Inequality in the Distribution of Healthcare Human Resources in Poland
Abstract
1. Introduction
2. Theory Background and Literature Review
3. The Characteristics of Polish Health Care System
4. Methodology
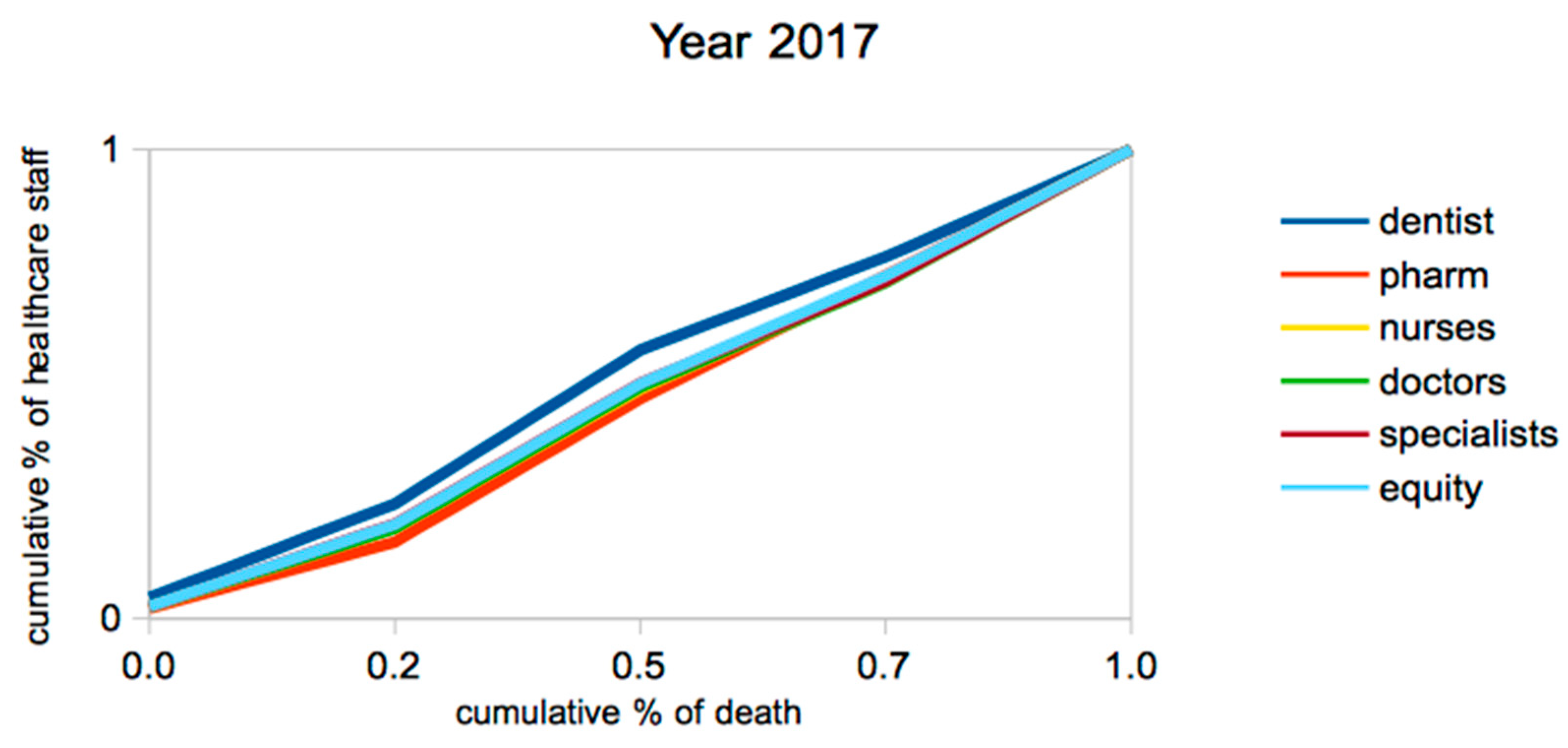
5. Results
6. Discussion
7. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Crisp, N. What would a sustainable health and care system look like? BMJ 2017, 358, j3895. [Google Scholar] [CrossRef] [PubMed]
- Bem, A.; Siedlecki, R.; Prędkiewicz, P.; Gazzola, P.; Ryszawska, B.; Ucieklak-Jeż, P. Hospitals’ Financial Health in Rural and Urban Areas in Poland: Does It Ensure Sustainability? Sustainability 2019, 11, 1932. [Google Scholar] [CrossRef]
- Kickbusch, I. The Food System—A Prism of Present and Future Challenges for Health Promotion and Sustainable Development; Triggering debate-White Paper; Health Promotion: Bern, Switzerland, 2010. [Google Scholar]
- Pantyley, V. Health inequalities among rural and urban population of Eastern Poland in the context of sustainable development. Ann. Agric. Environ. Med. 2017, 24, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Kabene, S.M.; Orchard, C.; Howard, J.M.; Soriano, M.A.; Leduc, R. The importance of human resources management in health care: A global context. Hum. Resour. Health 2006, 4, 20. [Google Scholar] [CrossRef]
- Dussault, G.; Dubois, C.-A. Human resources for health policies: A critical component in health policies. Hum. Resour. Health 2003, 1, 1. [Google Scholar] [CrossRef] [PubMed]
- WHO. A Universal Truth: No Health without a Workforce. Third Global Forum on Human Resources for Health Report. Available online: https://www.who.int/workforcealliance/knowledge/resources/hrhreport2013/en/ (accessed on 12 October 2018).
- Sowada, C.h.; Sagan, A.; Kowalska-Bobko, I. Poland Health System Review. Health Systems in Transition; European Observatory on Health Systems and Policies; WHO Regional Office for Europe: København, Denmark, 2019; Volume 21. [Google Scholar]
- OECD. Better Policies for Rural Development; OECD Publications: Paris, France, 1996. [Google Scholar]
- WCED. Our Common Future; Report of the World Commission on Environment and Development; Oxford University Press: Oxford, UK, 1987. [Google Scholar]
- Diesendorf, M. Sustainability and sustainable development. In Sustainability: The Corporate Challenge of the 21st Century; Dunphy, D., Benveniste, J., Griffiths, A., Sutton, P., Eds.; Allen & Unwin: Sydney, Australia, 2000; pp. 19–37. [Google Scholar]
- Ciegis, R.; Ramanauskiene, R.J.; Martinkus, B. The Concept of Sustainable Development and its Use for Sustainability Scenarios. Inz. Ekon. Eng. Econ. 2009, 2, 28–37. [Google Scholar]
- WHO. Constitution of the World Health Organization; World Health Organization: Geneva, Switzerland, 1948. [Google Scholar]
- McCartney, G.; Popham, F.; McMaster, R.; Cumbers, A. Defining health and health inequalities. Public Health 2019, 172, 22–30. [Google Scholar] [CrossRef]
- WHO. Making Fair Choices on the Path to Universal Health Coverage; Final report of the WHO Consultative Group on Equity and Universal Health Coverage; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Alsan, M.; Bloom, D.; Canning, D. The Effect of Population Health on Foreign Direct Investment; NBER Working Paper no.10596; National Bureau of Economic Research: Cambridge, MA, USA, 2004.
