Government Effectiveness and the COVID-19 Pandemic
Abstract
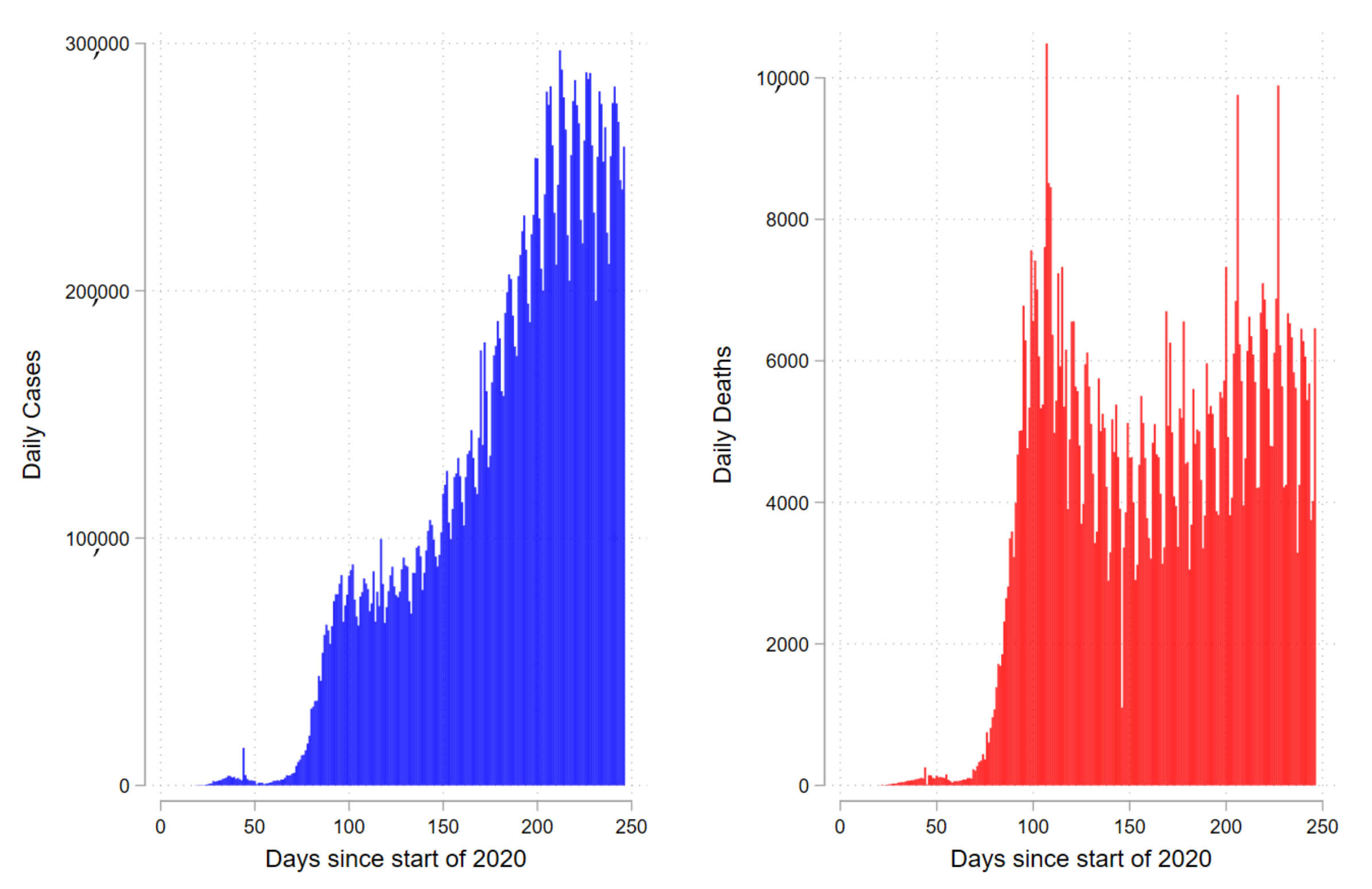
1. Introduction
Related Literature
2. Materials and Methods
3. Results and Discussion
Additional Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1
| Variable | Description | Source |
|---|---|---|
| Total deaths per million | Total deaths attributed to COVID-19 per 1,000,000 people | COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University |
| Govt Response | Overall Government Response Index | Oxford COVID-19 Government Response Tracker, Blavatnik School of Government |
| Economic Support | Economic Support Index | Oxford COVID-19 Government Response Tracker, Blavatnik School of Government |
| Containment Health | Containment and Health Index | Oxford COVID-19 Government Response Tracker, Blavatnik School of Government |
| Stringency | Stringency Index | Oxford COVID-19 Government Response Tracker, Blavatnik School of Government |
| GDPpc | Gross domestic product at purchasing power parity (constant 2011 international dollars), most recent year available | World Bank World Development Indicators, source from World Bank, International Comparison Program database |
| Hospital Beds per 1000 | Hospital beds per 1000 people, most recent year available since 2010 | OECD, Eurostat, World Bank, national government records and other sources |
| Diabetes prevalence | Diabetes prevalence (% of population aged 20 to 79) in 2017 | World Bank World Development Indicators, sourced from International Diabetes Federation, Diabetes Atlas |
| Median age | Median age of the population, UN projection for 2020 | UN Population Division, World Population Prospects, 2017 Revision |
| Obs | Mean | Std.Dev. | Min. | Max. | |
|---|---|---|---|---|---|
| Total Deaths per million | 34,740 | 50.69 | 140.60 | 0.00 | 1237.55 |
| Govt Response | 33,966 | 55.32 | 24.02 | 0.00 | 96.15 |
| Economic Support | 33,458 | 40.41 | 32.61 | 0.00 | 100.00 |
| Containment Health | 34,091 | 58.06 | 25.41 | 0.00 | 100.00 |
| Stringency | 34,105 | 57.84 | 28.16 | 0.00 | 100.00 |
| GDPpc | 32,987 | 21,561.03 | 21,235.55 | 661.24 | 116,935.60 |
| Hospital Beds per 1000 | 30,254 | 3.03 | 2.46 | 0.10 | 13.05 |
| Diabetes prevalence | 34,003 | 7.77 | 3.96 | 0.99 | 22.02 |
| Median age | 33,163 | 31.30 | 9.21 | 15.10 | 48.20 6p1.0 Sources: JHU CSSE COVID-19 Data, OxCGRT, World Bank, United Nations. |
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Total Cases per million | Total Cases per million | Total Cases per million | Total Cases per million | |
| Govt Response | 0.1540 | |||
| (0.0139) | ||||
| Govt Response Sq. | −0.0012 | |||
| (0.0001) | ||||
| Economic Support | 0.0599 | |||
| (0.0095) | ||||
| Economic Support Sq. | −0.0004 | |||
| (0.0001) | ||||
| Containment Health | 0.1323 | |||
| (0.0117) | ||||
| Containment Health Sq. | −0.0010 | |||
