the setting of mental nursing care for the elderly by measuring and comparing different strategies. Finally, the research aims to enhance healthcare practices and the general well-being of older patients in Saudi Arabia by finding and promoting the most efficient therapeutic approaches. The evaluation process throughout this investigation was carried out by a group of 100 senior healthcare professionals as experts with expertise in mental health nursing and therapeutic communication. Their role in the study was to evaluate the performance of mental health nurses in therapeutic communication scenarios involving elderly patients. This study employed measures such as training sessions, guidelines, and calibration exercises to ensure that the experts’ evaluations were consistent and reliable. Questionnaires were used by these experts to record individual responses from the “nurse”.
Instructors can provide opportunities for mental health nurses to engage with critical cases in the research lab. Numerous attentional records with gestures as well as words can be provided to the “mental elderly patient”, enabling gestures for circumstances such as an elderly patient yelling at the nurses. A further issue for practitioners is retracted and noncommunicative elderly patients. The experts could perceive whether the nurse exhibited behaviors as well as verbal exchanges focused on developing a professional relationship and incorporating total care. The experts could use a questionnaire to record individual responses from the “nurse”. Preparation could be classified as “met” or “not met”; examples include the following: welcomes the patient, demonstrates understanding, offers reassurance, orients the elderly patient to the environment, increases the elderly patient’s feeling of control, reacts to the elderly patient’s signals, and initiates the nurse–elderly patient relationship. Cue cards may necessitate the elderly patient to make demanding declarations and behaviors. The nurses must illustrate the capacity to remain calm and focused while assisting the client in participating in the treatment plan. If the experience is recorded, an analyst can assess it. Only 95 credible responses were recorded for the measurement of therapeutic communication among mental health nurses. Following the expert interviews, statistical analyses were performed on the collected data, and the expert viewpoints were aggregated.
This study did not include any ethical considerations because it was primarily concerned with evaluating and improving therapeutic communication approaches used by nurses with elderly patients. The study did not include any human subjects, patient data, or interventions that would create ethical concerns in research, such as informed permission or privacy concerns. As a result, in this setting, the study processes did not include ethical issues.
