Willingness to Pay for Mobile Health Live Streaming during the COVID-19 Pandemic: Integrating TPB with Compatibility
Abstract
1. Introduction
- Is TPB applicable to the MHLS environment?
- Can compatibility be applied to MHLS environments?
- How does compatibility integrate into the TPB when interpreting consumers’ WTP in an MHLS environment?
- incorporate compatibility into TPB to form an integrated framework for explaining the formation of WTP for MHLS.
- examine the structures that influence the process of attitude formation.
- examine the mediating role of attitude in the mechanism of WTP for MHLS.
2. Literature Review
2.1. TPB in MHLS
2.1.1. Attitude (AT)
2.1.2. Subjective Norms (SN)
2.1.3. Self-efficacy (SE)
2.2. Compatibility
2.2.1. Preferred Lifestyle (PL)
2.2.2. Information Quality (IQ)
2.2.3. Interactive Immersion (II)
3. Methodology
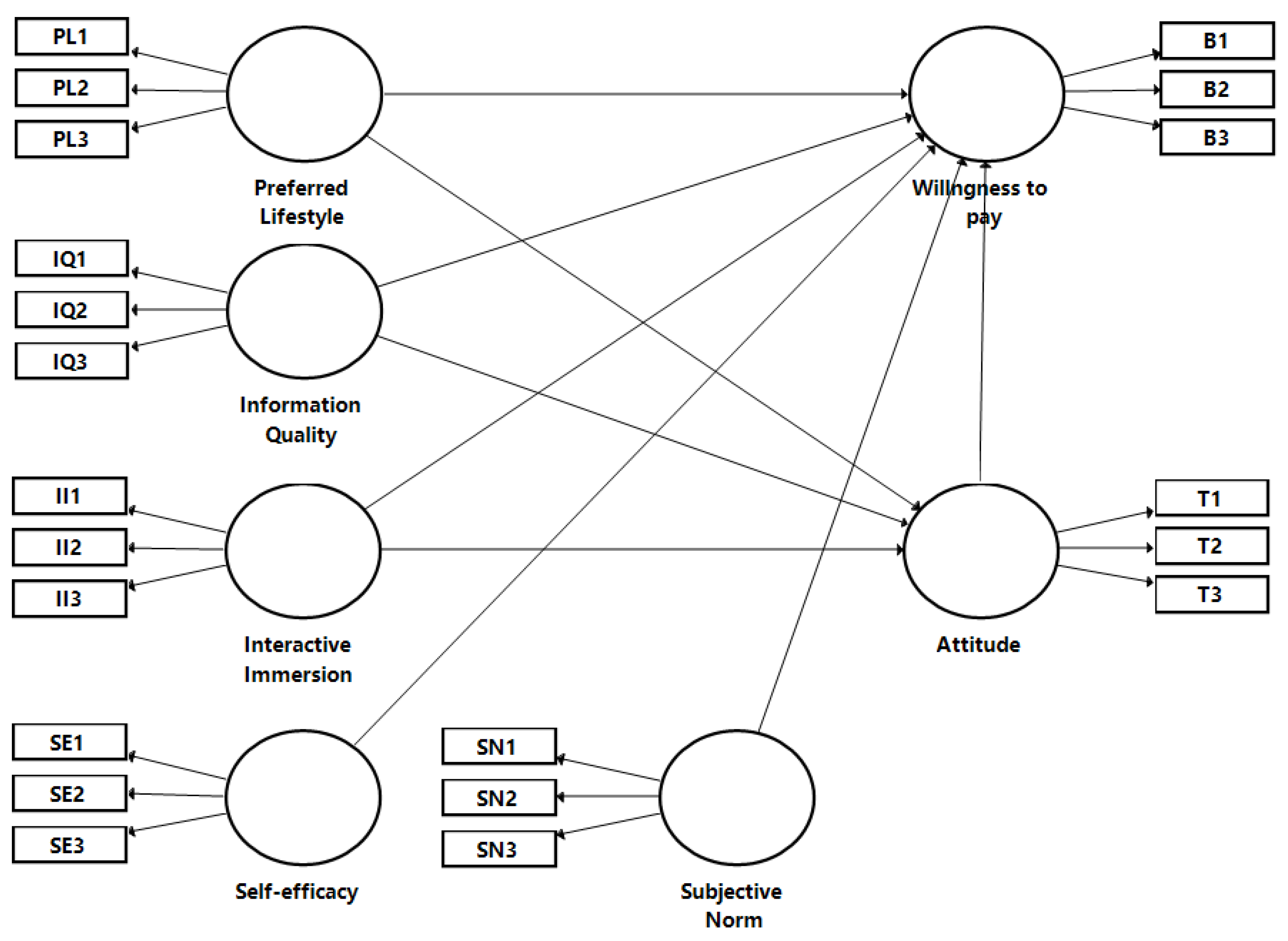
3.1. Research Model and Hypotheses
3.2. Construct Measures
3.3. Data Collection
3.4. Data Analysis Methods
4. Results
4.1. Respondents’ Background
4.2. Measurement Model Analysis
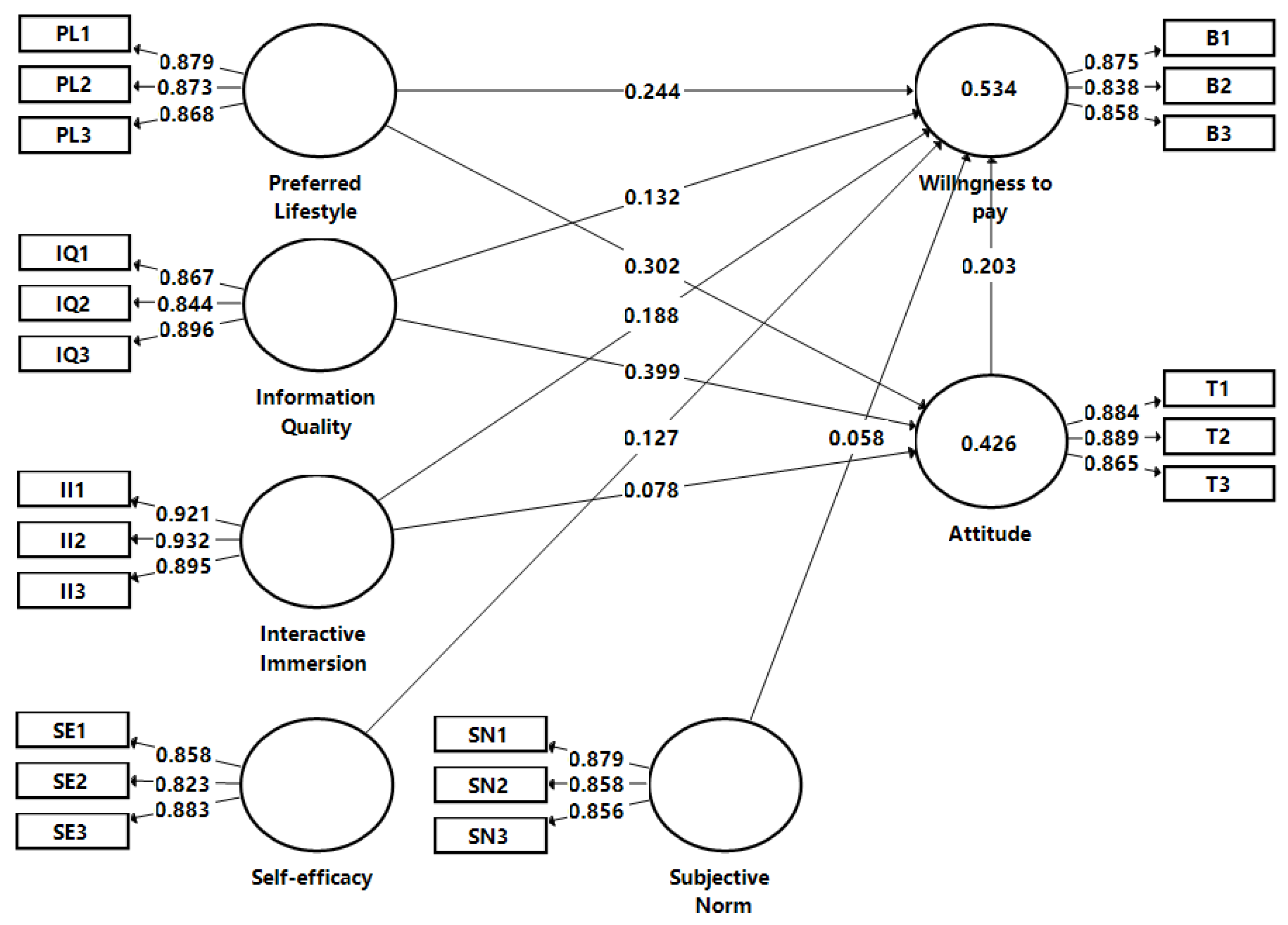
4.3. Structural Model Analysis
4.4. Mediation Effects
4.5. Control Variables
5. Discussion and Conclusions
5.1. Discussion
- The relationship between PL and WTP is supported and mediated by AT;PL’s influence on WTP is supported. Previous studies on social media found that PL has a significant, direct effect on WTP [68], whereas we discovered that its effect is mediated by AT (H4a). Researchers’ attention to lifestyle has exploded in recent years, possibly reflecting consumers’ adaptability to new technologies and health awareness to achieve basic values throughout life. Especially during the COVID-19 pandemic, people are more likely to use MHLS if it allows them to access health information at home and reduces unnecessary travel. Meanwhile, PL is important to maintain the balance between changes in health promotion and individuals’ value systems. Specifically, in MHLS, PL refers to a healthy or mobile lifestyle. In healthy lifestyle terms, many individuals start using health live streaming apps to promote healthy behavior as they desire to maintain a healthy lifestyle, even less helpful health information is available in most apps [105]. A healthy lifestyle requires a sustained attitude and the willingness to pay for MHLS. In mobile lifestyle terms, mobile live streaming services persist because they are often synchronous, authentic, and group-based and provide a means to pay for goods and services in virtually any situation. Each lifestyle may become an incentive that cultivates people to increase their WTP so that the use of a mobile live streaming platform is necessary for consumers. Therefore, the influence of PL remains critical in predicting consumers’ AT and WTP.
- The relationship between IQ and WTP is supported and mediated by AT;The study also contributes by integrating IQ into the TPB model. The findings support the role of IQ on WTP (H5), which is consistent with studies relating to live streaming commerce [75] and internet commerce services [106]. This study considers IQ in an MHLS case. Specifically, IQ is a measure of customers’ perceived value of the output generated by MHLS. Pursuing an effective medical consultation is a long and vigorous exploration, not a timely return, which implies that it can be challenging for consumers to achieve substantial positive results from just a few uses of MHLS. Thus, obtaining high-quality health care information is very helpful, as consumers feel the requirements are fulfilled, which can motivate them to pay for