Farmers’ Market Usage, Fruit and Vegetable Consumption, Meals at Home and Health–Evidence from Washington, DC
Abstract
:1. Introduction
2. Data and Methods
2.1. Data Collection
2.2. Variables and Measures
2.3. Empirical Strategy
3. Results
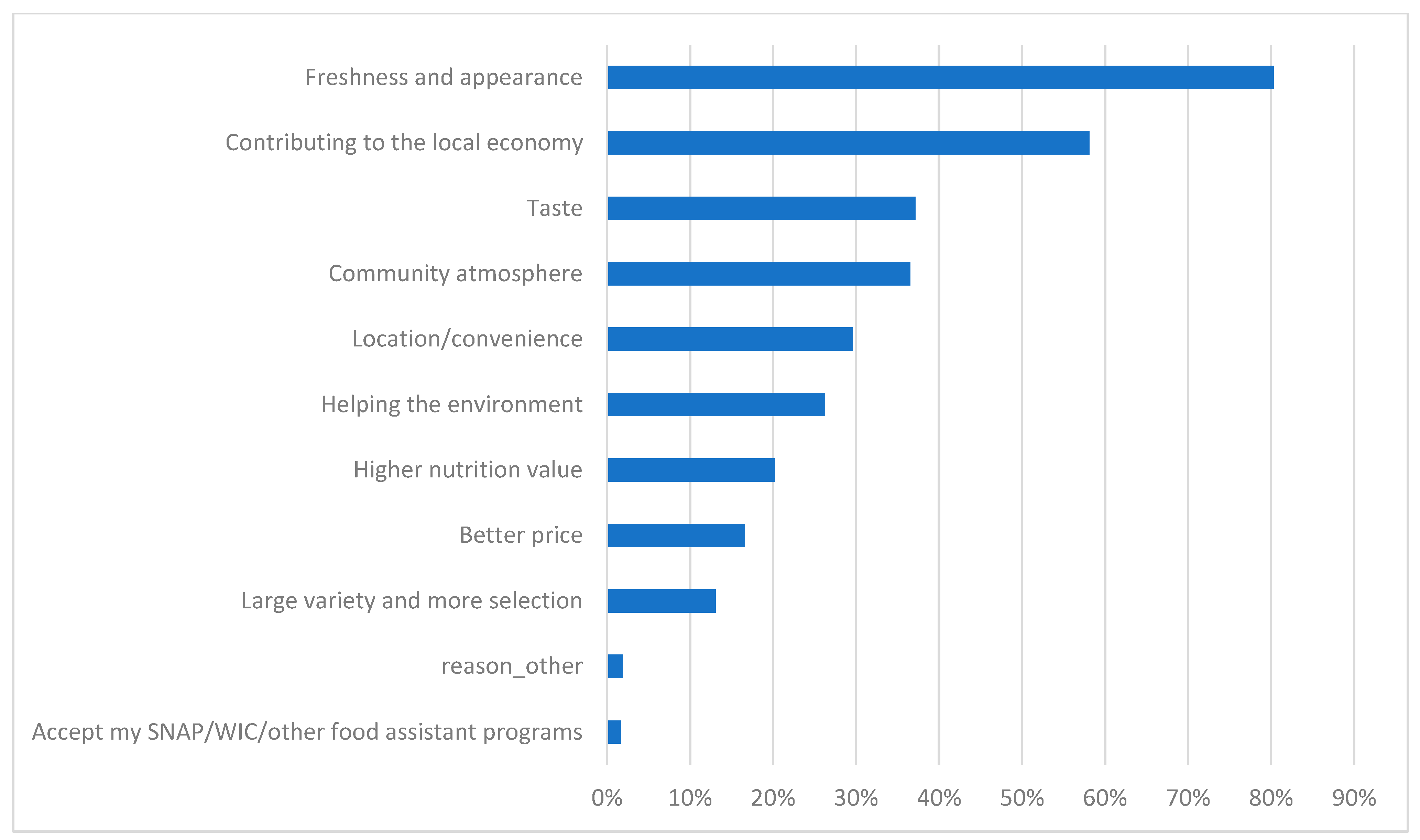
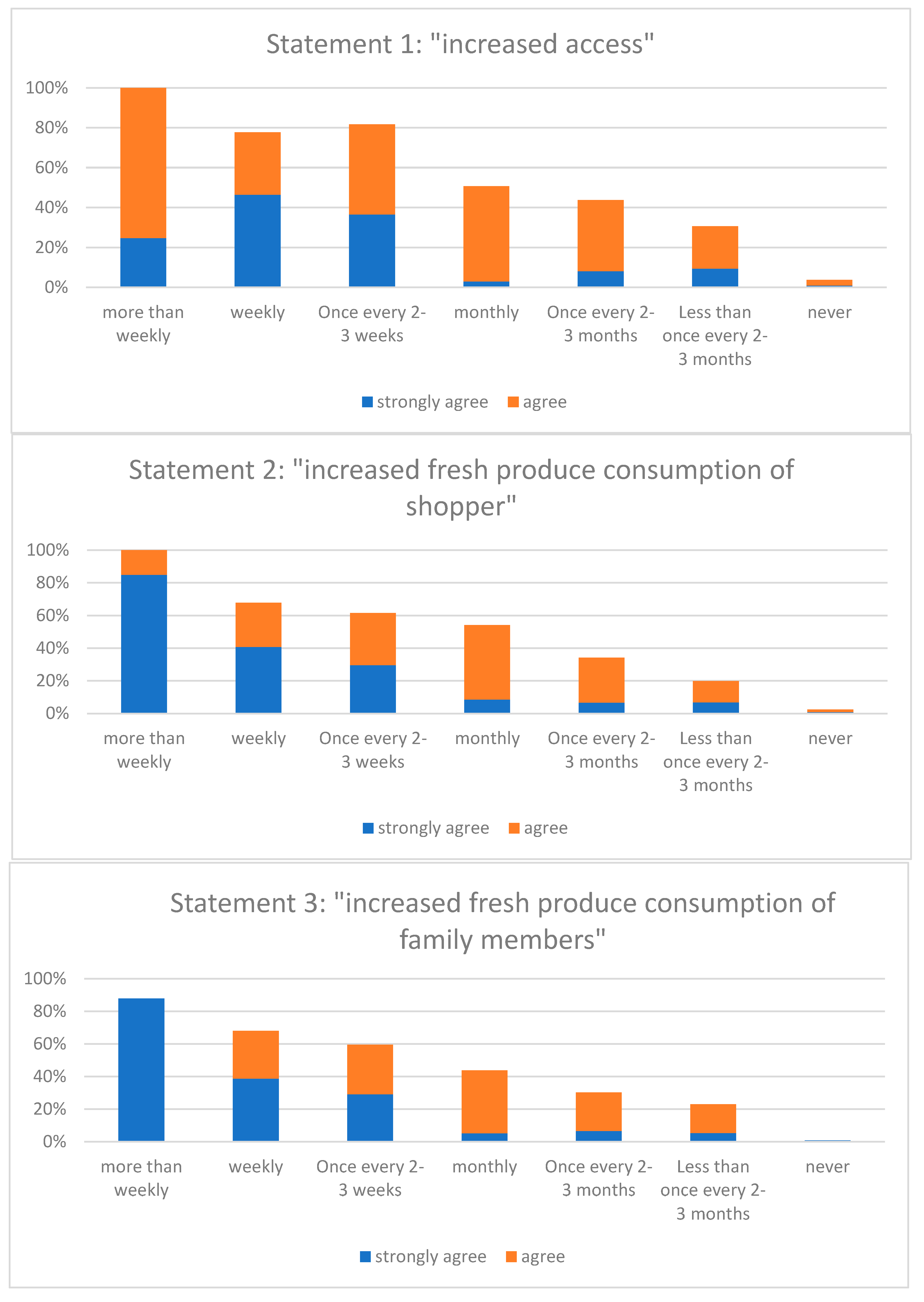
3.1. Link between Shopping at Farmers’ Market and Shopper’s Health Behaviors
- Statement 1: “It is easier for me to purchase fresh produce during the market season because of the farmers’ markets” (increased access)
- Statement 2: “I consume more fresh produce during the market season because of the farmers’ markets” (increased consumption of shoppers)
- Statement 3: “My family members consume more fresh produce during the market season because of the farmers’ markets” (increased consumption of family members).
