Evaluating the Inequality of Medical Resource Allocation Based on Spatial and Non-Spatial Accessibility: A Case Study of Wenzhou, China
Abstract
:1. Introduction
2. Materials and Methods
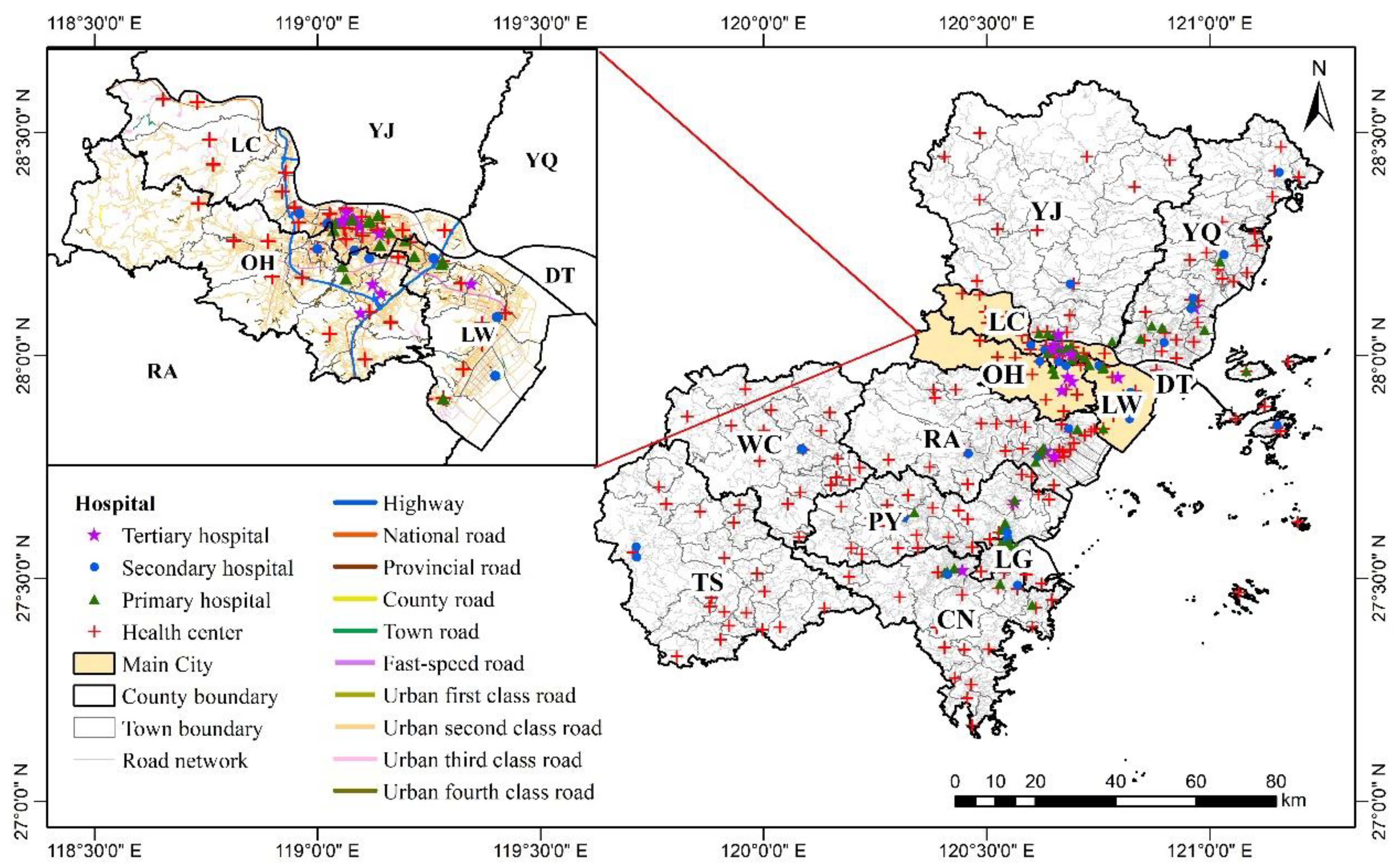
2.1. Study Area
2.2. Data Sources
2.2.1. Demographic and Economic Data
2.2.2. Medical Institutions’ Data
2.2.3. Road Network
2.3. Methods
2.3.1. Gini Coefficient
2.3.2. Agglomeration Degree
2.3.3. Network Analysis
2.3.4. Assessing Accessibility Using the Modified H2SFCA Method
2.3.5. Correlation Analysis
3. Results
3.1. General Description of Medical Institutions
3.2. Equality in Medical Resource Distribution
