Identification of Predictive Nursing Workload Factors: A Six Sigma Approach
Abstract
1. Introduction
1.1. Six Sigma in Healthcare
1.2. Methods for Identifying Factors Affecting Nursing Workload
2. Research Methodology
3. Case Study
3.1. Define
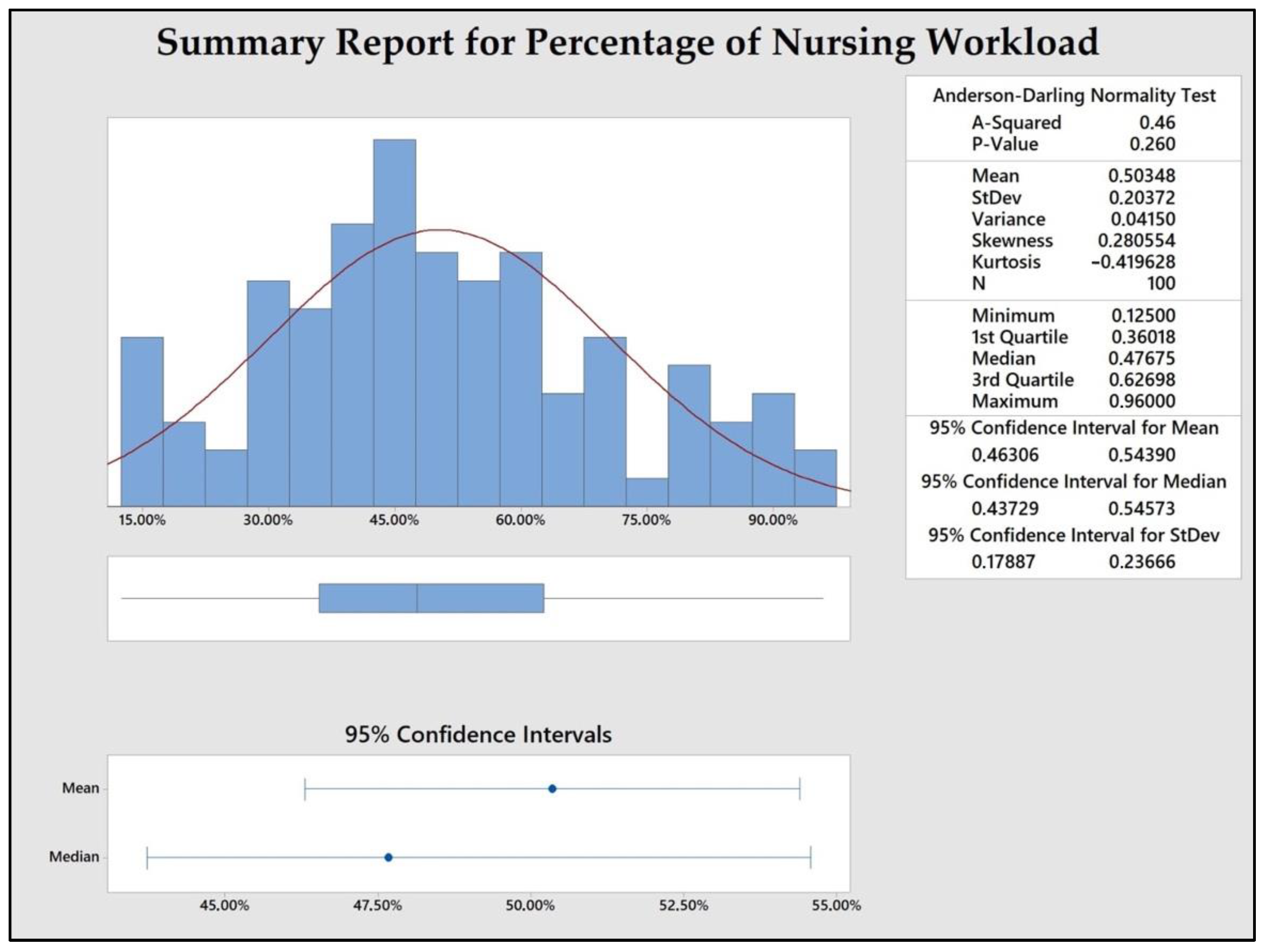
