Long-Term COVID: Case Report and Methodological Proposals for Return to Work
Abstract
:1. Introduction
2. Clinical Case
2.1. Work Context
2.2. Instrumental Assessments
2.3. Assessment of Causation
- The term “occasion of work” means any exposure to risk attributable to the performance of service activities, directly or indirectly, irrespective of the employee’s voluntary conduct: this circumstance (i.e., the occasion of work) is relevant for accidents protected by INAIL.
- With regard to “occupational risk”, it is necessary that the service activity carried out resulted in a “specific risk” for the employee arising from the particular conditions of the service activity carried out;
- An accident can also occur if there is an “aggravated generic occupational risk”, i.e., a risk which, although common to the general population, places a greater burden on the worker.
- Direct causation: Coronavirus injury is directly service-related in light of explicit service instructions/orders issued by the military authority;
- Preponderant causation: The specific activity contributed efficiently and decisively to the onset of the disease.
2.4. The Evaluation of Outcomes
- Severe respiratory failure;
- Anosmia with ageusia.
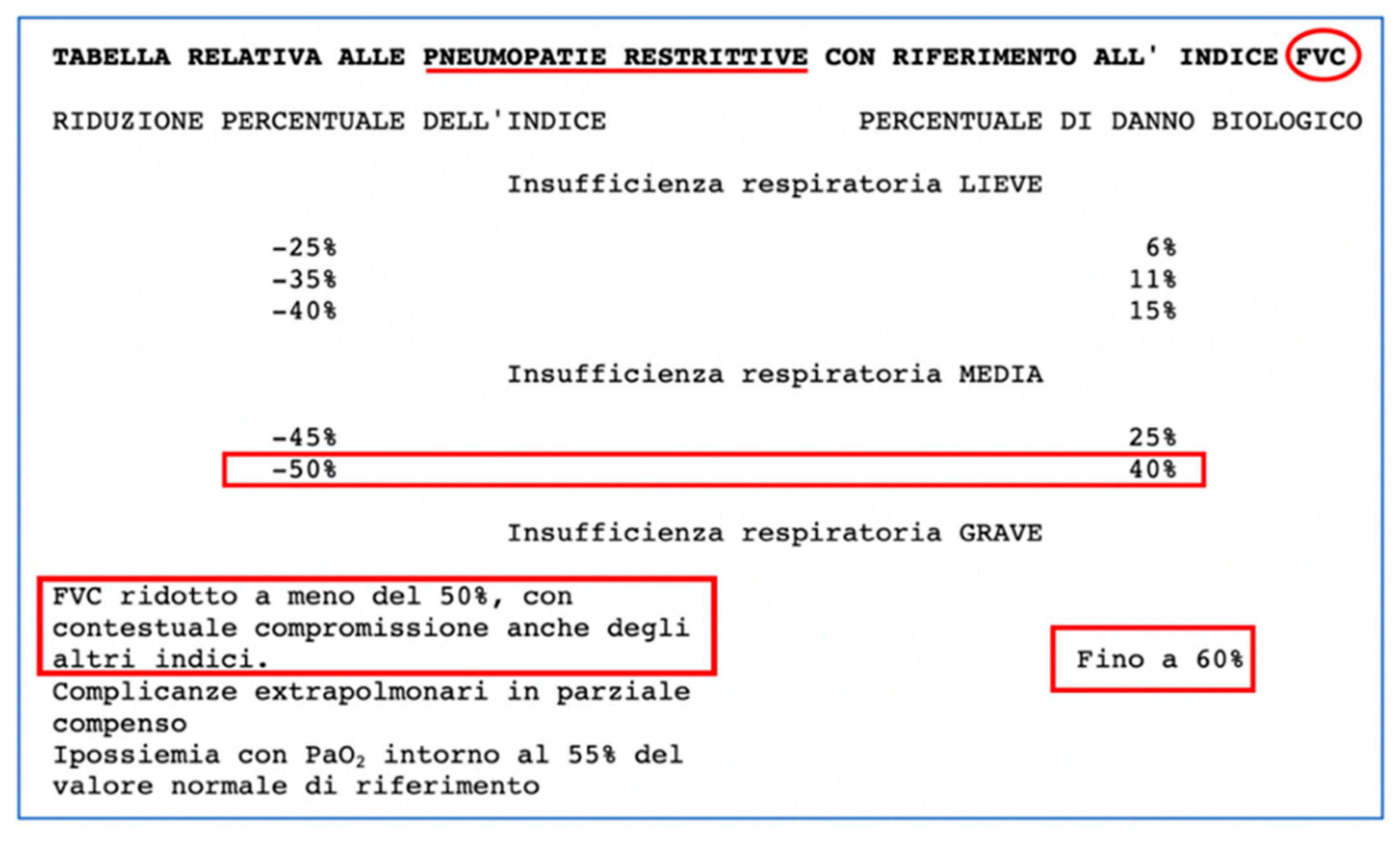
2.5. Assessment of Respiratory Function
2.6. Spirometry (1 Year Later)
2.7. Assessment of Anosmia/Ageusia
2.8. Olfactory Smart Threshold Test (OST) and Evoked Potentials (1 Year and 1 Month Later)
3. Discussion
- The outcomes observed, i.e., complete, permanent anosmia and respiratory difficulties more than a year after recovery from the disease, showed a medium-to-severe functional incidence in relation to the subject’s age, as well as anticipating what is now the much-discussed picture of so-called long-term COVID.
- The assessment of the aforementioned outcomes required the use of multiple assessment tables that illustrate the current difficulties in assessing outcomes resulting from SARS-CoV-2 infection, in this case, in light of the aforementioned codicil and regulatory elements.
- In Italy, this assessment requires the use of the current reference standards listed below:
- -
- Inps: Ministerial Decree 05/02/1992;
- -
- Inail: D.M. 12/07/2000;
- -
- Ministry of Defense: Tables annexed to Presidential Decree No. 915 of 23 December 1978 “Consolidated text of the regulations on war pensions”, tables annexed to Presidential Decree No. 834 of 30 December 1981 “Definitivo riordinamento delle pensioni di guerra, in attuazione della delegazione prevista dall’art. 1 della legge 23 settembre 1981, n. 533”.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arimany-Manso, J.; Martin-Fumadó, C. Medico-legal issues regarding from the COVID-19 pandemic. Med. Clin. (Engl. Ed.). 2020, 155, 344–346. [Google Scholar] [CrossRef] [PubMed]