3.3. Shortest Travel Time Cost to Medical Institutions
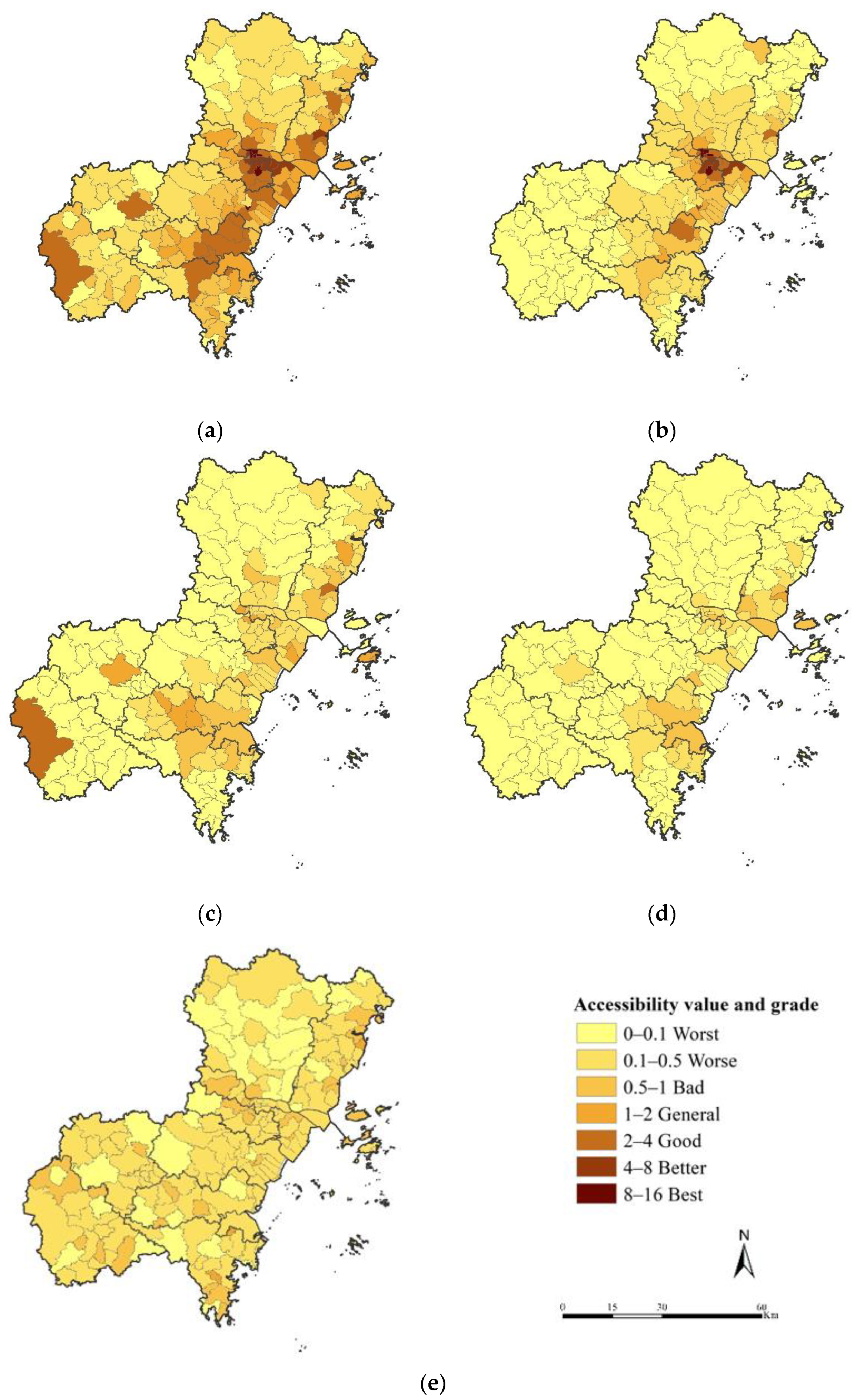
3.4. Spatial Accessibility of Medical Institutions at All Levels
3.5. Correlations between Spatial Accessibility and Influence Factors
4. Discussion
4.1. Unbalance Spatial Distribution of Medical Resources and the Need to Improve Geographical Equality
4.2. Apparent Differences in Medical Resources Accessibility at All Levels and the Need to Strengthen the “Graded Diagnosis and Treatment” Policy
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development 2015. Available online: https://sdgs.un.org/2030agenda (accessed on 13 September 2021).
