Abstract
This study aimed to evaluate the impact of the COVID-19 pandemic on routine immunization (RI) programs in six northern Nigerian states: Bauchi, Borno, Kaduna, Kano, Sokoto, and Yobe. This was a cross-sectional analytical study that compared programmatic data from 2019 and 2020, as well as survey data collected during the pandemic. RI program variables included service delivery, leadership and governance, monitoring and evaluation/supportive supervision, community engagement, vaccine supply chains, and health finance and management. Data were analyzed using SPSS (version 23, IBM), Student’s t-test, and structural equation modeling. The results showed that RI programs were affected by the pandemic in terms of reduced meetings and low completion rates for action points in certain states. However, routine immunization support services increased owing to improved monitoring techniques and consistent vaccine deliveries, with fewer reports of stockouts. The most significant impact of the pandemic was observed on activities coordinated at the healthcare facility level, whereas those at the state level were less impacted. The major challenges encountered during the pandemic included insufficient supplies and consumables, movement restrictions, shortages of human resources, and fear of infection. In building a more resilient health system, governments and non-state actors will need to invest in strengthening delivery mechanisms at the core implementation level with a focus on facilities and communities.
1. Introduction
1.1. Background
The SARS-CoV-2 virus (COVID-19), which was first detected in Wuhan, China, in January 2020 [1,2,3], spread around the world, including to Nigeria, which recorded its first case on 27 February 2020 [4].
According to the Nigerian Centers for Disease Control (NCDC), as of 24 April 2022, Nigeria had 2653 active cases of COVID-19 and 3143 fatalities [5]. However, there is evidence of a gradual decline in the outbreak owing to the response from the Nigerian healthcare system. The COVID-19 program in Nigeria was developed using various measures, such as a robust response framework, emergency operation centers (EOCs), and increased vaccination [6]. These steps, along with other active precautionary measures (such as non-pharmacological interventions), were instrumental in attaining epidemiological control [1,7,8].
However, in the early phases of the pandemic, most governments, including Nigeria’s, instituted standard epidemic control measures: travel restrictions, lockdowns, workplace hazard controls, closure of public spaces and facilities, and strict hygiene practices [9]. Although these measures helped limit the spread of the infection, they also interrupted implementation of crucial primary healthcare (PHC) programs, further exacerbating the prevailing healthcare system weaknesses and community distrust [10]. The following factors jointly culminated in far-reaching effects on the overall PHC landscape in Nigeria [11].
The routine immunization (RI) programs consist of various activities defined broadly by theme. These include service delivery (SD), leadership and governance (L&G), monitoring and evaluation/supportive supervision (M&E/SS), community engagement (CE), the vaccine supply chain (VSC), and health financing and management (HFM). These themes are crucial for maintaining the ongoing effectiveness of immunization campaigns [12,13,14,15,16,17,18,19].
Providing vaccinations and improving coverage are the fundamental concepts of service delivery (SD) in routine immunization (RI) programs [12,20]. A COVID-19 study conducted in 170 countries and territories found that disrupted RI sessions occurred in 17 out of 30 World Health Organization (WHO) member states in Africa (of which there are 47 in total). There was a partial suspension of fixed post-immunization services in 2 countries and partial or complete suspension of outreach services in 17 countries [21]. The inability to conduct immunization practices during the COVID-19 pandemic was the greatest threat to the gains regarding vaccine-preventable diseases [21,22,23,24]. According to the GAVI, WHO, and UNICEF, at least 80 million children are at risk of diphtheria, measles, and polio because of the disruption in routine vaccination efforts caused by the COVID-19 pandemic [24,25].
Leadership and governance (L&G) remain pivotal to the success of RI programs [13]. Studies have shown that, since the COVID-19 pandemic, government discussions on RI activities have decreased [26,27]. The weak healthcare systems in developing nations made other healthcare intervention programs vulnerable, as most governments’ attention shifted toward curtailing the direct health and economic impacts of COVID-19 [14].
Monitoring and evaluation (M&E)/supportive supervision (SS) have remained an integral aspect of immunization programs [15,28,29]. A study on the impact of COVID-19 on integrated SS in 19 countries in East and South Africa showed that 13 countries experienced different levels of decline in integrated SS visits in 2020 compared to 2019. Ten of the thirteen countries had decreases of over 59%, and there were significant reductions in integrated SS in eleven countries [15]. Studies have reported a significant association between increased SS and improved immunization coverage [28,29,30]. The complexities and uncertainties associated with the COVID-19 pandemic significantly affected the concepts and methodologies of M&E practices [31]. The difficulty in the healthcare system of switching from a manual M&E approach to the use of e-tools was a significant factor in determining vaccine coverage during the pandemic [32].
The COVID-19 pandemic caused a massive disruption in global supply chains, which significantly affected the supply of essential drugs and commodities [16]. The pandemic caused temporary and prolonged closure of healthcare facilities, which led to disruptions in healthcare commodities and other supplies, as well as the vaccine supply chain (VSC) [17,33]. According to Shet et al. [21], there was a 33% global reduction in the administration of the third dose of the diphtheria, pertussis, and tetanus (DPT) vaccine, with reductions ranging from 57% in Southeast Asia to 9% in the WHO African regions.
UNICEF has acknowledged the possibility that local COVID-19 response measures could have temporarily interrupted RI services, community engagement (CE), and demand generation [18]. At one point, to reduce the worsening community transmission of COVID-19, the WHO recommended the suspension of mass vaccination campaigns [34,35]. The International Federation of Red Cross and Red Crescent Societies (IFRC), UNICEF, and the WHO recognize that risk communication and enlightenment during a pandemic are important in enhancing continued CE and RI demand generation [36]. A recent publication on the impact of COVID-19 on immunization programs in Kaduna state, Nigeria, noted that risk communication, enlightenment, and trust were important factors that affected RI programs [37].
The sudden onset of the pandemic disrupted the manual approach to health financing and management (HFM), which caused a transition to digital approaches [38]. At a medical conference in Nigeria, it was reported that the national allocation for RI grew from NGN 17 billion to 139 billion between 2018 and 2021 [19]. However, it may not be possible to state that such increments occurred at the state and local government levels [19,39]. There is a paucity of information regarding the utilization and management of funds at different implementation levels.
1.2. Study Rationale
Although the COVID-19 pandemic could potentially derail and stifle the progress of PHC, particularly RI programs, it also provided a unique opportunity to garner system resilience, including increased attention from the government and international organizations; a surge in health financing and management; prompt agreement to health demands; and an increase in facility equipment and machines, molecular laboratories, and bed spaces in hospitals.
However, because of the COVID-19 pandemic, these achievements across all program themes were threatened. Major implications of these restrictive measures and the overwhelming increase in COVID-19 cases included disruption in the provision of essential healthcare services [22,27,33] and extra burden on frontline healthcare workers, diagnostic capacities, and management of facilities [27]. Beyond these disruptions, the pandemic also revealed weaknesses in the healthcare systems and challenged programmatic assumptions.
