1. Introduction
Pharmaceutical marketing has the same objectives as other industries to enhance the profitability and market share of the organization by fulfilling the needs and demands of the customers taking into account the preferable consideration of products. Other than the pharmaceutical industry, it is very easy to disseminate the marketing message to the end-users through above the line (ATL) and below the line (BTL) media communication strategies. However, in the pharmaceutical industry, the consumers are not the customer of the pharmaceutical industry; rather, the doctor community is the prime customer for the pharmaceutical companies [
1,
2]. Since the pharmaceutical industry is highly regulated, companies cannot advertise their drugs through electronic and print media channels. Pharmaceutical marketing is quite different as compared to the other industries where the consumer (patient) is not the direct customer of the pharmaceutical industry, however a doctor is the customer of the pharmaceutical industry and the patient is a customer of a doctor. Therefore, pharmaceutical companies target the physicians, and physicians decide to prescribe a certain medicine; thus, in pharmaceutical marketing, strategies are devised for the doctors, not for the patient. According to Campbell et al. [
3], Moynihan [
4], and Ahmed et al. [
5], the relationship between pharmaceutical companies and doctors has gained considerable attention that originates from a conflict between the doctor’s financial self-interest and the ethical professional interest. The pharmaceutical companies market their drugs through diverse marketing and promotional activities such as free sampling to the doctors, expensive and inexpensive gifts to the doctors, sponsored lecture/symposia for individual doctors and hospitals, sponsoring physicians in national and international conferences, medical detailing, and sponsorship of continuing medical educations (CMEs) for individual doctors. Thus, these marketing activities exert a significant impact on the prescription behavior of physicians, and doctors prescribe their medicine without a due cost and benefit analysis (side effects vs. cure effects) [
6,
7]. However, few studies demonstrated that the marketing activities of the pharmaceutical industry do not influence the majority of doctors; instead, doctors prescribe medicines on the merit of the drug [
7,
8,
9]. However, a substantial amount of literature has confirmed the influential effect of pharmaceutical marketing activities, which has a positive and significant on physician’s prescription behavior [
9,
10]. Besides the increasing trend of pharmaceutical marketing expenditure, another important concern is the inappropriate, expensive, irrational, and harmful drugs’ prescription. According to Hogerzeil [
10] and Carthy et al. [
11], this matter is two exhibitions; on the one hand, unnecessary and ineligible medicine are being prescribed to the patient, and on other hand, there are ample shreds of evidence of the prescribed drug being useless or misuse of medicines. The outcome of this misuse of drugs may result in the loss of health, loss of quality of life of the patient, and enhances the medical and healthcare expenditure, thus it is important to follow the prescription guidelines for prescription medicines [
5,
12].
Thus, in this context, there is a strong need to evaluate factors that alter or change the physician’s prescription decisions. Numerous medical pieces of literature concern the influential factor of physician’s prescription decisions, which demonstrates that few factors are fixed and cannot be changed or modified; however, several factors have a significant role to influence the physician’s prescription decisions [
13,
14]. Most of the literature considers the empirical analysis only. To date, literature regarding the physician’s decision-making process lacks the sound theoretical foundations [
15], as most studies have been based on an exploratory approach, and did not address the theoretical approach for the decision-making process of physicians regarding the selection and prescription of a drug [
7,
16,
17]. However, few research studies have incorporated different theoretical model to understand decision-making processes such as attitude–behavior models including the planned behavior theory (TPB) and the reasoned action theory [
18,
19,
20,
21,
22,
23,
24]. The main intention is to understand the rationale in the decision making of an individual through these theories; thus, the cognitive method can elucidate the individuals’ behavior. According to Raisch [
22], the cognitive models may address the physician’s decision-making process, however Godin et al. [
19] and Lee and Yun [
25] have demonstrated that the theory of planned behavior (TPB) has several drawbacks, and the TPB does not take into account the emotional approach of an individual. In the same vein, Conner et al. [
26] have recommended including the emotional variables to modify the behavioral theories. The impact of social media on emotions was studied in terms of technology acceptance [
27].