3.2. Statistical Analyses Results
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Brown, C.; Miller, S. The Impacts of Local Markets: A Review of Research on Farmers Markets and Community Supported Agriculture (CSA). Am. J. Agric. Econ. 2008, 90, 1298–1302. [Google Scholar] [CrossRef]
- Suarez-Balcazar, Y.; Martinez, L.I.; Cox, G.; Jayraj, A. African Americans’ Views on Access to Healthy Foods: What a Farmers’ Market Provides. J. Ext. 2006, 44, 2. Available online: https://www.joe.org/joe/2006april/a2.php (accessed on 9 December 2020).
- Olsho, L.E.; Payne, G.H.; Walker, D.K.; Baronberg, S.; Jernigan, J.; Abrami, A. Impacts of a farmers’ market incentive programme on fruit and vegetable access, purchase and consumption. Public Health Nutr. 2015, 18, 2712–2721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- USDA ERS. America’s Eating Habits: Food Away from Home. 2019. Available online: https://www.ers.usda.gov/webdocs/publications/90228/eib-196.pdf (accessed on 12 July 2019).
- USDA AMS. Local Food Directories: National Farmers Market Directory. 2019. Available online: https://www.ams.usda.gov/local-food-directories/farmersmarkets (accessed on 20 June 2019).
- Elder, K.; Krystal, B. Farmers Markets in the Washington, D.C. Area. Washington Post. Available online: https://www.washingtonpost.com/graphics/food/dc-farmers-markets-interactive-map/ (accessed on 29 April 2021).
- Jaramillo, C. Farmers Markets May Be Your Safest Bet for Food Shopping Right Now. Available online: https://whyy.org/articles/farmers-markets-may-be-your-safest-bet-for-food-shopping-during-the-coronavirus-pandemic/ (accessed on 29 April 2021).
- Klisch, S.; Soule, K. Farmers Markets: Working with Community Partners to Provide Essential Services during COVID-19. J. Agric. Food Syst. Community Dev. 2020, 9, 175–179. [Google Scholar] [CrossRef]
- Schmidt, C.; Tian, Z.; Goetz, S.; Bartley, B.; Moyer, B.; Rocker, S. Farms with Direct to Consumer Sales in the Northeast Region and COVID-19: Some Early Challenges and Responses. Available online: https://aese.psu.edu/nercrd/publications/covid-19-issues-briefs/covid-19-and-farms-with-direct-to-consumer-sales (accessed on 9 June 2021).
- Ellen Macarthur Foundation. Cities and Circular Economy for Food. Available online: https://www.ellenmacarthurfoundation.org/publications/cities-and-circular-economy-for-food (accessed on 8 June 2021).
