Public Health System and Socio-Economic Development Coupling Based on Systematic Theory: Evidence from China
Abstract
1. Introduction
2. Theory and Methodology
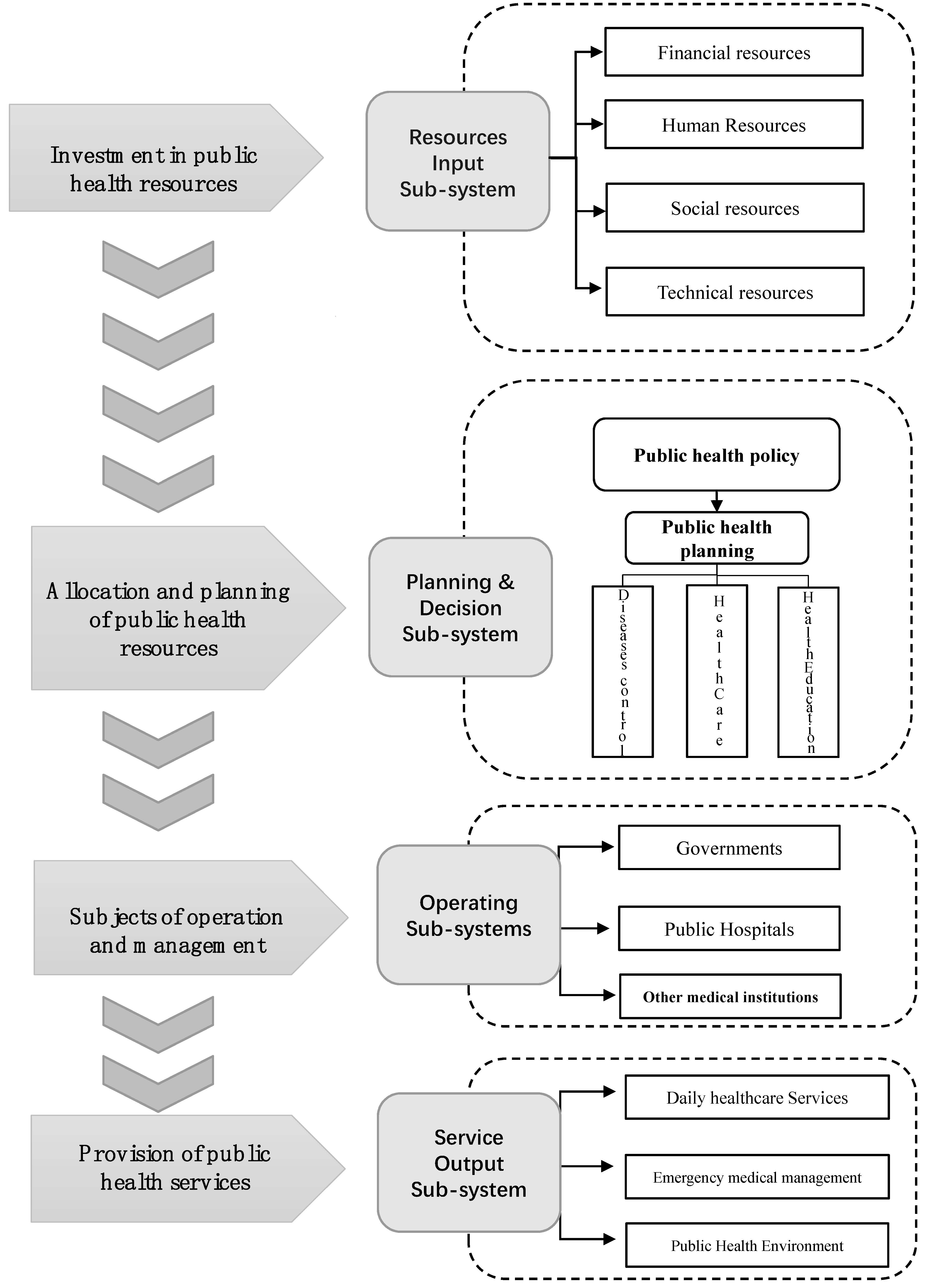
2.1. The Measurement of Public Health System Based on Systematic Theory
- (1)
- Resources input sub-system. Public health systems require a certain amount of resources to support them, mainly including human, financial, social, and technical recources. Generally speaking, a greater investment of resources means that the public health system can provide a richer range of health services to people. However, unlike private healthcare services, public health services often have a low price or are even free in some countries, so that excessive investment in public health resources may increase the financial pressure on the government.
- (2)
- Planning and decision sub-system. There is a key problem in the effective allocation and use the public health resources. According to the WHO report in 2007 (WHO, http://www.who.int/healthsystems/strategy/everybodys_business.pdf., accessed on 25 July 2022), public health systems should have seven main functions (service delivery, health workforce, information, medical products, vaccines and technologies, financing, leadership/governance), these functions can be summarised into three aspects: first, disease control and second, health care—this is the most basic function of the public health care system. The third is health education. With knowledge playing an increasingly important role in health management, health education has become a key factor in evaluating public health performance. The government should consider above three aspects in the process of making public health policies and programmes.
