Consequences of Confinement Due to COVID-19 in Spain on Anxiety, Sleep and Executive Functioning of Children and Adolescents with ADHD
Abstract
1. Introduction
2. Materials and Methods
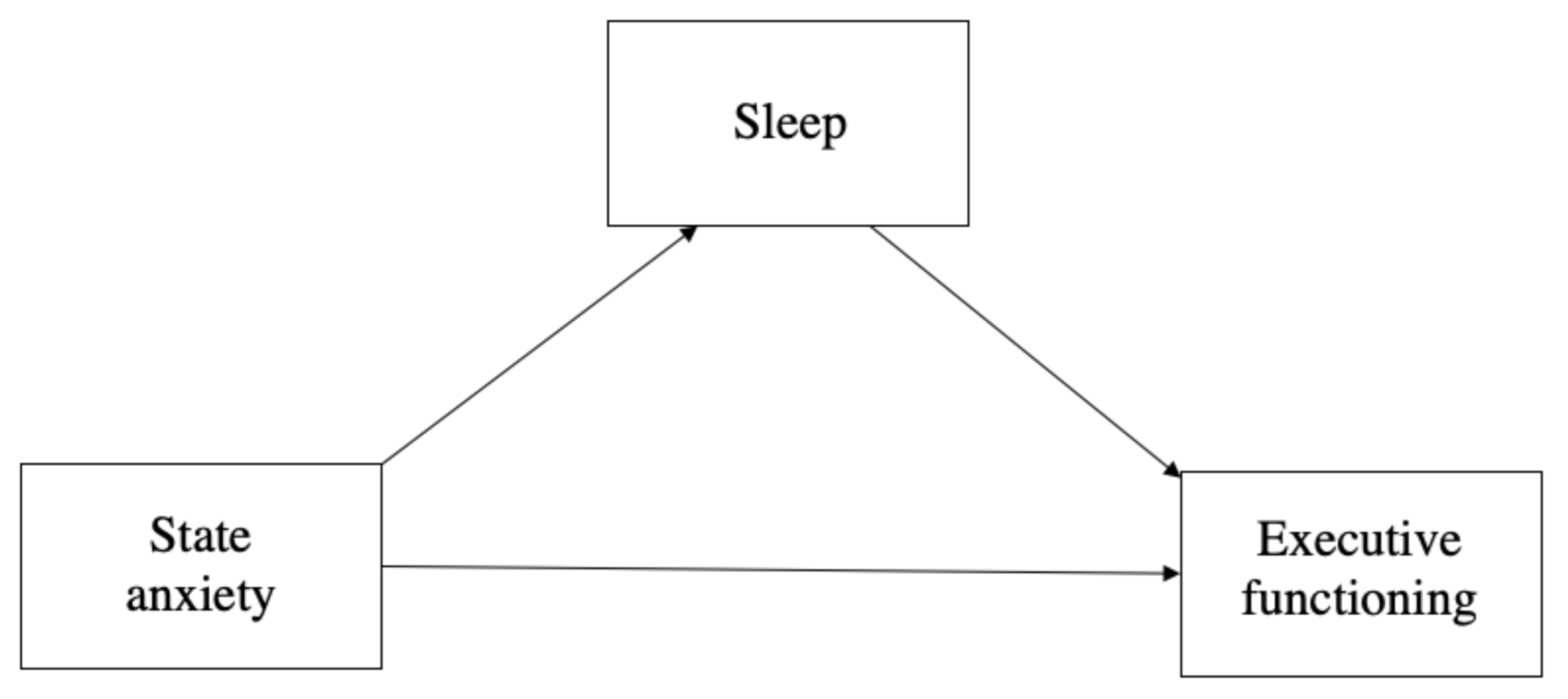
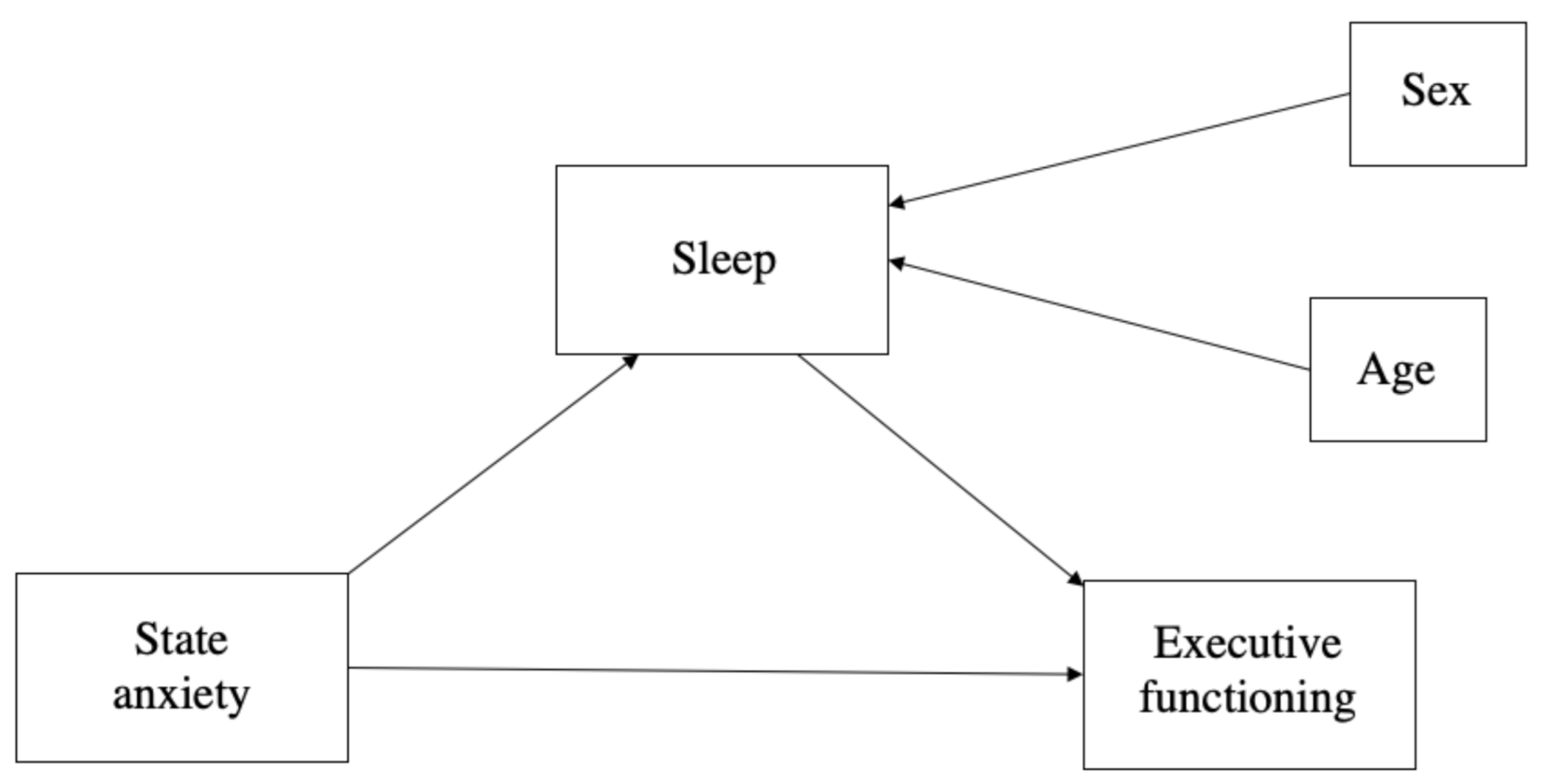
2.1. Design
2.2. Participants
2.3. Instruments
- Ad hoc sociodemographic and clinical data questionnaire
- State–Trait Anxiety Inventory for Children (STAIC) self-assessment questionnaire [52]
- Barkley Deficits in Executive Functioning Scale—Children and Adolescents (BDEFS-CA), short form [55]
2.4. Procedure
2.5. Ethics Committee
2.6. Statistical Analysis
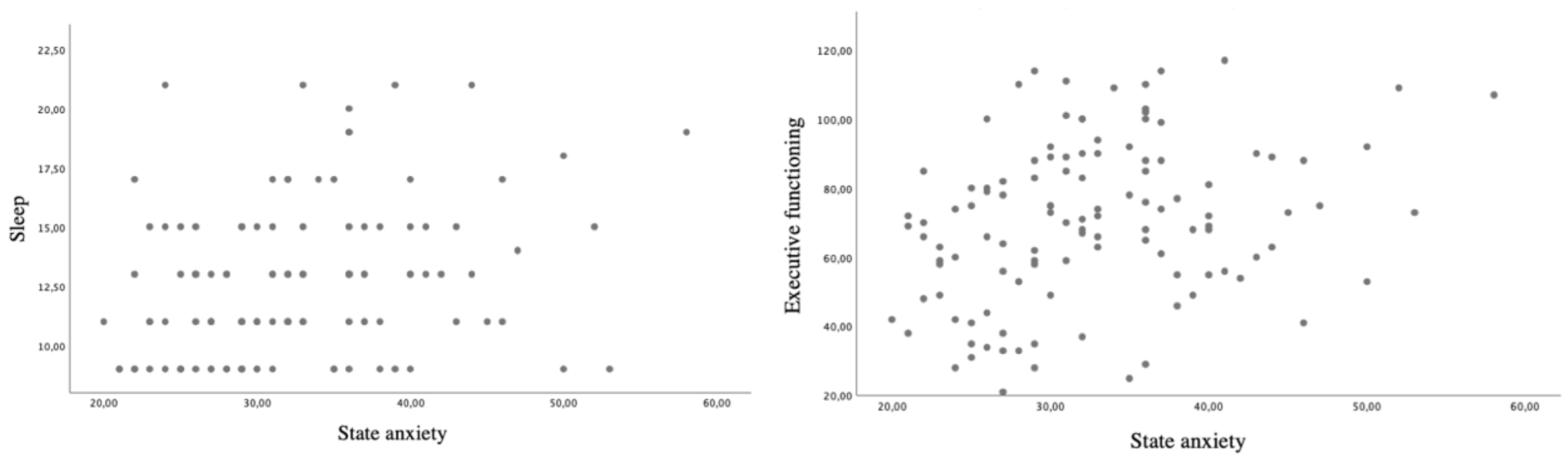
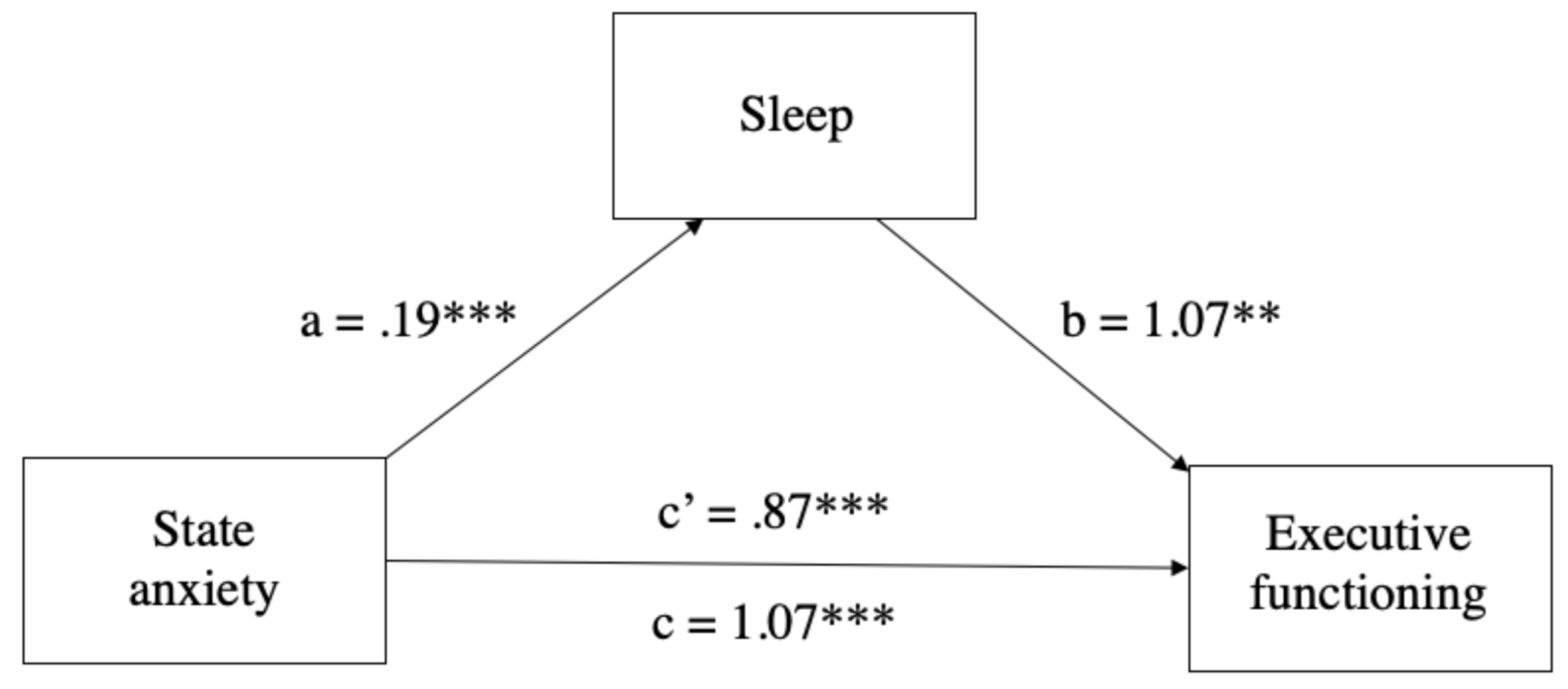
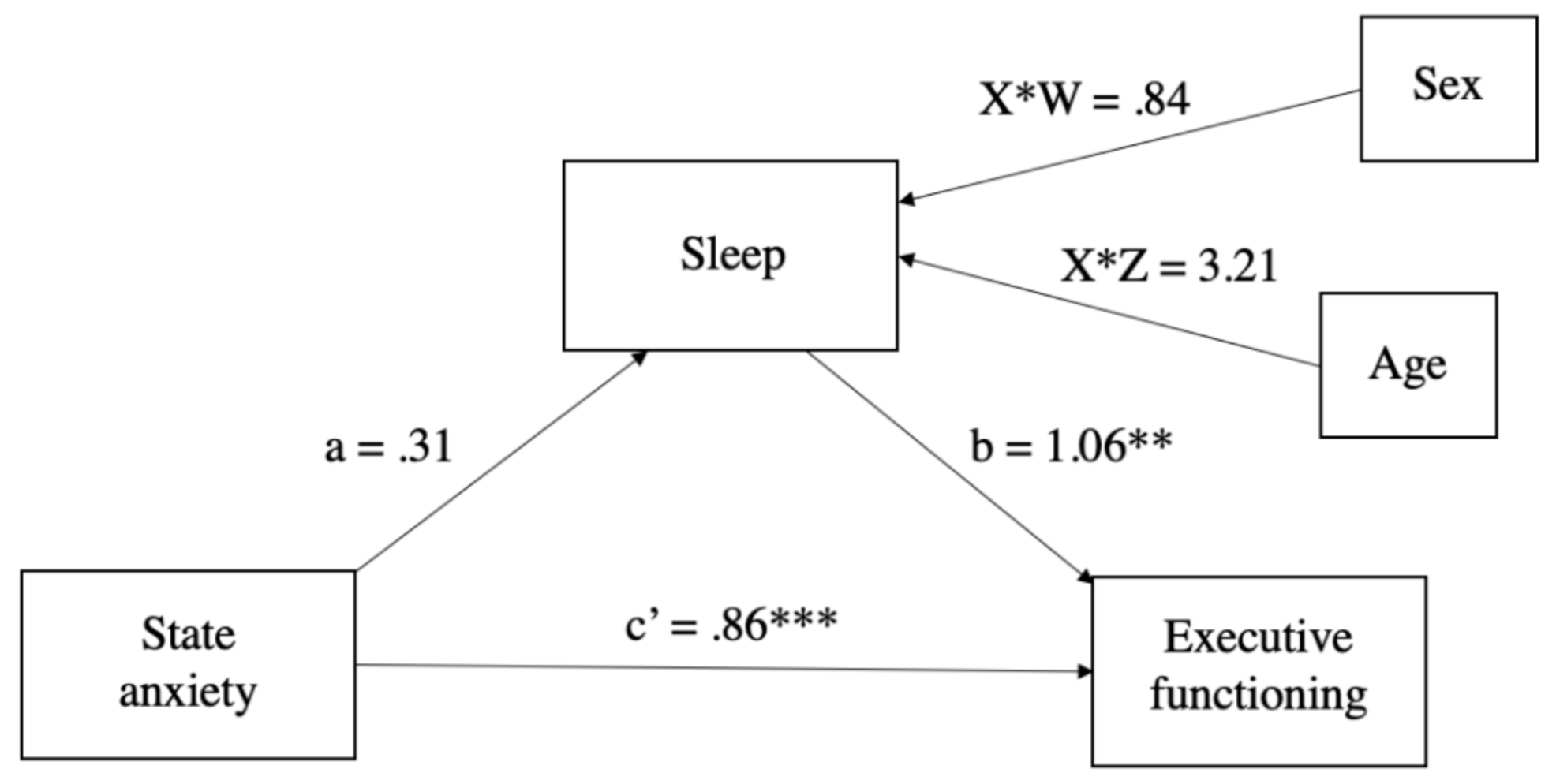
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De España, G. Real Decreto 463/2020, de 14 de Marzo, Por El Que Se Declara El Estado de Alarma Para La Gestión de La Situación de Crisis Sanitaria Ocasionada Por El COVID-19; BOE-A-2020-3692); Agencia Estatal Boletín Oficial del Estado: Madrid, Spain, 2020. [Google Scholar]
- Danese, A.; Smith, P.; Chitsabesan, P.; Dubicka, B. Child and adolescent mental health amidst emergencies and disasters. Br. J. Psychiatry 2020, 216, 159–162. [Google Scholar] [CrossRef]
- Moya, M.; Willis, G.B.; Paez, D.; Pérez, J.A.; Gómez, Á.; Sabucedo-Cameselle, J.M.; Alzate, M.; Hur, D.; Rodríguez, A.; Extremera, N. La Psicología Social Ante El COVID19: Monográfico Del International. J. Soc. Psychol. Rev. Psicol. Soc. 2020. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, 1–8. [Google Scholar]
- Duan, L.; Zhu, G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020, 7, 300–302. [Google Scholar] [CrossRef]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15–e16. [Google Scholar] [CrossRef]
