Abstract
Background: Telemedicine has been incorporated into daily clinical practice. The purpose of this paper is to evaluate the economic impact of electronic consultation as a means of referring patients between Primary Care (PC) services and the referral Cardiology Service (CS) of a tertiary hospital, in particular, the cost of reduced air pollution. Methods: The direct and indirect costs associated with all the interconsultations between PC and a CS of a tertiary hospital were analyzed under a universal single act model versus a prior e-consultation model that selected patients who would later attend the single-act consultation. The cost of pollution from private motor vehicle travel by road has been analyzed with a Cobb–Douglas cost function. Results: The total cost per patient, including the costs associated with death, represented a saving in the model with e-consultation of 25.6%. The economic value for the reduction of contamination would be EUR 12.86 per patient. Conclusions: The introduction of e-consultation in the outpatient management of patients referred from PC to a CS, helps to reduce direct and indirect costs for the patient and the Health Care System. The cost of pollution associated with the trips explains the total cost to a greater extent, except for the first face-to-face consultation.
1. Introduction
In the last two decades, telemedicine has progressively been incorporated into daily clinical practice, with the parallel development of information technologies and computer communication [1]. In some healthcare settings, it has been observed that telemedicine systems can be effective in reducing total mortality, as in the clinical trial Telemonitoring in the Management of Heart Failure study [2], and cost-effective, when the assessment can be made through the information available in the electronic medical record [3,4]. Due to the prevalence of cardiovascular diseases and the demand for care they cause, the Cardiology (CS) services are one of the places where telemedicine can have a greater application and utility, especially in view of the need for a rapid response and adequate to the consultation generated from Primary Care (PC), where it is possible to resolve, in a high percentage of cases, the demand for care through information and complementary tests performed on the patient at another level of care [5].
Although there are already some experiences and models in the cardiovascular area, such as telematic follow-up and telephone control by nurses of patients with heart failure [5], there are no data available on global strategies in which all patients, regardless of their disease or reason for consultation, are evaluated electronically through an e-consultation by a hospital specialist to later carry out a face-to-face follow-up in those who require some face-to-face diagnostic or therapeutic intervention.
However, for this interconnection to function correctly, it is essential that both levels of care share a single electronic medical record interconnected through the network.
Linked to the experiences of economy is the possible savings associated with a reduction in trips by private car and with it a lower CO2 emission and the consequent savings in pollution costs. Air pollution is largely an avoidable health risk that affects everyone, although the most vulnerable—the sick, the elderly, children, and the poor—face disproportionate risks. Fortunately, reducing air pollution can result in quick and substantial health gains [6]. In HEATCO (Development of Harmonized European Approaches to Transport, Project Costing and Evaluation), the health cost of land transport emissions was calculated on the exposure-response functions established in the EU ExternE project. According to the study, in urban areas in Austria and the United Kingdom, each ton of PM2.5 emissions caused annual health costs of EUR 450,000, and in France and Germany, EUR 430,000.
Based on the WHO report [7], the avoidable mortality due to the reduction in air pollutant emissions in 2030 is 74,000 deaths, of which 45,100 (61%) of all deaths are avoided in the EU member states. This figure represents around 10% of the health burden attributed to particulate air pollution in 2010. In terms of life expectancy years gained, the total benefit in the entire European Region is 736,000 life years gained, from of which 55% is attributed to the EU28 countries.
Environmental economics tends to develop analyses based on neoclassical theory and studies that are framed in what is known as “Natural Resource Economics”. The main idea of this approach is that environmental problems arise from what are known as market failures. That is, situations in which the market does not function as an optimal allocator of resources. The environment in general, and many natural resources are linked to the concepts of externality, public good, and common pool resources. The presence of these market failures is generally associated with the absence of markets for these environmental goods and services. As Arrow argues, when there is no market, there is an information gap for individual decision making, which must be filled with some form of guesswork [8]. The problem is that these conjectures are hardly consistent with the reality associated with the phenomenon under study, and consequently, the decision making derived from them results in a non-optimal allocation of resources. In such situations, the task of environmental economics is to provide analyses and tools to correct such deviations. This type of study is mainly aimed at the direct or indirect valuation in monetary terms of the changes that occur in the tarry terms of the changes in the quality of an environmental good or service.
In this sense, two types of approaches are recognized for the economic analysis of environmental impacts. First, the standard cost-benefit criterion is considered, comparing the benefits and costs associated with a particular action to determine whether it is worthwhile or not to undertake the action. This approach is generally used when comparing different alternatives or projects by identifying the associated environmental impacts and assigning an economic value to the resulting outcomes. An example of this might be the analysis of different technologies and the improvements in community health that they can generate.
However, in some cases, it may not be feasible or desirable to undertake a traditional cost-benefit analysis. For example, there are some natural areas that are considered unique in the world, and for that reason, it is agreed that they should be conserved without considering the cost of doing so. On the other hand, there may be cases where there is a high level of uncertainty about the benefits that the environmental goods and services under study may provide, both now and in the future, which creates significant problems in assigning appropriate monetary values. Where the loss of these environmental services may be irreversible, it is desirable to opt for a strategy that minimizes the losses associated with environmental damage unless the social cost of doing so is excessively high. This perspective is known as “safe minimum standards”. In these cases, a variant of traditional cost-benefit analysis is applied, the cost-effectiveness approach, which consists of finding the most efficient way to achieve a particular environmental objective. It is important to note that this approach indicates which alternative is the most efficient but does not assess whether the expected benefits justify the costs to be incurred. The answer to the latter question rests on informed judgement and the common sense of the person conducting the study [9]. The great advantage of cost-effectiveness analysis is that it does not require the measurement of benefits. The fact that the aim is to achieve a given objective in the most efficient way means that the analyst can limit himself to computing the costs of each of the alternatives to be studied. Implicitly, it would be assumed that the benefits derived from the achievement of that alternative are very high [10].