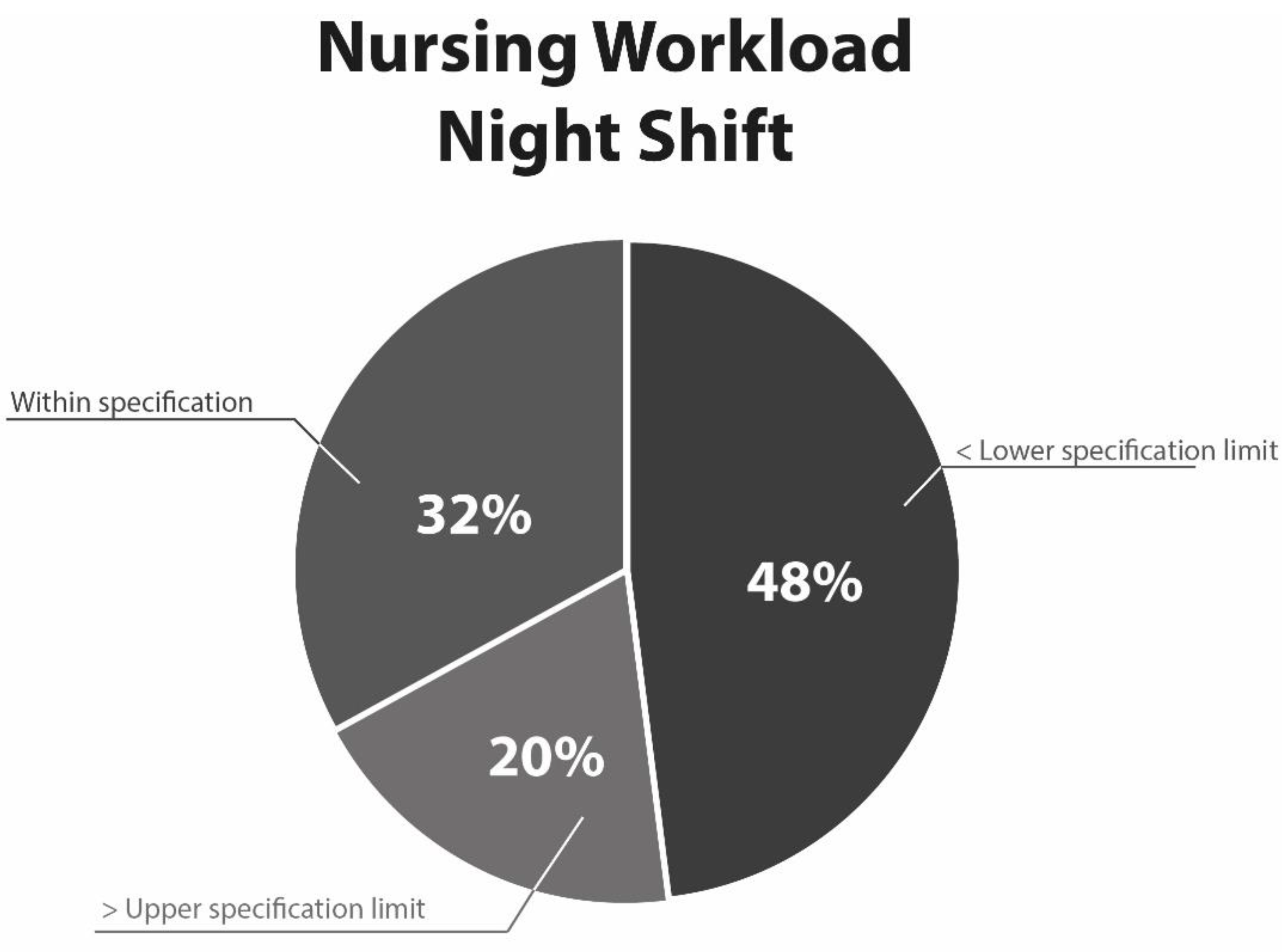
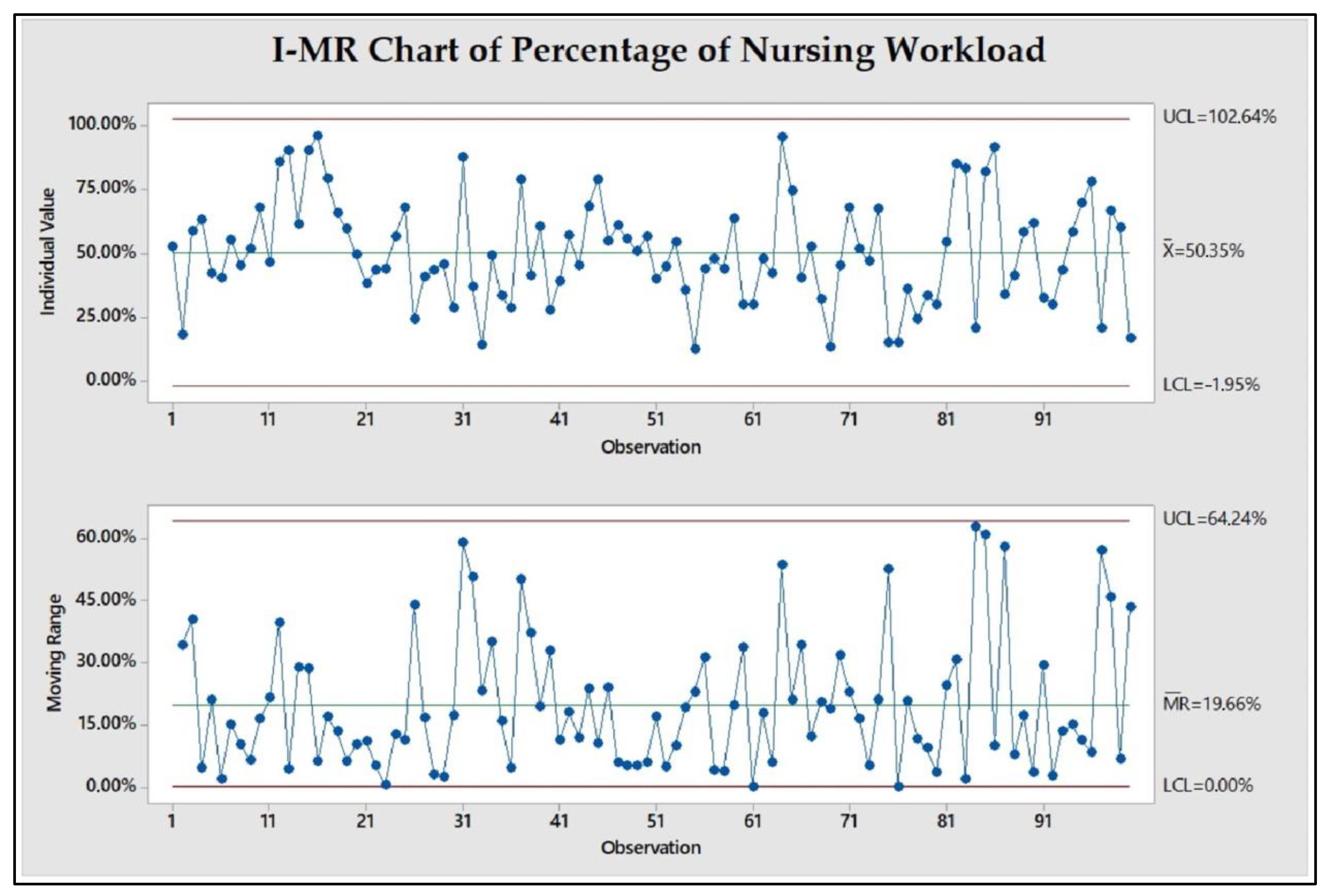
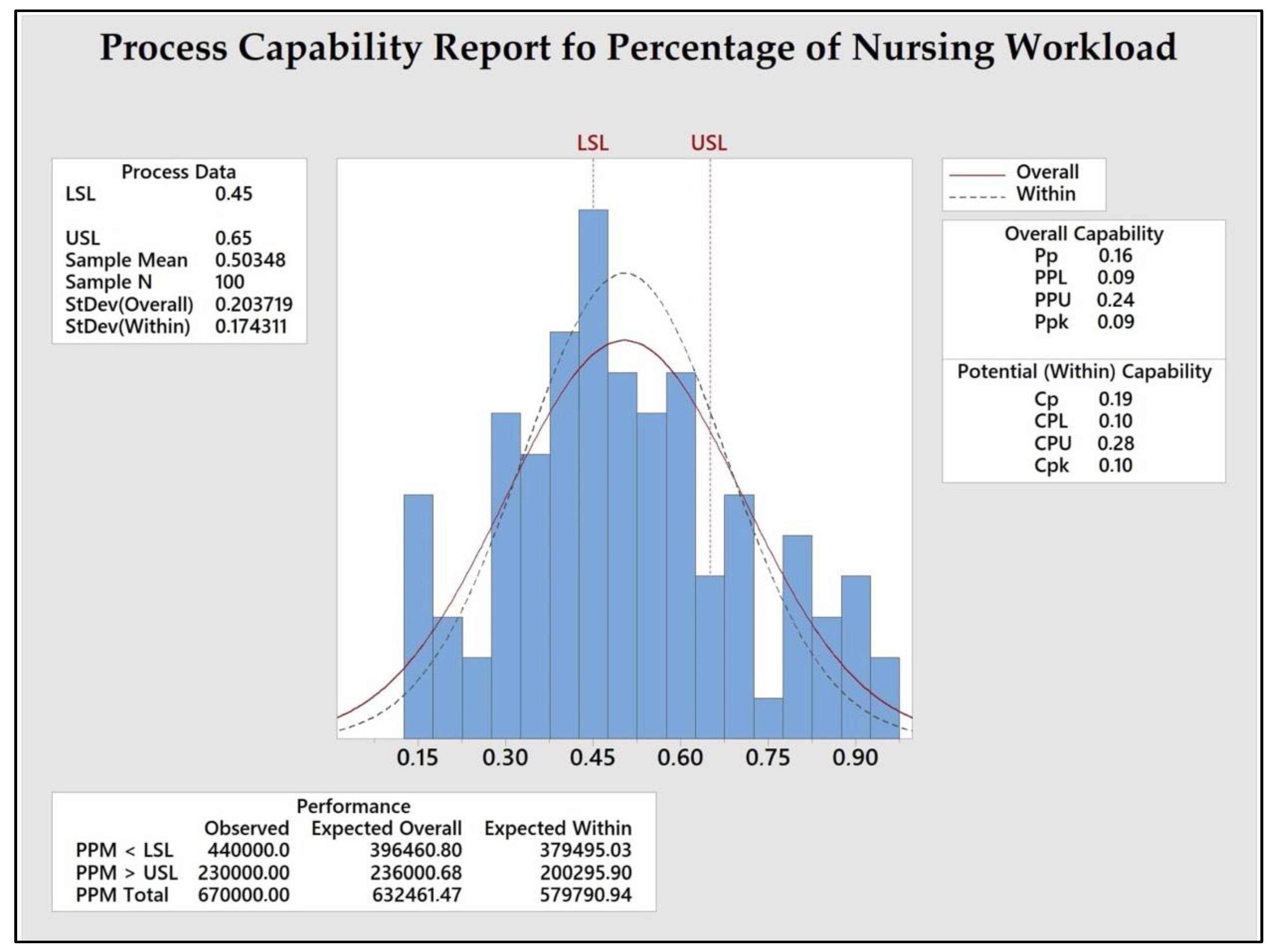
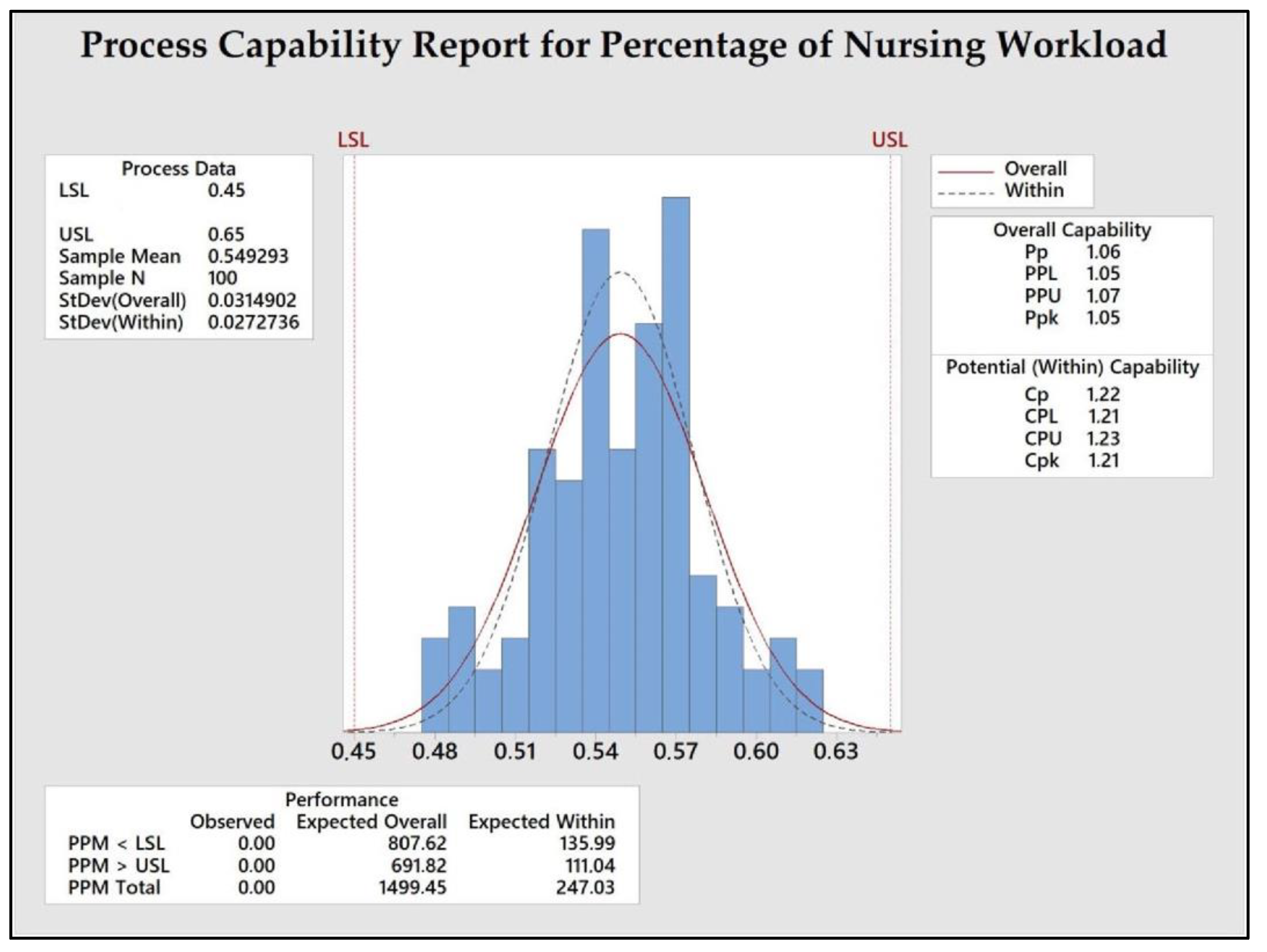
3.2. Measure
3.3. Analyze
3.4. Improve
- The number of times medication was administered per ward;
- The number of nurses assigned per ward;
- The shift.