- Dong, E.; Liu, S.; Chen, M.; Wang, H.; Chen, L.-W.; Xu, T.; Wang, T.; Zhang, L. Differences in regional distribution and inequality in health-resource allocation at hospital and primary health centre levels: A longitudinal study in Shanghai, China. BMJ Open 2020, 10, e035635. [Google Scholar] [CrossRef] [PubMed]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair allocation of scarce medical resources in the time of COVID-19. N. Eng. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.A. Fragility and challenges of health systems in pandemic: Lessons from India’s second wave of coronavirus disease 2019 (COVID-19). Glob. Health J. 2022, 6, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Xia, Y.; Hou, J. Health expenditure efficiency in rural China using the super-SBM model and the Malmquist productivity index. Int. J. Equity Health 2019, 18, 111. [Google Scholar] [CrossRef]
- Yang, F.; Yang, Y.; Liao, Z. Evaluation and analysis for Chinese medical alliance’s governance structure modes based on preker-harding model. Int. J. Integr. Care 2020, 20, 14. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, L.; Cui, Z.; Wang, Y. Study on Equity and Efficiency of Health Resources and Services Based on Key Indicators in China. PLoS ONE 2015, 10, e0144809. [Google Scholar] [CrossRef] [Green Version]
- Bigman, D.; ReVelle, C. The theory of welfare considerations in public facility location problems. Geogr. Anal. 1978, 10, 229–240. [Google Scholar] [CrossRef]
- Tao, Z.; Cheng, Y.; Zheng, Q.; Li, G. Measuring spatial accessibility to healthcare services with constraint of administrative boundary: A case study of Yanqing District, Beijing, China. Int. J. Equity Health 2018, 17, 7. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Qin, Y.; Xu, Y. Inequality and influencing factors of spatial accessibility of medical facilities in rural areas of China: A case study of Henan Province. Int. J. Environ. Res. Public Health 2019, 16, 1833. [Google Scholar] [CrossRef] [Green Version]
- Neutens, T. Accessibility, equity and health care: Review and research directions for transport geographers. J. Transp. Geogr. 2015, 43, 14–27. [Google Scholar] [CrossRef]
- Rosero-Bixby, L. Spatial access to health care in Costa Rica and its equity: A GIS-based study. Soc. Sci. Med. 2004, 58, 1271–1284. [Google Scholar] [CrossRef]
- Joseph, A.E.; Bantock, P.R. Measuring potential physical accessibility to general practitioners in rural areas: A method and case study. Soc. Sci. Med. 1982, 16, 85–90. [Google Scholar] [CrossRef]
- Huber, C.; Watts, A.; Grills, A.; Yong, J.H.E.; Morrison, S.; Bowden, S.; Tuite, A.; Nelson, B.; Cetron, M.; Khan, K. Modelling airport catchment areas to anticipate the spread of infectious diseases across land and air travel. Spat. Spatio-Temporal Epidemiol. 2021, 36, 100380. [Google Scholar] [CrossRef] [PubMed]
- Radke, J.; Mu, L. Spatial decompositions, modeling and mapping service regions to predict access to social programs. Ann. GIS 2000, 6, 105–112. [Google Scholar] [CrossRef]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- Langford, M.; Higgs, G. Measuring potential access to primary healthcare services: The influence of alternative spatial representations of population. Prof. Geogr. 2006, 58, 294–306. [Google Scholar] [CrossRef]
- Cervigni, F.; Suzuki, Y.; Ishii, T.; Hata, A. Spatial accessibility to pediatric services. J. Community Health 2008, 33, 444–448. [Google Scholar] [CrossRef]
- Mao, L.; Nekorchuk, D. Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health Place 2013, 24, 115–122. [Google Scholar] [CrossRef]
- Luo, J.; Tian, L.; Luo, L.; Yi, H.; Wang, F. Two-step optimization for spatial accessibility improvement: A case study of health care planning in rural China. BioMed Res. Int. 2017, 2017, 2094654. [Google Scholar] [CrossRef] [Green Version]