3.1. Hierarchy for Measurements
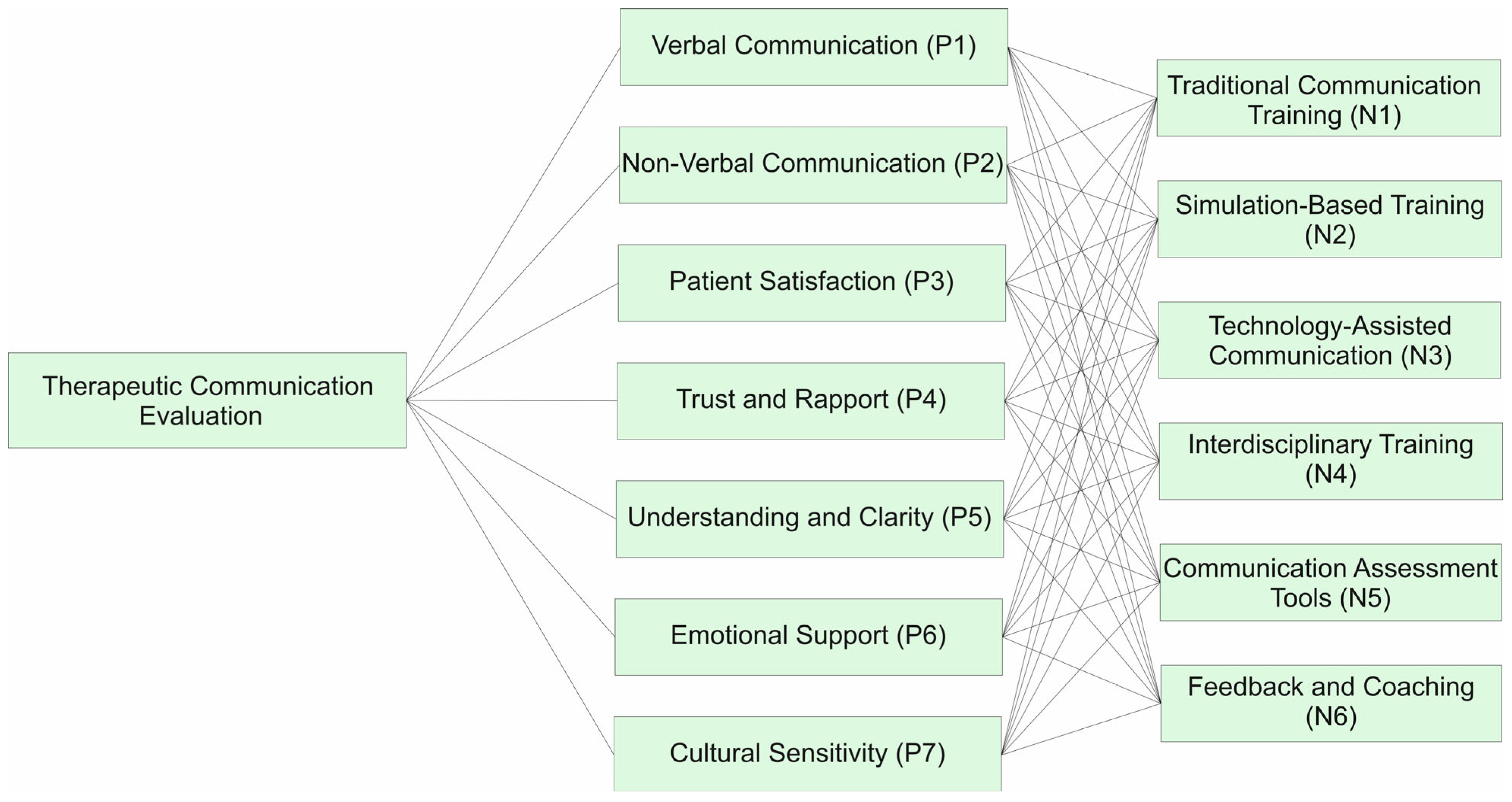
The nurse must be able to remain calm and focused while trying to aid the elderly patient in becoming a member of the therapeutic process. If the expertise is documented, an analyst can evaluate it. The assessment’s structural representation is composed of seven criterion categories [
17]: Verbal Communication, Nonverbal Communication, Patient Satisfaction, Trust and Rapport, Understanding and Clarity, Emotional Support, and Cultural Sensitivity, designated by P1, P2, P3, P4, P5, P6, and P7; these allow one to choose the most effective method of therapeutic communication among different alternatives. The six methods of therapeutic communication for mental health nurses as alternatives evaluated are Traditional Communication Training, Simulation-Based Training, Technology-Assisted Communication, Interdisciplinary Training, Communication Assessment Tools, and Feedback and Coaching, indicated by N1, N2, N3, N4, N5, and N6, respectively.
Table 1 lists the several criteria utilized for measuring the therapeutic communication of mental health nurses. Further,
Table 2 shows different methods of therapeutic communication for mental health nurses.
Figure 2 illustrates the hierarchical arrangement for measuring the therapeutic communication of mental health nurses.
After establishing the hierarchical system, the variables must be investigated in pairs to determine their relevancy as well as weights in accordance with the overall objective. The research was premeditated and observed in order to correlate the multiple parameters that observers as well as top-level specialists take into account when measuring therapeutic communication. A survey-based questionnaire was undertaken to determine the relevance of the characteristics that must be taken into consideration when measuring the therapeutic communication of mental health nurses.
3.2. Fuzzy-TOPSIS Method
TOPSIS is a widely recognized approach within the field of MCDM. It serves as a valuable and practical tool for assessing and choosing the most suitable options by considering calculated coefficients. In essence, TOPSIS provides a structured way to evaluate and rank alternatives based on multiple criteria, enabling a more informed decision-making process. Hwang and Yoon [
21] devised the TOPSIS technique, which is based on the premise that the preferable course of action should closely approximate the positive ideal solution (PIS). The PIS approach provides the highest competitive advantage across multiple criteria while minimizing cost issues. At the same time, it aims to maximize benefit criteria while significantly lowering profit-related concerns.