Most previous studies evaluated the effect of COVID-19 on healthcare systems as a whole [21,22,26,27,33,40,41,42]. However, from our perspective, we believe that RI program activities did not experience the same level of disruption due to the pandemic. We posit that the impact of COVID-19 on RI programs varied, with some programs being more resilient and less affected. Others programs may have been directly related to SD and, therefore, impacted SD more. The findings from such evaluations will provide the basis for scaling up or pivoting for adaptation and improvement in existing structures.
1.3. Objectives
The study objectives were as follows (see Appendix A for the research questions for the stated objectives):
- To determine the effects of the pandemic on RI programs, focusing on L&G, M&E (SS), CE, the VSC, HFM, and SD in six northern Nigerian states;
- To explore the perception of key stakeholders at different implementation levels (state, local government areas (LGAs), healthcare facilities (HFs), and the community) on the impact of COVID-19 on RI systems and services in six northern Nigerian states;
- To discuss the implications of the findings for RI and PHC program policies and implementation.
1.4. Analysis Framework and Research Hypothesis
Based on the theoretical perspectives and empirical evidences [12,17,18,19,21,22,23,26,27,28,29,30,36,39], a conceptual framework (Figure 1) was designed to comparatively analyze the RI program’s (CE, M&E, the VSC, HFM, L&G, and SD) performance between 2019 and 2020 as a measure of healthcare system resilience and to evaluate the relationships between the impacts of COVID-19 on RI programs using both programmatic and survey data.
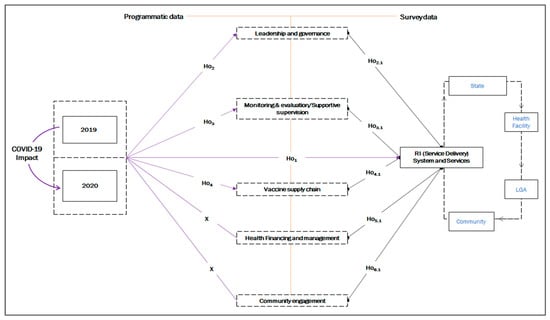
Figure 1.
The study framework and hypothesis.
Based on the conceptual framework in Figure 1, we hypothesized that, transitioning from 2019 to 2020 (the peak year of the pandemic in terms of the number of cases and mortality), RI systems and services were impacted. However, the impact was felt through various key aspects of the program. Therefore, we hypothesized the following.
1.5. Programmatic Themes
- Ho1: There was a change in SD due to the COVID-19 pandemic;
- Ho2: COVID-19 affected different L&G activities;
- Ho3: M&E (SS) were affected by the COVID-19 pandemic;
- Ho4: COVID-19 affected the VSC.
Additionally, we hypothesized that there was a perceived causal effect from the impact of COVID-19 RI programs on SD.
1.6. Survey Themes
- Ho2.1: The impact of COVID-19 on L&G directly affected RI SD;
- Ho3.1: The impact of COVID-19 on M&E (SS) directly affected RI SD;
- Ho5.1: The impact of the COVID-19 pandemic on the VSC directly affected RI SD;
- Ho6.1: The impact of the COVID-19 pandemic on HFM systems directly affected RI SD;
- Ho2.1: The impact of COVID-19 on CE directly affected RI SD.
For the structural equation model (SEM) framework, the exogenous variables included CE, M&E, the VSC, HFM, and L&G, while the endogenous variable was SD. The control variables were the state, work, and job experience (see Figure S2 for a graphical presentation of the frameworks).
2. Materials and Methods
2.1. Study Design
This study utilized a mixed-methods (quantitative and qualitative) approach to understand how the COVID-19 pandemic affected RI programs in six states in northern Nigeria and the challenges during the pandemic.
2.2. Study Setting
The study focused on six Nigerian states: Bauchi, Borno, Yobe, Kaduna, Kano, and Sokoto (See Figure S1) [43]. The majority of the population is rural with scattered settlements, although the states have some urban centers. Most of the population depend on PHC facilities for healthcare services.
The six states were part of the Northern Nigeria Routine Immunization Strengthening Program, in which the state government partnered with the Bill and Melinda Gates Foundation (BMGF), the Aliko Dangote Foundation (ADF), and, in some states, USAID; the Foreign, Commonwealth and Development Office (FCDO); UNICEF; Global Fund; and Global Affairs Canada. The program aimed to strengthen the PHC system through a basket-funding mechanism and was first introduced in Kano (2013) and Bauchi (2014), followed by the other four states (2015). The intervention established strong L&G structures, provided technical assistance, and ensured effective oversight and accountability among coordinating structures.
2.3. Study Sampling
2.3.1. Sample Size
For evaluations at the healthcare-facility and local-government levels, we employed a sample size-estimating formula for a proportion of a finite population from the work by Sharma et al. [44], since the study population was static.
where;
where m = sample size [45,46], n = correction for the sample size (m) as a finite population, p(L) = indicator percentage (proportion of HFs conducting RI out of all HFs in the respective states), z = Z-value (1.96), e = relative error margin (10% = 0.01), and the design effect = 1.15.
To obtain a realistic sample size, the proportion of accessible communities was factored into the calculations based on difficult terrain and security-compromised areas. The study arrived at a total sample size (m) of 267 (Bauchi (n = 37), Borno (n = 23), Kaduna (n = 54), Kano (n = 50), Sokoto (n = 47), and Yobe (n = 56)).
2.3.2. Sampling Technique
We employed a combination of multistage stratified random sampling and non-random (convenience) sampling methods due to factors such as accessibility challenges arising from difficult terrain and security concerns. To achieve this, we initially stratified selected accessible local government areas (LGAs) using a simple balloting technique. Subsequently, we selected health facilities (HFs) based on their categorization within the LGA classification (rural, rural–urban, and urban) [47,48] through computer-generated sampling.
In instances where an LGA or HF was located in an area classified as inaccessible, we adopted a convenience sampling approach to select a nearby location. This choice was made to maintain the intention of randomization while considering practical constraints.
2.3.3. Selection Criteria
The study sample comprised routine immunization (RI) professionals in charge of the selected health facilities from the sampled states. Only those within the selected areas who provided informed consent were included in the study. The exclusion criteria encompassed those who did not meet the inclusion criteria.
2.4. Instrument Design
The instrument used for programmatic data collection was part of the routine M&E tools for project implementation. The survey data, which included quantitative and qualitative data, were obtained using survey questionnaires (See Table S1). The tool was designed and administered in line with the USAID and UNICEF survey for different aspects of healthcare systems [49,50,51].
To ensure instrument validity (localization and adaptability), we considered phase and content validity. We achieved validations through constructive engagements and feedback from healthcare professionals across different institutions.
We tested the reliability of the instrument using two approaches. (1) To determine the internal consistency of the questionnaire, in the absence of a complex multidimensional structure, we conducted Cronbach’s alpha analysis (α) [52,53] and achieved α-values of 0.814, 0.783, and 0.823 for the questionnaire for the state, LGA, and HF, respectively. (2) To measure the external consistency of the instrument measurement over time, we used a test–retest method (Pearson’s product moment) [54,55] and obtained an r-value of 0.784.
2.5. Data Collection
Programmatic data were gathered continuously during the implementation of the routine immunization (RI) program. The programmatic data captured RI program performance between 2019 and 2020. The survey data were collected during the period from June to August 2020. The quantitative survey aimed to capture insights into the effects of the pandemic on various RI program themes. The qualitative questionnaire was employed to gather information about the RI challenges encountered during the pandemic.