- (3)
- Operating sub-system. In reality, the level of cooperation between the multiple agencies determines whether the public health plans or policies can be implemented effectively. Firstly, the government plays the role of leader and manager in the public health care system. Secondly, public hospitals are health institutions that are funded by the government, including both large-scaled hospitals and small healthcare institutions such as community clinics and family doctors. Public hospitals are the micro direct providers of public health services. Third, other medical institutions, such as universities, public laboratories, and epidemiological institutions, are becoming increasingly active in the public health system because knowledge, technology and management become new types of factors affecting the efficiency of public health systems.
- (4)
- Service output sub-system. The ultimate aim of a public health system is to provide sustainable public healthcare for the public. Therefore, public health performance is an important element in the evaluation of public health systems. In addition to daily healthcare services, the capacity to deal with public health emergencies, medical care for vulnerable groups, health awareness development, and training of medical talents are also dimension of the evaluation of the output of public health services.
2.2. The Coupling of Public Health System and Socio-Economic Development
3. Data
3.1. Data on China’s Public Health System
- (1)
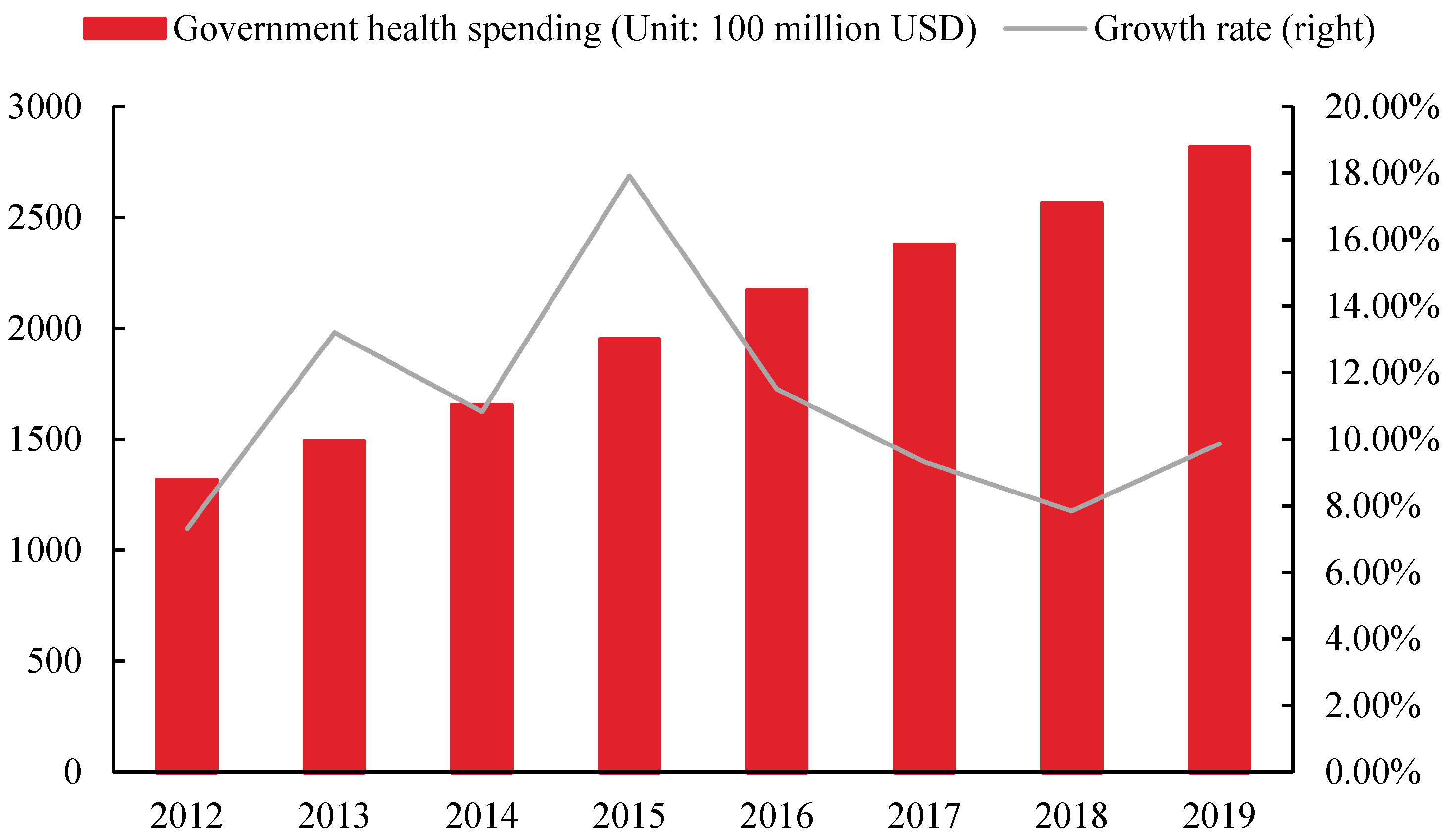
- Resources input sub-system. First, the human resource mainly selects the number of health technicians per 1000 population, the number of professionals in professional public health institutions and the number of primary medical and health institutions per 1000 population, which are used to measure the health personnel engaged in medical and scientific research, public health institutions, and primary medical institutions respectively. Second, government health expenditure is mainly used for measuring the level of financial security of public health services. Third, technology mainly chooses the number of equipment over 10,000 yuan in medical and health institutions to measure the technical level of public health services. Fourth, social is mainly selected per thousand the number of beds in medical institutions is used to measure the capacity of medical supplies.