According to Theodorou et al. [
15] and Prosser et al. [
28], the decision of the physician’s prescription is a multifaceted procedure, which encompasses several variables. Raisch [
22] and Schommer and Hansen [
29] have demonstrated that physicians take into account several factors while deciding to prescribe a drug and numerous sorts of precarious heuristics in performing their responsibilities of patient treatment. According to Reyna and Rivers [
30], there are several factors that have been narrated regarding the physician’s decision-making process in previous literature, but according to the literature, any single theory cannot explain the factors about the physician’s prescription behavior. Thus, the multifaceted model of theories is employed to comprehend the influencing variables for the decision-making process of physicians [
19]. The current studies demonstrated a lack of agreement amongst the researchers regarding the use of theories to examine the physician’s prescription behavior and its determinants for the decision-making process [
31,
32,
33]. According to the existing literature, the important factors include patient characteristics (expectations and requests), and marketing efforts of pharmaceutical companies. The pharmacist factor (pharmacist expert power and pharmacist–physician collaboration) has also been recognized as a cogent element for physician’s decision-making process for the responsible prescription behavior [
34,
35,
36,
37]. However, there is a need to understand these factors and approaches in a conclusive conceptual framework for the decision-making process of the physician’s decision to prescribe a drug [
19,
38].
The development of the theoretical model is important to address the comprehensiveness of the decision-making process of physicians, regarding any prescription pattern across the globe [
20,
39,
40]. For the development of a theoretical model, some research studies have been carried out such as those by Howie [
14], Raisch [
22], Hemminki [
23], and Knapp and Oeltjen [
41], but most of them are outdated. Therefore, there is a need to address more theoretical research studies to comprehend the physician’s decision-making process. Thus, Murshid and Mohaidin [
42] have carried out important research to develop a conceptual framework to understand the physician’s decision-making process regarding responsible prescription behavior towards medicines. However, there is no empirical evidence for the effectiveness of that theoretical framework. Thus, the undertaken study is an attempt to confirm the complex conceptual framework, which was developed by the Murshid and Mohaidin [
42]. The previous literature assessed the behavioral and social theories such as a theory of planned behavior (TPB), agency theory, the theory of social power, theory of stimulus–response behavior, and persuasion theory to ascertain the influence of marketing efforts, pharmacist factors, and patient characteristics on the physician’s prescription behavior. Hence, these social and behavioral theories and models were studied to comprehend the significant factors, which determine and develop the innovative conceptual paradigm to influence the physician’s prescription behavior [
22,
42].
This research is a shred of conclusive evidence for practical implications of that complex theoretical framework. Hence, this research fills the gap to employ an integrated theoretical model and to examine the practicality of this multi-dimensional theoretical model to assess the factors that contribute to reshaping the physician’s decision-making process regarding prescription behavior. This model used the theory of planned behavior (TPB) and agency theories that elucidate the twofold function of the doctor as an intermediary and customer. The TPB model is very much linked to the physician as an intermediary in a clinical environment [
19,
43]. The stimulus–response theory and persuasion theory have been demonstrated the role of pharmaceutical marketing efforts in reshaping the behavior of the physician to prescribe the drug [
42]. However, in this model, the social power theory is used in the context of the influential effects of pharmacist factors [
42].
The rest of the paper is comprised of several sections, such as: (1)
Section 2 deals with previous literature and conceptual framework; (2)
Section 3 contains the material and methods: (3)
Section 4 demonstrates the results and findings; (4)
Section 5 is comprised of the discussion; and (5)
Section 6 contains the conclusions, followed by the practical implications, limitations, and future areas of research studies.
2. Previous Literature and Conceptual Framework
According to previous literature, multiple factors influence the physician’s prescription behavior towards the drugs. Murshid and Mohaidin [
42] and Hartzema et al. [
44] have demonstrated that non-medical factors are significant predictors to influence the physician’s prescription behavior. However, Armstrong et al. [
45] have revealed that senior doctors’ prescription patterns can influence the behavior of general practitioners’ prescription habits. According to Kareem et al. [
46], tangible rewards used by the pharmaceutical companies as promotion tactics and frequent visits to medical representatives significantly increase the prescription loyalty of physicians. Though Rahmner et al. [
47] have identified new dimensions for influencing physician’s prescription behavior such as the physician–patient relationship, Taneja [
48] has exhibited that private doctors are more attracted towards the personalized activities and promotional tools, whereas the hospital’s associated physicians are attracted towards the scientific activities. According to Tan et al. [
49], family physicians give more weight to the promotional activities than the detailing and CMEs programs; however, Theodorou et al. [
15] have demonstrated that clinical effectiveness of the drugs is the major criteria for the physician’s prescription behavior. According to Kotwani et al. [
36], sales calls of Medical Representatives (MRs) exert a cogent influence on the physician’s prescription behavior; however, Karayanni [
50] has concluded that the personal obligation is a major factor to influence physician’s prescription behavior. Several research studies have investigated that trust and quality of the drug, effective marketing communication, MRs effectiveness, cost of the drug, and corporate image of pharmaceutical companies are the significant factors to influence the physician’s prescription behavior [
5,
47,
51,
52]. According to Wazana [
53], Prosser and Walley [
54], and Caudil et al. [
55], the interaction between doctors and pharmaceutical companies starts at the beginning of their careers, thus customer relationship employs a significant part in reshaping the responsible prescription behavior of physicians. However, Lieb and Brandtönies [
56], Chimonas et al. [
57], Saito et al. [
58], and Watkins et al. [
59] examine the pharmaceutical sales representatives’ (PSRs) association with the doctors, and effectiveness of PSRs, and concluded the major factors to influence the physician’s prescription behavior. Numerous studies have examined the impact of marketing tools and established a positive correlation with the prescription behavior of physicians [
9,
60,
61].