- Ríos-Osorio, L.A.; Zapata, W.A.S.; Ortiz-Lobato, M. Concepts Associated with Health from the Perspective of Sustainable Development. Saúde Soc. 2012, 21, 735–746. [Google Scholar] [CrossRef][Green Version]
- United Nations. Available online: https://www.un.org/sustainabledevelopment/development-agenda/ (accessed on 6 May 2019).
- Klarin, T. The Concept of Sustainable Development: From its Beginning to the Contemporary Issues. Zagreb Int. Rev. Econ. Bus. 2018, 21, 67–94. [Google Scholar] [CrossRef]
- Wong, Y.S.; Allotey, P.; Reidapth, D.D. Sustainable development goals, universal health coverage and equity in health systems: The Orang Asli commons approach. Glob. Health Epidemiol. Genom. 2016, 1, e12. [Google Scholar] [CrossRef]
- WHO. Arguing for Universal Health Coverage. World Health Organization 2013. Available online: https://apps.who.int/iris/handle/10665/204355 (accessed on 12 October 2018).
- Moreno-Serra, R.; Smith, P. The Effects of Health Coverage on Population Outcomes: A Country-Level Panel Data Analysis; Results for Development Institute: Washington, DC, USA, 2011. [Google Scholar]
- OECD. Universal Health Coverage and Health Outcomes; Final Report; OECD: Paris, France, 2016. [Google Scholar]
- Panteli, D.; Sagan, A. Health Systems in Transition Vol.13 No. 8 Poland. Health System Review. 2011 European Observatory on Health Systems and Policies. Available online: http://www.euro.who.int/__data/assets/pdf_file/0018/163053/e96443.pdf (accessed on 12 October 2018).
- Whitehead, M. The Concepts and Principles of Equity and Health. Available online: http://salud.ciee.flacso.org.ar/flacso/optativas/equity_and_health.pdf (accessed on 12 October 2018).
- Bem, A.; Ucieklak-Jeż, P.; Siedlecki, R. The Spatial Differentiation of the Availability of Health Care in Polish Regions. Procedia Soc. Behav. Sci. 2016, 220, 12–20. [Google Scholar] [CrossRef]
- Backman, G.; Hunt, P.; Khosla, R.; Jaramillo-Strouss, C.; Fikre, B.M.; Rumble, C.; Pevalin, D.; Paez, D.A.; Pineda, M.A.; Frisancho, A.; et al. Health systems and the right to health: An assessment of 194 countries. Lancet 2008, 372, 2047–2085. [Google Scholar] [CrossRef]
- EC 2019. Available online: https://ec.europa.eu/health/workforce/overview_en (accessed on 15 June 2019).
- The World Health Report 2000—Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000.
- Becker, G.S. Human capital. A Theoretical and Empirical Analysis with Special Reference to Education, 3rd ed.; The University of Chicago Press: Chicago, IL, USA, 1993. [Google Scholar]
- Scrutton, J.; Holley-Moore, G.; Bamford, S.M. Creating a Sustainable 21st Century Healthcare System; The International Longevity Centre–UK: London, UK, 2015. [Google Scholar]
- Prada, G.; Grimes, K.; Sklokin, I. Defining Health and Health Care Sustainability; The Conference Board of Canada: Ottawa, ON, Canada, 2014. [Google Scholar]
- Romanelli, M. Towards Sustainable Health Care Organizations. Manag. Dyn. Knowl. Econ. 2017, 5, 377–394. [Google Scholar] [CrossRef]
- Domagała, A.; Klich, J. Planning of Polish physician workforce—Systemic inconsistencies, challenges and possible ways forward. Health Policy 2018, 122, 102–108. [Google Scholar] [CrossRef]
- Folland, S.; Goodman, A.C.; Stano, M. The Economics of Health and Health Care; Macmillan Publishing Company: New York, NY, USA, 1993. [Google Scholar]
- Dussault, G.; Franceschini, M.C. Not enough there, too many here: Understanding geographical imbalances in the distribution of the health workforce. Hum. Resour. Health 2006, 4, 12. [Google Scholar] [CrossRef]
- European Commission. Commission Staff Working Document on an Action Plan for the EU Health Workforce. SWD (2012) 93 Final. Strasbourg: EC; 18 April 2012. Available online: https://ec.europa.eu/health/sites/health/files/workforce/docs/staff_working_doc_healthcare_workforce_en.pdf (accessed on 20 September 2019).
