Exploring, Diversifying and Debating Sustainable Health (Care) Approaches
Abstract
1. Introduction
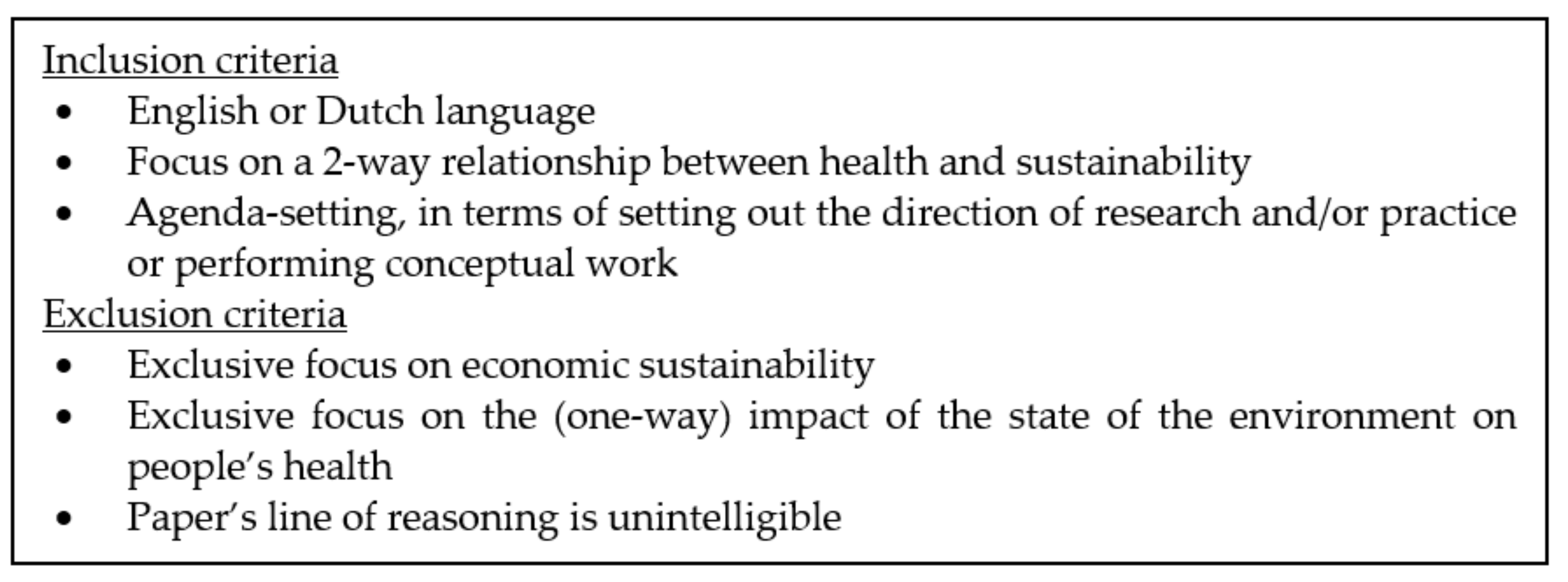
2. Methodology
3. Results
3.1. (Un)Healthy Environments, (Un)Healthy People
3.2. Sustainable Healthcare Systems
3.2.1. Socio-Ecologically Sustainable Healthcare Systems
3.2.2. Socio-Economically Sustainable Healthcare Systems
3.2.3. Towards Sustainable Healthcare Systems
Optimizing the Current Healthcare System
Healthcare System Transformation, and Beyond
Education for Sustainable Healthcare Systems
Rethinking Health and Care, the Medical Rationality and the Healthcare System
4. Discussion & road ahead
4.1. (Un)Healthy Environments, (Un)Healthy People, and (Un)Sustainable Healthcare Systems
4.2. Key Research Avenues
4.3. From Universality to Plurality: Opening up to a Wider Diversity of Voices
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Myers, S.; Frumkin, H. (Eds.) Planetary Health: Protecting Nature to Protect Ourselves; Island Press: Washington, DC, USA, 2020. [Google Scholar]
- Weisz, U.; Pichler, P.-P.; Jaccard, I.S.; Haas, W.; Matej, S.; Bachner, F.; Nowak, P.; Weisz, H. Carbon Emission Trends and Sustainability Options in Austrian Health Care. Resourc. Conserv. Recycl. 2020, 160, 104862. [Google Scholar] [CrossRef]
- Andermann, A.; Tcholakov, Y.; Tomatuk, R.; Buchman, S. Creating an Environmentally Sustainable Health System Demands a Socially Accountable Approach in a Post-COVID World. HealthcarePapers 2020, 19, 61–66. [Google Scholar] [CrossRef]
- Madden, D.L.; Capon, A.; Truskett, P.G.; Madden, D.L.; Truskett, P.G.; Capon, A.; Truskett, P.G.; McGain, F.; Chamberlin, M.; Milburn, J.; et al. Environmentally Sustainable Health Care: Now Is the Time for Action. Med. J. Aust. 2020, 213, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Atwoli, L.; Baqui, A.H.; Benfield, T.; Bosurgi, R.; Godlee, F.; Hancocks, S.; Horton, R.; Laybourn-Langton, L.; Monteiro, C.A.; Norman, I.; et al. Call for Emergency Action to Limit Global Temperature Increases, Restore Biodiversity, and Protect Health. BMJ 2021, 374, n1734. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Countdown. Available online: https://www.lancetcountdown.org/about-us/team/ (accessed on 29 November 2021).
- Lalonde, M. A New Perspective on the Health of Canadians: A Working Document; Government of Canada: Ottawa, ON, Canada, 1974. [Google Scholar]