- Yang, Y.; Li, W.; Zhang, Q.; Zhang, L.; Cheung, T.; Xiang, Y.-T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e19. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, R. Comparación de Tratamiento Farmacológico, Intervención Psicoeducativa y Tratamiento Combinado: La Importancia Del Sistema Ejecutivo y Sus Funciones; Universidad de Málaga: Málaga, Spain, 2009. [Google Scholar]
- Vallejo-Slocker, L.; Fresneda, J.; A Vallejo, M. Psychological Wellbeing of Vulnerable Children During the COVID-19 Pandemic. Psicothema 2020, 32, 501–507. [Google Scholar]
- De Miranda, D.M.; Athanasio, B.D.S.; Oliveira, A.C.S.; Simoes-E-Silva, A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. 2020, 51, 101845. [Google Scholar] [CrossRef] [PubMed]
- Ramadhan, M.H.A.; Putri, A.K.; Melinda, D.; Habibah, U.; Fajriyah, U.N.; Aini, S.; Prananjaya, B.A.; Ikhsan, D.S. Children’s Mental Health in the Time of COVID-19: How Things Stand and the Aftermath. Malays. J. Med Sci. 2020, 27, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, M.D.; Balluerka, N.; Gorostiaga, A.; Espada, J.P.; Santed, M.Á.; Padilla, J.L.; Gómez-Benito, J. The Psychological Consequences of COVID-19 and Lockdown in the Spanish Population: An Exploratory Sequential Design. Int. J. Environ. Res. Public Health 2020, 17, 8578. [Google Scholar] [CrossRef] [PubMed]
- Morgül, E.; Kallitsoglou, A.; Essau, C.A. Psychological Effects of the COVID-19 Lockdown on Children and Families in the UK. Rev. Psicol. Clínica Con Niños Adolesc. 2020, 7, 42–48. [Google Scholar] [CrossRef]
- Asmundson, G.J.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 102211. [Google Scholar] [CrossRef] [PubMed]
- Vahia, I.V.; Blazer, D.G.; Smith, G.S.; Karp, J.F.; Steffens, D.C.; Forester, B.P.; Tampi, R.; Agronin, M.; Jeste, D.V.; Reynolds, C.F. COVID-19, Mental Health and Aging: A Need for New Knowledge to Bridge Science and Service. Am. J. Geriatr. Psychiatry 2020, 28, 695–697. [Google Scholar] [CrossRef]