- Wismar, M.; Maier, C.B.; Glinos, I.A.; Dussault, G.; Figueras, J. Health Professional Mobility and Health Systems in Europe. Evidence from 17 European Countires; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2011. [Google Scholar]
- Kuhlmann, E.; Batenburg, R.; Groenewegen, P.; Larsen, C.H. Bringing a European perspective to the health human resources debate: A scoping study. Health Policy 2013, 110, 6–13. [Google Scholar] [CrossRef]
- Kroezen, M.; Dussault, G.; Craveiro, I.; Dieleman, M.; Jansen, C.H.; Buchan, J.; Barriball, L.; Rafferty, A.M.; Bremner, J.; Sermeu, W. Recruitment and retention of health professionals across Europe: A Literature review and multiple case study research. Health Policy 2015, 119, 1517–1528. [Google Scholar] [CrossRef]
- Buchan, J.; Twigg, D.; Dussault, G.; Duffield, C.H.; Stone, P.W. Policies to sustain the nursing workforce: An international perspective. Int. Nurs. Rev. 2015, 62, 162–170. [Google Scholar] [CrossRef]
- Sarkis, N.; Mwanri, L. The role of information technology in strengthening human resources for health: The case of the Pacific Open Learning Health Network. Health Educ. 2013, 114, 67–79. [Google Scholar] [CrossRef]
- Dussault, G.; Buchan, J.; Sermeus, W.; Padaiga, Z. Assessing Future Health Workforce Needs; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Mantzavinis, G.; Theodorakis, P.N.; Lionis, C.h.; Trell, E. Geographical inequalities in the distribution of general practitioners in Sweden. Lakartidningen 2003, 100, 4294–4297. [Google Scholar]
- Theodorakis, P.; Mantzavinis, G. Inequalities in the distribution of rural primary care physicians in two remote neighboring prefectures of Greece and Albania. Rural Remote Health 2005, 5, 457. [Google Scholar]
- Theodorakis, P.; Mantzavinis, G.; Rrumbullaku, L.; Lionis, C.; Trell, E. Measuring health inequalities in Albania: A focus on the distribution of general practitioners. Hum. Resour. Health 2006, 4, 5. [Google Scholar] [CrossRef]
- Johnston, G.; Wilkinson, D. Increasingly inequitable distribution of general practitioners in Australia, 1986–1996. Aust. New Zealand J. Public Health 2001, 25, 66–70. [Google Scholar] [CrossRef]
- Matsumoto, M.; Inoue, K.; Bowman, R.; Kajii, E. Self-employment, specialty choice, and geographical distribution of physicians in Japan: A comparison with the United States. Health Policy 2010, 96, 239–244. [Google Scholar] [CrossRef]
- Gravelle, H.; Sutton, M. Inequality in the geographical distribution of general practitioners in England and Wales 1974–1995. J. Health Serv. Res. Policy 2001, 6, 6–13. [Google Scholar] [CrossRef]
- Pallikadavath, S.; Singh, A.; Ogollah, R.; Dean, T.; Stones, W. Human resource inequalities at the base of India’s public health care system. Health Place 2013, 23, 26–32. [Google Scholar] [CrossRef]
- Erdenee, O.; Paramita, S.A.; Yamazaki, C.h.; Koyama, H. Distribution of health care resources in Mongolia using the Gini coefficient. Hum. Resour. Health 2017, 15, 56. [Google Scholar] [CrossRef]
- Rabbanikhah, F.; Moradi, R.; Mazaheri, E.; Shahbazi, S.; Barzegar, L.; Karyani, A.K. Trends of geographic distribution of general practitioners in the public health sector of Iran. J. Educ. Health Promot. 2018, 7, 89. [Google Scholar]
- Mobaraki, H.; Hassani, A.; Kashkalani, T.; Khalilnejad, R.; Chimeh, E.E. Equality in Distribution of Human Resources: The Case of Iran’s Ministry of Health and Medical Education. Iran. J. Public Health 2013, 42 (Suppl. 1), 161–165. [Google Scholar]
- Sefiddashti, S.A.; Arab, M.; Ghazanfari, S.; Kazemi, Z.; Rezaei, S.; Karyani, A.K. Trends of geographic inequalities in the distribution of human resources in healthcare system: The case of Iran. Electron. Physician 2016, 8, 2607–2613. [Google Scholar] [CrossRef]
- Paramita, S.A.; Yamazaki, C.h.; Koyama, H. Distribution trends of Indonesia’s health care resources in the decentralization era. Int. J. Health Plan. Manag. 2018, 33, e586–e596. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Zhou, Z.; Si, Y.; Xu, Y.; Shen, C.h.; Wang, Y.; Wang, X. Unequal distribution of health human resources in mainland China:what are the determinants from a comprehensive perspective? Int. J. Equity Health 2018, 17, 29. [Google Scholar] [CrossRef]
- Wu, J.; Yang, Y. Inequality trends in the demographic and geographic distribution of health care professionals in China: Data from 2002 to 2016. Int. J. Health Plan. Manag. 2019, 34, e487–e508. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Zeng, J. Inequalities in the geographic distribution of hospital beds and doctors in traditional Chinese medicine from 2004 to 2014. Int. J. Equity Health 2018, 17, 165. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Xu, Y.; Ren, J.; Sun, L.; Liu, C. Inequality in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Wang, J.; Ma, X.; Wang, Y.; Li, R. Equality of medical health resource allocation in China based on the Gini coefficient method. Iran J. Public Health 2015, 44, 445–457. [Google Scholar]
- Kobayashi, Y.; Takaki, H. Geographic distribution of physicians in Japan. Lancet 1992, 340, 1391–1393. [Google Scholar] [CrossRef]
- Toyabe, S. Trend in geographic distribution of physicians in Japan. Int. J. Equity Health 2009, 8, 5. [Google Scholar] [CrossRef]
- Munga, M.A.; Maestad, O. Measuring inequalities in the distribution of health workers: The case of Tanzania. Hum. Resour. Health 2009, 7, 4. [Google Scholar] [CrossRef]
- Wiseman, V.; Lagarde, M.; Batura, N.; Lin, S.; Irava, W.; Roberts, G. Measuring inequalities in the distribution of the Fiji Health Workforce. Int. J. Equity Health 2017, 16, 115. [Google Scholar] [CrossRef]
- Tandi, T.E.; Cho, Y.M.; Akam, A.J.-C.; Afoh, C.h.O.; Ryu, S.H.; Choi, M.S.; Kim, K.H.; Choi, J.W. Cameroon public health sector: Shortage and inequalities in geographic distribution of health personnel. Int. J. Equity Health 2015, 14, 43. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.C. Using Gini-style indices to evaluate the spatial patterns of health practitioners: Theoretical considerations and an application based on Alberta data. Soc. Sci. Med. 1994, 38, 1243–1256. [Google Scholar] [CrossRef]
- Correia, I.; Veiga, P. Geographic distribution of physicians. Port. Eur. J. Health Econ. 2010, 11, 383–393. [Google Scholar]
- Busch, L.; Dale, C. The changing distribution of physicians. Socio Econ. Plan. Sci. 1978, 12, 167–176. [Google Scholar] [CrossRef]
- Shinjo, D.; Toshiharu, A. Geographic distribution of healthcare resources, healthcare service provision, and patient flow in Japan: A cross sectional study. Soc. Sci. Med. 2012, 75, 1954–1963. [Google Scholar] [CrossRef] [PubMed]
- Sanders, L.J.; Bacon, C.J.; Aguilar, G.D. A spatial analysis of the geographic distribution of musculoskeletal and general practice healthcare clinics in Auckland, New Zealand. Appl. Geogr. 2013, 44, 69–78. [Google Scholar] [CrossRef]
- Buchan, J.; Perfilieva, G. Making Progress towards Health Workforce Sustainability in the WHO European Region; WHO Regional Office for Europe: København, Copenhagen, 2015. [Google Scholar]
- Negev, M.; Davidovitch, N.; Garb, Y.; Tal, A. Stakeholder participation in health impact assessment: A multicultural approach. Environ. Impact Assess. Rev. 2013, 43, 112–120. [Google Scholar] [CrossRef]
- Lee, K.; Pang, T. WHO: Retirement or reinvention? Public Health 2014, 128, 119–123. [Google Scholar] [CrossRef]
- WHO. Report from the Ministerial Summit on Health Research: Identify Challenges, Inform Actions, Correct Inequities. 2005. Available online: https://apps.who.int/iris/handle/10665/43226 (accessed on 21 May 2019).