| (0.0001) | ||||
| Stringency | 0.1046 | |||
| (0.0102) | ||||
| Stringency Sq. | −0.0009 | |||
| (0.0001) | ||||
| ln(GDPpc) | 0.0899 | 0.3071 | 0.2341 | 0.3188 |
| (0.1153) | (0.1344) | (0.1139) | (0.1179) | |
| ln(Hospital Beds per 1000) | 0.2305 | 0.1948 | 0.1949 | 0.2625 |
| (0.1179) | (0.1355) | (0.1136) | (0.1104) | |
| Diabetes prevalence | −0.0002 | −0.0082 | −0.0158 | −0.0218 |
| (0.0199) | (0.0248) | (0.0193) | (0.0189) | |
| Median age | 0.0317 | 0.0043 | 0.0311 | 0.0203 |
| (0.0145) | (0.0154) | (0.0148) | (0.0141) | |
| Total Cases per million | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| (0.0000) | (0.0000) | (0.0000) | (0.0000) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −6,849,649.631 | −7,234,408.436 | −7,149,392.860 | −7,371,750.750 |
| Obs | 27,796 | 27,804 | 27,796 | 27,809 |
| (1) Total Deaths (7-Day MA) | (2) Total Deaths (7-Day MA) | (3) Total Deaths (7-Day MA) | (4) Total Deaths (7-Day MA) | |
|---|---|---|---|---|
| Total Deaths (1 Week MA) | ||||
| Govt Response | 0.1212 | |||
| (0.0136) | ||||
| Govt Response Sq. | −0.0009 | |||
| (0.0001) | ||||
| Economic Support | 0.0638 | |||
| (0.0117) | ||||
| Economic Support Sq. | −0.0004 | |||
| (0.0001) | ||||
| Containment Health | 0.1180 | |||
| (0.0171) | ||||
| Containment Health Sq. | −0.0009 | |||
| (0.0002) | ||||
| Stringency | 0.0863 | |||
| (0.0112) | ||||
| Stringency Sq. | −0.0007 | |||
| (0.0001) | ||||
| ln(GDPpc) | −0.0270 | 0.1757 | 0.0748 | 0.1785 |
| (0.1186) | (0.1303) | (0.1177) | (0.1082) | |
| ln(Hospital Beds per 1000) | 0.0866 | 0.0546 | 0.0459 | 0.0920 |
| (0.1395) | (0.1673) | (0.1411) | (0.1332) | |
| Diabetes prevalence | 0.0165 | 0.0223 | 0.0030 | −0.0035 |
| (0.0189) | (0.0278) | (0.0187) | (0.0181) | |
| Median age | 0.0573 | 0.0316 | 0.0601 | 0.0526 |
| (0.0174) | (0.0175) | (0.0174) | (0.0160) | |
| Total Deaths (1 Week MA) | 0.0050 | 0.0048 | 0.0050 | 0.0049 |
| (0.0006) | (0.0006) | (0.0005) | (0.0006) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −205,123.251 | −197,363.853 | −207,796.534 | −218,102.169 |
| Obs | 27,008 | 27,016 | 27,008 | 27,021 |
| (1) Total Deaths (7-Day MA) | (2) Total Deaths (7-Day MA) | (3) Total Deaths (7-Day MA) | (4) Total Deaths (7-Day MA) | |
|---|---|---|---|---|
| Govt Response | 0.1195 | |||
| (0.0134) | ||||
| Govt Response Sq. | −0.0009 | |||
| (0.0001) | ||||
| Economic Support | 0.0624 | |||
| (0.0112) | ||||
| Economic Support Sq. | −0.0004 | |||
| (0.0001) | ||||
| Containment Health | 0.1178 | |||
| (0.0175) | ||||
| Containment Health Sq. | −0.0009 | |||
| (0.0002) | ||||
| Stringency | 0.0858 | |||
| (0.0113) | ||||
| Stringency Sq. | −0.0007 | |||
| (0.0001) | ||||
| ln(GDPpc) | −0.0221 | 0.1845 | 0.0788 | 0.1822 |
| (0.1188) | (0.1313) | (0.1178) | (0.1085) | |
| ln(Hospital Beds per 1000) | 0.0761 | 0.0437 | 0.0364 | 0.0838 |