2.1. Theories Relevant to Factors Influencing the Prescribing Decision
Besides the marketing and medical tools, previous literature also studied the link of these factors with different theories and models to influence the physician’s prescription behavior towards medicines, thus the literature has provided the theoretical and conceptual foundation to the elements that influence the responsible prescription behavior. Therefore, the previous literature assessed the behavioral and social theories such as a theory of planned behavior (TPB), agency theory, the theory of social power, theory of stimulus–response behavior, and persuasion theory to ascertain the influence of marketing efforts, pharmacist factors, and patient characteristics on the physician’s prescription behavior. Hence, these social and behavioral theories and models were studied to comprehend the significant factors, which determine and develop the innovative conceptual paradigm to influence the physician’s prescription behavior [
22,
42,
62].
2.1.1. Agency Theory
Jansen and Meckling [
63] have introduced the concept of agency theory, and Shapiro [
62] has introduced the different objectives of this theory. However, Eisenhardt [
64] has reviewed the context, concept, and different principles of agency theory, and he established that this theory offers a framework for examining the relationship between impartial to analyze the problem, which exists between two parties and instrument to resolve it. According to Eisenhardt [
64] and Mott et al. [
65], in agency theory, the association happens when the patient (first party) believes physician (second party) to accomplish certain activities on behalf of the client (the pharmaceutical company). Thus, based on this approach, the pharmaceutical company is motivated to sell its drugs by using different marketing and branding efforts and provide necessary prescribing information to the physician to prescribe the drugs. During the pharmaceutical and physician relationship, various environmental elements may have little control over the cost and benefit (side effects vs. cure effects) ratio of a drug, and persistence of physicians [
43]. Though in the physician and patient’s relationship, the patient entirely relies on the expert power of physician for diagnosis and prescription [
29]. However, Epstein and Ketcham [
66] exhibited that the patient is interested in cost-effective and appropriate treatment in terms of a physician’s prescription. According to Groves [
43], the physician’s decision to prescribe a certain drug is based on several influencing factors that the patient has little control over such as physician’s persistence, drug characteristics, and cost/benefit (side effects vs. cure effects) of the medicine. The physician–patient relationship is further strengthened when the doctor fulfils the patients’ requests and expectations for a certain drug [
37,
66].
2.1.2. Theory of Persuasion
Persuasion is a successful attempt to influence the decision-making process of an individual; persuasion is an art of changing the principles, philosophies, and behavior through effective communication [
29,
67]. Persuasion is comprised of cognition and emotional responses, and the interaction of emotion and cognition can change the physician’s behavior regarding a certain drug prescriptions. The process of persuasion consists of four elements, for instance, (1) sender information (medical representatives of pharmaceutical firm), (2) the physician (a receiver), (3) the interchange between receiver and sender (medical Representative and physician), and (4) the alteration in behavior (the physician’s prescription behavior). According to Bettinghaus [
68], the persuasion instructs an individuals’ behavior (doctors’ prescription behavior) voluntarily in reaction to a specific stimulus, which alters the mind. According to Storey [
69], the change of mind is associated with the particular desires of an individual (physician), for instance, prescriptions required for his/her patient, such changes might be accomplished immediately (prescription decision) or sometimes it requires several months or years. The previous literature demonstrated that the persuasion theory is used to enhance the physician’s prescribing behavior through effective pharmaceutical marketing and activities [
22,
29]. According to O’keefe [
67] and Petty and Cacioppo [
70], the elaboration likelihood model (ELM), which is widely employed in the model in persuasion theory’s perspective, suggests that the individual (the physician) uses both emotional and cognitive abilities and reactions to deduce data for decision-making. The influencing factors for physician’s prescription behavior include a personal relationship with the pharmacist and medical representatives, environmental stimuli (patient and pharmacist), marketing stimuli (brand name of a drug such as famous brands of multinational companies, for example Amoxil, Lipitor, Zocor, Augmentin, etc., in comparisons of local companies brands), sales promotion, drug information such as prescribing information of medicine such as dosage, indications, side effects, etc., drug characteristics, and physician’s characteristics (habit persistence) towards the medicines.