On the other hand, transport models usually use time and cost as explanatory variables of user behavior and modal choice, time, and cost. However, the cost perceived only includes a part of the costs. Therefore, the market does not allocate demand in a socially efficient way. Efficiently, in social terms, the market does not allocate demand among the various modes of transport, nor in the various time slots, different time slots, etc. For this to be the case, all would have to be considered: those borne personally by users and those borne by administrations and external costs. The first two are considered, with various allocation procedures in Cost-Benefit Analyses.
However, the costs that are clearly not perceived are externalities. They are effects of the transport system, which do not have a market price and are suffered by third parties, without compensation or payment. The most frequently considered externalities are the following: air pollution, noise, greenhouse gas emissions, accidents, barrier effects emissions, accidents, barrier effects, impacts on the natural environment, and, partially, congestion.
Not taking into account the costs of externalities—i.e., not internalizing them—sends the wrong signals to the transport market, which behaves inefficiently and, according to Maibach [11], increases congestion, safety, and environmental problems. This is especially true in an increasingly liberalized transport market, as already pointed out by the European Union in its White Paper, “Fair payment of infrastructure use” [12]. The Transport White Paper European transport policy for 2010: time to decide [13] expresses the need to integrate external costs and infrastructure costs into the pricing system to have an efficient and competitive European market on the right basis.
Although there is a consensus on the need to consider costs, their measurement is not straightforward, as it requires specific methodologies and measurement techniques based on the economic valuation of externalities. This valuation will be conducted through the measurement of the utility of such a good. However, these utilities are goods that are difficult to value—for example, clean air or the absence of noise—because they do not have a market price. Moreover, the scope of the impact is very varied; noise, for example, only affects a small geographical area close to the transport route, while CO2 emissions affect the entire planet, and not only this generation but also future generations.
The objective of this work is to evaluate the economic impact of electronic consultation as a means of referring patients between PC services and the referral CS of a tertiary hospital.
2. Methods
2.1. Population
The Healthcare Area under study and belonging to the Galicia–North Portugal Euroregion provides healthcare coverage to 446,603 citizens, 352,331 of which are over 14 years of age. This population is characterized by its great geographic dispersion and aging, being distributed in 46 population centers.
The number of citizens over 65 years of age is 107,812, which represents 24.2% of the population of the area. To provide assistance to the population over 14 years of age, the health area is endowed with 301 family doctor (FM) positions, who carry out their care activity in 56 health centers and 21 peripheral clinics, all of them functionally grouped into 25 Health Services and Primary Care (SAP).
For the present work, the patients referred from PC were selected, all of them registered in the computer system, with at least one consultation in the CS between 2010 and 2019, obtaining a final sample of 41,405 patients, and whose clinical and epidemiological characteristics have already been previously described [14].
2.2. Assistance Model in Access to Outpatient Cardiology Consultations
From 2008 to 2012, a “one-time” consultation model was implemented, according to which the visit to the cardiologist includes, on the same day, the performance of all those complementary tests that he considers necessary for the diagnosis of the patient. As of 2013 and up to the present, an electronic consultation or e-consultation model has been implemented from the PC to the CS, which consists of a telematic assessment, based on the information available in the electronic medical record of the patient, prior to the consultation of single act and that has been defined in previous articles [14].
2.3. Analysis
A cost analysis was carried out, through an analytical model in Microsoft Excel 2019, to calculate the costs generated after requesting a referral to the CS from the PC and the health results (clinical consequences). The results are expressed at three levels: (1) the costs generated for the patient, in terms of time and travel, (2) the benefits of the e-consultation program, calculated as saved costs for the National Health System (NHS) in terms of consultations and hospital admissions; and (3) costs to society, in terms of costs associated with death.
2.4. Costs and Definitions
The variables used for the analysis of healthcare activity and health outcomes of both models have been previously defined [14].
The expenses generated in medical consultations, as well as during hospital admissions are established as rates by Government Decree [15]. However, some costs need to be defined for a better understanding of the reader of our work:
- (1)
- The cost of the teleconsultation has not been defined by Government Decree. Following the results of the work by Moreno-Ramírez et al., a 40% reduction in the cost of a face-to-face consultation has been estimated [16].
- (2)
- The cost of the trip (which corresponds to the patient’s displacement to their health center (CS)) in the e-consultation has been calculated from the average distance between the parish without CS and the closest CS. In the territory Government Decree, the average has been set at 3.92 km [17], which is multiplied by EUR 0.19/km to calculate the cost of this distance [18].
- (3)
- The cost of the time invested in the trip to the hospital to attend the face-to-face consultation was estimated from the weighted mean time for our health area (39,084 min). To this time is added the average duration of the consultation (20 min) and the time to park and arrive at the consultation area (another 20 min), so the total time will be 79,084 min.
- For the working-age population, the cost was estimated taking into account the average gross income of the worker (EUR 18,768.21/year) and the unemployment rate (7.9%) in our health area as of 31 December 2019 [19] (Health area of Santiago encompasses 46 municipalities, and according to data from the Public Employment Service, dependent on the Ministry of Labour of the Spanish Government and weighted by the population of the municipalities, the average unemployment rate in the Santiago Health Area is 7.9%). On the other hand, leisure time was valued at 47% of the cost of working hours [20].
- For the retired population, the cost was estimated taking into account the percentage of people aged 65 or over who perform volunteer work according to the CIS-IMSERSO study (2.3%) [21]; those dedicated to caring for grandchildren according to the study “Living Conditions of the Elderly” carried out by the Sociological Research Center (22.6%) [22] and the Public Indicator of Multiple Effects Income (IPREM).
- (4)
- The cost of time on the waiting list has been analyzed based on the study by Propper et al. [23], valued at GBP 38.89 (in 1987) for each month.
Transferred to 2019 in EUR, they correspond to EUR 101.52. Therefore, the imputed cost in patients who stayed less than a month was EUR 0.
- (5)
- The cost of the death of the active population was estimated based on the expected benefits in terms of decreased incidence, mortality, and potential years of lost working life, estimating the economic value derived from lost wages for the average gross income per worker of the area (EUR 18,768.21/year).