| (0.1409) | (0.1687) | (0.1426) | (0.1344) | |
| Diabetes prevalence | 0.0149 | 0.0211 | 0.0017 | −0.0048 |
| (0.0188) | (0.0280) | (0.0186) | (0.0181) | |
| Median age | 0.0584 | 0.0326 | 0.0612 | 0.0536 |
| (0.0174) | (0.0176) | (0.0174) | (0.0160) | |
| Total Deaths (2 Week MA) | 0.0049 | 0.0048 | 0.0048 | 0.0048 |
| (0.0005) | (0.0005) | (0.0005) | (0.0005) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −194,709.841 | −188,724.385 | −196,368.352 | −206,054.168 |
| Obs | 26,058 | 26,063 | 26,058 | 26,067 |
| (1) Total Deaths per million | (2) Total Deaths per million | (3) Total Deaths per million | (4) Total Deaths per million | |
|---|---|---|---|---|
| Govt Response | −0.00359 | |||
| (0.00687) | ||||
| Govt Response Sq. | 0.00022 | |||
| (0.00009) | ||||
| Economic Support | 0.00846 | |||
| (0.00651) | ||||
| Economic Support Sq. | 0.00003 | |||
| (0.00010) | ||||
| Containment Health | 0.00617 | |||
| (0.00714) | ||||
| Containment Health Sq. | 0.00009 | |||
| (0.00008) | ||||
| Stringency | 0.00618 | |||
| (0.00630) | ||||
| Stringency Sq. | 0.00009 | |||
| (0.00007) | ||||
| ln(GDPpc) | 0.11763 | 0.20647 | 0.15461 | 0.17885 |
| (0.07044) | (0.07298) | (0.06972) | (0.06676) | |
| ln(Hospital Beds per 1000) | −0.10087 | −0.13248 | −0.11027 | −0.08741 |
| (0.07253) | (0.07584) | (0.07083) | (0.06838) | |
| Diabetes prevalence | −0.03441 | −0.02933 | −0.03756 | −0.03636 |
| (0.01527) | (0.01554) | (0.01511) | (0.01444) | |
| Median age | 0.01309 | 0.00403 | 0.01404 | 0.01222 |
| (0.01088) | (0.01198) | (0.01033) | (0.00997) | |
| Total Deaths per million | 1.00222 | 1.00193 | 1.00233 | 1.00248 |
| (0.00140) | (0.00151) | (0.00140) | (0.00137) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| Overall R2 | 0.9997 | 0.9997 | 0.9997 | 0.9997 |
| Obs | 27,796 | 27,804 | 27,796 | 27,809 |
References
- Hale, T.; Webster, S.; Petherick, A.; Phillips, T.; Kira, B. Oxford COVID-19 Government Response Tracker; Blavatnik School of Government Working Paper Series; Blavatnik School of Government: Oxford, UK, 2020. [Google Scholar]
- World Bank. Global Economic Prospects; Technical Report; The World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Jorda, O.; Singh, S.; Taylor, A. Longer-Run Economic Consequences of Pandemics. Covid Econ. 2020, 1, 1–15. [Google Scholar] [CrossRef]
- Barro, R.J.; Ursua, J.F.; Weng, J. The Coronavirus and the Great Influenza Epidemic—Lessons from the “Spanish Flu” for the Coronavirus’s Potential Effects on Mortality and Economic Activity; CESifo Working Paper Series 8166; CESifo: Munich, Germany, 2020. [Google Scholar]
- Brahmbhatt, M.; Dutta, A. On SARS type economic effects during infectious disease outbreaks; The World Bank: Washington, DC, USA, 2008. [Google Scholar]
- Maphanga, P.; Henama, U. The Tourism Impact of Ebola in Africa: Lessons on Crisis Management. Afr. J. Hosp. Tour. Leis. 2019, 8, 1–13. [Google Scholar]