their consultations. The effect of IQ on AT towards MHLS is also supported (H5a). Previous studies considered IQ in terms of its impact on health care management. For example, patients perceive that their attitudes toward mobile health services are positively influenced by the quality of mobile health systems [107]. However, prior investigations have not considered the relationship between IQ, AT, and WTP. Our findings illustrate the utility of IQ from a consumer perspective, elaborating on how IQ can motivate WTP via health apps where consumer attitudes are improved.
- The relationship between II and WTP is supported but not mediated by AT;Furthermore, it is found that II in MHLS significantly influences the WTP (H6). This relationship follows other studies which established the relationship between II and WTP [78]. Our finding implies that consumers’ active MHLS immersion drives their future purchase intentions. Unlike previous research [108], the results of our study indicated that II in MHLS is not mediated by AT (H6a), which may be due to two reasons. On the one hand, immersive experiences generate positive attitudinal effects in the form of consumers’ emotional and affective responses [108]. In times of pandemic, consumers may feel challenged to identify emotional states accurately because of a negative psychological condition caused by pandemic-induced anxiety [109]. On the other hand, in China, the primary purpose of new health promotion using ICTs may be to make profits rather than disseminate health information [110], which may explain why the II of consumers in MHLS may not lead to a greater AT.
- The relationship between SE and WTP is supported;SE’s significant effect on WTP (H3) is based on the work of Chang et al. [111] for health values on functional beverage purchase intentions. As a critical component in the extended TPB model, SE is a strong predictor of WTP in some ICT studies [112,113]. To accomplish health goals, most consumers will actively adopt the MHLS program, thereby making the SE of MHLS an important determinant of WTP. During the COVID-19 pandemic, the public was involved in MHLS with almost minimal technical professional help. This greatly reduces the psychological anxiety associated with the use of technology and strengthens individuals’ self-assurance in their ability to resist public health crises [114].
- The relationship between SN and WTP is not supported;Surprisingly, SN had no significant effect on WTP (H2). Our findings are inconsistent with the results of a study on online grocery shopping [115], which found a significant positive effect of SN on WTP. However, the emphasis of online grocery research is on social interaction, allowing consumers to share shopping knowledge or experiences through efficient interplay. The contrast between these two types of research may reveal that the impact of SN on MHLS will be less critical in the post-adoption phase. In the MHLS scenario, app developers rarely design relevant features for social interactions between consumers, which objectively renders it difficult for SN to play a contributing role. To be precise, consumers’ motivation to pay for medical consultations in MHLS is often tied to the characteristics of the private conditions, like disease type. Thus, in the case of MHLS, SN may not be predictive of consumers’ WTP. This is in line with the findings on e-services, where SN showed no significant effect on WTP [116]. Consequently, the impact of SN on consumers’ WTP diminishes before the payment phase, but the experience from the consumer’s own life may be highly influential.