2.6. Data Sources and Variables
Research on evaluation design often requires a combination of data types from different sources; therefore, we obtained both primary and secondary data from multiple sources. This aligned with the recommendation of the Measure Evaluation Manual Series No. 3 [51].
2.6.1. Secondary (Programmatic) Data
Secondary data included data from administrative sources (DHIS 2), along with CE reports, routine immunization support supervision (RISS) reports, LGA review meeting reports, minutes from working group meetings, and RI or PHC work plans.
2.6.2. Primary (Survey) Data
We conducted cross-sectional surveys using Likert-scale questionnaires and KIIs to further derive insights from RI programs during the pandemic. We interviewed stakeholders at the state, LGA, and HF levels to obtain information about the impact of the pandemic on various RI programs and the challenges during the pandemic.
2.6.3. Variables
The data variables obtained from the different data sources included service delivery (SD), leadership and governance (L&G), monitoring and evaluation (M&E)/supportive supervision (SS), the vaccine supply chain (VSC), community engagement (CE), and health financing and management (HFM).
2.7. Data Management and Analysis
2.7.1. Statistical Analysis
Data were analyzed using SPSS Amos ver. 28 (IBM, Armonk, NY, USA), with the confidence level set at 95% and p-values less than 0.05 considered significant.
The KMO test showed that the data obtained from the survey were well suited for factor analysis (KMO = 0.95, p < 0.001). Values closer to 1 indicated a good fit (Table S2). For the validity test, we performed principal component analysis and confirmatory factor analysis to establish the significance of the data. Among the measurement items, 24 variables were identified in four components (C1–4). The four components cumulatively explained 73.15% of the variance (Table S3), as shown in the scree plot in Figure S3, which confirmed that only four components were important to the model (eigenvalue not less than 1). Three variables with loading values less than 0.5 were removed from the study (two for SD (SD2, SD3) and one for L&G (L&G1)). Thus, only 21 variables were included in this model.
The confirmatory factor analysis results provided evidence of the discriminant validity of the theoretical constructs [56]. For the path analysis of the survey data using SEM, the fit indices indicated a satisfactory model fit (GFI = 0.884, CFI = 0.961, RMR = 0.054, and RMSEA = 0.062) [57,58,59,60,61]. However, the chi-square analysis of the model fit produced a significant value (chi-square[df=154] = 339.615, p < 0.001), which implied a lack of fit for the model. However, scientists do not rely much on the chi-square test as a useful metric for model fit [59,62].
All variables in the model were statistically significant at the 0.05 level, with standardized factor loadings ranging from 0.537 to 0.860 and reliability (Cronbach’s α) between 0.742 and 0.892 (Table S4; refer to Figure S4 for the diagrammatic representation of the factor loading in Table S4). This implies that the proposed structure for measuring the perceived impact of COVID-19 on RI SD could be achieved using five components (L&G, M&E, the VSC, CE, and the HFM).
2.7.2. Thematic Analysis
We coded the open-ended comments using the grounded theory approach for thematic analyses [63,64], which involved the use of two research team members to form concepts from the data and independent identification of several themes. The researchers agreed upon the themes and coded open-ended comments for each theme. We evaluated each comment using the constant comparative method of grounded theory [63,65].
3. Results
The analysis to test the hypotheses employed a two-way relationship. The first part was approached using an independent t-test analysis of the differences in the programmatic data for thematic areas pre- (2019) and post-COVID-19 (2020). The second part evaluated the relationship between thematic areas from the survey data using path model analysis.
The results of the independent t-test analysis of the programmatic data in Table 1 and Figure 2, Figure 3, Figure 4 and Figure 5 show that there were significant changes in the proportions of indicators for the different thematic areas across the states and for the general program. A graphical description of the path analysis is shown in Figure 6 and Figure 7.

Table 1.
The means (±SD) and comparison of the mean differences for the 2019–2020 program data for the thematic areas.
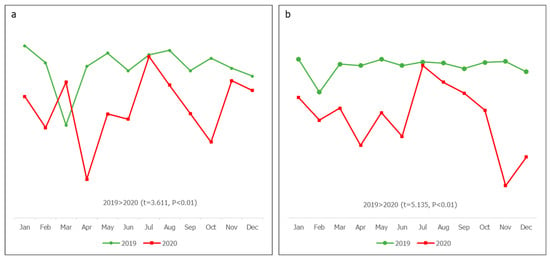
Figure 2.
Service delivery: (a) planned fixed sessions conducted and (b) planned outreach sessions conducted.
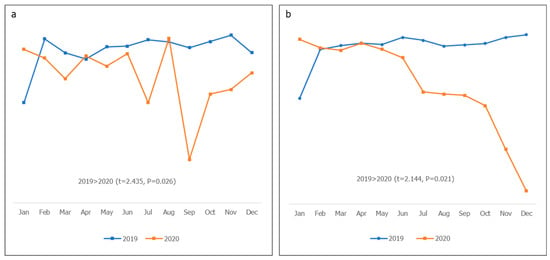
Figure 3.
Governance and leadership: (a) WG meetings conducted and (b) action-point completion rate.

Figure 4.
Supportive supervision: planned RISS visits conducted (LGA to HF).
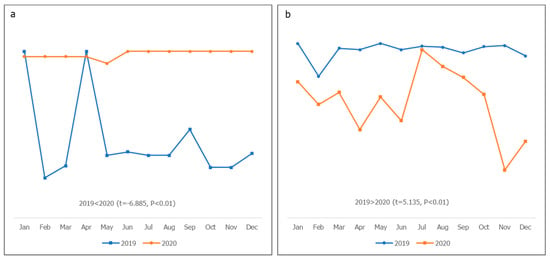
Figure 5.
Vaccine supply chain and logistics: (a) apex facilities that received vaccines on time and (b) vaccine stockout.
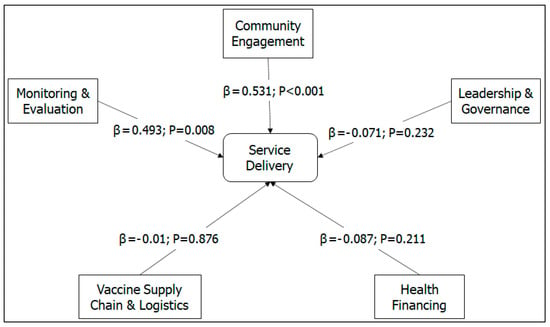
Figure 6.
Path model (standardized regression coefficients).
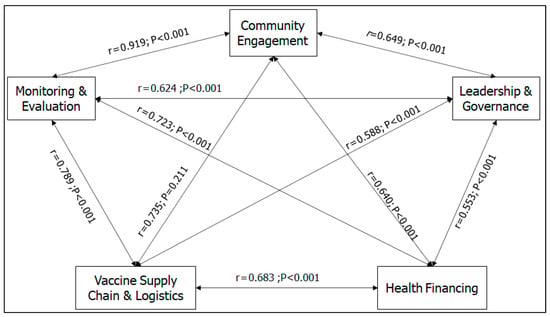
Figure 7.
Path model (correlation between variables).
