Abstract
Recent proposals for reform in England have presented widely available “smart” mainstream digital devices as a means to address some of the challenges facing adult social care and as alternatives to unsustainable analogue “telecare” systems. Drawing on 40 interviews with experts from local authorities, the care and technology sectors, and people with lived experience of social care services, we explored how mainstream technologies are being used in practice in England and critically examined their potential to contribute to policy priorities of wellbeing and sustainability. Across all expert groups interviewed, examples were cited in which the use of mainstream devices supported the economic sustainability of adult social care and/or enhanced aspects of wellbeing, moving the role of technology in care beyond monitoring and managing risks. However, when viewed through a three-dimensional conceptual lens that includes material, relational and subjective wellbeing, the use of smart devices in practice also created tensions and trade-offs between the dimensions, with implications for sustainability. The various ways mainstream devices are being used in adult social care also raised complexities related to risks, responsibilities, and inequalities and required “wraparound services”, tempering their ability to deliver cost savings. To address these issues, we suggest a person-centred approach to technology across local authorities, with investment in wraparound services and to mediate inequalities associated with the “digital divide”.
1. Introduction
1.1. The “Crisis” of Adult Social Care in England
Adult social care in England—which includes care and support in the community, residential and day services—has been described as being “in crisis” and unsustainable because of increased demand and reduced resources, creating issues related to service quality and high levels of unmet need [1]. Indeed, the UK government’s own Sustainable Development Unit [2] has noted that the “social care system is at an important crossroads. Whether we consider our demographics, our use of resources or the financial forecasts, it is widely accepted that the current health and care system is unsustainable without radical transformation”.
Statutory responsibility for adult social care policy in the UK has been devolved to the national administrations in England, Scotland, Wales, and Northern Ireland since 1998. Each nation can therefore introduce its own care legislation and standards and allocate funding according to its own priorities [3]. In England—the focus of this paper—the delivery of publicly-funded adult social care is the responsibility of 152 local authorities, and receipt of services is contingent on both a means and a needs test. The 2014 Care Act [4] is a key piece of English adult social care legislation, with the principles of “prevention”, “person-centred care”, and “wellbeing” at its core [5].
Demand-side challenges to England’s social care system cited in the recent White Paper on adult social care reform, “People at the Heart of Care” [6], include the ageing of the population due to increased longevity and changes in fertility. The proportion of the total population aged over 65 years is projected to increase from 18.2 to 20.7% between mid-2018 and mid-2028 [7], while the total fertility rate in England remains below replacement level (2.075) and fell to a record low in 2020 (1.58 children per woman) [8]. Although overall life expectancy in England has been increasing (with geographical differences [9]), healthy and disability-free life expectancies have not kept pace [10], with implications for the sustainability of social care systems due to longer periods of ill health at the end of life and the associated need for support. As a reflection of this misalignment between life expectancy generally and disability-free life expectancy, the number of people living with a disability is predicted to increase by 25.0%, from 2.25 million to 2.81 million, between 2015 and 2025, concentrated mainly among people aged over 85 [11].
Concurrently, changing family formations and the rising prevalence of solo living also affect the sustainability of a social care system that relies heavily on “unpaid” (informal) care. Prior to the COVID-19 pandemic, it was estimated there were 7.3 million unpaid carers in England [12] providing care valued at GBP 100 billion per year (more than six times the total value of care arranged by local authorities—GBP 16.5 billion) [13]. Most unpaid care in England is provided by spouses or children, but decreased fertility has resulted in rising numbers of older adults who are childless [14]. As such, solo living later in life has increased, driven in part by reduced fertility but also by changing family structures and out-migration of children. By 2033, it is projected that people living alone will make up 41% of all households in England (11.3 million people, nearly 30% more than in 1961) [15]. Solo living will be a particular issue for the “oldest old” (people aged over 85), with their numbers projected to increase by 145% between 2008 and 2033 [16].
The supply of formal, paid care workers is also an issue affecting the sustainability of England’s social care system. In 2019, the vacancy rate for adult social care was 7.3%, higher than that across all sectors (2.7%); of these, the majority were care workers (70,000 vacancies), with a vacancy rate of 8.2% (higher than for all other direct care-providing roles, e.g., personal assistants). The turnover rate for care workers in England in 2019/20 was 38.1% [17]. Issues of recruitment and retention within the social care workforce have been exacerbated by the UK’s withdrawal from the European Union and the COVID-19 pandemic [18].
Alongside the increase in demand for social care services and issues affecting the supply of care via paid care workers and unpaid carers, the “austerity” policies imposed after 2010 by UK Governments (under the coalition government 2010–2015 and Conservative administrations 2015–2019) have affected social care sustainability. In real terms, social care spending in England fell by 6.4% [19] in a context of increased demand [20]. This reduction in resources resulted in falling numbers of people receiving local authority-provided (or funded) social care support or services. At the local level, each of the 152 local authorities with social services responsibility in England decides how much funding to allocate to social care; uneven cuts to overall service budgets and unequal ability, since 2013, to generate income locally from the “social care precept” via local taxes and business rates have resulted in disparities in spending on social care geographically [20]. Furthermore, older adults are experiencing the greatest levels of unmet need due to the unequal allocation of cuts to adult social care funding across age groups [1].
1.2. Technology and Adult Social Care in England
Since the 2000s, technology has been presented by policy discourse in England as one way to address particular challenges to adult social care [21,22,23,24,25,26,27,28]. In a sector facing issues related to workforce recruitment and retention, policymakers have repeatedly argued that using technology in adult social care will increase capacity [29]; recently, the current Secretary of State for Health and Social Care, Sajid Javid [28], cited examples of where technology had freed up “[t]ime that could be spent on patient care”. Reflecting on the economic aspect of sustainability [Appendix A, note 1], many local authority directors of adult social care services view technology as a means to contain costs, with 92% of those surveyed in 2021 viewing assistive and communications technologies as “quite” or “very” important in making savings [30] and two-thirds making additional investments in digital and technology as part of a broader approach to economic sustainability (only 1% were disinvesting).
The use of technologies in adult social care is variable geographically, as there is no statutory requirement for local authorities to provide them as part of their services. Local authority provision is funded mainly from social care budgets, with services increasingly contracted out, including those for assessment, installation, monitoring (receiving alerts and processing them), and response (attending the user in an emergency). There are also variations among local authorities in charging and assessment policies and in the range of devices and services available to those who meet the applicable means and needs tests [31].
Though technology became the focus of policy discourse in the 2000s, it has been part of adult social care arrangements in practice since the 1960s. At this time, “first-generation” [32] telecare “pull cord” and user-worn pendant alarms in sheltered accommodation schemes were introduced [33], with “second-generation” systems emerging later, including continuous environmental monitoring equipment with sensors to raise an alarm in an emergency. The term “technology-enabled care services” (TECS) has recently come into use, which refers to telemedicine and telehealth systems alongside first- and second-generation devices. It has been estimated the vast majority of TECS users have first-generation pendant alarms (1.4 million out of a total 1.7 million) [34].
In the mid-2000s, national programmes of investment in England were launched to support the development of telecare services within adult social care. This included the Preventative Technology Grant in England to accelerate the development of local authorities’ TECS (GBP 80 million from 2006–2008) and programmes to create an evidence base related to the efficacy of telecare and telehealth, such as the Whole System Demonstrator (WSD) programme set up in 2008 (Appendix A, note 2), to date the largest randomized control trial of these devices. The government also funded a subsequent randomized control trial of technology use by people with dementia to further develop the evidence base (Assistive Technology and Telecare to maintain Independent Living At home for people with dementia [ATTILA]). Since the mid-2010s, national investment in funding programmes has shifted to focus on trials of newer digital technologies in adult social care, featuring robotics, artificial intelligence, and ICT systems [35]. More recently, technology featured in a long-awaited white paper on the future of adult social care in England [6], which allocated GBP 150 million to promote use of digital technologies across the adult social care sector.