- da Silveira Gorman, R.; Syed, I.U. Connecting the Dots in Emerging Mast Cell Research: Do Factors Affecting Mast Cell Activation Provide a Missing Link between Adverse COVID-19 Outcomes and the Social Determinants of Health? Med. Sci. 2022, 10, 29. [Google Scholar] [CrossRef]
- Anastassopoulou, C.; Gkizarioti, Z.; Patrinos, G.P.; Tsakris, A. Human genetic factors associated with susceptibility to SARS-CoV-2 infection and COVID-19 disease severity. Hum. Genom. 2020, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Washburn, T.; Diener, M.L.; Curtis, D.S.; Wright, C.A. Modern slavery and labor exploitation during the COVID-19 pandemic: A conceptual model. Glob. Health Action 2022, 15, 2074784. [Google Scholar] [CrossRef] [PubMed]
- Costantino, C.; Cannizzaro, E.; Alba, D.; Conforto, A.; Cimino, L.; Mazzucco, W. SARS-CoV-2 pandemic in the Mediterranean area: Epidemiology and perspectives. EuroMediterr. Biomed. J. 2020, 15, 102–106. [Google Scholar]
- Gambaro, E.; Gramaglia, C.; Marangon, D.; Azzolina, D.; Probo, M.; Rudoni, M.; Zeppegno, P. The Mediating Role of Gender, Age, COVID-19 Symptoms and Changing of Mansion on the Mental Health of Healthcare Workers Operating in Italy during the First Wave of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 13083. [Google Scholar] [CrossRef]
- Müller, I.; Mancinetti, M.; Renner, A.; Bridevaux, P.-O.; Brutsche, M.H.; Clarenbach, C.; Garzoni, C.; Lenoir, A.; Naccini, B.; Ott, S.; et al. Frailty assessment for COVID-19 follow-up: A prospective cohort study. BMJ Open Respir. Res. 2022, 9, e001227. [Google Scholar] [CrossRef] [PubMed]
- Moretti, A.; Menna, F.; Aulicino, M.; Paoletta, M.; Liguori, S.; Iolascon, G. Characterization of Home Working Population during COVID-19 Emergency: A Cross-Sectional Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6284. [Google Scholar] [CrossRef]
- Langmaid, L.; Ratner, L.; Huysman, C.; Curran, S.; Uluer, A. Supporting the Medically Fragile: Individualized Approach to Empowering Young Adults with Chronic Disease during the COVID-19 Pandemic. J. Adolesc. Health 2020, 67, 453–455. [Google Scholar] [CrossRef] [PubMed]
- Bellotti, L.; Zaniboni, S.; Balducci, C.; Grote, G. Rapid Review on COVID-19, Work-Related Aspects, and Age Differences. Int. J. Environ. Res. Public Health 2021, 18, 5166. [Google Scholar] [CrossRef]
- Martimbianco, A.L.C.; Pacheco, R.L.; Bagattini, M.; Riera, R. Frequency, signs and symptoms, and criteria adopted for long COVID-19: A systematic review. Int. J. Clin. Pract. 2021, 75, e14357. [Google Scholar] [CrossRef]