- WHO. Human Resources for Health in the WHO European Region; WHO Regional Office for Europe: København, Copenhagen, 2006. [Google Scholar]
- WHO. Global Health Workforce Alliance. 2016. Available online: www.who.int/workforcealliance (accessed on 21 May 2019).
- European Commission. Green Paper on the European Workforce for Health. European Commission. COM. (2008) 725 Final. Brussels, 10 December 2008. Available online: https://ec.europa.eu/health/ph_systems/docs/workforce_gp_en.pdf (accessed on 30 June 2019).
- WHO. Global Atlas of the Health Workforce. 2009. Available online: http://apps.who.int/globalatlas/default.asp (accessed on 30 June 2019).
- WHO. Global CODE of Practice on the International Recruitment of Health Personnel. 2017. Available online: http://www.who.int/hrh/migration/code/codeen.pdf?ua=1 (accessed on 30 June 2019).
- European Commission. Green Paper on Modernising the Professional Qualifications Directive. European Commission. COM. (2011) 367 Final. Brussels, 22 June 2011. Available online: https://ec.europa.eu/transparency/regdoc/rep/1/2011/EN/1-2011-941-EN-F1-1.Pdf (accessed on 30 June 2019).
- WHO. Global Strategy on Human Resources for Health: Workforce 2030. Geneva Switzerland. Available online: https://www.who.int/hrh/resources/globstrathrh-2030/en/ (accessed on 10 July 2019).
- Paulo, M.S.; Loney, T.; Lapão, L.V. How do we strengthen the health workforce in a rapidly developing high-income country? A case study of Abu Dhabi’s health system in the United Arab Emirates. Hum. Resour. Health 2019, 17, 9. [Google Scholar] [CrossRef]
- European Commission Health and Consumer Directorate-General. Action Plan for the EU Health Workforce. Available online: http://ec.europa.eu/health/workforce/policy/indexen.htm (accessed on 10 July 2019).
- Brommels, M.; Jaaskelainen, M. Measures of equity and efficiency in medical manpower planning. A prediction of internists needed in the Finnish national-health service. Health Policy 1984, 4, 3–11. [Google Scholar] [CrossRef]
- Jaaskelainen, M.; Brommels, M. The demand for physicians in Finland: Results from a speciality-based assessment of future development and need for service. Health Policy 1985, 5, 331–338. [Google Scholar] [CrossRef]
- Dubois, C.-A.; McKee, M.; Nolte, E. Human Resources for Health in Europe 2006; European Observatory on Health Systems and Policies series; Open University Press: Geneva, Switzerland, 2006. [Google Scholar]
- Malgieri, A.; Michelutti, P.; Van Hoegaerden, M. The Handbook on Health Workforce Planning Methodologies Across EU Countries; Ministry of Health of the Slovak Republic: Bratislava, Slovak Republic, 2015.
- Ono, T.; Lafortune, G.; Schoenstein, M. Health Workforce Planning in OECD Countries: A Review of 26 Projection Models from 18 Countries; OECD Health Working Papers, No. 62; OECD Publishing: Paris, France, 2013. [Google Scholar]
- WHO. Health Workforce Requirements for Universal Health Coverage and the Sustainable Development Goals. Human Resources for Health Observer, 2018, Issue No. 17. Available online: https://www.who.int/hrh/resources/health-observer17/en/ (accessed on 12 October 2018).
- Bem, A.; Ucieklak-Jeż, P.; Siedlecki, R. Effects of inequalities in access to health services in rural areas in Poland. Manag. Theory Stud. Rural Bus. Infrastruct. Dev. 2013, 35, 491–497. [Google Scholar]
- Ucieklak-Jeż, P.; Bem, A. Wpływ niefinansowych zasobów systemu ochrony zdrowia na stan zdrowia kobiet i mężczyzn w Polsce (The Effect of Non-financial Reserves of the Health Protection System on the State of Health of Women and Men in Poland). Prace Naukowe Akademii im Jana Długosza w Częstochowie. Pragmata Tes Oikonomias 2015, 9, 157–171. [Google Scholar]
- Haczyński, J.; Skrzypczak, Z.; Winter, M. Nurses in Poland—Immediate action needed. Eng. Manag. Prod. Serv. 2017, 9, 97–104. [Google Scholar] [CrossRef]
- Haczyński, J.; Ryć, K.; Skrzypczak, Z.; Suchecka, J. Physician Resources in the Health System—Comparison of Poland and Selected European Countries. Probl. Zarz. 2017, 15, 53–66. [Google Scholar]
- Polish Statistical Yearbook. Statistics Poland. Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/powierzchnia-i-ludnosc-w-przekroju-terytorialnym-w-2018-roku,7,15.html (accessed on 12 October 2018).
- NIL. Lekarze i Lekarze Dentyści w Polsce—Charaterystyka Demograficzna in 2017 [Doctors and Dentists in Poland—Demographic Characteristics in 2017]; Naczelna Izba Lekarska [National Chamber of Physician]: Warsaw, Poland, 2018; Available online: https://nil.org.pl/__data/assets/pdf_file/0014/132521/Demografia-2017.pdf (accessed on 20 July 2019).
- Mokrzycka, A.; Kowalska-Bobko, I.; Sagan, A.; Włodarczyk, W.C. The 2014 primary healthcare reform in Poland: Short-term fixes instead of a long-term strategy. Health Policy 2016, 120, 1226–1232. [Google Scholar] [CrossRef]
- OECD. Health at a Glance: Europe 2018: State of Health in the EU Cycle; OECD Publishing: Paris, France, 2018. [Google Scholar]
- The Constitution of the Republic of Poland of 2nd April, 1997, as Published in Dziennik Ustaw No.78, item 483. Available online: https://www.sejm.gov.pl/prawo/konst/angielski/kon1.htm (accessed on 6 April 2019).
- Rój, J. The Cost Efficiency of Hospitals in Poland. In Themes on Health Care: Challenges and Future Actions; Boutsioli, Z., Ed.; ATINER: Athens, Greece, 2009. [Google Scholar]
- The 1997 General Health Insurance Act. Available online: https://www.legislation.gov.au/Details/C2004A05239 (accessed on 12 June 2019).