- Dixon, S.; McDonald, S.; Roberts, J. The impact of HIV and AIDS on Africa’s economic development. BMJ 2002, 324, 232–234. [Google Scholar] [CrossRef] [PubMed]
- IMF. A Crisis Like No Other, An Uncertain Recovery; World Economic Outlook: Washington, DC, USA, 2020. [Google Scholar]
- Tan, W.J.; Enderwick, P. Managing threats in the global era: The impact and response to SARS. Thunderbird Int. Bus. Rev. 2006, 48, 515–536. [Google Scholar] [CrossRef]
- Deurenberg-Yap, M.; Foo, L.; Low, Y.; Chan, S.; Vijaya, K.; Lee, M. The Singaporean response to the SARS outbreak: Knowledge sufficiency versus public trust. Health Promot. Int. 2005, 20, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Inf. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Khan, J.R.; Awan, N.; Islam, M.M.; Muurlink, O. Healthcare Capacity, Health Expenditure, and Civil Society as Predictors of COVID-19 Case Fatalities: A Global Analysis. Front. Public Health 2020, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Banik, A.; Nag, T.; Chowdhury, S.R.; Chatterjee, R. Why Do COVID-19 Fatality Rates Differ Across Countries? An Explorative Cross-country Study Based on Select Indicators. Glob. Bus. Rev. 2020, 21, 607–625. [Google Scholar] [CrossRef]
- Haldar, A.; Sethi, N. The Effect of Country-level Factors and Government Intervention on the Incidence of COVID-19. Asian Econ. Lett. 2020, 1. [Google Scholar] [CrossRef]
- Mathur, P.; Rangamani, S. COVID-19 and noncommunicable diseases: Identifying research priorities to strengthen public health response. Int. J. Noncommunicable Dis. 2020, 5, 76. [Google Scholar] [CrossRef]
- Singh, A.K.; Misra, A. Impact of COVID-19 and comorbidities on health and economics: Focus on developing countries and India. Diabetes Metab. Syndr. 2020, 14, 1625–1630. [Google Scholar] [CrossRef] [PubMed]
- Dergiades, T.; Milas, C.; Mossialos, E.; Panagiotidis, T. Effectiveness of Government Policies in Response to the COVID-19 Outbreak. Ssrn Electron. J. 2020. [Google Scholar] [CrossRef]
- Allel, K.; Tapia-Muñoz, T.; Morris, W. Country-level factors associated with the early spread of COVID-19 cases at 5, 10 and 15 days since the onset. Glob. Public Health 2020, 15, 1589–1602. [Google Scholar] [CrossRef] [PubMed]
- United Nations. World Economic Situation and Prospects; Technical Report; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Amadeo, K. Emerging Market Countries and Their Five Defining Characteristics; The Balance; U.S. & World Economies: New York, NY, USA, 2020. [Google Scholar]
| (1) Total Deaths per million | (2) Total Deaths per million | (3) Total Deaths per million | (4) Total Deaths per million | |
|---|---|---|---|---|
| Govt Response | 0.0221 | |||
| (0.0019) | ||||
| Economic Support | 0.0249 | |||
| (0.0032) | ||||
| Containment Health | 0.0178 | |||