- Cortese, S.; Asherson, P.; Sonuga-Barke, E.; Banaschewski, T.; Brandeis, D.; Buitelaar, J.; Coghill, D.; Daley, D.; Danckaerts, M.; Dittmann, R.W.; et al. ADHD management during the COVID-19 pandemic: Guidance from the European ADHD Guidelines Group. Lancet Child Adolesc. Health 2020, 4, 412–414. [Google Scholar] [CrossRef]
- Chen, Z.; Tong, L.; Zhou, Y.; Hua, C.; Wang, W.; Fu, J.; Shu, Q.; Hong, L.; Xu, H.; Xu, Z.; et al. Childhood COVID-19: A multicentre retrospective study. Clin. Microbiol. Infect. 2020, 26, 1260.e1–1260.e4. [Google Scholar] [CrossRef]
- Castellanos, F.X.; Marvasti, F.F.; Ducharme, J.L.; Walter, J.M.; Israel, M.E.; Krain, A.; Pavlovsky, C.; Hommer, D.W. Executive Function Oculomotor Tasks in Girls With ADHD. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Capilla-González, A.; Fernández-González, S.; Campo, P.; Maestú, F.; Fernández-Lucas, A.; Mulas, F.; Ortiz, T. Magnetoencephalography in cognitive disorders involving frontal lobes. Revista de Neurología 2004, 39, 183–188. [Google Scholar]
- Román, A.C.; Grande, D.D.R.; González, A.C.; Unturbe, F.M.; Alonso, T.O. Bases neurobiológicas de las dificultades de aprendizaje. Revista de Neurología 2006, 42, S171. [Google Scholar] [CrossRef]
- Epstein, J.N.; Casey, B.; Tonev, S.T.; Davidson, M.C.; Reiss, A.L.; Garrett, A.; Hinshaw, S.P.; Greenhill, L.L.; Glover, G.; Shafritz, K.M.; et al. ADHD- and medication-related brain activation effects in concordantly affected parent-child dyads with ADHD. J. Child Psychol. Psychiatry 2007, 48, 899–913. [Google Scholar] [CrossRef]
- Tirapu, J.; Muñoz, J.M.; Pelegrín, C. Funciones ejecutivas: Necesidad de una integración conceptual. Revista de Neurología 2002, 34, 673. [Google Scholar] [CrossRef]