- Carenzo, L.; Costantini, E.; Greco, M.; Barra, F.L.; Rendiniello, V.; Mainetti, M.; Bui, R.; Zanella, A.; Grasselli, G.; Lagioia, M.; et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia 2020, 75, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.D.; Lavelle, M.; Boursiquot, B.C.; Wan, E.Y. Long-term complications of COVID-19. Am. J. Physiol. Cell Physiol. 2022, 322, C1–C11. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, K.M.; Vasarmidi, E.; Russell, A.-M.; Andrejak, C.; Crestani, B.; Delcroix, M.; Dinh-Xuan, A.T.; Poletti, V.; Sverzellati, N.; Vitacca, M.; et al. European Respiratory Society Statement on Long COVID-19 Follow-Up. Eur. Respir. J. 2022, 2102174, Epub ahead of print. [Google Scholar] [CrossRef]
- Bourmistrova, N.W.; Solomon, T.; Braude, P.; Strawbridge, R.; Carter, B. Long-term effects of COVID-19 on mental health: A systematic review. J. Affect. Disord. 2022, 299, 118–125. [Google Scholar] [CrossRef]
- Cannizzaro, E.; Cirrincione, L.; Mazzucco, W.; Scorciapino, A.; Catalano, C.; Ramaci, T.; Ledda, C.; Plescia, F. Night-Time Shift Work and Related Stress Responses: A Study on Security Guards. Int. J. Environ. Res. Public Health 2020, 17, 562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, S.; Mao, Y.; Jones, R.M.; Tan, Q.; Ji, J.S.; Li, N.; Shen, J.; Lv, Y.; Pan, L.; Ding, P.; et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020, 144, 106039. [Google Scholar] [CrossRef]
- Cirrincione, L.; Plescia, F.; Ledda, C.; Rapisarda, V.; Martorana, D.; Lacca, G.; Argo, A.; Zerbo, S.; Vitale, E.; Vinnikov, D.; et al. Technical note 1 COVID-19 Pandemic: New Prevention and Protection Measures. Sustainibility 2022, 14, 4766. [Google Scholar] [CrossRef]
- Tabah, A.; Ramanan, M.; Laupland, K.B.; Buetti, N.; Cortegiani, A.; Mellinghoff, J.; Conway Morris, A.; Camporota, L.; Zappella, N.; Elhadi, M.; et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): An international survey. J. Crit. Care 2020, 59, 70–75. [Google Scholar] [CrossRef]
- Vitale, E.; Vella, F.; Filetti, V.; Cirrincione, L.; Indelicato, G.; Cannizzaro, E.; Rapisarda, V. How to prevent SARS-CoV-2 transmission in the agri-food industry during the first pandemic wave: Effects on seroprevalence. Appl. Sci. 2021, 11, 10051. [Google Scholar] [CrossRef]
- Pontone, G.; Scafuri, S.; Mancini, M.E.; Agalbato, C.; Guglielmo, M.; Baggiano, A.; Muscogiuri, G.; Fusini, L.; Andreini, D.; Mushtaq, S.; et al. Role of computed tomography in COVID-19. J. Cardiovasc. Comput. Tomogr. 2021, 15, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.P.; Papenburg, J.; Desjardins, M.; Kanjilal, S.; Quach, C.; Libman, M.; Dittrich, S.; Yansouni, C.P. Diagnostic testing for severe acute respiratory syndrome-related Coronavirus-2: A narrative review. Ann. Intern. Med. 2020; published online ahead of print. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Antigen-Detection in the Diagnosis of SARS-CoV-2 Infection Using Rapid Immunoassays; Interim Guidance; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/antigen-detection-in-the-diagnosis-of-sars-cov-2infection-using-rapid-immunoassays (accessed on 24 June 2022).