5.2. Implications and Future Research
5.2.1. Implications
5.2.2. Limitations and Future Research Agenda
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variables | Items | Sources |
|---|---|---|
| Preferred lifestyle (PL) | PL1: MHLS is in line with my own personal health value PL2: MHLS fits the way I view health PL3: MHLS is consistent with the way I to keep healthy | Dhir et al. [122] |
| Information quality (IQ) | IQ1: MHLS provides appropriate information IQ2: MHLS provides important information IQ3: MHLS provides effective information | Kim & Lee [123] |
| Interactive immersion (II) | II1: I feel absorbed when using MHLS II2: I feel focused when using MHLS II3: I get a good interactive experience when using MHLS | Song et al. [124] |
| Self-efficacy (SE) | SE1: I can use MHLS if there is no one around to assist me SE2: I can use MHLS if the technology has never been similar to me before SE3: I believe I can use mobile technology effectively | Reychav et al. [125] |
| Subjective norms (SN) | SN1: people who matter to me prefer that I use MHLS SN2: People who affect me prefer that I use MHLS SN3: People who value me prefer that I use MHLS | Ajzen & Fishbein [126] |
| Attitude (AT) | AT1: I think it is wise to use MHLS AT2: I think it is a pleasant experience to use MHLS AT3: I am satisfied with MHLS | Deng et al. [127] |
| Willingness to pay (WTP) | WTP1: Assuming I have access to MHLS, I intend to pay more for it WTP2: Given that I have access to MHLS, I predict that I will pay more for it WTP3: If I have access to pay for MHLS, I want to pay as much as possible | Bettiga et al. [5] |
| Construct | Indicator | Substantive Factor Loading | Construct | Indicator | Substantive Factor Loading |
|---|---|---|---|---|---|
| Preferred lifestyle (PL) | PL1 | 0.922 | 0.850 | 0.073 | 0.005 |
| PL2 | 0.928 | 0.861 | 0.077 | 0.006 | |
| PL3 | 0.898 | 0.806 | 0.07 | 0.005 | |
| Information quality (IQ) | IQ1 | 0.872 | 0.760 | 0.066 | 0.004 |
| IQ2 | 0.848 | 0.719 | 0.064 | 0.004 | |
| IQ3 | 0.888 | 0.788 | 0.077 | 0.006 | |
| Interactive immersion (II) | II1 | 0.877 | 0.769 | 0.076 | 0.006 |
| II2 | 0.878 | 0.770 | 0.073 | 0.006 | |
| II3 | 0.865 | 0.748 | 0.076 | 0.006 | |
| Self-efficacy (SE) | SE1 | 0.857 | 0.734 | 0.068 | 0.005 |
| SE2 | 0.839 | 0.703 | 0.067 | 0.004 | |
| SE3 | 0.871 | 0.759 | 0.068 | 0.005 | |
| Subjective norms (SN) | SN1 | 0.871 | 0.759 | 0.068 | 0.005 |
| SN2 | 0.871 | 0.759 | 0.064 | 0.004 | |
| SN3 | 0.852 | 0.726 | 0.067 | 0.004 | |
| Attitude (AT) | AT1 | 0.887 | 0.787 | 0.076 | 0.006 |
| AT2 | 0.886 | 0.785 | 0.078 | 0.006 | |
| AT3 | 0.865 | 0.748 | 0.076 | 0.006 | |
| Willingness to pay (WTP) | WTP1 | 0.87 | 0.757 | 0.079 | 0.006 |
| WTP2 | 0.843 | 0.711 | 0.073 | 0.005 | |
| WTP3 | 0.859 | 0.738 | 0.076 | 0.006 | |
| Average | N. A | 0.874 | 0.763 | 0.072 | 0.005 |
References
- Silva, B.M.C.; Rodrigues, J.J.P.C.; de la Torre Díez, I.; López-Coronado, M.; Saleem, K. Mobile-Health: A Review of Current State in 2015. J. Biomed. Inform. 2015, 56, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Gong, X.; Ye, Z.; Liu, K.; Wu, N. The Effects of Live Platform Exterior Design on Sustainable Impulse Buying: Exploring the Mechanisms of Self-Efficacy and Psychological Ownership. Sustainability 2020, 12, 2406. [Google Scholar] [CrossRef]
- Jacob, C.; Sezgin, E.; Sanchez-Vazquez, A.; Ivory, C. Sociotechnical Factors Affecting Patients’ Adoption of Mobile Health Tools: Systematic Literature Review and Narrative Synthesis. JMIR mHealth uHealth 2022, 10, e36284. [Google Scholar] [CrossRef] [PubMed]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. The Emerging Field of Mobile Health. Sci. Transl. Med. 2015, 7, 283rv3. [Google Scholar] [CrossRef]
- Bettiga, D.; Lamberti, L.; Lettieri, E. Individuals’ Adoption of Smart Technologies for Preventive Health Care: A Structural Equation Modeling Approach. Health Care Manag. Sci. 2020, 23, 203–214. [Google Scholar] [CrossRef]
- Song, W.; Zhao, T.; Huang, E. How Does the COVID-19 Pandemic Affect People’s Willingness to Pay for Health in the Short and Long Term? A Longitudinal Study during and after the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2022, 19, 1568. [Google Scholar] [CrossRef]
- Bhatia, R. Telehealth and COVID-19: Using Technology to Accelerate the Curve on Access and Quality Healthcare for Citizens in India. Technol. Soc. 2021, 64, 101465. [Google Scholar] [CrossRef]
- IResearch. Available online: https://www.iresearch.com.cn/Detail/report?id=4057&isfree=0 (accessed on 5 May 2022).
- Liu, R.; Menhas, R.; Dai, J.; Saqib, Z.A.; Peng, X. Fitness Apps, Live Streaming Workout Classes, and Virtual Reality Fitness for Physical Activity during the COVID-19 Lockdown: An Empirical Study. Front. Public Health 2022, 10, 1–9. [Google Scholar] [CrossRef]
- Akbar, S.; Coiera, E.; Magrabi, F. Safety Concerns with Consumer-Facing Mobile Health Applications and Their Consequences: A Scoping Review. J. Am. Med. Inform. Assoc. 2020, 27, 330–340. [Google Scholar] [CrossRef]
- Kasilingam, D.; Krishna, R. Understanding the Adoption and Willingness to Pay for Internet of Things Services. Int. J. Consum. Stud. 2022, 46, 102–131. [Google Scholar] [CrossRef]
- Oe, H. Discussion of Digital Gaming’s Impact on Players’ Well-Being during the COVID-19 Lockdown. arXiv 2020, arXiv:2005.00594. [Google Scholar]
- Ajzen, I. The Theory of Planned Behavior: Frequently Asked Questions. Hum. Behav. Emerg. Technol. 2020, 2, 314–324. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What Factors Influence the Mobile Health Service Adoption? A Meta-Analysis and the Moderating Role of Age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Bosnjak, M.; Ajzen, I.; Schmidt, P. The Theory of Planned Behavior: Selected Recent Advances and Applications. Eur. J. Psychol. 2020, 16, 352–356. [Google Scholar] [CrossRef]
- Wang, X.; Shi, J.; Kong, H. Online Health Information Seeking: A Review and Meta-Analysis. Health Commun. 2021, 36, 1163–1175. [Google Scholar] [CrossRef] [PubMed]