- O’Hara, S.; Toussaint, E.C. Food access in crisis: Food security and COVID-19. Ecol. Econ. 2021, 180, 106859. [Google Scholar] [CrossRef]
- Young, C.R.; Aquilante, J.L.; Solomon, S.; Colby, L.; Kawinzi, M.A.; Uy, N.; Mallya, G. Improving Fruit and Vegetable Consumption among Low-Income Customers at Farmers Markets: Philly Food Bucks, Philadelphia, Pennsylvania, 2011. Prev. Chronic Dis. 2013, 10, E166. [Google Scholar] [CrossRef] [Green Version]
- Jilcott, S.B.; Wade, S.; McGuirt, J.T.; Wu, Q.; Lazorick, S.; Moore, J.B. The association between the food environment and weight status among eastern North Carolina youth. Public Health Nutr. 2011, 14, 1610–1617. [Google Scholar] [CrossRef] [Green Version]
- Pitts, S.B.J.; Hinkley, J.; Wu, Q.; McGuirt, J.T.; Lyonnais, M.J.; Rafferty, A.P.; Whitt, O.R.; Winterbauer, N.; Phillips, L. A possible dose–response association between distance to farmers’ markets and roadside produce stands, frequency of shopping, fruit and vegetable consumption, and body mass index among customers in the Southern United States. BMC Public Health 2017, 17, 65. [Google Scholar] [CrossRef] [Green Version]
- Leung, C.W.; Laraia, B.A.; Kelly, M.; Nickleach, D.; Adler, N.E.; Kushi, L.; Yen, I.H. The Influence of Neighborhood Food Stores on Change in Young Girls’ Body Mass Index. Am. J. Prev. Med. 2011, 41, 43–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allcott, H.; Diamond, R.; Dubb, J.-P. The Geography of Poverty and Nutrition: Food Deserts and Food Choices across the United States; SSRN: Rochester, NY, USA, 2018. [Google Scholar] [CrossRef] [Green Version]
- Foltz, J.L.; May, A.L.; Belay, B.; Nihiser, A.J.; Dooyema, C.A.; Blanck, H.M. Population-Level Intervention Strategies and Examples for Obesity Prevention in Children. Annu. Rev. Nutr. 2012, 32, 391–415. [Google Scholar] [CrossRef] [Green Version]
- Grin, B.M.; Gayle, T.L.; Saravia, D.C.; Sanders, L.M. Use of Farmers Markets by Mothers of WIC Recipients, Miami-Dade County, Florida, 2011. Prev. Chronic Dis. 2013, 10, E95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pitts, S.B.J.; Gustafson, A.; Wu, Q.; Mayo, M.L.; Ward, R.K.; McGuirt, J.T.; Rafferty, A.P.; Lancaster, M.F.; Evenson, K.R.; Keyserling, T.C.; et al. Farmers’ market use is associated with fruit and vegetable consumption in diverse southern rural communities. Nutr. J. 2014, 13, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conner, D.S.; Garnett, B.R. Economic and Environmental Drivers of Fruit and Vegetable Intake Among Socioeconomically Diverse Adults in Vermont. J. Hunger Environ. Nutr. 2016, 11, 263–271. [Google Scholar] [CrossRef]
- Strom, B.L.; Yaktine, A.L.; Oria, M. Sodium Intake and Health Outcomes. National Academies Press (US). 2013. Available online: https://www.ncbi.nlm.nih.gov/books/NBK201520/ (accessed on 9 December 2020).