- Meadows, D.H.; Meadows, D.L.; Randers, J.; Behrens, W. The Limits of Growth: Report for the Club of Rome’s Project on the Predicament of Mankind; Universe Books: New York, NY, USA, 1972. [Google Scholar]
- Goldsmith, E.; Allen, R. A Blueprint for Survival; Penguin: London, UK, 1972. [Google Scholar]
- Carson, R. Silent Spring; Houghton Mifflin: Boston, MA, USA, 1962. [Google Scholar]
- Spaargaren, G.; Loeber, A.; Oosterveer, P. (Eds.) Food Practices in Transition: Changing Food Consumption, Retail and Production in the Age of Reflexive Modernity; Routledge: London, UK, 2011. [Google Scholar]
- WCED. Our Common Future; Oxford University Press: Oxford, UK, 1987. [Google Scholar]
- Elkington, J. Cannibals with Forks: The Triple Bottom Line of 21st Century Business.; Capstone: Oxford, UK, 1997. [Google Scholar]
- Awochna Research in Environmental Health Sciences. Available online: https://publichealth.arizona.edu/departments/cep/ehs/research (accessed on 13 October 2021).
- Budd, W.W.; Young, G.L. Environmental Science. In Environmental Geology; Springer: Dordrecht, The Netherlands, 1999; p. 224. ISBN 978-1-4020-4494-6. [Google Scholar]
- Borgonovi, E.; Adinolfi, P.; Palumbo, R.; Piscopo, G. Framing the Shades of Sustainability in Health Care: Pitfalls and Perspectives from Western EU Countries. Sustainability 2018, 10, 4439. [Google Scholar] [CrossRef]
- Fleiszer, A.R.; Semenic, S.E.; Ritchie, J.A.; Richer, M.-C.; Denis, J.-L. The Sustainability of Healthcare Innovations: A Concept Analysis. J. Adv. Nurs. 2015, 71, 1484–1498. [Google Scholar] [CrossRef]
- Naylor, C.; Appleby, J. Environmentally Sustainable Health and Social Care: Scoping Review and Implications for the English NHS. J. Health Serv. Res. Policy 2013, 18, 114–121. [Google Scholar] [CrossRef]
- Lennox, L.; Maher, L.; Reed, J. Navigating the Sustainability Landscape: A Systematic Review of Sustainability Approaches in Healthcare. Implement. Sci. 2018, 13, 27. [Google Scholar] [CrossRef]
- Nicol, E. Sustainability in Healthcare: Efficiency, Effectiveness, economics and the Environment. Future Healthc. J. 2018, 5, 81. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Coleman, J. Help and Support: Systematic Reviews-Research Guide: Recommended Databases. Available online: https://libguides.murdoch.edu.au/systematic/databases (accessed on 13 October 2021).