1.3. The Sustainability of Technology in Adult Social Care: Time for Change?
The potential of technologies to address some of the demands on English adult social care is mediated by several key issues, the first being a practical challenge to TECS’ own sustainability — “the digital switchover”. Most existing TEC devices and services in England use a short-range radio frequency link from a device (for example a pendant alarm or sensors) to a base unit that alerts a monitoring centre via an analogue telephone line [36]. Telecommunications providers are moving their services to modern Internet protocol-based networks gradually with an end date of 2025. As services are migrated, devices using analogue lines will need to be replaced by digital alternatives to ensure reliable connectivity [37]. Most TECS designers and manufacturers have focused on adapting existing analogue equipment to use SIM cards or Ethernet cables; it is estimated that replacing existing analogue-enabled devices with digital versions in the UK will require investment of some GBP 150–300 million [34]. At a time when the gap is widening between the demands on adult social care services and their resources, many local authorities will find this unaffordable and unsustainable.
The second challenge relates to the misalliance between the centrality of “wellbeing” as a guiding principle for English adult social care policy and the way local authorities have traditionally commissioned and delivered TECS. The political interest in wellbeing in England has been argued to be part of the concept’s “second wave”, where global debates as to how to assess a nation’s progress moved beyond economic measures such as GDP to include “quality of life”, “happiness” and “wellbeing”. England, as part of the UK, has been identified as a having international “prominence in the politics and policy of wellbeing” [38] (p. 4) insofar as there has been explicit policy focus on both enhancing and measuring the wellbeing of UK citizens since the 2010s. The 2014 Care Act legislated that local authorities in England had a “general duty” to promote individual wellbeing through their adult social care services, with the concept defined as relating to:
“(a) personal dignity (including treatment of the individual with respect);
(b) physical and mental health and emotional wellbeing;
(c) protection from abuse and neglect;
(d) control by the individual over day-to-day life (including over care and support, or support, provided to the individual and the way in which it is provided);
(e) participation in work, education, training or recreation;
(f) social and economic wellbeing;
(g) domestic, family and personal relationships;
(h) suitability of living accommodation;
(i) the individual’s contribution to society” [4] (p. 1).
Globally, there is a long history of conceptualizing wellbeing as comprising different dimensions or domains [39,40], and the second wave of wellbeing in the UK was argued to have foregrounded the importance of the subjective element. Indeed, subjective wellbeing is central to the Care Act, which states each person is best placed to define their own wellbeing. The Care Act’s approach to wellbeing also aligns with research and theory, which has drawn together concepts of wellbeing from across the world to argue that the concept has three dimensions: “what a person has (the material), what they can do through their relationships with others (the relational) and how they feel and evaluate what they have and can do (the subjective)” [41] (p. 4). The relative importance of the dimensions is an area of contestation [38] with Austin [39] (p. 97), who argues for the core importance of relational wellbeing—“sociality” and “good social relationships”—as the “catalyst for overall wellbeing”.
When reflecting on this political focus on wellbeing, research has indicated that there is a misalignment between social care policy aspirations and the provision of telecare technology in England. Roberts and Mort [42] argued that first- and second-generation telecare systems focused on the monitoring aspect of care practice, with little consideration of what they termed the “social-emotional elements” of care (which correspond with the relational and subjective dimensions of wellbeing). Other studies have highlighted the commissioning and design of some TEC devices and services focused on supporting “ageing in place” and risk management, essentially requiring users to become housebound [43] and shifting the site of care from institutions to “extitutions” [44] with limited consideration of the ways technologies could contribute to the aspirations of users, including relational and subjective wellbeing [45]. The government-funded WSD randomized control trial also found that while users’ and their carers’ wellbeing was “enhanced”, it was not “transformed” [46,47,48,49], and yet it has been noted that these findings had little bearing on the continued policy enthusiasm for TECS [50,51] (Appendix A, note 3). Following the arguments of Keating et al. [41], in which the wellbeing of actors within care systems and the sustainability of said systems are linked, technology that enhances wellbeing should therefore contribute to sustainability. However, the way technologies in care arrangements have traditionally been commissioned and delivered in England appears to be out of step with the wider aims of care legislation focused on wellbeing, and in turn, this could be argued to curb technologies’ potential to support sustainable care arrangements.
An additional area of tension relates to the way policy discourse in England characterizes technologies as asocial, with entirely predictable and neutral outcomes. In contrast, technology in care settings has been characterized by authors influenced by Science and Technology Studies (STS) as a “complex intervention” [52] and a social phenomenon, with benefits that are contingent on both contexts and interactions with users [53,54]. Per this characterization, technologies’ outcomes are more conditional than presented in policy discourse in England. This gap between the presentation of technologies as producing very fixed and predictable outcomes versus the more variable results that may be experienced in practice could create an issue for those commissioning, designing, and using services, whose experiences may not correspond with the devices’ purported outcomes. An approach to technology that considers the importance of contextual factors and users in mediating outcomes is required [52] but is at odds with policy’s presentation of technology as a “silver bullet” [50] (p.1726). It also characterizes people who use technologies and care services as passive recipients rather than active stakeholders in a system that aspires to be grounded in the concepts of person-centred care and personalization.
Technology in English adult social care is therefore also at a crossroads. The vast majority of provision is currently delivered via analogue telephone lines and will therefore not be sustainable following the digital switchover taking place across the country. The replacement of these devices with digital equivalents is predicted to be extremely costly and not an economically sustainable option for many local authorities. There is now an opportunity to explore alternative devices and models of TECS delivery, and in this process, local authorities could investigate ways technologies could be used to contribute to wellbeing and sustainable social care rather than focusing on risk management and narrow conceptualizations of “ageing in place”.
This paper reflects on data collected as part of a project examining the potential of technologies to contribute to sustainable adult social care services and to wellbeing outcomes for those who receive support. Here, we focus on a particular area of emergent practice highlighted by our research: the use of mainstream technologies such as voice assistants, smart speakers, “wearables” (e.g., smart-watches, activity trackers), and other Internet of Things-enabled (IoT) devices [55] (Appendix A, note 4). These increasingly ubiquitous devices—in 2020, there were an estimated 10 Internet-enabled devices per household in the UK [56]—could be seen to represent Doughty et al.’s [32] third generation of telecare, which they predicted would utilize broadband and wireless technology to connect users to a “virtual neighbourhood” including health and social care professionals and facilitate social engagement. The aim of this paper was to provide insight into this nascent area of practice and research by elucidating the ways mainstream technologies are being deployed by English local authorities, the catalysts for their use, and their associated implications—including their potential to contribute to wellbeing outcomes and therefore sustainability—to identify key areas of learning. The paper is organized as per Figure 1 and addresses four questions:
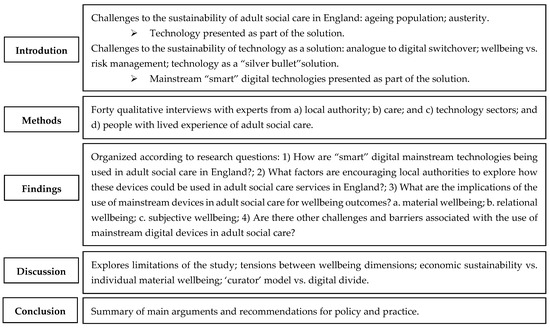
Figure 1.
Structure of the paper.
- How are “smart” digital mainstream technologies being used in adult social care in England?
- What factors are encouraging local authorities to explore how these devices could be used in adult social care services?
- What are the implications of the use of mainstream devices in adult social care for wellbeing outcomes?
- Are there other challenges and barriers associated with the use of mainstream digital devices in adult social care?
2. Materials and Methods
We present analysis of expert semistructured interviews (a mix of individual and group interviews) with actors from across local authorities, the care and technology sectors and people with experience of adult social care support. Our interviews (n = 40, 33 single and 7 group interviews, with 38 participants) were conducted in two rounds with four groups (24 interviews in spring 2020 and 16 interviews in winter 2020):
- local authority sector (13 interviews with 12 participants) from 9 English local authorities;
- technology sector (12 interviews with 9 participants);
- care sector (9 interviews with 6 participants);
- people with lived experience of adult social care services, unpaid carers, and their representative groups, including voluntary sector organizations (6 interviews with 11 participants).