- Park, Y.; Quinn, J.; Flórez, K.; Jacobson, J.; Neckerman, K.; Rundle, A. Hispanic immigrant women’s perspective on healthy foods and the New York City retail food environment: A mixed-method study. Soc. Sci. Med. 2011, 73, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Migliaretti, G.; Ame, C.; Ciullo, S.; Fontana, E.; Stura, I.; Nano, E.; Laino, F.; Isoardo, G. Metabolic and psychological effects of short-term increased consumption of less-processed foods in daily diets: A Pilot Study. Diabetes Metab. 2020, 46, 66–69. [Google Scholar] [CrossRef]
- Panzone, L.; Di Vita, G.; Borla, S.; D’Amico, M. When Consumers and Products Come from the Same Place: Preferences and WTP for Geographical Indication Differ Across Regional Identity Groups. J. Int. Food Agribus. Mark. 2016, 28, 286–313. [Google Scholar] [CrossRef] [Green Version]
- Cicia, G.; Furno, M.; Del Giudice, T. Do consumers’ values and attitudes affect food retailer choice? Evidence from a national survey on farmers’ market in Germany. Agric. Food Econ. 2021, 9, 3. [Google Scholar] [CrossRef]
- Gordon-Larsen, P. Food Availability/Convenience and Obesity. Adv. Nutr. 2014, 5, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Cobb, L.K.; Appel, L.J.; Franco, M.; Jones-Smith, J.C.; Nur, A.; Anderson, C.A. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity 2015, 23, 1331–1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zenk, S.N.; Tarlov, E.; Wing, C.; Matthews, S.A.; Jones, K.; Tong, H.; Powell, L.M. Geographic Accessibility of Food Outlets Not Associated With Body Mass Index Change Among Veterans, 2009–2014. Health Aff. 2017, 36, 1433–1442. [Google Scholar] [CrossRef] [PubMed]
- Burkhauser, R.; Cawley, J. Beyond BMI: The value of more accurate measures of fatness and obesity in social science research. J. Health Econ. 2008, 27, 519–529. [Google Scholar] [CrossRef] [Green Version]
- Saxe-Custack, A.; LaChance, J.; Hanna-Attisha, M.; Dawson, C. Flint Kids Cook: Positive influence of a farmers’ market cooking and nutrition programme on health-related quality of life of US children in a low-income, urban community. Public Health Nutr. 2021, 24, 1492–1500. [Google Scholar] [CrossRef]
- Pitts, S.B.J.; Wu, Q.; McGuirt, J.T.; Crawford, T.W.; Keyserling, T.C.; Ammerman, A.S. Associations between access to farmers’ markets and supermarkets, shopping patterns, fruit and vegetable consumption and health indicators among women of reproductive age in eastern North Carolina, USA. Public Health Nutr. 2013, 16, 1944–1952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bharucha, Z.P.; Weinstein, N.; Watson, D.; Boehm, S.; Böhm, S. Participation in local food projects is associated with better psychological well-being: Evidence from the East of England. J. Public Health 2019, 42, e187–e197. [Google Scholar] [CrossRef]
- Trapl, E.S.; Smith, S.; Joshi, K.; Osborne, A.; Benko, M.; Matos, A.T.; Bolen, S. Dietary Impact of Produce Prescriptions for Patients with Hypertension. Prev. Chronic Dis. 2018, 15, E138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riboli, E.; Norat, T. Epidemiologic evidence of the protective effect of fruit and vegetables on cancer risk. Am. J. Clin. Nutr. 2003, 78, 559S–569S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terry, P.; Terry, J.B.; Wolk, A. Fruit and vegetable consumption in the prevention of cancer: An update. J. Intern. Med. 2008, 250, 280–290. [Google Scholar] [CrossRef]
- Sauvaget, C.; Nagano, J.; Hayashi, M.; Spencer, E.; Shimizu, Y.; Allen, N. Vegetables and fruit intake and cancer mortality in the Hiroshima/Nagasaki Life Span Study. Br. J. Cancer 2003, 88, 689–694. [Google Scholar] [CrossRef] [Green Version]
- Law, M.R.; Morris, J. By how much does fruit and vegetable consumption reduce the risk of ischaemic heart disease? Eur. J. Clin. Nutr. 1998, 52, 549–556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A Clinical Trial of the Effects of Dietary Patterns on Blood Pressure. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [Green Version]
- Deaconu, A.; Berti, P.; Cole, D.; Mercille, G.; Batal, M. Market Foods, Own Production, and the Social Economy: How Food Acquisition Sources Influence Nutrient Intake among Ecuadorian Farmers and the Role of Agroecology in Supporting Healthy Diets. Sustainability 2021, 13, 4410. [Google Scholar] [CrossRef]
- Sorlie, P.; Rogot, E.; Anderson, R.; Johnson, N.; Backlund, E. Black-white mortality differences by family income. Lancet 1992, 340, 346–350. [Google Scholar] [CrossRef]
- Bainum Family Foundation. Insights on Fresh-Produce Distribution in D.C.’s Wards 7 and 8. Available online: http://bainumfdn.org/wp-content/uploads/2019/11/Bainum_FSI-Insights-Part-1_Nov2019.pdf (accessed on 20 March 2021).