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding Human Health in the Anthropocene Epoch: Report of The Rockefeller Foundation–Lancet Commission on Planetary Health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Marks, L.; Hunter, D.J.; Alderslade, R. Strengthening Public Health Capacity and Services in Europe: A Concept Paper; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Acheson, D. Public Health in England. The Report of the Committee of Inquiry into the Future Development of the Public Health Function; HMSO: London, UK, 1988. [Google Scholar]
- Crutzen, P.J. Geology of Mankind: The Anthropocene. Nature 2002, 415, 23. [Google Scholar] [CrossRef] [PubMed]
- Brondizio, E.S.; O’Brien, K.; Bai, X.; Biermann, F.; Steffen, W.; Berkhout, F.; Cudennec, C.; Lemos, M.C.; Wolfe, A.; Palma-Oliveira, J.; et al. Re-Conceptualizing the Anthropocene: A Call for Collaboration. Glob. Environ. Chang. 2016, 39, 318–327. [Google Scholar] [CrossRef]
- Latour, B. We Have Never Been Modern; Harvard University Press: Cambridge, MA, USA, 1993. [Google Scholar]
- Lorimer, J. Multinatural Geographies for the Anthropocene. Prog. Hum. Geogr. 2012, 36, 593–612. [Google Scholar] [CrossRef]
- Gostin, L.O.; Monahan, J.T.; Kaldor, J.; DeBartolo, M.; Friedman, E.A.; Gottschalk, K.; Kim, S.C.; Alwan, A.; Binagwaho, A.; Burci, G.L.; et al. The Legal Determinants of Health: Harnessing the Power of Law for Global Health and Sustainable Development. Lancet 2019, 393, 1857–1910. [Google Scholar] [CrossRef]
- Novice, R. Overview of the Environment and Health in Europe in the 1990s; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Henry, C.J.; Phillips, R.; Carpanini, F.; Corton, J.C.; Craig, K.; Igarashi, K.; Leboeuf, R.; Marchant, G.; Osborn, K.; Pennie, W.D.; et al. Use of Genomics in Toxicology and Epidemiology: Findings and Recommendations of a Workshop. Environ. Health Perspect. 2002, 110, 1047–1050. [Google Scholar] [CrossRef]
- National Research Council. Environmental Epidemiology, Volume 1: Public Health and Hazardous Wastes; The National Academies Press: Washington, DC, USA, 1991; ISBN 978-0-309-07352-3. [Google Scholar]
- Toxicology. Available online: https://www.niehs.nih.gov/health/topics/science/toxicology/index.cfm (accessed on 20 November 2021).
- World Bank. Environmental Health and Sustainable Development. Africa Region Findings & Good Practice Infobriefs; No. 82.; World Bank: Washington, DC, USA, 1997. [Google Scholar]
- US National Institute of Environmental Health Sciences. Global Environmental Health and Sustainable Development; National Institute of Environmental Health Sciences: Durham, NC, USA, 2011. [Google Scholar]
- Bikomeye, J.C.; Rublee, C.S.; Beyer, K.M.M. Positive Externalities of Climate Change Mitigation and Adaptation for Human Health: A Review and Conceptual Framework for Public Health Research. Int. J. Environ. Res. Public Health 2021, 18, 2481. [Google Scholar] [CrossRef]
- Hancock, T. Health and Sustainability in the Urban Environment. Environ. Impact Assess. Rev. 1996, 16, 259–277. [Google Scholar] [CrossRef]
- Centre for Disease Control and Prevention One Health Basics | One Health | CDC. Available online: https://www.cdc.gov/onehealth/basics/index.html (accessed on 14 October 2021).