2.1.3. The Buyer Behaviour—Stimulus–Response (SR) Theory
Both buying behavior models such as the stimulus–response (SR) model and elaboration likelihood model (ELM) are similar because both consider emotions and cognizance to influence the individual. Xing and Othman [
71] conclude that the SR model is linked to the black box model in which emphasis is not on the process, instead it deals with the relationship between the stimuli and the consequential reaction. However, original communication inferred from this model is the procedure of physician’s awareness from the outward stimuli for the prescription decision towards medicines. Similar to a consumer, the physician is faced with numerous influences that may reshape his/her prescription behavior; the SR model offers a combined stimulus with appropriate modification. The pharmaceutical companies generate different stimuli through marketing mix factors, which influence the physician’s intention to prescribe a drug; these stimuli trespass into the black box of a doctor and ultimately translate into influences. According to Kotler [
72], it comprises two elements; firstly, physician characteristics influence the way in which stimuli are perceived, imagined, and translated through the marketers, and such features of a physician can be accredited to secretive factors, for instance psychological and social variables. However, secondly, the process of decision making of the physician eventually defines the physician’s prescription behavior [
73].
2.1.4. Theory of Planned Behavior (TPB)
According to Eccles et al. [
74], the theory of planned behavior (TPB) is one of the most applicable and repeatedly employed behavioral theories to understand the responsible prescription behavior of physicians. Ponnet et al. [
18], Godin et al. [
19], Perkins et al. [
75], and Kramer et al. [
76] have successfully used TPB theory to comprehend the underlying factors for prescribing behavior of doctors in different specialties. The literature is based on the TPB model of Ajzen [
24] that explains and examines the personal norms’ capability, attitude, and a device of perceived behavioral force that changes the intentions and responsible prescription behavior of physicians. The degree that the doctor is favorable or unfavorable depends on their attitude towards the marketing efforts and other factors such as availability of drug information (prescribing information of medicine such as dosage, indications, side effects, etc.), sales promotion, medical representatives’ effectiveness, and brand name of a drug (famous brands of multinational companies such as Amoxil, Lipitor, Zocor, Augmentin, etc. in comparison to local companies brands) [
42]. The second element of the TPB theory concerning subjective norms measures the influencing pressure of patients’ demand for a certain drug, expectations of patients, pharmacists’ expert power, and pharmacist and physician collaboration for the prescription of a certain drug. However, the third factor of the TPB theory deals with the perceived behavioral control that is a function of behavior, which suggests experience or product knowledge that deals with future problems. Thus, perceived behavioral control (PBC) directly influences the physician’s responsible prescription behavior because of the first-hand experience of a physician [
24]. However, drug characteristics, physician’s persistence, cost/benefit ratio (side effects vs. cure effects) of the drug, and trustworthiness of physicians on the expert power of pharmacist are contextual factors, which influence the physician’s responsible prescription behavior [
42].
2.1.5. Theory of Social Power (TSP)
According to Basak et al. [
77], in the healthcare context, there will always be cooperation and communication amongst team members, which will usually have an effect due to the social power of team members. For understanding the crucial role of the pharmacist, the social power theory is the best application; the power is expressed as the ability to influence. However, the social power is the ability to influence the behavior of someone else through persuasion, which in the healthcare context concerns the role of an individual to have a significant influence on team members to alter their behavior [
77,
78,
79]. However, expert power refers to the knowledge, work experience, and skills of an individual that are mostly based on intensive education and work experience, and credentials of an individual. Thus, in the context of healthcare, pharmacists’ expert power influences the physician’s prescription intentions due to their intensive education and working experience, and physicians rely on the recommendations of a pharmacist [
78,
80]. The power and influence are the two significant components of the theory of social power, following the control relational theory, the pharmacist and physician collaboration, the pharmacist education, and experience, which drive the responsible prescription behavior of physicians by providing information, indications, advice, and safety profile regarding the drug. On the other hand, the literature exhibited that trustworthiness is the moderating factor in a relationship between pharmacist factors and physician’s prescription behavior [
42,
78].