We used a purposive sampling approach to capture a diverse range of experiences and perspectives from within the four groups. We also took advice from our project advisory board to create the initial participant list (with attention given to obtaining a diverse range of perspectives) and used a “snowball” sampling technique [57], asking participants who else they would recommend we approach to engage with the project. For the local authority participants, we recruited commissioners/TECS managers as key stakeholders with significant decision-making power in shaping TECS at the local level. As there is considerable variation in local authorities’ commissioning arrangements and policy and practice approaches [31], we used a purposive sampling technique to include different commissioning arrangements, governance structures, and internal expertise related to TECS. The technology sector too is diverse, and we strove to include the designers, manufacturers, and developers of a range of different types of technologies focused on care as well as associated service providers and “brokers” (mediating between technology providers and clients including local authorities). The care sector experts included providers from a range of different business and operational models as well as provider representative bodies and membership groups. For our sample of people with lived experience of adult social care services (including unpaid carers), we endeavoured to include a diverse mix of people in terms of age, gender, and ethnicity and also included interviews with staff from voluntary sector representative groups.
In our first phase of interviews, we utilized a topic guide focused on exploring the role of technologies in adult social care services, including developing trends, the catalysts for change, and the associated benefits or risks of new or emergent technologies in practice. These topic guides provided an “anchor” for the interviews, which were semistructured to allow for participants to raise issues they felt were pertinent. All interviews were recorded (with consent), transcribed, and analysed abductively [58]. We first coded the data deductively, with codes drawn from topic guides designed to explore issues related to our research questions (as set out above), and then inductively, to produce second-level codes to draw out additional complexities. We analysed data from the four groups separately before contrasting the codes produced to highlight areas of agreement and tension. We analysed the first phase of interviews as we continued to collect new data, reflecting on our emergent findings. This enabled us to pause once we reached a point of “meaning saturation” in our first phase of interviews, when we had not only “heard it all”, but “understood it all” [59] (p. 591). We then produced a short 1-page summary of our findings from the first round of interviews and returned to our experts, asking them to reflect on these with the aim of validating our data. For this phase, we returned to the majority of our phase 1 sample, and where this was not possible, we recruited additional participants with expertise on topics raised in the first round of fieldwork. Fourteen participants were interviewed in both rounds of interviews, with an additional seventeen participants took part only in round 1 and seven only in round 2. Following the completion of the second round of interviews, we returned to our initial coding frameworks for each expert group and refined them further. We then contrasted these frameworks to explore points of convergence and divergence in responses. As we explore below, the data indicated broad agreement across a number of areas related to the research questions, particularly among stakeholders from local authorities and the technology and care sectors (findings that echoed other studies of technology and care in England [45,60]). There were, however, some key areas of disagreement and tension, which we detail in the next section.
3. Results
3.1. How Are Smart Digital Mainstream Technologies Being Used in Adult Social Care in England?
In our fieldwork, we explored emerging trends and practice related to technology in adult social care and found many examples of local authorities piloting or trialling mainstream devices, including voice-controlled virtual assistants and smart speakers (e.g., Amazon’s Alexa, Echo, Dot, and Spot; Google’s Assistant and Home), wearables such as smart watches, and other IoT devices. Examples of pilots extended beyond the nine local authorities included in our sample, with participants from local authorities and the technology and care sectors citing practice from other areas of England and further afield. Table 1 includes some illustrative examples provided by these participants of technologies being piloted by local authorities in England. Smart speakers were a particular area of interest, experimentation, and investment for all the local authorities included in our sample, and participants from the local authority, care, and technology sectors cited further examples underway across adult social care in other geographical areas. Participants from local authorities that were exploring smart speakers were either using existing “skills” (voice-activated apps) not specific to care (for example, to turn off the lights or play music) or working with technology providers to develop bespoke care-related skills (for example, medication reminders; a messaging system between people receiving care and their carers; or a system for care workers to record care tasks).

Table 1.
Illustrative examples of pilots exploring the use of mainstream technologies in adult social care.
Enthusiasm for digital technologies had a trickle-down effect to care providers, as those delivering care commissioned by local authorities were increasingly required to include digital record keeping as part of their service. As such, care workers were often provided with a company smart phone or required to use their personal phone to record information about care visits via dedicated apps or platforms. These systems ranged in functionality from those focused on electronic call monitoring (to record the duration of care visits) to those that allowed care workers to log information on the content of care visits, including tasks completed, medication taken, fluid intake, and “softer” wellbeing outcomes.
In our interviews, people accessing care services and unpaid carers cited examples of how they or the people they cared for were using mainstream devices to make their lives easier. Participants spoke of controlling their home environment through voice-activated smart speakers, which meant that small tasks such as switching lights on and off no longer required the assistance of a caregiver. Examples were also given in which smartphones were used to facilitate financial arrangements through online banking and apps that allowed for easy payments when shopping. Table 2 outlines the ways in which the four expert groups’ responses regarding the uses of mainstream digital technologies in adult social care were in agreement or disagreement.

Table 2.
Research question 1—summary table of convergence and divergence between expert responses.
3.2. What Factors Are Encouraging Local Authorities to Explore How These Devices Could Be Used in Adult Social Care Services?
In our interviews, we also explored the factors the experts felt were influencing the use of mainstream technologies in adult social care. This was an area of divergence among the stakeholder groups, with those using services reflecting on their own personal reasons for the use of these devices as opposed to the external factors influencing change as cited by the experts from the local authority, care, and technology sectors (Table 3). For example, some commissioners and technology sector experts felt the digital switchover offered an opportunity to redesign services and was the catalyst for increased interest in use of smart technologies in adult social care. The costs of replacing analogue TEC devices with digital versions were considered unsustainable; one local authority included in our sample estimated that transferring its existing 4000 users of analogue TECS to digital alternatives (SIM-enabled devices) would cost in excess of GBP 230,000. For some local authorities, the switchover had prompted new thinking, which included exploring ways of integrating mainstream devices into their services. However, among technology experts, there was a concern that some local authorities were viewing the digital switchover as an insurmountable challenge that would widen geographical variation in services rather than an opportunity to redesign services. One remarked: “there’s still a lot of councils out there that are in a ‘box-ticking’ exercise, and the pendant alarm ticks that box. And it’s one less thing for them to—they’ve performed their duties, for the citizens of their locality. Are they giving them the best service? No. It’s a pendant that’s probably sat in a drawer somewhere that’s never ever going to be used” (round 1, participant 15, technology provider). This approach created frustration for those working in technology sector, who were reliant on commissioners of services as gatekeepers to the adult social care market.

Table 3.
Research question 2—summary table of convergence of divergence between expert responses.
In addition to the digital switchover, two further drivers were cited as initiating interest in mainstream devices by the local authority, care, and technology sectors. First, national and some international (e.g., European Union) funding opportunities for “experimentation” had been used several local authorities included in our sample to trial and pilot new technologies, including mainstream devices. This was argued to be a low-risk way of trialling devices and new partnerships with technology and homecare providers. These had a ripple effect, with other local authorities subsequently trialling similar approaches they heard about via professional networks, representative bodies and funders.
The experts interviewed from the local authority, care, and technology sectors also cited the COVID-19 pandemic as a catalyst for change in local authority TEC policy and practice, with mainstream technologies used to connect service users to health and social care professionals and wider caring networks or hobbies. One local authority commissioner said the pandemic “gave us a real political focus, allowed us to support the areas like adults that were really progressing the use of technology, and frankly to challenge and to encourage—kick up the backside—whatever you want to say, areas that weren’t adopting quite so well” (round 1, participant 3, commissioner). Experts from the care sector also reported accelerated technology use, including use of mainstream devices to conduct virtual care visits, training, and staff meetings. The experts interviewed with lived experience of care services and their carers also felt the COVID-19 pandemic had increased mainstream technology use not only by themselves, as some of their support services moved online, but also more broadly as social distancing requirements in England necessitated a greater use of digital technologies to “stay connected”, with previously “technology-averse” populations starting to use digital devices. They also argued the cost and design of specialist equipment, compared with those of mainstream devices, were factors influencing their use in caring contexts, with the latter argued to be both cheaper and more aesthetically pleasing.
3.3. What Are the Implications of the Use of Mainstream Devices in Adult Social Care for Wellbeing Outcomes?
There was agreement across all expert groups interviewed that mainstream devices have the potential to enhance the wellbeing of people using adult social care services, an important consideration for local authorities because of the requirements of the 2014 Care Act. Some experts from the local authority, technology, and care sectors felt analogue TECS had served a purpose in terms of keeping people safe, but that there were now opportunities created by the catalysts outlined above to explore how technologies could contribute to other outcomes, including wellbeing. Using the three-dimensional model of wellbeing outlined in Section 1.3, we explored how participants discussed the potential of mainstream devices to support people in ways that either enhanced or did not damage their wellbeing (summarised in Table 4).