- WHO. One Health. Available online: https://www.euro.who.int/en/health-topics/health-policy/one-health (accessed on 22 November 2021).
- Loeber, A. The Food Chain Reforged: Novel Food Risk Arrangements and the Metamorphosis of a Metaphor. Sci. Cult. 2011, 20, 231–253. [Google Scholar] [CrossRef]
- Gibbs, E.P. The Evolution of One Health: A Decade of Progress and Challenges for the Future. Vet. Rec. 2014, 174, 85–91. [Google Scholar] [CrossRef]
- Ribeiro, C.d.S.; van den Burgwal, L.H.M.; Regeer, B.J. Overcoming Challenges for Designing and Implementing the One Health Approach: A Systematic Review of the Literature. One Health 2019, 7, 100085. [Google Scholar] [CrossRef] [PubMed]
- Mori, C.; Todaka, E. Establishment of Sustainable Health Science for Future Generations: From a Hundred Years Ago to a Hundred Years in the Future. Environ. Health Prev. Med. 2009, 14, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Richie, C. Can United States Healthcare Become Environmentally Sustainable? Towards Green Healthcare Reform. J. Law Med. Ethics 2020, 48, 643–652. [Google Scholar] [CrossRef]
- Charlesworth, K.E.; Jamieson, M. Healthcare in a Carbon-Constrained World. Aust. Health Rev. 2019, 43, 241–245. [Google Scholar] [CrossRef]
- Crowley, R.A. Climate Change and Health: A Position Paper of the American College of Physicians. Ann. Intern. Med. 2016, 164, 608. [Google Scholar] [CrossRef]
- Pencheon, D. Developing a Sustainable Health Care System: The United Kingdom Experience. Med. J. Aust. 2018, 208, 284–285. [Google Scholar] [CrossRef] [PubMed]
- Johansen, F.; Loorbach, D.; Stoopendaal, A. Exploring a Transition in Dutch Healthcare. JHOM 2018, 32, 875–890. [Google Scholar] [CrossRef]
- Australian Medical Association. Environmental Sustainability in Health Care; Australian Medical Association: Canberra, Australia, 2019. [Google Scholar]
- WHO. Environmentally Sustainable Health Systems: A Strategic Document; WHO: Geneva, Switzerland, 2017; p. 28. [Google Scholar]
- Toebes, B. Towards an Improved Understanding of the International Human Right to Health. Hum. Rights Q. 1999, 21, 661–679. [Google Scholar] [CrossRef]
- Broerse, J.E.W.; Bunders, J.F.G. Transitions in Health Systems: Dealing with Persistent Problems; VU University Press: Amsterdam, The Netherlands, 2010. [Google Scholar]
- Braithwaite, J.; Mannion, R.; Matsuyama, Y.; Shekelle, P.G.; Whittaker, S.; Al-Adawi, S.; Ludlow, K.; James, W.; Ting, H.P.; Herkes, J.; et al. The Future of Health Systems to 2030: A Roadmap for Global Progress and Sustainability. Int. J. Qual. Health Care 2018, 30, 823–831. [Google Scholar] [CrossRef]
- Sturmberg, J.P. Health System Redesign: How to Make Health Care Person-Centered, Equitable, and Sustainable; Springer: Berlin/Heidelberg, Germany, 2017; p. 297. ISBN 978-3-319-64605-3. [Google Scholar]
- Pelster, M.; Hagemann, V.; Laporte Uribe, F. Key Aspects of a Sustainable Health Insurance System in Germany. Appl. Health Econ. Health Policy 2016, 14, 293–312. [Google Scholar] [CrossRef]
- Grin, J.; Broerse, J.E.W. Introduction. In The Future of Health Systems: Beyond the Persistence of Contemporary Challenges; Routledge: London, UK, 2017. [Google Scholar]
- Broerse, J.E.W.; Grin, J. The Future of Health Systems: Beyond the Persistence of Contemporary Challenges. In The Future of Health Systems: Beyond the Persistence of Contemporary Challenges; Chapter 11; Routledge: London, UK, 2017. [Google Scholar]
- Borowy, I.; Aillon, J.-L. Sustainable Health and Degrowth: Health, Health Care and Society beyond the Growth Paradigm. Soc. Theory Health 2017, 15, 346–368. [Google Scholar] [CrossRef]