- Carlson, A.; Lino, M.; Juan, W.; Hanson, K.; Basiotis, P.P. Thrifty Food Plan, 2006. United States Department of Agriculture, Center for Nutrition Policy and Promotion, 42899. Available online: https://ideas.repec.org/p/ags/usacnr/42899.html (accessed on 29 April 2021).
- Jabs, J.; Devine, C.M.; Bisogni, C.A.; Farrell, T.J.; Jastran, M.; Wethington, E. Trying to Find the Quickest Way: Employed Mothers’ Constructions of Time for Food. J. Nutr. Educ. Behav. 2007, 39, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Stewart, H.; Blisard, N.; Jolliffe, D.; Bhuyan, S. The Demand for Food away from Home: Do Other Preferences Compete with Our Desire to Eat Healthfully. J. Agric. Resour. Econ. 2005, 30, 3. Available online: https://econpapers.repec.org/article/agsjlaare/30984.htm (accessed on 29 April 2021).
- Cohen, A.J.; Lachance, L.L.; Richardson, C.R.; Mahmoudi, E.; Buxbaum, J.D.; Noonan, G.K.; Murphy, E.C.; Roberson, D.N.; Hesterman, O.B.; Heisler, M.; et al. “Doubling Up” on Produce at Detroit Farmers Markets: Patterns and Correlates of Use of a Healthy Food Incentive. Am. J. Prev. Med. 2018, 54, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.M.; Dooley, E.E.; Ganzar, L.A.; Jovanovic, C.E.; Janda, K.; Salvo, D. Neighborhood Food Environment and Physical Activity Among U.S. Adolescents. Am. J. Prev. Med. 2019, 57, 24–31. [Google Scholar] [CrossRef]
| Group | Variable | Mean | St. Dev | Min | Max | N |
|---|---|---|---|---|---|---|
| Health Indicators | Weekly meals away from home | 3.6 | 3.2 | 0 | 22 | 360 |
| BMI | 28.0 | 6.0 | 17.0 | 65.0 | 354 | |
| Daily time spent in preparing meal (mins) | 44.3 | 27.5 | 0 | 200 | 362 | |
| Daily fresh FV consumption (cups) | 3.4 | 2.1 | 0 | 18 | 360 | |
| Farmers’ market Usage | FM usage (percent of FM purchase in total household food purchase) | 4.6 | 7.36 | 0.04 | 48.07 | 358 |
| Control Variables | Male | 0.42 | -- | -- | -- | 364 |
| Age | 46.4 | 20 | 89 | 364 | ||
| Bachelor’s degree or higher | 0.60 | -- | -- | -- | 364 | |
| Non-Hispanic White | 0.52 | -- | -- | -- | 364 | |
| Non-Hispanic Black | 0.20 | -- | -- | -- | 364 | |
| Non-Hispanic Asian | 0.12 | -- | -- | -- | 364 | |
| Hispanic | 0.14 | -- | -- | -- | 364 | |
| Living with children under 18 | 0.24 | -- | -- | -- | 364 |
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| FV Consumption (log) | Meal Preparation Time (log) | Meals Bought | BMI (log) | FV Consumption (log)-with Market Accessibility as IV | Meal Preparation Time (log)-with Market Accessibility as IV | |
| Farmers’ market usage (log) | 0.065 *** | 0.094 ** | −0.271 ** | 0.008 | 0.254 ** | 0.377 * |
| (0.021) | (0.042) | (0.135) | (0.008) | (0.127) | (0.212) | |
| Bachelor’s degree or higher | 0.195 ** | 0.093 | 0.401 | −0.068 ** | ||
| (0.077) | (0.181) | (0.440) | (0.033) | |||
| Education level | 0.038 | −0.052 | ||||