- Rój, J. Relationship between Funding Mechanism and Service Effectiveness of Hospital. In The Economics of Health Reforms; ATINER: Athens, Greece, 2004. [Google Scholar]
- Rój, J. Productivity of university hospitals in Poland: A Malmquist-index approach. Ekonomika 2010, 89, 131–142. [Google Scholar] [CrossRef]
- Kuszewski, K.; Gericke, C.H. Health Systems in Transitions Poland; WHO: Geneva, Switzerland, 2005. [Google Scholar]
- Sagan, A.; Sobczak, A. Implementation of the 2011 Therapeutic Activity Act: Will commercialization improve the financial performance of Polish hospitals? Health Policy 2014, 118, 153–158. [Google Scholar] [CrossRef]
- The Act of 27 August 2004 About Health Care Benefits Financed from Public Funds. Available online: https://www.global-regulation.com/translation/poland/3353836/the-act-of-27-august-2004-about-health-care-benefits-financed-from-public-funds.html (accessed on 19 June 2019).
- Rój, J. Competition measurement of hospitals in Poland: The Herfindahl-Hirschman Index approach. Ekonomika 2016, 95, 166–181. [Google Scholar] [CrossRef]
- Knowledge Database Health and Health Care of Statistic Poland. Statistics Poland. Available online: http://swaid.stat.gov.pl/ZdrowieOchronaZdrowia_dashboards/Raporty_predefiniowane/RAP_DBDZDR_5.aspx (accessed on 12 October 2018).
- Druckman, A.; Jackson, T. Measuring resource inequalities: The concepts and methodology for an area-based gini coefficient. Ecol. Econ. 2008, 65, 242–252. [Google Scholar] [CrossRef]
- Wagstaff, A.; Paci, P.; Van Doorslaer, E. On the measurement of inequalities in health. Soc. Sci. Med. 1991, 33, 545–557. [Google Scholar] [CrossRef]
- Gini, C. Variabilita e mutabilita 1912 reprinted. In Memorie di Metodologica Statistica; Pizetti, E., Salvemini, T., Eds.; Libreria Eredi Virgilio Veschi: Rome, Italy, 1955. [Google Scholar]
- Gini, C. On the measurement of concentration and variability of characters. Metron Int. J. Stat. 2005, LXIII, 1–38. [Google Scholar]
- Theil, H. Economics and Information Theory; North Holland Publishing Company: Amsterdam, The Netherlands, 1967. [Google Scholar]
- Zhu, B.; Hsieh, C.h.W.; Zhang, Y. Incorporating Spatial Statistics into Examining Equity in Health Workforce Distribution: An Empirical Analysis in the Chinese Context. Int. J. Environ. Res. Public Health 2018, 15, 1309. [Google Scholar] [CrossRef] [PubMed]
- Anand, S. Measuring Health Workforce Inequalities: Methods and Application to China and India; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Sousa, A.; Dal Poz, M.R.; Carvalho, C.L. Monitoring inequalities in the health workforce: The case study of Brazil 1991–2005. PLoS ONE 2012, 7, e33399. [Google Scholar] [CrossRef]
- Ucieklak-Jeż, P.; Bem, A. Dostępność opieki zdrowotnej na obszarach wiejskich w Polsce (Availability of health care in rural areas in Poland). Probl. Drob. Gospod. Rol. Probl. Small Agric. Hold. 2017, 4, 117–131. [Google Scholar]
- EU. The Joint Action on Health Workforece Planning. Available online: http://www.euro.who.int/en/health-topics/Health-systems/health-workforce/news/news/2016/06/completion-of-the-eu-joint-action-on-health-workforce-planning-and-forecasting (accessed on 18 June 2019).
- NIK. Kształcenie i Przygotowanie Zawodowe Kadr Medycznych [Training and Professional Development of Medical Staff]; Najwyzsza Izba Kontroli [The Polish Supreme Audit Office]: Warsaw, Poland, 2016. Available online: https://www.nik.gov.pl/plik/id,10242,vp,12565.pdf (accessed on 14 July 2019).
- WHO. Models and Tools for Health Workforce Planning and Projections; Human Resources for Health Observer 3; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
| Authors | Range of Research | Methods |
|---|---|---|
| Mantzavinis, G., Theodorakis, P. N., Lionis, Ch. and Trell, E. | trends in the inequalities in the distribution of general practitioners in Sweden [44]; | Lorenz Curve; Gini coefficients; |
| Theodorakis, P.N., Mantzavinis, G.D., Rrumbullaku, L., Lionis, C., and Trell, E. | equity in distribution of primary care physician using population per physician ratio; comparison between Ioannina prefecture in Greece and Gjirokaster prefecture in Albania [45]; | Gini coefficient; |
| Theodorakis, P.N., Mantzavinis, G.D., Rrumbullaku, L., Lionis, C., and Trell, E. | distribution of general practitioners with adjustment for mortality and consultation rates [46]; | Gini coefficient; Atkinson and Robin Hood indices; decile ratios; |
| Johnston, G. and Wilkinson, D. | distribution of general practitioners (GPs) in Australia adjusted for community need (population size and crude mortality) [47]; | Robin Hood Index; |
| Matsumoto, M., Inoue, K., Farmer, J., Inada, H. and Kajii, E. | geographic distribution of the physicians in each specialty and their associations with physician employment status in Japan, in comparison with the US [48]; | Gini coefficient; correlations; |