- Jameton, A.; Pierce, J. Toward a Sustainable US Health Policy: Local Congruities and Global Incongruities. Soc. Indic. Res. 1997, 40, 125–146. [Google Scholar] [CrossRef]
- Wass, S.; Vimarlund, V. Healthcare in the Age of Open Innovation—A Literature Review. HIM J. 2016, 45, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Fleuren, M.; Wiefferink, K.; Paulussen, T. Determinants of Innovation within Health Care Organizations: Literature Review and Delphi Study. Int. J. Qual. Health Care 2004, 16, 107–123. [Google Scholar] [CrossRef]
- Thakur, R.; Hsu, S.H.Y.; Fontenot, G. Innovation in Healthcare: Issues and Future Trends. J. Bus. Res. 2012, 65, 562–569. [Google Scholar] [CrossRef]
- La Rocca, A. Networked Innovation. In Controversies in Healthcare Innovation: Service, Technology and Organization; Hoholm, T., La Rocca, A., Aanestad, M., Eds.; Palgrave Macmillan UK: London, UK, 2018; pp. 247–277. ISBN 978-1-137-55780-3. [Google Scholar]
- Mohrman, S.A.; Kanter, M.H. Designing for Health: Learning from Kaiser Permanente; Organizing for Sustainable Health Care, Emerald Group Publishing Limited: Bingley, UK, 2012; Volume 2. [Google Scholar]
- WHO. WHO Guidance for Climate Resilient and Environmentally Sustainable Health Care Facilities; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- MacNeill, A.J.; McGain, F.; Sherman, J.D. Planetary Health Care: A Framework for Sustainable Health Systems. Lancet Planet. Health 2021, 5, e66–e68. [Google Scholar] [CrossRef]
- Fineberg, H.V. A Successful and Sustainable Health System—How to Get There from Here. N. Engl. J. Med. 2012, 366, 1020–1027. [Google Scholar] [CrossRef]
- Corvalan, C.; Prats, E.V.; Sena, A.; Campbell-Lendrum, D.; Karliner, J.; Risso, A.; Wilburn, S.; Slotterback, S.; Rathi, M.; Stringer, R.; et al. Towards Climate Resilient and Environmentally Sustainable Health Care Facilities. Int. J. Environ. Res. Public Health 2020, 17, 8849. [Google Scholar] [CrossRef]
- Bevan, H.; Fairman, S. The New Era of Thinking and Practice in Change and Transformation: A Call to Action for Leaders of Health and Care; United Kingdom NHS Improving Quality: Leeds, UK, 2014. [Google Scholar]
- Ratnanesan, A.; Howard, P. Future Solutions in Australian Healthcare. White Paper: Innovative Ideas and Strategies for Sustainable Healthcare; Energesse: Sidney, Australia, 2014. [Google Scholar]
- Doebbeling, B.; Flanagan, M. Emerging Perspectives on Transforming the Healthcare System: Redesign Strategies and a Call for Needed Research. Med. Care 2011, 49, S59–S64. [Google Scholar] [CrossRef]
- Charlesworth, K.; Jamieson, M.; Davey, R.; Butler, C.D. Transformational Change in Healthcare: An Examination of Four Case Studies. Aust. Health Rev. 2016, 40, 163–167. [Google Scholar] [CrossRef]
- Oliver, T.H.; Boyd, E.; Balcombe, K.; Benton, T.G.; Bullock, J.M.; Zaum, D. Overcoming Undesirable Resilience in the Global Food System. Glob. Sustain. 2018, 1, E9. [Google Scholar] [CrossRef]
- Kok, K.P.W.; de Hoop, E.; Sengers, F.; Broerse, J.E.W.; Regeer, B.J.; Loeber, A. Governing Translocal Experimentation for Sustainability Transitions. Environ. Innov. Soc. Trans. 2021, 16, 1811–1826. [Google Scholar]
- Charlesworth, K.E.; Madden, D.L.; Capon, A.G. Environmentally Sustainable health Care: Using an Educational Intervention to Engage the Public Health Medical Workforce in Australia. N. S. W. Public Health Bull. 2013, 24, 76–80. [Google Scholar] [CrossRef]
- Hart, E.; Kuijpers, G.; Laverack, G.; Scheele, F. The Process Leading to Physician Activism for Sustainable Change. Sustainability 2021, 13, 10003. [Google Scholar] [CrossRef]