As shown in
Figure 1, 13 causal factors are classified and merged; this novel model consists of marketing efforts, patients’ characteristics, and pharmacist factors as direct influencers. However, trustworthiness has been used as a moderating variable in a relationship between pharmacist factors and physician’s decision to prescribe drugs [
42,
80]. Moreover, the suggested model assimilates several features of seven recognized conceptual models; thus, the undertaken research is an empirical effort to examine the physician’s decision to prescribe the drug based on different theories and models, which were discussed earlier. This research also evaluates or empirically tests previously featured models and theories that were demonstrated in several research studies [
19,
23,
39,
41,
42]. The undertaken research aims to empirically examine the theoretical framework in the context of the Pakistani healthcare sector; thus, the results of this study provide new aspects that influence the physician’s prescription behavior. Hence, this study will also be beneficial to the marketers of the pharmaceutical industry to develop effective and efficient marketing strategies to get maximum ROI of their investments.
2.2. Hypotheses Formulation
Thus, based on previous literature about the social and behavioral theories, the following hypotheses have been developed:
Hypotheses about the DIRECT relationship
Hypothesis 1 (H1). Drug information availability has a significant and positive effect on a physician’s decision to prescribe a drug.
Hypothesis 2 (H2). Brands of the drug have a significant and positive influence on physician’s decision to prescribe a drug.
Hypothesis 3 (H3). Sales promotion has a significant and positive effect on a physician’s decision to prescribe a drug.
Hypothesis 4 (H4). Medical representatives’ effectiveness has a significant and positive effect on a physician’s decision to prescribe a drug.
Hypothesis 5 (H5). Patient’s request for a drug has a significant and positive effect on a physician’s decision to prescribe a drug.
Hypothesis 6 (H6). Patient’s expectation has a significant and positive effect on a physician’s decision to prescribe a drug.
Hypothesis 7 (H7). Pharmacist expert power has a significant and positive effect on a physician’s decision to prescribe a drug.