3.1. Programmatic Data Analysis
Meetings significantly decreased in 2020 compared to 2019 in Bauchi (p < 0.01), Sokoto (p < 0.01), and Yobe (p < 0.05), whereas the changes in Borno, Kaduna, and Kano were not significant (p > 0.05). The changes in the action-point completion rate were not significant in Bauchi, Borno, Kaduna, and Kano but were significantly lower in Sokoto (p < 0.01) and Yobe (p < 0.05) in 2020 than in 2019. The proportions of planned fixed sessions conducted were lower in 2019 than in 2020 in Bauchi, Kano, Sokoto, and Yobe (p < 0.05), whereas the proportions of planned outreach sessions conducted in 2019 significantly decreased in 2020 in Bauchi, Sokoto, Yobe (p < 0.05), Borno, and Kano (p < 0.01). Planned RISS visits conducted (LGA to HF) in 2019 and 2020 did not significantly change in Borno, Kaduna, and Sokoto (p > 0.05); however, in Bauchi, Kano (p < 0.01), and Yobe (p < 0.05), there was a significant increase in 2020 compared to 2019. All six states showed a significant increase in the timely distribution of vaccines to their apex facilities in 2020 compared to 2019 (p < 0.01). Vaccine stockouts in Borno, Sokoto, and Yobe were significantly greater in 2019 than in 2020 (p < 0.01).
As shown in Figure 2, the planned fixed and outreach sessions in 2019 were steady, between 107% and 98%, compared to 2020, demonstrating higher fluctuations with lower values. There were significantly more planned fixed and outreach sessions in 2019 (p < 0.01). As shown in Figure 3, the proportions of working group (WG) meetings conducted and action points completed in 2019 were more progressive and stable than in 2020, and a significant fluctuation in WG meetings was observed (p = 0.026); there was also a rapid drop in action-point completion in 2020 (p = 0.021). There were significantly more M&E activities involving visits to HFs in 2020 than in 2019 (p < 0.01). Although declines were observed in 2019, the activities in 2020 showed steeper fluctuations (Figure 3). As shown in Figure 5, the vaccine supply to facilities in 2020 was significantly steadier than it was in 2019, with more than 98% timely receipt of supplies (p < 0.01). There was a significantly higher stockout in 2019 than in 2020 (p < 0.01).
3.2. Survey Data Analysis
The survey data analysis showed that 256 (95.9%) respondents had a tertiary educational qualification. The mean work experience of the respondents was 17.34 ± 8.32 years, and most of them had more than 16 years of work experience (191/267; 71.5%). Most of the respondents had spent less than five years at their current job (139; 52.1%), with a mean of 7.67 ± 6.61 years of experience (Table 2).

Table 2.
Demographic characteristics of survey participants.
Figure 6 describes the direct effects of leadership and governance (L&G), monitoring and evaluation (M&E)/supportive supervision (SS), the vaccine supply chain (VSC), community engagement (CE), and health financing and management (HFM) on service delivery (SD). The SEM path analysis showed a direct relationship between the changes in SD, CE (β = 0.53; p < 0.001), and M&E (β = 0.49; p = 0.008) during the COVID-19 pandemic. VSCL were an independent factor for SD resilience. L&G and HFs were negative factors for SD resilience, although the effects did not significantly influence SD.
Figure 7 presents the correlation between the thematic areas. The results showed that all the predictor variables were significantly positively correlated (p < 0.001). The impact of COVID-19 on one RI program was positively related to its impact on other programs, though at different levels.
From the thematic analysis and word mapping shown in Figure 8, we identified four major challenges with RI program activities during the COVID-19 pandemic: insufficient equipment and consumables, restriction of movement, human resource scarcity, and perception and fear of infection. Other challenges included noncompliance with protective measures against COVID-19, reduced funding, leadership failure, and insecurity.
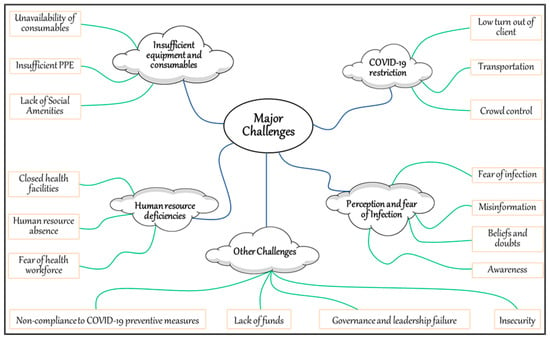
Figure 8.
Challenges in routine immunization program activities during the COVID-19 pandemic.
4. Discussion
This study described the impact of the pandemic on various RI programs and how it affected SD from both the programmatic and survey perspectives. The study highlighted the changes in programmatic data regarding RI services in the pre- and post-pandemic periods and also showed how the perceived changes in RI programs during the peak of the COVID-19 pandemic affected RI SD.
Provision of vaccination services is an indicator that measures RI SD [12,20] and hinges on various RI aspects, such as strong L&G structures [13], M&E (SS) [28,29,30,31], VSCL [17,33], CE [34,35,37], and HFM [19,39]. However, the impact of COVID-19 on these RI aspects may not have had a converging effect on RI SD because of differences in program administration.
Although L&G play a crucial role in RI programs [13], the focus shifted to controlling the spread of the virus during the pandemic [26,27]. More resources were redirected toward COVID-19 activities [66]. Programmatically, owing to restrictions on physical meetings and the unavailability of key stakeholders in Bauchi, Sokoto, and Yobe, the coordination and completion rates for action points were affected. The shift to virtual meetings allowed for continued coordination, but existing weaknesses in L&G and HFM were exacerbated [67]. These issues had a limited direct impact on RI SD during the pandemic.
CE and M&E are essential for successful RI SD because they are the key drivers of demand generation [37,68,69] and program improvement [28,29,30], respectively. During the pandemic, CE was hindered by the lockdown restrictions and vaccine hesitancy. However, SS was optimized through improved monitoring techniques and increased frequency for supervisory visits. The programmatic data showed improvement in this area, while the survey data indicated that the impact of COVID-19 on CE and SS directly affected SD during the pandemic. This highlights the significance of the role of healthcare workers in RI programs at the HF level, as they are responsible for CE and M&E (SS).
VSCL are a vital component of vaccination programs that operate using a multi-structural approach linked to good L&G and HFM [70,71]. The State Primary Health Care Board (SPHCB) teams initially used vaccine delivery systems to distribute essential PPE and later added COVID-19 vaccines. The effective RI–COVID integration showed the potential of PHC programs. Stockout rates improved owing to low demand, which was strongly associated with fears, restrictions, and lack of information among RI service users. The study found that SD activities were not influenced by VSCL, likely because VSCL activities are coordinated by subnational governments [32,72] and not by RI service providers at HFs. The study observed resilience in VSCL with on-time delivery of vaccines to endpoints, sustaining program coverage and preventing vaccine-preventable disease (VPD) outbreaks. The direct-to-facility delivery model operated by states eliminated the need for HFs to pick up vaccines [73], allowing them to focus on SD with minimal disruptions to the VSCL.