- (6)
- The cost of the death of the retired population was estimated based on the expected benefits in terms of decreased incidence, mortality and potential years of life lost (in relation to the average age of life expectancy) estimating the economic value, derived of the contribution of those over 65 to volunteer work and care for grandchildren (IPREM: EUR 7519.59/year).
- (7)
- The cost of pollution from private motor vehicle travel by road. A significant part of transport studies focusses on carbon dioxide (CO2) emissions, and, in turn, CO2 emissions are directly related to fuel consumption and fuel efficiency [24,25]. Chester and Horvath estimate that the total emissions of a passenger car are 0.36 kg CO2e per passenger and mile [26], and the cost of CO2 emission is EUR 0.0770235 per gram [27].
Depending on the type of externalities and the information or budget available for their quantification, indirect methods or direct methods will be used. The former tries to establish a cause–effect relationship, e.g., valuing noise by the cost of avoiding it: noise protection screens. Direct methods are based on users’ choices. Hedonic pricing, for example, yields price differences for the same good depending on environmental conditions: two houses of the same type may have a different price depending on their proximity to a noisy road. Other times, it is necessary to resort to contingent valuation or willingness to pay/accept a compensatory payment to improve the environmental conditions of a good. This valuation also frequently uses stated preference surveys.
According to the European CAPRI project [28] external costs due to congestion, space shortages, and accidents should be assessed using methods based on the acceptance of payment. In contrast, the cost of air pollution should be determined by a total impact method, incorporating emission, dispersion, and cause–effect (dose–response), with an assessment of the final health impact.
According to economic theory, the economic optimum occurs when prices correspond to marginal costs. Therefore, the European Union’s White Paper on Transport [13] proposes pricing all modes at marginal costs, including infrastructure costs and externalities. Many studies have therefore been carried out to determine the marginal costs of numerous case studies. The difficulty of this approach lies in the problems of extrapolating the values thus determined, as the marginal costs correspond to each specific situation. Moreover, it is not operational to set variable prices—with the level of congestion, according to the area, etc.—as this would hinder market transparency. This approach is the so-called bottom-up approach. From a multitude of case studies, valid values can be proposed for several contexts, duly typified.
The other approach, which is called top-down, is to calculate average costs. This is performed by calculating the total costs for a given geographical area for each of the externalities (accidents, pollution, etc.) and then dividing them by the transport units (vehicles or passenger-km). The costs determined in this way do not reflect the theoretical economic optimum, but they have less variability and can be allocated to larger geographical areas.
Perhaps the most complete study, and with a more homogeneous methodology, has been carried out by the team formed by the Swiss consultancy INFRAS and the IWW Institute of the University of Karlsruhe [29]. This group has calculated the average costs of the various means of transport for all the countries of the European Union for the year 2000.
The Cobb–Douglas function that was estimated by Charles W. Cobb and Paul H. Douglas [30], although it was already anticipated by Knut Wicksell (1901, 1923) and, according to some authors, by J.H. von Thünen [31], presents the following form:
where TC, X1, X2, and Xn represent the Total Cost and the different costs and α, β1, β2, and βn are constants.
The model is linearized by calculating the natural logarithms on both sides of the equality as follows:
For the four models (1. Teleconsultation and resolution in said Teleconsultation; 2. Teleconsultation followed by a first face-to-face consultation and resolution in that first consultation; 3. Teleconsultation followed by a first face-to-face consultation and successive face-to-face consultations; 4. No Teleconsultation, there is a first face-to-face consultation that can solve the problem or require successive face-to-face consultations), the following equations are proposed:
ln TC = β0 + β1 ln Cost of Consultation Time + β2 ln Cost of Pollution External Consultations + β3 ln Cost of Cardiology Admission + β4 ln Cost of Exitus + β5 Cost of Exitus with IPREM
ln TC = β0 + β1 ln Cost of Time for Teleconsultation + β2 ln Cost of Travel for Teleconsultation + β3 ln Cost of Time for Teleconsultation + β4 ln Cost of Pollution of Teleconsultation + β5 ln Cost of Time for 1st Outpatient Consultation + β6 ln Cost of Time for 2nd Outpatient Consultation + β7 Cost of 2nd Outpatient + β8 Contamination Cost 1st Outpatient Consultation + β9 Contamination Cost 2nd Outpatient Consultation + β10 ln Cardiology Admission Cost + β11 ln Exitus Cost + β12 Exitus Cost with IPREM
ln TC = β0 + β1 ln Cost Time Teleconsultation + β0 ln Cost Contamination Teleconsultation + β3 ln Cost 1st External Consultation + β4 ln Cost 2nd External Consultation + β5 ln Cost Time 1st External Consultation + β6 ln Cost Time 2nd External Consultation + β7 Cost Contamination 1st Outpatient Consultation + β8 Contamination Cost 2nd Outpatient Consultation + β9 ln Cardiology Admission Cost + β11 ln Exitus Cost + β11 Exitus Cost with IPREM
ln TC = β0 + β1 ln Cost of Time for Outpatient Consultation + β2 ln Cost of Travel 2nd Outpatient Consultation + β3 ln Cost of 1st Outpatient Consultation + β4 ln Cost of 2nd Outpatient Consultation + β5 ln Cost of Time for 2nd Outpatient Consultation + β6 Cost of Contamination of 2nd Outpatient Consultation + β7 ln Cardiology Admission Cost + β8 ln Exitus Cost + β9 Exitus Cost with IPREM
Each one of the Beta coefficients of the previous function represents the partial elasticities of each variable, showing the weight of each variable in the Total Cost and allows evaluating the possible existence of economies of scale (EE). The economies of scale are calculated by adding the partial derivatives of the cost function:
EE < 1 presence of economies of scale;
EE = 1 constant returns to scale;
EE > 1 presence of diseconomies of scale.