3.3.1. Material Wellbeing
Reflecting on the material dimension of wellbeing, there were some tensions between the perspectives of the different expert groups interviewed. While at the macro-level, the potential for mainstream devices to contribute to the economic sustainability of social care arrangements was highlighted by participants from all expert groups, some also emphasized potential implications for material wellbeing at the micro-level. At the macro-level, among the experts who received local authority-funded care, there were examples of how they had used mainstream devices to deliver cost savings in terms of their allocated “care packages” of support; one family carer provided an example of how the annual care package costs for the person she supported had been more than quartered through the use of technologies, including mainstream devices. These savings, when scaled up across local authorities, were cited by local authority commissioners as a key benefit of using mainstream devices in their services. For example, within our local authority sample, one had been at the forefront of using mainstream technologies in adult social care, having been the first local authority to trial smart speakers. In a state-funded pilot of 50 people, savings were reported in excess of GBP 60,000 by reducing short, in-person care visits. This approach was subsequently publicized as an exemplar across local authorities and the technology sector and was therefore cited by experts interviewed from these groups.
A further, and related, way that the use of mainstream devices were proposed by commissioners as a potential means of contributing to macro-level economic sustainability was raised by some local authority commissioners, who said they were considering the savings that could be generated by “nudging” users to buy their own multipurpose, consumer digital devices and providing (or recommending) apps, or assisting them to make fuller use of devices they already owned, rather than providing large-scale TECS. One commissioner how the local authority role would shift to “becoming the curators of knowledge as opposed to deliverers of service” (round 1, participant 11, commissioner). This, other commissioners agreed, was a more economically prudent option, as “from a cost point of view, pushing out an app onto existing devices is where we want to be. I don’t want to give people physical Android phones or handsets that are then going to be out of date in three years and I have to update” (round 2, participant 9, commissioner).
However, the shifting role of local authorities from “providers” to “curators” did raise issues related to the “digital divide” (Appendix A, note 5) in access to these technologies, as some participants, including from the local authority expert group, noted that though cheap when compared to specialist equipment, some people may be excluded from mainstream devices’ benefits because of their cost and the expense of the Internet connectivity they required. Thus, the curator model and “nudging” people needing care toward purchasing mainstream devices could have potential implications for some users’ material wellbeing.
3.3.2. Relational Wellbeing
Turning to relational wellbeing, again, there was tension in the balance between supporting this aspect of wellbeing for people using care services and the aim of local authorities to achieve economic sustainability. In discussing the deployment of mainstream devices in adult social care, some experts from the local authority, care, and technology sectors used arguments that echoed the policy discourse in relation to technology’s capacity to free up scarce workforce resources at a time when demand is outstripping supply. One commissioner explained the potential benefits of using mainstream technologies to perform “checking” care visits remotely via video calling: “we’ve got massive financial pressures; I would never underplay that. But our single biggest pressure is people and staffing […] if we can free up staff time, that is every bit as valuable as actually making a cashable saving” (round 2, participant 15, commissioner). There was some agreement from people who used services and carers interviewed that technologies could contribute to independence and reduce the need for formal care that may be intrusive, but there were concerns regarding the potential unintended consequence of social isolation when using technology to replace care visits. Experts with lived experience of care services highlighted examples of when they had used mainstream devices to connect with others by choice, but also raised concerns about the wellbeing of those who were more socially isolated, for whom even short care worker visits may be the totality of their social contact. Mainstream devices were not seen as a good substitute in these contexts. One commissioner too noted the replacement of care visits for particularly isolated people could be a short-sighted strategy: “there are financial savings with technology—if you do something with a piece of equipment rather than a human being, it’s cheaper, immediately. However, what you then have is the impact around social isolation and everything else, that kind of bites you later on” (round 1, participant 8, commissioner). From the care sector, some experts argued that rather than replace all care visits, there was the potential to use technologies to perform checking tasks with a view to saving up the time allocated to create longer, more meaningful visits.
3.3.3. Subjective Wellbeing
The ability of mainstream devices to support people needing care without damaging their sense of self was highlighted as a key benefit across all stakeholder groups. One care sector expert explained that “nobody wants to wear pendant alarms, most of the time they end folded up in the sock drawer because they stigmatize people” (round 2, participant 22, care sector), whereas mainstream devices were comparatively more “everyday”. For the people we interviewed with lived experience of adult social care services, mainstream technologies could offer independence and control; one highlighted how they used smart speakers to control their lighting, allowing them to turn the lights off and on once their care worker had left. It was important for those using adult social care services to have the choice to blend together their own mix of specialist and mainstream technologies alongside other forms of support, but for the reasons outlined in the following section, this is currently at odds with practice in the sector, which requires approval before purchasing equipment using state-provided resources, with narrowly defined outcomes.

Table 4.
Research question 3—summary table of convergence and divergence among expert responses.
Table 4.
Research question 3—summary table of convergence and divergence among expert responses.
| How Can Mainstream Devices Be Used in Adult Social Care to Contribute to Wellbeing Outcomes? | |||
|---|---|---|---|
| Expert Group | |||
| Local Authorities | Technology Sector | Home Care Sector | People Who Use Care Services and Carers |
| |||
3.4. Are There Other Challenges and Barriers Associated with the Use of Mainstream Digital Devices in Adult Social Care?
When reflecting on the potential for mainstream technologies to contribute to wellbeing, there was an overarching challenge emphasized by the participants who used services related to the attitude of some staff working within local authorities to “choice” broadly and technologies specifically. Some of the participants were receiving publicly-funded support through Direct Payments—a mechanism intended to deliver person-centred care and choice (Appendix A, note 6)—but stressed that they still had to negotiate with local authorities to purchase anything, including technologies. There was a consensus among those with experience of adult social care that technologies were seen as “luxuries” rather than necessities by local authorities. Even when a “business case” could be demonstrated by comparing the costs of relatively cheap technologies versus other types of support, participants with experience of care still found it hard to persuade “risk-averse” local authorities to consider devices outside of their commissioning framework. This narrow, prescriptive approach to technologies was argued to ignore their potential to deliver wellbeing outcomes, as one family carer interviewed explained: “They never ask the question about what impact has technology had on someone’s life. So people get technology but then they don’t know how does this support your wellbeing. They just don’t ask these questions. You know there’s no relationship between the technology and wellbeing because they don’t ask the question” (round 2, participant 38, family carer). It would therefore appear that for some people receiving services, the deployment of mainstream technologies was on the margins of practice—being piloting and trialled—rather than part of wider local authority approaches or TECS strategies.
In the interviews, experts raised other challenges related to the use of mainstream technology in adult social care. The digital divide explored in relation to the material dimension of wellbeing in Section 3.3.1 extends beyond the capacity to pay for technologies or Internet connections. Regardless of individual resources, the inequality in access to good-quality Internet connections across England [9] presents a further challenge, as mainstream digital devices require broadband of good speed and quality or 4/5G infrastructure to function securely and reliably. This issue was highlighted by some experts interviewed, and there were local authorities interviewed and cited as examples with which these issues were being tackled through the installation of LoRaWAN (Long Range Wide-Area Network] for IoT devices and 5G mesh networks to enable users to connect digital devices without additional Internet connection costs, facilitating use of digital devices in adult social care by both people using services and care providers.
The digital divide also encompasses issues related to the skills and confidence to use technologies. Experts interviewed from all four groups noted that the marketplace for technologies was confusing for local authorities, care providers, and people who needed care and support. For that reason, some experts argued some people needed assistance to select appropriate technologies, and although mainstream digital devices are increasingly prevalent and purportedly “user-friendly”, there were concerns some people may lack the ability, skills, and confidence to utilize them, particularly older adults. There was thus a risk that some people in need of care and support would be left behind as services become increasingly digital. Care sector experts also highlighted the digital divide within the care workforce in terms of skills, with some care workers less comfortable and familiar with technologies, including mainstream devices.