Hypothesis 8 (H8). Pharmacist–physician collaboration has a significant and positive effect on a physician’s decision to prescribe a drug.
2.3. The Moderating Variables for the Recommended Model
The suggested model proposes an association between the influences (moderation) of numerous variables, which have been found in distinctive physician’s models for prescription intentions towards the medicines. Thus, based on previous literature, the cost and benefit ratio of a drug has a significant moderating effect between endogenous variables and physician’s decision to prescribe a drug [
29,
37,
43]. However, in the physician and patient relationship, the patient entirely relies on the expert power of physician for diagnosis and prescription, hence physician’s habit persistence is also a significant moderating variable [
29,
39,
66]. According to Groves [
43], the physician’s decision to prescribe a certain drug is based on several influencing (moderating) factors that the patient has a little control over such as physician’s persistence, drug characteristics, and cost/benefit of a medicine [
37,
42,
64,
66]. Similarly, the literature exhibited that trustworthiness is a moderating factor in the relationship between pharmacist factors and physician’s prescription behavior [
42,
78,
80]. Hence, the undertaken model, the cost and benefit ratio of drug (CBR), drugs’ characteristics (DCH), and physician’s habit persistence (PHP) have been taken as moderating factors in an association between medical representative effectiveness (MRE) and patient expectations (PEX), and physician’s decision to prescribe drugs (PDP) [
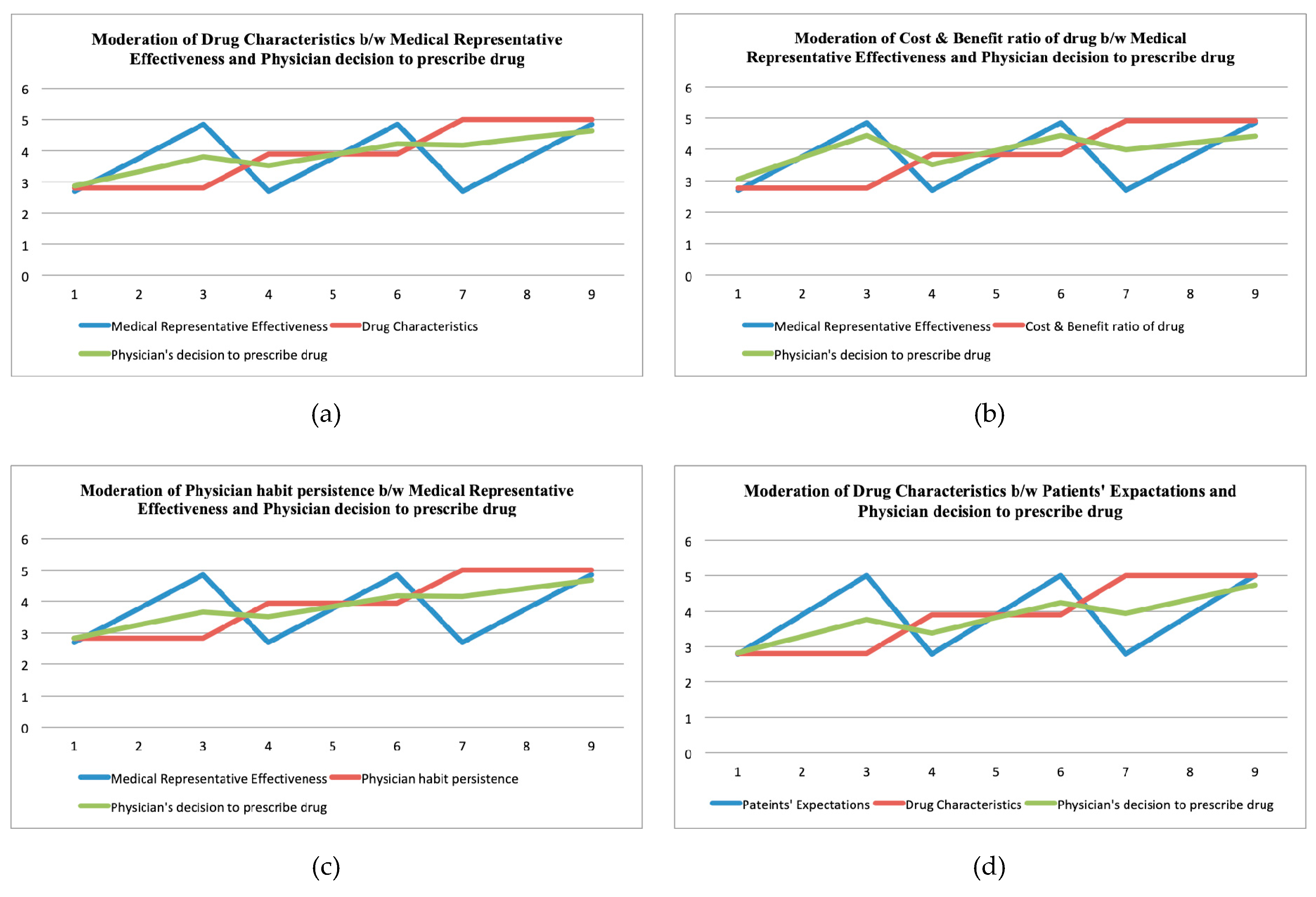
29,
39,
41,
42,
66]. The conceptual frame also included trustworthiness (TRU) as the moderating factor in an association between pharmacists’ expert power (PEP) and pharmacist–physician collaboration (PPC), and physician’s decision to prescribe drugs (PDP) [
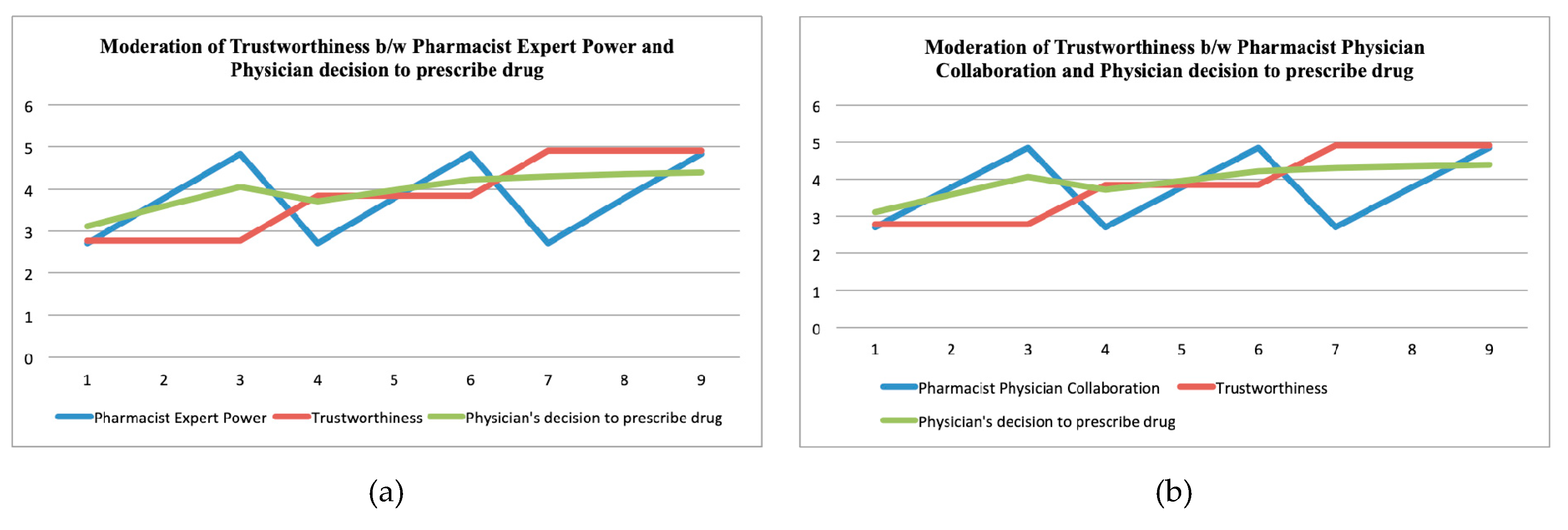
43,
66,
78,
80].
2.4. Hypotheses about Moderating Effect
The moderating variables have a direct relationship with physician’s decision to prescribe a drug. The direct relationship is defined as “If the value of moderating variable increases, then the value of outcome variable also increases or vice versa”. However, the values of exogenous variables are considered constant as explained in results section.