| Gravelle, H. and Sutton, M. | comparison of geographical inequality in the distribution of general practitioners (GPs), other resources and mortality in England and Wales [49]; | decile ratio; Gini coefficient; Atkinson index; standard deviation; |
| Pallikadavath, S., Singh, A., Ogollah, R., Dean, T. and Stones, W. | the extent of inequalities in human resource provision at India’s Heath Sub-Centres (HSC) [50]; | Gini coefficient; Theil index; |
| Erdenee, O., Paramita, S.A., Yamazaki, Ch. and Koyama, H. | comparison of the distributions of health care resources (physicians, nurses, and hospital beds) in urban, suburban, and rural areas of Mongolia [51]; | Mann-Whitney U test; Gini coefficient; |
| Rabbanikhah, F., Moradi, R., Mazaheri, E., Shahbazi, S., Barzegar, L. and Karyani, A.K. | geographical distribution of GPs in public health sector in Iran [52]; | descriptive statistics; Gini coefficient; |
| Mobaraki, H., Hassani, A., Kashkalani, T., Khalilnejad, R., and Chimeh, E.E. | equity of human resources’ distribution among Iran’s medical science universities [53]; | Gini coefficient; Robin hood indexes; |
| Sefiddashti, S.E., Mohammad Arab, M., Ghazanfari, S., Kazemi, Z., Rezaei, S., and Karyani, A.K. | inequality of in the allocation of human resources in the health sector in Teheran (specialists, general practitioners, pharmacists, paramedics, dentists, nurses and community health workers) [54]; | Gini coefficient; regression analysis; dissimilarity index; |
| Paramita, S.A. Yamazaki, Ch., and Koyama, H. | distribution trends of physicians, puskesmas (community health centers), hospitals, and hospital beds in Indonesia [55]; | Gini coefficient; |
| Li, D., Zhou, Z., Si Y., Xu Y., Shen Ch., Wang, Y. and Wang X. | distribution inequality of health human resources (doctors and nurses) in China; quantification of the contribution of economic-status to the total inequality [56]; | Concentration Index; |
| Wu. J. and Yang, Y. | trends in the demographic and geographic distribution inequality of healthcare professionals (nurses and physicians) in China; contributions by intra-regional and inter-regional differences on total inequality in China [57]; | Gini coefficient; Theil index; |
| Lu, L. and Zeng. J. | geographic and population distribution of hospital beds and doctors across different regions in China [58]; | Moran’s index local Moran’s index; Gini coefficient; Pearson correlation; |
| Zhang, T., Xu, Y., Ren, J., Sun, L. and Liu, C. | distribution of numbers of institutions, health workers and beds; and outcomes such as per capita outpatient visits and annual hospitalization rates in China [59]; | Gini coefficient; Concentration Index; |
| Jin, J., Wang, J., Ma, X., Wang, Y. and Li, R. | distribution of health care institutions, beds, medical personnel in China [60]; | Gini Coefficient; |
| Kobayashi, Y. and Takaki, H. | geographic distribution of physicians in Japan [61]; | Gini coefficient; Lorenz Curve; |
| Toyabe, S. | time trends in number and distribution of physicians (according to place of working as general hospitals, university hospitals and clinics) in Japan [62]; | Gini coefficient; Atkinson index; Theil index; |
| Munga, M.A. and Maestad, O. | inequalities in the distribution of health workers in Tanzania [63]; | Lorenz Curve/ Gini coefficient; concentration index |
| Wiseman, V., Lagarde, M., Batura, N., Lin, S., Irava, W. and Roberts G. | equity in the distribution of three categories of health workers: doctors, nurses, and all health workers (doctors, nurses, dentists and health support staff); population size and crude death rates are used as proxies for health care needs in Fiji [64]; | Lorenz Curve/ Gini coefficient; Theil Index; |
| Tandi, T.E., Cho, Y.M., Akam, A.J-C., Afoh, Ch.O., Ryu, S.H., Choi, M.S., Kim, K.H. and Choi, J.W. | inequalities in the distribution of physicians, nurses and paramedics in Cameroon; comparison with outcome maternal mortality, under-five infant mortality and measles immunization coverage [65]; | Gini coefficient Lorenz curve; linear regression; concentration curves; |
| Year | Physician | Dentist | Nurse | Pharmacist |
|---|---|---|---|---|
| 2010 | 20.6 | 3.2 | 47.9 | 6.5 |
| 2011 | 20.9 | 3.3 | 48.4 | 6.8 |
| 2012 | 22.1 | 3.2 | 54.9 | 7.0 |
| 2013 | 22.1 | 3.2 | 52.1 | 7.1 |
| 2014 | 22.7 | 3.4 | 51.7 | 7.2 |
| 2015 | 23.0 | 3.3 | 51.4 | 7.3 |
| 2016 | 23.9 | 3.5 | 51.0 | 7.6 |
| 2017 | 23.5 | 3.5 | 50.4 | 7.6 |
| change | 14.08% | 9.38% | 5.22% | 16.92% |
| Year | Physician | Dentist | Nurse | Pharmacist |
|---|---|---|---|---|
| 2010 | 0.254 | 0.039 | 0.591 | 0.080 |
| 2011 | 0.257 | 0.041 | 0.597 | 0.084 |
| 2012 | 0.272 | 0.040 | 0.677 | 0.086 |
| 2013 | 0.273 | 0.039 | 0.642 | 0.088 |
| 2014 | 0.280 | 0.042 | 0.637 | 0.089 |