Ethical and privacy implications, in particular in relation to the ownership of and access to the data mainstream technologies capture, were raised by some of the experts interviewed, and there were discussions as to whether when devices were provided by local authorities, there was a duty to ensure people understood how their data were being used and stored. One technology sector expert highlighted the risks associated with the use of mainstream devices in care due to the general lack of understanding required to give informed consent to issues related to data usage, as well as what he felt was the “unacceptable” monetization of personal data by organizations manufacturing these devices. However, some local authority commissioners felt issues of privacy and data governance could be “bypassed” because of the “consumer” relationship between service users and their mainstream devices under the “local authorities as curators” model, but were more wary when considering providing devices directly to people: “the way we’ve worked round that [issues of data ownership] at this point in time is that we’ve tried to encourage self-funders to buy the equipment for their own loved ones and for themselves because they made the choice about how they’re going to use and share the data. I think we feel that if we’ve provided it, yeah then we’re in a trickier position in terms of consent, because that’s what it’s about, consent for that use and I think […] we’re not quite there yet” (round 2, participant 5, commissioner).
A significant issue with some local authority approaches taken in practice to the use of mainstream devices in adult social care relates back to third challenge raised by traditional TECS provision in England in Section 1.3. It was apparent during the interviews that there was a tendency among some commissioners both within the sample and, as argued by the experts interviewed, more broadly across the adult social care sector, to focus on devices as “silver bullet” solutions, thereby neglecting the social nature of technologies and the importance of context and the wider services in making technologies “care”. For example, the commissioner from the local authority interviewed that had first trialled these devices emphasized caution in assuming that mainstream devices could simply produce economic sustainability and free up staff time, noting that, if provided as part of adult social care, seemingly standalone and intuitive mainstream technologies still needed to be installed and maintained. The commissioner argued that with a narrow focus on the functionality of the devices alone, there was a risk of “a complete underestimation of the amount of effort that’s required to make it happen […] we’ve shown really clearly the level of support people need on [an] ongoing basis is quite severe” (round 1, participant 11, commissioner), with both cost and workforce implications. This underestimation of the wraparound services needed alongside mainstream devices was highlighted by other local authority commissioners, who cited examples of the deployment of devices without consideration of the ongoing assistance users may need, or indeed of whether they had the Internet at home to enable them to function, resulting in the “failure” of pilots and trials as the technologies were abandoned or underutilized (see Table 5).

Table 5.
Research question 4—summary table of convergence and divergence among expert responses.
4. Discussion
This paper examined the use of mainstream smart digital technologies as an emerging area of policy and practice in adult social care in England, contributing to an accordingly burgeoning area of research. There are some limitations to our research, including the small sample size for each expert group. Our sample is therefore not representative of all 152 local authorities with responsibility for adult social care delivery, all care or technology providers, or all people with experience of receiving adult social care services or caring. We therefore cannot provide a definitive account of the deployment of mainstream technologies in adult social care—and, influenced by STS, we argue technologies’ and their outcomes are always more complex than “good” or “bad” [54]—but aim to open discussion as to the possible implications for their use, which are likely to continue to be pertinent as their integration into adult social care services becomes more widespread. It is also important to highlight here that the focus of the paper was on the potential of the ways these devices were being deployed to enhance or damage the different dimensions of wellbeing rather than the inherent functionality of the devices.
Our data highlighted that smart devices, including phones, voice-activated speakers, wearables, and environmental controls, are an area of increasing experimentation and use in commissioned services, by care providers, and by people who draw on support. The cost of replacing analogue TECS with digital versions as the former become unreliable, funding opportunities, and the “accelerating” effect of the COVID-19 pandemic encouraged local authorities and care providers to explore the potential of mainstream devices in care settings, while those who use services found them to be more affordable and visually pleasing than specialist equipment.
Although mainstream devices are currently the focus of investment in terms of pilots and trials, our interviews with people who use care services and their carers suggested that in practice, they remain on the periphery of service delivery in many local authorities. Many of the participants who had experience of receiving statutory social care support, including via Direct Payments, which ostensibly facilitate choice and control, found their options regarding technologies narrowly confined by local authorities’ commissioning practices or expectations as to which devices were for care and which were a “luxury” and therefore outside of their remit. This approach is at odds with the person-centred way wellbeing itself is framed within English social care legislation and perpetuates the issues Pols and Willems [54] highlighted related to telecare, i.e., tensions between the “promises” of telecare (meeting the demands of an ageing population, replacing in-person care visits, improving efficiency) and the “local goals” of individual users (improving the quality of care).
All expert groups interviewed viewed the use of mainstream digital devices in adult social care largely positively, though with some important caveats. Using a three-dimensional model of wellbeing as the conceptual lens through which to explore mainstream technologies’ potential role in adult social care systems [40,41], we now reflect on the implications of this emerging area of practice for each dimension in turn.
When exploring the benefits of these devices, expert responses aligned most strongly in relation to the subjective and relational dimensions of wellbeing, and as such, there were examples cited of how when used to connect with others and to enable independence and choice. Mainstream devices were being used in ways that went beyond the “monitoring” aspect of Roberts and Mort’s [42] three distinct domains of care practice to deliver “social–emotional care”, shifting the role of technology in English adult social care away from the risk-focused delivery model that dominated first- and second-generation telecare services. Experts from all groups argued that mainstream devices were less stigmatizing than traditional telecare devices and could support users to connect with others in a dialogue rather than purely to summon help.
However, there were key areas of tension where rather than enhancing aspects of wellbeing, some of the ways in which mainstream devices were being used in adult social care arrangements presented additional challenges. For example, some experts from the care and technology sectors and local authority commissioners argued that by replacing short care visits with mainstream devices, there was the potential to free up care staff time and ultimately reduce costs. When used in this way, some experts interviewed, in particular those who used services, raised the risk that the replacement of care visits by care workers with mainstream devices could exacerbate the social isolation of some people, thereby damaging their relational wellbeing, as has been highlighted as an issue in other research on telecare [42]. This is a particularly important consideration, as relational wellbeing has been argued to underpin all other elements that make up the concept [39], and loneliness has been linked to poor health outcomes, thereby increasing the use of health and social care services [61].
In our interviews, inequalities of access to mainstream devices raised important issues related to the way these technologies were being integrated into adult social care. Among our sample, some commissioners of services were exploring mainstream technologies with a view to nudging people to purchase their own equipment or harnessing devices people may already have. Our data underscored the possible repercussions of this curator model on material wellbeing, including the potential to perpetuate or generate inequalities, with those on low incomes or without necessary connectivity excluded from accessing local authority services, including care, delivered via mainstream devices [62]. Though mainstream smart devices are seemingly ubiquitous, there are still digital divides in access in England. For example, data indicated that 46% of people with a disability in Great Britain had used an IoT device or system within the previous three months, compared with 68% of people without a disability [63]. The same data highlighted that though almost half of adults in Great Britain aged 25 to 34 years used a virtual assistant smart speaker or app within the last three months, this fell to 17% of those aged 65 years and over; while 84% of all adults in Great Britain used a smart phone, for those aged over 65, only 53% did [63]. The aspiration of some local authorities that they could harness devices already in people’s homes may therefore be more challenging for certain population groups. Cost as a barrier also varies across different groups. While 8% of all age groups indicated that costs were an issue that had prevented their use of IoT devices, for those aged 25–34, this rose to 15% [63]. Therefore, for some people who require support, the curator model may contribute to care systems’ economic sustainability at the expense of their material wellbeing.
Wright described the curator model as part of a shift in the balance of rights and responsibilities between citizen and state, creating the term “the Alexafication of adult social care” [55] (referring to Amazon’s Alexa smart speaker) in which “[i]n piloting new consumer technologies such as smart speakers, some LAs [local authorities] seem to be piloting new versions of what a LA can and should be in the future, in relation to its citizens […] LAs may find their role becoming closer to that of an app developer and data broker than a commissioner of social care services, to some extent mediating and facilitating the monetization of a consumer relationship between powerful technology companies and citizens for the purposes of care” [55] (pp. 11,12) (Appendix A, note 7). A key area of responsibility associated with the use of mainstream devices in adult social care is understanding the data sharing and privacy implications of using these technologies; some commissioners felt that privacy and data ownership issues would be addressed through the consumer relationship between users and the companies supplying mainstream devices, but the wider literature has highlighted limited public awareness of how smart speakers process (via human review) and store data (routinely uploading it to the Cloud) [64,65,66]. Therefore, there needs to be a wider discussion as to whether, when encouraging users to bring these devices into caring arrangements, local authorities should ensure that people using services adequately understand the data and privacy implications [67]. Data indicated that concerns regarding security, privacy, and protection of personal data are barriers to the use of IoT devices and, again, are not evenly distributed across the population. More than half of those with a disability cited these issues as reasons for not using IoT devices and systems within the previous three months, compared to a third of adults without a disability [63]. Awareness of IoT devices more generally appears to be an issue for older adults, with almost a third of those aged over 65% and 23% of people with a disability indicating that they did not know how to use IoT devices or systems or were not aware of them compared with 17% of the population generally [63].