- (2)
- Planning and decision sub-system. This paper chose the number of infectious disease prevented, the number of health supervision and punishment cases in public places, and the number of public health education activities to measure the ability of public health planning and decision.
- (3)
- Operating sub-system. First, the government usually does not directly participate in public health services. However, they provide public health services indirectly through human, financial, and material investment in medical institutions and public health institutions. Therefore, we select the scale of public health insurance in China to reflect the level of government participation in public health operations. Second, medical institutions mainly choose the number of hospitals and primary medical and health institutions, which are used to measure the situation of conventional medical institutions and primary medical institutions, respectively. Third, public hospitals mainly select the number of public health institutions.
- (4)
- Service output sub-system. First, we select the qualification rate of regular hygiene monitoring in public places to measure daily healthcare services. Second, the effective prevention and control of public health emergencies is mainly based on the incidence of notifiable infectious diseases in Class A and B. Class A and B notifiable infectious diseases are high-risk infectious diseases, and the lower the incidence rate indicates a lower probability of an outbreak. The third is to measure the increase in public health awareness by the number of health education programmes and people trained.
3.2. Data on Socio-Economics Development in China
4. Analysis of Measurement Results
4.1. Measurement of Public Health System in China
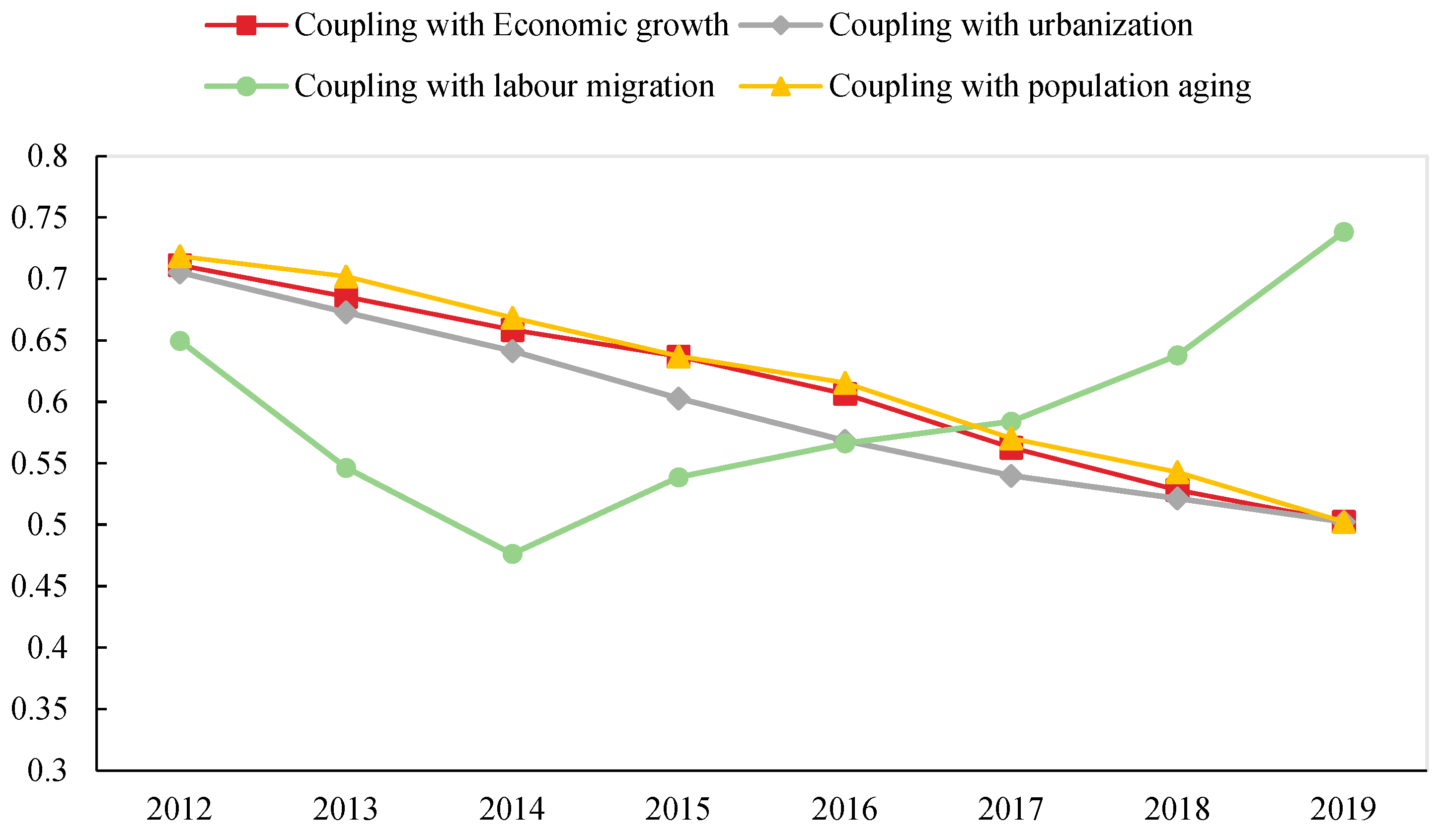
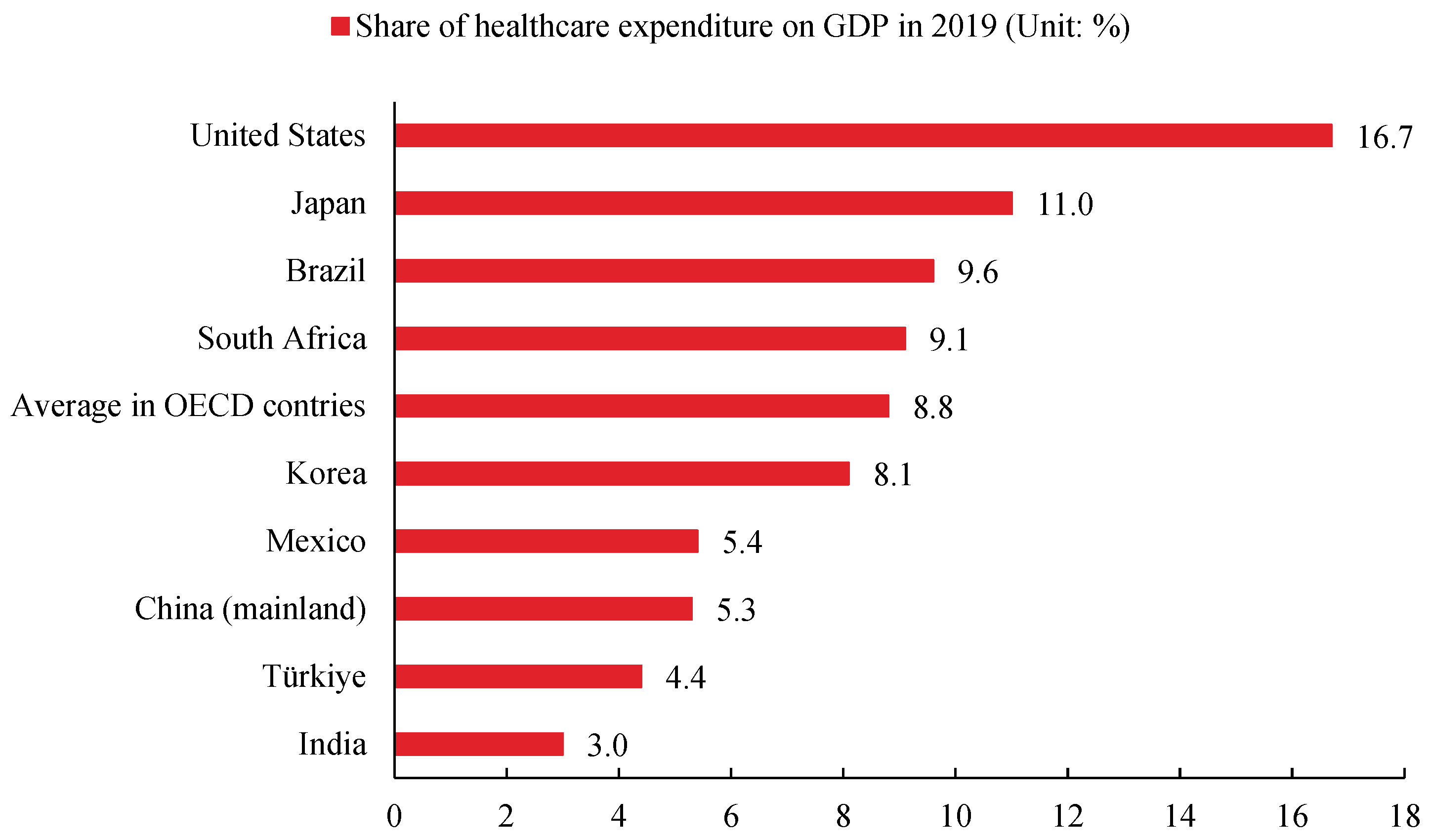
4.2. Mismatch between Public Health System and Socio-Economic Development in China
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| First-Level Indicator | Bottom Variables | Weights |
|---|---|---|
| Resources input sub-system | X1: Number of health technicians per 1000 population | 0.0441 |
| X2: Personnel in professional public health institutions per thousand population | 0.0512 | |
| X3: Number of staff in primary medical and health institutions | 0.0488 | |
| X4: Government health spending | 0.0506 | |
| X5: The number of medical and health institutions more than 10,000 yuan of equipment | 0.0484 | |
| X6: Number of professional public health institutions with equipment of more than 10,000 yuan | 0.0496 | |
| X7: Number of units of equipment above 10,000 yuan in primary health institutions | 0.0531 | |
| X8: Number of beds in medical institutions per 1000 people | 0.0443 | |
| X9: Number of hygienic beds in primary medical institutions | 0.0426 | |
| X10: Number of beds in professional public health institutions | 0.0417 | |
| Operating sub-system | X11: Number of hospitals | 0.0504 |
| X12: Number of primary medical and health institutions | 0.0543 | |
| X13: Number of professional public health institutions | 0.0608 | |
| Planning and decision sub-system | X14: Number of Infectious Disease Prevention Supervision and Punishment Cases | 0.0626 |