- den Boer, A.C.L.; Teherani, A.; de Hoop, E. Discussing Climate Change and Other Forms of Global Environmental Change during the Clinical Encounter: Exploring US Physicians’ Perspectives. J. Clim. Chang. Health 2021, 4, 100058. [Google Scholar] [CrossRef]
- Sperna Weiland, N. Gastcollege Duurzame Gezondheid En Zorg. In Proceedings of the Zicht op Gezondheid en Leven, Amsterdam, The Netherlands, 27 October 2021. [Google Scholar]
- Essink, D.; Spanjers, R.R.; Broerse, J.E.W.; de Cock Buning, J.T. Sustainable Development: A Guiding Vision in Health System Innovation. In Transitions in Health Systems: Dealing with Persistent Problems; Broerse, J.E.W., Bunders, J.F.G., Eds.; VU University Press: Amsterdam, The Netherlands, 2010; pp. 87–112. [Google Scholar]
- Mortimer, F.; Isherwood, J.; Vaux, E. Sustainability in Quality Improvement: Redefining Value. Future Healthc. J. 2018, 5, 88–93. [Google Scholar] [CrossRef] [PubMed]
- McLean, M.; Gibbs, T.; McKimm, J. Educating for Planetary Health and Environmentally Sustainable Health Care: Responding with Urgency. Med. Teach. 2020, 42, 1082–1084. [Google Scholar] [CrossRef]
- McKimm, J.; Redvers, N.; El Omrani, O.; Parkes, M.W.; Elf, M.; Woollard, R. Education for Sustainable Healthcare: Leadership to Get from Here to There. Med. Teach. 2020, 42, 1123–1127. [Google Scholar] [CrossRef]
- Isherwood, J.; Laybourn-Langton, L. Health and Sustainability. Future Healthc. J. 2018, 5, 84. [Google Scholar] [CrossRef]
- Barna, S.; Maric, F.; Simons, J.; Kumar, S.; Blankestijn, P.J. Education for the Anthropocene: Planetary Health, Sustainable Health Care, and the Health Workforce. Med. Teach. 2020, 42, 1091–1096. [Google Scholar] [CrossRef]
- Tun, M.S. Fulfilling a New Obligation: Teaching and Learning of Sustainable Healthcare in the Medical Education Curriculum. Med. Teach. 2019, 41, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Huss, N.; Ikiugu, M.N.; Hackett, F.; Sheffield, P.E.; Palipane, N.; Groome, J. Education for Sustainable Health Care: From Learning to Professional Practice. Med. Teach. 2020, 42, 1097–1101. [Google Scholar] [CrossRef] [PubMed]
- Schuitmaker, T.J. Persistent Problems in the Dutch Health Care System: Learning from Novel Practices for a Transition in Health Care with the UPP Framework. Ph.D. Thesis, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands, 2013. [Google Scholar]
- Dunphy, J.L. Healthcare Professionals’ Perspectives on Environmental Sustainability. Nurs. Ethics 2014, 21, 414–425. [Google Scholar] [CrossRef] [PubMed]
- Van Bortel, T.; Wickramasinghe, N.D.; Morgan, A.; Martin, S. Health Assets in a Global Context: A Systematic Review of the Literature. BMJ Open 2019, 9, e023810. [Google Scholar] [CrossRef]
- Dooris, M. Holistic and Sustainable Health Improvement: The Contribution of the Settings-Based Approach to Health Promotion. Perspect. Public Health 2009, 129, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Sturmberg, J.P.; Njoroge, A. People-Centred Health Systems, a Bottom-up Approach: Where Theory Meets Empery. J. Eval. Clin. Pract. 2017, 23, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Lautensach, A.K. Sustainable Health for All? The Tension between Human Security and the Right to Health Care. J. Hum. Secur. 2015, 11, 5–18. [Google Scholar] [CrossRef][Green Version]
- Arora, S.; Stirling, A. Don’t Save “the World”—Embrace a Pluriverse! Available online: https://steps-centre.org/blog/dont-save-the-world-embrace-a-pluriverse/ (accessed on 20 October 2021).