- Hashtarkhani, S.; Kiani, B.; Bergquist, R.; Bagheri, N.; Vafaeinejad, R.; Tara, M. An age-integrated approach to improve measurement of potential spatial accessibility to emergency medical services for urban areas. Int. J. Health Plan. Manag. 2020, 35, 788–798. [Google Scholar] [CrossRef]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Dai, D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place 2010, 16, 1038–1052. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Pan, J. Assessing the disparity in spatial access to hospital care in ethnic minority region in Sichuan Province, China. BMC Health Serv. Res. 2016, 16, 399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Luo, W. Assessing spatial and nonspatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health Place 2005, 11, 131–146. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary care in rural areas: Improving the effectiveness of the two-step floating catchment area method. Appl. Geogr. 2009, 29, 533–541. [Google Scholar] [CrossRef]
- Jin, M.; Liu, L.; Tong, D.; Gong, Y.; Liu, Y. Evaluating the spatial accessibility and distribution balance of multi-level medical service facilities. Int. J. Environ. Res. Public Health 2019, 16, 1150. [Google Scholar] [CrossRef] [Green Version]
- JTGB01-2014; Highway Bureau Ministry of Transport of The People’s Republic of China. Technical Standard of Highway Engineering. People’s Communications Press: Beijing, China, 2014; p. 120.
- Zhang, T.; Xu, Y.; Ren, J.; Sun, L.; Liu, C. Inequality in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef] [Green Version]
- Theodorakis, P.N.; Mantzavinis, G.D.; Rrumbullaku, L.; Lionis, C.; Trell, E. Measuring health inequalities in Albania: A focus on the distribution of general practitioners. Hum. Resour. Health 2006, 4, 5. [Google Scholar] [CrossRef] [Green Version]
- Yu, Q.; Yin, W.; Huang, D.; Sun, K.; Chen, Z.; Guo, H.; Wu, D. Trend and equity of general practitioners’ allocation in China based on the data from 2012–2017. Hum. Resour. Health 2021, 19, 20. [Google Scholar] [CrossRef]
- Wu, X.; Hu, Y.; Li, D.; Zhu, X.; Li, J.; Qi, Z. Study on the allocation equity of medical insurance designated retail pharmacies in Shenzhen. Chin. J. Health Policy 2021, 14, 28–34. [Google Scholar]
- Wang, Y.; Li, Y.; Qin, S.; Kong, Y.; Yu, X.; Guo, K.; Meng, J. The disequilibrium in the distribution of the primary health workforce among eight economic regions and between rural and urban areas in China. Int. J. Equity Heal. 2020, 19, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Han, P.; Sun, Y.; Zhao, J.; Yang, L. Assessing spatial accessibility to primary health care services in Beijing, China. Int. J. Environ. Res. Public Health 2021, 18, 13182. [Google Scholar] [CrossRef] [PubMed]
- Peeters, D.; Thomas, I. Distance predicting functions and applied location-allocation models. J. Geogr. Syst. 2000, 2, 167–184. [Google Scholar] [CrossRef]
- Jin, J.; Wang, J.; Ma, X.; Wang, Y.; Li, R. Equality of medical health resource allocation in China based on the gini coefficient method. Iran. J. Public Health 2015, 44, 445–457. [Google Scholar]
- Li, Q.; Wei, J.; Jiang, F.; Zhou, G.; Jiang, R.; Chen, M.; Zhang, X.; Hu, W. Equity and efficiency of health care resource allocation in Jiangsu Province, China. Int. J. Equity Health 2020, 19, 211. [Google Scholar] [CrossRef]
- The State Council of China. The National Planning for Medical and Health Service System from 2015 to 2020, Government Document 2015. Available online: http://www.gov.cn/zhengce/content/2015-03/30/content_9560.htm (accessed on 13 September 2021).