| X15: Number of visits to medical and health institutions | 0.0358 | |
| X16: The number of public places health supervision and punishment cases | 0.0492 | |
| X17: Number of public health education activities | 0.0320 | |
| Service output sub-system | X18: Class A and B notifiable infectious disease mortality | 0.0434 |
| X19: Qualification rate of regular hygiene monitoring in public places | 0.0412 | |
| X20: Number of health education trainees | 0.0538 | |
| X21: Incidence of Class A and B Notifiable Infectious Diseases | 0.0421 |
References
- Chen, X.; de Vries, S.; Assmuth, T.; Dick, J.; Hermans, T.; Hertel, O.; Jensen, A.; Jones, L.; Kabisch, S.; Lanki, T.; et al. Research challenges for cultural ecosystem services and public health in (peri-)urban environments. Sci. Total Environ. 2019, 651, 2118–2129. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F. Vaccination during a pandemic-a public health challenge. Indian J. Community Health 2020, 32, 617–619. [Google Scholar] [CrossRef]
- Jevtic, M.; Savic, S. One health in urban environment- public health challenge for the future. Eur. J. Public Health 2021, 31 (Suppl. S3), ckab164-566. [Google Scholar] [CrossRef]
- Navarro, J.A.; Markel, H. Politics, pushback, and pandemics: Challenges to public health orders in the 1918 influenza pandemic. Am. J. Public Health 2021, 111, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.J.; Turner, K.; Lichtenstein, C.M. Responding to the pandemic: Challenges with public health surveillance systems and development of a COVID-19 national surveillance case definition to support case-based morbidity surveillance during the early response. J. Public Health Manag. Pract. 2021, 27, S80–S86. [Google Scholar] [CrossRef]
- Clarfield, A.M.; Dwolatzky, T. Age and ageing during the COVID-19 pandemic; challenges to public health and to the health of the public. Front. Public Health 2021, 9, 655831. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Nguyen, H.; Dao, A.; Nguyen, T.; Nguyen, P.; Le, P.; Vu, K.; Tran, A.; Dao, P.; Nguyen, C.; et al. The COVID-19 pandemic in Australia: Public health responses, opportunities and challenges. Int. J. Health Plan. Manag. 2022, 37, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Koivusalo, M.; Mackintosh, M. Global public health security: Inequality, vulnerability and public health system capabilities: Assessment: Global public health security. Dev. Change 2008, 39, 1163–1169. [Google Scholar] [CrossRef]
- Defraites, R.F. The armed forces health surveillance center: Enhancing the military health systems public health capabilities. BMC Public Health 2011, 11, S1. [Google Scholar] [CrossRef]
- Månsdotter, A.; Ekman, B.; Feldman, I.; Hagberg, L.; Hurtig, A.; Lindholm, L. We propose a novel measure for social welfare and public health: Capability-adjusted life-years, CALYs. Appl. Health Econ. Health Policy 2017, 15, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Ahn, D.; Shin, H.; Kim, M.; Lee, S.; Kim, H.; Myoung, J.; Kim, B.; Kim, S. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). J. Microbiol. Biotechnol. 2020, 30, 313–324. [Google Scholar] [CrossRef]