| (0.0017) | ||||
| Stringency | 0.0130 | |||
| (0.0016) | ||||
| ln(GDPpc) | 0.2500 | 0.2058 | 0.2956 | 0.3266 |
| (0.1072) | (0.1246) | (0.1056) | (0.1050) | |
| ln(Hospital Beds per 1000) | 0.0445 | 0.0838 | 0.0265 | 0.0444 |
| (0.1548) | (0.1668) | (0.1560) | (0.1463) | |
| Diabetes prevalence | 0.0124 | 0.0260 | 0.0063 | 0.0040 |
| (0.0210) | (0.0242) | (0.0209) | (0.0202) | |
| Median Age | 0.0376 | 0.0279 | 0.0393 | 0.0400 |
| (0.0174) | (0.0179) | (0.0176) | (0.0172) | |
| Total Deaths per million | 0.0057 | 0.0050 | 0.0059 | 0.0061 |
| (0.0007) | (0.0006) | (0.0007) | (0.0007) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −243,301.674 | −220,033.856 | −254,352.726 | −263,453.359 |
| Obs | 27,796 | 27,804 | 27,796 | 27,809 |
| (1) Total Deaths per million | (2) Total Deaths per million | (3) Total Deaths per million | (4) Total Deaths per million | |
|---|---|---|---|---|
| Govt Response | 0.1258 | |||
| (0.0139) | ||||
| Govt Response Sq. | −0.0009 | |||
| (0.0001) | ||||
| Economic Support | 0.0662 | |||
| (0.0118) | ||||
| Economic Support Sq. | −0.0004 | |||
| (0.0001) | ||||
| Containment Health | 0.1205 | |||
| (0.0172) | ||||
| Containment Health Sq. | −0.0009 | |||
| (0.0002) | ||||
| Stringency | 0.0874 | |||
| (0.0111) | ||||
| Stringency Sq. | −0.0007 | |||
| (0.0001) | ||||
| ln(GDPpc) | −0.0354 | 0.1693 | 0.0682 | 0.1732 |
| (0.1188) | (0.1303) | (0.1180) | (0.1085) | |
| ln(Hospital Beds per 1000) | 0.0927 | 0.0582 | 0.0509 | 0.0965 |
| (0.1393) | (0.1672) | (0.1407) | (0.1331) | |
| Diabetes prevalence | 0.0177 | 0.0231 | 0.0040 | −0.0024 |
| (0.0189) | (0.0279) | (0.0187) | (0.0182) | |
| Median Age | 0.0572 | 0.0313 | 0.0601 | 0.0525 |
| (0.0174) | (0.0175) | (0.0174) | (0.0160) | |
| Total Deaths per million | 0.0051 | 0.0049 | 0.0050 | 0.0050 |
| (0.0006) | (0.0006) | (0.0005) | (0.0006) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −210,701.111 | −201,951.388 | −215,056.338 | −226,469.993 |
| Obs | 27,796 | 27,804 | 27,796 | 27,809 |
| (1) Africa | (2) Asia | (3) Europe | (4) Americas | |
|---|---|---|---|---|
| Total Deaths per million | ||||
| Govt Response | 0.1434 | 0.1303 | 0.1208 | 0.1986 |
| (0.0353) | (0.0229) | (0.0148) | (0.0655) | |
| Govt Response Sq. | −0.0013 | −0.0010 | −0.0009 | −0.0014 |
| (0.0003) | (0.0002) | (0.0001) | (0.0005) | |
| ln(GDPpc) | −0.0003 | 0.3606 | −0.0908 | −0.0429 |
| (0.2908) | (0.2430) | (0.2191) | (0.4063) | |
| ln(Hospital Beds per 1000) | 0.2113 | 0.1549 | −0.2944 | 0.2144 |
| (0.1817) | (0.3220) | (0.2105) | (0.3721) | |
| Diabetes prevalence | 0.0264 | 0.0535 | 0.0383 | 0.0004 |
| (0.0280) | (0.0651) | (0.0519) | (0.0590) | |
| Median age | 0.0061 | −0.0748 | 0.0155 | −0.0207 |
| (0.0419) | (0.0423) | (0.0430) | (0.0487) | |
| Total Deaths per million | 0.0204 | 0.0170 | 0.0042 | 0.0051 |