Program SD across MoU states was notably affected by disruptions in outreach and fixed sessions. These disruptions were due to lockdown measures limiting the movement of healthcare workers and clients, the unavailability of protective gear leading to the closure of some facilities, and fear among healthcare workers. Immunization intensification efforts post-lockdown [74], such as the state-led periodic intensification of routine immunization (PIRI), were crucial to ensure recovery of lost ground and overall improvements in conducting sessions. The results of this study showed that the impact of the pandemic on L&G, HFM, and VSCL was indirectly related to SD, although the effect was not significant. The impact of the pandemic on CE and M&E during COVID-19 was directly and strongly related to the impact of COVID-19 on SD, whereas VSCL were an independent factor for SD.
The perceived impact of COVID-19 on RI programs was unidirectional and significant. As previously reported, COVID-19 significantly affected RI program activities across all thematic areas [14,24,26,27,32,34,38,67]. However, the effect was stronger in some areas compared to others; L&G, HFM, and VSCL were the least affected by COVID-19 compared to M&E, CE, and SD. This suggests that the pandemic had the most negative effect on activities at the health-facility level, whereas those at the subnational level were less affected.
The study identified four major challenges associated with RI program activities during the COVID-19 pandemic: insufficient equipment and consumables, restriction of movement, human resource scarcity, and perception and fear of infection. Other challenges included noncompliance with protective measures against COVID-19, reduced funding, leadership failure, and insecurity. Studies have shown that global challenges have been observed during the pandemic [14,21,22,27]. However, in Nigeria, there were more frequent reports of the unavailability of consumables across HFs, such as personal protective equipment (PPE) [39,75]. This was associated with poor funding and coordination, which resulted in fear and mistrust among healthcare workers, which inadvertently affected RI SD [33,39].
5. Conclusions
The COVID-19 pandemic significantly impacted and disrupted RI programs. The RI programs were only resilient for planned RISS visits from the LGA to HFs and vaccine supply to apex facilities; interventions were largely coordinated and executed by non-frontline healthcare workers. However, other subthematic areas suffered significant setbacks during the pandemic.
The effect of this pandemic on RI programs was contingent on the level at which it was coordinated. The greatest impact was observed for activities at the HF level, which had a direct effect on SD. However, activities coordinated at the state and LGA levels had little to no effect on SD.
Therefore, this study recommends that the government increase its investments in oversight for RI program interventions executed at the HF and community levels. A renewed focus on and prioritization of these interventions, which have a more direct effect on SD, will improve the resilience of RI and PHC systems and ultimately guarantee improved performance even in future pandemics.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/su151712966/s1. Figure S1: The six (6) northern states. SCIDaR provides RI strengthening support [43], Figure S2: The study model/framework using SEM-designed path analysis (hypotheses H2.1–H6.1), Figure S3: Components with factor loadings matrix, Figure S4: Factor loading in components, Table S1: Questionnaire guide for survey, Table S2: Kaiser–Meyer–Olkin and Bartlett’s tests, Table S3: Initial eigenvalues and rotation sums of squared loadings, Table S4: Initial eigenvalues and rotation sums of squared loadings.
Author Contributions
Conceptualization, E.O.A.J., R.I., Y.Y., U.I. and M.A.; methodology, E.O.A.J., R.I. and U.I.; software, E.O.A.J.; validation, Y.Y., U.I., C.O., A.A., H.T., M.M. and R.M.F.; formal analysis, E.O.A.J., R.I., C.O. and A.A.; investigation, E.O.A.J., C.O., A.A., H.T., M.M. and R.M.F.; resources, Y.Y., R.I., U.I. and M.A.; data curation, Y.Y., C.O., A.A., H.T., M.M. and R.M.F.; writing—original draft preparation, E.O.A.J., R.I., U.I. and C.O.; writing—review and editing, Y.Y., A.A., H.T., M.M. and R.M.F.; visualization, E.O.A.J., R.I., U.I. and C.O.; supervision, Y.Y., U.I. and M.A.; project administration, R.I., U.I. and M.A.; funding acquisition, Y.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research and APC were funded by the Bill and Melinda Gates Foundation (BMGF), grant number OPP1127484.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Nigerian National Health Research Ethics Committee with approval number NHREC/01/01/2007-23/08/2022 on 23 August 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to restrictions on usage from the different levels of government represented in the study.
Acknowledgments
The authors are grateful to all McKing consultants, state immunization officers, coordinators of the state emergency operations centers (EOCs), members of the state primary health care development agencies, and management boards for their unwavering support and invaluable contributions towards the successful implementation of this research program. Your dedication and commitment to this project have been instrumental in enabling us to achieve our research goals. Thank you for your cooperation and assistance.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
| CB | capacity building |
| CE | community engagement |
| CFI | comparative fit index |
| DVD | digital vaccine delivery |
| DPT | diphtheria, tetanus, and pertussis |
| EOC | emergency operation center |
| FGD | focused group discussion |
| GLS | generalized least square |
| GFI | goodness-of-fit index |
| HCD | human-centered design |
| HF | health facility |
| HFM | health financing and management |
| IFRC | International Federation of Red Cross and Red Crescent Societies |
| IMOP | integrated medical outreach program |
| ISS | integrated supportive supervision |
| KMO | Kaiser–Meyer–Olkin |
| LGA | local government area |
| L&G | leadership and governance |
| M&E/SS | monitoring and evaluation/supportive supervision |
| NCDC | Nigeria Centers for Disease Control |
| NPI | national provider identifier |
| OECD | Organization for Economic Cooperation and Development |
| PIRI | periodic intensification of routine immunization |
| PCA | principal component analysis |
| PHC | primary health care |
| PPE | personal protective equipment |
| RI | routine immunization |
| SD | service delivery |
| SEM | structural equation modeling |
| SPSS | Statistics Package for Social Science |
| TWG | technical working group |
| UNICEF | United Nations Children Funds |
| USAID | United States Agency for International Development |
| VSCL | vaccine supply chain logistics |
| WG | working group |
| WHO | World Health Organization |
Appendix A
Research questions
- To what extent has the COVID-19 pandemic affected the performance of RI programs in the six northern Nigerian states in terms of:
- a.
- Leadership and governance;
- b.
- Service delivery;
- c.
- Monitoring and evaluation/supportive supervision;
- d.
- Community engagement;
- e.
- The caccine supply chain;
- f.
- Funding and financial management;
- g.
- Capacity building.
- What was the performance of the RI program during pre-pandemic periods and how has this changed?
- What adaptive measures were utilized and how did they influence the RI program during the COVID-19 pandemic?
- Which stakeholders, processes, and factors were responsible for/have contributed to the resilience of the RI program amidst the pandemic strains?
- What are the persisting challenges?
- What policy and program changes can be made to bolster the existing RI program and support the integration of COVID-19 interventions?
References
- Liu, J.; Liao, X.; Qian, S.; Yuan, J.; Wang, F.; Liu, Y.; Wang, Z.; Wang, F.-S.; Liu, L.; Zhang, Z. Community transmission of severe acute respiratory syndrome Coronavirus 2, Shenzhen, China, 2020. Emerg. Infect. Dis. 2020, 26, 1320–1323. [Google Scholar] [CrossRef] [PubMed]
- Li, Q. An Outbreak of NCIP (2019-nCoV) Infection in China—Wuhan, Hubei Province, 2019−2020. China CDC Wkly. 2020, 2, 79–80. [Google Scholar] [CrossRef]
- NHS. Landmark Moment as First NHS Patient Receives COVID-19 Vaccination. 2020. Available online: https://www.england.nhs.uk/2020/12/landmark-moment-as-first-nhs-patient-receives-covid-19-vaccination/ (accessed on 19 October 2022).