There is also a key area of tension between a curator model of delivery on the one hand and the narrow, paternalistic approach to technologies as described by those with lived experience of care services in our sample. Both approaches have risks: the latter has possible implications for the subjective and relational dimensions of wellbeing and is at odds with the spirit of the Care Act, while the curator model assumes that all population groups are au fait with smart devices and shifts the responsibility for resourcing and understanding the ethical and privacy implications onto people who need care and support. In the context of the English social care system, which includes a means test, the deciding factor as to who is exposed to which risks could then be related to peoples’ the ability to resource their own care. For those who can, adult social care is shifting to a model in which it will facilitate the integration of a wider range of technologies into personalized caring arrangements (but with the associated risks borne by users), and for those who cannot, their options for technologies could be more limited and prescribed. From the use of mainstream devices in adult social care, a new divide could potentially emerge as an unintended consequence. However, a potential way forward was included in the recent white paper on adult social care reform [6] which outlined the aspiration that Disabled Facilitates Grants (DLGs)—available to disabled people to make adaptions to their homes—will be used to purchase “affordable technologies that can help make someone’s home environment easier to use” (p. 38), including smart devices. The paper acknowledges that these kinds of purchases are already technically permitted via DLGs, but poor awareness means that in practice, the vast majority fund accessible showers and stair lifts.
The way some local authorities were deploying mainstream devices in practice raised a further challenge. Stepping back from the curator model to one in which local authorities directly provide mainstream devices, their merit of being “affordable” aligns with the way technologies are conceptualized and presented in policy discourse as standalone solutions for an overstretched system. However, this limits their potential to contribute to wellbeing and other outcomes, including, paradoxically, economic sustainability. We heard from our experts about local authorities that had taken a “tech-first” approach, purchasing relatively affordable devices without full consideration of the wider costs required for the wraparound services to support their use, which in turn led to the “failure” of the technologies [29]. As studies that have drawn on STS to explore first- and second-generation TECS have underscored, the services associated with these devices—assessment, installation, monitoring, response—enable technologies to “care”. For example, people who work in telecare monitoring centres who answer calls when alerts are triggered “act as the ‘glue’ providing the all-important link between otherwise fragmented services” [68] (p. 79) and have been found to “co-produce care” alongside unpaid carers and installation and response staff. Drawing on this wider literature related to TECS and our findings, we argue that the potential of mainstream devices to contribute to saving of financial and workforce resources is contingent on factors that extend beyond a focus on individual devices and their functionalities: there needs to be full consideration of the services needed to facilitate their use. These wraparound services require both financial investment and staff time, which are challenging for local authorities under significant financial and workforce pressures. However, there is a risk that underestimating the importance of wraparound services will waste resources, as some users will either abandon technologies or be unable to take full advantage of any benefits. As Stirling and Burgess [60] noted in a recent paper exploring smart digital TEC devices, “[t]he technology won’t work on its own” (p. 52). If there is no provision of wraparound support, there is also a risk that unpaid carers will be burdened by additional tasks, as has been highlighted in research exploring telecare [69]. This could then be argued to create an imbalance between the wellbeing of actors within care ecosystems and arrangements, which affects sustainability [41] and could create costs in the long term as unpaid carers themselves require the support of adult social care following “burnout”.
5. Conclusions
The use of mainstream devices in adult social care in England is a growing area of practice and, given the attention paid to it in the adult social care white paper, is likely to continue to expand. Social care in England has been described as being “in crisis” because of increased demand for care at a time when the supply of both paid and unpaid care is not keeping pace. Widespread cuts to public services have also had implications for the sustainability of the social care system in England. Policy has framed technology as a potential means to address some of these sustainability challenges by saving costs, freeing up care workforce time, and improving outcomes, yet the sustainability of much of England’s TECS is being challenged by the switchover from analogue to digital connectivity. Political enthusiasm for the potential of technology, and more recently digital devices and systems, to support care arrangements has been reflected in investment, with funding opportunities for local authorities and care providers.
Influenced by STS, we conceptualize technology as a social phenomenon with outcomes that are ultimately contingent and coproduced with both users and contexts. As such, our aim in this paper was not to make an assessment as to whether any technologies are inherently “good” or “bad”. We instead explored the various ways smart digital mainstream technologies are being incorporated into practice in adult social care settings and the rationales, benefits, and challenges attributed to how they are being deployed and used. In our expert interviews, we heard about examples of mainstream devices being deployed in ways that went beyond traditional, risk-focused TECS to support dimensions of wellbeing. However, the data also revealed tensions and trade-offs among the dimensions of wellbeing and unintended consequences and challenges related to the ways mainstream devices were being used in services. For example, just as mainstream devices could reduce the need for what some people who need support might see as intrusive in-person care visits, for others, these visits could be a vital source of interaction. Thus, the ability of users to personalize their care arrangements, including whatever technologies support their wellbeing, is an important consideration for future practice. A curator model—with local authorities guiding citizens through a confusing marketplace or advising how devices they already own could be turned to the task of care—could arguably facilitate personalization but if the ability to choose is contingent on the ability to purchase technologies and the skills to use them, some people will be excluded because of the various levels of the digital divide [70]. A curator model therefore has the potential to widen inequalities between people who need care, with some facing disproportionate risks, responsibilities, and costs while others are closed off from co-creating their own care arrangements by prescriptive commissioning practices.
Another key finding with implications for practice is that mainstream devices, as with all technologies deployed in caring contexts, need the full consideration of and investment in the necessary wraparound services, which include installation, ongoing support, and skills. This then presents a paradox: among the experts interviewed, there was hope that these devices would save costs and workforce resources, yet in order for them to be deployed effectively, technologies require the investment of funds and staff time. We argue for a person-centred, outcomes-focused approach, moving the focus beyond the cost savings mainstream devices could generate to include careful deliberation of the implications for wellbeing, inequalities, risks, rights, and responsibilities as well as the ongoing support required.
Funding
The author gratefully acknowledges the support the (U.K.) Economic and Social Research Council (ESRC) for the Sustainable Care: connecting people and systems programme (grant reference: ES/P009255/1, 2017-21, principal investigator: Professor Sue Yeandle, University of Sheffield).
Institutional Review Board Statement
The study was approved by the was approved by the University of Sheffield Research Ethics Committee (reference number: 026350); received the ADASS endorsement (reference number: RG19-08) and the University of Sheffield research governance sponsorship (reference number: 148644); and followed relevant local authority research governance procedures (where applicable).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
Data are available through the UK Data Service ReShare portal: reshare.ukdataservice.ac.uk/855010/, accessed on 20 January 2022.
Acknowledgments
The author acknowledges the contributions of James Wright to the fieldwork this paper draws on. The author would also like to thank Sue Yeandle for her feedback on a draft version of the paper. Thanks also go to the those who participated in the expert interviews.
Conflicts of Interest
The author declares no conflict of interest.
Appendix A
Note 1: Sustainability is often conceptualized in line with the United Nation’s Sustainable Development Goals, which aim to create a balance among economic, social, and environmental sustainability, with consideration of the long term and implications for future generations. Arguments have been made for greater consideration of the social and environmental aspects of sustainability in social care in England rather than a primary focus on economic sustainability [71].
Note 2: The WSD findings related to telecare indicated “no statistically significant” differences between the intervention and control groups in terms of admissions to residential care or to hospital [46] and no demonstrable cost savings [47].
Note 3: The ATTILA trial also found that telecare did not increase the length of time that people with dementia were able to live at home or decrease caregiver burden, depression, or anxiety [72].
Note 4: Our fieldwork took place in 2020, and the use of these devices was subsequently included in the personal stories woven through in the recent white paper on adult social care reform [6].