- Lv, Q.; Jiang, Y.; Qi, J.; Zhang, Y.; Zhang, X.; Fang, L.; Tu, L.; Yang, M.; Liao, Z.; Zhao, M.; et al. Using Mobile Apps for Health Management: A New Health Care Mode in China. JMIR mHealth uHealth 2019, 7, e10299. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Perugini, M.; Bagozzi, R.P. The Role of Desires and Anticipated Emotions in Goal-directed Behaviours: Broadening and Deepening the Theory of Planned Behaviour. Br. J. Soc. Psychol. 2001, 40, 79–98. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Wang, L.; Zhang, Y.; Wang, J. Mobile Health Service Adoption in China: Integration of Theory of Planned Behavior, Protection Motivation Theory and Personal Health Differences. Online Inf. Rev. 2019, 44, 1–23. [Google Scholar] [CrossRef]
- Chao, D.Y.P.; Lin, T.M.Y.; Ma, W.-Y. Enhanced Self-Efficacy and Behavioral Changes among Patients with Diabetes: Cloud-Based Mobile Health Platform and Mobile App Service. JMIR Diabetes 2019, 4, e11017. [Google Scholar] [CrossRef]
- Ajzen, I. Perceived Behavioral Control, Self-efficacy, Locus of Control, and the Theory of Planned Behavior 1. J. Appl. Soc. Psychol. 2002, 32, 665–683. [Google Scholar] [CrossRef]
- Karahanna, E.; Agarwal, R.; Angst, C.M. Reconceptualizing Compatibility Beliefs in Technology Acceptance Research. MIS Q. 2006, 30, 781–804. [Google Scholar] [CrossRef]
- Jacob, C.; Sanchez-Vazquez, A.; Ivory, C. Social, Organizational, and Technological Factors Impacting Clinicians’ Adoption of Mobile Health Tools: Systematic Literature Review. JMIR mHealth uHealth 2020, 8, e15935. [Google Scholar] [CrossRef] [PubMed]
- Saheb, T. An Empirical Investigation of the Adoption of Mobile Health Applications: Integrating Big Data and Social Media Services. Health Technol. 2020, 10, 1063–1077. [Google Scholar]
- Octavius, G.S.; Antonio, F. Antecedents of Intention to Adopt Mobile Health (MHealth) Application and Its Impact on Intention to Recommend: An Evidence from Indonesian Customers. Int. J. Telemed. Appl. 2021, 2021, 6698627. [Google Scholar] [CrossRef]
- Liao, X.; Wu, D.; Zhang, Q.; Han, G. How to Improve Users’ Loyalty to Smart Health Devices? The Perspective of Compatibility. Sustainability 2021, 13, 10722. [Google Scholar] [CrossRef]
- Anderson, K.; Burford, O.; Emmerton, L. Mobile Health Apps to Facilitate Self-Care: A Qualitative Study of User Experiences. PLoS ONE 2016, 11, e0156164. [Google Scholar] [CrossRef]
- Broussard, J.D.; Teng, E.J. Models for Enhancing the Development of Experiential Learning Approaches within Mobile Health Technologies. Prof. Psychol. Res. Pract. 2019, 50, 195–203. [Google Scholar] [CrossRef]
- Ning, G.; Daggett, Q.; Perivolaris, A.; Kapralos, B.; Quevedo, A.; Collins, K.C.; Kanev, K.; Dubrowski, A. Rethinking Audio-Haptic Perceptual Immersion from in-Person to Remote Testing during COVID-19. In Proceedings of the Interactive Mobile Communication, Technologies and Learning (IMCL 2021), Thessaloniki, Greece, 4–5 November 2021; pp. 102–110. [Google Scholar]
- Zheng, Y.; Wang, W.; Zhong, Y.; Wu, F.; Zhu, Z.; Tham, Y.-C.; Lamoureux, E.; Xiao, L.; Zhu, E.; Liu, H. A Peer-to-Peer Live-Streaming Intervention for Children during COVID-19 Homeschooling to Promote Physical Activity and Reduce Anxiety and Eye Strain: Cluster Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e24316. [Google Scholar] [CrossRef]
- Razmak, J.; Bélanger, C. Using the Technology Acceptance Model to Predict Patient Attitude toward Personal Health Records in Regional Communities. Inf. Technol. People 2018, 31, 306–326. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, X.; Yuen, K.F. Augmented Reality Shopping Application Usage: The Influence of Attitude, Value, and Characteristics of Innovation. J. Retail. Consum. Serv. 2021, 63, 102720. [Google Scholar] [CrossRef]
- Pavlou, P.A.; Fygenson, M. Understanding and Predicting Electronic Commerce Adoption: An Extension of the Theory of Planned Behavior. MIS Q. 2006, 30, 115–143. [Google Scholar] [CrossRef]
- Mainardes, E.W.; de Souza, I.M.; Correia, R.D. Antecedents and Consequents of Consumers Not Adopting E-Commerce. J. Retail. Consum. Serv. 2020, 55, 102138. [Google Scholar] [CrossRef]
- Hansen, J.M.; Saridakis, G.; Benson, V. Risk, Trust, and the Interaction of Perceived Ease of Use and Behavioral Control in Predicting Consumers’ Use of Social Media for Transactions. Comput. Human Behav. 2018, 80, 197–206. [Google Scholar] [CrossRef]
- Mohammed, A.; Ferraris, A. Factors Influencing User Participation in Social Media: Evidence from Twitter Usage during COVID-19 Pandemic in Saudi Arabia. Technol. Soc. 2021, 66, 101651. [Google Scholar] [CrossRef]
- Yang, S.; Lu, Y.; Gupta, S.; Cao, Y.; Zhang, R. Mobile Payment Services Adoption across Time: An Empirical Study of the Effects of Behavioral Beliefs, Social Influences, and Personal Traits. Comput. Human Behav. 2012, 28, 129–142. [Google Scholar] [CrossRef]
- Belanche, D.; Guinalíu, M.; Albás, P. Customer Adoption of P2p Mobile Payment Systems: The Role of Perceived Risk. Telemat. Inform. 2022, 72, 101851. [Google Scholar] [CrossRef]
- Wang, Z.; Li, J.; Chen, P. Factors Influencing Chinese Flower and Seedling Family Farms’ Intention to Use Live Streaming as a Sustainable Marketing Method: An Application of Extended Theory of Planned Behavior. Environ. Dev. Sustain. 2022, 24, 4322–5299. [Google Scholar] [CrossRef]
- Pang, Q.; Meng, H.; Fang, M.; Xing, J.; Yao, J. Social Distancing, Health Concerns, and Digitally Empowered Consumption Behavior Under COVID-19: A Study on Livestream Shopping Technology. Front. Public Health 2021, 9, 1–11. [Google Scholar] [CrossRef]
- Xu, Y.; Ye, Y.; Liu, Y. Understanding Virtual Gifting in Live Streaming by the Theory of Planned Behavior. Hum. Behav. Emerg. Technol. 2022, 2022, 8148077. [Google Scholar] [CrossRef]
- Cheng, Z.; Gu, T.; Zhang, Y.; Zhang, Z. The Application of Multimedia Computer Technology in Live-Stream Shopping—From the Perspective of User’s Purchasing Behavior. In Proceedings of the 2020 International Conference on Computer Science and Management Technology (ICCSMT), Shanghai, China, 20–22 November 2020; pp. 195–198. [Google Scholar]