3. Results
The 41,405 patients referred from PC to CS between 2010 and 2019 were included for the analysis. The mean age (SD) was 63.2 ± 18.5 years and 50% were women.
Between 2010 and 2012, 12,182 (29.4%) patients were referred to the SC, all assessed in person in a single-act consultation. Between 2013 and 2019, 29,223 (70.6%) patients were referred for a telematic assessment through an e-consultation through the integrated electronic medical record (HCEI). After this assessment, the cardiologist could resolve the request without the need to see the patient in person, by issuing a written response through the electronic medical record to the PC doctor (n = 6240, 15.1%), or he would make an appointment with the patient in person in a single-act consultation. In the single act consultation, after performing all the diagnostic tests on the same day, the patient could be discharged (n = 8906, 21.5%) or continue their care in any of the specific consultations of the CS (n = 14,077, 34%).
Table 1 shows the costs corresponding to each of the healthcare activities carried out, the time spent by the patient attending the consultation and the costs generated by admissions for cardiovascular causes and mortality.

Table 1.
Unit costs used for analysis.
If we take into account these defined costs, the e-consultation represents a saving of EUR 110.23 compared to the face-to-face consultation, for each medical act, which represents 48.9% in the cost reduction (Table 2). Moreover, 96.3% of this reduction is attributable to the cost associated with moving the patient.

Table 2.
Differences in unit costs between e-consultation and face-to-face consultation.
Table 3 shows the analysis of costs associated with medical acts (e-consultation, face-to-face consultation, and hospital admissions the first year after requesting the interconsultation) for each comparison model. The cost of the e-consultation act is between EUR 110.98, for retired patients, and EUR 111.52, for patients of working age. The average cost of the first face-to-face consultation was lower in the e-consultation model for both the active population (EUR 153.54 vs. EUR 600.03) and the retired population (EUR 228.89 vs. EUR 682.76). The mean time spent on the waiting list was less than 7 days in the e-consultation patients [8], so the cost was higher in the single act model patients (EUR 157.48). The cost associated with hospital admissions was lower in the e-consultation model, both in the active population (EUR 72.70 vs. EUR 190.85) and the retired (EUR 460.63 vs. EUR 1130.71).

Table 3.
Cost of care provided in outpatient consultations, hospital admissions and on the waiting list.
Table 4 shows the results of the indirect cost analysis of the interconsultation. The cost of travel was lower in the e-consultation model, both in the first consultation (EUR 4.50 vs. EUR 19.37, in assets, and EUR 7.03 vs. EUR 23.05, in retired people) and in the successive (EUR 4.69 vs. EUR 11.09, in assets, and EUR 6.14 vs. EUR 11.32, in retirees). Similarly, the costs associated with the time allocated by the patient to attend consultations were lower for the e-consultation model, both in the first consultation (EUR 10.68 vs. EUR 43, in assets, and EUR 1.68 vs. 5, EUR 20, in retirees) as in the successive ones (EUR 9.67 vs. EUR 20, in assets, and EUR 1.24 vs. EUR 2.07).

Table 4.
Travel costs and time spent to visit the clinic (Primary Care or Hospital Care).
In the same way, the costs associated with pollution by CO2 emissions as a consequence of transport, (EUR 0.302 in assets and retirees vs. EUR 7.85 in assets and EUR 9.34 in retirees for first consultations and EUR 4.43 in assets and EUR 4.59 in retirees for subsequent consultations). With a total saving for the number of patients contemplated in this study, by reducing the levels of CO2 contamination of EUR 102,638.56 (Table 5).

Table 5.
Pollution cost per trip.
Finally, the costs associated with death were lower for the e-consultation model in the active population (EUR 109,490.61 vs. EUR 171,640.19) but not in the retired population (EUR 21,968.74 vs. EUR 10,404.63) (Table 6).

Table 6.
Costs associated with the death of patients.
The final balance of the costs associated with both models averaged per patient shows us that the costs are lower in the e-consultation model, even in deaths globally, Figure 1. The total cost per patient, without taking into account deaths, shows a 59.6% decrease in e-consultation with respect to the previous classical model; if the indirect social costs due to the death of the patient are taken into account, this saving percentage drops to 25.6%.
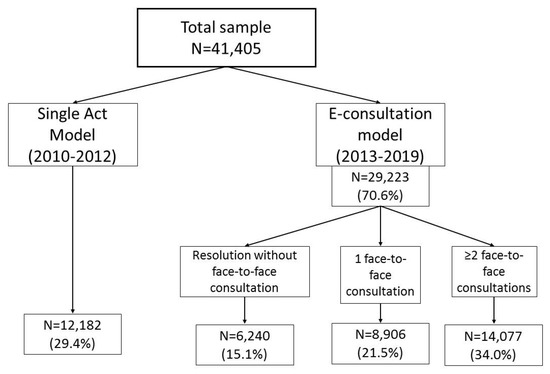
Figure 1.
Final balance of associated costs to medical care models.
Table 7 shows the results of the Cobb–Douglas function for the four models (A, B, C, and D). In the first model, the constant absorbs the value of the teleconsultation costs, except the cost of time of the same as they are constant variables. In this model, the variables with the highest level of explanation of the total cost are deaths (with and without IPREM). The cost of contamination for the first face-to-face consultation is not significant. With respect to the second model, the variable that explains the total cost to a greater extent is the cost of pollution associated with the trip for the first face-to-face consultation, followed by the cost of pollution associated with the trip for subsequent consultations, although this has a negative and significant sign, in addition to the cost of time for subsequent consultations and the cost of travel for the Teleconsultation.

Table 7.
Cobb–Douglas cost function analysis type of patient.
For the third model, the main explanatory variables of the total cost are the cost of successive consultations, the cost of contamination of the trips associated with both the Teleconsultation and the first and subsequent consultations, and the cost associated with Exitus. The fourth model presents as variables with the greatest impact on the total cost, the cost of the first consultation, and the cost of pollution associated with the trips of subsequent consultations.