- Mays, G.P.; Smith, S.A.; Ingram, R.C.; Racster, L.J.; Lamberth, C.D.; Lovely, E.S. Public health delivery systems. evidence, uncertainty, and emerging research needs. Am. J. Prev. Med. 2009, 36, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Rutter, H.; Savona, N.; Glonti, K.; Bibby, J.; Cummins, S.; Finegood, D.T.; Greaves, F.; Harper, L.; Hawe, P.; Moore, L.; et al. The need for a complex systems model of evidence for public health. Lancet 2017, 390, 2602–2604. [Google Scholar] [CrossRef]
- Nanda, M.; Aashima, S.R.; Aashima. COVID-19: A comprehensive review of epidemiology and public health system response in nordic region. Int. J. Health Serv. 2021, 51, 287–299. [Google Scholar] [CrossRef] [PubMed]
- von Bertalanffy, L. General System Theory: Foundations, Development, Applications; George Braziller Incorporated: New York, NY, USA, 1969. [Google Scholar]
- Lipsitz, L.A. Understanding health care as a complex system: The foundation for unintended consequences. JAMA-J. Am. Med. Assoc. 2012, 308, 243–244. [Google Scholar] [CrossRef] [PubMed]
- Durrani, H. Healthcare and healthcare systems: Inspiring progress and future prospects. Mhealth 2016, 2, 3. [Google Scholar] [CrossRef]
- Handler, A.; Issel, M.; Turnock, B. A conceptual framework to measure performance of the public health system. Am. J. Public Health 2001, 91, 1235–1239. [Google Scholar] [CrossRef] [PubMed]
- Savoia, E.; Agboola, F.; Biddinger, P.D. A conceptual framework to measure systems’ performance during emergency preparedness exercises. Int. J. Environ. Res. Public Health 2014, 11, 9712–9722. [Google Scholar] [CrossRef]
- Vincenten, J.; MacKay, J.M.; Schröder-Bäck, P.; Schloemer, T.; Brand, H. Factors influencing implementation of evidence-based interventions in public health systems—A model. Cent. Eur. J. Public Health 2019, 27, 198–203. [Google Scholar] [CrossRef]
- McGill, E.; Er, V.; Penney, T.; Egan, M.; White, M.; Meier, P.; Whitehead, M.; Lock, K.; Anderson de Cuevas, R.; Smith, R.; et al. Evaluation of public health interventions from a complex systems perspective: A research methods review. Soc. Sci. Med. 2021, 272, 113697. [Google Scholar] [CrossRef]
- Mahamoud, A.; Roche, B.; Homer, J. Modelling the social determinants of health and simulating short-term and long-term intervention impacts for the city of Toronto, Canada. Soc. Sci. Med. 2013, 93, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Morton, A. Aversion to health inequalities in healthcare prioritisation: A multicriteria optimisation perspective. J. Health Econ. 2014, 36, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Öhman, A.; Burman, M.; Carbin, M.; Edin, K. ‘The public health turn on violence against women’: Analysing swedish healthcare law, public health and gender-equality policies. BMC Public Health 2020, 20, 753. [Google Scholar] [CrossRef] [PubMed]
- Katrakazas, P.; Pastiadis, K.; Bibas, A.; Koutsouris, D. A general systems theory approach in public hearing health: Lessons learned from a systematic review of general systems theory in healthcare. IEEE Access 2020, 8, 53018–53033. [Google Scholar] [CrossRef]