- Apasrawirote, D.; Yawised, K. Factors Influencing the Behavioral and Purchase Intention on Live-Streaming Shopping. Asian, J. Bus. Res. 2022, 12, 39–56. [Google Scholar] [CrossRef]
- Godin, G.; Kok, G. The Theory of Planned Behavior: A Review of Its Applications to Health-Related Behaviors. Am. J. Health Promot. 1996, 11, 87–98. [Google Scholar] [CrossRef]
- Alzubaidi, H.; Slade, E.L.; Dwivedi, Y.K. Examining Antecedents of Consumers’ pro-Environmental Behaviours: TPB Extended with Materialism and Innovativeness. J. Bus. Res. 2021, 122, 685–699. [Google Scholar] [CrossRef]
- Parkinson, J.; David, P.; Rundle-Thiele, S. Self-Efficacy or Perceived Behavioural Control: Which Influences Consumers’ Physical Activity and Healthful Eating Behaviour Maintenance? J. Consum. Behav. 2017, 16, 413–423. [Google Scholar] [CrossRef]
- Ajzen, I.; Fishbein, M. The Prediction of Behavior from Attitudinal and Normative Variables. J. Exp. Soc. Psychol. 1970, 6, 466–487. [Google Scholar] [CrossRef]
- Jaber, D.; Aburuz, S.; Hammad, E.A.; El-Refae, H.; Basheti, I.A. Patients’ Attitude and Willingness to Pay for Pharmaceutical Care: An International Message from a Developing Country. Res. Soc. Adm. Pharm. 2019, 15, 1177–1182. [Google Scholar] [CrossRef]
- Di Blasio, A.; Morano, T.; Lancia, F.; Viscioni, G.; Di Iorio, A.; Grossi, S.; Cianchetti, E.; Pippi, R.; Gobbo, S.; Bergamin, M. Effects of Activity Tracker-Based Counselling and Live-Web Exercise on Breast Cancer Survivors’ Sleep and Waking Time during Italy’s COVID-19 Lockdown. Home Health Care Serv. Q. 2022, 41, 1–19. [Google Scholar] [CrossRef]
- Gong, Z.; Han, Z.; Li, X.; Yu, C.; Reinhardt, J.D. Factors Influencing the Adoption of Online Health Consultation Services: The Role of Subjective Norm, Trust, Perceived Benefit, and Offline Habit. Front. Public Health 2019, 7, 1–9. [Google Scholar] [CrossRef]
- Lee, S.E.; Choi, M.; Kim, S. They Pay for a Reason! The Determinants of Fan’s Instant Sponsorship for Content Creators. Telemat. Inform. 2019, 45, 101286. [Google Scholar] [CrossRef]
- Liu, Y.; Gan, W.; Zhang, Q. Decision-Making Mechanism of Online Retailer Based on Additional Online Comments of Consumers. J. Retail. Consum. Serv. 2021, 59, 102389. [Google Scholar] [CrossRef]
- Vedel, I.; Ramaprasad, J.; Lapointe, L. Social Media Strategies for Health Promotion by Nonprofit Organizations: Multiple Case Study Design. J. Med. Internet Res. 2020, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Han, X.; Dang, Y.; Meng, F.; Guo, X.; Lin, J. User Acceptance of Mobile Health Services from Users’ Perspectives: The Role of Self-Efficacy and Response-Efficacy in Technology Acceptance. Inform. Health Soc. Care 2017, 42, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.M. Diffusion of Innovations: Modifications of a Model for Telecommunications. In Die Diffusion von Innovationen in der Telekommunikation; Springer: Berlin/Heidelberg, Germany, 1995; pp. 25–38. [Google Scholar]
- Rodriguez-Gil, L.; Orduña, P.; García-Zubia, J.; López-de-Ipiña, D. Interactive Live-Streaming Technologies and Approaches for Web-Based Applications. Multimed. Tools Appl. 2018, 77, 6471–6502. [Google Scholar] [CrossRef]
- Clement, A.P.; Jiaming, F.; Li, L. Green Advertising and Purchase Decisions in Live-Streaming B2C and C2C Interactive Marketing. Int. J. Inf. Manag. Sci. 2020, 31, 191–212. [Google Scholar]
- Belanche, D.; Flavián, M.; Pérez-Rueda, A. Mobile Apps Use and WOM in the Food Delivery Sector: The Role of Planned Behavior, Perceived Security and Customer Lifestyle Compatibility. Sustainability 2020, 12, 4275. [Google Scholar] [CrossRef]
- Wu, X.; Guo, X.; Zhang, Z. The Efficacy of Mobile Phone Apps for Lifestyle Modification in Diabetes: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e12297. [Google Scholar] [CrossRef]
- Wood, C.S.; Thomas, M.R.; Budd, J.; Mashamba-Thompson, T.P.; Herbst, K.; Pillay, D.; Peeling, R.W.; Johnson, A.M.; McKendry, R.A.; Stevens, M.M. Taking Connected Mobile-Health Diagnostics of Infectious Diseases to the Field. Nature 2019, 566, 467–474. [Google Scholar] [CrossRef]
- Xiong, S.; Berkhouse, H.; Schooler, M.; Pu, W.; Sun, A.; Gong, E.; Yan, L.L. Effectiveness of MHealth Interventions in Improving Medication Adherence Among People with Hypertension: A Systematic Review. Curr. Hypertens. Rep. 2018, 20, 86. [Google Scholar] [CrossRef]
- Rajak, M.; Shaw, K. Evaluation and Selection of Mobile Health (MHealth) Applications Using AHP and Fuzzy TOPSIS. Technol. Soc. 2019, 59, 101186. [Google Scholar] [CrossRef]
- Coreil, J.; Levin, J.S.; Jaco, E.G. Life Style—An Emergent Concept in the Sociomedical Sciences. Cult. Med. Psychiatry 1985, 9, 423–437. [Google Scholar]
- Horley, J. A Longitudinal Examination of Lifestyles. Soc. Indic. Res. 1992, 26, 205–219. [Google Scholar] [CrossRef]
- Sequi-Dominguez, I.; Alvarez-Bueno, C.; Martinez-Vizcaino, V.; Fernandez-Rodriguez, R.; del Saz Lara, A.; Cavero-Redondo, I. Effectiveness of Mobile Health Interventions Promoting Physical Activity and Lifestyle Interventions to Reduce Cardiovascular Risk among Individuals with Metabolic Syndrome: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Cenfetelli, R.; Benbasat, I. The Influence of E-Commerce Live Streaming on Lifestyle Fit Uncertainty and Online Purchase Intention of Experience Products. In Proceedings of the Annual Hawaii International Conference on System Sciences, Maui, HI, USA, 8–11 January 2019; pp. 5081–5090. [Google Scholar]
- Zhang, Y.; Li, X.; Hamari, J. How Does Mobility Affect Social Media Advertising Effectiveness? A Study in WeChat. Ind. Manag. Data Syst. 2020, 120, 2081–2101. [Google Scholar] [CrossRef]
- Lee, H.J. The Effect of Anti-Consumption Lifestyle on Consumer’s Attitude and Purchase Intention toward Commercial Sharing Systems. Asia Pac. J. Mark. Logist. 2019, 31, 1422–1441. [Google Scholar] [CrossRef]