- Lavigne, R.; Romero, J.F. Modelo Teórico Del Trastorno Por Déficit de Atención Con Hiperactividad I: Definición Operativa. Electron. J. Res. Educ. Psychol. 2010, 8, 1303–1338. [Google Scholar] [CrossRef]
- Bausela, E.; Tirapu, J.; Cordero, P. Déficits ejecutivos y trastornos del neurodesarrollo en la infancia y en la adolescencia. Revista de Neurología 2019, 69, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A.; Wasserstein, J. ADHD and The Nature of Self-Control. J. Cogn. Psychother. 2000, 14, 111–113. [Google Scholar] [CrossRef]
- Colomer, C.; Miranda, A.; Herdoiza, P.; Presentación, M.J. Funciones ejecutivas y características estresantes de niños con trastorno por déficit de atención/hiperactividad: Influencia en los resultados durante la adolescencia. Revista de Neurología 2012, 54, 117–126. [Google Scholar] [CrossRef]
- Humphreys, K.L.; Watts, E.L.; Dennis, E.L.; King, L.S.; Thompson, P.M.; Gotlib, I.H. Stressful Life Events, ADHD Symptoms, and Brain Structure in Early Adolescence. J. Abnorm. Child Psychol. 2018, 47, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Herreros, Ó.; Sánchez, F.; Ajoy, M.; Gracia, R. Evaluación de Niños y Adolescentes Con Trastorno Por Déficit de Atención Con Hiperactividad/Trastornos Hipercinéticos (TDAH). Rev. Psiquiatr. Infanto-Juv. 2002, 19, 199–214. [Google Scholar]
- Gotlib, I.H.; Joormann, J. Cognition and Depression: Current Status and Future Directions. Annu. Rev. Clin. Psychol. 2010, 6, 285–312. [Google Scholar] [CrossRef]
- Martínez, L.; Prada, E.; Satler, C.; Tavares, M.C.H.; Tomaz, C. Executive Dysfunctions: The Role in Attention Deficit Hyperactivity and Post-traumatic Stress Neuropsychiatric Disorders. Front. Psychol. 2016, 7, 1230. [Google Scholar] [CrossRef] [PubMed]