- Faulkner, A. Medical Technology into Healthcare and Society: A Sociology of Devices, Innovation and Governance; Palgrave Macmillan US: New York, NY, USA, 2009. [Google Scholar]
- Zuiderent-Jerak, T.; Grit, K.; van der Grinten, T. Critical Composition of Public Values: On the Enactment and Disarticulation of What Counts in Health-Care Markets. In Value Practices in the Life Sciences and Medicine; Dussauge, I., Helgesson, C.-F., Lee, F., Eds.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Rohracher, H.; Spaeth, P. Cities as Arenas of Low-Carbon Transitions Friction Zones in the Negotiation of Low-Carbon Futures. In Urban Sustainability Transitions; Frantzeskaki, N., Castán Broto, V., Coenen, L., Loorbach, D., Eds.; Routledge: London, UK, 2017. [Google Scholar]
- de Hoop, E.; Arora, S. Material Meanings: “Waste” as a Performative Category of Land in Colonial India. J. Hist. Geogr. 2017, 55, 82–92. [Google Scholar] [CrossRef][Green Version]
- de Hoop, E.; van der Vleuten, E. Sustainability Knowledge Politics: Southeast Asia, Europe, and the Transregional History of Palm Oil Sustainability Research. Glob. Environ. J. Transdiscip. Hist. 2022. submitted. [Google Scholar]
- Myers, S.S. Planetary Health: Protecting Human Health on a Rapidly Changing Planet. Lancet 2017, 390, 2860–2868. [Google Scholar] [CrossRef]
- Louro, A.; Marques da Costa, N.; Marques da Costa, E. Sustainable Urban Mobility Policies as a Path to Healthy Cities—The Case Study of LMA, Portugal. Sustainability 2019, 11, 2929. [Google Scholar] [CrossRef]
- Nayna Schwerdtle, P.; Horton, G.; Kent, F.; Walker, L.; McLean, M. Education for Sustainable Healthcare: A Transdisciplinary Approach to Transversal Environmental Threats. Med. Teach. 2020, 42, 1102–1106. [Google Scholar] [CrossRef] [PubMed]
- de Boer, J.; Aiking, H. Pursuing a Low Meat Diet to Improve Both Health and Sustainability: How Can We Use the Frames That Shape Our Meals? Ecol. Econ. 2017, 142, 238–248. [Google Scholar] [CrossRef]
- de la Cadena, M.; Blaser, M. A World of Many Worlds; Duke University Press: Durham, UK, 2018; ISBN 978-1-4780-0431-8. [Google Scholar]
- Tandon, A. Analysis: The Lack of Diversity in Climate-Science Research. Available online: https://www.carbonbrief.org/analysis-the-lack-of-diversity-in-climate-science-research (accessed on 29 November 2021).