- Michaelidou, N.; Hassan, L.M. Modeling the Factors Affecting Rural Consumers’ Purchase of Organic and Free-Range Produce: A Case Study of Consumers’ from the Island of Arran in Scotland, UK. Food Policy 2010, 35, 130–139. [Google Scholar] [CrossRef]
- Lederer, A.L.; Maupin, D.J.; Sena, M.P.; Zhuang, Y. Technology Acceptance Model and the World Wide Web. Decis. Support Syst. 2000, 29, 269–282. [Google Scholar] [CrossRef]
- Xu, X.; Wu, J.H.; Li, Q. What Drives Consumer Shopping Behavior in Live Streaming Commerce? J. Electron. Commer. Res. 2020, 21, 144–167. [Google Scholar]
- Dong, X.; Zhao, H.; Li, T. The Role of Live-Streaming E-Commerce on Consumers’ Purchasing Intention Regarding Green Agricultural Products. Sustainability 2022, 14, 4374. [Google Scholar] [CrossRef]
- Handayani, P.W.; Meigasari, D.A.; Pinem, A.A.; Hidayanto, A.N.; Ayuningtyas, D. Critical Success Factors for Mobile Health Implementation in Indonesia. Heliyon 2018, 4, e00981. [Google Scholar] [CrossRef]
- Lu, B.; Chen, Z. Live Streaming Commerce and Consumers’ Purchase Intention: An Uncertainty Reduction Perspective. Inf. Manag. 2021, 58, 103509. [Google Scholar] [CrossRef]
- Kaplan, B. Revisiting Health Information Technology Ethical, Legal, and Social Issues and Evaluation: Telehealth/Telemedicine and COVID-19. Int. J. Med. Inform. 2020, 143, 104239. [Google Scholar] [CrossRef] [PubMed]
- Palmer, M.T. Interpersonal Communication and Virtual Reality: Mediating Interpersonal Relationships. In Communication in the Age of Virtual Reality; Routledge: London, UK, 1995; pp. 277–299. [Google Scholar]
- Sun, Y.; Shao, X.; Li, X.; Guo, Y.; Nie, K. How Live Streaming Influences Purchase Intentions in Social Commerce: An IT Affordance Perspective. Electron. Commer. Res. Appl. 2019, 37, 100886. [Google Scholar] [CrossRef]
- Huang, T.L. Restorative Experiences and Online Tourists’ Willingness to Pay a Price Premium in an Augmented Reality Environment. J. Retail. Consum. Serv. 2021, 58, 102256. [Google Scholar] [CrossRef]
- Shin, D. How Does Immersion Work in Augmented Reality Games? A User-Centric View of Immersion and Engagement. Inf. Commun. Soc. 2019, 22, 1212–1229. [Google Scholar] [CrossRef]
- Fang, J.; Chen, L.; Wen, C.; Prybutok, V.R. Co-Viewing Experience in Video Websites: The Effect of Social Presence on E-Loyalty. Int. J. Electron. Commer. 2018, 22, 446–476. [Google Scholar] [CrossRef]
- Song, H.K.; Baek, E.; Choo, H.J. Try-on Experience with Augmented Reality Comforts Your Decision: Focusing on the Roles of Immersion and Psychological Ownership. Inf. Technol. People 2020, 33, 1214–1234. [Google Scholar] [CrossRef]
- Chen, J.H.; Fu, J.R. On the Effects of Perceived Value in the Mobile Moment. Electron. Commer. Res. Appl. 2018, 27, 118–128. [Google Scholar] [CrossRef]
- Zhang, J.; Luximon, Y.; Li, Q. Seeking Medical Advice in Mobile Applications: How Social Cue Design and Privacy Concerns Influence Trust and Behavioral Intention in Impersonal Patient–Physician Interactions. Comput. Human Behav. 2022, 130, 107178. [Google Scholar] [CrossRef]
- Yim, M.Y.C.; Chu, S.C.; Sauer, P.L. Is Augmented Reality Technology an Effective Tool for E-Commerce? An Interactivity and Vividness Perspective. J. Interact. Mark. 2017, 39, 89–103. [Google Scholar] [CrossRef]
- Jung, N.; Im, S. The Mechanism of Social Media Marketing: Influencer Characteristics, Consumer Empathy, Immersion, and Sponsorship Disclosure. Int. J. Advert. 2021, 40, 1265–1293. [Google Scholar] [CrossRef]
- Chengoden, R.; Victor, N.; Huynh-The, T.; Yenduri, G.; Jhaveri, R.H.; Alazab, M.; Bhattacharya, S.; Hegde, P.; Maddikunta, P.K.R.; Gadekallu, T.R. Metaverse for Healthcare: A Survey on Potential Applications, Challenges and Future Directions. arXiv 2022, arXiv:2209.04160. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural Equation Modeling in Practice: A Review and Recommended Two-Step Approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Hair Jr, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage Publications: Thousand Oaks, CA, USA, 2021; pp. 174–180. [Google Scholar]
- Yuan, K.; Wu, R.; Bentler, P.M. Ridge Structural Equation Modelling with Correlation Matrices for Ordinal and Continuous Data. Br. J. Math. Stat. Psychol. 2011, 64, 107–133. [Google Scholar] [CrossRef] [PubMed]
- Lijauco, F.; Gajendran, T.; Brewer, G.; Rasoolimanesh, S.M. Impacts of Culture on Innovation Propensity in Small to Medium Enterprises in Construction. J. Constr. Eng. Manag. 2020, 146, 04019116. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 17th ed.; Kennesaw State University: Kennesaw, GA, USA, 2014. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Chin, W.W. The Partial Least Squares Approach to Structural Equation Modeling. Modern Methods Bus. Res. 1998, 295, 295–336. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common Method Biases in Behavioral Research: A Critical Review of the Literature and Recommended Remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Kock, N. Common Method Bias in PLS-SEM: A Full Collinearity Assessment Approach. Int. J. e-Collab. 2015, 11, 1–10. [Google Scholar] [CrossRef]
- Iacobucci, D. Structural Equations Modeling: Fit Indices, Sample Size, and Advanced Topics. J. Consum. Psychol. 2010, 20, 90–98. [Google Scholar] [CrossRef]
- Iacobucci, D. Everything You Always Wanted to Know about SEM (Structural Equations Modeling) but were Afraid to Ask. J. Consum. Psychol. 2009, 19, 673–680. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988; pp. 410–414. [Google Scholar]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a Silver Bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Helm, S.; Eggert, A.; Garnefeld, I. Modeling the Impact of Corporate Reputation on Customer Satisfaction and Loyalty Using Partial Least Squares. In Handbook of Partial Least Squares; Springer: Berlin/Heidelberg, Germany, 2010; pp. 515–534. [Google Scholar]