Hypothesis 9A (H9A). Drug characteristics have a significant and direct moderating effect between medical representatives’ effectiveness and physician’s decision to prescribe a drug.
Hypothesis 9b (H9b). Drug characteristics have a significant and direct moderating effect between the patient’s expectations and the physician’s decision to prescribe a drug.
Hypothesis 10A (H10A). Cost and benefit ratio of a drug has a significant and direct moderating effect between medical representatives’ effectiveness and physician’s decision to prescribe a drug.
Hypothesis 10B (H10B). Cost and benefit ratio of a drug has a significant and direct moderating effect between patient’s expectations and physician’s decision to prescribe a drug.
Hypothesis 11A (H11A). Physician’s habit persistence has a significant and direct moderating effect between medical representatives’ effectiveness and physician’s decision to prescribe a drug.
Hypothesis 11B (H11B). Physician’s habit persistence has a significant and direct moderating effect between a patient’s expectations and the physician’s decision to prescribe a drug.
Hypothesis 12A (H12A). Trustworthiness has a significant moderating effect between pharmacist expert power and a physician’s decision to prescribe a drug.
Hypothesis 12B (H12B). Trustworthiness has a significant and direct moderating effect between pharmacist–physician collaboration and physician’s decision to prescribe a drug.
2.5. Proposed Model of the Study
The previous review helps to understand and assimilate the important theories and frameworks to build a concrete model to comprehend the multifaceted physician’s decision to prescribe the medicines. The challenge of this model is to test and measure the conceptual framework because it is comprised of different theories and models. This empirical study tests the theoretical framework of different scholarly works such as French and Raven [
79], Ajzen [
24], Kotler [
73], Petty and Cacioppo [
70], Jansen and Meckling [
63], and Murshid and Mohaidin [
42]. The undertaken study not only tests and validates the existing findings, but also enhances the current knowledge base on the foundation of a newly derived model of
Figure 2. These relationships have been based on previous theories, which were discussed earlier and mentioned in
Figure 1 [
42].