| 2015 | 0.283 | 0.040 | 0.631 | 0.090 |
| 2016 | 0.293 | 0.043 | 0.626 | 0.094 |
| 2017 | 0.289 | 0.043 | 0.619 | 0.094 |
| change | 13.80% | 8.15% | 4.85% | 16.76% |
| Year | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Change * |
|---|---|---|---|---|---|---|---|---|---|
| specialist in general | 13.81 | 15.20 | 15.16 | 15.01 | 15.47 | 15.60 | 15.84 | 15.64 | 13.26% |
| anesthesiologist | 0.78 | 0.80 | 0.89 | 0.92 | 0.97 | 0.96 | 0.96 | 0.96 | 23.06% |
| cardiologist | 0.45 | 0.47 | 0.53 | 0.55 | 0.63 | 0.71 | 0.76 | 0.76 | 67.44% |
| dermatologist | 0.23 | 0.23 | 0.25 | 0.24 | 0.23 | 0.24 | 0.25 | 0.23 | 1.34% |
| family medicine | 1.57 | 1.62 | 1.69 | 1.67 | 1,73 | 1.73 | 1.75 | 1.75 | 11.92% |
| internist | 1.84 | 1.87 | 1.94 | 1.86 | 1.80 | 1.74 | 1.72 | 1.66 | −10.00% |
| lung diseases | 0.33 | 0.34 | 0.36 | 0.35 | 0.35 | 0.36 | 0.35 | 0.33 | 0.48% |
| neurologist | 0.54 | 0.58 | 0.62 | 0.60 | 0.54 | 0.62 | 0.64 | 0.63 | 15.32% |
| obstetrics and gynecology | 1.01 | 1.01 | 1.02 | 0.99 | 1.00 | 0.99 | 1.02 | 0.97 | −4.13% |
| occupational medicine | 0.21 | 0.22 | 0.21 | 0.20 | 0.16 | 0.19 | 0.21 | 0.21 | −1.06% |
| oncologist | 0.09 | 0.10 | 0.12 | 0.13 | 0.13 | 0.18 | 0.19 | 0.19 | 115.51% |
| ophthalmologist | 0.46 | 0.47 | 0.51 | 0.49 | 0.52 | 0.53 | 0.53 | 0.52 | 14.26% |
| otolaryngology | 0.33 | 0.33 | 0.34 | 0.34 | 0.32 | 0.34 | 0.35 | 0.35 | 5.34% |
| pediatrician | 0.84 | 0.84 | 0.84 | 0.84 | 0.86 | 0.88 | 0.94 | 0.93 | 10.67% |
| psychiatrist | 0.52 | 0.58 | 0.60 | 0.62 | 0.59 | 0.65 | 0.64 | 0.64 | 22.47% |
| radiologist | 0.51 | 0.52 | 0.59 | 0.59 | 0.59 | 0.60 | 0.58 | 0.59 | 15.96% |
| surgeon | 1.94 | 1.98 | 2.18 | 2.13 | 2.20 | 2.21 | 2.24 | 2.18 | 12.45% |
| Year | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Change * |
|---|---|---|---|---|---|---|---|---|---|
| specialist in general | 0.169 | 0.173 | 0.187 | 0.185 | 0.190 | 0.192 | 0.195 | 0.192 | 14.05% |
| anesthesiologist | 0.010 | 0.010 | 0.011 | 0.011 | 0.012 | 0.012 | 0.012 | 0.012 | 23.92% |
| cardiologist | 0.006 | 0.006 | 0.006 | 0.007 | 0.008 | 0.009 | 0.009 | 0.009 | 68.60% |
| dermatologist | 0.003 | 0.003 | 0.003 | 0.003 | 0.003 | 0.003 | 0.003 | 0.003 | 2.04% |
| family medicine | 0.019 | 0.020 | 0.021 | 0.021 | 0.021 | 0.021 | 0.022 | 0.022 | 12.70% |
| internist | 0.022 | 0.023 | 0.024 | 0.023 | 0.022 | 0.020 | 0.021 | 0.020 | −9.37% |
| lung diseases | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 1.18% |
| neurologist | 0.007 | 0.007 | 0.008 | 0.007 | 0.007 | 0.008 | 0.008 | 0.008 | 16.12% |
| obstetrics and gynecology | 0.012 | 0.012 | 0.013 | 0.012 | 0.012 | 0.012 | 0.013 | 0.012 | −3.46% |
| occupational medicine | 0.003 | 0.003 | 0.003 | 0.002 | 0.002 | 0.002 | 0.003 | 0.003 | −0.37% |
| oncologist | 0.001 | 0.001 | 0.002 | 0.002 | 0.002 | 0.002 | 0.002 | 0.002 | 117.01% |
| ophthalmologist | 0.006 | 0.006 | 0.006 | 0.006 | 0.006 | 0.006 | 0.006 | 0.006 | 15.06% |
| otolaryngology | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 0.004 | 6.07% |
| pediatrician | 0.010 | 0.010 | 0.010 | 0.010 | 0.011 | 0.011 | 0.012 | 0.011 | 11.44% |
| psychiatrist | 0.006 | 0.007 | 0.007 | 0.008 | 0.007 | 0.008 | 0.008 | 0.008 | 23.33% |
| radiologist | 0.006 | 0.006 | 0.007 | 0.007 | 0.007 | 0.007 | 0.007 | 0.007 | 16.77% |
| surgeon | 0.024 | 0.024 | 0.027 | 0.026 | 0.027 | 0.027 | 0.028 | 0.027 | 13.23% |
| Year | Physician | Dentist | Nurse | Pharmacist |
|---|---|---|---|---|
| 2010 | 0.08 | 0.16 | 0.06 | 0.11 |
| 2011 | 0.08 | 0.17 | 0.06 | 0.10 |
| 2012 | 0.08 | 0.16 | 0.04 | 0.10 |
| 2013 | 0.07 | 0.16 | 0.05 | 0.09 |
| 2014 | 0.07 | 0.14 | 0.05 | 0.09 |
| 2015 | 0.07 | 0.14 | 0.06 | 0.09 |
| 2016 | 0.07 | 0.13 | 0.06 | 0.09 |
| 2017 | 0.06 | 0.14 | 0.07 | 0.09 |
| Year | Physician | Dentist | Nurse | Pharmacist |
|---|---|---|---|---|
| 2010 | 0.30 | 0.26 | 0.30 | 0.32 |
| 2011 | 0.30 | 0.27 | 0.30 | 0.32 |
| 2012 | 0.30 | 0.27 | 0.28 | 0.32 |
| 2013 | 0.29 | 0.26 | 0.28 | 0.31 |
| 2014 | 0.29 | 0.25 | 0.29 | 0.32 |
| 2015 | 0.30 | 0.29 | 0.29 | 0.31 |
| 2016 | 0.30 | 0.29 | 0.29 | 0.31 |
| 2017 | 0.30 | 0.27 | 0.29 | 0.30 |
| Year | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|
| specialist in general | 0.07 | 0.08 | 0.07 | 0.07 | 0.07 | 0.07 | 0.07 | 0.06 |
| anesthesiologist | 0.07 | 0.07 | 0.06 | 0.08 | 0.07 | 0.07 | 0.06 | 0.07 |
| cardiologist | 0.15 | 0.15 | 0.14 | 0.21 | 0.15 | 0.14 | 0.15 | 0.18 |
| dermatologist | 0.12 | 0.14 | 0.12 | 0.15 | 0.12 | 0.12 | 0.13 | 0.12 |
| family medicine | 0.22 | 0.22 | 0.20 | 0.21 | 0.19 | 0.19 | 0.19 | 0.18 |
| internist | 0.11 | 0.12 | 0.10 | 0.10 | 0.12 | 0.12 | 0.12 | 0.12 |
| lung diseases | 0.14 | 0.11 | 0.11 | 0.10 | 0.08 | 0.07 | 0.08 | 0.08 |
| neurologist | 0.10 | 0.11 | 0.11 | 0.11 | 0.10 | 0.10 | 0.10 | 0.10 |