- Milani, F. COVID-19 outbreak, social response, and early economic effects: A global VAR analysis of cross-country interdependencies. J. Popul. Econ. 2021, 34, 223–252. [Google Scholar] [CrossRef] [PubMed]
- McBride, O.; Murphy, J.; Shevlin, M.; Gibson, M.J.; Hartman, T.K.; Hyland, P.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; et al. Monitoring the psychological, social, and economic impact of the COVID-19 pandemic in the population: Context, design and conduct of the longitudinal COVID-19 psychological research consortium (C19PRC) study. Int. J. Methods Psychiatr. Res. 2021, 30, e1861. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, N.; Abbas, K.; Nathwani, D. Public health and social measures to mitigate the health and economic impact of the COVID-19 pandemic in turkey, egypt, ukraine, kazakhstan, and poland during 2020-2021: Situational analysis. BMC Public Health 2022, 22, 991. [Google Scholar] [CrossRef] [PubMed]
- Rutta, E.; Liana, J.; Embrey, M.; Johnson, K.; Kimatta, S.; Valimba, R.; Lieber, R.; Shekalaghe, E.; Sillo, H. Accrediting retail drug shops to strengthen Tanzania’s public health system: An ADDO case study. J. Pharm. Policy Pract. 2015, 8, 23. [Google Scholar] [CrossRef]
- Shapira, B.; Schaefer, E.; Poperno, A.; Hess, Z.; Rosca, P.; Berkovitz, R. The methanol content of illicit alcoholic beverages seized in a low socio-economic area of tel-aviv: Public health impact and policy implications. J. Public Health 2019, 27, 37–42. [Google Scholar] [CrossRef]
- Ruiz-Arrondo, I.; Oteo, J.A.; Lucientes, J.; Muniesa, A.; de Blas, I. Surveillance of a pest through a public health information system: The case of the blackfly (Simulium erythrocephalum) in Zaragoza (Spain) during 2009–2015. Int. J. Environ. Res. Public Health 2020, 17, 3734. [Google Scholar] [CrossRef] [PubMed]
- Yeager, V.A.; Beitsch, L.M.; Hasbrouck, L. From the schools and programs of public health: A mismatch between the educational pipeline and public health workforce: Can it be reconciled? Public Health Rep. 2016, 131, 507–509. [Google Scholar] [CrossRef]
- Gordon, T.; Booysen, F.; Mbonigaba, J. Socio-economic inequalities in the multiple dimensions of access to healthcare: The case of South Africa. BMC Public Health 2020, 20, 289. [Google Scholar] [CrossRef] [PubMed]
- Watts, R.D.; Bowles, D.C.; Fisher, C.; Li, I.W. What do public health graduates do and where do they go? an analysis of job destinations and mismatch in Australian public health graduates. Int. J. Environ. Res. Public Health 2021, 18, 7504. [Google Scholar] [CrossRef] [PubMed]
- Moscelli, G.; Siciliani, L.; Gutacker, N.; Cookson, R. Socioeconomic inequality of access to healthcare: Does choice explain the gradient? J. Health Econ. 2018, 57, 290–314. [Google Scholar] [CrossRef] [PubMed]
- Booysen, F.; Gordon, T. Trends and socio-economic inequality in public perceptions of healthcare delivery in South Africa. Int. J. Qual. Health Care 2020, 32, 135–139. [Google Scholar] [CrossRef]
- Rodrıíguez-Álvarez, A.; Fernández-Blanco, V.; Lovell, C.A.K. Allocative inefficiency and its cost:: The case of Spanish public hospitals. Int. J. Prod. Econ. 2004, 92, 99–111. [Google Scholar] [CrossRef]