| (0.0048) | (0.0039) | (0.0005) | (0.0008) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −17,505.631 | −31,313.826 | −77,022.193 | −59,259.656 |
| Obs | 5940 | 9068 | 7911 | 4877 |
| (1) Africa | (2) Asia | (3) Europe | (4) Americas | |
|---|---|---|---|---|
| Total Deaths per million | ||||
| Containment Health | 0.1554 | 0.1162 | 0.1065 | 0.2119 |
| (0.0351) | (0.0192) | (0.0189) | (0.0842) | |
| Containment Health Sq. | −0.0013 | −0.0009 | −0.0008 | −0.0015 |
| (0.0003) | (0.0002) | (0.0002) | (0.0006) | |
| ln(GDPpc) | 0.0992 | 0.4108 | 0.0568 | −0.0857 |
| (0.2503) | (0.2310) | (0.2020) | (0.4367) | |
| ln(Hospital Beds per 1000) | 0.1979 | 0.1211 | −0.2535 | 0.0980 |
| (0.1852) | (0.3172) | (0.2207) | (0.3502) | |
| Diabetes prevalence | 0.0217 | 0.0452 | 0.0327 | −0.0059 |
| (0.0267) | (0.0646) | (0.0506) | (0.0511) | |
| Median age | 0.0062 | −0.0746 | 0.0137 | 0.0116 |
| (0.0385) | (0.0445) | (0.0422) | (0.0502) | |
| Total Deaths per million | 0.0188 | 0.0169 | 0.0043 | 0.0051 |
| (0.0043) | (0.0039) | (0.0005) | (0.0007) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −16,756.492 | −32,168.453 | −82,180.944 | −59,089.920 |
| Obs | 5940 | 9068 | 7911 | 4877 |
| (1) Africa | (2) Asia | (3) Europe | (4) Americas | |
|---|---|---|---|---|
| Total Deaths per million | ||||
| Economic Support | 0.0311 | 0.0758 | 0.0605 | 0.0705 |
| (0.0148) | (0.0187) | (0.0184) | (0.0171) | |
| Economic Support Sq. | −0.0000 | −0.0004 | −0.0004 | −0.0005 |
| (0.0002) | (0.0001) | (0.0001) | (0.0001) | |
| ln(GDPpc) | 0.0249 | 0.2816 | 0.1185 | 0.1717 |
| (0.2319) | (0.2427) | (0.2200) | (0.4066) | |
| ln(Hospital Beds per 1000) | 0.3672 | 0.2462 | −0.3895 | 0.2154 |
| (0.1758) | (0.2980) | (0.2219) | (0.4065) | |
| Diabetes prevalence | 0.0002 | 0.0773 | 0.0677 | −0.1004 |
| (0.0296) | (0.0651) | (0.0525) | (0.0490) | |
| Median age | 0.0169 | −0.0896 | −0.0107 | −0.0318 |
| (0.0491) | (0.0430) | (0.0444) | (0.0474) | |
| Total Deaths per million | 0.0175 | 0.0153 | 0.0043 | 0.0051 |
| (0.0067) | (0.0033) | (0.0006) | (0.0010) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −16,801.643 | −27,031.301 | −77,990.057 | −61,516.709 |
| Obs | 5948 | 9067 | 7911 | 4878 |
| (1) Africa | (2) Asia | (3) Europe | (4) Americas | |
|---|---|---|---|---|
| Total Deaths per million | ||||
| Stringency | 0.1246 | 0.1090 | 0.0726 | 0.1727 |
| (0.0256) | (0.0184) | (0.0116) | (0.0587) | |
| Stringency Sq. | −0.0012 | −0.0009 | −0.0006 | −0.0012 |
| (0.0002) | (0.0002) | (0.0001) | (0.0004) | |
| ln(GDPpc) | 0.1645 | 0.4787 | 0.1722 | −0.0436 |
| (0.2404) | (0.2157) | (0.1950) | (0.3371) | |
| ln(Hospital Beds per 1000) | 0.2283 | −0.0155 | −0.1337 | 0.2010 |
| (0.1746) | (0.3372) | (0.2141) | (0.3632) | |
| Diabetes prevalence | 0.0178 | 0.0240 | 0.0297 | 0.0408 |
| (0.0242) | (0.0605) | (0.0494) | (0.0379) | |
| Median age | 0.0284 | -0.0620 | 0.0130 | 0.0625 |