Based on the results of the Durbin Watson test, there are no autocorrelation problems for any of the models. Likewise, the hypothesis of the non-existence of collinearity is accepted.
Regarding the existence or not of Economies of Scale (EE), economies of scale are observed in models 1 (0.413), 3 (0.601), and 4 (0.521), and diseconomies of scale are observed in model 2 (2.344).
4. Discussion
The results observed in the present analysis confirm that the introduction of an electronic consultation as a first assessment, prior to the single-act consultation, of patients referred from PC to a CS is useful in reducing the social and healthcare costs associated with face-to-face care in a CS. This reduction is obtained in the three cost levels analyzed: healthcare, time, and patient travel and in those linked to health consequences, such as admissions and deaths.
To our knowledge, this is the first time that an analysis of the social and healthcare costs associated with the implementation of a management model for ambulatory care for referrals to a CS has been carried out that incorporates a telematic consultation (e-consultation). We believe that our results may have implications for the implementation of outpatient care management programs as the introduction of e-consultation is associated with improvements in health outcomes [14] and a reduction in healthcare costs.
In the present study, the difference between the cost of the e-consultation and that of the face-to-face consultation, both understood as the cost of the medical consultation act (which includes the amortization of technological equipment, as well as the cost of human resources and the allocation of general costs) is 48.9% lower in e-consultation. If the costs of hospitalization admissions are incorporated into the study, the difference in cost is 61.9% lower for e-consultation per working-age patient and 59.3% per retired patient. If the cost associated with the loss of productivity due to mortality is considered, the savings for an average patient from the e-consultation with respect to the face-to-face consultation are 59.6% for patients of working age and 25% and 6% for retirees.
Compared with the results of the present study, Mold et al. [32] in a systematic review show that several studies have found specific advantages when using electronic consultations that include time and cost savings, including lost wages [33]. In particular, a study evaluating joint teleconsultation between general practitioners (GPs), specialists, and patients, found cost savings for patients between EUR 1000.06 and EUR 2700.50 due to the fact that patients avoid traveling to services of urgency, to the clinical visits in the hospital, and to the realization of diagnostic tests; therefore, our results would be in the lower level of the band of the comparative study [34].
For Abbott et al. in their study on specialized care consultations, the cost of the face-to-face consultation was USD 228 per consultation and person versus USD 120 for the e-consultation, which represents a reduction of 47.4%, similar to our study, although they only estimated travel expenses for the face-to-face consultation (USD 112) and no travel expenses for the e-consultation, an aspect that we have included in our work since the patient goes to his Primary Care center to receive the result of the telematic consultation [35].
In a comparison of 4635 virtual visits and a control group of 55,310 face-to-face visits in PC, Gordon et al. found that the total costs per episode were USD 162 more expensive in face-to-face consultations [36]. In addition, the adjusted mean cost of the initial visit was lower for the virtual group (USD 49) than for the face-to-face (USD 109). The authors add that the follow-up medical expenses of the virtual group were similar to or lower than the costs of face-to-face consultations.
It is interesting to note that Mendell et al. carried out a qualitative analysis, without addressing the possible cost savings, in the virtual cardiac rehabilitation consultations and confirmed that they managed to address the same aspects as in the face-to-face consultations regarding issues related to exercise, diet, and positive behavior changes to limit risk factors [37]; López Seguí et al. agree in their study on the implementation of telematic consultations, and they conclude that teleconsultation meets the objective of solving consultations without the need for a face-to-face medical act, saving the differential time between the face-to-face visit and the virtual [38].
Corporate Social Responsibility (CSR) is a new form of business management that goes beyond social actions: It involves an ethic of being and doing linked to transparency in business practices, communication with stakeholders (customers, professionals, citizens), as well as contributing to improving the internal functioning of organizations in aspects related to labor relations, gender equality, reconciliation of personal, family and work life, and occupational risk prevention.
We can understand the hospital as an organization where environmental, economic, and social dimensions are present. From the health point of view, its social role is indisputable, almost exclusive, since it provides complete medical healthcare to the population, and its external services radiate into the family sphere. From the economic perspective, it behaves as a mega-company that offers products and services, possesses physical and human capital, consumes and transforms materials, uses inputs and equipment, and incorporates increasingly complex technology. From an environmental perspective, hospitals interact with the environment through the flow of energy and materials and the generation of waste and emissions.
Hospital activity generates environmental, social and environmental, and social and cultural impacts that, without adequate proper management, create risks to human and environmental health, creating environmental health issues, creating inadequate conditions for personnel in their performance and productivity [39]. Human health interventions could be compromised if health determinants and the determinants of health linked to the ecosystem are not managed [40].
In that sense, the World Health Organization (WHO) is promoting an initiative called Health in the Green Economy, which focuses on reducing the carbon footprint of the health sector. The design of a programmatic framework capable of guiding actions to make hospitals sustainable, and which should aim to support their efforts to promote greater sustainability and environmental health, has been the motivation for the formulation of the Global Green and Healthy Hospitals Agenda and Network, which brings together hospitals from all over the world to exchange projects and experiences among hospitals that are working to improve environmental health. This programmatic framework is intended to be developed in parallel, among others already mentioned, with the Agenda of the Healthy Hospitals Initiative centered in the United States [41].
Over the last 20 years, telemedicine has been incorporated into clinical practice, showing that it can lower healthcare costs, drive up efficiency, and provide patients better access to healthcare services, thus reducing pollution and CO2. The present study evaluates the introduction of telemedicine in the Cardiology Service of a tertiary hospital advancing interesting results and conclusions.
Regarding the existence of savings as a consequence of less air pollution by CO2 due to the reduction of trips to attend face-to-face consultations, for Paquette and Lin, the total reduction in emissions of environmental pollutants from passenger cars, including carbon dioxide, carbon monoxide, nitric oxides, and volatile organic compounds. was 1632 kg, 42.867 g, 3160 g, and 4715 g, respectively, with a total of 194 gallons of gasoline saved, although, unlike our study, it does not incorporate an economic quantification of the cost or savings of reducing the level of air pollution [42].