- Desai, A.N.; Patel, P. Stopping the Spread of COVID-19. J. Am. Med. Assoc. (JAMA) 2020, 323, 1516. [Google Scholar] [CrossRef] [Green Version]
- Adams, J.G.; Walls, R.M. Supporting the Health Care Workforce during the COVID-19 Global Epidemic. J. Am. Med. Assoc. (JAMA) 2020, 323, 1439–1440. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Coronavirus (2019-nCoV) Infection Is Suspected; Interim Guidance; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Carod-Artal, F.J. Neurological complications of coronavirus and COVID-19. Rev. Neurol. 2020, 70, 311–322. (In Spanish) [Google Scholar] [CrossRef]
- Puelles, V.G.; Lütgehetmann, M.; Lindenmeyer, M.T.; Sperhake, J.P.; Wong, M.N.; Allweiss, L.; Chilla, S.; Heinemann, A.; Wanner, N.; Liu, S.; et al. Multiorgan and Renal Tropism of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 590–592. [Google Scholar] [CrossRef]
- Di Nunno, N.; Esposito, M.; Argo, A.; Salerno, M.; Sessa, F. Pharmacogenetics and Forensic Toxicology: A New Step towards a Multidisciplinary Approach. Toxics 2021, 9, 292. [Google Scholar] [CrossRef] [PubMed]
- Cirrincione, L.; Rapisarda, V.; Mazzucco, W.; Provenzano, R.; Cannizzaro, E. SARS-CoV-2 and the Risk Assessment Document in Italian Work; Specific or Generic Risk Even If Aggravated? Int. J. Environ. Res. Public Health 2021, 18, 3729. [Google Scholar] [CrossRef] [PubMed]
- Sangiorgio, V.; Parisi, F. A multicriteria approach for risk assessment of COVID-19 in urban district lockdown. Saf. Sci. 2020, 130, 104862. [Google Scholar] [CrossRef]
- Carpenter, C.R.; Mudd, P.A.; West, C.P.; Wilber, E.; Wilber, S.T. Diagnosing COVID-19 in the Emergency Department: A Scoping Review of Clinical Examinations, Laboratory Tests, Imaging Accuracy, and Biases. Acad. Emerg. Med. 2020, 27, 653–670. [Google Scholar] [CrossRef]
- Cirrincione, L.; Rapisarda, V.; Ledda, C.; Vitale, E.; Provenzano, R.; Cannizzaro, E. Considerations on the Update of the Risk Assessment Document during the Pandemic State by COVID-19 in Italy. Front. Public Health 2021, 9, 655927. [Google Scholar] [CrossRef]
- Available online: https://www.istat.it/it/files//2022/03/Report_ISS_ISTAT_2022_tab3.pdf (accessed on 24 June 2022).