Note 5: The digital divide can be conceived as comprising different levels: the first relating to access to technologies and the second to the skills to use technologies [70]. There are also disparities in the digital infrastructure across England, with variation in the availability of high-quality broadband and 4G/5G connectivity [9]
Note 6: Direct payments refer to cash payments from local authorities that allow individuals to arrange and pay directly for their own care. They can include the purchase of equipment, but the local authorities must be satisfied that the chosen technology would meet a person’s needs and desired outcomes.
Note 7: Wright [55] also highlighted wider ethical considerations related to economic sustainability when considering mainstream devices. While they may appear to deliver costs savings for local authorities, Wright highlighted that the “affordability” of some mainstream devices reflects their manufacturers’ relationships with taxation systems; thus, as they appear to give the gift of cost savings to adult social care, they do so by avoiding contributing to the system further “upstream” through taxation. There are also issues regarding the manufacturing practices of smart mainstream devices that raise questions related to both social and environmental sustainability [67].
References
- Glasby, J.; Zhang, Y.; Bennett, M.R.; Hall, P. A lost decade? A renewed case for adult social care reform in England. J. Soc. Policy 2021, 50, 406–437. [Google Scholar] [CrossRef]
- Sustainable Development Unit. Sustainable, Resilient, Healthy People & Places. A Sustainable Development Strategy for the NHS, Public Health and Social Care System; NHS England/Public Health England: London, UK, 2014. [Google Scholar]
- Gray, A.M.; Birrell, D. Transforming Adult Social Care; Policy Press: Bristol, UK, 2013. [Google Scholar]
- HM Government. The Care Act 2014, c. 23. 2014. Available online: http://www.legislation.gov.uk/ukpga/2014/23/contents/enacted (accessed on 4 April 2018).
- Hall, P.; Needham, C.; Hamblin, K. Social Care. In Handbook of Society and Social Policy; Ellison, N., Haux, T., Eds.; Edward Elgar: Cheltenham, UK, 2020. [Google Scholar]
- Department of Health and Social Care (DHSC). People at the Heart of Care: Adult Social Care Reform White Paper; HSMO: London, UK, 2021. [Google Scholar]
- ONS. Subnational Population Projections for England: 2018-Based. 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/subnationalpopulationprojectionsforengland/2018based (accessed on 9 December 2021).
- ONS. Births in England and Wales: 2020. 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2020 (accessed on 9 December 2021).
- Hamblin, K. Care System, Sustainability: What Role for Technology? An Evidence Review; Sustainable Care Paper 3; University of Sheffield: Sheffield, UK, 2020. [Google Scholar]
- Jagger, C. Trends in Life Expectancy and Healthy Life Expectancy; Government Office for Science: London, UK, 2015. [Google Scholar]
- Kingston, A.; Comas-Herrera, A.; Jagger, C. Forecasting the care needs of the older population in England over the next 20 years: Estimates from the Population Ageing and Care Simulation (PACSim) modelling study. Lancet Public Health 2018, 3, e447–e455. [Google Scholar] [CrossRef] [Green Version]
- Carers UK. Facts about Carers: Policy Briefing; Carers UK: London, UK, 2019. [Google Scholar]
- National Audit Office (NAO). Adult Social Care at a Glance. 2021. Available online: https://www.nao.org.uk/wp-content/uploads/2021/03/The-adult-social-care-market-in-England.pdf (accessed on 19 January 2022).
- ONS. Childbearing for Women Born in Different Years, England and Wales: 2017. 2018. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/conceptionandfertilityrates/bulletins/childbearingforwomenbornindifferentyearsenglandandwales/2017 (accessed on 4 July 2019).
- Department of Communities and Local Government (DCLG). Household Projections, 2008 to 2033 England; DGLC: London, UK, 2010. [Google Scholar]
- Age UK. Evidence Review: Loneliness in Later Life; Age UK: London, UK, 2014. [Google Scholar]
- Skills for Care. The State of the Adult Social Care Sector and Workforce in England. 2020. Available online: https://www.skillsforcare.org.uk/adult-social-care-workforce-data/Workforce-intelligence/publications/national-information/The-state-of-the-adult-social-care-sector-and-workforce-in-England.aspx (accessed on 27 April 2021).
- Turnpenny, A.; Hussein, S. Recruitment and Retention of the Social Care Workforce: Longstanding and Emerging Challenges during the COVID-19 Pandemic; PSSRU: Canterbury, UK, 2021. [Google Scholar]
- Luchinskaya, D.; Simpson, P.; Stoye, G. UK health and social care spending. In Institute for Fiscal Studies (IFS) Green Budget 2017; Emmerson, C., Johnson, P., Joyce, R., Eds.; Institute for Fiscal Studies: London, UK, 2018; Available online: https://www.ifs.org.uk/publications/8879 (accessed on 21 August 2019).
- Phillips, D.; Simpson, P. National Standards, Local Risks: The Geography of Local Authority Funded Social Care, 2009–2010 to 2015–16; The Institute for Fiscal Studies: London, UK, 2017. [Google Scholar]
- Department of Health [DH]. Building Telecare in England; TSO: London, UK, 2005. [Google Scholar]
- DH. Shaping the Future of Care Together; TSO: London, UK, 2009. [Google Scholar]
- DH. Our Health, Our Care, Our Say: A New Direction for Community Services; TSO: London, UK, 2006. [Google Scholar]
- DH. Concordat between the Department of Health and the Telehealth and Telecare Industry; TSO: London, UK, 2012. [Google Scholar]
- Department of Health and Social Care (DHSC). Policy Paper: COVID-19: Our Action Plan for Adult Social Care; HMSO: London, UK, 2020. [Google Scholar]
- HM Government. Building the National Care Service. 2010. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/238441/7854.pdf (accessed on 21 March 2019).
- Hancock, M. My Priorities for the Health and Social Care System, speech 20 July 2018. Available online: https://www.gov.uk/government/speeches/matt-hancock-my-priorities-for-the-health-and-social-care-system (accessed on 8 March 2021).
- Javid, S. Using the Power of Technology to Make the World a Safer and Healthier Place. Keynote speech at the Founders Forum Health Tech Summit, London Tech Week 21st September 2021. Available online: https://www.gov.uk/government/speeches/using-the-power-of-technology-to-make-the-world-a-safer-and-healthier-place (accessed on 19 January 2022).
- Hamblin, K. Technology in care systems: Displacing, reshaping, reinstating or degrading roles? New Technol. Work. Employ. 2022. Online First. [Google Scholar] [CrossRef]
- ADASS. ADASS Spring Survey 2021. 2021. Available online: https://www.adass.org.uk/adass-spring-survey-21 (accessed on 10 February 2022).
- Wright, J.; Hamblin, K. England. In Care Technologies for Ageing Societies: An International Comparison of Care Systems; Hamblin, K., Lariviere, M., Eds.; Policy Press: Bristol, UK, forthcoming.
- Doughty, K.; Cameron, K.; Garner, P. Three generations of telecare of the elderly. J. Telemed. Telecare 1996, 2, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Fisk, M.J. Social Alarms to Telecare: Older People’s Services in Transition; Policy Press: Bristol, UK, 2003. [Google Scholar]
- TSA. Connecting People, Improving Lives: A Digital Future for Technology Enabled Care. 2017. Available online: https://www.tsa-voice.org.uk/downloads/content_from_old_site/tsa301664_whitepaper_oct17_120917_online_version_only.pdf (accessed on 4 July 2019).