The allocation of quality weights among different MCDM techniques signifies the differing importance of elements within the decision-making process. It is recognized that not all assessment criteria hold equal weight, as the evaluation process encompasses a range of perspectives and interpretations [
22]. This acknowledgment underscores the need for a systematic approach that considers the varying significance of each criterion in the decision-making context. Weighting methods are typically classified into two categories: subjective and objective techniques. Subjective approaches rely on decision makers’ preferences and judgments to assign weights to criteria. In contrast, objective methods utilize computational strategies like the eigenvector approach, weighted least squares, and mathematical programming principles to calculate the overall assessments made by each decision maker. This categorization distinguishes between methods that incorporate personal judgments and those that employ more mathematical and computational processes to determine criteria weights. The likelihood tactic, multiple-objective logic, and other objective procedures compute weights by comprehensively running statistical equations without reference to the decision maker’s preferences. Two very different subjective and objective weighting strategies are used in the comparison to exemplify that the weighting methods have an impact on the observation sequence. Subjective weighting is controlled by a centralized decision maker’s perception, whereas objective weighting is derived from analytical estimates. Whenever appropriate subjective weights are unavailable, the quantitative weighting approach comes in handy [
23,
24,
25,
26,
27,
28,
29,
30].
In accordance with
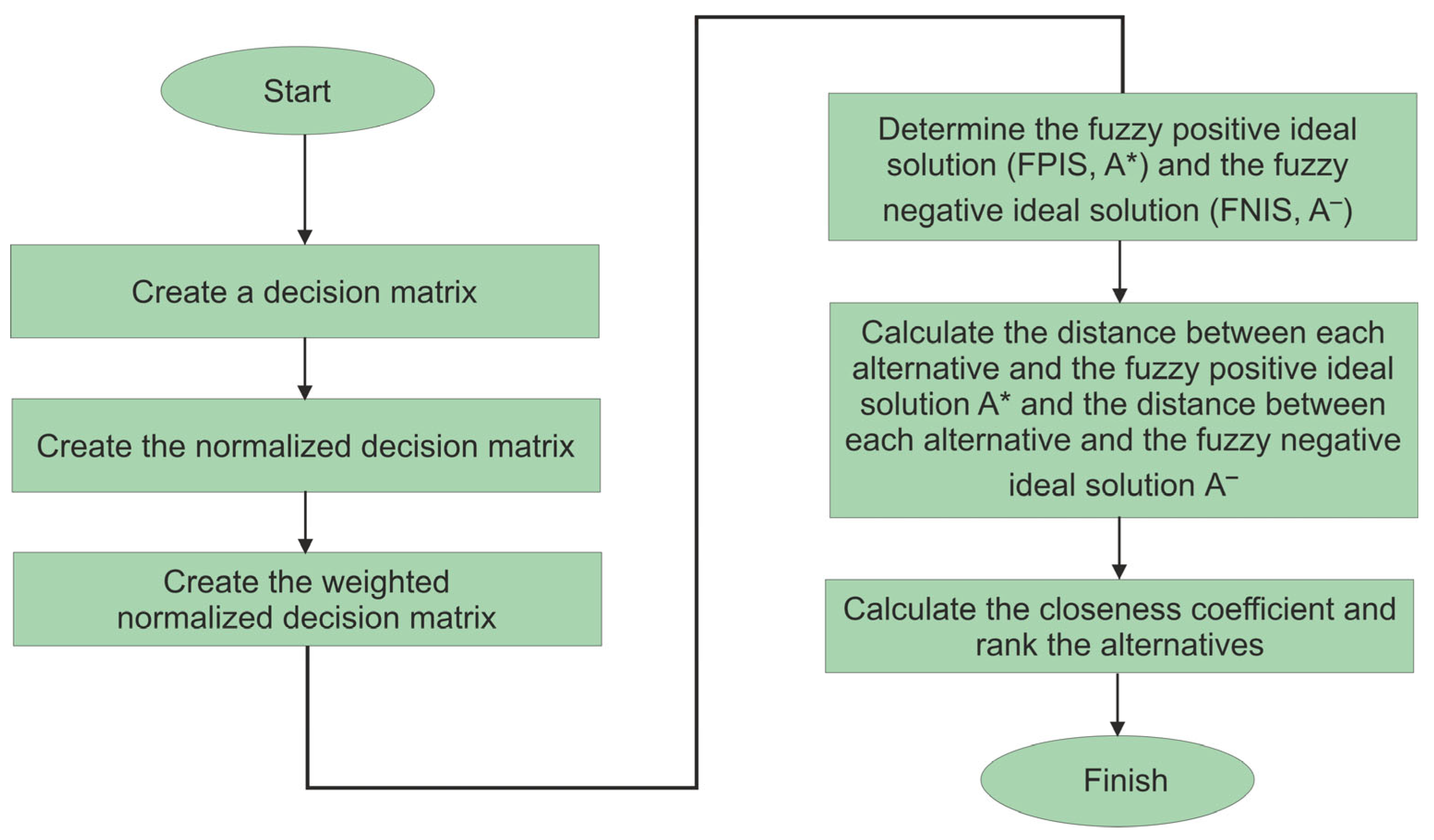
Figure 3, the step-by-step strategic approach for weighting estimation and relevance rating with fuzzy TOPSIS support is as follows.