- Christopher, S.M.; Parfait, B.B.; Max, M.N. Determinants of the inefficiency of public hospitals in Cameroon. Int. J. Acad. Res. Bus. Soc. Sci. 2017, 7, 2998. [Google Scholar] [CrossRef]
- Piubello Orsini, L.; Leardini, C.; Vernizzi, S.; Campedelli, B. Inefficiency of public hospitals: A multistage data envelopment analysis in an Italian region. BMC Health Serv. Res. 2021, 21, 1281. [Google Scholar] [CrossRef]
- Smith, T.; Philmon, C.; Johnson, G.; Ward, W.; Rivers, L.; Williamson, S.; Goodman, E. Antimicrobial stewardship in a community hospital: Attacking the more difficult problems. Hosp. Pharm. 2014, 49, 839–846. [Google Scholar] [CrossRef]
- Shikino, K.; Mito, T.; Ohira, Y.; Yokokawa, D.; Katsuyama, Y.; Ota, T.; Sato, E.; Hirose, Y.; Yamashita, S.; Suzuki, S.; et al. Frequency of difficult patient encounters in a Japanese university hospital and community hospitals: A cross-sectional study. Intern. Med. 2022; in press. [Google Scholar] [CrossRef]
- Song, W.; Li, Y.; Hao, Z.; Li, H.; Wang, W. Public health in China: An environmental and socio-economic perspective. Atmos. Environ. 2016, 129, 9–17. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, G.; Su, B. The spatial impacts of air pollution and socio-economic status on public health: Empirical evidence from China. Socio-Econ. Plan. Sci. 2022, 83, 101167. [Google Scholar] [CrossRef]
- Egan, M.; McGill, E.; Penney, T.; Meier, P.S.; Savona, N.; de Vocht, F.; Popay, J.; Cummins, S.; Smith, R.; White, M.; et al. Complex systems for evaluation of public health interventions: A critical review. Lancet 2018, 392, S31. [Google Scholar] [CrossRef]
- Littlecott, H.J.; Moore, G.F.; Gallagher, H.C.; Murphy, S. From complex interventions to complex systems: Using social network analysis to understand school engagement with health and wellbeing. Int. J. Environ. Res. Public Health 2019, 16, 1694. [Google Scholar] [CrossRef]
- Haghi, F.; Goli, S.; Rezaei, R.; Akhormi, F.; Eskandari, F.; Isfahani, Z.N. Study of complexity systems in public health for evaluating the correlation between mental health and age-related demographic characteristics: A general health study. J. Healthc. Eng. 2022, 2022, 2117031. [Google Scholar] [CrossRef]
- Ahirwar, M.K.; Shukla, P.K.; Singhai, R. CBO-IE: A data mining approach for healthcare IoT dataset using chaotic biogeography-based optimization and information entropy. Sci. Program. 2021, 2021, 8715668. [Google Scholar] [CrossRef]
- Khan, S.; Saravanan, V.N.G.C.; Lakshmi, T.J.; Deb, N.; Othman, N.A. Privacy protection of healthcare data over social networks using machine learning algorithms. Comput. Intell. Neurosci. 2022, in press. [CrossRef]
- Xing, Y. Japanese economy: Facing the constraint of an ageing and declining population. East Asian Policy 2016, 8, 79–94. [Google Scholar] [CrossRef]
- Vierkötter, A.; Hüls, A.; Yamamoto, A.; Stolz, S.; Krämer, U.; Matsui, M.S.; Morita, A.; Wang, S.; Li, Z.; Jin, L.; et al. Extrinsic skin ageing in German, Chinese and Japanese women manifests differently in all three groups depending on ethnic background, age and anatomical site. J. Dermatol. Sci. 2016, 83, 219–225. [Google Scholar] [CrossRef]