- Merli, R.; Preziosi, M.; Acampora, A.; Ali, F. Why Should Hotels Go Green? Insights from Guests Experience in Green Hotels. Int. J. Hosp. Manag. 2019, 81, 169–179. [Google Scholar] [CrossRef]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. Partial Least Squares Structural Equation Modeling: Rigorous Applications, Better Results and Higher Acceptance. Long Range Plann. 2013, 46, 1–12. [Google Scholar] [CrossRef]
- Surendran, A.; Sekar, C. An Economic Analysis of Willingness to Pay (WTP) for Conserving the Biodiversity. Int. J. Soc. Econ. 2010, 37, 637–648. [Google Scholar] [CrossRef]
- Leung, L.; Chen, C. E-Health/m-Health Adoption and Lifestyle Improvements: Exploring the Roles of Technology Readiness, the Expectation-Confirmation Model, and Health-Related Information Activities. Telecomm. Policy 2019, 43, 563–575. [Google Scholar] [CrossRef]
- Zarei, G.; Asgarnezhad Nuri, B.; Noroozi, N. The Effect of Internet Service Quality on Consumers’ Purchase Behavior: The Role of Satisfaction, Attitude, and Purchase Intention. J. Internet Commer. 2019, 18, 197–220. [Google Scholar] [CrossRef]
- Guo, X.; Chen, S.; Zhang, X.; Ju, X.; Wang, X. Exploring Patients’ Intentions for Continuous Usage of MHealth Services: Elaboration-Likelihood Perspective Study. JMIR mHealth uHealth 2020, 8, e1725. [Google Scholar] [CrossRef]
- Xu, X.Y.; Tayyab, S.M.U. How the Intensity of the Immersive Experience Impels the Extent of Social Streaming App Dependency? An Empirical Assessment with Mediation and Moderation Effects. Telemat. Inform. 2021, 63, 101661. [Google Scholar] [CrossRef]
- Wang, X.; Wong, Y.D.; Liu, F.; Yuen, K.F. A Push–Pull–Mooring View on Technology-Dependent Shopping under Social Distancing: When Technology Needs Meet Health Concerns. Technol. Forecast. Soc. Change 2021, 173, 121109. [Google Scholar] [CrossRef]
- Sax, M. Optimization of What? For-Profit Health Apps as Manipulative Digital Environments. Ethics Inf. Technol. 2021, 23, 345–361. [Google Scholar] [CrossRef]
- Chang, H.P.; Ma, C.C.; Chen, H.S. The Impacts of Young Consumers’ Health Values on Functional Beverages Purchase Intentions. Int. J. Environ. Res. Public Health 2020, 17, 3479. [Google Scholar] [CrossRef] [PubMed]
- San-Martín, S.; Jimenez, N.; Camarero, C.; San-José, R. The Path between Personality, Self-Efficacy, and Shopping Regarding Games Apps. J. Theor. Appl. Electron. Commer. Res. 2020, 15, 59–75. [Google Scholar] [CrossRef]
- Peña-García, N.; Gil-Saura, I.; Rodríguez-Orejuela, A.; Siqueira-Junior, J.R. Purchase Intention and Purchase Behavior Online: A Cross-Cultural Approach. Heliyon 2020, 6, e04284. [Google Scholar] [CrossRef] [PubMed]
- Avery, E.J.; Park, S. Perceived Knowledge as [Protective] Power: Parents’ Protective Efficacy, Information-Seeking, and Scrutiny during COVID-19. Health Commun. 2021, 36, 81–88. [Google Scholar] [CrossRef]
- Tyrväinen, O.; Karjaluoto, H. Online Grocery Shopping before and during the COVID-19 Pandemic: A Meta-Analytical Review. Telemat. Inform. 2022, 71, 101839. [Google Scholar] [CrossRef]
- Son, J.; Jin, B.; George, B. Consumers’ Purchase Intention toward Foreign Brand Goods. Manag. Decis. 2013, 51, 434–450. [Google Scholar] [CrossRef]
- Popovič, A.; Hackney, R.; Coelho, P.S.; Jaklič, J. Towards Business Intelligence Systems Success: Effects of Maturity and Culture on Analytical Decision Making. Decis. Support Syst. 2012, 54, 729–739. [Google Scholar] [CrossRef]
- Stoyanov, S.R.; Hides, L.; Kavanagh, D.J.; Zelenko, O.; Tjondronegoro, D.; Mani, M. Mobile App Rating Scale: A New Tool for Assessing the Quality of Health Mobile Apps. JMIR mHealth uHealth 2015, 3, e3422. [Google Scholar] [CrossRef]
- Aceto, G.; Persico, V.; Pescapé, A. Industry 4.0 and Health: Internet of Things, Big Data, and Cloud Computing for Healthcare 4.0. J. Ind. Inf. Integr. 2020, 18, 100129. [Google Scholar] [CrossRef]
- Ahsan, M.M.; Siddique, Z. Industry 4.0 in Healthcare: A Systematic Review. Int. J. Inf. Manag. Data Insights 2022, 2, 100079. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.N. How Purchase Intention Consummates Purchase Behaviour: The Stochastic Nature of Product Valuation in Electronic Commerce. Behav. Inf. Technol. 2015, 34, 57–68. [Google Scholar] [CrossRef]
- Dhir, A.; Malodia, S.; Awan, U.; Sakashita, M.; Kaur, P. Extended Valence Theory Perspective on Consumers’ e-Waste Recycling Intentions in Japan. J. Clean. Prod. 2021, 312, 127443. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, K. A Quality Measurement Method of Context Information in Ubiquitous Environments. In Proceedings of the Proceedings—2006 International Conference on Hybrid Information Technology, ICHIT 2006, Cheju, Korea, 9 November 2006; pp. 576–581. [Google Scholar]
- Song, S.; Zhao, Y.C.; Yao, X.; Ba, Z.; Zhu, Q. Short Video Apps as a Health Information Source: An Investigation of Affordances, User Experience and Users’ Intention to Continue the Use of TikTok. Internet Res. 2021, 31, 2120–2142. [Google Scholar] [CrossRef]
- Reychav, I.; Beeri, R.; Balapour, A.; Raban, D.R.; Sabherwal, R.; Azuri, J. How Reliable Are Self-Assessments Using Mobile Technology in Healthcare? The Effects of Technology Identity and Self-Efficacy. Comput. Human Behav. 2019, 91, 52–61. [Google Scholar] [CrossRef]
- Ajzen, I.; Fishbein, M. Attitude-Behavior Relations: A Theoretical Analysis and Review of Empirical Research. Psychol. Bull. 1977, 84, 888–918. [Google Scholar] [CrossRef]
- Deng, Z.; Mo, X.; Liu, S. Comparison of the Middle-Aged and Older Users’ Adoption of Mobile Health Services in China. Int. J. Med. Inform. 2014, 83, 210–224. [Google Scholar] [CrossRef]
| Characteristics | Frequency | Percent (%) |
|---|---|---|
| Gender | ||
| Male | 269 | 53.2% |
| Female | 237 | 46.8% |
| Age | ||
| 20s | 63 | 12.5% |
| 30s | 150 | 39.6% |
| 40s | 162 | 32.0% |
| 50s | 131 | 15.9% |
| Mean age = 41.49 years old | ||
| Education level | ||
| High school certificate or below | 79 | 15.6% |
| Technical school | 97 | 19.2% |
| Undergraduate degree | 267 | 52.8% |
| Master or higher degree | 63 | 12.4% |
| Monthly household income, $ | ||
| <700 | 32 | 6.3% |