- Gad, M.; Kazibwe, J.; Quirk, E.; Gheorghe, A.; Homan, Z.; Bricknell, M. Civil-military cooperation in the early response to the COVID-19 pandemic in six European countries. BMJ Mil. Health 2021, 167, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Baig, A.M. Chronic COVID syndrome: Need for an appropriate medical terminology for long-COVID and COVID long-haulers. J. Med. Virol. 2021, 93, 2555–2556. [Google Scholar] [CrossRef] [PubMed]
- Salian, V.S.; Wright, J.A.; Vedell, P.T.; Nair, S.; Li, C.; Kandimalla, M.; Tang, X.; Porquera, E.M.C.; Kalari, K.R.; Kandimalla, K.K. COVID-19 Transmission, Current Treatment, and Future Therapeutic Strategies. Mol. Pharm. 2021, 18, 754–771. [Google Scholar] [CrossRef] [PubMed]
- Carraturo, F.; del Giudice, C.; Morelli, M.; Cerullo, V.; Libralato, G.; Galdiero, E.; Guida, M. Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ. Pollut. 2020, 265 Pt B, 115010. [Google Scholar] [CrossRef]
- Ledda, C.; Cannizzaro, E.; Cinà, D.; Filetti, V.; Vitale, E.; Paravizzini, G.; Di Naso, C.; Iavicoli, I.; Rapisarda, V. Oxidative stress and DNA damage in agricultural workers after exposure to pesticides. J. Occup. Med. Toxicol. 2021, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Bilotta, C.; Perrone, G.; Adelfio, V.; Spatola, G.F.; Uzzo, M.L.; Argo, A.; Zerbo, S. COVID-19 Vaccine-Related Thrombosis: A Systematic Review and Exploratory Analysis. Front. Immunol. 2021, 12, 729251. [Google Scholar] [CrossRef] [PubMed]
- Beyerstedt, S.; Casaro, E.B.; Rangel, É.B. COVID-19: Angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 905–919. [Google Scholar] [CrossRef] [PubMed]
- Eliezer, M.; Hautefort, C.; Hamel, A.-L.; Verillaud, B.; Herman, P.; Houdart, E.; Eloit, C. Sudden and Complete Olfactory Loss of Function as a Possible Symptom of COVID-19. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 674–675. [Google Scholar] [CrossRef] [Green Version]
- Avenali, M.; Martinelli, D.; Todisco, M.; Canavero, I.; Valentino, F.; Micieli, G.; Alfonsi, E.; Tassorelli, C.; Cosentino, G. Clinical and Electrophysiological Outcome Measures of Patients with Post-Infectious Neurological Syndromes Related to COVID-19 Treated with Intensive Neurorehabilitation. Front. Neurol. 2021, 12, 643713. [Google Scholar] [CrossRef]
- Mazzatenta, A.; Neri, G.; D’Ardes, D.; De Luca, C.; Marinari, S.; Porreca, E.; Cipollone, F.; Vecchiet, J.; Falcicchia, C.; Panichi, V.; et al. Smell and Taste in Severe COVID-19: Self-Reported vs. Testing. Front. Med. 2020, 7, 589409. [Google Scholar] [CrossRef]
- Miller, M.R.; Quanjer, P.H.; Swanney, M.P.; Ruppel, G.; Enright, P.L. Interpreting lung function data using 80% predicted and fixed thresholds misclassifies more than 20% of patients. Chest 2011, 139, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.M.; Zheng, J.; et al. Multi-ethhnic reference values for spirometry for the 3–95 years age range: The Global Lung Function 2012 equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Scoppettuolo, P.; Borrelli, S.; Naeije, G. Neurological involvement in SARS-CoV-2 infection: A clinical systematic review. Brain Behav. Immun. Health 2020, 5, 100094. [Google Scholar] [CrossRef] [PubMed]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 6683–6690. [Google Scholar] [CrossRef] [Green Version]