3.5. Control
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moreno-Serra, R.; Anaya-Montes, M.; Smith, P.C. Potential determinants of health system efficiency: Evidence from Latin America and the Caribbean. PLoS ONE 2019, 14, e0216620. [Google Scholar] [CrossRef]
- Ortuzar, I.; Renart, G.; Xabadia, A. Effects of public healthcare budget cuts on life satisfaction in Spain. Soc. Indic. Res. 2021, 156, 311–337. [Google Scholar] [CrossRef]
- United Nations. Department of Economics Social Affairs, Popular Division, World Population Ageing: Highlights (ST/ESA/SER. A/430); United Nations: New York, NY, USA, 2019. [Google Scholar]
- Askari, M.; Klaver, N.S.; van Gestel, T.J.; van de Klundert, J. Intention to use medical apps among older adults in the Netherlands: Cross-sectional study. J. Med. Internet Res. 2020, 22, e18080. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 1–17. [Google Scholar] [CrossRef]
- Allen, S.B. The Nurse-Patient Assignment. J. Nurs. Adm. 2015, 45, 628–635. [Google Scholar] [CrossRef]
- Browne, J.; Braden, C.J. Nursing turbulence in critical care: Relationships with nursing workload and patient safety. Am. J. Crit. Care 2020, 29, 182–191. [Google Scholar] [CrossRef]
- Jansson, M.M.; Syrjälä, H.P.; Ala-Kokko, T.I. Association of nurse staffing and nursing workload with ventilator-associated pneumonia and mortality: A prospective, single-center cohort study. J. Hosp. Infect. 2019, 101, 257–263. [Google Scholar] [CrossRef]
- Brennan, C.W.; Daly, B.J.; Jones, K.R. State of the science: The relationship between nurse staffing and patient outcomes. West. J. Nurs. Res. 2013, 35, 760–794. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.-F.; Lee, S.; Chia, P.-F.; Chi, S.-C.; Yin, Y.-C. Exploring the association between nurse workload and nurse-sensitive patient safety outcome indicators. J. Nurs. Res. 2012, 20, 300–309. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidous, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Aycan, I.O.; Celen, M.K.; Yilmaz, A.; Almaz, M.S.; Dal, T.; Celik, Y.; Bolat, E. Colonización bacteriana debido al aumento de la carga de trabajo del equipo de enfermería en una unidad de cuidados intensivos. Rev. Bras. Anestesiol. 2015, 65, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Junttila, J.K.; Koivu, A.; Fagerström, L.; Haatainen, K.; Nykänen, P. Hospital mortality and optimality of nursing workload: A study on the predictive validity of the RAFAELA Nursing Intensity and Staffing system. Int. J. Nurs. Stud. 2016, 60, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.-H.; Kim, C.-W.; Lee, S.-Y. Nurse-perceived patient adverse events depend on nursing workload. Osong Public Health Res. Perspect. 2016, 7, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.-C.; Peng, N.L.; Fuang, N.H.; Sin, K.L. Impacts of job-related stress and patient safety culture on patient safety outcomes among nurses in Taiwan. Int. J. Healthc. Manag. 2021, 14, 1–9. [Google Scholar] [CrossRef]
- Muabbar, H.; Alsharqi, O. The impact of short-term solutions of nursing shortage on nursing outcome, nurse perceived quality of care, and patient safety. Am. J. Nurs. Res. 2021, 9, 35–44. [Google Scholar] [CrossRef]
- da Silva, R.; Baptista, A.; Serra, R.L.; Magalhães, D.S. Mobile application for the evaluation and planning of nursing workload in the intensive care unit. Int. J. Med. Inform. 2020, 137, 104120. [Google Scholar] [CrossRef]
- Holland, P.; Tham, T.L.; Sheehan, C.; Cooper, B. The impact of perceived workload on nurse satisfaction with work-life balance and intention to leave the occupation. Appl. Nurs. Res. 2019, 49, 70–76. [Google Scholar] [CrossRef]