Step 1: Construct an assessment matrix.
The fuzzy TOPSIS approach was used in this study to examine seven separate criteria and six alternative options. These criteria include a variety of parameters with varying features. Considering the decision-making set, this may include various memberships or categories, denoted by K. This method enables a thorough evaluation of possibilities in a multifaceted decision-making setting. The fuzzy ranking and priority weight of the
kth analysis expert for the
ith potential substitute on the
jth criterion are as follows:
In this context,
= 1, 2, …,
and
= 1, 2, …,
, where “
i” represents a range from 1 to “
m”, and “
j” ranges from 1 to “
n”; the combined fuzzy scores, denoted by
, are determined for each option “
i” concerning each specific criterion “
j”. These fuzzy scores are represented by
= (
).
Table 3 provides an overview of the criterion categories and the corresponding weights assigned to each criterion. This information is crucial for the comprehensive evaluation of the options, considering the significance of different criteria in the decision-making process.
The abbreviation TFN stands for triangular fuzzy number, represented as (L, M, U). Within this configuration, the parameters L, M, and U correspond to the lowest, median, and highest levels of effectiveness, respectively. A representation of the fuzzy measurement instrument used in this approach can be found in
Table 4. This table illustrates the values associated with these parameters, serving as a key reference in the methodology.
Step 2: Consider making standardized choice matrices.
To standardize the choice matrix, the given relationship is applied to both the positive and negative ideal options. Standardization is a critical step in the evaluation process, as it allows for a fair and consistent comparison of alternatives against these ideal solutions. By implementing this transformation to both positive and negative benchmarks, the study ensures that each alternative’s performance is assessed on a level playing field concerning these reference points.
Step 3: Construct an importance weight decision model.
The weighted standardized decision matrix is constructed by multiplying each criterion’s weight within the standardized fuzzy choice challenge by an expression that considers the varying importance of each characteristic. This calculation is a pivotal component of the assessment process, ensuring that criteria with differing significance are appropriately incorporated into the evaluation of alternatives. By accounting for the dynamic relevance of these characteristics, this method offers a more accurate representation of each alternative’s performance in relation to the weighted criteria. This means that the weight of each criterion is assigned to the standardized data, permitting an extensive assessment of the decision options while taking into account the importance of different qualities in the decision-making process.
where
denotes the weight of criterion
.
Step 4: Determine the fuzzy positive ideal solution (FPIS, A*) as well as the fuzzy negative ideal solution ().
Employing Equations (4) and (5), the FPIS and FNIS for the alternatives can be clearly determined. The FPIS in these equations indicates the most favorable combination of criterion values that the alternatives strive to accomplish, whilst the FNIS indicates the least acceptable values for each criterion. These approaches are useful for analyzing and ranking alternatives during the decision-making process.
where
is the greatest quantity of i for all possibilities, and
is the smallest value of I for all choices. B and C represent the positive and negative optimized solutions, respectively.
Step 5: Compute the gaps between each interim solution and the fuzzy positive ideal solution (A*), as well as the gaps between each option and the fuzzy negative ideal solution (A−).
Equations (6) and (7) are used to calculate the distance from each alternative to the FPIS and the distance from each alternative to the FNIS. These computations are critical for determining how far each alternative is from the best-case scenario (FPIS) as well as how near or far it is from the worst-case scenario (FNIS). These data assist in ranking and analyzing alternatives during the decision-making process.