- Hu, B.; Huang, S.; Yin, L. The cytokine storm and COVID-19. J. Med. Virol. 2021, 93, 250–256. [Google Scholar] [CrossRef] [PubMed]



| Forced Vital Capacity | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | UM | Description | Teor | Test#2 | %Teor | Post#3 | %Test#2 |
| Best VCF | L | Best CVT | 5.14 | 3.62 | 70 | 3.66 | +1.2 |
| FVC | L | Forced vital capacity | 5.14 | 3.62 | 70 | 3.66 | +1.2 |
| FEV1 | L | Volume exhaled after 1 s | 4.26 | 3.30 | 77 | 3.29 | −0.3 |
| PEF | L/s | Peak expiratory flow | 9.74 | 8.86 | 91 | 10.59 | +19.5 |
| PIF | L/s | Peak inspiratory flow | 5.34 | 6.20 | +16.1 | ||
| FEV1/FVC% | % | FEV1 as a percentage of FVC | 81.1 | 91.1 | 112 | 89.7 | |
| FEV1/VC% | % | FEV1 as a percentage of VC | 81.1 | 107.7 | 133 | 107.3 | |
| FEF25–75% | L/s | Average exp. flow 25–75% FVC | 4.73 | 4.22 | 89 | 4.53 | +7.5 |
| MEF 75% | L/s | Exposed flow at 25% of FVC | 8.37 | 8.75 | 104 | 9.43 | +7.8 |
| MEF 50% | L/s | Exposed flow at 50% of FVC | 5.42 | 4.80 | 89 | 5.17 | +7.9 |
| MEF 25% | L/s | Exposed flow at 75% of FVC | 2.47 | 2.11 | 85 | 2.11 | +0.3 |
| FET 100% | s | Forced breathing time | 2.1 | 2.6 | +21.7 | ||
| PEFr | L/min | Peak expiratory flow (L/min) | 584.4 | 531.6 | 91 | 635.2 | +19.5 |
| Lung Volumes and Ventilatory Profile | |||||||
| Parameter | UM | Description | Teor | Test#1 | %Teor | ||
| IVC | L | Inspiratory vital capacity | 5.39 | 3.06 | 57 | ||
| ERV | L | Expiratory reserve volume | 1.55 | 0.96 | 62 | ||
| IRV | L | Inspiratory reserve volume | 1.43 | ||||
| VE | L/min | Ventilation espiratory minute | 20.00 | ||||
| Rf | L/min | Respiratory frequency | 29.50 | ||||
| Vt | L | Current volume | 0.68 | ||||
| VT/Ti | - | Mean inspiratory flow | 0.85 | ||||
| Ti/Ttot | - | Ti/Ttot ratio | 0.39 | ||||
| SVC PRE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mis | Normal | Pred | % Pred | Z Score | |||||||
| ERV | L | 0.88 | - | 1.55 | 56 | - | |||||
| IC | L | 1.21 | - | 3.87 | 31 | - | |||||
| VC | L | 2.08 | 4.46–6.30 | 5.38 | 39 | −5.89 | |||||
| IRV | L | 0.81 | - | - | - | - | |||||
| VT | L (btps) | 0.397 | - | - | - | - | |||||
| PRE | POST DB (Salbutamol 400 mcg) | ||||||||||
| Mis | Normal | Pred | % Pred | Z Score | Mis | Var | %Variation | % Pred | Z Score | ||
| FVC | L | 3.36 | 4.14–6.15 | 5.14 | 65 | −2.92 | 3.36 | 0.00 | 0 | 65 | −2.92 |
| FEV1 | L | 3.23 | 3.43–5.10 | 4.26 | 76 | −2.03 | 3.24 | 0.01 | 0 | 76 | −2.00 |
| FEV1/FVC% | % | 96.1 | 69.3–92.9 | 81.1 | 119 | 2.10 | 96.5 | 0.3 | 0 | 119 | 2.14 |
| PEF | L/S | 8.79 | 7.75–11.73 | 9.74 | 90 | −0.79 | 8.81 | 0.02 | 0 | 90 | −0.77 |
| FEF 25–75% | L/S | 4.34 | 3.02–6.44 | 4.73 | 92 | −0.37 | 6.00 | 1.66 | 38 | 127 | 1.22 |
| MEF 25% | L/S | 2.40 | 1.19–3.76 | 2.47 | 97 | −0.10 | 3.20 | 0.80 | 33 | 129 | 0.93 |