- Sir, M.Y.; Dundar, B.; Steege, L.M.B.; Pasupathy, K.S. Nurse–patient assignment models considering patient acuity metrics and nurses’ perceived workload. J. Biomed. Inform. 2015, 55, 237–248. [Google Scholar] [CrossRef]
- Liang, B.; Turkcan, A. Acuity-based nurse assignment and patient scheduling in oncology clinics. Health Care Manag. Sci. 2016, 19, 207–226. [Google Scholar] [CrossRef]
- Hoi, S.Y.; Ismail, N.; Ong, L.C.; Kang, J. Determining nurse staffing needs: The workload intensity measurement system. J. Nurs. Manag. 2010, 18, 44–53. [Google Scholar] [CrossRef]
- Alghamdi, M.G. Nursing workload: A concept analysis. J. Nurs. Manag. 2016, 24, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.; MacNeela, P.; Scott, A.; Treacy, P.; Hyde, A. Reconsidering the conceptualization of nursing workload: Literature review. J. Adv. Nurs. 2007, 57, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Hauck, E.L.; Snyder, L.A.; Cox-Fuenzalida, L.-E. Workload variability and social support: Effects on stress and performance. Curr. Psychol. 2008, 27, 112–125. [Google Scholar] [CrossRef]
- Salah, S.; Rahim, A.; Carretero, J.A. The integration of Six Sigma and lean management. Int. J. Lean Six Sigma 2010, 1, 249–274. [Google Scholar] [CrossRef]
- Chakraborty, A.; Chuan, T.K. An empirical analysis on Six Sigma implementation in service organisations. Int. J. Lean Six Sigma 2013, 4, 141–170. [Google Scholar] [CrossRef]
- DelliFraine, J.L.; Wang, Z.; McCaughey, D.; Langabeer, J.R.; Erwin, C.O. The use of six sigma in health care management: Are we using it to its full potential? Qual. Manag. Healthc. 2013, 22, 210–223. [Google Scholar] [CrossRef]
- Varkey, P.; Kollengode, A. A framework for healthcare quality improvement in India: The time is here and now! J. Postgrad. Med. 2011, 57, 237. [Google Scholar] [CrossRef]
- Hussein, N.A.; Abdelmaguid, T.F.; Tawfik, B.S.; Ahmed, N.G. Mitigating overcrowding in emergency departments using Six Sigma and simulation: A case study in Egypt. Oper. Res. Health Care 2017, 15, 1–12. [Google Scholar] [CrossRef]
- Furterer, S.L. Applying Lean Six Sigma methods to reduce length of stay in a hospital’s emergency department. Qual. Eng. 2018, 30, 389–404. [Google Scholar] [CrossRef]
- Al-Qatawneh, L.; Abdallah, A.A.; Zalloum, S.S. Six sigma application in healthcare logistics: A framework and a case study. J. Healthc. Eng. 2019, 2019, 1–12. [Google Scholar] [CrossRef]
- Mason, S.; Nicolay, C.; Darzi, A. The use of Lean and Six Sigma methodologies in surgery: A systematic review. Surgeon 2015, 13, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Sunder, M.V.; Kunnath, N.R. Six Sigma to reduce claims processing errors in a healthcare payer firm. Prod. Plan. Control. 2020, 31, 496–511. [Google Scholar] [CrossRef]
- Bhat, S.; Antony, J.; Gijo, E.; Cudney, E.A. Lean Six Sigma for the healthcare sector: A multiple case study analysis from the Indian context. Int. J. Qual. Reliab. Manag. 2019, 37, 90–111. [Google Scholar] [CrossRef]
- Curatolo, N.; Lamouri, S.; Huet, J.-C.; Rieutord, A. A critical analysis of Lean approach structuring in hospitals. Bus. Process Manag. J. 2014, 20, 433–454. [Google Scholar] [CrossRef]
- Taner, M.T.; Kagan, G.; Çelik, S.; Erbas, E.; Kagan, M.K. Formation of Six Sigma infrastructure for the coronary stenting process. Int. Rev. Manag. Mark. 2013, 3, 232–242. [Google Scholar]
- Roberts, R.J.; Wilson, A.E.; Quezado, Z. Using Lean Six Sigma methodology to improve quality of the anesthesia supply chain in a pediatric hospital. Anesth. Analg. 2017, 124, 922–924. [Google Scholar] [CrossRef]