- Huo, J. An Analysis of China Health Resource Allocation on the View of Economics; Ningbo University: Ningbo, China, 2011. [Google Scholar]
- Sun, J.; Luo, H. Evaluation on equality and efficiency of health resources allocation and health services utilization in China. Int. J. Equity Health 2017, 16, 127. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Li, N.X. Research on the equity of the nursing human resource allocation in China, 2013–2017. Mod. Prev. Med. 2021, 48, 858–861. [Google Scholar]
- Yue, J.; Fu, Q.; Zhou, Y.; Zhang, Y.; Ning, J.; Yin, G.; Tao, H. Evaluating the accessibility to healthcare facilities under the Chinese hierarchical diagnosis and treatment system. Geospat. Health 2021, 16, 995. [Google Scholar] [CrossRef]
- Pan, J.; Zhao, H.; Wang, X.; Shi, X. Assessing spatial access to public and private hospitals in Sichuan, China: The influence of the private sector on the healthcare geography in China. Soc. Sci. Med. 2016, 170, 35–45. [Google Scholar] [CrossRef]
- Gu, X.; Zhang, L.; Tao, S.; Xie, B. Spatial accessibility to healthcare services in metropolitan suburbs: The case of Qingpu, Shanghai. Int. J. Environ. Res. Public Health 2019, 16, 225. [Google Scholar] [CrossRef] [Green Version]
- Zhang, S.; Song, X.; Zhou, J. An equity and efficiency integrated grid-to-level 2SFCA approach: Spatial accessibility of multilevel healthcare. Int. J. Equity Health 2021, 20, 229. [Google Scholar] [CrossRef] [PubMed]


| Town | Number of Counties | Area (km2) | Registered Population (In Thousands) | Road Length (104 km) | GDP (Billion Yuan) | Number of Medical Institutions | Number of Beds Per Thousand | Number of Doctors Per Thousand | Number of Nurses Per Thousand | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tertiary Hospitals | Secondary Hospitals | Primary Hospitals | Health Centers | |||||||||
| LC | 14 | 293 | 786 | 136 | 1137 | 6 | 3 | 9 | 23 | 13.44 | 6.89 | 8.73 |
| LW | 10 | 319 | 340 | 105 | 705 | 1 | 3 | 4 | 9 | 1.42 | 2.06 | 1.65 |
| OH | 13 | 466 | 463 | 167 | 661 | 3 | 2 | 2 | 11 | 1.59 | 1.7 | 1.42 |
| DT | 7 | 254 | 155 | 39 | 108 | 0 | 1 | 2 | 7 | 3.49 | 2.99 | 2.25 |
| YJ | 22 | 2677 | 988 | 315 | 445 | 1 | 1 | 4 | 14 | 3.78 | 3.01 | 2.34 |
| PY | 16 | 1042 | 884 | 227 | 510 | 1 | 2 | 4 | 25 | 4.78 | 3.12 | 2.63 |
| CN | 18 | 1069 | 970 | 243 | 352 | 1 | 2 | 5 | 18 | 6.81 | 3.38 | 3.49 |
| WC | 17 | 1296 | 411 | 189 | 105 | 0 | 2 | 1 | 17 | 3.62 | 3.36 | 2.8 |
| TS | 19 | 1768 | 373 | 240 | 111 | 0 | 2 | 0 | 19 | 4.47 | 3.4 | 2.61 |
| RA | 23 | 1350 | 1258 | 299 | 1004 | 2 | 3 | 4 | 29 | 3.31 | 2.95 | 2.53 |
| YQ | 25 | 1391 | 1315 | 303 | 1210 | 1 | 5 | 6 | 24 | 3.53 | 2.91 | 2.35 |
| LG | 1 | 184 | 381 | 50 | 301 | 0 | 2 | 5 | 4 | 2.45 | 2.26 | 2.07 |
| Medical Resources | Population | Geography |
|---|---|---|