Similarly, in the work of Vidal-Alaball et al., for a total of 12,322 referrals to telemedicine services in primary care centers, a total of 9034 face-to-face visits were avoided, which represented an average reduction of 3248.3 g of carbon dioxide, 4.05 g of carbon monoxide, 4.86 g of nitric oxide, and 3.2 g of sulfur dioxide, without indicating an economic value for the reduction of contamination as we have established in our study: EUR 12.86 per patient or, for the total of our sample, EUR 102,638.56 euros [43].
As in our study, Webb et al. found that telemedicine reduces the need for patient transport, the average length of stay in hospital and ICU, and the use of invasive therapies in their comparative study of children cared for by telemedicine and the comparison with the control group cared for in hospital [44].
Similarly, a study by Dullet et al. shows evidence of the potential efficiency of reduced travel and waiting time, cost-effectiveness, and positive environmental impact of telemedicine in outpatient consultations, which would support a long-term environmentally sustainable option to reduce the burden on families to receive quality healthcare [45]. In this regard, telemedicine consultations resulted in total air emissions savings of 1969 tons of CO2 for 19,246 consultations on 11,281 patients.
A study by Smith Rodriguez and de Titto revealed that the emission sources of greatest emissions correspond to energy consumption (electricity and natural gas), followed by emissions associated with staff travel [46].
This economic savings from teleconsultations have been observed in other specialties. Thus, Vidal et al. analyzed the economic impact of teledermatology in their Service and observed that this telematic activity represented a saving of practically 50% [47]. Along the same lines, Jones et al. observed that in a telematic urinary incontinence consultation, costs were also reduced by half (GBP 31.75 vs. GBP 72.17), mainly due to the duration of the consultation and associated labor costs [48].
However, not all authors find economically favorable results for the telematic consultation. Edwards et al. analyzed the impact of electronic consultation in PC, and observed that the average cost of an electronic consultation was higher than the face-to-face consultation (GBP 36.28 vs. GBP 33.00), which they attributed mainly to the time required for the family doctor to classify the electronic consultations and the relatively high proportion of these electronic consultations; in addition, the cost was increased to GBP 45.39 if the follow-up consultations were included in the next 30 days [49]. Based on these results, López Seguí concludes that the acceptance of teleconsultation is still very low, and it needs to increase its dissemination if it is to have a real impact on the demand resolved in PC, both in reducing the workload as of costs [50].
Obviously, our work is not without limitations, commented on in the original study [14]. If we focus on this economic sub-analysis, the most important limitations are the lack of knowledge of the real costs in our environment of some concepts, such as the cost of time on the waiting list, which has forced us to assume the published costs for some costs by other authors. In any case, we understand that these limitations do not detract from the validity of our work since the costs have been equally imputed to both comparison groups, so that, in any case, if there were other differences, they would further increase the associated cost reduction to the e-consultation, so our results would be confirmed.
5. Conclusions
In view of the observed results, we can conclude that the introduction of an e-consultation in the outpatient management of patients referred from PC to a CS, helps to reduce direct and indirect costs for the patient and the Health System compared to a classic model of face-to-face consultation for all patients referred from PC. This cost saving is observed regardless of the patient’s employment situation, both in direct costs of the health consultation and the health consequences, such as hospital admissions or death, as well as indirect costs related to the time and travel made by the patient to receive assistance to health centers.
Key points:
- What is known about the subject?
Outpatient care in Cardiology that aims to improve and integrate care usually focuses on single-act, face-to-face consultations. There are only experiences of telematic consultations in particular cases, such as heart failure or ischemic heart disease. An outpatient care management program that includes an e-consultation prior to the single act has been shown to reduce waiting times and improve health outcomes.
- What does it bring back?
We present the economic analysis that showed that the model that incorporates e-consultation as an assessment prior to the single act contributes a reduction in the direct and indirect costs involved in outpatient care in both retired patients and those who are of active age. This cost reduction is associated with a reduction in waiting times, a reduction in unnecessary travel, and a reduction in both income and mortality that we already observed in the general analysis of our work.
Author Contributions
J.R.G.-J. conceived the study and were in charge of overall direction and planning; F.R.S. participated in the design of the study, performed the analytic calculations and helped to draft the manuscript; D.R.A., P.M.R., M.P.R., S.C.S., B.Á.Á., R.A.B. and F.G.S. participated in the design of the study and helped to draft the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No additional data available.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bhavnani, S.; Narula, J.; Sengupta, P.P. Mobile technology and the digitization of healthcare. Eur. Heart J. 2016, 37, 1428–1438. [Google Scholar] [CrossRef]