| MEF 50% | L/S | 4.68 | 3.25–7.59 | 5.42 | 86 | −0.56 | 6.75 | 2.07 | 44 | 125 | 1.01 |
| MEF 75% | L/S | 8.01 | 5.56–11.18 | 8.37 | 96 | −0.21 | 8.53 | 0.53 | 7 | 102 | 0.09 |
| FEV6 | L | 0.00 | - | - | - | 0.00 | 0.00 | - | - | - | |
| FEV1/FEV6% | % | 0.0 | - | - | - | 0.0 | 0.0 | - | - | - | |
| FEV1/VCmax% | % | 96.1 | 69.3–92.9 | 81.1 | 119 | 2.10 | 96.5 | 0.3 | 0 | 119 | 2.14 |
| DLCO Test Results | |||||||||||
| Mis | Normal | Pred | % Pred | Z score | |||||||
| DLCO | mL/min/mmHg | 24.10 | 28.07–41.95 | 35.01 | 69 | −2.58 | |||||
| DLCO corr | mL/min/mmHg | 24.10 | 28.07–41.95 | 35.01 | 69 | −2.58 | |||||
| DLCO/VA | mL/min/mmHg/L | 5.59 | 3.51–6.28 | 4.89 | 114 | 0.83 | |||||
| VA | L | 4.31 | 6.00–8.30 | 7.15 | 60 | −4.06 | |||||
| TLC (DLCO) | L | 4.48 | 6.15–8.45 | 7.30 | 61 | −4.03 | |||||
| DLCO 3eq | mL/min/mmHg | 21.01 | 28.07–41.95 | 35.01 | 60 | −3.32 | |||||
| Test Results N2 Multiple Breath Washout | |||||||||||
| Mis | Normal | Pred | % Pred | Z score | |||||||
| FRC | L | 4.19 | 2.44–4.42 | 3.43 | 122 | 1.27 | |||||
| TLC (N2 WO) | L | 6.68 | 6.15–8.45 | 7.30 | 91 | −0.89 | |||||
| RV (N2 WO) | L | 3.32 | 1.20–2.55 | 1.88 | 177 | 3.51 | |||||
| RV/TLV (N2 WO) | % | 49.7 | 18.2–36.2 | 27.2 | 182 | 4.11 | |||||
| FRC/TLC (N2 WO) | % | 62.8 | 39.9–62.0 | 50.9 | 123 | 1.76 | |||||
| LCI | - | 11.39 | 5.49–6.58 | 6.03 | 189 | 16.25 | |||||
| VC | L | 3.36 | 4.46–6.30 | 5.38 | 62 | −3.60 | |||||
| Outcome | Assessments | ||
|---|---|---|---|
| INPS | INAIL | MdD | |
| Anosmia | 20% | 8 | 50–40% (Item neurosis/neuritis—VI cat) |
| Moderate Respiratory Distress | 41–50% | Up to 40% | 40–30% (Item neurosis/neuritis—VII cat) |
| Type of Worker | Risk Classes—Impact of Long-Term COVID Damage on Job Activities (Considering Pulmonary and Neurological Damage) |
|---|---|
| Farmers | High |
| Health workers | High, especially for shift work and subcategories such as anesthetists working with gases |
| Administrative staff | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malta, G.; Cirrincione, L.; Plescia, F.; Campagna, M.; Montagnini, C.; Cannizzaro, E. Long-Term COVID: Case Report and Methodological Proposals for Return to Work. Sustainability 2022, 14, 9332. https://doi.org/10.3390/su14159332
Malta G, Cirrincione L, Plescia F, Campagna M, Montagnini C, Cannizzaro E. Long-Term COVID: Case Report and Methodological Proposals for Return to Work. Sustainability. 2022; 14(15):9332. https://doi.org/10.3390/su14159332
Chicago/Turabian StyleMalta, Ginevra, Luigi Cirrincione, Fulvio Plescia, Marcello Campagna, Claudia Montagnini, and Emanuele Cannizzaro. 2022. "Long-Term COVID: Case Report and Methodological Proposals for Return to Work" Sustainability 14, no. 15: 9332. https://doi.org/10.3390/su14159332
APA StyleMalta, G., Cirrincione, L., Plescia, F., Campagna, M., Montagnini, C., & Cannizzaro, E. (2022). Long-Term COVID: Case Report and Methodological Proposals for Return to Work. Sustainability, 14(15), 9332. https://doi.org/10.3390/su14159332