- OCHA Services. First Case of Coronavirus Disease Confirmed in Nigeria—Nigeria. Available online: https://reliefweb.int/report/nigeria/first-case-coronavirus-disease-confirmed-nigeria (accessed on 19 October 2022).
- NCDC. NCDC Coronavirus COVID-19 Microsite. 2022. Available online: https://covid19.ncdc.gov.ng/advisory/ (accessed on 19 October 2022).
- GAVI. Combining COVID-19 and Routine Vaccination: Nigeria Implements a ‘Whole Family’ Approach. Available online: https://www.gavi.org/vaccineswork/combining-covid-19-and-routine-vaccination-nigeria-implements-whole-family-approach?gclid=Cj0KCQjw6pOTBhCTARIsAHF23fI2oGsW8VwCEdYfjFrVquJm6PPpW0NOMp_3rq0ZjMbFusJ1L4zyGyAaApeOEALw_wcB (accessed on 10 September 2022).
- Mader, S.; Rüttenauer, T. The Effects of Non-pharmaceutical Interventions on COVID-19 Mortality: A Generalized Synthetic Control Approach Across 169 Countries. Front. Public Health 2022, 10, 820642. [Google Scholar] [CrossRef] [PubMed]
- Watson, O.J.; Barnsley, G.; Toor, J.; Hogan, A.B.; Winskill, P.; Ghani, A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022, 22, 1293–1302. [Google Scholar] [CrossRef] [PubMed]
- Dan-Nwafor, C.; Ochu, C.L.; Elimian, K.; Oladejo, J.; Ilori, E.; Umeokonkwo, C.; Steinhardt, L.; Igumbor, E.; Wagai, J.; Okwor, T.; et al. Nigeria’s public health response to the COVID-19 pandemic: January to May 2020. J. Glob. Health 2020, 10, 020399. [Google Scholar] [CrossRef] [PubMed]
- Owhonda, G.; Onyekwere, N.; Kanee, R.B.; Maduka, O.; Nwadiuto, I.; Okafor, C.; Chibianotu, O.; Aigbogun, E.O. Community awareness, perceptions, enablers and potential barriers to non-pharmaceutical interventions (npis) in the COVID-19 pandemic in Rivers State, Nigeria. Biomed. J. Sci. Tech. Res. 2021, 36, 28984–28995. [Google Scholar] [CrossRef]
- Abubakar, I.; Dalglish, S.L.; Angell, B.; Sanuade, O.; Abimbola, S.; Adamu, A.L.; Adetifa, I.M.O.; Colbourn, T.; Ogunlesi, A.O.; Onwujekwe, O.; et al. The Lancet Nigeria Commission: Investing in health and the future of the nation. Lancet 2022, 399, 1155–1200. [Google Scholar] [CrossRef]
- Mbaeyi, C.; Kamawal, N.S.; Porter, K.A.; Azizi, A.K.; Sadaat, I.; Hadler, S.; Ehrhardt, D. Routine Immunization Service Delivery Through the Basic Package of Health Services Program in Afghanistan: Gaps, Challenges, and Opportunities. J. Infect. Dis. 2017, 216, S273–S279. [Google Scholar] [CrossRef]
- Oku, A.; Oyo-Ita, A.; Glenton, C.; Fretheim, A.; Eteng, G.; Ames, H.; Muloliwa, A.; Kaufman, J.; Hill, S.; Cliff, J.; et al. Factors affecting the implementation of childhood vaccination communication strategies in Nigeria: A qualitative study. BMC Public Health 2017, 17, 200. [Google Scholar] [CrossRef]
- OECD. The Territorial Impact of COVID-19: Managing The Crisis Across Levels of Government. Organ. fo Econ. Coop. Dev. 2020, 2–44. Available online: https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-across-levels-of-government-d3e314e1/ (accessed on 19 October 2022).
- Bello, I.M.; Lebo, E.; Shibeshi, M.E.; Akpan, G.U.; Chakauya, J.; Masresha, B.G.; Daniel, F. Implementation of integrated supportive supervision in the context of coronavirus 19 pandemic: Its effects on routine immunization and vaccine preventable surveillance diseases indicators in the East and Southern African countries. Pan Afr. Med. J. 2021, 38, 164. [Google Scholar] [CrossRef] [PubMed]
- Faiva, E.; Hashim, H.T.; Ramadhan, M.A.; Musa, S.K.; Bchara, J.; Tuama, Y.D.; Adebisi, Y.A.; Kadhim, M.H.; Essar, M.Y.; Ahmad, S.; et al. Drug supply shortage in Nigeria during COVID-19: Efforts and challenges. J. Pharm. Policy Pr. 2021, 14, 17. [Google Scholar] [CrossRef] [PubMed]
- Olutuase, V.O.; Iwu-Jaja, C.J.; Akuoko, C.P.; Adewuyi, E.O.; Khanal, V. Medicines and vaccines supply chains challenges in Nigeria: A scoping review. BMC Public Health 2022, 22, 11. [Google Scholar] [CrossRef] [PubMed]
- WHO and UNICEF. Maintaining Routine Immunization Services Vital during the COVID-19 Pandemic. 2020. Available online: https://www.unicef.org/tajikistan/press-releases/maintaining-routine-immunization-services-vital-during-covid-19-pandemic-who-and (accessed on 19 October 2022).
- The Impact of COVID-19 on Digital Financial Inclusion. Available online: https://www.gpfi.org/sites/gpfi/files/sites/default/files/5_WB%20Report_The%20impact%20of%20COVID-19%20on%20digital%20financial%20inclusion.pdf (accessed on 25 April 2022).
- Uba, B.V.; Waziri, N.E.; Akerele, A.; Biya, O.; Adegoke, O.J.; Gidado, S.; Ugbenyo, G.; Simple, E.; Usifoh, N.; Sule, A.; et al. Strengthening facility-based immunization service delivery in local government areas at high risk for polio in Northern Nigeria, 2014–2015. Pan. Afr. Med. J. 2021, 40 (Suppl. 1), 6. [Google Scholar] [PubMed]
- Shet, A.; Carr, K.; Danovaro-Holliday, M.C.; Sodha, S.V.; Prosperi, C.; Wunderlich, J.; Wonodi, C.; Reynolds, H.W.; Mirza, I.; Gacic-Dobo, M.; et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: Evidence of disruption and recovery from 170 countries and territories. Lancet Glob. Health 2022, 10, e186–e194. [Google Scholar] [CrossRef]
- Causey, K.; Fullman, N.; Sorensen, R.J.D.; Galles, N.C.; Zheng, P.; Aravkin, A.; Danovaro-Holliday, M.C.; Martinez-Piedra, R.; Sodha, S.V.; Velandia-González, M.P.; et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: A modelling study. Lancet 2021, 398, 522–534. [Google Scholar] [CrossRef]
- Hirabayashi, K. The Impact of COVID-19 on Routine Vaccinations|UNICEF East Asia and Pacific. Unicef. 2020. Available online: https://www.unicef.org/eap/stories/impact-covid-19-routine-vaccinations (accessed on 18 October 2022).