- Jung, Y. Fiscal policy and redistribution in a small open economy with aging population. East Asain Econ. Rev. 2021, 25, 421–461. [Google Scholar] [CrossRef]
| First-Level Indicator | Secondary-Level Indicators | Weights |
|---|---|---|
| Resources input sub-system | Human resources | 0.1441 |
| Financial resources | 0.0506 | |
| Technical resources | 0.1511 | |
| Social resources | 0.1286 | |
| Operating sub-system | Government | 0.0412 |
| Public hospitals | 0.0608 | |
| Other medical institutions | 0.1047 | |
| Planning and decision sub-system | Public health policy | 0.0626 |
| Medical care | 0.0358 | |
| Disease control | 0.0492 | |
| Health education | 0.0320 | |
| Service output sub-system | Daily healthcare services | 0.0434 |
| Increased public health awareness | 0.0538 | |
| public health emergency management | 0.0421 |
| Year | Economics Growth (Unit: CNY) | Urbanization Rate (Unit: %) | Labour Migration (Unit: 100 Million People) | Population Aging (Unit: %) | ||||
|---|---|---|---|---|---|---|---|---|
| Scale | Change Rate | Scale | Change Rate | Scale | Change Rate | Scale | Change Rate | |
| 2012 | 39,771 | 7.1 | 53.1 | 2.45 | 2.36 | 2.61 | 9.4 | 3.30 |
| 2013 | 43,497 | 7.1 | 54.49 | 2.62 | 2.45 | 3.81 | 9.7 | 3.19 |
| 2014 | 46,912 | 6.8 | 55.75 | 2.31 | 2.53 | 3.27 | 10.1 | 4.12 |
| 2015 | 49,922 | 6.4 | 57.33 | 2.83 | 2.47 | −2.37 | 10.5 | 3.96 |
| 2016 | 53,783 | 6.2 | 58.84 | 2.63 | 2.45 | −0.81 | 10.8 | 2.86 |
| 2017 | 59,592 | 6.3 | 60.24 | 2.38 | 2.44 | −0.41 | 11.4 | 5.56 |
| 2018 | 65,534 | 6.2 | 61.5 | 2.09 | 2.41 | −1.23 | 11.9 | 4.39 |
| 2019 | 70,328 | 6.0 | 62.71 | 1.97 | 2.36 | −2.07 | 12.6 | 5.88 |
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|
| Resources input sub-system | 0.4743 | 0.5274 | 0.6151 | 0.6659 | 0.7108 | 0.7548 | 0.8189 | 0.8784 | 0.9452 |
| Operating sub-system | 0.1726 | 0.1709 | 0.2309 | 0.2484 | 0.2517 | 0.2469 | 0.2501 | 0.2670 | 0.2810 |
| Planning and decision sub-system | 0.2007 | 0.2244 | 0.2051 | 0.2435 | 0.2823 | 0.2722 | 0.2804 | 0.3256 | 0.3527 |
| Service output sub-system | 0.2259 | 0.2372 | 0.2624 | 0.2751 | 0.2874 | 0.3242 | 0.2973 | 0.3141 | 0.2812 |
| Total | 1.0735 | 1.1599 | 1.3135 | 1.4329 | 1.5322 | 1.5981 | 1.6467 | 1.7851 | 1.8601 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, J.; Wang, C.; Zhang, X.; Wang, S. Public Health System and Socio-Economic Development Coupling Based on Systematic Theory: Evidence from China. Sustainability 2022, 14, 12757. https://doi.org/10.3390/su141912757
Zhou J, Wang C, Zhang X, Wang S. Public Health System and Socio-Economic Development Coupling Based on Systematic Theory: Evidence from China. Sustainability. 2022; 14(19):12757. https://doi.org/10.3390/su141912757
Chicago/Turabian StyleZhou, Jian, Chuhan Wang, Xinyu Zhang, and Shuang Wang. 2022. "Public Health System and Socio-Economic Development Coupling Based on Systematic Theory: Evidence from China" Sustainability 14, no. 19: 12757. https://doi.org/10.3390/su141912757
APA StyleZhou, J., Wang, C., Zhang, X., & Wang, S. (2022). Public Health System and Socio-Economic Development Coupling Based on Systematic Theory: Evidence from China. Sustainability, 14(19), 12757. https://doi.org/10.3390/su141912757