5. Discussion
The purpose of the undertaken study is to test the model empirically, which encompasses different theories and models. The outcomes of this study concluded that the marketing factors such as brands of the drug, sales promotion, drug information availability, and medical representatives’ effectiveness, as well as the characteristics of patients including patients’ expectations, patients’ request for a particular drug, and pharmacist factors, for instance, pharmacist expert power and pharmacist physician collaborations, have a positive and significant influence on the decision of a physician to prescribe a medicine. Thus, the outcomes of the direct relationship validated the theoretical construct such as attitudes and marketing stimuli, which were derived from the theory of planned behavior (TPB) [
18,
19,
24,
74,
75,
76], theory of persuasion [
22,
29,
67,
68,
69,
70], theory of social power [
77,
78,
79,
80], and stimulus–response (SR) theory [
71,
72,
73] for marketing factors such as brands of the drug, sales promotion, drug information availability (prescribing information), and MR effectiveness. Similarly, results also validated theoretical constructs such as social norm and social stimuli, which were extracted from the theory of planned behavior [
18,
19,
24,
74,
75,
76], theory of persuasion [
22,
29,
67,
68,
69,
70,
71], agency theory [
29,
37,
43,
62,
63,
64,
65,
66], and stimulus–response (SR) theory [
71,
72,
73] for the characteristics of patients including patients’ expectations, patients’ request for a particular medicine. Finally, the outcomes of direct relationship also confirmed the similar theoretical constructs such as social norm and social stimuli, which were also taken from TPB [
18,
19,
24,
74,
75,
76], theory of persuasion [
22,
29,
67,
68,
69,
70], social power theory [
71,
77,
78,
79,
80], and SR theory [
71,
72,
73] for the factors of pharmacist including pharmacist–physician collaboration and expert power of pharmacist. The outcomes of the indirect relationship (moderation) validated the theoretical construct of moderating variables such as physician’s habit persistence, cost and benefit ratio of the drug, and drug characteristics, which were derived from the theory of planned behavior (TPB) [
18,
19,
24,
74,
75,
76], theory of persuasion [
22,
29,
67,
68,
69,
70], and agency theory [
29,
37,
43,
62,
63,
64,
65,
66]. Moreover, physician’s habit persistence, and cost and benefit (side effects vs. cure effects) ratio of the drug have a significant moderating effect between the expectations of patients and the decision of physician to prescribe a medicine. The results further confirmed moderating variables such as DCH, CBR, and PHP that were extracted from TPB [
18,
19,
24,
74,
75,
76], theory of persuasion [
22,
29,
67,
68,
69,
70], and agency theory [
29,
37,
43,
62,
63,
64,
65,
66]. The outcomes of the indirect relationship (moderation) of trustworthiness, which was derived from the theory of planned behavior (TPB) [
18,
19,
24,
74,
75,
76], theory of persuasion [
22,
29,
67,
68,
69,
70], the theory of social power [
77,
78,
79,
80], and agency theory [
29,
37,
43,
62,
63,
64,
65,
66] were validated.
6. Conclusions
The undertaken study not only tests and validates the existing findings, but also enhances the current knowledge that is based on the foundation of a newly derived model in which 13 causal factors are classified and merged. Thus, the undertaken research is an attempt to empirically examine the intentions of physicians to prescribe a certain medicine based on different theories and models that were embedded into the considered model. The outcomes of this study concluded that marketing factors such as brands of the drug, sales promotion, drug information availability, and medical representatives’ effectiveness, as well as the characteristics of patient including patients’ expectations and patients’ request for a particular drug, and pharmacist factors, for instance pharmacist expert power and pharmacist physician collaborations, have a positive and significant influence on the decision of physician to prescribe a medicine. Thus, the outcomes of the direct relationship validated the theoretical construct such as attitude and marketing stimuli, which were derived from the theory of planned behavior (TPB). It is also concluded from the moderation analysis that physician’s habit persistence and cost and benefit (side effects vs. cure effects) ratio of the drug have played a significant moderating effect between medical representative effectiveness and the decision of physician to prescribe a certain medicine. However, drug characteristics do not have any moderating impact between the expectations of patients, and the decision of physicians to prescribe the medicine. Similarly, trustworthiness has a significant moderating effect between pharmacist–physician collaboration, and expert power of pharmacists and the decision of physician to prescribe a medicine. Finally, it is concluded that the considered conceptual model has been validated from the results of an undertaken study for both direct and indirect relationships amongst the variables. Hence, the outcomes of the undertaken research specify the new aspects that influence the physician’s prescription behavior towards a certain medicine. Hence, this study will also be beneficial to the marketers of the pharmaceutical industry to develop their effective and efficient marketing strategies to get maximum ROI of their investments.