- Amaratunga, T.; Dobranowski, J. Systematic review of the application of lean and six sigma quality improvement methodologies in radiology. J. Am. Coll. Radiol. 2016, 13, 1088–1095. [Google Scholar] [CrossRef]
- Montella, E.; Di Cicco, M.V.; Ferraro, A.; Centobelli, P.; Raiola, E.; Triassi, M.; Improta, G. The application of Lean Six Sigma methodology to reduce the risk of healthcare–associated infections in surgery departments. J. Eval. Clin. Pract. 2017, 23, 530–539. [Google Scholar] [CrossRef]
- Peimbert-García, R.E.; Gutiérrez-Mendoza, L.M.; García-Reyes, H. Applying lean healthcare to improve the discharge process in a Mexican Academic Medical Center. Sustainability 2021, 13, 10911. [Google Scholar] [CrossRef]
- Nar, R.; Emekli, D.I. The evaluation of analytical performance of immunoassay tests by using six-sigma method. J. Med. Biochem. 2017, 36, 301–308. [Google Scholar] [CrossRef][Green Version]
- Punnakitikashem, P.; Rosenberger, J.M.; Behan, D.B. Stochastic programming for nurse assignment. Comput. Optim. Appl. 2008, 40, 321–349. [Google Scholar] [CrossRef]
- Allen, S. The nurse-patient assignment process: What clinical nurses and patients think. Medsurg. Nurs. 2018, 27, 77–82. [Google Scholar]
- Myny, D.; De Bacquer, D.; Van Hecke, A.; Beeckman, D.; Verhaeghe, S.; Van Goubergen, D. Validation of standard times and influencing factors during the development of the Workload Indicator for Nursing. J. Adv. Nurs. 2014, 70, 674–686. [Google Scholar] [CrossRef] [PubMed]
- Bahadori, M.; Ravangard, R.; Raadabadi, M.; Mosavi, S.M.; Fesharaki, M.G.; Mehrabian, F. Factors affecting intensive care units nursing workload. Iran. Red Crescent Med. J. 2014, 16, 8. [Google Scholar] [CrossRef]
- Busari, J.O.; Burghgraef, J.; Faverey, L.C. The workload Intens-o-meteR: A novel instrument designed to determine workload intensity and adequacy of nurse staffing in a pediatric ward. Int. J. Healthc. Manag. 2016, 9, 149–154. [Google Scholar] [CrossRef]
- Azimi Nayebi, B.; Mohebbifar, R.; Azimian, J.; Rafiei, S. Estimating nursing staff requirement in an emergency department of a general training hospital: Application of Workload Indicators of Staffing Need (WISN). Int. J. Healthc. Manag. 2019, 12, 54–59. [Google Scholar] [CrossRef]
- Moghri, J.; Kokabisaghi, F.; Tabatabaee, S.S. Nurse staffing norms in a hospital: Determining a golden standard using a new estimation method. Int. J. Healthc. Manag. 2021, 14, 1367–1372. [Google Scholar] [CrossRef]
- Ivziku, D.; Ferramosca, F.M.P.; Filomeno, L.; Gualandi, R.; De Maria, M.; Tartaglini, D. Defining nursing workload predictors: A pilot study. J. Nurs. Manag. 2022, 30, 473–481. [Google Scholar] [CrossRef]
- Yin, R.K. Case Study Research: Design and Methods; SAGE Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Flynn, B.B.; Sakakibara, S.; Schroeder, R.G.; Bates, K.A.; Flynn, E.J. Empirical research methods in operations management. J. Oper. Manag. 1990, 9, 250–284. [Google Scholar] [CrossRef]
- Hurst, K. Selecting and Applying Methods for Estimating the Size and Mix of Nursing Teams: A Systematic Review of the Literature Commissioned by the Department of Health; Nuffield Institute for Health: Leeds, UK, 2003. [Google Scholar]
- Riklikienė, O.; Didenko, O.; Čiutienė, R.; Daunorienė, A.; Čiarnienė, R. Balancing nurses’ workload: A case study with nurse anaesthetists and intensive care nurses. Econ. Sociol. 2020, 13, 11–25. [Google Scholar] [CrossRef]
- World Health Organization. WHO Nursing and Midwifery Progress Report 2008–2012; World Health Organization: Geneva, Switzerland, 2013.