- Dendale, P.; De Keulenaer, G.; Troisfontaines, P.; Weytjens, C.; Mullens, W.; Elegeert, I.; Ector, B.; Houbrechts, M.; Willekens, K.; Hansen, D. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur. J. Heart Fail. 2012, 14, 333–340. [Google Scholar] [CrossRef]
- Snoswell, C.; Finnane, A.; Janda, M.; Soyer, H.P.; Whitty, J.A. Cost-effectiveness of Store-and-Forward Teledermatology. JAMA Dermatol. 2016, 152, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Lee, S. Telemedicine Cost–Effectiveness for Diabetes Management: A Systematic Review. Diabetes Technol. Ther. 2018, 20, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Gu, X.; Xu, C. Effectiveness of telemedicine systems for adults with heart failure: a meta-analysis of randomized controlled trials. Heart Fail. Rev. 2020, 25, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Schraufnagel, D.E.; Balmes, J.R.; De Matteis, S.; Hoffman, B.; Kim, W.J.; Perez-Padilla, R.; Rice, M.; Sood, A.; Vanker, A.; Wuebbles, D.J.; et al. Health Benefits of Air Pollution Reduction. Ann. Am. Thorac. Soc. 2019, 16, 1478–1487. [Google Scholar] [CrossRef]
- WHO. Achieving Health Benefits from Carbon Reductions; Manual for CaRBonH calculation tool; WHO Regional Office for Europe: Copenhagen, Denmark, 2018. [Google Scholar]
- Arrow, K. Rationality of Self and Others in an Economic System. In Rational Choice. The Contrast between Economics and Psychology; Hogarth, R.M., Reder, M.W., Eds.; University of Chicago Press: Chicago, IL, USA, 1986. [Google Scholar]
- World Bank. How Much Is an Ecosystem Worth? Assessing the Economic Value of Conservation; Working Paper No. 30893; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2004. [Google Scholar]
- Azqueta Oyarzún, D. Gestión y Valoración de Proyectos de Recursos Naturales, Dirección de Proyectos y Programación de Inversiones; Instituto Latinoamericano y del Caribe de Planificación Económica y Social–ILPES, CEPAL: Santiago de Chile, Chile, 1994. [Google Scholar]
- Banfi, S.; Doll, C.; Maibach, M.; Rothengatter, W.; Schenkel, P.; Sieber, N.; Zuber, J.E. External Costs of Transport: Accident, Environmental and Congestion Costs of Transport in Western Europe; INFRAS-IWW, UIC: Zurich, Switzerland, 2000. [Google Scholar]
- UE. White Book on Fair Payment of Infrastructure Use; European Commission: Luxembourg, 1998. [Google Scholar]
- UE. White Paper European Transport Policy for 2010: Time to Decide; European Commission: Luxembourg, 2001. [Google Scholar]
- Rey-Aldana, D.; Cinza-Sanjurjo, S.; Portela-Romero, M.; López-Barreiro, J.L.; Garcia-Castelo, A.; Pazos-Mareque, J.M.; Mazon-Ramos, P.; Gonzalez-Juanatey, J.R. Universal electronic consultation (e-consultation) program of a cardiology service. Long-term results. Rev. Esp. Cardiol. 2020. [Google Scholar] [CrossRef]
- Tarifas de los Servicios Sanitarios en los Centros Dependientes del Servicio Gallego de Salud. DOG nº 96 del Miércoles, 21 de Mayo de 2014. Available online: https://www.xunta.gal/dog/Publicados/2014/20140521/AnuncioC3K1-140514-0001_es.html (accessed on 10 September 2019).
- Moreno-Ramírez, D.; Ferrandiz, L.; Ruiz-De-Casas, A.; Nieto-Garcia, A.; Moreno-Alvarez, P.; Galdeano, R.; Camacho, F.M. Economic evaluation of a store-and-forward teledermatology system for skin cancer patients. J. Telemed. Telecare 2009, 15, 40–45. [Google Scholar] [CrossRef]
- BOE núm. 266 del 4 de Noviembre de 2009, en el que se Regulan las Prestaciones por Desplazamiento. Available online: https://www.boe.es/boe/dias/2009/11/04/pdfs/BOE-A-2009-17495.pdf (accessed on 11 September 2019).
- Presentación para el Workshop sobre Financiación Autonómica. 2018. Available online: http://documentos.fedea.net/pubs/fpp/2018/07/FPP2018-07.pdf (accessed on 8 October 2019).
- Robusté, F. Campos Cacheda, J.M. Els comptes del Transport de Viatgers a la Regió Metropolitana de Barcelona; Autoritat del Transport Metropolità: Barcelona, Spain, 2000. [Google Scholar]
- Cabañés Argudo, M.L. Implicaciones renta-trabajo-ocio en el contexto norte-sur. Cuadernos Economía 2002, 25, 185–204. [Google Scholar]
- CIS-IMSERSO. Encuesta Sobre Personas Mayores. 2010. Available online: https://www.imserso.es/imserso_01/espaciomayores/esprec/enc_ppmm/index.htm (accessed on 2 September 2021).
- Centro de Investigaciones Sociológicas. Estudio “Condiciones de Vida de las Personas Mayores”. Available online: http://www.cis.es/cis/opencm/ES/1_encuestas/estudios/ver.jsp?estudio=7740&cuestionario=8954&muestra=14085 (accessed on 2 September 2021).
- Propper, C. Agency and incentives in the NHS internal market. Soc. Sci. Med. 1995, 40, 1683–1690. [Google Scholar] [CrossRef]
- Čokorilo, O.; Ivković, I.; Kaplanović, S. Prediction of Exhaust Emission Costs in Air and Road Transportation. Sustainability 2019, 11, 4688. [Google Scholar] [CrossRef]
- Ivković, I.S.; Kaplanović, S.M.; Milovanović, B.M. Influence of Road and Trac Conditions on Fuel Consumption and Fuel Cost for Different Bus Technologies. Therm. Sci. 2017, 21, 693–706. [Google Scholar] [CrossRef]
- Mikhail Chester and Arpad Horvath. Environmental Life-Cycle Assessment of Passenger Transportation: Detailed Methodology for Energy, Greenhouse Gas and Criteria Pollutant Inventories of Automobiles, Buses, Light Rail, Heavy Rail and Air, UC Berkeley Center for Future Urban Transport. 2008. Available online: http://repositories.cdlib.org/its/future_urban_transport/vwp-2008-2 (accessed on 2 September 2021).
- Litman, T. Air Pollution Costs Spreadsheet. 2006. Available online: www.vtpi.org/airpollution.xls (accessed on 2 September 2021).