| Number of medical institutions | 0.057 | 0.232 |
| Number of beds | 0.332 | 0.514 |
| Number of doctors | 0.232 | 0.667 |
| Number of nurses | 0.605 | 0.505 |
| Town | Population | Institutions | Beds | Doctors | Nurses | ||||
|---|---|---|---|---|---|---|---|---|---|
| Value | Ratio | Value | Ratio | Value | Ratio | Value | Ratio | ||
| LC | 3.75 | 4.11 | 1.10 | 15.3 | 4.08 | 11.5 | 3.06 | 15.00 | 4.00 |
| LW | 1.89 | 3.01 | 1.59 | 1.08 | 0.57 | 2.30 | 1.21 | 1.90 | 1.01 |
| OH | 1.39 | 1.92 | 1.38 | 0.86 | 0.62 | 1.34 | 0.97 | 1.16 | 0.83 |
| DT | 1.18 | 0.89 | 0.75 | 0.54 | 0.46 | 0.68 | 0.58 | 0.53 | 0.45 |
| YJ | 0.52 | 0.43 | 0.83 | 0.31 | 0.60 | 0.36 | 0.70 | 0.29 | 0.56 |
| PY | 1.28 | 1.31 | 1.02 | 1.05 | 0.82 | 1.01 | 0.78 | 0.87 | 0.68 |
| CN | 1.31 | 1.01 | 0.77 | 1.11 | 0.85 | 0.75 | 0.57 | 0.83 | 0.64 |
| WC | 0.44 | 0.22 | 0.50 | 0.18 | 0.41 | 0.25 | 0.56 | 0.21 | 0.48 |
| TS | 0.30 | 0.18 | 0.61 | 0.17 | 0.58 | 0.19 | 0.64 | 0.15 | 0.51 |
| RA | 1.39 | 1.60 | 1.51 | 0.99 | 0.71 | 1.29 | 0.93 | 1.14 | 0.82 |
| YQ | 1.43 | 1.55 | 1.09 | 1.03 | 0.72 | 1.24 | 0.87 | 1.04 | 0.73 |
| LG | 3.57 | 3.50 | 0.98 | 1.69 | 0.47 | 2.28 | 0.64 | 2.15 | 0.60 |
| Analysis Index | Accessibility Score | Number of Medical Institutions | Number of Doctors | Population Density | Road Density |
|---|---|---|---|---|---|
| Number of medical institutions | 0.585 ** | ||||
| Number of doctors | 0.670 ** | 0.799 ** | |||
| Population density (person/km2) | 0.769 ** | 0.493 ** | 0.590 ** | ||
| Road density (km/km2) | 0.792 ** | 0.512 ** | 0.592 ** | 0.826 ** | |
| GDP (ten thousand) | 0.310 ** | 0.374 ** | 0.536 ** | 0.326 ** | 0.266 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, M.; Zhao, Y.; Fang, T.; Fan, L.; Zhang, M.; Huang, H.; Mei, K. Evaluating the Inequality of Medical Resource Allocation Based on Spatial and Non-Spatial Accessibility: A Case Study of Wenzhou, China. Sustainability 2022, 14, 8331. https://doi.org/10.3390/su14148331
Du M, Zhao Y, Fang T, Fan L, Zhang M, Huang H, Mei K. Evaluating the Inequality of Medical Resource Allocation Based on Spatial and Non-Spatial Accessibility: A Case Study of Wenzhou, China. Sustainability. 2022; 14(14):8331. https://doi.org/10.3390/su14148331
Chicago/Turabian StyleDu, Miao, Yuhua Zhao, Tao Fang, Linyu Fan, Minghua Zhang, Hong Huang, and Kun Mei. 2022. "Evaluating the Inequality of Medical Resource Allocation Based on Spatial and Non-Spatial Accessibility: A Case Study of Wenzhou, China" Sustainability 14, no. 14: 8331. https://doi.org/10.3390/su14148331
APA StyleDu, M., Zhao, Y., Fang, T., Fan, L., Zhang, M., Huang, H., & Mei, K. (2022). Evaluating the Inequality of Medical Resource Allocation Based on Spatial and Non-Spatial Accessibility: A Case Study of Wenzhou, China. Sustainability, 14(14), 8331. https://doi.org/10.3390/su14148331