| (0.040) | (0.066) | |||||
| Age | −0.002 | −0.001 | −0.015 | 0.002 ** | −0.004 | −0.007 |
| (0.002) | (0.004) | (0.014) | (0.001) | (0.003) | (0.006) | |
| Male | −0.157 ** | −0.126 | 0.045 | 0.070 ** | −0.085 | 0.016 |
| (0.079) | (0.174) | (0.498) | (0.031) | (0.095) | (0.196) | |
| Non-Hispanic Black (Non-Hispanic White as default) | −0.222 ** | −0.256 | 1.136 | 0.072 ** | ||
| (0.112) | (0.230) | (0.689) | (0.032) | |||
| Non-Hispanic, Other (Non-Hispanic White as default) | −0.356 *** | −0.010 | 0.808 | −0.011 | ||
| (0.135) | (0.235) | (0.801) | (0.054) | |||
| Hispanic (Non-Hispanic White as default) | −0.034 | −0.175 | 0.558 | 0.036 | ||
| (0.152) | (0.342) | (0.842) | (0.061) | |||
| Non-Hispanic, 2+ Race (Non-Hispanic White as default) | −0.510 * | 0.080 | 2.716 * | 0.041 | ||
| (0.308) | (0.197) | (1.626) | (0.106) | |||
| Household income | 0.006 | 0.012 | −0.084 * | 0.002 | 0.017 | 0.039 * |
| (0.009) | (0.015) | (0.050) | (0.004) | (0.014) | (0.023) | |
| With children | 0.050 | −0.296 | 0.476 | 0.038 | 0.206 | −0.054 |
| (0.101) | (0.252) | (0.690) | (0.040) | (0.150) | (0.312) | |
| constant. | 0.810 *** | 3.309 *** | 4.988 *** | 3.300 *** | 1.690 ** | 5.552 *** |
| (0.239) | (0.507) | (1.563) | (0.110) | (0.853) | (1.273) | |
| N | 354 | 355 | 355 | 348 | 353 | 354 |
| R-Squared | 15.46% | 10.17% | 8.77% | 11.89% | 18.87% | 19.02% |
| Independent Variable Instrumented: Log Farmers’ Market Usage | Dependent Variable | |||
|---|---|---|---|---|
| Statistics | (log) FV | (log) meal preparation time | (log) meals bought | |
| Instrument: whether someone visits two or more markets | Coefficient | 0.75 *** | 0.74 *** | 0.64 ** |
| F-statistics for IV | 12.16 | 12.15 | 8.84 | |
| N | 353 | 354 | 357 | |
| Instrument: non-health incentivized | Coefficient | −0.119 | −0.15 | −0.252 |
| F-statistics for IV | 9.49 | 10.04 | 6.11 | |
| N | 293 | 294 | 297 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, X.; Clarke, L.W.; Zendehdel, K. Farmers’ Market Usage, Fruit and Vegetable Consumption, Meals at Home and Health–Evidence from Washington, DC. Sustainability 2021, 13, 7437. https://doi.org/10.3390/su13137437
Hu X, Clarke LW, Zendehdel K. Farmers’ Market Usage, Fruit and Vegetable Consumption, Meals at Home and Health–Evidence from Washington, DC. Sustainability. 2021; 13(13):7437. https://doi.org/10.3390/su13137437
Chicago/Turabian StyleHu, Xiaochu, Lorraine W. Clarke, and Kamran Zendehdel. 2021. "Farmers’ Market Usage, Fruit and Vegetable Consumption, Meals at Home and Health–Evidence from Washington, DC" Sustainability 13, no. 13: 7437. https://doi.org/10.3390/su13137437
APA StyleHu, X., Clarke, L. W., & Zendehdel, K. (2021). Farmers’ Market Usage, Fruit and Vegetable Consumption, Meals at Home and Health–Evidence from Washington, DC. Sustainability, 13(13), 7437. https://doi.org/10.3390/su13137437