- Wright, J. Technology in Social Care: A Review of the UK Policy Landscape; University of Sheffield: Sheffield, UK, 2020. [Google Scholar]
- TSA. OfCom 800 MHz and 2.6 GHz Competition Assessment and award Proposals Telecare Services Association Position; TSA: Wilmslow, UK, 2011. [Google Scholar]
- Cruickshank, J.; Trim, H. Inform Report: Care Technology Landscape Review, Socitm Inform and Socitm Advisory for Essex County Council; Soctim Inform: Northampton, UK, 2019. [Google Scholar]
- Bache, I.; Reardon, L. The politics and Policy of Wellbeing: Understanding the Rise and Significance of a New Agenda; Edward Elgar Publishing: Cheltenham, UK, 2016. [Google Scholar]
- Austin, A. A Universal Declaration of Human Well-Being; Springer International Publishing: New York, NY, USA, 2020. [Google Scholar]
- McGregor, J.A. Reconciling Universal Frameworks and Local Realities in Understanding and Measuring Wellbeing: The Politics of Wellbeing; Palgrave Macmillan: Basingstoke, UK, 2018. [Google Scholar]
- Keating, N.; McGregor, J.; Yeandle, S. Sustainable care: Theorising the wellbeing of caregivers to older persons. Int. J. Care Caring 2021, 5, 611–630. [Google Scholar] [CrossRef]
- Roberts, C.; Mort, M. Reshaping what counts as care: Older people, work and new technologies. Alter 2009, 3, 138–158. [Google Scholar] [CrossRef]
- Aceros, J.C.; Pols, J.; Domènech, M. Where is grandma? Home telecare, good aging and the domestication of later life. Technol. Forecast. Soc. Change 2009, 93, 102–111. [Google Scholar] [CrossRef]
- Milligan, C.; Roberts, C.; Mort, M. Telecare and older people: Who cares where? Soc. Sci. Med. 2011, 72, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.K.; Glasby, J.; Robinson, S. If telecare is the answer, what was the question? Storylines, tensions and the unintended consequences of technology-supported care. Crit. Soc. Policy 2019, 39, 44–65. [Google Scholar] [CrossRef]
- Steventon, A.; Bardsley, M.; Billings, J.; Dixon, J.; Doll, H.; Beynon, M.; Hirani, S.; Cartwright, M.; Rixon, L.; Knapp, M.; et al. Effect of telecare on use of health and social care services: Findings from the Whole Systems Demonstrator cluster randomised trial. Age Ageing 2013, 42, 501–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henderson, C.; Knapp, M.; Fernández, J.L.; Beecham, J.; Hirani, S.P.; Beynon, M.; Cartwright, M.; Rixon, L.; Doll, H.; Bower, P.; et al. Cost-effectiveness of telecare for people with social care needs: The Whole Systems Demonstrator cluster randomised trial. Age Ageing 2014, 43, 794–800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newman, A.; Bardsley, S. Evaluating Telecare and Telehealth Interventions, WSDAN Briefing Paper. 2011. Available online: http://www.kingsfund.org.uk/sites/files/kf/Evaluating-telecare-telehealth-interventions-Feb2011.pdf (accessed on 20 August 2021).
- Hirani, S.P.; Beynon, M.; Cartwright, M.; Rixon, L.; Doll, H.; Henderson, C.; Bardsley, R.; Steventon, A.; Knapp, M.; Rogers, A.; et al. The effect of telecare on the quality of life and psychological well-being of elderly recipients of social care over a 12-month period: The Whole Systems Demonstrator cluster randomised trial. Age Ageing 2014, 43, 334–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eccles, A. Remote care technologies, older people, and the social care crisis in the United Kingdom: A multiple streams approach to understanding the ‘silver bullet’ of telecare policy. Ageing Soc. 2020, 41, 1726–1747. [Google Scholar] [CrossRef] [Green Version]
- Woolham, J.G.; Steils, N.; Fisk, M.; Porteus, J.; Forsyth, K. The UTOPIA Project. Using Telecare for Older People in Adult Social Care: The Findings of a 2016-17 National Survey of Local Authority Telecare Provision for Older People in England; Social Care Workforce Research Unit, King’s College London: London, UK, 2018. [Google Scholar]
- Hamblin, K.; Yeandle, S.; Fry, G. Researching telecare: The importance of context. J. Enabling Technol. 2017, 11, 75–84. [Google Scholar] [CrossRef] [Green Version]
- Akrich, M.; Latour, B. A Summary of a Convenient Vocabulary for the Semiotics of Human and Nonhuman Assemblies. In Shaping Technology/Building Society; Bijker, W., Law, J., Eds.; MIT Press: London, UK, 1992. [Google Scholar]
- Pols, J.; Willems, D. Innovation and evaluation: Taming and unleashing telecare technology. Sociol. Health Illn. 2011, 33, 484–498. [Google Scholar] [CrossRef] [PubMed]
- Wright, J. The Alexafication of Adult Social Care: Virtual Assistants and the Changing Role of Local Government in England. Int. J. Environ. Res. Public Health 2021, 18, 812. [Google Scholar] [CrossRef]
- Aviva. Tech Nation: Number of Internet-Connected Devices Grows to 10 Per Home. 2021. Available online: https://www.aviva.com/newsroom/news-releases/2020/01/tech-nation-number-of-internet-connected-devices-grows-to-10-per-home/ (accessed on 16 September 2021).
- Parker, C.; Scott, S.; Geddes, A. Snowball Sampling. In SAGE Research Methods Foundations; Atkinson, P., Delamont, S., Cernat, A., Sakshaug, J.W., Williams, R.A., Eds.; SAGE Publications Ltd.: London, UK, 2019. [Google Scholar]
- Timmermans, S.; Tavory, I. Theory construction in qualitative research: From grounded theory to abductive analysis. Sociol. Theory 2012, 30, 167–186. [Google Scholar] [CrossRef]
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code saturation versus meaning saturation: How many interviews are enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef]
- Stirling, P.; Burgess, G. The promises and the reality of smart, digital telecare in England. Hous. Care Support 2021, 24, 65–79. [Google Scholar] [CrossRef]
- Wang, H.; Zhao, E.; Fleming, J.; Dening, T.; Khaw, K.T.; Brayne, C. Is loneliness associated with increased health and social care utilisation in the oldest old? Findings from a population-based longitudinal study. BMJ Open 2019, 9, e024645. [Google Scholar] [CrossRef]
- Yeandle, S. From Provider to Enabler of Care? Reconfiguring Local Authority Support for Older People and Carers in Leeds, 2008 to 2013. J. Soc. Serv. Res. 2016, 42, 218–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ONS. Internet Access—Households and Individuals, Great Britain: 2020. 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/bulletins/internetaccesshouseholdsandindividuals/2020 (accessed on 15 February 2022).
- Blythe, J.M.; Sombatruang, N.; Johnson, S.D. What security features and crime prevention advice is communicated in consumer IoT device manuals and support pages? J. Cybersecur. 2019, 5, 1–10. [Google Scholar] [CrossRef]
- Lau, J.; Zimmerman, B.; Schaub, F. Alexa, are you listening? privacy perceptions, concerns and privacy-seeking behaviors with smart speakers, 2018. In Proceedings of the ACM on Human-Computer Interaction, November 2018; Volume 2, pp. 1–31. Available online: https://dl.acm.org/doi/10.1145/3274371 (accessed on 22 February 2022). [CrossRef]
- Malkin, N.; Deatrick, J.; Tong, A.; Wijesekera, P.; Egelman, S.; Wagner, D. Privacy Attitudes of Smart Speaker Users. In Proceedings on Privacy Enhancing Technologies. 2019, Volume 4, pp. 250–271. Available online: https://sciendo.com/pdf/10.2478/popets-2019-0068 (accessed on 22 February 2022).
- Hamblin, K. Technology and social care in a digital world: Challenges and opportunities in the UK. J. Enabling Technol. 2020, 14, 115–125. [Google Scholar] [CrossRef]
- Procter, R.; Wherton, J.; Greenhalgh, T.; Sugarhood, P.; Rouncefield, M.; Hinder, S. Telecare call centre work and ageing in place. Comput. Supported Coop. Work. (CSCW) 2016, 25, 79–105. [Google Scholar] [CrossRef]
- Steils, N.; Woolham, J.; Fisk, M.; Porteus, J.; Forsyth, K. Carers’ involvement in telecare provision by local councils for older people in England: Perspectives of council telecare managers and stakeholders. Ageing Soc. 2021, 41, 456–475. [Google Scholar] [CrossRef] [Green Version]
- Stern, M.J. Inequality in the Internet age: A twenty-first century dilemma. Sociol. Inq. 2010, 80, 28–33. [Google Scholar] [CrossRef]
- Naylor, C.; Appleby, J. Sustainable Health and Social Care; Kings Fund: London, UK, 2012. [Google Scholar]
- Gathercole, R.; Bradley, R.; Harper, E.; Davies, L.; Pank, L.; Lam, N.; Davies, A.; Talbot, E.; Hooper, E.; Winson, R.; et al. Assistive technology and telecare to maintain independent living at home for people with dementia: The ATTILA RCT. Health Technol. Assess. 2021, 25, 1–156. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).