The “d” parameter denotes the distance between two fuzzy numbers. When we take into account two triangular fuzzy numbers, represented by (
) and (
), we can determine the distance “e” between them using the equation described in (8). This equation aids in measuring the difference or separation between two fuzzy numbers, which is important for examining and comparing the qualities or significance of these figures in the overall setting of the study.
Keep in mind that and are crisp figures.
Step 6: Calculate the closeness coefficient precisely and arrange the possibilities. The procedure that follows can be used to calculate the closeness coefficient for each viable solution. The closeness coefficient is a measure that indicates how closely each solution corresponds to the ideal answer in regard to the set criteria. This computation aids in rating the alternatives and determining which ones are most appropriate for the particular decision-making environment.
There are a number of solutions for measuring and ranking alternatives using a distinct group of standards. Each strategy has advantages and disadvantages over the others. The fuzzy TOPSIS method has the advantage of being mathematically modest, easy to use to verify human objectives, and enabling clearly defined tradeoffs among various objectives [
31,
32]. Furthermore, this technique is classified as an identifying concept, functioning on the premise that, while an optimized situation is not always accessible, an alternative that incorporates optimized values throughout all criteria is feasible. As a result, in the framework of this research paper, the fuzzy TOPSIS approach is used to analyze the efficiency of therapeutic communication by mental health nurses using trapezoidal membership importance. This approach provides for the selection of the best possible alternative while taking into account all aspects of assessment in instances when obtaining perfection on all criteria may be challenging.
5. Discussion
Healthcare services in the KSA have substantially increased over the last few years, but this has also introduced obstacles for stakeholders trying to emphasize the demand to strengthen the quality of healthcare. Such obstacles include increased requirements for healthcare service providers, increasing prices, changing patterns of disease, insufficient resources, the absence of a national healthcare information system, the absence of indigenous medical providers, a substantial increase in the pilgrim population, an increase in the occurrence of medication mistakes, and long wait times. As a result, the Saudi Ministry of Health (MOH) has increased its efforts to strengthen the performance of mental health support service providers in Saudi Arabia, primarily through the development of health programs and strategies. Depending on their therapeutic communication abilities, this study assessed the therapeutic communication of mental health nurses.
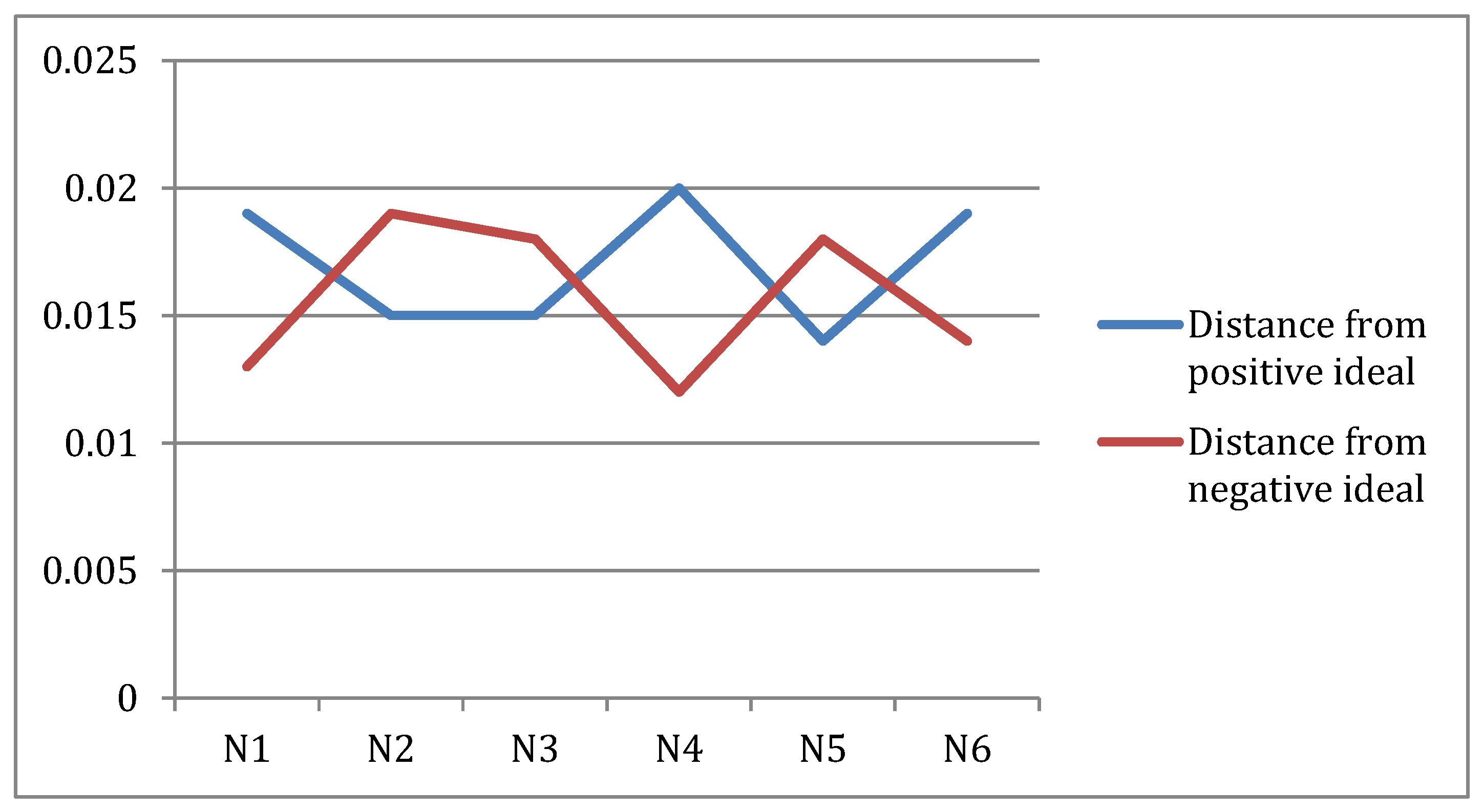