- World Health Organization. COVID-19 Pandemic Fuels Largest Continued Backslide in Vaccinations in Three Decades, pp. 1–5. 2022. Available online: https://www.who.int/news/item/15-07-2022-covid-19-pandemic-fuels-largest-continued-backslide-in-vaccinations-in-three-decades (accessed on 18 October 2022).
- GAVI. At least 80 Million Children at Risk of Disease as COVID-19 Disrupts Vaccination Efforts, Warn Gavi, WHO and UNICEF. Gavi, the Vaccine Alliance. 2020. Available online: https://www.gavi.org/news/media-room/least-80-million-children-risk-disease-covid-19-disrupts-vaccination-efforts (accessed on 18 October 2022).
- SeyedAlinaghi, S.; Karimi, A.; Mojdeganlou, H.; Alilou, S.; Mirghaderi, S.P.; Noori, T.; Shamsabadi, A.; Dadras, O.; Vahedi, F.; Mohammadi, P.; et al. Impact of COVID-19 pandemic on routine vaccination coverage of children and adolescents: A systematic review. Health Sci. Rep. 2022, 5, e00516. [Google Scholar] [CrossRef]
- Sharma, L.; Sharma, M.; Singh, S.; Dwiwedi, M.; Agarwal, D.; Gupta, G.; Dhiman, R. Magnitude and causes of routine immunization disruptions during COVID-19 pandemic in developing countries. J. Fam. Med. Prim. Care 2021, 10, 3991–3997. [Google Scholar] [CrossRef]
- Bosch-Capblanch, X.; Liaqat, S.; Garner, P. Managerial supervision to improve primary health care in low- and middle-income countries. Cochrane Database Syst. Rev. 2011, 2011, CD006413. [Google Scholar] [CrossRef]
- Bradley, S.; Kamwendo, F.; Masanja, H.; de Pinho, H.; Waxman, R.; Boostrom, C.; McAuliffe, E. An in-depth exploration of health worker supervision in Malawi and Tanzania. Hum. Resour. Heal. 2013, 11, 43. [Google Scholar] [CrossRef]
- Madede, T.; Sidat, M.; McAuliffe, E.; Patricio, S.R.; Uduma, O.; Galligan, M.; Bradley, S.; Cambe, I. The impact of a supportive supervision intervention on health workers in Niassa, Mozambique: A cluster-controlled trial. Hum. Resour. Health 2017, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Onyango, R.O. Designing an M&E System during a Pandemic: Successes and Failures at a Project’S Inception Phase. Indep. Dev. Eval. (IDEV)—Afr. Dev. Bank. 2021. Available online: http://idev.afdb.org/en/content/designing-me-system-during-pandemic-successes-and-failures-projects-inception-phase (accessed on 19 October 2022).
- UNICEF. The Critical Role of UNICEF in Accelerating COVID-19 Vaccine Rollout through National Logistics Work. Supply Div. 2021. Available online: https://www.unicef.org/supply/stories/critical-role-unicef-accelerating-covid-19-vaccine-rollout-through-national-logistics-work (accessed on 8 January 2023).
- Essoh, T.-A.; Adeyanju, G.C.; Adamu, A.A.; Ahawo, A.K.; Aka, D.; Tall, H.; Aplogan, A.; Wiysonge, C.S. Early Impact of SARS-CoV-2 Pandemic on Immunization Services in Nigeria. Vaccines 2022, 10, 1107. [Google Scholar] [CrossRef] [PubMed]
- GAVI. Routine Vaccinations during a Pandemic—Benefit or Risk? 2020. Available online: https://www.gavi.org/vaccineswork/routine-vaccinations-during-pandemic-benefit-or-risk?gclid=Cj0KCQiAzeSdBhC4ARIsACj36uGt_uOFfiMwXitGM_dO30qknvxXbswogi3cOo7YW1X0hO9Ay--0Bu0aAmaIEALw_wcB (accessed on 8 January 2023).
- World Health Organisation. Guiding Principles for Immunization Activities during the COVID-19 Pandemic. WHO/2019-nCoV/immunization_services/2020.1, no. March, pp. 17–20. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331590/WHO-2019-nCoV-immunization_services-2020.1-eng.pdf (accessed on 15 August 2022).
- World Health Organization. COVID-19 Global Risk Communication and Community Engagement Strategy—Interim Guidance. 2020, 20–21. Available online: https://www.who.int/publications/i/item/covid-19-global-risk-communication-and-community-engagement-strategy (accessed on 15 August 2022).
- Musa, E. The Impact of the COVID-19 Pandemic on Immunization Programs in Kaduna State Nigeria. Sabin Vaccine Inst. 2020. Available online: https://www.sabin.org/resources/the-impact-of-the-covid-19-pandemic-on-immunization-programs-in-kaduna-state-nigeria/ (accessed on 19 October 2022).
- G20 Italian Presidency. The Impact of COVID-19 on Digital Financial Inclusion. In Glob. Partnersh. Financ. Incl. By World Bank; 2021; pp. 1–29. Available online: https://www.mef.gov.it/inevidenza/2021/article_00064/Annex-II-Reports-and-Documents-Received-Fourth-G20-FMCBGs-13-Octob....pdf (accessed on 19 October 2022).
- Alagboso, C. Overcoming the Challenges of Financing Routine Immunisation Beyond COVID-19. Nigeria Health Watch 2022. Available online: https://nigeriahealthwatch.com/overcoming-the-challenges-of-financing-routine-immunisation-beyond-covid-19/ (accessed on 19 October 2022).
- Aregbeshola, B.S.; Folayan, M.O. Nigeria’s financing of health care during the COVID-19 pandemic: Challenges and recommendations. World Med. Health Policy 2022, 14, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Abbas, K.; Procter, S.R.; van Zandvoort, K.; Clark, A.; Funk, S.; Mengistu, T.; Hogan, D.; Dansereau, E.; Jit, M.; Flasche, S.; et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: A benefit–risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob. Health 2020, 8, e1264–e1272. [Google Scholar] [CrossRef]
- Ranganathan, R.; Khan, A.M. Routine immunization services during the coronavirus (COVID-19) pandemic. Indian J. Community Health 2020, 32, 236–239. [Google Scholar] [CrossRef]
- USAID. The Power of Partnerships for Improved Routine Immunization in Nigeria. 2019. Available online: https://mcsprogram.org/the-power-of-partnerships-for-improved-routine-immunization-in-nigeria/ (accessed on 26 September 2022).
- Sharma, S.; Mudgal, S.; Thakur, K.; Gaur, R. How to calculate sample size for observational and experiential nursing research studies? Natl. J. Physiol. Pharm. Pharmacol. 2020, 10, 1. [Google Scholar] [CrossRef]
- Fox, N.; Hunn, A.; Mathers, N. Sampling and Sample Size Calculation. NIHR RDS East Midl. 2022, 1, 1–4. Available online: https://www.bdct.nhs.uk/wp-content/uploads/2019/04/Sampling-and-Sample-Size-Calculation.pdf (accessed on 14 May 2022).