- Pechtel, P.; Pizzagalli, D.A. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacol. 2010, 214, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Hodgkins, P.; Setyawan, J.; Mitra, D.; Davis, K.; Quintero, J.; Fridman, M.; Shaw, M.; Harpin, V. Management of ADHD in children across Europe: Patient demographics, physician characteristics and treatment patterns. Eur. J. Nucl. Med. Mol. Imaging 2013, 172, 895–906. [Google Scholar] [CrossRef]
- Guerrero, F. El Lado Oscuro Del TDAH En La Vida Adulta; Ediciones Aljibe: Málaga, Spain, 2014. [Google Scholar]
- Sciberras, E.; Lycett, K.; Efron, D.; Mensah, F.; Gerner, B.; Hiscock, H. Anxiety in Children with Attention-Deficit/Hyperactivity Disorder. Pediatrics 2014, 133, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Mogg, K.; Salum, G.A.; Bradley, B.P.; Gadelha, A.; Pan, P.; Alvarenga, P.G.; Rohde, L.A.; Pine, D.S.; Manfro, G.G. Attention network functioning in children with anxiety disorders, attention-deficit/hyperactivity disorder and non-clinical anxiety. Psychol. Med. 2015, 45, 2633–2646. [Google Scholar] [CrossRef]
- Rothbart, M.K.; Sheese, B.E.; Rueda, M.R.; Posner, M.I. Developing Mechanisms of Self-Regulation in Early Life. Emot. Rev. 2011, 3, 207–213. [Google Scholar] [CrossRef]
- Eysenck, M.W.; Derakhshan, N.; Santos, R.; Calvo, M.G. Anxiety and cognitive performance: Attentional control theory. Emotion 2007, 7, 336–353. [Google Scholar] [CrossRef] [PubMed]
- Posner, M.I.; Rothbart, M.K. Research on Attention Networks as a Model for the Integration of Psychological Science. Annu. Rev. Psychol. 2007, 58, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, M.A. Attention-deficit/hyperactivity disorder (ADHD) symptoms, anxiety symptoms, and executive functioning in emerging adults. Psychol. Assess. 2016, 28, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.O.; Chilcoat, H.D.; Breslau, N. Trouble sleeping and anxiety/depression in childhood. Psychiatry Res. 2000, 94, 93–102. [Google Scholar] [CrossRef]