- Buestán, M.N.; Pérez, C.C.; Castillo, R.; Ayala, A. Nursing-patient assignment optimization model using Lean Six Sigma in IIE Annual Conference. In Proceedings of the 2017 Institute of Industrial and Systems Engineers (IISE), Pittsburgh, PA, USA, 20–23 May 2017. [Google Scholar]
- Mark, B.A. What explains nurses’ perceptions of staffing adequacy? JONA J. Nurs. Adm. 2002, 32, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Souder, E.; O’Sullivan, P. Disruptive Behaviors of Older Adults in an Institutional Setting; SLACK Incorporated: Thorofare, NJ, USA, 2003; pp. 31–36. [Google Scholar]
- Spence, K.; Tarnow-Mordi, W.; Duncan, G.; Jayasuryia, N.; Elliott, J.; King, J.; Kite, F. Measuring nursing workload in neonatal intensive care. J. Nurs. Manag. 2006, 14, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Welton, J.M.; Decker, M.; Adam, J.; Zone-Smith, L. How far do nurses walk? Medsurg Nurs. 2006, 15, 213. [Google Scholar]
- Blegen, M.A.; Vaughn, T.; Vojir, C.P. Nurse staffing levels: Impact of organizational characteristics and registered nurse supply. Health Serv. Res. 2008, 43, 154–173. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.; Saville, C.; Ball, J.; Jones, J.; Pattison, N.; Monks, T. Nursing workload, nurse staffing methodologies and tools: A systematic scoping review and discussion. Int. J. Nurs. Stud. 2020, 103, 103487. [Google Scholar] [CrossRef] [PubMed]
- Özkan, Ş.; Yıldırım, T. General dentists staffing requirement based on workload in the public dental health centers in Turkey. Int. J. Healthc. Manag. 2022, 1–10. [Google Scholar] [CrossRef]
- Stankovic, S.; Milicevic, M.S. Use of the WISN method to assess the health workforce requirements for the high-volume clinical biochemical laboratories. Hum. Resour. Health 2022, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.F.; Plummer, V.; Lam, L.; Wang, Y.; Cross, W.; Zhang, J.P. The effects of resilience and turnover intention on nurses’ burnout: Findings from a comparative cross-sectional study. J. Clin. Nurs. 2019, 28, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Patri, R.; Suresh, M. Factors influencing lean implementation in healthcare organizations: An ISM approach. Int. J. Healthc. Manag. 2018, 11, 25–37. [Google Scholar] [CrossRef]
- Sreedharan, V.R.; Sunder, M.V.; Raju, R. Critical success factors of TQM, Six Sigma, Lean and Lean Six Sigma: A literature review and key findings. Benchmarking Int. J. 2018, 25, 3479–3504. [Google Scholar] [CrossRef]
- Singh, G.; Singh, D. CSFs for Six Sigma implementation: A systematic literature review. J. Asia Bus. Stud. 2020, 14, 795–818. [Google Scholar] [CrossRef]
- Antony, J.; Palsuk, P.; Gupta, S.; Mishra, D.; Barach, P. Six Sigma in healthcare: A systematic review of the literature. Int. J. Qual. Reliab. Manag. 2018, 35, 1075–1092. [Google Scholar] [CrossRef]
- Henrique, D.B.; Filho, M.G. A systematic literature review of empirical research in Lean and Six Sigma in healthcare. Total Qual. Manag. Bus. Excell. 2020, 31, 429–449. [Google Scholar] [CrossRef]


| Potential Factors | Statistical Tool | p-Value |
|---|---|---|
| X1: Number of patients per ward | Regression Analysis | <0.0001 |
| Number of patients from: X2: Intensive care unit/X3: Post-surgery | Multiple Regression Analysis | 0.801/0.853 |
| X4: Number of times medication administered per ward | Regression Analysis | <0.0001 |
| X5: Number of nurses assigned per ward | Regression Analysis | <0.0001 |
| X6: Hour of day | Pearson correlation | 0.051 |
| X7: Shift type | t-test | <0.0001 |
| X8: Ward | ANOVA | 0.20 |
| X9: Age of the nurses | Pearson correlation | 0.113 |
| X10: Years of experience | Pearson correlation | 0.637 |
| Day | Shift | Nurses | Number of Times Medication Administered | Predicted Nursing Workload | Observed Nursing Workload | Difference |
|---|---|---|---|---|---|---|
| 1 | 2 | 2 | 71 | 56.8% | 56.72% | 0.08% |
| 2 | 1 | 2 | 48 | 54.01% | 49.7% | 4.31% |
| 3 | 1 | 2 | 38.33 | 41.89% | 41.76% | 6.13% |
| 4 | 2 | 1 | 65.33 | 53.65% | 54.13% | 0.48% |
| 5 | 1 | 1 | 50 | 63.14% | 48.75% | 14.39% |
| 6 | 1 | 2 | 51 | 55.23% | 62.94% | 7.71% |
| 7 | 1 | 2 | 28 | 42.4% | 45% | 2.60% |
| Nursing workload average difference | 5.1% | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buestan, M.; Perez, C. Identification of Predictive Nursing Workload Factors: A Six Sigma Approach. Sustainability 2022, 14, 13169. https://doi.org/10.3390/su142013169
Buestan M, Perez C. Identification of Predictive Nursing Workload Factors: A Six Sigma Approach. Sustainability. 2022; 14(20):13169. https://doi.org/10.3390/su142013169
Chicago/Turabian StyleBuestan, Marcos, and Cinthia Perez. 2022. "Identification of Predictive Nursing Workload Factors: A Six Sigma Approach" Sustainability 14, no. 20: 13169. https://doi.org/10.3390/su142013169
APA StyleBuestan, M., & Perez, C. (2022). Identification of Predictive Nursing Workload Factors: A Six Sigma Approach. Sustainability, 14(20), 13169. https://doi.org/10.3390/su142013169