| (0.0505) | (0.0506) | (0.0402) | (0.0499) | |
| Total Deaths per million | 0.0178 | 0.0168 | 0.0045 | 0.0049 |
| (0.0038) | (0.0038) | (0.0006) | (0.0008) | |
| Chamberlain | Yes | Yes | Yes | Yes |
| LogLik | −16,061.114 | −31,846.813 | −91,586.176 | −58,733.588 |
| Obs | 5940 | 9079 | 7911 | 4879 |
| Advanced | Emerging | LDC |
|---|---|---|
| Australia | Argentina | Afghanistan |
| Austria | Brazil | Angola |
| Belgium | Chile | Bangladesh |
| Bulgaria | China | Benin |
| Canada | Colombia | Bhutan |
| Croatia | Egypt | Burkina Faso |
| Cyprus | Hong Kong | Burundi |
| Czech Republic | India | Cambodia |
| Denmark | Indonesia | Central African Republic |
| Estonia | Jordan | Chad, Comoros |
| Finland | Korea | DR of the Congo |
| France | Kuwait | Djibouti |
| Germany | Malaysia | Eritrea |
| Greece | Mexico | Ethiopia |
| Hungary | Pakistan | Gambia |
| Iceland | Peru | Guinea |
| Ireland | Philippines | Guinea-Bissau |
| Italy | Qatar | Haiti |
| Japan | Russia | Kiribati |
| Latvia | Saudi Arabia | Lao PDR |
| Lithuania | Singapore | Lesotho |
| Luxembourg | South Africa | Liberia |
| Malta | Taiwan | Madagascar |
| Netherlands | Thailand | Malawi |
| Norway | Turkey | Mali |
| New Zealand | United Arab Emirates | Mauritania |
| Poland | Vietnam | Mozambique |
| Portugal | Myanmar | |
| Slovakia | Nepal | |
| Slovenia | Niger | |
| Spain | Rwanda | |
| Sweden | Sao Tome and Principe | |
| Switzerland | Senegal | |
| United Kingdom | Sierra Leone | |
| United States | Solomon Islands | |
| Somalia | ||
| South Sudan | ||
| Sudan | ||
| Timor-Leste | ||
| Togo | ||
| Tuvalu | ||
| Uganda | ||
| Tanzania | ||
| Vanuatu | ||
| Yemen | ||
| Zambia |
| (1) Advanced | (2) Emerging | (3) LDC | |
|---|---|---|---|
| Total Deaths per million | |||
| Govt Response | 0.1222 | 0.2730 | 0.0381 |
| (0.0150) | (0.0810) | (0.0303) | |
| Govt Response Sq. | −0.0009 | −0.0020 | −0.0003 |
| (0.0001) | (0.0006) | (0.0003) | |
| ln(GDPpc) | 1.0610 | 0.9588 | −1.0584 |
| (0.3408) | (0.6387) | (0.7484) | |
| ln(Hospital Beds per 1000) | −0.5320 | 0.3131 | −0.4070 |
| (0.2861) | (0.3739) | (0.3207) | |
| Diabetes prevalence | −0.0055 | −0.0770 | 0.2122 |
| (0.0558) | (0.0627) | (0.0981) | |
| Median age | 0.1254 | −0.1380 | 0.0680 |
| (0.0500) | (0.1037) | (0.1063) | |
| Total Deaths per million | 0.0042 | 0.0051 | 0.0841 |
| (0.0004) | (0.0011) | (0.0280) | |
| Chamberlain | Yes | Yes | Yes |
| LogLik | −64,247.637 | −47,840.717 | −7769.830 |
| Obs | 7561 | 5345 | 4969 |
| (1) Advanced | (2) Emerging | (3) LDC | |
|---|---|---|---|
| Total Deaths per million | |||
| Containment Health | 0.1001 | 0.3239 | 0.0306 |
| (0.0178) | (0.0860) | (0.0225) | |
| Containment Health Sq. | −0.0007 | −0.0024 | −0.0003 |
| (0.0002) | (0.0006) | (0.0002) | |
| ln(GDPpc) | 1.0972 | 0.9287 | −1.1951 |
| (0.3328) | (0.5924) | (0.9703) | |