- Valdizán, J.R. Trastornos generalizados del desarrollo y sueño. Revista de Neurología 2005, 41, S135. [Google Scholar] [CrossRef]
- Cortese, S.; Faraone, S.V.; Konofal, E.; Lecendreux, M. Sleep in Children with Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Subjective and Objective Studies. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 894–908. [Google Scholar] [CrossRef] [PubMed]
- Mulas, F.; Rojas, M.; Gandía, R. Sueño En Los Trastornos Del Neurodesarrollo, Déficit de Atención e Hiperactividad y En El Espectro Autista. Med. B. Aires. 2019, 79, 33–36. [Google Scholar]
- Madrid, J.A. Los Trastornos Del Sueño En Niños Pueden Provocar Problemas de Memoria, Sobrepeso y Depresión. El País. 2020. Available online: https://elpais.com/elpais/2020/05/25/mamas_papas/1590428224_998413.html (accessed on 14 February 2021).
- National Child Traumatic Stress Network. Guía de Ayuda Para Padres y Cuidadores Para Ayudar a Las Familias a Enfrentar La Enfermedad Coronavirus 2019 (COVID-19). April 2020. Available online: https://www.nctsn.org/sites/default/files/resources/fact-sheet/parent_caregiver_guide_to_helping_families_cope_with_the_coronavirus_disease_2019-sp.pdf (accessed on 14 February 2021).
- Lavigne, R.; Costa, B.; Juárez-Ruíz de Mier, R.; Real, M.; Sánchez-Muñoz de León, M.; Navarro, I. Consequences of Covid-19 Confinement on Anxiety, Sleep and Executive Functions of Children and Adolescents in Spain. Front. Psychol. 2021, 12, 1–11. [Google Scholar]
- Daley, P. We Face a Pandemic of Mental Health Disorders. Those Who Do It Hardest Need Our Support. Guard. 24 March 2021. Available online: https://www.theguardian.com/commentisfree/2020/mar/25/we-face-a-pandemic-of-mental-health-disorders-those-who-do-it-hardest-need-our-support (accessed on 14 February 2021).