| obstetrics and gynecology | 0.08 | 0.09 | 0.08 | 0.09 | 0.08 | 0.08 | 0.09 | 0.09 |
| occupational medicine | 0.19 | 0.22 | 0.22 | 0.24 | 0.23 | 0.20 | 0.21 | 0.18 |
| oncologist | 0.25 | 0.27 | 0.23 | 0.19 | 0.21 | 0.19 | 0.15 | 0.16 |
| ophthalmologist | 0.12 | 0.12 | 0.11 | 0.13 | 0.12 | 0.12 | 0.12 | 0.10 |
| otolaryngology | 0.09 | 0.08 | 0.09 | 0.10 | 0.09 | 0.08 | 0.09 | 0.11 |
| pediatrician | 0.10 | 0.08 | 0.09 | 0.10 | 0.09 | 0.09 | 0.10 | 0.10 |
| psychiatrist | 0.14 | 0.13 | 0.13 | 0.12 | 0.12 | 0.12 | 0.12 | 0.09 |
| radiologist | 0.15 | 0.15 | 0.15 | 0.11 | 0.13 | 0.13 | 0.13 | 0.11 |
| surgeon | 0.05 | 0.05 | 0.05 | 0.06 | 0.06 | 0.06 | 0.06 | 0.06 |
| Year | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|
| specialist in general | 0.29 | 0.29 | 0.28 | 0.29 | 0.29 | 0.29 | 0.29 | 0.29 |
| anesthesiologist | 0.29 | 0.30 | 0.29 | 0.29 | 0.30 | 0.29 | 0.28 | 0.30 |
| cardiologist | 0.37 | 0.38 | 0.37 | 0.37 | 0.37 | 0.38 | 0.37 | 0.37 |
| dermatologist | 0.27 | 0.29 | 0.26 | 0.28 | 0.27 | 0.27 | 0.25 | 0.26 |
| family medicine | 0.39 | 0.42 | 0.41 | 0.43 | 0.43 | 0.40 | 0.38 | 0.37 |
| internist | 0.37 | 0.37 | 0.35 | 0.35 | 0.36 | 0.36 | 0.36 | 0.35 |
| lung diseases | 0.30 | 0.30 | 0.29 | 0.30 | 0.28 | 0.28 | 0.29 | 0.30 |
| neurologist | 0.32 | 0.32 | 0.32 | 0.31 | 0.32 | 0.32 | 0.31 | 0.31 |
| obstetrics and gynecology | 0.25 | 0.26 | 0.27 | 0.26 | 0.26 | 0.26 | 0.26 | 0.26 |
| occupational medicine | 0.38 | 0.39 | 0.39 | 0.41 | 0.41 | 0.38 | 0.37 | 0.36 |
| oncologist | 0.38 | 0.42 | 0.39 | 0.36 | 0.38 | 0.38 | 0.35 | 0.33 |
| ophthalmologist | 0.33 | 0.32 | 0.32 | 0.33 | 0.32 | 0.33 | 0.31 | 0.31 |
| otolaryngology | 0.31 | 0.29 | 0.29 | 0.29 | 0.29 | 0.30 | 0.30 | 0.31 |
| pediatrician | 0.30 | 0.30 | 0.30 | 0.31 | 0.32 | 0.31 | 0.31 | 0.32 |
| psychiatrist | 0.31 | 0.32 | 0.31 | 0.30 | 0.30 | 0.31 | 0.31 | 0.31 |
| radiologist | 0.32 | 0.32 | 0.32 | 0.31 | 0.32 | 0.31 | 0.32 | 0.32 |
| surgeon | 0.29 | 0.29 | 0.28 | 0.28 | 0.28 | 0.28 | 0.28 | 0.28 |
| Types of Healthcare Human Resources | Theil Index | Contribution Rate | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Poland | Central | South West | North West | South | North | East | Within Groups | Among Groups | |
| dentist | 0.171 | 0.009 | 0.006 | 0.431 | 0.012 | 0.001 | 0.003 | 47.25% | 52.75% |
| pharmacist | 0.079 | 0.002 | 0.004 | 0.012 | 0.000 | 0.015 | 0.012 | 10.16% | 89.84% |
| physician | 0.093 | 0.000 | 0.000 | 0.019 | 0.000 | 0.002 | 0.002 | 3.75% | 96.25% |
| nurse | 0.088 | 0.001 | 0.000 | 0.003 | 0.000 | 0.005 | 0.001 | 1.71% | 98.29% |
| specialist in general | 0.009 | 0.000 | 0.000 | 0.023 | 0.001 | 0.004 | 0.002 | 52.56% | 47.44% |
| anesthesiologist | 0.010 | 0.002 | 0.002 | 0.002 | 0.006 | 0.007 | 0.016 | 59.89% | 40.11% |
| cardiologist | 0.040 | 0.006 | 0.000 | 0.023 | 0.001 | 0.018 | 0.015 | 25.80% | 74.20% |
| dermatologist | 0.028 | 0.002 | 0.000 | 0.113 | 0.013 | 0.007 | 0.008 | 83.84% | 16.16% |
| family medicine | 0.054 | 0.000 | 0.001 | 0.126 | 0.018 | 0.002 | 0.031 | 54.69% | 45.31% |
| internist | 0.022 | 0.007 | 0.003 | 0.013 | 0.003 | 0.002 | 0.004 | 24.05% | 75.95% |
| lung diseases | 0.011 | 0.004 | 0.003 | 0.010 | 0.002 | 0.006 | 0.007 | 46.71% | 53.29% |
| neurologist | 0.019 | 0.009 | 0.001 | 0.006 | 0.006 | 0.000 | 0.008 | 29.54% | 70.46% |
| obstetrics and gynecology | 0.012 | 0.003 | 0.022 | 0.032 | 0.002 | 0.018 | 0.001 | 92.78% | 7.22% |
| occupational medicine | 0.054 | 0.000 | 0.005 | 0.044 | 0.035 | 0.073 | 0.083 | 75.03% | 24.97% |
| oncologist | 0.039 | 0.031 | 0.033 | 0.006 | 0.001 | 0.017 | 0.028 | 46.80% | 53.20% |
| ophthalmologist | 0.022 | 0.001 | 0.001 | 0.064 | 0.017 | 0.003 | 0.008 | 72.12% | 27.88% |
| otolaryngology | 0.017 | 0.002 | 0.003 | 0.031 | 0.008 | 0.010 | 0.026 | 78.58% | 21.42% |
| pediatrician | 0.016 | 0.006 | 0.003 | 0.005 | 0.001 | 0.006 | 0.007 | 28.94% | 71.06% |
| psychiatrist | 0.016 | 0.002 | 0.001 | 0.012 | 0.001 | 0.010 | 0.009 | 36.83% | 63.17% |
| surgeon | 0.007 | 0.000 | 0.003 | 0.015 | 0.002 | 0.007 | 0.005 | 72.44% | 27.56% |
| radiologist | 0.019 | 0.001 | 0.087 | 0.007 | 0.011 | 0.017 | 0.005 | 83.88% | 16.12% |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rój, J. Inequality in the Distribution of Healthcare Human Resources in Poland. Sustainability 2020, 12, 2043. https://doi.org/10.3390/su12052043
Rój J. Inequality in the Distribution of Healthcare Human Resources in Poland. Sustainability. 2020; 12(5):2043. https://doi.org/10.3390/su12052043
Chicago/Turabian StyleRój, Justyna. 2020. "Inequality in the Distribution of Healthcare Human Resources in Poland" Sustainability 12, no. 5: 2043. https://doi.org/10.3390/su12052043
APA StyleRój, J. (2020). Inequality in the Distribution of Healthcare Human Resources in Poland. Sustainability, 12(5), 2043. https://doi.org/10.3390/su12052043