Simulation-Based Training is ranked at the top, indicating its superiority in improving therapeutic communication skills between nurses and elderly patients. Simulation-Based Training is an effective approach for nurses to practice and enhance their skills in therapeutic communication [
33,
34,
35]. This training method provides a simulated environment where nurses can engage in realistic scenarios and interactions with elderly patients. Through role playing and simulated patient encounters, nurses can develop their communication techniques, active listening skills, empathy, and rapport-building abilities. The simulated scenarios allow nurses to experience different challenging situations and practice appropriate responses, enabling them to build confidence and competence in their communication with elderly patients. By incorporating feedback and debriefing sessions into Simulation-Based Training, nurses can reflect on their performance, identify areas for improvement, and refine their communication strategies. This hands-on approach not only enhances the practical skills of nurses but also cultivates their ability to adapt to varying patient needs and establish trust and understanding. However, it is important to note that this ranking is specific to the findings of this research and may not apply universally. Different studies or contexts may yield different rankings or results. To reduce misconceptions as well as improve communication between nurses and elderly patients, foreign mental health nurses must be compelled to undergo Arabic classes. Another option would be to hire more Arabic-speaking nursing staff in mental health facilities. Furthermore, the emergence of therapeutic relationships for nursing staff within the KSA’s psychological health framework is urgently needed. Collaboration guidance may be enough to achieve competent nursing services. Also, there is an urgent demand for good communication about anticipated decisions in relation to therapeutic interventions between mentally ill elderly patients and nursing staff; this is a critical component of rehabilitation [
36,
37,
38,
39,
40,
41,
42].
The findings of this study have major implications for the future in the setting of Saudi Arabia’s growing healthcare sector. As the country places a greater emphasis on the well-being of its elderly, the necessity for good therapeutic communication becomes even more critical. Taking the results of this study into account can help make healthcare treatments better suited to the specific needs of Saudi Arabia. Saudi Arabia may increase not just the quality of care but also patient happiness by encouraging improved therapeutic communication between nurses and senior patients, thereby contributing to the long-term development of its healthcare system. This study identifies the most effective approach for enhancing therapeutic communication in the context of mental health nursing care for elderly patients in Saudi Arabia.