- Ezpeleta, D.; García-Azorín, D. Manual COVID-19 Para El Neurólogo General; Ediciones SEN: Madrid, Spain, 2020. [Google Scholar]
- Wright, A.; Salazar, A.; Mirica, M.; Volk, L.A.; Schiff, G.D. The Invisible Epidemic: Neglected Chronic Disease Management During COVID-19. J. Gen. Intern. Med. 2020, 35, 2816–2817. [Google Scholar] [CrossRef]
- Ato, M.; López-García, J.J.; Benavente, A. Un sistema de clasificación de los diseños de investigación en psicología. Anales de Psicología 2013, 29, 1038–1059. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Edwards, C.D.; Montuori, J.; Lushene, R. Manual for the State-Trait Inventory for Children; Mind Garden, Inc.: Menlo Park, CA, USA, 1973. [Google Scholar]
- Owens, J.A.; Dalzell, V. Use of the ‘BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: A pilot study. Sleep Med. 2005, 6, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Vélez, R.R.; Zamora, L.H.; Bautista, J.E.C.; Calderón, E.G.C. Confiabilidad y Validez Del Cuestionario de Trastornos de Sueño BEARS En Niños y Adolescentes Escolares de Bogotá, DC, Colombia: Estudio FUPRECOL. Retos Nuevas Tend. Educ. Física Deporte Recreación. 2018, 34, 89–93. [Google Scholar]
- Barkley, R.A. Barkley Deficits in Executive Functioning Scale—Children and Adolescents (BDEFS-CA); Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using SPSS:(And Sex and Drugs and Rock’n’Roll); Sage: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Cohen, J. The Effect Size Index: D. Statistical Power Analysis for the Behavioral Sciences 2; Lawrence Erlbaum, Associates, Inc.: London, UK, 1988. [Google Scholar]
- Hernández Lalinde, J.D.; Espinosa Castro, J.F.; Peñaloza Tarazona, M.E.; Fernández González, J.E.; Chacón Rangel, J.G.; Toloza Sierra, C.A.; Arenas Torrado, M.K.; Carrillo Sierra, S.M.; Bermúdez Pirela, V.J. Sobre El Uso Adecuado Del Coeficiente de Correlación de Pearson: Definición, Propiedades y Suposiciones. Archivos Venezolanos de Farmacología y Terapéutica 2018, 37, 587–595. [Google Scholar]
- Urzúa, A.; Vera-Villarroel, P.; Caqueo-Urízar, A.; Polanco-Carrasco, R. La Psicología en la prevención y manejo del COVID-19. Aportes desde la evidencia inicial. Terapia Psicológica 2020, 38, 103–118. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Chandler, J.L.; Randel, A.B.; Turner-McGrievy, G.M.; Moore, J.B.; Huberty, J.L.; Ward, D.S. Children’s Moderate to Vigorous Physical Activity Attending Summer Day Camps. Am. J. Prev. Med. 2017, 53, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Zhang, J.; Shuai, L.; Yu, H.; Wang, Z.; Qiu, M.; Lu, L.; Cao, X.; Xia, W.; Wang, Y.; Chen, R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102077. [Google Scholar] [CrossRef]
- Xie, X.; Xie, J. Parental phubbing accelerates depression in late childhood and adolescence: A two-path model. J. Adolesc. 2020, 78, 43–52. [Google Scholar] [CrossRef]
- Power, T.J.; Costigan, T.E.; Eiraldi, R.B.; Leff, S.S. Variations in Anxiety and Depression as a Function of ADHD Subtypes Defined by DSM-IV: Do Subtype Differences Exist or Not? J. Abnorm. Child Psychol 2004, 32, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Lee, J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health 2020, 4, 421. [Google Scholar] [CrossRef]
- González-Castro, P.; Rodríguez, C.; Cueli, M.; García, T.; Alvarez-García, D. State, trait anxiety and selective attention differences in Attention Deficit Hyperactivity Disorder (ADHD) subtypes. Int. J. Clin. Health Psychol. 2015, 15, 105–112. [Google Scholar] [CrossRef][Green Version]
- Sadeh, N.; Bredemeier, K. Individual differences at high perceptual load: The relation between trait anxiety and selective attention. Cogn. Emot. 2011, 25, 747–755. [Google Scholar] [CrossRef]
- Airaksinen, E.; Larsson, M.; Forsell, Y. Neuropsychological functions in anxiety disorders in population-based samples: Evidence of episodic memory dysfunction. J. Psychiatr. Res. 2005, 39, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, M.A.; Ollendick, T.H. Treatment of comorbid attention-deficit/hyperactivity disorder and anxiety in children: A multiple baseline design analysis. J. Consult. Clin. Psychol. 2012, 80, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Golberstein, E.; Wen, H.; Miller, B.F. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatr. 2020, 174, 819. [Google Scholar] [CrossRef]