| (700, 1200] | 188 | 37.2% |
| (1200, 1700] | 206 | 40.7% |
| >1700 | 80 | 15.8% |
| Mobile live streaming experience | ||
| Under 1 year | 56 | 11.0% |
| 1–3 years | 225 | 44.5% |
| Over 3 years | 225 | 44.5% |
| Disease type | ||
| Chronic disease | 279 | 55.1% |
| Acute disease | 227 | 44.9% |
| Variables | Items | Ladings | Cronbach’s α | CR | Rho_A | AVE |
|---|---|---|---|---|---|---|
| Preferred lifestyle (PL) | PL1 | 0.875 | 0.844 | 0.906 | 0.846 | 0.763 |
| PL2 | 0.838 | |||||
| PL3 | 0.858 | |||||
| Information quality (IQ) | IQ1 | 0.867 | 0.838 | 0.903 | 0.849 | 0.755 |
| IQ2 | 0.844 | |||||
| IQ3 | 0.896 | |||||
| Interactive immersion (II) | II1 | 0.879 | 0.904 | 0.940 | 0.910 | 0.839 |
| II2 | 0.858 | |||||
| II3 | 0.856 | |||||
| Self-efficacy (SE) | SE1 | 0.879 | 0.817 | 0.891 | 0.831 | 0.731 |
| SE2 | 0.873 | |||||
| SE3 | 0.868 | |||||
| Subjective norms (SN) | SN1 | 0.858 | 0.832 | 0.899 | 0.838 | 0.747 |
| SN2 | 0.823 | |||||
| SN3 | 0.883 | |||||
| Attitude (AT) | AT1 | 0.921 | 0.854 | 0.911 | 0.854 | 0.774 |
| AT2 | 0.932 | |||||
| AT3 | 0.895 | |||||
| Willingness to pay (WTP) | WTP1 | 0.884 | 0.820 | 0.893 | 0.822 | 0.735 |
| WTP2 | 0.889 | |||||
| WTP3 | 0.865 |
| Items | (1) PL | (2) IQ | (3) II | (4) SE | (5) SN | (6) AT | (7) WTP |
|---|---|---|---|---|---|---|---|
| (1) PL | 0.873 | ||||||
| (2) IQ | 0.465 | 0.869 | |||||
| (3) II | 0.537 | 0.495 | 0.916 | ||||
| (4) SE | 0.526 | 0.456 | 0.351 | 0.855 | |||
| (5) SN | 0.468 | 0.350 | 0.475 | 0.482 | 0.865 | ||
| (6) AT | 0.530 | 0.579 | 0.438 | 0.540 | 0.528 | 0.880 | |
| (7) WTP | 0.607 | 0.534 | 0.545 | 0.519 | 0.476 | 0.590 | 0.857 |
| Items | (1) PL | (2) IQ | (3) II | (4) SE | (5) SN | (6) AT | (7) WTP |
|---|---|---|---|---|---|---|---|
| PL1 | 0.875 | 0.498 | 0.424 | 0.576 | 0.473 | 0.451 | 0.519 |
| PL2 | 0.838 | 0.385 | 0.405 | 0.486 | 0.427 | 0.468 | 0.498 |
| PL3 | 0.858 | 0.485 | 0.394 | 0.496 | 0.432 | 0.484 | 0.501 |
| IQ1 | 0.408 | 0.867 | 0.259 | 0.391 | 0.416 | 0.384 | 0.490 |
| IQ2 | 0.473 | 0.844 | 0.226 | 0.353 | 0.347 | 0.415 | 0.430 |
| IQ3 | 0.505 | 0.896 | 0.409 | 0.459 | 0.423 | 0.484 | 0.576 |
| II1 | 0.444 | 0.290 | 0.879 | 0.402 | 0.412 | 0.478 | 0.440 |
| II2 | 0.364 | 0.300 | 0.858 | 0.404 | 0.395 | 0.364 | 0.465 |
| II3 | 0.418 | 0.319 | 0.856 | 0.409 | 0.441 | 0.379 | 0.466 |
| SE1 | 0.568 | 0.416 | 0.426 | 0.879 | 0.464 | 0.449 | 0.454 |
| SE2 | 0.491 | 0.431 | 0.357 | 0.873 | 0.472 | 0.458 | 0.443 |
| SE3 | 0.528 | 0.372 | 0.438 | 0.868 | 0.442 | 0.499 | 0.489 |
| SN1 | 0.445 | 0.400 | 0.391 | 0.474 | 0.858 | 0.323 | 0.429 |
| SN2 | 0.378 | 0.396 | 0.447 | 0.463 | 0.823 | 0.296 | 0.477 |
| SN3 | 0.496 | 0.380 | 0.407 | 0.420 | 0.883 | 0.286 | 0.482 |
| AT1 | 0.489 | 0.438 | 0.440 | 0.498 | 0.336 | 0.921 | 0.386 |
| AT2 | 0.542 | 0.468 | 0.449 | 0.507 | 0.370 | 0.932 | 0.431 |
| AT3 | 0.462 | 0.455 | 0.414 | 0.469 | 0.253 | 0.895 | 0.384 |
| WTP1 | 0.520 | 0.491 | 0.455 | 0.456 | 0.504 | 0.364 | 0.884 |
| WTP2 | 0.511 | 0.535 | 0.451 | 0.491 | 0.458 | 0.427 | 0.889 |
| WTP3 | 0.527 | 0.500 | 0.486 | 0.450 | 0.463 | 0.364 | 0.865 |
| Construct | VIF | Construct | VIF |
|---|---|---|---|
| PL1 | 2.047 | SN1 | 1.961 |
| PL2 | 2.113 | SN2 | 2.008 |
| PL3 | 1.926 | SN3 | 1.806 |
| IQ1 | 2.049 | AT1 | 2.218 |
| IQ2 | 1.819 | AT2 | 2.216 |
| IQ3 | 2.105 | AT3 | 1.951 |
| II1 | 3.148 | WTP1 | 1.933 |
| II2 | 3.252 | WTP2 | 1.734 |
| II3 | 2.539 | WTP3 | 1.852 |
| SE1 | 1.821 | ||
| SE2 | 1.739 | ||
| SE3 | 1.898 |
| Hypotheses | Path Coefficient | Standard Deviation | Lower CI 2.5% | Upper CI 97.5% | p-Value | Supported | f2 | |
|---|---|---|---|---|---|---|---|---|
| H1 | AT→WTP | 0.203 | 0.065 | 0.074 | 0.328 | 0.002 | Yes | |
| H2 | SN→WTP | 0.058 | 0.052 | −0.042 | 0.161 | 0.266 | No | 0.004 |
| H3 | SE→WTP | 0.127 | 0.049 | 0.033 | 0.227 | 0.010 | Yes | 0.020 |
| H4 | PL→AT | 0.302 | 0.048 | 0.209 | 0.394 | 0.000 | Yes | 0.105 |
| H5 | IQ→AT | 0.399 | 0.050 | 0.297 | 0.494 | 0.000 | Yes | 0.194 |
| H6 | II→AT | 0.078 | 0.046 | −0.012 | 0.168 | 0.092 | No | 0.007 |
| Hypotheses | Path Coefficient | Standard Deviation | Lower CI 2.5% | Upper CI 97.5% | Bias-Corrected Lower CI 2.5% | Bias-Corrected Upper CI 97.5% | Lower CI 2.5% | |
|---|---|---|---|---|---|---|---|---|
| Standardized direct effects | ||||||||
| H4a | PL→WTP | 0.244 | 0.048 | 0.150 | 0.339 | 0.150 | 0.339 | 0.000 |
| H5a | IQ→WTP | 0.132 | 0.047 | 0.038 | 0.022 | 0.044 | 0.227 | 0.005 |
| H6a | II→WTP | 0.188 | 0.044 | 0.100 | 0.274 | 0.099 | 0.274 | 0.000 |
| Standardized indirect effects | ||||||||
| H4a | PL→WTP | 0.062 | 0.021 | 0.022 | 0.106 | 0.026 | 0.110 | 0.004 |
| H5a | IQ→WTP | 0.081 | 0.030 | 0.027 | 0.143 | 0.028 | 0.146 | 0.007 |
| H6a | II→WTP | 0.016 | 0.011 | −0.002 | 0.040 | −0.001 | 0.044 | 0.145 |
| Standardized total effects | ||||||||
| H4a | PL→WTP | 0.305 | 0.048 | 0.210 | 0.397 | 0.211 | 0.398 | 0.000 |
| H5a | IQ→WTP | 0.213 | 0.053 | 0.104 | 0.314 | 0.109 | 0.317 | 0.000 |
| H6a | II→WTP | 0.203 | 0.065 | 0.112 | 0.294 | 0.111 | 0.292 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, F.; Huang, X.; Wang, X. Willingness to Pay for Mobile Health Live Streaming during the COVID-19 Pandemic: Integrating TPB with Compatibility. Sustainability 2022, 14, 15932. https://doi.org/10.3390/su142315932
Lu F, Huang X, Wang X. Willingness to Pay for Mobile Health Live Streaming during the COVID-19 Pandemic: Integrating TPB with Compatibility. Sustainability. 2022; 14(23):15932. https://doi.org/10.3390/su142315932
Chicago/Turabian StyleLu, Fuyong, Xian Huang, and Xintao Wang. 2022. "Willingness to Pay for Mobile Health Live Streaming during the COVID-19 Pandemic: Integrating TPB with Compatibility" Sustainability 14, no. 23: 15932. https://doi.org/10.3390/su142315932
APA StyleLu, F., Huang, X., & Wang, X. (2022). Willingness to Pay for Mobile Health Live Streaming during the COVID-19 Pandemic: Integrating TPB with Compatibility. Sustainability, 14(23), 15932. https://doi.org/10.3390/su142315932