- The Lancet Voice. COP26: Inequality in Climate Research; The Lancet Voice: London, UK, 2021. [Google Scholar]
- Swyngedouw, E. Apocalypse Forever? Theory Cult. Soc. 2010, 27, 213–232. [Google Scholar] [CrossRef]
- Stirling, A. “Opening Up” and “Closing Down”: Power, Participation, and Pluralism in the Social Appraisal of Technology. Sci. Technol. Hum. Values 2008, 33, 262–294. [Google Scholar] [CrossRef]
- Latour, B. Anthropology at the Time of the Anthropocene: A Personal View of What Is to Be Studied. In The Anthropology of Sustainability; Brightman, M., Lewis, J., Eds.; Palgrave Macmillan US: New York, NY, USA, 2017; pp. 35–49. ISBN 978-1-137-56635-5. [Google Scholar]
- Kenis, A. From Individual to Collective Change and beyond: Ecological Citizenship and Politicisation. Ph.D. Thesis, KU Leuven, Leuven, Belgium, 2015. [Google Scholar]
- Reedy, J.; Orr, R.; Spicer, P.; Blanchard, J.W.; Hiratsuka, V.Y.; Ketchum, T.S.; Saunkeah, B.; Wark, K.; Woodbury, R.B. Deliberative Democracy and Historical Perspectives on American Indian/Alaska Native Political Decision-Making Practices. Humanit. Soc. Sci. Commun. 2020, 7, 16. [Google Scholar] [CrossRef]
- Datta, P.K. Exploring the Dynamics of Deliberative Democracy in Rural India: Lessons from the Working of Gram Sabhas in India and Gram Sansads in West Bengal. Indian J. Public Adm. 2019, 65, 117–135. [Google Scholar] [CrossRef]
- Jasanoff, S. Just Transitions: A Humble Approach to Global Energy Futures. Energy Res. Soc. Sci. 2018, 35, 11–14. [Google Scholar] [CrossRef]
- Avelino, F.; Grin, J. Beyond Deconstruction. a Reconstructive Perspective on Sustainability Transition Governance. Environ. Innov. Soc. Trans. 2017, 22, 15–25. [Google Scholar] [CrossRef]

| (Un)Healthy Environments, Unhealthy People | Socio-Ecologically Sustainable Healthcare Systems | Socio-Economically Sustainable Healthcare Systems | |
|---|---|---|---|
| Articles | 10 | 22 | 16 |
| Book chapters | 2 | 0 | 7 |
| Reports | 6 | 5 | 2 |
| Total | 18 | 27 | 25 |
| (Un)healthy Environments, Unhealthy People(Planetary Health, Environmental Health and one Health Literature) | Socio-Ecologically Sustainable Healthcare Systems | Socio-Economically Sustainable Healthcare Systems | |
|---|---|---|---|
| How are intertwinements between health and sustainability, and their challenges, represented? | 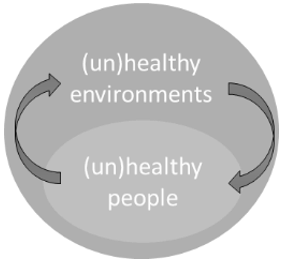 |  |  |
| What suggestions are raised to address the challenges identified? | Creating healthier environments, inspired by solutions developed in wider sustainability research, environmental sciences, ecology, veterinary sciences, etc. | Optimizing the current healthcare system; transforming healthcare systems and interrelated systems (food, energy, industry, etc.); educating healthcare professionals; rethinking health and care, the medical rationality and the healthcare system. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoop, E.d.; Loeber, A.; Essink, D. Exploring, Diversifying and Debating Sustainable Health (Care) Approaches. Sustainability 2022, 14, 1698. https://doi.org/10.3390/su14031698
Hoop Ed, Loeber A, Essink D. Exploring, Diversifying and Debating Sustainable Health (Care) Approaches. Sustainability. 2022; 14(3):1698. https://doi.org/10.3390/su14031698
Chicago/Turabian StyleHoop, Evelien de, Anne Loeber, and Dirk Essink. 2022. "Exploring, Diversifying and Debating Sustainable Health (Care) Approaches" Sustainability 14, no. 3: 1698. https://doi.org/10.3390/su14031698
APA StyleHoop, E. d., Loeber, A., & Essink, D. (2022). Exploring, Diversifying and Debating Sustainable Health (Care) Approaches. Sustainability, 14(3), 1698. https://doi.org/10.3390/su14031698