- Hong, H.; Wang, Y.; Chung, H.-T.; Chen, C.-J. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr. Neonatol. 2020, 61, 131–132. [Google Scholar] [CrossRef]
- Martel, M.M.; Nigg, J.T.; Wong, M.M.; Fitzgerald, H.E.; Jester, J.M.; Puttler, L.I.; Glass, J.M.; Adams, K.M.; Zucker, R.A. Childhood and adolescent resiliency, regulation, and executive functioning in relation to adolescent problems and competence in a high-risk sample. Dev. Psychopathol. 2007, 19, 541–563. [Google Scholar] [CrossRef] [PubMed]
- Garon, N.; Moore, C.; Waschbusch, D.A. Decision Making in Children with ADHD Only, ADHD-Anxious/Depressed, and Control Children Using a Child Version of the Iowa Gambling Task. J. Atten. Disord. 2006, 9, 607–619. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898. [Google Scholar] [CrossRef] [PubMed]
- Jiao, W.Y.; Na Wang, L.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhou, Y.; Song, Y.; Ren, L.; Ng, C.H.; Xiang, Y.-T.; Tang, Y. Tackling the mental health burden of frontline healthcare staff in the COVID-19 pandemic: China’s experiences. Psychol. Med. 2020, 1–2. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Y.; Liu, Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020, 289, 113070. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Alvis, L.; Shook, N.; Oosterhoff, B. Adolescents’ Prosocial Experiences during the Covid-19 Pandemic: Associations with Mental Health and Community Attachments. PsyArXiv 2020, 1–25. Available online: https://psyarxiv.com/2s73n# (accessed on 14 February 2021). [CrossRef]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J. Psychiatry 2020, 51, 102092. [Google Scholar] [CrossRef] [PubMed]
- Bayés, R.; Ribes, E. Un Modelo Psicológico de Enfermedad: Su Aplicación al Caso Del SIDA. In J. A. Piña (Comp.), Psicología y Salud: Aportes Del Análisis de La Conducta; Unison: Hermosillo, México, 1992. [Google Scholar]

| Variable | Frequence (n) | Percentage (%) | |
|---|---|---|---|
| State anxiety * | Low | 21 | 18.1 |
| Average | 38 | 32.8 | |
| High | 57 | 49.1 | |
| Sleep | Low | 18 | 15.4 |
| Average | 41 | 35.0 | |
| High | 58 | 49.6 | |
| EF (BDEFS-CA) | Low | 10 | 8.5 |
| Average | 22 | 18.8 | |
| High | 85 | 72.6 |
| Instrument | Group | Mean Rank | Z | p | r |
|---|---|---|---|---|---|
| STAICs | ADHD | 130.36 | −2.91 | 0.004 | 0.19 |
| Non-ADHD | 104.64 | ||||
| BEARS | ADHD | 129.64 | 2.78 | 0.005 | 0.18 |
| Non-ADHD | 105.36 | ||||
| BDEFS-CA | ADHD | 153.54 | −8.15 | 0.001 | 0.53 |
| Non-ADHD | 81.46 |
| Total Mean (6–18 Years) | |||
|---|---|---|---|
| Non-Confinement Samples | Non-ADHD and Confinement Sample | ADHD and Confinement Sample | |
| State Anxiety (STAIC) | 31.2 | 32.60 | 36.10 |
| Sleep (BEARS) | 7.4 | 12.60 | 13.57 |
| EF (BDEFS-CA) | 33.2 | 70.30 | 80.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarro-Soria, I.; Real-Fernández, M.; Juárez-Ruiz de Mier, R.; Costa-López, B.; Sánchez, M.; Lavigne, R. Consequences of Confinement Due to COVID-19 in Spain on Anxiety, Sleep and Executive Functioning of Children and Adolescents with ADHD. Sustainability 2021, 13, 2487. https://doi.org/10.3390/su13052487
Navarro-Soria I, Real-Fernández M, Juárez-Ruiz de Mier R, Costa-López B, Sánchez M, Lavigne R. Consequences of Confinement Due to COVID-19 in Spain on Anxiety, Sleep and Executive Functioning of Children and Adolescents with ADHD. Sustainability. 2021; 13(5):2487. https://doi.org/10.3390/su13052487
Chicago/Turabian StyleNavarro-Soria, Ignasi, Marta Real-Fernández, Rocío Juárez-Ruiz de Mier, Borja Costa-López, Marta Sánchez, and Rocío Lavigne. 2021. "Consequences of Confinement Due to COVID-19 in Spain on Anxiety, Sleep and Executive Functioning of Children and Adolescents with ADHD" Sustainability 13, no. 5: 2487. https://doi.org/10.3390/su13052487
APA StyleNavarro-Soria, I., Real-Fernández, M., Juárez-Ruiz de Mier, R., Costa-López, B., Sánchez, M., & Lavigne, R. (2021). Consequences of Confinement Due to COVID-19 in Spain on Anxiety, Sleep and Executive Functioning of Children and Adolescents with ADHD. Sustainability, 13(5), 2487. https://doi.org/10.3390/su13052487