- CAPRI. Concerted Action on Transport Pricing Research Integration; Final Report; EU, RTD IV FP: Brussels, Belgium, 2001. [Google Scholar]
- Schereyer, C. External Cost of Transport; Update Study; INFRAS-IWW, UIC: Zurich, Switzerland; Karlsruhe, Germany, 2004. [Google Scholar]
- Cobb, C.W.; Douglas, P.H. A Theory of Production. Am. Econ. Rev. 1928, 18, 139–165. [Google Scholar]
- Von Thünen, J.H. The Isolated State; Pergamon: London, UK, 1863. [Google Scholar]
- Mold, F.; Hendy, J.; Lai, Y.-L.; De Lusignan, S. Electronic Consultation in Primary Care Between Providers and Patients: Systematic Review. JMIR Med. Inform. 2019, 7, e13042. [Google Scholar] [CrossRef] [PubMed]
- Sevean, P.; Dampier, S.; Spadoni, M.; Strickland, S.; Pilatzke, S. Patients and families experiences with video telehealth in rural/remote communities in Northern Canada. J. Clin. Nurs. 2009, 18, 2573–2579. [Google Scholar] [CrossRef] [PubMed]
- Zanaboni, P.; Scalvini, S.; Bernocchi, P.; Borghi, G.; Tridico, C.; Masella, C. Teleconsultation service to improve healthcare in rural areas: Acceptance, organizational impact and appropriateness. BMC Health Serv. Res. 2009, 9, 238. [Google Scholar] [CrossRef]
- Abbott, D.E.; Macke, R.A.; Kurtz, J.; Safdar, N.; Greenberg, C.C.; Weber, S.M.; Voils, C.I.; Fisher, D.A.; Maloney, J.D. Financial and Temporal Advantages of Virtual Consultation in Veterans Requiring Specialty Care. Mil. Med. 2018, 183, e71–e76. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.S.; Adamson, W.C. Virtual Visits for Acute, Nonurgent Care: A Claims Analysis of Episode-Level Utilization. J. Med. Internet Res. 2017, 19, e35. [Google Scholar] [CrossRef]
- Mendell, J.; Bates, J.; Banner-Lukaris, D.; Horvat, D.; Kang, B.; Singer, J.; Ignaszewski, A.; Lear, S.A. What Do Patients Talk About? A Qualitative Analysis of Online Chat Sessions with Health Care Specialists During a “Virtual” Cardiac Rehabilitation Program. Telemed. e-Health 2019, 25, 71–78. [Google Scholar] [CrossRef]
- Seguí, F.L.; Walsh, S.; Solans, O.; Mas, C.A.; Ferraro, G.; García-Altés, A.; Cuyàs, F.G.; Carulla, L.S.; Castro, M.S.; Vidal-Alaball, J. Teleconsultation Between Patients and Health Care Professionals in the Catalan Primary Care Service: Message Annotation Analysis in a Retrospective Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e19149. [Google Scholar] [CrossRef]
- Pérez, D.; Diago, Y.; Corona, B.; Espinosa, R.; Gonzalez, J. Enfoque actual de la salud ambiental. Rev. Cubana Epidemiol. 2011, 49, 84–92. [Google Scholar]
- Prüss-Üstün, A.; Corvalán, C. Preventing Disease through Healthy Environments. Toward Sanestimate of the Environmental Burden of Disease; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Health and Environment. Managing the Linkages for Sustainable Development: A Toolkit for Decision-Makers; WHO/UNEP Health and Environment Linkages Initiative, Synthesis Report; WHO/UNEP: Geneva, Switzerland, 2008. [Google Scholar]
- Paquette, S.; Lin, J.C. Outpatient Telemedicine Program in Vascular Surgery Reduces Patient Travel Time, Cost, and Environmental Pollutant Emissions. Ann. Vasc. Surg. 2019, 59, 167–172. [Google Scholar] [CrossRef]
- Vidal-Alaball, J.; Franch-Parella, J.; Seguí, F.L.; Cuyàs, F.G.; Peña, J.M. Impact of a Telemedicine Program on the Reduction in the Emission of Atmospheric Pollutants and Journeys by Road. Int. J. Environ. Res. Public Health 2019, 16, 4366. [Google Scholar] [CrossRef] [PubMed]
- Webb, C.L.; Waugh, C.L.; Grigsby, J.; Busenbark, D.; Berdusis, K.; Sahn, D.J.; Sable, C.A. Impact of Telemedicine on Hospital Transport, Length of Stay, and Medical Outcomes in Infants with Suspected Heart Disease: A Multicenter Study. J. Am. Soc. Echocardiogr. 2013, 26, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- Dullet, N.W.; Geraghty, E.M.; Kaufman, T.; Kissee, J.L.; King, J.; Dharmar, M.; Smith, A.C.; Marcin, J.P. Impact of a University-Based Outpatient Telemedicine Program on Time Savings, Travel Costs, and Environmental Pollutants. Value Health 2017, 20, 542–546. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Smith, M.R.; de Titto, E. Hospitales sostenibles frente al cambio climático: huella de carbono de un hospital público de la ciudad de Buenos Aires. Rev. Argent Salud Pública 2018, 9, 7–13. [Google Scholar]
- Vidal-Alaball, J.; Garcia-Domingo, J.L.; Cuyàs, F.G.; Peña, J.M.; Flores-Mateo, G.; Rosanas, J.D.; Valmaña, G.S. A cost savings analysis of asynchronous teledermatology compared to face-to-face dermatology in Catalonia. BMC Health Serv. Res. 2018, 18, 650. [Google Scholar] [CrossRef]
- Jones, G.; Brennan, V.; Jacques, R.; Wood, H.; Dixon, S.; Radley, S. Evaluating the impact of a ‘virtual clinic’ on patient experience, personal and provider costs of care in urinary incontinence: A randomised controlled trial. PLoS ONE 2018, 13, e0189174. [Google Scholar] [CrossRef]
- Edwards, H.; Marques, E.; Hollingworth, W.; Horwood, J.; Farr, M.; Bernard, E.; Salisbury, C.; Northstone, K. Use of a primary care online consultation system, by whom, when and why: evaluation of a pilot observational study in 36 general practices in South West England. BMJ Open 2017, 7, e016901. [Google Scholar] [CrossRef]
- López Seguí, F.; Vidal-Alaball, J.; Sagarra Castro, M.; García-Altés, A.; García Cuyàs, F. General Practitioners’ Perceptions of Whether Teleconsultations Reduce the Number of Face-to-face Visits in the Catalan Public Primary Care System: Retrospective Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e14478. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