| ln(Hospital Beds per 1000) | −0.5033 | 0.2324 | −0.3695 |
| (0.2845) | (0.3180) | (0.3816) | |
| Diabetes prevalence | −0.0104 | −0.0878 | 0.2147 |
| (0.0596) | (0.0633) | (0.1422) | |
| Median age | 0.1203 | −0.1291 | 0.0239 |
| (0.0493) | (0.1003) | (0.0854) | |
| Total Deaths per million | 0.0044 | 0.0050 | 0.0831 |
| (0.0005) | (0.0009) | (0.0278) | |
| Chamberlain | Yes | Yes | Yes |
| LogLik | −72,145.225 | −45,344.604 | −7789.105 |
| Obs | 7561 | 5345 | 4969 |
| (1) Advanced | (2) Emerging | (3) LDC | |
|---|---|---|---|
| Total Deaths per million | |||
| Economic Support | 0.0846 | 0.1064 | 0.0151 |
| (0.0092) | (0.0230) | (0.0172) | |
| Economic Support Sq. | −0.0005 | −0.0007 | −0.0001 |
| (0.0001) | (0.0002) | (0.0002) | |
| ln(GDPpc) | 1.1074 | 1.0170 | −1.1742 |
| (0.3450) | (0.7477) | (1.1239) | |
| ln(Hospital Beds per 1000) | −0.4767 | 0.2079 | −0.1275 |
| (0.3123) | (0.6626) | (0.2679) | |
| Diabetes prevalence | 0.0211 | −0.0894 | 0.1178 |
| (0.0452) | (0.1051) | (0.0703) | |
| Median age | 0.0982 | −0.1579 | −0.0472 |
| (0.0651) | (0.1906) | (0.0704) | |
| Total Deaths per million | 0.0039 | 0.0045 | 0.0838 |
| (0.0004) | (0.0009) | (0.0253) | |
| Chamberlain | Yes | Yes | Yes |
| LogLik | −59,564.850 | −43,714.656 | −7741.987 |
| Obs | 7561 | 5345 | 4977 |
| (1) Advanced | (2) Emerging | (3) LDC | |
|---|---|---|---|
| Total Deaths per million | |||
| Stringency | 0.0667 | 0.1734 | 0.0508 |
| (0.0108) | (0.0352) | (0.0246) | |
| Stringency Sq. | −0.0005 | −0.0013 | −0.0005 |
| (0.0001) | (0.0003) | (0.0002) | |
| ln(GDPpc) | 1.1694 | 0.8301 | −1.2336 |
| (0.3320) | (0.6075) | (1.1679) | |
| ln(Hospital Beds per 1000) | −0.3679 | 0.3416 | −0.4268 |
| (0.2838) | (0.3340) | (0.5771) | |
| Diabetes prevalence | −0.0129 | −0.0481 | 0.2119 |
| (0.0556) | (0.0645) | (0.1783) | |
| Median age | 0.1151 | −0.1079 | 0.0431 |
| (0.0500) | (0.0994) | (0.1095) | |
| Total Deaths per million | 0.0046 | 0.0047 | 0.0781 |
| (0.0005) | (0.0009) | (0.0285) | |
| Chamberlain | Yes | Yes | Yes |
| LogLik | −81,171.943 | −48,069.052 | −7737.934 |
| Obs | 7561 | 5347 | 4979 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chisadza, C.; Clance, M.; Gupta, R. Government Effectiveness and the COVID-19 Pandemic. Sustainability 2021, 13, 3042. https://doi.org/10.3390/su13063042
Chisadza C, Clance M, Gupta R. Government Effectiveness and the COVID-19 Pandemic. Sustainability. 2021; 13(6):3042. https://doi.org/10.3390/su13063042
Chicago/Turabian StyleChisadza, Carolyn, Matthew Clance, and Rangan Gupta. 2021. "Government Effectiveness and the COVID-19 Pandemic" Sustainability 13, no. 6: 3042. https://doi.org/10.3390/su13063042
APA StyleChisadza, C., Clance, M., & Gupta, R. (2021). Government Effectiveness and the COVID-19 Pandemic. Sustainability, 13(6), 3042. https://doi.org/10.3390/su13063042