- Lakens, D. Sample size justification. Collabra Psychol. 2022, 8, 33267. [Google Scholar] [CrossRef]
- Aliyu, A.; Amadu, L. Urbanization, cities and health: The challenges to Nigeria—A review. Ann. Afr. Med. 2017, 16, 149–158 . [Google Scholar] [CrossRef] [PubMed]
- Farrell, K. An Inquiry into the Nature and Causes of Nigeria’s Rapid Urban Transition. Urban Forum 2018, 29, 277–298. [Google Scholar] [CrossRef]
- IA2030. Monitoring and Monitoring & Evaluation (M&E) Framework. Immun. Agenda 2020, 2030, 1–34. [Google Scholar]
- Khatiwada, A.P.; Maskey, S.; Shrestha, N.; Shrestha, S.; Khanal, S.; Kc, B.; Paudyal, V. Impact of the first phase of COVID-19 pandemic on childhood routine immunisation services in Nepal: A qualitative study on the perspectives of service providers and users. J. Pharm. Policy Pract. 2021, 14, 79. [Google Scholar] [CrossRef]
- Turner, A.G.; Angels, G.; Tsui, A.O.; Wilkinson, M.; Magnani, R. Sampling Manual For Facility Surveys, 3rd ed.; MEASURE Evaluation Manual Series; 2001; Available online: https://www.measureevaluation.org/resources/publications/ms-01-03/at_download/document (accessed on 14 April 2022).
- Green, S.B.; Yan, Y. Evaluation of Dimensionality in the Assessment of Internal Consistency Reliability: Coefficient Alpha and Omega Coefficients. Educ. Meas. Issues Pract. 2015, 34, 14–20. [Google Scholar] [CrossRef]
- Davenport, E.C.; Davison, M.L.; Liou, P.Y.; Love, Q.U. Reliability, Dimensionality, and Internal Consistency as Defined by Cronbach: Distinct Albeit Related Concepts. Educ. Meas. Issues Pract. 2015, 34, 4–9. [Google Scholar] [CrossRef]
- Collins, L.M. Research Design and Methods. Encycl. Gerontol. 2007, 433–442. [Google Scholar] [CrossRef]
- Yu, C.H. Test-Retest Reliability. Encycl. Soc. Meas. 2005, 777–784. [Google Scholar] [CrossRef]
- Wood, P. Confirmatory Factor Analysis for Applied Research. Am. Stat. 2008, 62, 91–92. [Google Scholar] [CrossRef]
- Pavlov, G.; Maydeu-Olivares, A.; Shi, D. Using the Standardized Root Mean Squared Residual (SRMR) to Assess Exact Fit in Structural Equation Models. Educ. Psychol. Meas. 2020, 81, 110–130. [Google Scholar] [CrossRef] [PubMed]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K. A Beginner’s Guide to Structural Equation Modeling, 3rd ed.; Psychology Press: London, UK, 2012; pp. 828–829. [Google Scholar] [CrossRef]
- Parry, S. Fit Indices commonly reported for CFA and SEM. Cornell Univ. Cornell Stat. Consult. Unit. 2020, 1, 2021. [Google Scholar]
- Tanaka, J.S.; Huba, G.J. A fit index for covariance structure models under arbitrary GLS estimation. Br. J. Math. Stat. Psychol. 1985, 38, 197–201. [Google Scholar] [CrossRef]
- Stone, B.M. The Ethical Use of Fit Indices in Structural Equation Modeling: Recommendations for Psychologists. Front. Psychol. 2021, 12, 5221. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.W. Qualitative Inquiry & Research Design: Choosing among Five Approaches, vol. 2. 2007. Available online: https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=1807302 (accessed on 16 September 2022).
- Khan, S.N. Qualitative Research Method: Grounded Theory. Int. J. Bus. Manag. 2014, 9, p224. [Google Scholar] [CrossRef]
- Cohen, L.; Manion, L.; Morrison, K. Research Methods in Education; Routledge: London, UK, 2007. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Pandemic Leads to Major Backsliding on Childhood Vaccinations, New WHO, UNICEF Data Shows. News Release 2021. Available online: https://www.unicef.org/press-releases/covid-19-pandemic-leads-major-backsliding-childhood-vaccinations-new-who-unicef-data (accessed on 8 January 2023).
- Save the Children. SCALING UP ROUTINE IMMUNISATION COVERAGE IN NIGERIA. 2022. Available online: https://www.savethechildren.org.uk/blogs/2022/scaling-up-routine-immunisation-coverage-in-nigeria (accessed on 8 January 2023).
- NPHCDA. Community Engagement Strategy for Strengthening Routine immunization in northern nigeria. pp. 1–20. 2022. Available online: https://publications.jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=22337&lid=3 (accessed on 22 June 2022).
- Oyo-Ita, A.; Bosch-Capblanch, X.; Ross, A.; Oku, A.; Esu, E.; Ameh, S.; Oduwole, O.; Arikpo, D.; Meremikwu, M. Effects of engaging communities in decision-making and action through traditional and religious leaders on vaccination coverage in Cross River State, Nigeria: A cluster-randomised control trial. PLoS ONE 2021, 16, e0248236. [Google Scholar] [CrossRef] [PubMed]
- Gooding, E.; Spiliotopoulou, E.; Yadav, P. Impact of vaccine stockouts on immunization coverage in Nigeria. Vaccine 2019, 37, 5104–5110. [Google Scholar] [CrossRef]
- Molemodile, S.; Wotogbe, M.; Abimbola, S. Evaluation of a pilot intervention to redesign the decentralised vaccine supply chain system in Nigeria. Glob. Public Health 2017, 12, 601–616. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Lessons Learned and Good Practices: Country-Specific Case Studies on Immunization Activities during the COVID-19 Pandemic. 2021. Available online: https://www.unicef.org/media/115221/file/Lessons-Learned-and-Good-Practices-Immunization-Activities-During-the-COVID-19-Pandemic-2021.pdf (accessed on 19 October 2022).
- Aina, M.; Igbokwe, U.; Jegede, L.; Fagge, R.; Thompson, A.; Mahmoud, N. Preliminary results from direct-to-facility vaccine deliveries in Kano, Nigeria. Vaccine 2017, 35, 2175–2182. [Google Scholar] [CrossRef] [PubMed]
- Uchenna, A.A.; Saleh, J.-E.; Saddiq; Eze, O.L.; Ogbonna, P.E.; Calista, U.N.; Abonyi, I.; Isaac, E.; Obianuju, I.C.; Ugochukwu, E.N.; et al. Intensified Routine Immunization (RI) Activities as A Strategy for Improving Routine Immunization and Acute Flaccid Paralysis (AFP) Surveillance outcomes; Lessons from Intensified Activities Conducted in 2 LGAs in Abia State Nigeria. J. Community Med. Public Health 2018, 2, 100032. [Google Scholar] [CrossRef][Green Version]
- allAfrica.com. Nigeria: Rising Cost of Healthcare in Nigeria Amid COVID-19. 2020. Available online: https://allafrica.com/stories/202103070279.html (accessed on 8 January 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).